Abstract
Physiological processes in facial development show that cleft lip and palate (CLP) malformations are not defect malformations but dislocation malformations. The consideration of these processes and their integration into an operative concept significantly improve the growth of the midface and nose in CLP malformations and outcomes. An understanding and adoption of these concepts has the potential to consolidate optimal outcomes in LMICs.
Keywords: CLAP malformation, Dislocation malformation, Functional reconstruction, Primary rhinoplasty, Facial growth chromatography
1. Unilateral CLAP
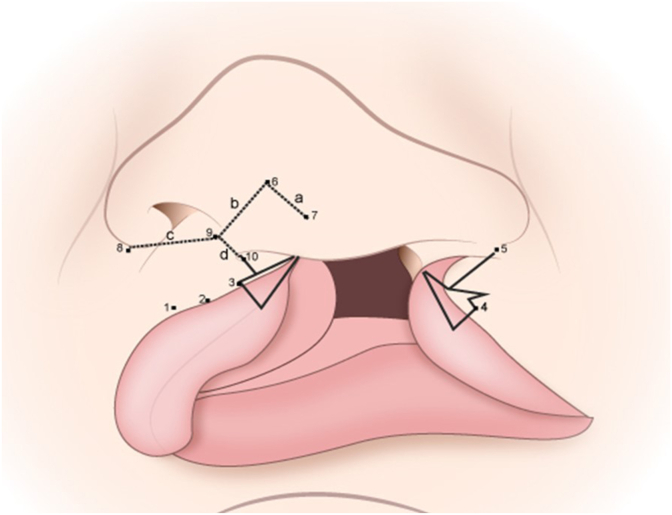
The incision in the upper lip is not made as usual through all layers of the upper lip, but in such a way that the skin is dissected from the muscles (Fig. 1). After intraoral incision, the soft tissue becomes strictly subperiostal, mobilized with the muscles up to the zygomatico-nasal suture around the nose to the bridge of the nose and to the top of the dome. This is followed by primary rhinoplasty with mobilization of the alar cartilage, the nasal septum up to the triangular cartilage without opening the perichondrium and is restricted to the cleft side. With intranasal incisions at the medial and lateral nasal floor, the soft tissue and nose can be completely detached from the skeleton and then be re-orientated. After the entire nasal floor has been closed, the nasal, midface and orbicularis muscles are reconstructed. Intraoral vestibuloplasty is performed together with a gingivoplasty of the alveolar cleft (Fig. 2).
Fig. 1.
Incision design unilateral CLAP.
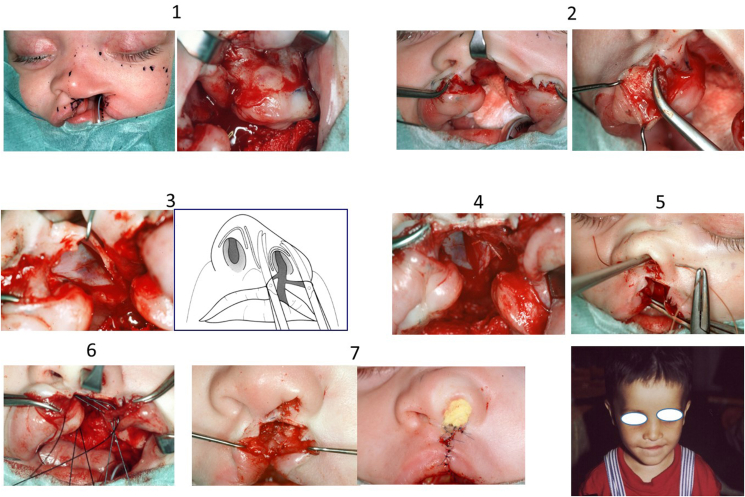
Fig. 2.
Operative procedure lip and nose unilateral CLAP.
2. Bilateral CLAP
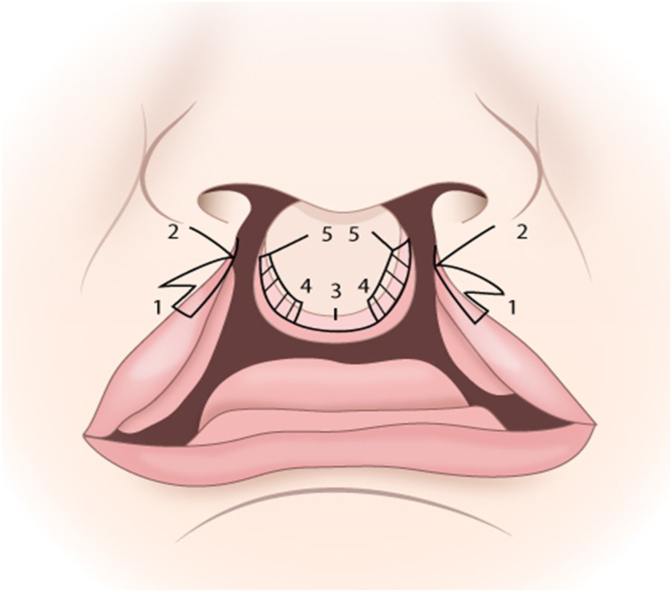
The design of the incision must take into account that lip closure is performed only from the lateral side and does not involve premaxillary skin and mucosa. Accordingly, our planning is not based on the frequently used philtral points, but points that are displaced medially to the point where the philtrum edge lowers and tapers out. This point corresponds exactly to the median plane and thus the maximum concavity of the Cupid's bow (Fig. 3).
Fig. 3.
Incision design bilateral CLAP.
A further incision runs from the ala of the nose to the vermilion, then turns laterally to form a triangle comparable to the incision according to Veau/Delaire.1 This is done symmetrically on both lateral halves of the lip. The premaxillary incision runs from the basal point of the columella to the vermilion and from there to both philtral points in the usual manner (these are maintained for safety reasons if ever median closure of the lip is not possible). In the vermilion area, separation is carried out in such a way that the inside of the prolabium with elements of the lip vermilion are mobilized, resulting in division of the prolabium into cutaneous and mucosal areas. Next, a sparing excision of the lateral prolabial mucosa is done. It is imperative that the incision is limited only to the skin and does not in any way damage the underlying muscles. Meticulous dissection, both in the region of the orbicularis oris and of the paranasal mimic muscles, is essential. Next, in order to achieve sufficient mobilization, a wide subperiosteal dissection is performed. The aim is to detach the whole soft tissue mask. including the nose. from the skeleton thus making re-orientation of the facial soft tissues possible. In contrary to commonly used surgical techniques, the soft tissue mobilization must be subperiosteal to avoid the destruction of the periosteum and detachment of its blood supply which would otherwise result in severe growth deficits, as Knese et al. has demonstrated.2
Primary rhinoplasty is then carried out in a way that mobilizes only the nose from the skeleton and the skin from the cartilaginous part, but does not free the perichondrium in the region of the nasal cartilages(Fig. 1). After such a complete mobilization, the nasal floor can be closed on both sides to the furthermost dorsal point. Following this, the alar and triangular cartilages of the nose are repositioned and good positioning of the nose is achieved through meticulous reconstruction of the paranasal musculature with attachment to the base of the nasal septum (Fig. 4a–d). This is followed by a stepwise closure of the orbicularis oris muscle up to the nasal spine (Fig. 4e–i). Intraoral mobilization of the prolabial mucosa thus creates a vestibule. The next stage is intraoral closure of the lip, with bilateral coverage of the cleft alveolus and creation of a median vestibule using prolabial mucosa. Skin closure is carried out in such a way that initially the philtrum is joined in the median plane. Then the lower third of the prolabial skin, including the red lip/white lip margin is excised. The skin in the median plane is sutured stepwise with Y sutures only in the cranial third of the nasal base. Fig. 5 shows the situation after 6 months.
Fig. 4.
One-step operation bilateral CLAP.
a: muscle dissection b: dissection skin and mucosa premaxilla c: closure of nasal floor d: reconstruction of muscles of the midface e. Situation after muscle reconstruction f: reconstruction of orbicularis oris muscle g: gingivoplasty of the cleft alveolus h: situation before skin closure. i: closure of skin in the lip; columella skin not integrated.
Fig. 5.
Outcome after 6 months. Before palatal closure.
The entire hard and soft palate is repaired at the age of about 9 months. Usually the hard palate is closed using vomer flaps with minimal mobilization on both sides as described by Pichler,3 as well as a bridge flap method. This is not a problem as the closure of the nasal floor had already been extended as far dorsally as possible during closure of the lip. In the region of the soft palate, triangular excision of the mucosa on the posterior surface of the uvula is carried out, and after mobilization of the muscles, meticulous muscle reconstruction, especially of the palatoglossus and palatopharyngeus is performed, using the same technique as applied in unilateral CLAP.4
3. Results
In 2000, the author published in Oral and Maxillofacial Clinics of North America5 a comparison of 2 different treatment protocols for unilateral cleft lip and palate patients at the age of 7 years and 17 years. From amongst many parameters, it was found the nasal airflow quotients from cleft/non-cleft side was best with 0.85 in the group treated with the described physiological concept compared to 0.5 in the group with traditional treatment protocol.
Comparable differences were found in the aesthetic evaluation for the nose with the vertical position of the nose and the deviation of the nasal axis from the midsagittal plane. Most of the patients who had deviations between 0° and 1° were in the physiological concept group. The patients with most severe deviations all had significantly reduced nasal airflow and the nasal deviation correlated with the presence of symptoms of chronic maxillary sinusitis. The vertical alar base was with 0.9 more symmetric in the physiological concept group than the traditional group even after secondary rhinoplasty (0.82).
Evaluating the symmetry of the columella-tip complex and the transverse position of the alae, it was noted that the highest range of symmetrical alar-columellar complex was in physiological concept group. Most patients with the traditional protocol had appreciable deviations from the norm.
Analysis of the lateral photographs and showed all angles of physiological concept group came closest to the normal range. Cephalometric analysis showed that only 12% (6 patients) of the patients in physiological concept group had Class III relationship, in contrast to 80% (48 patients) of the traditional protocol. The detailed results were published in several different journals.4, 5, 6, 7
In a retrospective study8 with 78 patients with unilateral cleft lip and palate, 9 patients with bilateral cleft lip and palate and 47 patients with isolated cleft palate (cleft palate group) we performed profilometric measurements of the faces using an optical 3D scanner based on the strip projection technology. The control group consisted of 165 healthy volunteers. The asymmetry of the entire face, midface, nose and upper lip was objectively quantified using calculated symmetry indices. Local asymmetries were determined with the distances of medial and corresponding lateral landmarks to the plane of symmetry (Fig. 6).
Fig. 6.
Profilometrical study.8
The overall symmetry indices with the physiological concept group showed asymmetries of 1.26 mm for the unilateral, 1.40 mm for bilateral cleft group and 0.63 mm for cleft palate group in comparison to the normal control group.8 It must be noted, however, that even in the normal control group there are symmetry differences of 2.11 mm (Fig. 7).
Fig. 7.
Differences in facial symmetry.8
If one considers that differences of up to 2 mm are not perceived as noticeable,9 our study in the unilateral cleft group shows the side differences of 1.15 in the transverse distance of the lateral landmarks to the plane of symmetry is mostly not visible.
4. Discussion
Since 1980, we have carefully reconstructed the perinasal and perioral muscles with due regard to restoration of physiology and growth without any type of previous dentofacial orthopaedic or orthodontic treatment. Analyses of both the dental cast and the teleradiograph showed that the skeletal development in the group that underwent reconstruction of the perioral and perinasal muscles was better than in the group treated according to the more commonly used techniques, despite the fact that no orthopaedic growth stimulation was applied.5 A possible explanation for this improved skeletal growth of the midface may be that the immediate reconstruction and reorientation of the musculo-periosteal apparatus enables interaction between the primary and secondary growth centres, which in turn activates the normal physiological and growth stimuli and improves the development of the midfacial skeleton.10
Comparing the patients at 16.5 years of age, it also becomes clear that the overall midfacial growth is significantly better in patients who had muscular reconstruction than those with conventional surgery. One reason might be that functional disturbances are significantly reduced after muscular reconstruction.5 It is postulated that the careful reconstruction of the perioral and perinasal muscles combined with the restoration of the musculo-periosteal apparatus and the union of the primary and secondary growth centres is responsible for the better skeletal growth. An additional advantage is that the restoration of the functional units reduces the scar formation that is so often seen in the lip area. This in turn allows the maxilla to exercise its physiological forwards rotation during growth.4,6,7
If all functional units in patients with cleft lip and palate are not carefully restored during primary operation, severe scar formation in the anterior part of the face will hinder the normal development of the face.11 This means that the first lip operation will decide the fate of the cleft patient and if this operation is inadequate, orthopaedic treatment will not be able to improve skeletal growth. In this respect we agree with Ross12 who compared different treatments and came to the same conclusion. The goal of our surgical measures must therefore be the timely reconstruction of the functional units interrupted by the cleft formation to encourage normal development as early as possible.
Between 1995 and 2016, 2358 primary cleft patients, including 68 bilateral CLAP patients, underwent surgery by the author according to the described concept, with follow-up performed by a multidisciplinary CLAP team on a regular basis. In these special consulting sessions, the children were examined by oral and maxillofacial surgeons, otolaryngologists/audiologists, orthodontists and speech therapists. The clinical examinations included hearing assessment, speech assessment consisting of conventional speech/language evaluation, NasalView system analysis and, if necessary, nasendoscopy, as well as model analysis and cephalometric analysis according to Delaire.13,14 Hearing and speech/language assessments confirmed normal development of the children corresponding to the results in unilateral CLAP patient.14,15 Good alignment of the premaxilla, which before surgery had been in an anterior position, and good dental arch form, were achieved under the influence of the normalised musculature up to 6 years of age, with only one patient, with an extremely protrusive premaxilla, undergoing preoperative orthodontic treatment. Our results also showed good transverse development of the maxillary arch and good occlusion (Fig. 8). Sagittal midfacial growth was normal, and there were nearly normal cephalometric values (Table 1) (see Fig. 9).
Fig. 8.
Lateral X-ray.
Table 1.
Delaire analysis.
| Maxillary analysis | ||
|---|---|---|
| CF1 | -o,8 cm | Retrognathic Maxilla |
| CF4 | 3.28° | Posterior Rotation of Maxilla |
| C1 | −0,68 cm | Sagittal overdevelopment maxillary base |
| Mandibular analysis | ||
| C1 | −0.12 cm | Condyle to far dorsal to skullbase |
| C4 | 0.34 cm | Condyle to far dorsal to craniospinal articulation |
| C3 | 0.0° | Normal position |
| CF1 | −1.72 cm | Mandibular retrognathia to midface |
| CF2 | 27.05 cm | Prognathic mandible relative to skull |
| VF6 | 11.28° | Posterior rotation of mandibular body |
| CF3 | 297.07 | Anterior rotation of mandibular ramus |
| Cranial analysis | ||
| C2 | 0.38 cm | Slight reduction of skull height |
| Dental analysis | ||
| I | −0.04° | Slight reclination of maxillary incisors |
| I | −0.23° | Slight reclination of mandibular incisors |
| Li | −6.92° | Slight frontal inclination |
Fig. 9.
a+b:. Bilateral CLP. Facial and maxillary development after bilateral cleft lip and palate.
Bilateral CLP, same patient as in Fig. 8. Occlusion after bilateral cleft lip and palate, development over 17 years, orthodontic treatment, no corrective surgery.
It should also be noted that the development of the nose was clinically normal and that it was well shaped (Fig. 8) Orthodontic treatment, if required, was started before any alveolar bone grafting procedures, at the age of about 7 years, after eruption of the lateral incisors, as recommended by Semb et al.16
Our experience shows that, as is the case in unilateral CLAP, meticulous reconstruction of the facial units such as lip, nose, jaw, vestibule and palate can significantly improve the skeletal growth of the midface.5 Our patients did not usually have either preoperative or postoperative orthodontic treatment prior to the eruption of the first teeth of the permanent dentition at about 7 years of age, and there was no retropositioning of the maxilla. There was good alignment of the premaxilla and good maxillary arch dimensions. The commonly observed flattening and widening of the nose was avoided, which produced a better aesthetic outcome.
These results show that a surgical technique based on the physiology of growth encourages better normal growth than reconstructive techniques as applied in plastic reconstructive techniques for management of a defect. Furthermore, orthodontic treatment is easier and the treatment time shorter when the principles described here are followed. As both sides of the lip are closed within 3–4 months and the complete palate within 7–10 months, the number of surgical interventions, and thus the time of hospitalization, is reduced enormously. This is of psychological benefit to both the children and their parents.
These outcomes suggest the management of cleft lip and palate needs a completely new way of thinking and philosophy. In the past, all operative procedures were based on the false assumption that one needs to close a defect due to deficiency of different tissues, as seen after tumour surgery. As a consequence of this approach, many classic operative procedures use full thickness flaps to close the defect, such as the Millard17 or the Pfeiffer18 technique. These procedures result in multiple scars which have the potential for hindering normal growth and development. However, based on these developmental outcomes, we can show that with careful preservation and restoration of all existing muscles and other related soft tissues, normal growth can be achieved. Consequently, one should no longer consider cleft lip and palate a defect but a dislocation malformation since all the normal structures exist and can be restored.
5. Conclusion
Physiological processes in facial development show that CLAP malformations are not defect malformations but dislocation malformations. The consideration of these processes and their integration into an operative concept significantly improve the growth of the midface and nose in CLAP malformations and lead to optimal outcomes. Transfer of these concepts will enable surgeons in low resource situations to achieve results that will require no or minimal revision and the attendant costs.
Authors’ contributions
The author contributed solely to the article.
Financial support and sponsorship
None.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2020.
Declaration of competing interest
The author declared that there are no conflicts of interest.
References
- 1.Veau V., Recamier J. Masson; Paris: 1938. Bec-de-lievre. Formes Cliniques-Chirurgie. (in French) [Google Scholar]
- 2.Knese K.H., Geidel H. Size, surface and volume of cell nuclei in the periosteum. Z Mikr Anat Forsch. 1972;85:223–244. [PMID: 4672849] (in German) [PubMed] [Google Scholar]
- 3.Pichler H. [Surgical Methods in bilateral total palatal clefts] Zentralbl Chir. 1927;54:860. in German) [Google Scholar]
- 4.Joos U. Evaluation of the result of surgery on cleft lip and palate due to skeletal growth determinants of the cranial base. J Craniomsaxillofac Surg. 1989;17(Suppl 1):23–25. doi: 10.1016/s1010-5182(89)80034-4. [PMID: 2606983. [DOI] [PubMed] [Google Scholar]
- 5.Joos U. Long-term results after repair of unilateral cleft lip alveolus and palate. Oral Maxillofac Surg Clin. 2000;12:3. [Google Scholar]
- 6.Joos U. Skeletal growth after muscular reconstruction for cleft lip, alveolus and palate. Br J Oral Maxillofac Surg. 1995;33:139–144. doi: 10.1016/0266-4356(95)90285-6. [PMID: 7654656. [DOI] [PubMed] [Google Scholar]
- 7.Joos U. Muscle reconstruction in primary cleft lip surgery. J Cranio-Maxillo-Fac Surg. 1989;17(Suppl 1):8–10. doi: 10.1016/s1010-5182(89)80029-0. [PMID: 2606989. [DOI] [PubMed] [Google Scholar]
- 8.Rako I. University of Münster; 2013. Quantitative Symmetry Analysis of the Face in Patients with Cleft Lip, Alveolus and Palate. [dissertation] [Google Scholar]
- 9.Pfeifer G., Schmitz R., Gundlach K., Herwerth-Lenck M. In: Craniofacial Abnormalities and Clefts of the Lip, Alveolus and Palate. Pfeifer G., editor. Thieme; Stuttgart: 1991. Long-term results following primary lifting of the nose and labioplasty according to the waveline procedure in bilateral symmetrical clefts of the lip, alveolus and palate; p. 320. [Google Scholar]
- 10.Anastassov G.E., Joos U. Comprehensive management of cleft lip and palate deformities. J Oral Maxillofac Surg. 2001;59:1062–1075. doi: 10.1053/joms.2001.25852. [PMID: 11526580. [DOI] [PubMed] [Google Scholar]
- 11.Göz G., Joos U., Schilli W. The influence of lip function on the sagittal and transversal development of the maxilla in cleft patients. Scand J Plast ReConstr Surg Hand Surg. 1987;21:31–34. doi: 10.3109/02844318709083576. [PMID: 3589576. [DOI] [PubMed] [Google Scholar]
- 12.Ross R.B. Treatment variables affecting growth in unilateral cleft lip and palate. Cleft Palate J. 1987;24:5–77. [PMID: 3542303] [PubMed] [Google Scholar]
- 13.Delaire J. Architectural and structural craniofacial analysis (lateral view). Theoretical principles. Some example of its use in maxillofacial surgery. Rev Stomatol Chir Maxillofac. 1978;79:1–33. [PMID: 276904] (in French) [PubMed] [Google Scholar]
- 14.Löhle E., Joos U., Göz G. Pfeifer G: Craniofacial Abnormalities and Clefts of the Lip, Alveolus and Palate. Thieme; Stuttgart: 1991. Phoniatric results following reconstruction of palatoglossus and palatopharyngeus muscles; pp. 393–395. [Google Scholar]
- 15.Joos U., Wermker K., Kruse-Löesler B., Kleinheinz J. Influence of treatment concept, velopharyngoplasty, gender and age on hypernasality in patients with cleft lip, alveolus and palate. J Cranio-Maxillo-Fac Surg. 2006;34:472–477. doi: 10.1016/j.jcms.2006.07.858. [PMID: 17157520. [DOI] [PubMed] [Google Scholar]
- 16.Semb G., Bergland O., Abyholm F. Significance of secondary osteoplasty in orthodontic treatment of facial cleft patients. Fortschr Kieferorthop. 1986;47:519–528. doi: 10.1007/bf02164531. PMID: 3549487. (in German) [DOI] [PubMed] [Google Scholar]
- 17.Millard D.R., Latham R., Huifen X., Spiro S., Morovic C. Cleft lip and palate treated by presurgical orthopedics, gingivoperiosteoplasty, and lip adhesion (POPLA) compared with previous lip adhesion method: a preliminary study. Plast Reconstr Surg. 1999;103:1630–1644. doi: 10.1097/00006534-199905060-00009. [PMID: 10323695. [DOI] [PubMed] [Google Scholar]
- 18.Pfeifer G. [An embryologically based method for the repair of cleft lips] Dtsch Zahn Mund Kieferheilkd. 1970;54:69–77. [PMID: 4913615] (in German) [PubMed] [Google Scholar]