Abstract
Background & Aims:
The Affordable Care Act provided the opportunity for states to expand Medicaid for low-income individuals. Not all states adopted Medicaid expansion, and the timing of adoption among expansion states varied. Prior studies demonstrated that Medicaid expansion improved mortality for several chronic conditions. Although there are data on the association between Medicaid expansion on insurance type among patients waitlisted for a liver transplant, there are no data on its impact on liver disease-related mortality in the broader population. We therefore sought to evaluate the association between Medicaid expansion and state-level liver disease-related mortality using a quasi-experimental study design.
Methods:
We evaluated age-adjusted state-level liver disease-related mortality rates using CDC data. We fit multivariable linear regression models that accounted for socio-demographic, clinical, and access-to-care variables at the state level, and a difference-in-difference estimator to evaluate the association between Medicaid expansion and liver disease-related mortality.
Results:
In multivariable linear regression models, there was a significant association between Medicaid expansion and liver disease-related mortality (p=0.02). Medicaid expansion was associated with 8.3 (95% CI: 1.6–15.1) fewer deaths from liver disease per 1,000,000 adult residents per year after Medicaid expansion compared to what would have been expected to occur if those states followed the same trajectory as non-expansion states. The impact of Medicaid expansion translated to 870 fewer liver-related deaths per year in expansion states (4,350 in the post-expansion study period from 2014–2018).
Conclusions:
These data support the contention that Medicaid expansion has been associated with significantly decreased liver disease-related mortality. Universal Medicaid expansion could further decrease liver disease-related mortality in the US.
Introduction
In 2010, the Patient Protection and Affordable Care Act (ACA) created a paradigm shift in provision of insurance to low-income individuals. The ACA not only offered the opportunity for states to expand Medicaid eligibility to individuals with incomes at or below 138% of the federal poverty line, but it emphasized preventive care.1 The ACA offered the potential to provided health insurance to many more individuals, with studies demonstrating that utilization of health resources and preventive care measures increased as a result.1 Though the implementation of the ACA began in January 2014, the uptake of Medicaid expansion was not uniform across the 50 states, and varied in scope and timing.2
Previous studies have demonstrated improvements in population-level mortality (state- and county-level) due to Medicaid expansion. States that expanded Medicaid had improvements in cardiovascular mortality (smaller increase in mortality in expansion vs non-expansion states) and a decrease in all-cause mortality among patients with end-stage renal disease and newly initiated hemodialysis.3–6 Although Medicaid expansion was associated with an increase in the proportion of liver transplant waitlist candidates enrolled in Medicaid,7 its impact on liver mortality remains unknown. In the broader context of policy debates about Medicaid expansion to all states, potential repeals of the ACA, and even universal healthcare, the question of the impact of Medicaid expansion on liver mortality is of utmost importance.
There are several potential mechanisms by which Medicaid expansion may have impacted liver-related mortality at the state level within a short period of time. First, the period of Medicaid expansion coincided with the approval of all-oral direct acting antivirals (DAA’s) for patients with hepatitis C virus (HCV) at the end of 20138–10, which could lower mortality for HCV-infected patients within a matter of a few years.11,12 Secondly, provision of health insurance (i.e., Medicaid) for patients with cirrhosis could provide access to specialty care (gastroenterologists and/or hepatologists), which has been shown to be associated with improved care and lower mortality for patients with cirrhosis.13–20 It is for these reasons that we sought to evaluate the association between Medicaid expansion and liver-related mortality at the state level.
Methods
This was a retrospective cohort study evaluating the association between Medicaid expansion and liver morality employing a difference-in-differences (DID) method.3,6,21 The primary outcome was annual state-level annual age-adjusted liver-related mortality rates using International Classification of Disease, 10th revision (ICD −10) codes included in prior studies from the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research mortality database (CDC Wonder) between 2010–2018.22,23 We only included adults aged 25–64 years of age given patients become Medicare eligible at age 65.17,18 Data were evaluated at the state, rather than county level, due to the available data and small sample sizes of mortality in counties in any given calendar year (CDC Wonder only provides age-adjusted mortality rates for subgroups with at least 20 deaths during the requested time period). State-level data were the unit of analysis to assess whether a policy change (i.e., Medicaid expansion) impacted liver-related mortality at the broader population-level, rather than for the individual patient.
Study Covariates
We included several socio-demographic, clinical, and access-to-care variables that may be associated with state-level liver-related mortality rates: 1) race/ethnicity and gender using 2010 US Census data available from CDC Wonder23; 2) percentage of adults with a household income <138% of the federal poverty level (FPL) based on the Small Area Income and Poverty Estimates (SAIPE) program;24 3) percentage of adults with health insurance among those at or below 138% federal poverty level in 2010 based on the Small Area Health Insurance Estimates (SAHIE) program25;) percentage of adults with diabetes, obesity, and heavy alcohol use in 2010 based on the CDC Behavioral Risk Factor Surveillance System26; 4) percentage of adults that were unemployed in 2010 from the Bureau of Labor Statistics;27 5) median household income from the SAIPE;24 and 6) the number of primary care physicians and board-certified gastroenterologists per 100,000 population in 2010 based on the Health Resources and Services Administration Area Health Resources Files.28 These covariates had been considered in prior studies addressing the impact of Medicaid expansion on cardiovascular mortality.18 Importantly, although there have been changes in the demographics of the United States during the study period, the annual percentage of adults ages 25–64 in a given state that were a specific race, ethnicity, or gender were largely stable from year to year, and therefore using 2010 ‘baseline’ demographics data were valid.
Study Design
The goal of this study was to determine whether Medicaid expansion under the ACA was associated with improved liver-related mortality rates at the state level. We used a quasi-experimental study design using a DID estimator3,6,17,18,21 which allowed us to compare changes in liver-related mortality over time in the ‘intervention’ group (states with Medicaid expansion) to a comparator group (states that did not expand Medicaid). This approach also accounts for differences in baseline mortality pre-2014 across expansion vs non-expansion states. The comparator group allowed us to determine whether changes in mortality in expansion states was associated with the policy change, or rather some other broader intervention that would impact liver-related mortality. This approach was needed for this study given the temporal relationship between Medicaid expansion and approval of all-oral DAA’s. The DID method therefore would provide insight as to whether changes in mortality in expansion states pre- vs post-expansion was related simply to approval of DAA’s (which would apply in non-expansion states as well), or some other policy change (i.e., Medicaid expansion).
States classified as ‘expansion were states that expanded Medicaid eligibility as of January 1, 2014, and/or those that expanded Medicaid during the intervention period, consistent with prior studies.3,17,18 The years 2010–2013 were universally deemed pre-expansion years for all states, and was adjusted to later (e.g., 2015 was post-expansion year rather than 2014) for the states that expanded Medicaid during the intervention period but after January 1, 2014).
Statistical Analysis
We first compared the baseline characteristics of the Medicaid expansion and non-expansion states using rank-sum tests due to the non-normal distribution of the data. We also compared baseline liver mortality rate among expansion and non-expansion states in 2010. To evaluate potential covariates associated with state-level liver-related mortality, we fit multilevel mixed effects model with random intercepts at each state. This method allowed us to account for differences in the baseline liver disease-related mortality rate for each state and to account for correlation within states due to repeated measures across years. We evaluated all the covariates listed above in univariable models and considered those with a p-value <0.1 for inclusion in the final multivariable model. We fit a multivariable linear regression model using a backwards selection process and retained covariates with a p-value <0.1 in the final model. We then used the predict command in Stata to estimate fully adjusted annual state-level liver-related mortality rates, accounting for all factors except for those related to Medicaid expansion.
To specifically evaluate the association between Medicaid expansion and state-level liver-related mortality, we fit similar models to those described above, including the covariates that were significant in the models with a p-value <0.1. These models included a variable for expansion status (expansion vs non-expansion state), indicator for pre-expansion and post-expansion period (i.e., 2010–2013 was pre-expansion for all states, and 2014–2018 was post-expansion unless otherwise specified above), and an interaction term between expansion status and period. This interaction term represented the DID estimator and signified whether Medicaid expansion was associated with a difference in liver-related mortality in expansion vs non-expansion states (formula shown in Supplementary Material).
Secondary Analysis
The underlying cause of death for patients with liver disease-related mortality in CDC Wonder focused largely on cirrhosis or complications of portal hypertension (e.g., ascites, variceal bleed) rather than the etiology of liver disease other than alcohol-induced cirrhosis (e.g., HCV).22 Therefore, we could not specifically evaluate changes in HCV-related mortality pre- vs post-expansion. However, to explore whether access to DAA’s could help to explain changes in mortality with Medicaid expansion, we compared the ‘grade’ of expansion vs non-expansion states related to access to DAA treatment. This score was based on 2017 data released by the Center for Health Law and Policy Innovation (CHLPI) in conjunction with the National Viral Hepatitis Roundtable (NVHR) entitled, “Hepatitis C: The State of Medicaid Access.”29 A state’s HCV grade was based on coverage restrictions related to: extent of liver fibrosis, amount of time in sobriety, and who can prescribe the DAA agents (i.e., provider type/specialty). Based on these restrictions, states were assigned a letter grade from A-F for their Medicaid accessibility to DAA’s.29 To further investigate the impact of DAA’s, we refit models only among states with HCV grades A and B.
Analyses were conducted using STATA version 16 (College Station, Texas). This study was deemed exempt by the Institutional Review Board at the University of Miami.
Results
During the study period, there were 31 states (including Washington D.C.) that had adopted Medicaid expansion, while 20 states did not. In 2010, age-adjusted liver mortality did not vary significantly between expansion and non-expansion states (P= 0.97). Expansion and non-expansion states were not significantly different with respect to the percentage of their adult population that was Black race, Hispanic ethnicity, or female gender (Table 1). In addition, expansion and non-expansion states did not differ in the percentage of adults that were unemployed, or the number of primary care doctors or board-certified gastroenterologists per 100,000 population (Table 1). The household income and percentage of adults that were insured were significantly higher in expansion states, and while there was a higher percentage of adults with heavy alcohol use in expansion states, there was a greater prevalence of obesity in non-expansion states (Table 1).
Table 1:
Comparison of socio-demographic and clinical characteristics of expansion vs non-expansion states based on 2010 data
| Variable | Medicaid expansion N=31 | Medicaid non-expansion N=20 | P-value |
|---|---|---|---|
| Black race | 7.4% (2.9–14.0%) | 11.9% (3.1–23.7%) | 0.24 |
| Hispanic ethnicity | 8.1% (3.8–14.5%) | 7.5% (3.8–8.6%) | 0.46 |
| Female sex | 50.4% (49.9–51.1%) | 50.7% (49.7–51.2%) | 0.73 |
| History of diabetes | 8.5% (7.4–9.3%) | 9.6% (7.8–10.4%) | 0.07 |
| Obese | 25.6% (23.9–29.1%) | 29.4% (27.1–31.7%) | 0.006 |
| Heavy Alcohol Use | 5.3% (4.4–5.8%) | 4.8% (3.8–5.3%) | 0.03 |
| Insured among those at or below 138% of the federal poverty level | 63.0% (57.0–71.1%) | 57.8% (54.0–60.8%) | 0.02 |
| Living below federal poverty level | 13.8% (11.5–15.8%) | 16.2% (13.3–18.0%) | 0.07 |
| Unemployed | 8.6% (7.7–10.3%) | 8.4% (7.1–10.4%) | 0.67 |
| Median state household income | $52,053 (45,354–60,729) | $45,126 (42,313–48518) | 0.005 |
| Primary care doctors/100,000 population | 30.7 (23.9–38.7) | 31.1 (26.8–41.5) | 0.69 |
| Gastroenterologists/100,000 population | 3.8 (3.1–5.2) | 3.4 (2.8–4.0) | 0.13 |
Data presented as median (IQR), with the unit of analysis each state
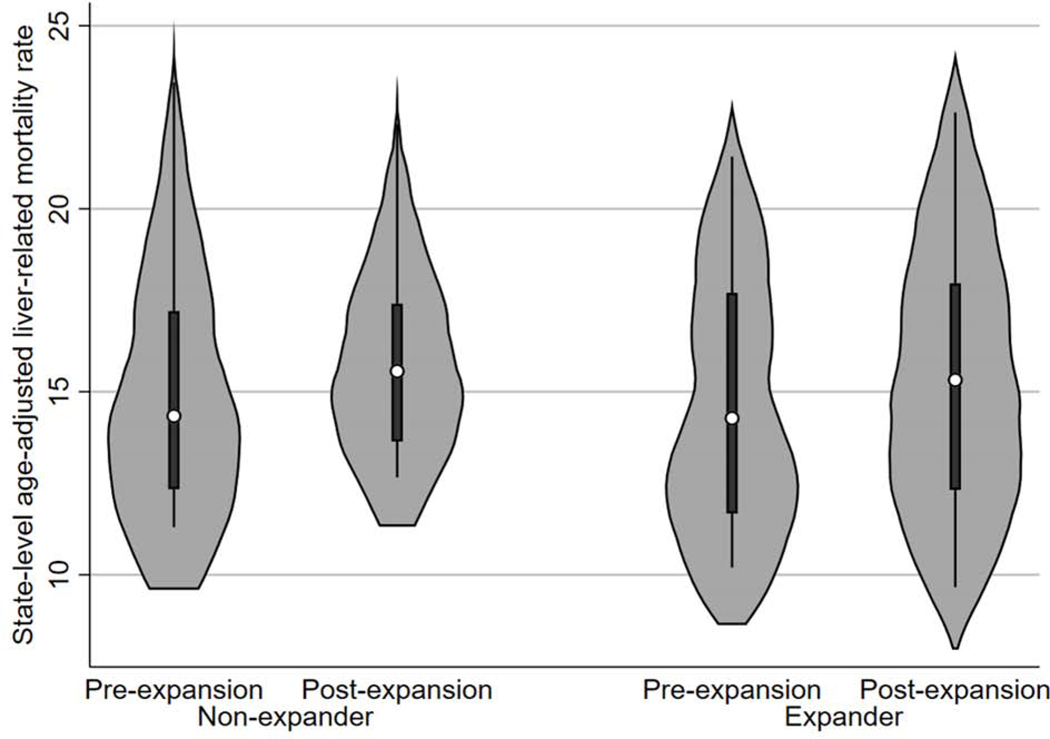
When the data for each state was aggregated into pre- vs post-expansion periods, the increase in liver-related mortality was less pronounced in expansion states. In expansion states, the median state-level age-adjusted liver-related mortality rate increased from 14.5 deaths per 100,000 population (interquartile range [IQR]: 11.7–18.3) in the pre-expansion period to 15.5 deaths per 100,000 population (IQR: 12.3–19.3) in the post-expansion period. The increase in state-level mortality was greater in non-expansion states, increasing from 14.3 deaths per 100,000 population (IQR: 12.3–17.2) in the pre-expansion period to 15.9 deaths per 100,000 population (IQR: 13.7–18.7) in the post-expansion period (Figure 1).
Figure 1: Age-adjusted liver disease-related mortality states in expansion vs non-expansion states in pre- vs post-expansion periods*.
a. State-level data aggregated into pre- vs post-expansion period
b. 3 expansion states and 2 non-expansion states not shown as they were outliers with age-adjusted liver disease-related mortality rates of >25 deaths per 100,000 population
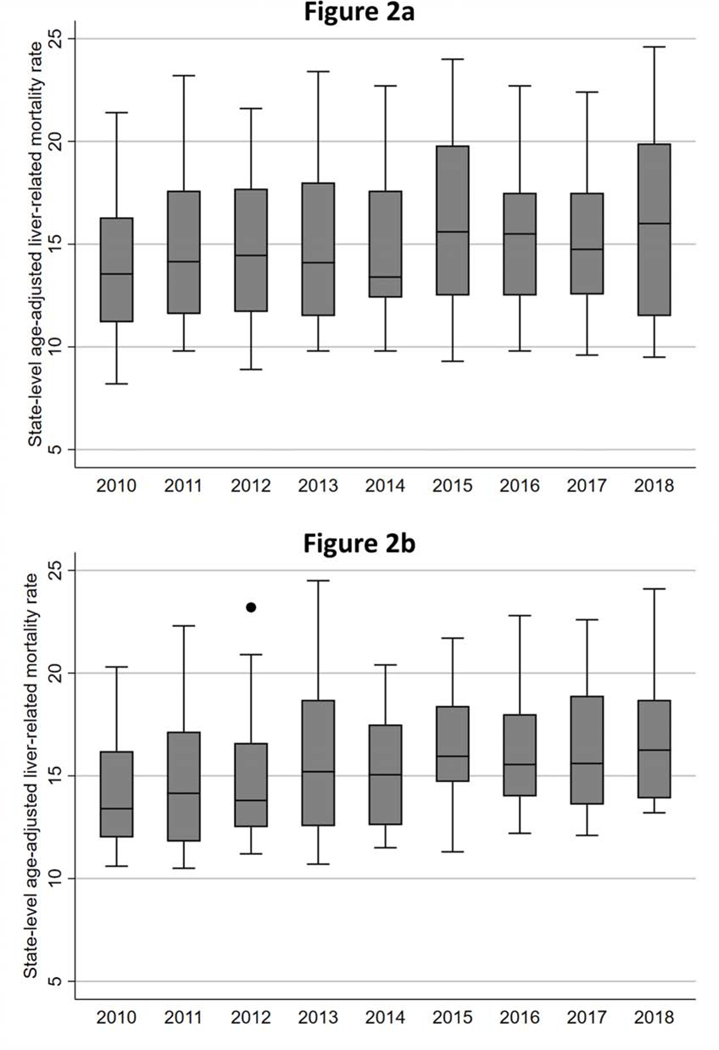
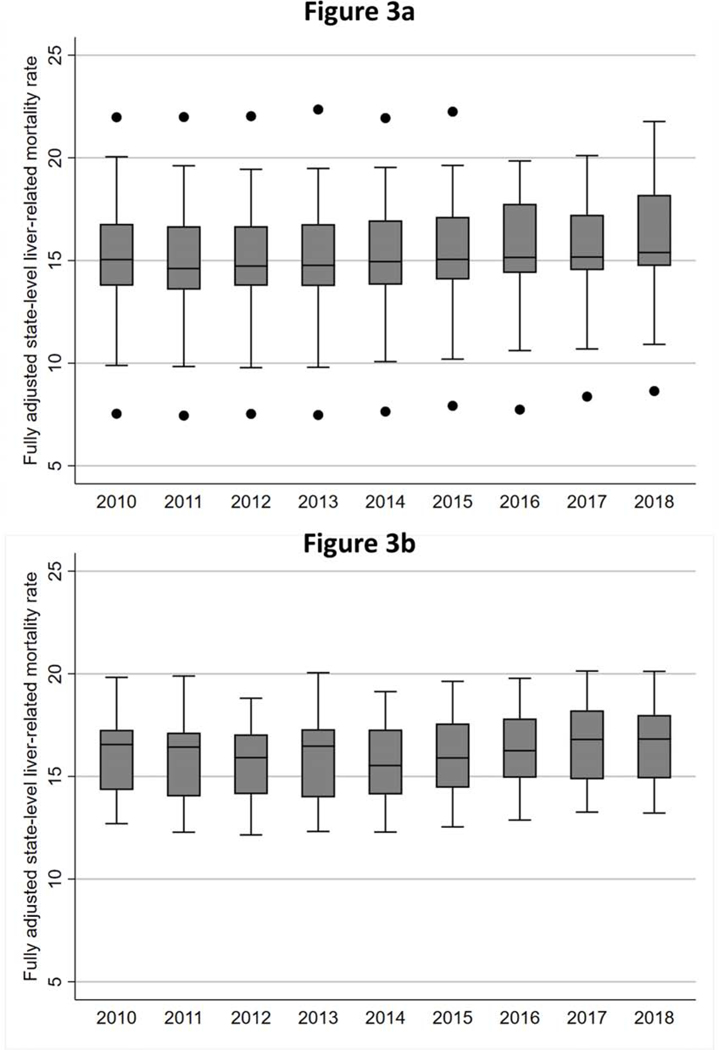
The year-to-year age-adjusted (but otherwise unadjusted) state-level liver disease-related mortality rates followed a similar pattern in expansion vs non-expansion states (Figures 2a and 2b). However, the pattern of year-to-year changes in mortality for expansion vs non-expansion states was apparent after adjusting for significant covariates (Figures 3a and 3b).
Figure 2 (two panels): Annual distribution of age-adjusted liver disease-related mortality rates in expansion and non-expansion states*.
a. Figure 2a: Annual age-adjusted liver disease-related mortality rates among expansion states
b. Figure 2b: Annual age-adjusted liver disease-related mortality rates among non-expansion states
i. * States with liver disease-related mortality rates that were outliers (>25 deaths per 100,000 population) not shown in Figures 2a (n=13), 2b (n=10)
Figure 3 (two panels): Annual distribution of fully adjusted liver disease-related mortality rates in expansion and non-expansion states*.
a. Figure 3a: Annual fully adjusted liver disease-related mortality rates among expansion states†
b. Figure 3b: Annual fully adjusted liver disease-related mortality rates among non-expansion states†
i. * States with liver disease-related mortality rates that were outliers (>25 deaths per 100,000 population) not shown in Figure 3a (n=9)
ii. † Fully adjusted mortality rates based on post-estimation values from final multivariable linear regression model
Multivariable model
In unadjusted models, the DID estimate comparing expansion vs non-expansion states was not statistically significant: −0.56 (95% CI: −1.22, 0.09; p=0.09). Yet in the multivariable model, after accounting for important confounders (Table 2), the adjusted DID estimate was statistically significant: 0.83 (95% CI: −1.51, −0.16; p=0.02). Therefore, after adjustment for socio-demographic, clinical, and access-to-care variables across the 50 states + Washington, D.C., expansion states on average had 8.3 (95% CI: 1.6–15.1) fewer deaths from liver disease per 1,000,000 adult residents per year after Medicaid expansion compared to what would have been expected to occur if those states followed the same trajectory as non-expansion states. For example, based on the adult populations ages 25–64 years in California (20.9 million) and New York (10.6 million), then an average of 175 and 88 liver disease-related deaths were averted each year between 2014–2018 in each state, respectively, due to Medicaid expansion in those states.
Table 2:
Results of multivariable linear regression model*
| Variable | Beta coefficient | P-value |
|---|---|---|
| Percentage in state female gender† | −1.75 (−2.53, −0.96) | <0.001 |
| Percentage in state Hispanic ethnicity†‡ | ||
| <10% | Reference | |
| 10–19.9% | −0.28 (−1.11, 0.56) | 0.52 |
| 20–39.9% | −0.53 (−2.41, 1.35) | 0.58 |
| ≥40% | 18.39 (12.93, 23.85) | <0.001 |
| Percentage in state living below poverty level† | 0.16 (−0.16, 0.34) | 0.075 |
| Percentage with health insurance† | −0.15 (−0.25, −0.06) | 0.001 |
| Medicaid expander state | 0.44 (−1.23, 2.11) | 0.60 |
| Post-expansion period | 2.26 (1.66, 2.87) | <0.001 |
| Medicaid expander * expansion interaction | −0.83 (−1.51, −0.16) | 0.02 |
Beta coefficient represents change in age-adjusted mortality per 100,000 population per unit change of each variable. Variables not included in the final model because they were not significant (p>0.1) in univariable or multivariable models included: median household income, Black race, unemployment, number of gastroenterologists and primary care physicians per 100,000 population
Based on 2010 data among those living at or below 138% of the federal poverty level
Hispanic ethnicity modeled as a categorical variable due to the distribu8on of the data
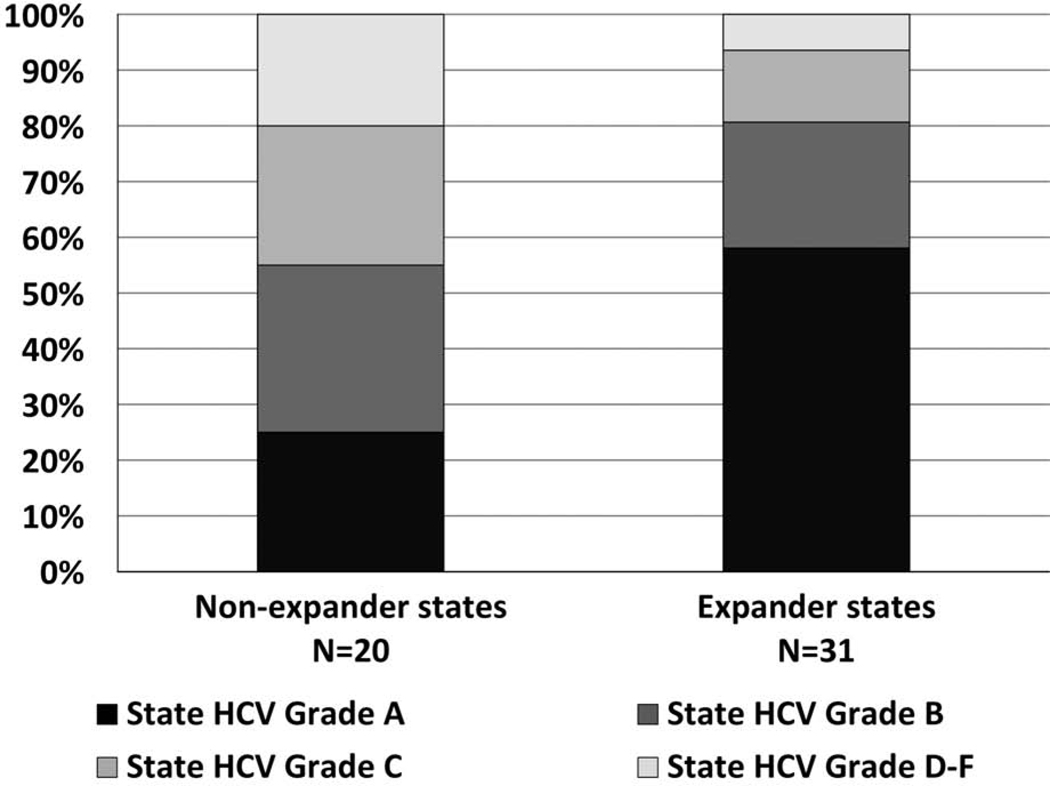
Lastly, in an exploratory analysis, we evaluated the state HCV grade of expansion vs non-expansion states based on the CHLPI report.29 Although not statistically significant (p=0.11 in chi-squared test), expansion states were more likely to have a state HCV grade of A (58.1% vs 25.0%; Figure 4). In models using only states with HCV grades A and B, the DID estimate comparing expansion vs non-expansion states was not statistically significant in univariable models: −0.16 (95% CI: −1.03, 0.7; p=0.71), or multivariable models: −0.46 (95% CI: −1.36, 0.4; p=0.30).
Figure 4: State grades for access to DAA therapy for expansion vs non-expansion states.
Discussion
States that adopted Medicaid expansion saw a significantly smaller increase in liver disease-related mortality among adults ages 25–64 when compared to states that did not expand Medicaid. By virtue of adopting Medicaid, expansion states on average saw 8.3 fewer liver disease-related deaths per million population per year than would have otherwise been expected had they not adopted Medicaid. Given the adult population ages 25–64 in these states represented an average of 105 million persons between 2014–2018 this translated to 870 fewer liver-related deaths per year, or more than 4,000 deaths in the post-expansion period under study (2014–2018). These data confirm prior studies of improvements in mortality related to cardiovascular and end-stage renal disease,3–6 and therefore further support the contention that access to insurance for the Medicaid-eligible population reaps immediate public health benefits in the form of decreased mortality.
Although previous studies have demonstrated that Medicaid expansion led to an increase in the proportion of liver transplant waitlist candidates who were Medicaid enrolles,7 the impact of Medicaid expansion on liver disease-related mortality has not been evaluated at the population-level. Several studies have demonstrated improved survival for several chronic conditions following Medicaid expansion, including cardiovascular and end-stage renal disease, at the population-level (e.g., county, state).3–6 However, beyond these epidemiologic studies at the population-level, patient-level analyses have identified potential mechanisms for improved survival with Medicaid expansion, including access to preventive outpatient care for diabetes and cardiovascular disease, in addition to high-priced inpatient care such as coronary artery bypass surgery.1,4,30,31 Although our study did not allow us to identify the specific mechanisms by which Medicaid expansion was associated with relative improvements in liver disease-related mortality, there are several plausible hypotheses.
The improvements in liver disease-related mortality in a short period of time (‘improvement’ defined as a slower increase in mortality) points towards immediate interventions to improve survival in patients with advanced liver disease, similar to the benefit seen in patients with cardiovascular disease. There are several potential mechanisms to explain our findings which would need to be confirmed in future studies. First, as previously shown, there was an increased proportion of patients waitlisted for a liver transplant with Medicaid.7 Thus access to this lifesaving procedure may have improved survival. Second, treatment of HCV, especially in patients with more advanced liver disease, improves survival in a short period of time.11,12 Medicaid expansion would likely have increased the number of HCV-infected patients who received treatment, and therefore experienced a survival benefit. Although we did not see a statistically significant difference in models limited to Grade A and B states, the point estimate (−0.46) was in a similar direction to that of the overall model (−0.83). Additionally, because state HCV grades were released in 2017, there may have been changes to DAA access between 2014–2017 that we could not fully account for. Lastly, access to specialty care (gastroenterologists and/or hepatologists), has been shown to be associated with improved care and lower mortality for patients with cirrhosis in both the outpatient and inpatient setting.13–20 As a result, by expanding the pool of insured patients with advanced liver disease, more patients would have had access to specialty care (and likely at an earlier course of their disease), which could plausibly decrease mortality in the short-term. Despite the apparent benefit of Medicaid expansion, both expansion and non-expansion states saw an increase in liver-related mortality. Liver mortality has risen, especially among younger individuals with alcohol-induced cirrhosis, and patients with cirrhosis from NAFLD/NASH.22 Moreover, though advents in HCV treatment have decreased the burden of HCV-related decompensated cirrhosis, the incidence of alcohol-induced and non-alcoholic fatty liver diseases is rising, and there is still a burden of HCC among patients previously infected with HCV.22,32
Despite the robustness of our results, our study had limitations. First, analyses were at the level of the state, rather than the patient. However, our approach is similar to other high-profile studies that explored the impact of Medicaid expansion.3–6 Second, we could not explore the potential mechanisms leading to improved survival, although we offer several potential hypotheses supported by new and/or published data. Third, other factors may have differentially affected survival of patients with advanced liver disease during this period, although we would not expect other aspects of the ACA, applied on a national level, to have differentially affected patients in expansion states. The quasi-experimental DID approach allowed us to account for other broader practice changes that could have impacted survival (e.g., our DID approach takes into account the advent of all-oral DAAs in 2014 and may be in the causal pathway of improved survival in expansion states). Fourth, specific liver etiology such as HCV/NASH cannot be assessed using death certificate data. These diagnoses are not considered the underlying cause of death, unlike cirrhosis or HCC, and they are often missing on death certificates. Lastly, our denominator was the overall population, and not specifically Medicaid-eligible persons, similar to prior studies.3–6 While this prevents us from examining whether Medicaid expansion improved survival of the Medicaid-eligible population, it still addressed our question of whether Medicaid expansion leads to decreased mortality at the state level.
In conclusion, this study demonstrates an association between Medicaid expansion and lower relative liver disease-related mortality in expansion states. Given the burden of liver disease in the Medicaid population, and ongoing debates about Medicaid expansion vs ACA repeal vs universal health insurance, these results should serve to inform policymakers considering the potential impact of broader health insurance coverage to low-income individuals.
Supplementary Material
What You Need to Know.
Background:
Data are lacking on the impact of Medicaid expansion on state-level mortality among patients with advanced liver disease.
Findings:
Although liver disease-related mortality increased in Medicaid expansion and non-expansion state, the increase in mortality was lower in Medicaid expansion states. Medicaid expansion was associated with 8.3 (95% CI: 1.6–15.1) fewer deaths from liver disease per 1,000,000 adult residents per year after Medicaid expansion compared to what would have been expected to occur if those states followed the same trajectory as non-expansion states.
Implications for patient care:
These data support the contention that Medicaid expansion has been associated with significantly decreased liver disease-related mortality. Universal Medicaid expansion could further decrease liver disease-related mortality in the US.
Acknowledgments
Dr. Goldberg receives funding from NIH R01 DK120561.
Footnotes
Conflicts of interest: None of the authors have any conflicts of interests as it relates to this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance. JAMA internal medicine. 2016;176(10):1501–1509. [DOI] [PubMed] [Google Scholar]
- 2.Kaiser Family Foundation Status of State Action on the Medicaid Expansion Decision. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaidunder-the-affordable-careact/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed July 3, 2020.
- 3.Khatana SAM, Bhatla A, Nathan AS, et al. Association of Medicaid Expansion With Cardiovascular Mortality. JAMA Cardiol. 2019;4(7):671–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Charles EJ, Johnston LE, Herbert MA, et al. Impact of Medicaid Expansion on Cardiac Surgery Volume and Outcomes. Ann Thorac Surg. 2017;104(4):1251–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akhabue E, Pool LR, Yancy CW, Greenland P, Lloyd-Jones D. Association of State Medicaid Expansion With Rate of Uninsured Hospitalizations for Major Cardiovascular Events, 2009–2014. JAMA network open. 2018;1(4):e181296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Swaminathan S, Sommers BD, Thorsness R, Mehrotra R, Lee Y, Trivedi AN. Association of Medicaid Expansion With 1-Year Mortality Among Patients With End-Stage Renal Disease. JAMA. 2018;320(21):2242–2250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tumin D, Beal EW, Mumtaz K, et al. Medicaid Participation among Liver Transplant Candidates after the Affordable Care Act Medicaid Expansion. Journal of the American College of Surgeons. 2017;225(2):173–180.e172. [DOI] [PubMed] [Google Scholar]
- 8.Bickerstaff C. The cost-effectiveness of novel direct acting antiviral agent therapies for the treatment of chronic hepatitis C. Expert Rev Pharmacoecon Outcomes Res. 2015;15(5):787–800. [DOI] [PubMed] [Google Scholar]
- 9.Lu CY, Zhang F, Golonski N, Lupton C, Jeffrey P, Wagner AK. State Medicaid Reimbursement for Medications for Chronic Hepatitis C Infection from 2012 through 2015. Value Health. 2018;21(6):692–697. [DOI] [PubMed] [Google Scholar]
- 10.Lo Re V 3rd, Gowda C, Urick PN, et al. Disparities in Absolute Denial of Modern Hepatitis C Therapy by Type of Insurance. Clinical gastroenterology and hepatology. 2016;14(7):1035–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Backus LI, Belperio PS, Shahoumian TA, Mole LA. Impact of Sustained Virologic Response with Direct-Acting Antiviral Treatment on Mortality in Patients with Advanced Liver Disease. Hepatology. 2019;69(2):487–497. [DOI] [PubMed] [Google Scholar]
- 12.Backus LI, Belperio PS, Shahoumian TA, Mole LA. Direct-acting antiviral sustained virologic response: Impact on mortality in patients without advanced liver disease. Hepatology. 2018;68(3):827–838. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Potentially Excess Deaths from the Five Leading Causes of Death in Metropolitan and Nonmetropolitan Counties — United States, 2010–2017. https://www.cdc.gov/mmwr/volumes/68/ss/ss6810a1.htm?s_cid=ss6810a1_w. Accessed August 3, 2020. [DOI] [PubMed]
- 14.Cicalese L, Shirafkan A, Jennings K, Zorzi D, Rastellini C. Increased Risk of Death for Patients on the Waitlist for Liver Transplant Residing at Greater Distance From Specialized Liver Transplant Centers in the United States. Transplantation. 2016;100(10):2146–2152. [DOI] [PubMed] [Google Scholar]
- 15.Ross K, Patzer RE, Goldberg DS, Lynch RJ. Sociodemographic Determinants of Waitlist and Posttransplant Survival Among End-Stage Liver Disease Patients. American Journal of Transplantation. 2017;17(11):2879–2889. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg DS, Newcomb C, Gilroy R, et al. Increased Distance to a Liver Transplant Center Is Associated With Higher Mortality for Patients With Chronic Liver Failure. Clinical gastroenterology and hepatology. 2017;15(6):958–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldberg DS, French B, Forde KA, et al. Association of distance from a transplant center with access to waitlist placement, receipt of liver transplantation, and survival among US veterans. JAMA. 2014;311(12):1234–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patwardhan V, Paul S, Corey KE, et al. Hepatocellular carcinoma screening rates vary by etiology of cirrhosis and involvement of gastrointestinal sub-specialists. Digestive diseases and sciences. 2011;56(11):3316–3322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bini EJ, Weinshel EH, Generoso R, et al. Impact of gastroenterology consultation on the outcomes of patients admitted to the hospital with decompensated cirrhosis. Hepatology. 2001;34(6):1089–1095. [DOI] [PubMed] [Google Scholar]
- 20.Kanwal F, Kramer JR, Buchanan P, et al. The quality of care provided to patients with cirrhosis and ascites in the Department of Veterans Affairs. Gastroenterology. 2012;143(1):70–77. [DOI] [PubMed] [Google Scholar]
- 21.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312(22):2401–2402. [DOI] [PubMed] [Google Scholar]
- 22.Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999–2016: observational study. BMJ. 2018;362:k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention; National Center for Health Statistics. Compressed Mortality File 1999–2018 on CDCWONDER online database; 2020. http://wonder.cdc.gov/cmf-icd10.html. Accessed March 3, 2020.
- 24.US Census Bureau. Small Area Income and Poverty Estimates (SAIPE) Program. https://www.census.gov/programs-surveys/saipe.html. Accessed March 3, 2020.
- 25.US Census Bureau. Small Area Health Insurance Estimates (SAHIE) Program. https://www.census.gov/programs-surveys/sahie.html. Accessed March 3, 2020.
- 26.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. https://www.cdc.gov/brfss/annual_data/annual_data.htm. Accessed March 3, 2020.
- 27.Bureau of Labor Statistics. Local Area Unemployment Statistics Home Page https://www.bls.gov/lau/. Accessed March 3, 2020.
- 28.Health Resources & Services Administration. Area Health Resources Files https://data.hrsa.gov/topics/health-workforce/ahrf. Accessed March 3, 2020.
- 29.National Viral Hepatitis Roundtable. Hepatitis C: State of Medicaid Access Report. https://nvhr.org/content/hepatitis-c-state-medicaid-access-report. Accessed July 11, 2020.
- 30.Cole MB, Galárraga O, Wilson IB, Wright B, Trivedi AN. At Federally Funded Health Centers, Medicaid Expansion Was Associated With Improved Quality Of Care. Health Aff (Millwood). 2017;36(1):40–48. [DOI] [PubMed] [Google Scholar]
- 31.McCarthy M. Medicaid expansion is associated with improved access to care and self reported health, US study finds. BMJ. 2016;354:i4455. [DOI] [PubMed] [Google Scholar]
- 32.Goldberg D, Ditah IC, Saeian K, et al. Changes in the Prevalence of Hepatitis C Virus Infection, Nonalcoholic Steatohepatitis, and Alcoholic Liver Disease Among Patients With Cirrhosis or Liver Failure on the Waitlist for Liver Transplantation. Gastroenterology. 2017;152(5):1090–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.