Abstract
Introduction:
The COVID-19 pandemic has had a devastating worldwide effect on mental health. Recent studies correlate the spreading of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) with symptoms of depression, most prominent in postpartum women. Our systematic literature review scope is to identify the risk factors and predictors for postpartum depression (PPD) and describe the steps that should be taken to help postpartum women. This study will help clinicians, researchers, and policymakers to elucidate the predictors of PPD during this pandemic and prevent these adverse outcomes in future crises.
Methods:
We conducted a systematic search by employing databases PubMed, Google Scholar, Scopus, and Embase to identify articles published before March 2021. About 463 publications were generated during our search process and from those, 36 were reviewed, summarized, and synthesized. Studies qualified the criteria if they (1) utilized qualitative or quantitative design, (2) explored the risk factors for PPD, and (3) were written in English. Quality evaluation of each study was achieved by using criteria set by Lincoln and Guba.
Results:
Prevalence of depression symptoms ranged from 7% to 80.8% in postpartum women during the SARS-COV 2 pandemic. The risk factors for PPD were classified into 6 major categories: socio-demographic, psychological, pre-existing pathology, metabolic factors, previous events of miscarriage, and media misinformation.
Conclusion:
It is extremely vital to care for women’s mental health during pregnancy and after childbirth during these unprecedented times. This review urges the need to design adequate interventions for this vulnerable population to prevent negative consequences of PPD.
Keywords: postpartum depression, postnatal depression, women, anxiety, COVID-19, sars-cov-2, mental health
Introduction
Coronavirus disease is caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), a virus belonging to the Coronaviridae family. The COVID-19 pandemic, which began to spread worldwide in early 2020, has led to a myriad of unexpected challenges, affecting people physically, mentally, emotionally, and economically. Many of the hard-hit countries have taken very stringent measures, such as total lockdowns, in an attempt to limit the spread of SARS-COV-2. The lack of general support during these tough times due to social distancing and quarantine measures, the stigma associated with the virus, and a prevailing sense of fear and uncertainty have caused or worsened mental health issues such as depression, anxiety, stress, frustration, phobias, obsessive-compulsive symptoms, and post-traumatic stress disorder (PTSD) among the general populations. 1
Essentially, people worst affected by the adverse mental and psychological effects of this pandemic are those with pre-existing physical or mental health problems, the elderly, victims of sexual violence, people going through domestic or substance abuse, people living in poverty, refugees, and immigrants, and hospitalized patients. 2 Another major group significantly affected by the pandemic is pregnant and postpartum women. The process of childbirth in itself encompasses many biological, psychological, and social adjustments. That, coupled with the emotional distress brought on by the COVID 19 pandemic puts postpartum females at an increased risk of mental health issues, especially depressive symptoms.
Postpartum depression (PPD) is the depression suffered by a mother following childbirth, typically arising from the combination of hormonal changes, psychological adjustment to motherhood, and fatigue; postnatal depression. 3 The CDC reports that about 1 in 8 women experience symptoms of PPD in the USA. 3 Although there has been a multitude of developments in the management of PPD, it is still an underdiagnosed condition. In 2014, a US survey of 1400 women revealed that 40% of people with symptoms of PPD did not seek help and the reasons cited for the same were shame, guilt, and stigma of mental illness. One of the main reasons cited for underreporting was the stigmatization of mental illness during the COVID-19 pandemic was the barrier to diagnosis and treatment. 4 PPD not only impacts the mother’s life and overall functioning but also was noted to increase the odds of delays in language skills, including the production of voices in dialog (OR = 1.86, 95% CI: 1.39-2.49) and speaking 2 to 3 words (OR = 1.22, 95% CI: 1.13-1.35) in children. PPD is also associated with 1.5 times increased odds of delays in personal-social skills.5,6
This systematic review assesses the effect of the COVID-19 pandemic on the mental health of postpartum women, with a focus on the risk factors during the pandemic that increased levels of depression in new mothers.
Methods
Literature Search
Literature review related to postpartum depression was examined through a search of peer-reviewed articles and followed PRISMA guidelines. 7 The databases PubMed, Scopus, Google Scholar, and Embase were searched by using the following terms: “COVID 19,” “Sars-Cov-2,” “Coronavirus,” “Postpartum Depression,” “Postpartum,” “Postpartum depression lockdown.” In total, 463 publications were generated during our search process. The titles and abstracts of all records were reviewed to determine if they met inclusion criteria. Authors S.U and S.J screened all abstracts and full texts for eligibility.
Inclusion and Exclusion Criteria
Inclusion criteria were (1) Covid 19 pregnancy, (2) Mental health impacts during the postpartum period, pp depression, pp blues, (3) Observational Studies, RCTs, (4) Articles in English, and (5) No limitation to age, country. We omitted systematic reviews, meta-analyses, letters to editors, and commentaries.
Review and Data Extraction
Three reviewers (S.U, E.G, W.S) independently extracted data about studies, and the articles that met inclusion criteria were reviewed in full and the following data were extracted, if available: (a) socio-demographic indicators; (b) psychological factors; (c) pre-existing pathologies; (d) metabolic factors; (e) previous miscarriage; and (f) media coverage. The assessment was done at the study level and focused on the main study outcome.
Quality Evaluation
Quality evaluation was achieved by using criteria set out by Lincoln and Guba (1985). 8 Each study was evaluated on the degree of credibility, transferability, dependability, confirmability. We used a 1- to 5-point scale for the process of evaluation; with 1 indicating very little confirmation to support the criterion and 5 indicating strong confirmation to support the criterion. This process was done independently by 4 different authors.
Results
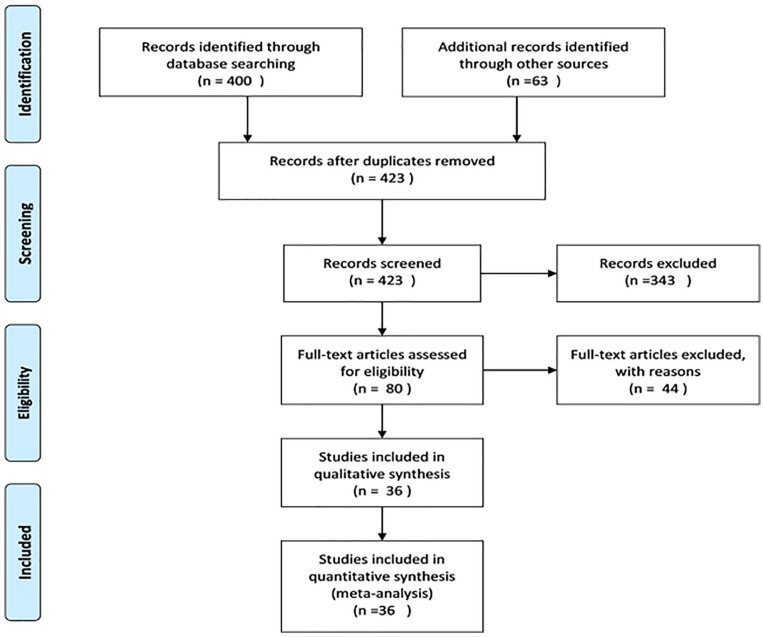
Of the 463 studies initially identified during the search process, 36 studies were included in this systematic review (Figure 1). All the included studies were observational, ranging from cross-sectional to cohort studies.
Figure 1.
PRISMA flowchart.
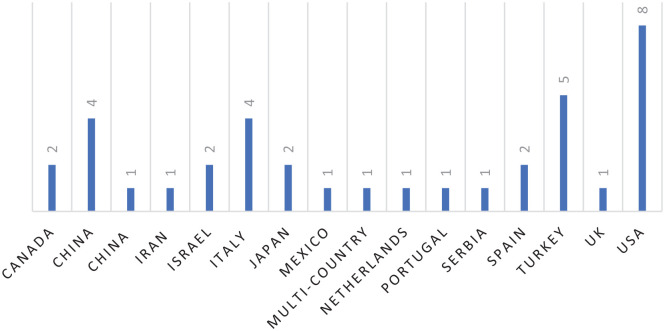
The total number of women identified was 35 424 in number (Table 1). The highest representation of countries was noted for the United States (n = 8), followed by Turkey (n = 5), and Italy/China (n = 4) (Figure 2).
Table 1.
Characteristics of included studies.
| Author; country | Design | Sample size | Time of PPD | Mean level of depressive symptomatology |
|---|---|---|---|---|
| Liang et al 24 ; China | Cross-sectional | 253 PPD (S.N = 845) | 6-12 week | EPDS = 10; P = 30% |
| Ostacoli et al 4 ; Italy | Cross-sectional | 163PPD (S.N = 268) | 3 months | P = 44.2% B.P; P = 42.9% A. P |
| Pariente et al 10 ; Israel | Cohort study | 346 | 2 months | P = 31.3% B.P; P = 16.7% A. P |
| Silverman et al 22 ; US | Cohort study | 516 | <5 month | 64 women (12.4%) EPDS ≥ 9, and 33 women (6.4%) EPDS ≥ 12 |
| An et al 14 ; China | Cross-sectional | 209 | 3 months | P = 56.7% EPDS = 10. |
| Suárez-Rico et al 37 ; Mexico | Cross-sectional | 293 | 4-12 weeks | P = 39.2% |
| Spinola et al 6 ; Italy | Cross-sectional study | 243 | 1 month | P = 44% |
| Stojanov et al 16 ; Serbia | Cross-sectional study | 108 | <1 month | P = 14.8%; EPDS > 10 |
| Shayganfard et al 15 ; Iran | Cross-sectional study | 103 PPD (S.N = 120) | No longer than 6 weeks | P = 36% |
| Fallon et al 12 ; UK | Cross sectional study | 614 | 12 weeks | P = 43%; EPDS > 10 |
| Ayaz et al 17 ; Turkey | Cross-sectional | 63 | N/A | IDAS = 202.6 ± 52.9 B.P; IDAS = 184.8 ± 49.8; P = 38.7% mild PPD;P = 60% severe PPD |
| Perzow et al 29 ; USA | Longitudinal analysis | 135 | N/A | P = 30%; EPDS = 10 |
| Zhou et al 34 ; China | Cross-sectional | 859 | N/A | OR = 0.23; 95% CI: 0.12-0.45; P < .001 |
| Ravaldi et al 13 ; Italy | Cross-sectional | 2448 | N/A | P = 9.6% |
| Guvenc et al 23 ; Turkey | Cross-sectional | PPD 212 | 1 month | P = 34% EPDS > 13 |
| Durankuş and Aksu 21 ; Turkey | Cross-sectional | PPD 260 | N/A | EPDS > 13%; P = 35% |
| Ceulemans et al 18 ; Multinational | Cross-sectional | PPD 9041 | N/A | EPDS ≥ 13 P = 15% in the pregnancy cohort 13% the breastfeeding cohort |
| Zanardo et al 38 ; Italy | Case-control | PPD 192 | N/A | P = 26%; EPDS > 13% |
| Liu et al 19 ; USA | Cross-sectional | 1123 | N/A | P = 36.4% |
| Farewell et al 39 ; USA | Mixed methods pilot study | 31 | N/A | PHQ-2 = 3; P = 12% |
| Mariño-Narvaez et al 40 ; Spain | Cross-sectional study | 162 | 1 month | χ2 = 4.31; P = 38% |
| Bo et al 30 ; China | Cross-sectional study | 359 PPD (S.N 1309) | 1 week | P = 27.43% |
| Chaves et al 25 ; Spain | N/A | 158 PPD (SN 274) | N/A | P = 58% |
| Hiiragi et al 33 ; Japan | Retrospective study | 279 | 3 months | OR = 1.48 |
| Masters et al 47 ; USA | Cross-sectional study | 131 PPD (Sample n = 163) | >3 months | P = 80.8% |
| Suzuki et al 41 ; Japan | N/A | 39 PPD (S.N 132) | <1 month | P = 39% |
| Koyuncu et al 20 ; Turkey | Cross-sectional study | 360 PPD (S. N = 900) | N/A | EPDS score > 13; P = 40.7% |
| Boekhorst et al 32 ; Netherlands | Longitudinal prospective cohort study | 268 | 2 months | (IQR = 5) in the first trimester, (IQR = 6) in the second trimester, (IQR = 6) in the third trimester |
| Davenport et al 28 ; Canada | Cross-sectional study | 360 PPD (S. N = 900) | <1 month | EPDS score > 13; P = 40.7% |
| Racine et al 42 ; Canada | Cohort | 3387 | 3 months | The mean depression score (8.31, 95% CI: 7. 97-8.65); 2.30 points (95% CI: 1.95-2.65) at the COVID-19 |
| Kinser et al 27 ; USA | Cross-sectional observational study | 2435 | 2 months | P = 12% |
| Fernandes et al 43 ; Portugal | Review | 567 | N/A | P = 27.5% |
| Li et al 44 ; China | Cross-sectional study | 2201 | 2 months | P = 36.3% |
| Gluska et al 45 ; Israel | Multicenter prospective cohort study | 421 | N/A | EPDS = 8; P = 23% |
| Oskovi-Kaplan et al 46 ; Turkey | Survey | 223 | N/A | EPDS = 33; P = 14.7% |
| Basu et al 26 ; USA | Online, cross-sectional survey | 7562 | 3 months | P = 30% |
Abbreviations: A.P, after pandemic; B.P, before pandemic; P, prevalence; PPD, postpartum depression; SZ, sample size.
EPDS (The scale has 10 self-reported questions, rated on a 4-point Likert scale which are scored from 0 to 3. The scale is scored between 0 and 30 and the cut-off point of 13 or higher scores are considered as the probable risk for the presence of postpartum depression); PHQ (Patient Health Questionnaire score is 16. Scores of 5, 10, 15, and 20 represent cut points for mild, moderate, moderately severe and severe depression, respectively. Sensitivity to change has also been confirmed.).
Figure 2.
Countries of origin for all included studies.
Our study has explored (1) the mean level of depressive symptomatology of post-partum women over time, (2) the prevalence of depression after the postpartum period, (3) risk factors that predict the course of PPD (Table 2).
Table 2.
Risk Factors for postpartum depression during the COVID-19 pandemic.
| Author; country | Risk factors | Risk categories |
|---|---|---|
| Perzow et al 29 ; USA | Low income | Socio-demographic |
| Racine et al 27 ; Canada | ||
| Spinola et al 6 ; Italy; Stojanov et al 16 ; Serbia | Self/partner unemployment due to Covid-19 | |
| Liang et al 24 ; China | Immigrant women | |
| Bo et al 30 ;China | Women in western and central China | |
| Masters et al 46 ; USA | Participants of color (Black, Asian, Multiracial, and/or Hispanic/Latinx) | |
| Spinola et al 6 ; Italy; Shayganfad et al 15 ; Iran | Concerns about self/family contracting Covid-19; Covid-19 lockdown; Strict Covid-19 protocols | Psychological |
| Guvenc et al 23 ; Turkey | Worrying about future | |
| Ostocoli et al 4 ; Italy; Mariño-Narvaez et al 40 ; Spain | Perceived pain during birth, childbirth stress | |
| Liang et al 24 ; China; Stojanov et al 16 ; Serbia; Farewell et al 39 ; USA; Mariño-Narvaez et al 32 ; Spain; Koyuncu et al 32 ; Turkey | Poor social support/single | |
| An et al 14 ; China | Perceived stress | |
| Stojanov et al 16 ; Serbia; Fallon et al 12 ; UK; Perzow et al 29 ; USA; Durankus and Aksu 21 ;Turkey; | Social isolation/social distancing/loneliness | |
| Perzow et al 20 ; USA; Koyuncu et al 32 ; Turkey; Davenport et al 42 ; Canada; Fernandes 44 ; Portugal | Social isolation/social distancing/loneliness | Psychological |
| Ostocoli et al 4 ; Italy; Stojanov et al 16 ; Serbia | Dismissive and fearful avoidant attachment styles/emotional problems | |
| Masters et al 46 ; USA; Li et al 45 ; China; Ceulemans et al 18 ; Multinational | Pre-existing psychiatric illness | Pre-existing pathology |
| Gluska et al 46 ; Israel | Maternal disability | |
| Ayaz et al 17 ; Turkey | BMI/obesity | Metabolic factors |
| Ostocoli et al 4 ; Italy | Younger age 33-36 | |
| Stojanov et al 16 ; Serbia | Age > 35 | |
| Ceulemans et al 18 ; Multinational | Smoking | |
| Liang et al 24 ; China | Fever | |
| An et al 14 ; China; Spinola et al 6 ; Italy | History of abortion | Previous events |
| Kinser et al 43 ; USA; Basu et al 26 ; USA | Lack of proper information | Social media |
| Shayganfad et al 15 ; Iran; Bo et al 30 ; China | Postponed/canceled medical appointments | Others |
| Ayaz et al 17 ; Turkey; Koyuncu et al 32 ; Turkey | Relationship with spouse | |
| Ceulemans et al 18 ; Multinational | Unplanned pregnancy |
Mean Level of Depressive Symptomatology
Nine studies12,16,18,23,26,32,38,42,46 (Table 1)—explored mean depression levels in the postnatal period. Follow-up in these studies ranged from 4 weeks to 3 months. One study 34 found that there is a statistically significant decrease, while in contrary 5 studies14,24,29,34,39,46 described a decrease but did not calculate statistical significance. In 5 studies,18,23,26,32,38,42 the mean level of depression decreased to below the cutoff value for depression defined in each study.
In conclusion, depression levels do not always decrease below the cutoff, however, the decrease is not always statistically significant. In addition, the standard deviations are relatively high, which represent a change in depression levels within a sample is highly variable, proposing that depressed mothers cannot be considered a homogeneous group.
Prevalence of PPD Period
Studies suggest that 14.8% to 40.7% (median = 35%) of mothers with PPD still met criteria for major depression with EPDS > 13 at less than 3 month (n = 8 studies12,16,18,20,21,23,28,38 ); 27.4% at 1 week (n = 1 study 30 ) 38% to 44% (median = 39%) at 1 month (n = 3 studies6,40,41); 30% to 39% (median = 36%) at 4 to 12 weeks (n = 3 studies15,24,47); 12% to 36.3% (median 23.3%) at 2 months (n = 4 studies4,27,32,44 ); and 30% to 80% (median = 33%) at 3 months (n = 6 studies4,14,22,26,42,46); 9.6% to 60% (median = 27%), duration of months is not applicable (n = 11 studies13,17,19,25,29,34,39,43,45,46), 12.4% at <5 months (n = 1 study 22 ). Overall, these findings suggest that at any time point between 1 week and <5 months postpartum, about 27% of mothers diagnosed with PPD still meet criteria for depression.
Risk Factors That Predict the Course of PPD
Various risk factors were identified across the included studies. These included first, sociodemographic risk categories, addressing (1) low income, (2) self/partner unemployment due to COVID-19, (3) immigrant status, (4) women in Western and Central China, and (5) participants of color (Black, Asian, Multiracial, and/or Hispanic/Latinx). Second, psychological risk categories addressing (1) concerns about self/family contracting COVID-19/COVID-19 lockdown/strict COVID-19 protocols, (2) worrying about the future, (3) perceived pain during birth; childbirth stress, (4) poor social support; no close family member or spouse, (5) perceived stress, (6) social isolation/social distancing/loneliness, and (7) dismissive and fearful-avoidant attachment styles/emotional stressors. Third, pre-existing pathologies including (1) pre-existing psychiatric illness, and (2) maternal disability. Fourth, metabolic factors including (1) BMI/Obesity, (2) age group of 33 to 36, (3) age >35, (4) smoking, and (5) fever. Fifth, previous events such as a history of abortion. Sixth, misinformation due to social media. Finally, other factors such as (1) postponed/canceled medical appointments, (2) relationship with spouse, and (3) unplanned pregnancy (Table 2).
Discussion
During the early months of the pandemic, not much was known about the management strategies for pregnant and postpartum women. With most of the medical resources being directed toward the care of COVID-19 infected patients, there was uncertainty among pregnant women and new mothers of receiving timely care.
Childbirth is noted to be a challenging journey for a woman as there are abrupt and dramatic changes in the woman’s body physiologically as well as anatomically. The potential role of hormonal variations on a woman’s mood in the postpartum period, particularly considering estrogen, progesterone, testosterone, prolactin, and thyroxine has been studied. It is noted that roughly about 14% of women experience depressive moods during the early postpartum period. Women have reported having noticed the peripartum mood changes from the time of the onset of delivery up to 4 weeks of postpartum. It is during this period where women are at heightened vulnerability to feel depressed. The spectrum of peripartum mood changes varies from the mother feeling fatigued, tearful, and being overwhelmed with the unfolding of new responsibilities.9,28
A review of our selected studies found that some common risk factors for developing PPD or anxiety included maternal factors like preexisting chronic autoimmune diseases, gestational diabetes, preeclampsia, 10 histories of abortion or pregnancy loss,6,13,14 higher maternal age,15,16 obesity, 17 events of the pregnancy being unplanned. 18
A history of mental illness was also strongly associated with developing postpartum depression, anxiety, or PTSD.19,20 It was observed that mothers with lower social support from family or friends, single mothers, strained marital relationships, 17 higher number of children,15,21 immigrants, lower-income families,16,20,22 and working women, 23 victims of domestic abuse or who do not have access to protective services also had higher levels of PPD and anxiety.6,24
Complications during delivery or admission of newborn to the neonatal intensive care unit,6,20 lack of support in breastfeeding, 25 early use of formula, 12 were also associated with higher levels of PPD and anxiety.
The COVID-19 pandemic has also had an impact on the mental health of new mothers. Mothers who were infected by the virus during the peripartum or postpartum period, or who lived with or were in close contact with people infected with COVID-196,15 showed higher levels of PPD and anxiety. It was observed that these fears were exacerbated by excessive information from external sources like social media messages, news, or well-meaning friends and family found that increased media consumption led to increased levels of anxiety.26,27
The effect of lockdowns and social distancing during the pandemic has also played a role in the higher-than-normal levels of mental health issues in new mothers. Reduced physical activity during pregnancy, 28 boredom, and feeling of isolation, 29 loss of job or housing, 6 missing medical appointments due to lack of transport or city shutdowns, fear of visiting hospitals during the pandemic, lack of a support person during delivery, changes in delivery plan, worrying about family being unable to visit after delivery, absence of childcare facilities, lack of postpartum health care, have all contributed to increased anxiety and depressive symptoms in postpartum women. 26
The fear of the baby or themselves contracting the virus in the hospital was a common cause of PPD and anxiety found in multiple studies.21,29-31 On the other hand, the show of support, empathy, and kindness by the attending hospital staff and the ability to rest due to quietness in the wards are protective against depression. 4
Our review also found, that in contrast, Boekhorst et al 32 reported that during the pandemic, higher levels of maternal stress during pregnancy were found, but there was no increase in depressive levels during pregnancy, nor any increase in stress or depressive levels in the postpartum period. Pariente et al and Silverman et al also found that delivering during the COVID-19 pandemic was independently associated with a lower risk of postpartum depression. Hiiragi et al found no apparent increase in maternal psychological stress due to the COVID-19 pandemic in Yokohama, Japan. A study conducted in China by Zhou et al even found that pregnant women show less depression, anxiety, insomnia, and PTSD symptoms than non-pregnant women during the pandemic.10,22,32-34
Postpartum depression is still a poorly addressed medical issue, as the emphasis is laid mostly on the health of the newborn child. However, if not rightfully addressed, it could cause detrimental effects in both the mother and the child. Depressed new mothers are less sensitive to their infant’s needs which in turn negatively affects mother-child bonding and breastfeeding. 6 This could impact both the short-term and long-term development of the child. Postpartum depression causes parenting difficulties and adverse outcomes for early child development, which again negatively impacts the mental health of the mother. 35
In addition to this, children born to mothers with postpartum depression are reported to be at increased risk of developing anxiety or major depressive disorder in the later parts of their adult life. The mothers are also at increased risk of developing postpartum psychosis characterized by hallucinations, delusions, and thoughts of harming the baby or self. Post-partum psychosis could require emergency hospital admission and inpatient care. 11
It is advised that good social support from the family along with a follow-up to assess for a possible major depressive disorder is recommended. However, as noticed with most psychiatric illnesses, the new mother fears talking about their depressed moods or seeking help. This puts them at an increased risk of progressing to a major depressive disorder (MDD) with peripartum onset.
Health workers may conduct early screening and interventions for postpartum women who are at an increased risk for postpartum depression. New mothers should be encouraged to discuss their mental state and seek help for any symptoms of depression or anxiety. Efforts must be made to destigmatize postpartum depression or anxiety. Mental health screenings should be adapted to the current situation. Currently, some women have chosen remote medical services, such as telemedicine, as a more feasible way to communicate with their health care providers during the postpartum period. While this serves as an important and useful option for patients, it can have disadvantages, such as poor service experience or barriers to physical examination. 36 Patients should also be advised to set up different pathways of receiving support from their family and friends who cannot necessarily be present physically. Virtual meetings or support groups that could include friends, family, or even other new mothers.
While certain lifestyle changes during the COVID-19 pandemic brought impositions that led to increased anxiety and depressive symptoms, some studies suggested these changes had positive outcomes as well. Despite having a sudden change in priorities and social limitations, many new mothers reported enjoying the slower pace, increase in family time, and the opportunity to get more rest. With the stay-at-home orders in place, some women expressed an appreciation of having more time with their partners and the extra help around the house. Virtual technology also provided support to some new mothers, by gaining social support from family and friends using social media and meeting other pregnant and postpartum women online to share experiences. Women even reported using certain available resources such as virtual mental health services, obstetric/pediatric providers, lactational specialists, and others. 27
Conclusion
Our literature review’s purpose was to identify risk factors for anxiety and postpartum depression in women during the SARS COV-2 pandemic. The mental health impacts of the pandemic are of great concern in postpartum women as it affects the wellness of not just the woman herself but the family and her children. Observing these challenges and incorporating changes in our healthcare system can serve as guidelines for incidents like these in the future. Social support for pregnant and postpartum women can play an important role in dealing with depression and anxiety. It is also important to strengthen the knowledge of ways to improve maternal health services during the pandemic. This will help facilitate mental health screening for postpartum women and promote maternal and child health.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Zouina Sarfraz  https://orcid.org/0000-0002-5132-7455
https://orcid.org/0000-0002-5132-7455
Azza Sarfraz  https://orcid.org/0000-0001-8206-5745
https://orcid.org/0000-0001-8206-5745
References
- 1. Nalbandian A, Sehgal K, Gupta A. Post-acute COVID-19 syndrome. Nat Med. 2021;27:601-615. doi: 10.1038/s41591-021-01283-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Razai MS, Oakeshott P, Kankam H, Galea S, Stokes-Lampard H. Mitigating the psychological effects of social isolation during the COVID-19 pandemic. BMJ. 2020;369:m1904. doi: 10.1136/bmj.m1904 [DOI] [PubMed] [Google Scholar]
- 3. Bauman BL, Ko JY, Cox S, et al. Vital signs: postpartum depressive symptoms and provider discussions about perinatal depression—United States, 2018. MMWR Morb Mortal Wkly Rep. 2020;69:575-581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ostacoli L, Cosma S, Bevilacqua F, et al. Psychosocial factors associated with postpartum psychological distress during the COVID-19 pandemic: a cross-sectional study. BMC Pregnancy Childbirth. 2020;20(1):703. doi: 10.1186/s12884-020-03399-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lubotzky-Gete S, Ornoy A, Grotto I, Calderon-Margalit R. Postpartum depression and infant development up to 24 months: a nationwide population-based study. J Affect Disord. 2021;285:136-143. doi: 10.1016/j.jad.2021.02.042 [DOI] [PubMed] [Google Scholar]
- 6. Spinola O, Liotti M, Speranza AM, Tambelli R. Effects of COVID-19 epidemic lockdown on postpartum depressive 7 Journal of Primary Care & Community Health symptoms in a sample of Italian mothers. Front Psychiatry. 2020;11(17):589916. doi: 10.3389/fpsyt.2020.589916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Moher D, Liberati A, Tetzlaff J, Altman DG; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lincoln YS, Guba EG. Naturalistic Inquiry. Sage; 1985. [Google Scholar]
- 9. Trifu S, Vladuti A, Popescu A. The neuroendocrinological aspects of pregnancy and postpartum depression. Acta Endocrinol. 2019;15(3):410-415. doi: 10.4183/aeb.2019.410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pariente G, Wissotzky Broder O, Sheiner E, et al. Risk for probable post-partum depression among women during the COVID-19 pandemic. Arch Womens Ment Health. 2020;23(6):767-773. doi: 10.1007/s00737-020-01075-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kamau C. Postpartum depression or psychosis and return to work. Lancet Psychiatry. 2017;4(2):96-97. doi: 10.1016/S2215-0366(16)30444-8 [DOI] [PubMed] [Google Scholar]
- 12. Fallon V, Davies SM, Silverio SA, Jackson L, De Pascalis L, Harrold JA. Psychosocial experiences of postnatal women during the COVID-19 pandemic. A UK-wide study of prevalence rates and risk factors for clinically relevant depression and anxiety. J Psychiatr Res. 2021;136:157-166. doi: 10.1016/j.jpsychires.2021.01.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ravaldi C, Vannacci A. The COVID-ASSESS dataset - COVID-19 related anxiety and stress in pregnancy, post-partum, and breastfeeding during lockdown in Italy. Data Brief. 2020;33:106440. doi: 10.1016/j.dib.2020.106440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. An R, Chen X, Wu Y, et al. A survey of postpartum depression and health care needs among Chinese postpartum women during the pandemic of COVID-19. Arch Psychiatr Nurs. 2021;35(2):172-177. doi: 10.1016/j.apnu.2021.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shayganfard M, Mahdavi F, Haghighi M, Sadeghi Bahmani D, Brand S. Health anxiety predicts postponing or cancelling routine medical health care appointments among women in perinatal stage during the COVID-19 lockdown. Int J Environ Res Public Health. 2020;17(21):8272. doi: 10.3390/ijerph17218272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stojanov J, Stankovic M, Zikic O, Stankovic M, Stojanov A. The risk for nonpsychotic postpartum mood and anxiety disorders during the COVID-19 pandemic. Int J Psychiatr Med. 2021;56(4):228-239. doi: 10.1177/0091217420981533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ayaz R, Hocaoğlu M, Günay T, Yardımcı OD, Turgut A, Karateke A. Anxiety and depression symptoms in the same pregnant women before and during the COVID-19 pandemic. J Perinat Med. 2020;48(9):965-970. doi: 10.1515/jpm-2020-0380 [DOI] [PubMed] [Google Scholar]
- 18. Ceulemans M, Foulon V, Ngo E, et al. Mental health status of pregnant and breastfeeding women during the COVID-19 Pandemic-A multinational cross-sectional study. Acta Obstet Gynecol Scand. 2021;100(7):1219-1229. doi: 10.1111/aogs.14092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Liu CH, Erdei C, Mittal L. Risk factors for depression, anxiety, and PTSD symptoms in perinatal women during the COVID-19 pandemic. Psychiatry Res. 2021;295:113552. doi: 10.1016/j.psychres.2020.113552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Koyuncu K, Alan Y, Sakin Ö, Aktaş HA, Angın AD. Conditions affecting postpartum depression in the COVID-19 pandemic. Med Sci Discov. 2020;7(8):611-616. doi: 10.36472/msd.v7i8.413 [DOI] [Google Scholar]
- 21. Durankuş F, Aksu E. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: a preliminary study. J Matern Fetal Neonatal Med. Published online May 18, 2020. doi: 10.1080/14767058.2020.1763946 [DOI] [PubMed] [Google Scholar]
- 22. Silverman ME, Burgos L, Rodriguez ZI, et al. Postpartum mood among universally screened high and low socioeconomic status patients during COVID-19 social restrictions in New York City. Sci Rep. 2020;10(1):22380. doi: 10.1038/s41598-020-79564-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Guvenc G, Yesilcinar İ, Ozkececi F, et al. Anxiety, depression, and knowledge level in postpartum women during the COVID-19 pandemic. Perspect Psychiatr Care. 2021;57:1449-1458. doi: 10.1111/ppc.12711 [DOI] [PubMed] [Google Scholar]
- 24. Liang P, Wang Y, Shi S, Liu Y, Xiong R. Prevalence and factors associated with postpartum depression during the COVID-19 pandemic among women in Guangzhou, China: a cross-sectional study. BMC Psychiatry. 2020;20(1):557. doi: 10.1186/s12888-020-02969-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chaves C, Marchena C, Palacios B, Salgado A, Duque A. Effects of the COVID-19 pandemic on perinatal mental health in Spain: Positive and negative outcomes [published online January 15, 2021]. Women Birth. doi: 10.1016/j.wombi.2021.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Basu A, Kim HH, Basaldua R, et al. A cross-national study of factors associated with Women’s perinatal mental health and wellbeing during the COVID-19 pandemic. PLoS One. 2021;16(4):e0249780. doi: 10.1371/journal.pone.0249780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kinser PA, Jallo N, Amstadter AB, et al. Depression, anxiety, resilience, and coping: the experience of pregnant and new mothers during the first few months of the COVID-19 pandemic. J Womens Health. 2021;30(5):654-664. doi: 10.1089/jwh.2020.8866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Davenport MH, Meyer S, Meah VL, Strynadka MC, Khurana R. Moms are not OK: COVID-19 and maternal mental health. Front Glob Womens Health. 2020;1(1):65. doi: 10.3389/fgwh.2020.00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Perzow SED, Hennessey EP, Hoffman MC, Grote NK, Davis EP, Hankin BL. Mental health of pregnant and postpartum women in response to the COVID-19 pandemic. Affect Disord Rep. 2021;4:100123. doi: 10.1016/j.jadr.2021.100123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bo HX, Yang Y, Chen J, et al. Prevalence of depressive symptoms among pregnant and postpartum women in China during the COVID-19 pandemic. Psychosom Med. 2021;83(4):345-350. doi: 10.1097/PSY.0000000000000904 [DOI] [PubMed] [Google Scholar]
- 31. Zanardo V, Tortora D, Guerrini P, et al. Infant feeding initiation practices in the context of COVID-19 lockdown. Early Hum Dev. 2021;152:105286. doi: 10.1016/j.earlhumdev.2020.105286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Boekhorst MGBM, Muskens L, Hulsbosch LP, et al. The COVID-19 outbreak increases maternal stress during pregnancy, but not the risk for postpartum depression. Arch Womens Ment Health. Published online April 8, 2021. doi: 10.1007/s00737-021-01104-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hiiragi K, Obata S, Misumi T, Miyagi E, Aoki S. Psychological stress associated with the COVID-19 pandemic in postpartum women in Yokohama, Japan. J Obstet Gynaecol Res. 2021;47(6):2126-2130. doi: 10.1111/jog.14776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zhou Y, Shi H, Liu Z, et al. The prevalence of psychiatric symptoms of pregnant and non-pregnant women during the COVID-19 epidemic. Transl Psychiatry. 2020;10:319. doi: 10.1038/s41398-020-01006-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. DeYoung SE, Mangum M. Pregnancy, birthing, and postpartum experiences during COVID-19 in the United States. Front Sociol. 2021;6:611212. doi: 10.3389/fsoc.2021.611212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Galle A, Semaan A, Huysmans E, et al. A double-edged sword-telemedicine for maternal care during COVID-19: findings from a global mixed-methods study of healthcare providers. BMJ Glob Health. 2021;6:e004575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Suárez-Rico BV, Estrada-Gutierrez G, Sánchez-Martínez M, et al. Prevalence of depression, anxiety, and perceived stress in postpartum Mexican women during the COVID-19 lockdown. Int J Environ Res Public Health. 2021;18:4627. doi: 10.3390/ijerph18094627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zanardo V, Manghina V, Giliberti L, Vettore M, Severino L, Straface G. Psychological impact of COVID-19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. Int J Gynecol Obstet. 2020;150:184-188. doi: 10.1002/ijgo.13249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Farewell CV, Jewell J, Walls J, Leiferman JA. A mixed-methods pilot study of perinatal risk and resilience during COVID-19. J Prim Care Community Health. 2020;11:2150132720944074. doi: 10.1177/2150132720944074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mariño-Narvaez C, Puertas-Gonzalez JA, Romero-Gonzalez B, Peralta-Ramirez MI. Giving birth during the COVID-19 pandemic: the impact on birth satisfaction and postpartum depression. Int J Gynecol Obstet. 2021;153:83-88. doi: 10.1002/ijgo.13565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Suzuki S. Psychological status of postpartum women under the COVID-19 pandemic in Japan. J Matern Fetal Neonatal Med. Published online May 18, 2020. doi: 10.1080/14767058.2020.1763949 [DOI] [PubMed] [Google Scholar]
- 42. Racine N, Hetherington E, McArthur BA, et al. Maternal depressive and anxiety symptoms before and during the COVID-19 pandemic in Canada: a longitudinal analysis. Lancet Psychiatry. 2021;8(5):405-415. doi: 10.1016/s2215-0366(21)00074-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Fernandes DV, Canavarro MC, Moreira H. Postpartum during COVID-19 pandemic: Portuguese mothers’ mental health, mindful parenting, and mother-infant bonding. J Clin Psychol. 2021;77:1997-2010. doi: 10.1002/jclp.23130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Li C, Huo L, Wang R, et al. The prevalence and risk factors of depression in prenatal and postnatal women in China with the outbreak of Corona Virus disease 2019. J Affect Disord. 2021;282:1203-1209. doi: 10.1016/j.jad.2021.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Gluska H, Mayer Y, Shiffman N, et al. The use of personal protective equipment as an independent factor for developing depressive and post-traumatic stress symptoms in the postpartum period. Eur Psychiatry. 2021;64(1):e34. doi: 10.1192/j.eurpsy.2021.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Oskovi-Kaplan ZA, Buyuk GN, Ozgu-Erdinc AS, Keskin HL, Ozbas A, Moraloglu Tekin O. The effect of COVID-19 pandemic and social restrictions on depression rates and maternal attachment in immediate postpartum women: a preliminary study. Psychiatr Q. 2021;92(2):675-682. doi: 10.1007/s11126-020-09843-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Masters GA, Asipenko E, Bergman AL, et al. Impact of the COVID-19 pandemic on mental health, access to care, and health disparities in the perinatal period. J Psychiatr Res. 2021;137:126-130. doi: 10.1016/j.jpsychires.2021.02.056 [DOI] [PMC free article] [PubMed] [Google Scholar]