Abstract
Objectives
As specialists of the upper airway, otolaryngologists are at high risk for COVID-19 transmission. N95 and half-face respirator (HFR) masks are commonly worn, each with advantages in functionality and comfort. In this study, physiologic and psychological parameters of prolonged N95 vs HFR wear were compared.
Study Design
Prospective crossover cohort study.
Setting
Single academic tertiary care hospital.
Methods
A prospective crossover cohort study was performed. Healthy otolaryngology trainees and medical students (N = 23) participated and wore N95 and HFR masks continuously for 3 hours each on separate days. Various measures were analyzed: vitals, spirometry variables, scores on the State-Trait Anxiety Inventory and HIT-6 (Headache Impact Test–6), distress, and “difficulty being understood.”
Results
The average age was 26.3 years (SD, 3.42). There were no significant differences in vital signs and spirometry variables between N95 and HFR wear. N95 wear was associated with decreases in oxygen saturation of approximately 1.09% more than with HFRs (95% CI, 0.105-2.077). State-Trait Anxiety Inventory scores increased more with HFR wear when compared with mean changes with N95 wear (95% CI, 1.350-8.741). There were no significant differences in HIT-6 scores or distress levels between masks. The proportions of participants reporting difficulty being understood was significantly higher with HFRs.
Conclusions
Oxygen saturation decreases with prolonged N95 wear, but anxiety and difficulty being understood are greater with HFR wear. Although HFRs have less resistance to gas exchange, N95 respirators may produce less anxiety and distress in clinical situations. Further studies are warranted to evaluate the clinical significance of these differences.
Level of Evidence
2.
Keywords: N95, half-face respirators, COVID-19, residents, anxiety, otolaryngologist, oxygen saturation, physiologic effects, psychological effects, pandemic
In December 2019, SARS-CoV-2 cases emerged in China’s Hubei province and have since resulted in a COVID-19 pandemic.1,2 The virus presents variably from asymptomatic or mild symptoms, such as cough, body aches, and gastrointestinal disturbance, to severe illness leading to respiratory compromise, multiorgan system failure, and death. According to the Centers for Disease Control and Prevention, >30,000,000 cases and 550,000 deaths have been reported in the United States alone. 3
COVID-19 can be transmitted through inhalation of contaminated droplets aerosolized by sneezing or coughing or through contact via oral, nasal, and eye mucous.2,4 As specialists of the upper aerodigestive tract, otolaryngologists are particularly vulnerable to transmission. Otolaryngologists commonly perform flexible nasopharyngoscopy and tracheotomy, which generate large quantities of aerosol-generating secretions.5,6 Utilization of respiratory personal protective equipment is of the utmost importance during the pandemic, especially for high-risk otolaryngologists. 6
The World Health Organization recommends using disposable N95 respirators for aerosolizing procedures. The N95 class of filtering facepiece respirator is the most commonly used respiratory protection device in health care settings in the United States. 7 “N95” indicates that the respirator blocks at least 95% of 300-nm particles.8,9 N95 respirators do not contain exhalation valves, contributing to increased resistance to exhalation and recirculation of carbon dioxide. The half-face respirator (HFR) is a nondisposable approved alternative to N95 respirators. HFRs filter at least 95% of aerosolized particles and are similarly fitted. Additionally, HFRs are less subject to the effect of varying temperature and humidity, prolonged wear, and repeat use.
Due to the nature of the surgery and clinic procedures, otolaryngologists often wear respirators for many continuous hours. Several studies have demonstrated that N95 respirators contribute to headaches, anxiety, higher temperature sensation, and faster breathing.10-13 We theorized that HFRs would cause less distress due to decreased exhalation resistance and therefore increase comfort.14-18 To our knowledge, studies investigating the physiologic and psychologic impact of prolonged wear of both masks have not been conducted. We aim to analyze the physiologic and psychological impact of prolonged, continuous N95 and HFR wear in otolaryngology trainees and medical students while performing activities mimicking several hours of typical trainee hospital tasks.
Materials and Methods
Participant Recruitment
This prospective crossover cohort study was conducted at the campus of the Miller School of Medicine, University of Miami, over several weekends between July and October 2020. Informational flyers were sent to university otolaryngology residents, fellows, and medical students for recruitment. Volunteers with preexisting cardiopulmonary conditions (except mild asthma) and anxiety disorders were excluded. Volunteers who were pregnant, had symptoms of viral infection, and/or had a history of COVID-19 diagnosis were also excluded. Participants committed to 2 study dates and served as their own controls, wearing an N95 mask (1860 or 1860S; 3M) on 1 day and an HFR (6000, 6500, or 7500 series; 3M) another day, each for 3 consecutive hours. The HFR was utilized with P95 or P100 pancake filters or cartridges. Participants were randomly assigned to wear either mask on day 1 of the two-day study. Experimental days were dependent on participant availability, but mask wear was separated by at least 21 hours if experimental days were consecutive. Subjects donned masks and performed a user seal check. If participants had not been fitted for an N95 or HFR, a standardized fit test (Bitrex; Allegro) was performed on-site prior to study initiation. Social distancing was enforced as standard COVID-19 precautions.
Experimental Design and Data Collection
The study design was approved by the University of Miami institutional review board. Informed consent was obtained on the first day. Upon arrival, participants completed a general health questionnaire that included information on demographics, tobacco and alcohol use, medical and surgical history, and medications. Baseline distress measures were obtained with the Headache Impact Test–6 (HIT-6) and the state portion of the State-Trait Anxiety Inventory (STAI; Form Y). HIT-6 has been validated as a tool that assesses the psychometric impact of headaches in patients, and STAI is a validated questionnaire that is sensitive in predicting caregiver distress.19-21
Physiologic parameters of heart rate, blood pressure, temperature, and oxygen saturation level were recorded after survey administration, prior to caffeine or food intake. A noninvasive capnography machine was used to record respiratory rate and carbon dioxide levels (partial pressure of carbon dioxide [PaCO2]), and spirometry was performed by an experienced pulmonologist. Spirometry values of interest included forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), FEV1/FVC, and peak expiratory flow (PEF). All baseline measurements were gathered with participants wearing a provided hospital-grade ear-loop mask. The ear-loop mask was worn over the experimental mask for the remainder of the experiment.
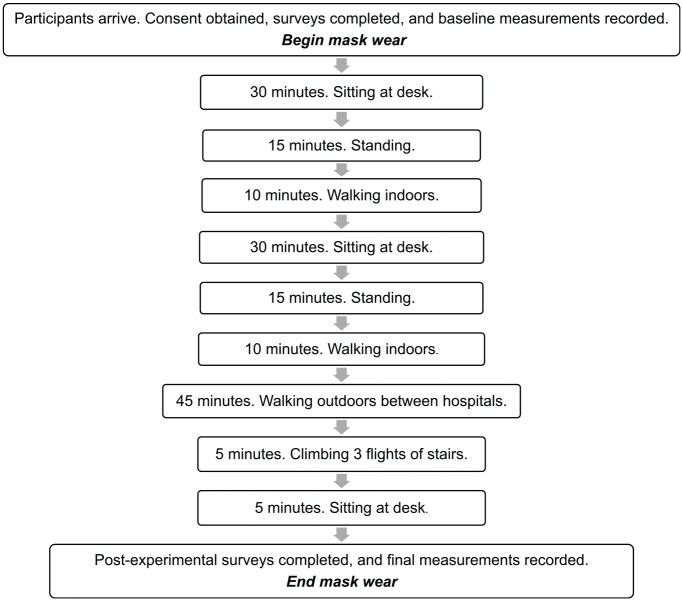
The day was structured to mimic a typical work morning for trainees. Contiguous activities were performed as outlined in Figure 1 : sitting upright in a chair, standing upright, climbing up and down stairs, and walking briskly indoors and outdoors. At the end of the scheduled activities, participants completed the HIT-6 and STAI questionnaires again. A series of additional questions were administered, assessing if participants felt that others had difficulty understanding them in regular conversation during mask wear (yes/no), duration of this difficulty (0%, 25%, 50%, 75%, 100% of time), feelings of distress during mask wear (yes/no), and duration of this distress (0%, 25%, 50%, 75%, 100% of time). These questions were created by investigators prior to the study based on common complaints in the workplace with respirator wear. Postexperimental evaluation of distress levels on a scale of 0 to 10 was also included, similar to the validated Subjective Units of Distress Scale for anxiety. 22 Postactivity vitals, PaCO2, and spirometry measures were recorded. The same experimental design was repeated on a second day with the other mask.
Figure 1.
Flow of day. Flowchart depicting the structure of experimental days. Total duration of mask wear was approximately 3 hours each.
Statistical Analysis
Continuous variables were summarized with means and 95% CIs for both masks, before and after completion of tasks. For these measures, change from baseline was calculated for each individual with the N95 and HFR. To determine whether the changes seen with N95 masks were different from the HFR, we calculated the difference in their shifts (ie, N95 shift – HFR shift), which was important for controlling between-person variation. The difference in shifts was considered significant if the 95% CI excluded zero, suggesting evidence in favor of a difference between HFR and N95. Due to the order of the subtraction (ie, N95 shift – HFR shift), if the difference in shifts was negative, we infer that the change for HFRs was larger than for N95 masks. Normality was assessed with the Shapiro-Wilk test and quantile-quantile plots. Categorical variables were displayed as proportions, and differences between N95 and HFR were determined through Fisher’s exact test with Bonferroni correction. Significance was declared for P < .05. For a sample size of 22 and a paired difference for which a 95% CI is calculated, we are powered to detect an effect size of 0.62 with an 80% chance of detection, which is a medium effect size. 23 Analyses were performed in R version 4.0.0 and SAS version 9.4 (SAS Institute).
Results
Demographics
In total, 23 volunteers participated in the study: 9 otolaryngology trainees and 14 medical students. One trainee participated in only the N95 arm due to scheduling conflicts and was therefore excluded from paired analyses. The average age of participants was 26.3 years with a standard deviation of 3.42 (range, 20-33). Pertinent preexisting conditions included mild asthma (8.7%), allergic rhinitis (26.1%), and prior diagnosis of headaches/migraines (30.4%). None of the participants were immunocompromised, reported regular tobacco use, consumed >1 alcoholic beverage daily, or indicated voice disorders. Demographic features and medical histories are summarized in Table 1 .
Table 1.
Demographic Features of Participants.
| No. (%) | |
|---|---|
| Sex | |
| Male | 13 (56.5) |
| Female | 10 (43.5) |
| Race | |
| White | 18 (78.2) |
| Asian | 2 (8.7) |
| More than one | 2 (8.7) |
| Other | 1 (4.3) |
| Ethnicity | |
| Hispanic | 5 (21.7) |
| Non-Hispanic | 18 (78.3) |
| Medical history | |
| Mild asthma | 2 (8.7) |
| Allergic rhinitis | 6 (26.1) |
| Headaches or migraines | 7 (30.4) |
| Smoking history | |
| Never | 21 (91.3) |
| Irregular use | 1 (4.3) |
| Regular use | 1 (4.3) |
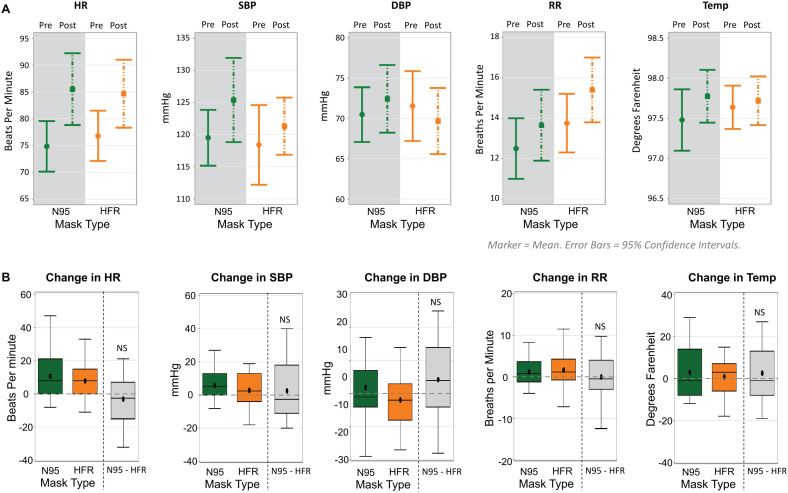
Vital Signs
Figure 2A displays the distribution of vital signs before and after completion of tasks with N95 and HFR masks. We found no significant difference for any vital sign with N95 or HFR mask use. We also found no significant differences in vital sign shifts between N95 and HFR masks ( Figure 2B ).
Figure 2.
Vital signs. (A) Dot plots depicting vitals with masks pre- and postwear. (B) Box plots reflecting changes in vitals after experiment. DBP, diastolic blood pressure; HFR, half-face respirator; HR, heart rate; RR, respiratory rate; SBP, systolic blood pressure; Temp, temperature.
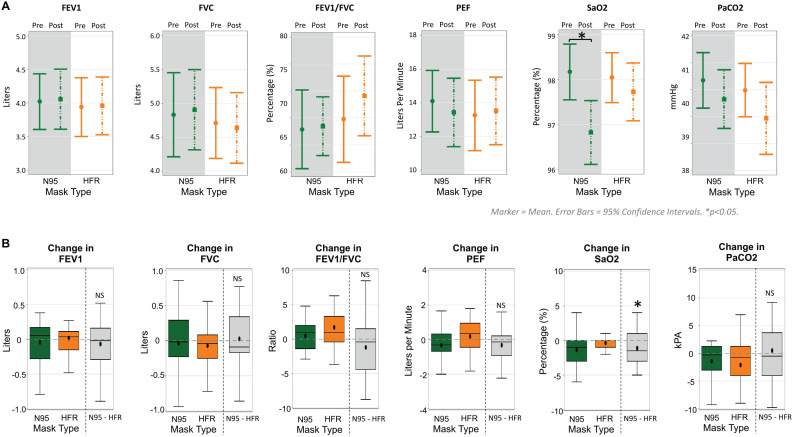
Spirometry
Spirometry variables, oxygen saturation (SaO2), and PaCO2 for each mask before and after task completion are depicted as vertical dot plots with 95% CI ( Figure 3A ). The SaO2 values were significantly different before and after N95 use, with mean values of 98.2% (95% CI, 97.6%-98.8%) and 96.8% (95% CI, 96.1%-97.5%), respectively. Although the difference in mean SaO2 before and after N95 use was small (1.35%), this finding suggests that N95 mask wear for 3 continuous hours may reduce SaO2. The clinical significance of this finding is unknown and likely dependent on clinical context. There were no other significant differences in spirometry variables and PaCO2 after use of the N95 or HFR mask. We found no significant differences for the shifts from baseline between the N95 and HFR groups for FEV1, FVC, FEV1/FVC, peak expiratory flow, and PaCO2 ( Figure 3B ). However, use of N95 masks was significantly associated with greater reductions in SaO2 than with HFR masks by an average of −1.09% (95% CI, −2.08% to −0.11%).
Figure 3.
Spirometry, oxygen saturation (SaO2), partial pressure of carbon dioxide (PaCO2). (A) Dot plots for each mask pre- and postwear. (B) Box plots reflecting measure changes. FEV1, forced expiratory volume (1 second); FVC, forced vital capacity; HFR, half-face respirator; PEF, peak expiratory flow.
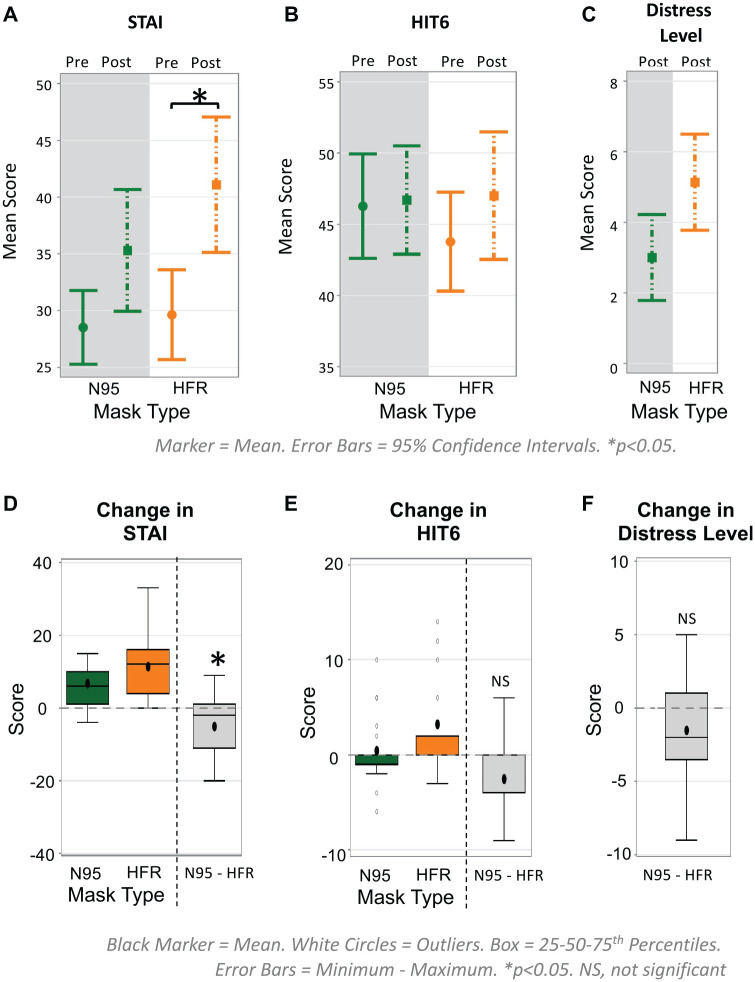
STAI, HIT-6, and Distress Levels
The distributions of STAI, HIT6, and distress scores with N95 and HFR masks are depicted as vertical dot plots with 95% CIs ( Figure 4A ). The STAI scores were significantly different before and after HFR mask use, with mean scores of 29.65 (95% CI, 25.68-33.59) and 41.09 (95% CI, 35.12-47.06), respectively. No differences in STAI scores were seen before and after N95 wear. Although there seemed to be an increase in mean HIT-6 scores after HFR wear, there were no statistically significant changes before and after HFR use. There were also no significant differences in mean distress levels after mask wear between conditions.
Figure 4.
Psychological parameters. (A) Dot plots depicting psychological measures with masks pre- and postwear. (B) Box plots reflecting measure changes after experiment. HFR, half-face respirator; HIT-6, Headache Impact Test–6; STAI, State-Trait Anxiety Inventory. Subjective distress level rated 0 to 10.
Shifts from baseline for the STAI and HIT-6 scores for the N95 and HFR masks are displayed in Figure 4B . N95 masks were associated with smaller increases in STAI scores than HFR masks by a mean of −5.05 (95% CI, −8.74 to −1.35), which was significant. The increase in HIT-6 scores with HFRs was on average 2.5 points greater than in N95 scores; however, this was not significant (95% CI, −5.03 to 0.33).
The mean distress levels after N95 and HFR wear were 3.00 (95% CI, 1.78-4.22) and 5.14 (95% CI, 3.77-6.50), respectively. Although the mean distress level was 1.5 points higher with HFRs, the difference was not significant (95% CI, −0.42 to 3.42).
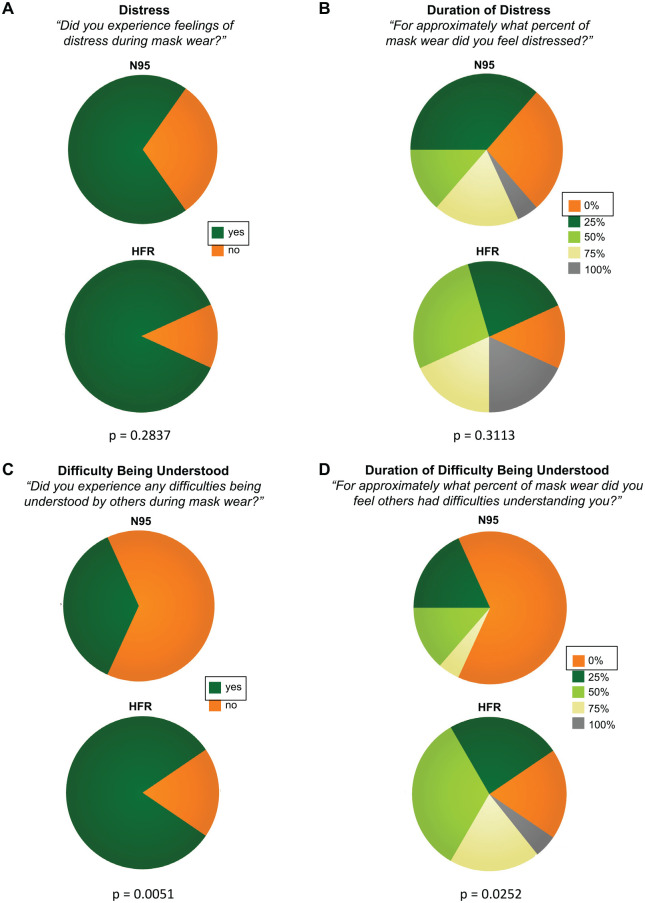
Distress and Difficulty Being Understood
The proportions of participants experiencing distress and the approximate duration of distress during N95 and HFR were analyzed ( Figure 5A and B ). Although the proportions of participants who experienced no distress and 0% duration of distress were higher with N95, there were no significant differences between masks. The proportions of participants experiencing difficulty being understood with the N95 and HFRs and the approximate duration of difficulty are depicted in Figure 5C and D . There was a nearly significant difference in the proportions for difficulty being understood between the masks (P = .0051), with more participants reporting difficulty with HFRs. We also observed a difference for duration of difficulty between the N95 and HFRs per Fisher’s exact tests (P = .0252), with a greater proportion reporting 0% duration with N95 masks; however, this was not statistically significant after Bonferroni correction for multiple comparisons.
Figure 5.
Distress and difficulty being understood during mask wear: (A, B) feeling and duration of distress and (C, D) difficulty being understood and duration.
Discussion
Disposable N95 masks and nondisposable HFRs are 2 types of particulate-filtering facepiece respirators. HFRs possess exhalation valves that keep exhalation resistance low and prevent humidity buildup within the mask. Several studies have investigated the effects of particulate filtering facepiece respirators without exhalation valves on CO2 retention.16,17 Epstein et al reported that exercising with N95 masks was associated with a significant increase in end-tidal CO2 (EtCO2) levels. Rebreathing expired air may increase dead space and contribute to mild hypercapnia. 17 This CO2 buildup in the bloodstream can lead to acute respiratory acidosis, or “sick building syndrome,” which may present with headache, fatigue, difficulty concentrating, anxiety, or increases in heart rate and blood pressure.16-18 Exhalation valves may therefore help maintain physiologic homeostasis and improve comfort during prolonged mask wear.14-18 Despite this, the relative effect of filtering facepiece respirator choice on the wearer has not been widely characterized. Our study is the first to assess the physiologic and psychological impact of prolonged, continuous use of N95 respirators and HFRs.
Physiologic Impact
Our study demonstrated no significant changes in heart rate, systolic and diastolic blood pressure, or respiratory rate after mask wear, and there were no significant differences between mask types. Our study corroborates the findings of Roberge et al when investigating the thermal burden imposed by N95 wear; the authors found no significant increase in participants’ temperatures after 1 to 2 hours of low-moderate work. 10
Bansal et al analyzed 56 subjects to determine the respiratory effects of HFR and N95 wear in 8- to 10-minute simulated work conditions, with breaks between tasks. 12 They found that respirator type did not affect respiratory volume parameters and flow rates. However, they demonstrated that HFRs led to increased inspiratory time, reduced expiratory time, and increases in the duty cycle when compared with N95 masks. 12 With a longer study time of 3 continuous hours, our study also revealed no differences in respiratory volume parameters or flow rate.
Although respirators without expiratory valves have been shown to increase EtCO2, we found no significant change in PaCO2 levels with either mask or between the masks.16,17 Although PaCO2 is not a perfect estimation of EtCO2, we may not have noted any changes due to lower-intensity physical activity (ie, walking and climbing stairs) when compared with other experiments (ie, maximal exercise test). 17
Interestingly, our study demonstrated a significant difference in SaO2 with prolonged N95 wear. Moreover, SaO2 was statistically worse with N95 masks than with HFRs. In our cohort of generally young and healthy adults, this small difference is likely physiologically and clinically insignificant, especially when considering other studies that define a 2%-3% decrease in SaO2 as being clinically relevant.24,25 Meanwhile, Kao et al analyzed the effects of N95 masks worn for 4 hours during hemodialysis in 39 patients with end-stage renal disease. They found a significant 9–mmHg decrease in the partial pressure of oxygen with N95 wear, in addition to increased respiratory rate and chest discomfort. 26 Patients with comorbidities may be more susceptible to reductions in SaO2, and effects may be more clinically significant than in our study population. However, in our study and prior investigations, cognitive and physical testing were not performed to determine if a drop in oxygen saturation values is detrimental to cognitive brain function or physical endurance. Future studies should assess these parameters to evaluate the clinical impact of diminished oxygen saturation rates in mask wearers.
Psychological Impact
Significantly elevated anxiety scores were recorded in participants after prolonged wear of HFR as compared with N95. Harber et al found similar increases in STAI scores with HFR wear when compared with N95 respirators. 11 Of note, there is a history of mental burden on health care professionals in prior pandemics.27-30 Studies from COVID-19 demonstrate increased mental strain on health care workers, with several highlighting a prevalence of distress, anxiety, and burnout in otolaryngology trainees.30,31 It is of the utmost importance to take trainee well-being and personal preference into account when choosing mask wear, when N95 and HFR provide similar levels of protection. Our study highlights that HFRs may be associated with an increase in distress and anxiety levels in a population that is already facing alarming rates of burnout.32-39 Being aware of interventions that may be associated with negative psychological parameters is vital to ensure the well-being of physicians and avoid poor patient outcomes.
Although speaking time was not standardized, participants experienced more difficulty being understood by others during regular conversation when wearing HFRs. This can contribute to increased levels of anxiety and distress, especially when attempting to communicate in critical clinical scenarios or the operating room. Bandaru et al recruited 20 health care workers with normal hearing and obtained speech reception thresholds and speech discrimination scores without personal protective equipment and with an N95 mask and face shield. They found a significant increase in speech reception threshold and decrease in speech discrimination score with use of the N95. 40 To our knowledge, our study is the first to evaluate and compare conversational speech understanding from a participant’s perspective using a subjective questionnaire. Participants designated the N95 mask as being superior to HFR due to improved understandability. We propose that prolonged HFR use may negatively affect the well-being of wearers by increasing distress during communication. Our study’s findings are timely and important for the well-being of health care personnel, as ongoing use of personal protective equipment is expected to continue for the unforeseen future.
Limitations
Limitations of this study include a small cohort due to recruitment barriers during the pandemic. Testing was performed for 3 continuous hours, and a single model of N95 and HFR masks was used; as such, findings cannot be extrapolated to effects with more prolonged use that is typical for an average physician workday or to other types of respirators. Additional psychological parameters were not evaluated, such as sleep before testing, hydration, and personal life stressors. It is also important to note that HFRs may provide greater protection than N95 respirators when P100 filters are used and can therefore be more beneficial in select clinical situations. In addition, participants may have been more familiar with N95 masks from prior use, thus rendering the distress level lower. Future studies should investigate other respirator types, such as P100 disposable respirators with a 1-way valve, which may offer the increased protection of HFRs and decreased distress seen with N95 wear.
Conclusion
As of March 2021, >132 million COVID-19 cases with 2.86 million deaths have been reported worldwide. 3 New variants have alarming implications on the efficiency of current vaccines, 41 signaling a pandemic that is far from over. Heath care personnel will continue to remain on the frontlines and therefore require respirator use. The present study contributes significantly to the understanding of the differences between N95 and HFR when worn continuously. Our findings suggest that HFRs may offer advantages over N95 in maintaining objective oxygen saturation levels, but HFR wear may contribute to worsened speech understandability and feelings of anxiety. However, future studies should assess the clinical relevance of these changes. Studies evaluating parameters affected by respirator use in health care personnel is of the utmost importance to maximize provider well-being to ensure that healthy personnel are available and capable to treat our most vulnerable patients.
Author Contributions
Erin R. Cohen, study design, participant recruitment, data collection, manuscript editing; Stefanie Peña, data collection, manuscript writing, manuscript editing; Carly Misztal, data collection, manuscript writing, manuscript editing; Thomas Iglesias, participant recruitment, study design revisions; Alejandro Mantero, data analysis, data interpretation; Christine T. Dinh, data analysis, data interpretation; Gregory Holt, data collection, manuscript editing; Giovana R. Thomas, study conception, study design, data collection, manuscript editing
Disclosures
Competing interests: None.
Sponsorships: None.
Funding source: None.
Footnotes
ORCID iD: Carly Misztal  https://orcid.org/0000-0002-6724-8890
https://orcid.org/0000-0002-6724-8890
References
- 1. Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99:481-487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Esakandari H, Nabi-Afjadi M, Fakkari-Afjadi J, Farahmandian N, Miresmaeili S-M, Bahreini E. A comprehensive review of COVID-19 characteristics. Biol Proced Online. 2020;22:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention. COVID data tracker. Accessed April 6, 2021. https://covid.cdc.gov/covid-data-tracker/#datatracker-home
- 4. Riou J, Althaus CL. Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020. Euro Surveill. 2020;25:2000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Piccirillo JF. Otolaryngology–head and neck surgery and COVID-19. JAMA. 2020;324:1145-1146. [DOI] [PubMed] [Google Scholar]
- 6. Howard BE. High-risk aerosol-generating procedures in COVID-19: respiratory protective equipment considerations. Otolaryngol Head Neck Surg. 2020;163:98-103. [DOI] [PubMed] [Google Scholar]
- 7. Martyny J, Glazer CS, Newman LS. Respiratory protection. N Engl J Med. 2002;347:824-830. [DOI] [PubMed] [Google Scholar]
- 8. de Perio MA, Dowell CH, Delaney LJ, et al. Strategies for optimizing the supply of N95 filtering facepiece respirators during the coronavirus disease 2019 (COVID-19) pandemic. Disaster Med Public Health Prep. 2020;14:658-669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhang M, Emery AR, Tannyhill RJ, 3rd, Zheng H, Wang J. Masks or N95 respirators during COVID-19 pandemic—which one should I wear? J Oral Maxillofac Surg. 2020;78:2114-2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Roberge R, Benson S, Kim J-H. Thermal burden of N95 filtering facepiece respirators. Ann Occup Hyg. 2012;56:808-814. [DOI] [PubMed] [Google Scholar]
- 11. Wu S, Harber P, Yun D, Bansal S, Li Y, Santiago S. Anxiety during respirator use: comparison of two respirator types. J Occup Environ Hyg. 2011;8:123-128. [DOI] [PubMed] [Google Scholar]
- 12. Bansal S, Harber P, Yun D, et al. Respirator physiological effects under simulated work conditions. J Occup Environ Hyg. 2009;6:221-227. [DOI] [PubMed] [Google Scholar]
- 13. Ong JJY, Bharatendu C, Goh Y, et al. Headaches associated with personal protective equipment—a cross-sectional study among frontline healthcare workers during COVID-19. Headache. 2020;60:864-877. [DOI] [PubMed] [Google Scholar]
- 14. Patel B, Hardman JC, Yang W, et al. Reusable respirators as personal protective equipment during ENT surgery. J Laryngol Otol. 2020;134:732-734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sozkes S, Sozkes S. COVID-19 and respiratory protection for healthcare providers. Int J Occup Med Environ Health. 2021;34(2):307-318. [DOI] [PubMed] [Google Scholar]
- 16. Redlich CA, Sparer J, Cullen MR. Sick-building syndrome. Lancet. 1997;349:1013-1016. [DOI] [PubMed] [Google Scholar]
- 17. Epstein D, Korytny A, Isenberg Y, et al. Return to training in the COVID-19 era: the physiological effects of face masks during exercise. Scand J Med Sci Sports. 2021;31:70-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Madan M, Madan K, Mohan A, Hadda V, Tiwari P, Mittal S. Personal protective equipment and particulate filter use during the COVID-19 pandemic: “acidotic times.” Arch Bronconeumol. 2021;57(suppl 1):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kosinski M, Bayliss MS, Bjorner JB, et al. A six-item short-form survey for measuring headache impact: the HIT-6. Qual Life Res. 2003;12:963-974. [DOI] [PubMed] [Google Scholar]
- 20. Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press; 1983. [Google Scholar]
- 21. Greene J, Cohen D, Siskowski C, Toyinbo P. The relationship between family caregiving and the mental health of emerging young adult caregivers. J Behav Health Serv Res. 2017;44(4):551-5663. [DOI] [PubMed] [Google Scholar]
- 22. Tanner BA. Validity of global physical and emotional SUDS. Appl Psychophysiol Biofeedback. 2012;37(1):31-34. [DOI] [PubMed] [Google Scholar]
- 23. Cohen J. A power primer. Psychol Bull. 1992;112(1):155-159. [DOI] [PubMed] [Google Scholar]
- 24. Greenhalgh T, Javid B, Matthew BJ, Inada-Kim M. What is the efficacy and safety of rapid exercise tests for exertional desaturation in COVID-19? Centre for Evidence-Based Medicine website. Posted April 21, 2020. Accessed October 4, 2020. https://www.cebm.net/covid-19/what-is-the-efficacy-and-safety-of-rapid-exercise-tests-for-exertional-desaturation-in-covid-19/
- 25. Chan NC, Li K, Hirsh J. Peripheral oxygen saturation in older persons wearing nonmedical face masks in community settings. JAMA. 2020;324(22):2323-2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kao TW, Huang KC, Huang YL, Tsai TJ, Hsieh BS, Wu MS. The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end-stage renal disease. J Formos Med Assoc. 2004;103:624-628. [PubMed] [Google Scholar]
- 27. Bai Y, Lin CC, Lin CY, Chen JY, Chue CM, Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. 2004;55:1055-1057. [DOI] [PubMed] [Google Scholar]
- 28. Chua SE, Cheung V, Cheung C, et al. Psychological effects of the SARS outbreak in Hong Kong on high-risk health care workers. Can J Psychiatry. 2004;49:391-393. [DOI] [PubMed] [Google Scholar]
- 29. Lehmann M, Bruenahl CA, Addo MM, et al. Acute Ebola virus disease patient treatment and health-related quality of life in health care professionals: a controlled study. J Psychosom Res. 2016;83:69-74. [DOI] [PubMed] [Google Scholar]
- 30. Civantos AM, Byrnes Y, Chang C, et al. Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: national study. Head Neck. 2020;42:1597-1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chou DW, Staltari G, Mullen M, Chang J, Durr M. Otolaryngology resident wellness, training, and education in the early phase of the COVID-19 pandemic. Ann Otol Rhinol Laryngol. 2021;130(8):904-914. [DOI] [PubMed] [Google Scholar]
- 32. Kavanagh KR, Spiro J. Faculty wellness: educator burnout among otolaryngology graduate medical educators. Otolaryngol Head Neck Surg. 2018;158:991-994. [DOI] [PubMed] [Google Scholar]
- 33. Pereira-Lima K, Loureiro SR. Burnout, anxiety, depression, and social skills in medical residents. Psychol Health Med. 2015;20:353-362. [DOI] [PubMed] [Google Scholar]
- 34. Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50:132-149. [DOI] [PubMed] [Google Scholar]
- 35. Ambrose EC, Devare J, Truesdale CM, et al. Two novel approaches to improve otolaryngology resident wellness: the ACGME Back to Bedside Initiative. Otolaryngol Head Neck Surg. 2018;158:979-980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Maslach C. Maslach Burnout Inventory. In: Evaluating Stress: A Book of Resources. American Psychological Association; 1997:191-218. [Google Scholar]
- 37. Balch CM, Shanafelt TD, Sloan JA, Satele DV, Freischlag JA. Distress and career satisfaction among 14 surgical specialties, comparing academic and private practice settings. Ann Surg. 2011;254:558-568. [DOI] [PubMed] [Google Scholar]
- 38. Welp A, Meier LL, Manser T. Emotional exhaustion and workload predict clinician-rated and objective patient safety. Front Psychol. 2014;5:1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995-1000. [DOI] [PubMed] [Google Scholar]
- 40. Bandaru SV, Augustine AM, Lepcha A, et al. The effects of N95 mask and face shield on speech perception among healthcare workers in the coronavirus disease 2019 pandemic scenario. J Laryngol Otol. Published online September 28, 2020. doi: 10.1017/S0022215120002108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Priyanka Choudhary OP, Singh I. Evolution of SARS-CoV-2: a prediction on the lineages and vaccine effectiveness. Travel Med Infect Dis. 2021;40:101983. [DOI] [PMC free article] [PubMed] [Google Scholar]