ABSTRACT
Although glutathione (GSH) has been shown to influence the antimicrobial effects of many kinds of antibiotics, little is known about its role in relation to trimethoprim (TMP), a widely used antifolate. In this study, several genes related to glutathione metabolism were deleted in different Escherichia coli strains (i.e., O157:H7 and ATCC 25922), and their effects on susceptibility to TMP were tested. The results showed that deleting gshA, gshB, grxA, and cydD caused TMP resistance, and deleting cydD also caused resistance to other drugs. Meanwhile, deleting gshA, grxA, and cydD resulted in a significant decrease of the periplasmic glutathione content. Supplementing exogenous GSH or further deleting glutathione importer genes (gsiB and ggt) restored TMP sensitivity to ΔcydD. Subsequently, the results of quantitative-reverse transcription PCR experiments showed that expression levels of acrA, acrB, and tolC were significantly upregulated in both ΔgrxA and ΔcydD. Correspondingly, deleting cydD led to a decreased accumulation of TMP within bacterial cells, and further deleting acrA, acrB, or tolC restored TMP sensitivity to ΔcydD. Inactivation of CpxR and SoxS, two transcriptional factors that modulate the transcription of acrAB-tolC, restored TMP sensitivity to ΔcydD. Furthermore, mutations of gshA, gshB, grxA, cydC, and cydD are highly prevalent in E. coli clinical strains. Collectively, these data suggest that reducing the periplasmic glutathione content of E. coli leads to increased expression of acrAB-tolC with the involvement of CpxR and SoxS, ultimately causing drug resistance. To the best of our knowledge, this is the first report showing a linkage between periplasmic GSH and drug resistance in bacteria.
IMPORTANCE After being used extensively for decades, trimethoprim still remains one of the key accessible antimicrobials recommended by the World Health Organization. A better understanding of the mechanisms of resistance would be beneficial for the future utilization of this drug. It has been shown that the AcrAB-TolC efflux pump is associated with trimethoprim resistance in E. coli clinical strains. In this study, we show that E. coli can sense the periplasmic glutathione content with the involvement of the CpxAR two-component system. As a result, reducing the periplasmic glutathione content leads to increased expression of acrA, acrB, and tolC via CpxR and SoxS, causing resistance to antimicrobials, including trimethoprim. Meanwhile, mutations in the genes responsible for periplasmic glutathione content maintenance are highly prevalent in E. coli clinical isolates, indicating a potential correlation of the periplasmic glutathione content and clinical antimicrobial resistance, which merits further investigation.
KEYWORDS: Escherichia coli, periplasm, glutathione, trimethoprim, resistance
INTRODUCTION
The biosynthesis of purines, thymine, glycine, methionine, and pantothenic acid requires folates as cofactors. Thus, folate is essential for all living organisms. Bacteria require de novo synthesis of folate, whereas mammals can uptake it from the environment. Therefore, the folate biosynthesis pathway is an ideal target for the design of new antimicrobial drugs (1). Trimethoprim (TMP), an antifolate that inhibits bacterial dihydrofolate reductase (DHFR), has been extensively used for decades as a broad-spectrum antibacterial drug in combination with sulfamethoxazole (SMX) (2, 3). However, the widespread use of TMP has caused increased antimicrobial resistance, similar to that occurring with other antimicrobial agents. Therefore, it has become urgent to further investigate the mechanisms of TMP resistance, which may facilitate the design of new antifolates.
Glutathione (GSH) is the major cellular thiol that protects cells against oxidative stress, and it is required for both disulfide-bond reduction and GSH-dependent peroxidase activities (4, 5). Recently, it has been proposed that GSH may contribute to antioxidant defense and redox homeostasis in the periplasm (6). In Escherichia coli, GSH is synthesized through two steps by γ-glutamyl cysteine synthetase (GshA) and GSH synthetase (GshB). Mutations in gshA and gshB are both devoid of GSH (7). Glutaredoxins (Grxs) are ubiquitous proteins that catalyze the reduction of disulfides via reduced GSH. E. coli contains three Grxs (Grx1, Grx2, and Grx3, encoded by grxA, grxB, and grxC, respectively) and two Grx-like proteins (Grx4, encoded by grxD, and NrdH). In E. coli, a continuous cycling of GSH between cells and the growth medium has been reported in exponentially growing aerobic cultures (6, 8); GsiABCD and GGT promote the uptake of GSH from the medium into the cytoplasm, and the CydDC transporter mediates the export of GSH from the cytoplasm to the periplasm.
Besides its role in maintaining cellular redox homeostasis, GSH can also influence the antimicrobial effects of different kinds of antibiotics, including beta-lactams, quinolones, and aminoglycosides (9–11). Exogenous GSH can reverse the effects of ciprofloxacin in E. coli by neutralizing ciprofloxacin-induced oxidative stress and increasing its efflux (9). Similarly, GSH-mediated protection against norfloxacin has been shown to be more efficient in the presence of the AcrAB-TolC efflux system (12). GSH-mediated protection has also been observed in aminoglycosides, such as spectinomycin. However, the decreased sensitivity of E. coli to streptomycin caused by exogenous GSH is not due to antioxidant-mediated scavenging of reactive oxygen species (11), and GSH-mediated increased antibiotic efflux is assumed to play a role in this process (13). These observations indicate the involvement of efflux systems in reversing the antimicrobial effects of antibiotics by GSH, which merits further investigation.
The AcrAB-TolC system is one of the best-characterized drug-efflux systems in E. coli, which belongs to the resistance-nodulation-cell division (RND) superfamily and has a wide range of substrates (14–16). In addition, SoxS has been shown to be a global transcriptional activator of acrAB and tolC (17, 18).
Although GSH has been shown to influence the antimicrobial effects of many drugs, whether it also affects that of TMP has remained unknown. To this aim, in the present study, several genes related to GSH biosynthesis, utilization, and transport were deleted in E. coli W3110, and their effects on TMP susceptibility were tested. Meanwhile, the effects of deleting these genes on GSH content in the bacterial periplasm were also determined. To further investigate the mechanism by which disrupting GSH metabolism affects TMP susceptibility, we measured the gene expression levels for acrAB and tolC, as well as the accumulation of TMP within bacterial cells upon drug treatment.
RESULTS
Deletion of gshA, gshB, grxA, and cydD causes resistance to multiple antimicrobial drugs in E. coli.
To elucidate the effects of GSH on TMP sensitivity in E. coli, genes involved in GSH biosynthesis (gshA and gshB), utilization (grxA, grxB, grxC, grxD, and nrdH), transport (gsiA, gsiB, gsiC, gsiD, cydC, ggt, and cydD), and recycling (gor) were knocked out in different strains of E. coli (W3110, MG1655, BW25113, O157:H7, and ATCC 25922). The results of drug susceptibility tests showed that four of the single-gene-deletion mutants (ΔgshA, ΔgshB, ΔgrxA, and ΔcydD) were resistant to TMP (MIC = 1.28 mg/L) compared with their parental strain W3110 (MIC = 0.32 mg/L) (Table 1), suggesting that GSH affected TMP sensitivity in E. coli. Furthermore, we also tested the TMP sensitivity in the gene complement strains with the pCA24N vector, and the TMP MICs of the complement strains were similar to that of the wild-type strain (Table 1). The results of TMP (4 mg/L) exposure experiments also showed that the above four mutants were more resistant to TMP treatment (Fig. S1). In addition, deleting gshA, gshB, grxA, and cydD also caused TMP resistance in other E. coli strains (BW25113, MG1655, O157:H7, and ATCC 25922) (Table S1). We also found that double gene-knockout mutants—namely, ΔcydDΔgrxA, ΔcydDΔgshA, ΔcydDΔgshB, ΔgrxAΔgshA, and ΔgrxAΔgshB—showed the same levels of TMP resistance (MIC = 1.28 mg/L) as the four single-gene knockout mutants (Table 1), indicating that decreased GSH content in the periplasmic space might cause TMP resistance in E. coli. In addition, deleting cydD also caused resistance to other antimicrobial drugs, including aminoglycosides (e.g., kanamycin, neomycin, gentamicin, spectinomycin, and streptomycin), chloramphenicol, and rifampin. We also tested the susceptibilities to other antibiotics in the complemented strain of ΔcydD. The results showed that complementing the ΔcydD mutant with an intact cydD gene could completely restore the susceptibility to TMP, largely restore the susceptibility to kanamycin and neomycin, but only partially restore the susceptibility to gentamicin (Table S2). Susceptibility to chloramphenicol was not tested in the complemented strain, since the pCA24N vector contains a chloramphenicol resistance cassette.
TABLE 1.
MICs of TMP for different strains
| Strain | MIC of TMP (μg/mL) |
|---|---|
| E. coli W3110 | 0.32 |
| E. coli W3110 ΔgshA | 1.28 |
| E. coli W3110 ΔgshB | 1.28 |
| E. coli W3110 ΔgrxA | 1.28 |
| E. coli W3110 ΔcydD | 1.28 |
| E. coli W3110 ΔcydDΔgrxA | 1.28 |
| E. coli W3110 ΔcydDΔgshA | 1.28 |
| E. coli W3110 ΔcydDΔgshB | 1.28 |
| E. coli W3110 ΔgrxAΔgshA | 1.28 |
| E. coli W3110 ΔgrxAΔgshB | 1.28 |
| E. coli W3110 pCA24N | 0.32 |
| E. coli W3110 ΔgshA pCA24N | 1.28 |
| E. coli W3110 ΔgshB pCA24N | 1.28 |
| E. coli W3110 ΔgrxA pCA24N | 1.28 |
| E. coli W3110 ΔcydD pCA24N | 1.28 |
| E. coli W3110 ΔgshA pCA24N::gshA | 0.16 |
| E. coli W3110 ΔgshB pCA24N::gshB | 0.32 |
| E. coli W3110 ΔgrxA pCA24N::grxA | 0.32 |
| E. coli W3110 ΔcydD pCA24N::cydD | 0.32 |
Mutations of gshA, gshB, grxA, cydC, and cydD are highly prevalent in E. coli clinical strains.
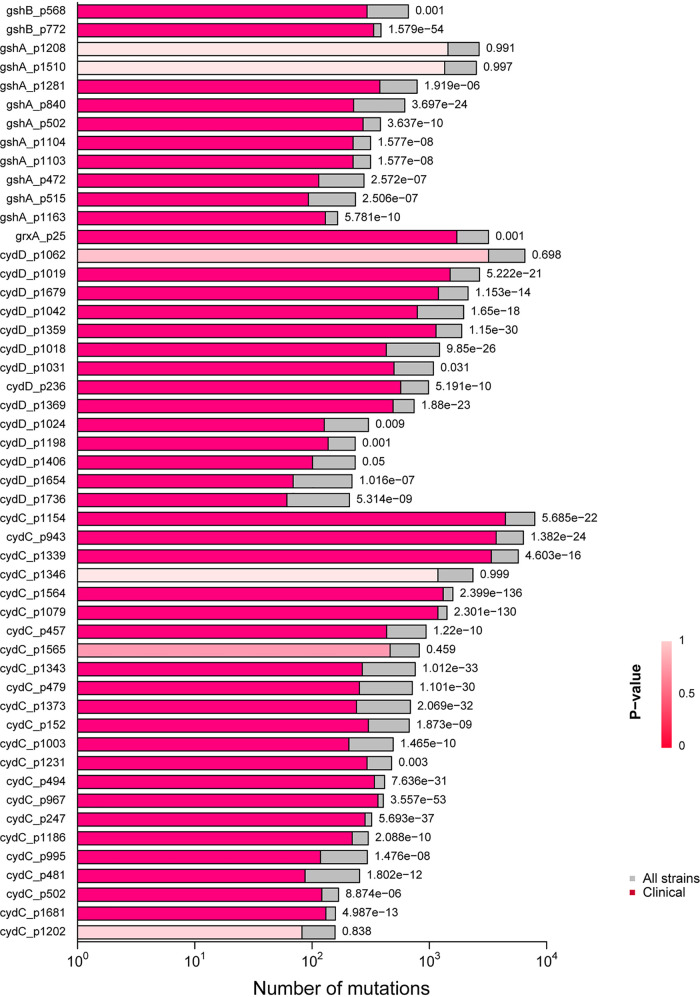
Our data showed that reducing the periplasmic GSH content through deleting gshA, gshB, grxA, cydC, or cydD made E. coli resistant to TMP. To further probe the clinical relevance of this observation, we analyzed a genome database of pathogenic E. coli downloaded from NCBI according to the research of Lopatkin et al. (19), searched for mutations in the coding region of gshA, gshB, grxA, cydD, and cydC (Table S3), and finally picked up the top 50 mutation sites to draw the graphics (Fig. 1). For example, the mutation cydD_p1679 (CGG, R->CAG, Q) was found in 2,137 of 7,992 pathogenic strains, and 1,195 of 3,903 were designated clinical strains (P < 0.001, Fisher’s exact test) (Table S3). Overall, all of the five genes had many mutations in the pathogenic strains and showed a high proportion in the clinical strains, although the gene mutations may not necessarily mean the loss of gene function.
FIG 1.
Horizontal bar chart showing the high prevalence of mutations of gshA, gshB, grxA, cydD, and cydC in clinical E. coli strains. The coding mutations of E. coli gshA, gshB, grxA, cydC, and cydD were searched in a genome database of pathogenic E. coli strains downloaded from NCBI. The bars in shades of red indicate the number of strains with the specific mutation in clinical strains, and those in gray indicate the values for all strains. The P value of each mutation within the subset of clinical strains is indicated next to each bar; the reddish bars are shaded from dark to light red to indicate high significance to not significant, respectively. The x axis represents the number of mutations, and the y axis labels consist of the gene name and the position of the mutation.
Deletion of gshA, grxA, and cydD leads to decreased GSH content in the periplasm.
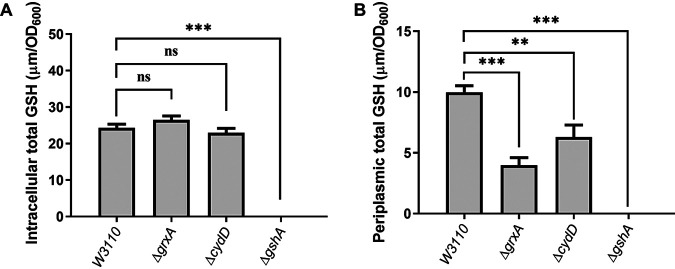
To further test the hypothesis that decreasing GSH content in the periplasmic space causes TMP resistance in E. coli, GSH levels in both the intracellular space and periplasm were compared among ΔgshA, ΔgrxA, ΔcydD, and W3110. As expected, deleting gshA led to significantly decreased GSH levels in both the intracellular and periplasmic spaces (Fig. 2A, Table S4). In contrast, deleting grxA and cydD only led to significantly decreased GSH levels in the periplasm (60% decrease for ΔgrxA and 37% decrease for ΔcydD) (Fig. 2B, Table S4). In addition, the TMP-resistant phenotypes of ΔgshA, ΔgshB, ΔgrxA, and ΔcydD were partially or completely reversed by the addition of exogenous GSH (Table S5). These data suggested that decreasing GSH content in the periplasm causes TMP resistance in E. coli W3110.
FIG 2.
GSH content in E. coli W3110, ΔgrxA, ΔcydD, and ΔgshA. (A) Intracellular concentrations of total GSH. (B) Concentrations of total GSH in the periplasm. DTNB [5,5′-dithiobis-(2-nitrobenzoic acid)] assays were used to quantify GSH levels, which were normalized by the optical density at 600 nm (OD600). The data represent the mean ± standard deviation (SD) from three independent experiments. P values were calculated using t tests (**, P < 0.01; ***, P < 0.001; ns, not significant).
Further inactivation of GSH importers restores TMP sensitivity to ΔcydD.
In E. coli, although CydDC is the only known transporter that exports GSH from the cytoplasm to the periplasm (20), several importers (e.g., GsiABCD and GGT) are involved in importing extracellular GSH into the cytoplasm to maintain the periplasmic concentration of GSH at an optimal level together with that of CydDC (6, 21). To further test the hypothesis that decreasing GSH content in the periplasm causes TMP resistance in E. coli, we knocked out gsiA, gsiB, gsiAB, gsiC, gsiD, and ggt in both W3110 and ΔcydD. The results of the subsequent TMP susceptibility tests showed that although the deletion of all these genes had no effects on TMP sensitivity in E. coli W3110, further deleting gsiB and ggt restored TMP sensitivity to ΔcydD (Table 2), demonstrating a connection between the periplasmic GSH content and TMP susceptibility.
TABLE 2.
MICs of TMP for GSH efflux-related mutant strains
| Strain | MIC for TMP (μg/mL) |
|---|---|
| E. coli W3110 | 0.32 |
| E. coli W3110 ΔgsiA | 0.32 |
| E. coli W3110 ΔgsiB | 0.32 |
| E. coli W3110 ΔgsiAB | 0.32 |
| E. coli W3110 Δggt | 0.32 |
| E. coli W3110 ΔgsiC | 0.32 |
| E. coli W3110 ΔgsiD | 0.32 |
| E. coli W3110 ΔcydDΔgsiA | 1.28 |
| E. coli W3110 ΔcydDΔgsiB | 0.32 |
| E. coli W3110 ΔcydDΔgsiAB | 0.32 |
| E. coli W3110 ΔcydDΔggt | 0.32 |
| E. coli W3110 ΔcydDΔgsiC | 1.28 |
| E. coli W3110 ΔcydDΔgsiD | 1.28 |
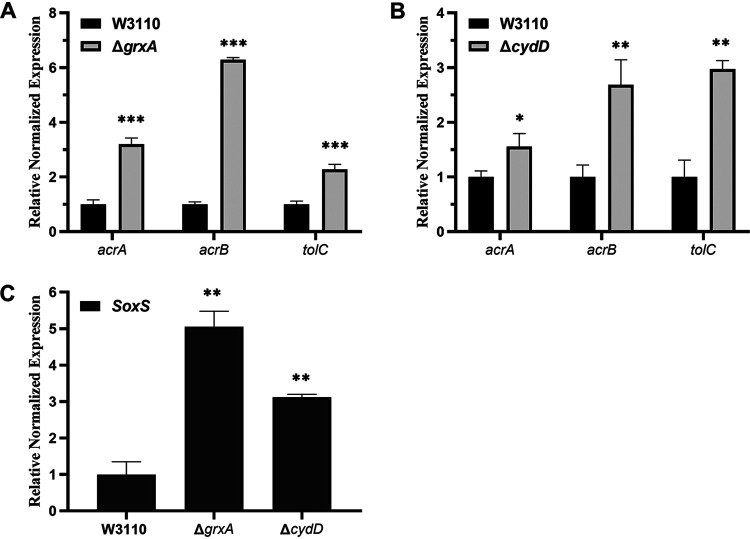
Deletion of grxA and cydD leads to increased expression of acrAB, tolC, and SoxS.
Since previous studies have indicated the involvement of the AcrAB-TolC efflux system in GSH-mediated protection against antibiotics (12), we investigated whether this system also played a role in TMP-resistant phenotypes caused by grxA and cydD gene deletions. The results of reverse transcription-quantitative PCR (RT-qPCR) experiments showed that the deletion of grxA and cydD both caused significantly increased expression levels of acrA, acrB, and tolC (Fig. 3). Specifically, 3.20-, 6.29-, and 2.28-fold increases in acrA, acrB, and tolC levels, respectively, were observed in the grxA deletion mutant (Fig. 3A, Table S6), and corresponding 1.55-, 2.69-, and 2.97-fold increases were observed in the cydD deletion mutant, compared with those in the wild-type strain W3110 (Fig. 3B, Table S6). Meanwhile, as SoxS is one of the transcriptional factors modulating the expression levels of acrAB and tolC (14, 17), we also found that the expression level of the soxS gene was also upregulated by 5.05- and 3.12-fold in the grxA and cydD deletion mutants, respectively (Fig. 3C, Table S6).
FIG 3.
Relative expression levels of acrAB, tolC, and soxS via RT-qPCR. (A) Expression levels of acrAB and tolC in E. coli W3110 and ΔgrxA. (B) Expression levels of acrAB and tolC in E. coli W3110 and ΔcydD. (C) Expression levels of soxS in E. coli W3110, ΔgrxA, and ΔcydD. The resulting cycle threshold (CT) values were normalized using gapA as the reference gene. The data represent the mean ± SD from three independent experiments. P values were calculated using t tests (*, P < 0.05; **, P < 0.01; ***, P < 0.001).
Inactivating the AcrAB-TolC efflux system restores TMP sensitivity to ΔgrxA and ΔcydD.
To further investigate the involvement of the AcrAB-TolC efflux system in TMP-resistant phenotypes caused by grxA and cydD gene deletions, the acrA, acrB, and tolC genes were knocked out in the wild-type strain W3110, as well as in ΔgrxA and ΔcydD. The results of the subsequent TMP susceptibility tests revealed that deleting acrA, acrB, and tolC in the wild-type strain each caused increased sensitivity to TMP, and the further deletion of acrA completely reversed the TMP-resistant phenotypes of ΔgrxA and ΔcydD (Table 3). The further deletion of acrB and tolC partially reversed the TMP-resistant phenotypes of ΔgrxA and ΔcydD. These data suggest that the AcrAB-TolC efflux system was involved in the TMP-resistant phenotypes caused by grxA and cydD gene deletions.
TABLE 3.
Effects of deletion mutants of efflux-pump genes on TMP sensitivity
| Strain | MIC for TMP (μg/mL) |
|---|---|
| E. coli W3110 | 0.32 |
| E. coli W3110 ΔcydD | 1.28 |
| E. coli W3110 ΔacrA | 0.08 |
| E. coli W3110 ΔacrB | 0.04 |
| E. coli W3110 ΔtolC | 0.16 |
| E. coli W3110 ΔcydDΔacrA | 0.08 |
| E. coli W3110 ΔcydDΔacrB | 0.16 |
| E. coli W3110 ΔcydDΔtolC | 0.16 |
| E. coli W3110 ΔgrxAΔacrA | 0.08 |
| E. coli W3110 ΔgrxAΔtolC | 0.16 |
| E. coli W3110 ΔgshAΔacrA | 0.08 |
| E. coli W3110 ΔgshAΔtolC | 0.32 |
| E. coli W3110 ΔgshBΔacrA | 0.08 |
Deletion of soxS and cpxR restores TMP sensitivity to ΔcydD.
The above findings demonstrate that decreasing periplasmic GSH by deleting grxA and cydD led to increased expression levels of acrA, acrB, and tolC, which subsequently caused TMP resistance. To further investigate how changes in GSH content in the periplasm affect the transcription of acrA, acrB, and tolC—which usually occurs in the cytoplasm—two transcriptional-factor-coding genes, soxS and cpxR, were deleted in W3110 and ΔcydD. The results of drug susceptibility tests showed that although deleting soxS and cpxR only led to slightly increased sensitivity to TMP, these deletions fully restored TMP susceptibility to ΔcydD (Table 4), suggesting that SoxS and CpxR were involved in transferring GSH content from the periplasm into the cytoplasm. In addition, the further deletion of cpxR in ΔcydD caused significant decreases in the expression levels of acrA, acrB, tolC, and soxS (Fig. 4, Table S6).
TABLE 4.
TMP MICs for the cpxAR and soxS gene mutants in ΔcydD
| Strain | MIC of TMP (μg/mL) |
|---|---|
| E. coli W3110 | 0.32 |
| E. coli W3110 ΔcydD | 1.28 |
| E. coli W3110 ΔcpxA | 2.56 |
| E. coli W3110 ΔcpxR | 0.16 |
| E. coli W3110 ΔcpxAΔcpxR | 0.32 |
| E. coli W3110 ΔsoxS | 0.16 |
| E. coli W3110 ΔcydDΔcpxA | 1.28 |
| E. coli W3110 ΔcydDΔcpxR | 0.32 |
| E. coli W3110 ΔcydDΔsoxS | 0.16 |
FIG 4.
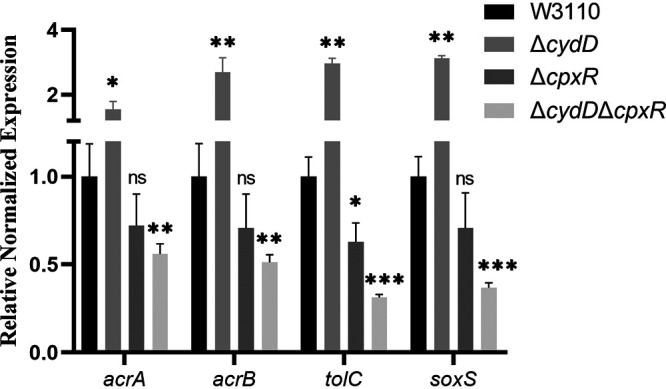
Relative expression levels of acrAB, tolC, and SoxS in E. coli ΔcpxR and ΔcydDΔcpxR via RT-qPCR. The resulting CT values were normalized using gapA as the reference gene. The data represent the mean ± SD from three independent experiments. P values were calculated using t tests (*, P < 0.05; **, P < 0.01; ***, P < 0.001; ns, not significant).
Deletion of cydD leads to decreased accumulation of TMP following TMP treatment.
Since the AcrAB-TolC efflux system has been shown to be involved in the TMP-resistant phenotype caused by grxA and cydD gene deletions, the accumulated levels of TMP between different strains were compared through liquid chromatography-mass spectrometry (LC-MS) analysis. As shown in Fig. 5 (Table S7), the deletion of cydD caused a significantly decreased accumulation of TMP within the bacterial cells, which was reversed by the further deletion of acrA and tolC. In contrast, deleting acrA, acrB, and tolC in W3110 each led to increased accumulation of TMP within the bacterial cells following TMP treatment.
FIG 5.
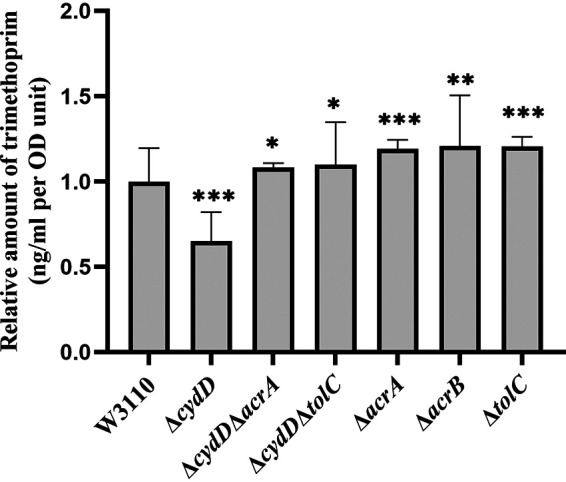
Column chart representing the relative E. coli intracellular levels of TMP after challenging with 1 mg/L of the drug compared with the control sample W3110 detected by LC-MS analysis; the relative concentration levels of TMP were normalized to the OD600 readings. Six replicates were used for each strain, and the data represent the mean ± SD from three independent experiments. P values were calculated using t tests (*, P < 0.05; **, P < 0.01; ***, P < 0.001).
DISCUSSION
Many studies have shown that GSH influences the effects of different types of antimicrobial drugs. As one of the two thiol-dependent antioxidant systems in bacteria, the GSH system participates in the direct detoxification of reactive oxygen species, which has been suggested to play an important role in the bactericidal effects of many drugs, including TMP (9, 22). In contrast, GSH also seems to protect bacterial cells against some antibiotics with the involvement of drug efflux (12, 23). TMP, in combination with sulfamethoxazole (SMX), is one of the most commonly used antimicrobial drugs recommended by the World Health Organization. At present, the interplay between TMP and GSH has not been examined in bacteria. Here, we found that GSH influenced the antimicrobial effects of TMP, since disrupting its biosynthesis, utilization, and transport resulted in TMP resistance in E. coli.
Among the four genes related to GSH metabolism, gshA and gshB encode the two enzymes required for GSH biosynthesis in E. coli, grxA encodes one of the three glutaredoxins, and cydD encodes one subunit of the CydDC transporter, the latter of which is the only known transporter responsible for transporting GSH from the cytoplasm into the periplasm (20). Interestingly, the four mutants (ΔgshA, ΔgshB, ΔgrxA, and ΔcydD) showed the same levels of TMP resistance compared with that of their parental strain. This led us to speculate that all four mutants shared a common mechanism of TMP resistance, namely, that decreased GSH content in the periplasm causes TMP resistance. If this hypothesis is true, then any double-knockout mutant of the three genes (gshA, grxA, and cydD) should show the same level of TMP resistance as that of any corresponding single-gene knockout mutants, which our present results confirmed. Our hypothesis was further confirmed by the fact that the deletion of gshA, grxA, and cydD each led to a significant decrease in the periplasmic GSH content. Deleting gshA blocks the biosynthesis of GSH in E. coli and consequently decreases the periplasmic GSH content to a markedly low level. We found that deleting grxA caused a significant decrease in the periplasmic GSH content but only a slight increase in the intracellular GSH content. Although deleting cydD resulted in a significant decrease in the periplasmic GSH content, this decrease was less than that caused by deleting gshA and grxA. These data suggest the following in E. coli: (i) the majority of GSH in the periplasm is exported from the cytoplasm; (ii) CydDC is not the only exporter of GSH; and (iii) Grx1 modulates the export of GSH from the cytoplasm into the periplasm. Surprisingly, the deletion of cydD also caused a slight decrease in the intracellular GSH content. Previously, Holyoake et al. showed that deleting cydD in E. coli led to decreased expression of the CysB regulon (24), which is involved in the biosynthesis and transport of cysteine, one of the precursors for GSH biosynthesis. We thus reasoned that the decreased production and uptake of cysteine caused by cydD deletion might lead to decreased biosynthesis of GSH.
Despite our present findings, it remains unclear as to how decreased GSH content in the periplasm leads to TMP resistance in E. coli. Previously, Jawali et al. showed that antibiotic-efflux machinery is involved in GSH-mediated decreased ciprofloxacin activity in E. coli (23). In our present study, through RT-qPCR analysis, we found that deleting cydD and grxA led to increased gene expression of acrAB and tolC. In addition, the further deletion of acrA completely reversed the TMP-resistant phenotypes of ΔcydD and ΔgrxA, confirming that increased expression levels of acrAB and tolC caused TMP resistance in these two mutants. Increased expression levels of acrAB and tolC resulted in augmented efflux and diminished accumulation of TMP within the bacterial cells when treated with TMP, which is the direct cause of TMP resistance.
At present, it is unclear whether GSH affects the redox status of the periplasm, although some previous studies have provided related insights (6, 25). Although we found that decreased GSH content in the periplasm of E. coli led to increased expression of genes coding for the AcrAB-TolC drug-efflux pump, it remains unclear as to how bacteria transfer the information about fluctuations in the periplasmic GSH content into the cytoplasm, where transcription occurs. Fortunately, previous studies have already identified several transcriptional factors that modulate the expression of acrAB and tolC, including SoxS, one of the global regulators of multidrug resistance in E. coli (18, 26). Our RT-qPCR analysis data revealed that the gene expression levels of soxS were upregulated in the grxA and cydD deletion mutants compared to the wild-type strain, suggesting that elevated expression of SoxS activated the expression of acrAB and tolC. Additionally, the further deletion of soxS fully restored TMP sensitivity to the cydD deletion mutant, confirming the role of SoxS in mediating TMP resistance. However, there was no evidence showing the presence of SoxS in the periplasm or its shuttling between the cytoplasm and periplasm, indicating the involvement of other transcription factors that may interplay with GSH in the periplasmic space and thus affect the expression of soxS. CpxR is a response regulator in the CpxAR two-component system, which has been shown to sense and respond to the stress of periplasmic proteins misfolding and aggregating (27). Previously, Huang et al. showed that overexpression of CpxR in the cpxR deletion mutant of Salmonella enterica serovar Typhimurium resulted in the decreased expression of soxS, acrB, and tolC (28), indicating a role of CpxR in modulating the expression of arcB and tolC via SoxS. Our present data showed that the further deletion of cpxR led to significantly decreased expression of soxS, acrA, acrB, and tolC, thus restoring TMP sensitivity to the cydD deletion mutant and confirming the role of CpxR in mediating the TMP-resistant phenotype. Currently, there is no evidence showing that CpxR can directly modulate the expression of acrA, acrB, and tolC in E. coli. Based on our own present findings in combination with previous observations, we reasoned that decreasing the GSH content in the periplasm may activate the CpxAR two-component system, which would then upregulate the expression of soxS; increased expression of soxS would then cause increased expression of acrAB and tolC. Hence, the E. coli organism would then sense fluctuations in the GSH content in the periplasm and transduce this signal from the periplasm into the cytoplasm. However, future studies are required to elucidate how CpxR modulates the expression of soxS, acrA, acrB, and tolC.
In addition, we found that deleting gshA, gshB, grxA, or cydD also caused TMP resistance in pathogenic E. coli strains (O157:H7 and ATCC 25922). By analyzing a genome database of pathogenic E. coli downloaded from NCBI, we also found that mutations of these four genes are highly prevalent in E. coli clinical strains, indicating that mutations of these four genes may be associated with resistance to antimicrobial drugs, including TMP. Further studies are required to explore the physiological consequence of these mutations and to verify our hypothesis.
In summary, we found that decreasing the periplasmic GSH content in E. coli led to the increased expression of soxS via CpxR, which then activated the expression of genes coding for the AcrAB-TolC efflux pump, ultimately causing TMP resistance. Thus, we identified a novel interplay between periplasmic GSH and drug susceptibility in E. coli. In addition, our findings provide the first evidence that signals reflecting fluctuations in periplasmic GSH content in E. coli can be transduced from the periplasmic space into the cytoplasm with the involvement of SoxS and CpxAR, which merits further investigation.
MATERIALS AND METHODS
Construction of bacterial strains and culture conditions.
The strains used in the present study were derivatives of E. coli K-12 W3110, MG1655, and BW25113, which were obtained from laboratory stock. The enterohemorrhagic E. coli (EHEC) strain O157:H7 was purchased from the China Center of Industrial Culture Collection (CICC) and numbered CICC 21530, and the standard strain ATCC 25922 was obtained from Qingdao Rishui Bio-Technologies Co., Ltd. All strains were grown in LB medium. The gene knockout mutants were constructed using the λ-red recombination system, as previously described (29). The mutants were verified by junction PCR and subsequent sequencing using primers that anneal to the genomic region outside the recombination locus. The double knockout mutants were generated using the same procedures, except that the kanamycin-resistance gene of the single-gene knockout mutant was first eliminated by transforming the plasmid pCP20. The gene-complemented strains of all of the mutants were constructed as follows: the target gene was amplified and cloned into the pCA24N vector and then transformed into the corresponding mutant strain. All plasmids, primers, and strains that we used are listed in Table S9.
Preparation of reagents and drug susceptibility tests.
The reagents used in this study, including TMP and GSH, were purchased from Sigma-Aldrich. All reagents were solubilized according to the manufacturer’s recommendations, and stock solutions were filter-sterilized and stored in aliquots at −20°C.
For drug susceptibility tests, bacterial cells were grown to an optical density at 600 nm (OD600) of 0.8 and were diluted to approximately 105 CFU/mL via 10-fold serial dilutions in fresh LB. Then, 10-fold serial dilutions were plated onto solid LB agar plates containing various concentrations of different tested drugs. The plates were incubated overnight at 37°C. The MIC was defined as the lowest concentration of a given compound required to inhibit the growth of 99% of bacterial CFU.
Measurement of the growth curve and the time-kill curve.
Bacterial cells were grown to the mid-log phase (OD600, ∼0.8) and diluted to an OD600 of 0.1 in fresh LB medium; then, approximately 106 CFU/mL was set as the initial bacteria amount. Bacterial cells were grown aerobically at 37°C. For the bacterial growth curve, the OD600 was continuously observed using a Synergy H1 hybrid reader (BioTek, USA) with shaking at 150 rpm. For the TMP (4 mg/L) exposure experiment, static cultivation serial dilutions were performed before plating onto LB plates.
Comparative analysis of target gene mutations in an NCBI genome database of pathogenic E. coli.
Following the method of Lopatkin et al., we downloaded a genome database of pathogenic E. coli from NCBI, which contains 10,906 genomes classified as clinical, environmental, or other (19). We then mapped the target coding sequence of E. coli W3110 gshA, gshB, grxA, cydC, and cydD using the alignment software minimap2 to extract variation information. Specifically, we used the python module pysam to extract the base information of each genome for each gene locus, respectively, and to retain single-nucleotide polymorphism (SNP) and indel information. Then, comparative analysis of the variation information associated with the phenotype and statistics of the proportion of mutations in the clinical strains were performed using Fisher’s test with the R programming language. We filtered out the nonsense mutations in the process and finally picked up the top 50 mutation sites to draw graphics.
Periplasm separation and GSH measurements.
Periplasmic fractions were isolated using a modified osmotic-shock procedure (20). In brief, bacterial cells were grown to the mid-log phase (OD600, ∼0.8), harvested by centrifugation (3,000 × g for 10 min at 4°C), resuspended in 1 mL supernatant solution, and then supplemented with an equal volume of 20% (wt/vol) sucrose solution containing 10 mM Tris-HCl (pH 8.0). Subsequently, lysozyme (final concentration, 50 μg/mL) and EDTA (final concentration, 1 mM) were added. After incubation on ice for 30 min, centrifugation (10,000 × g for 5 min at 4°C) was performed, and then the pellets were collected and resuspended in 10 mM Tris-HCl (pH 8.0). After incubation on ice for 30 min, centrifugation (12,000 × g for 10 min at 4°C) yielded a supernatant fraction that was retained as the periplasmic fraction.
The periplasmic GSH levels were measured using a total GSH assay kit (Beyotime Biotech) according to the manufacturer’s instructions. The periplasmic-fraction supernatant was treated with DTNB [5,5′-dithiobis-(2-nitrobenzoic acid)] in combination with GSH reductase enzyme and NADPH. Finally, the absorbance values were measured at a wavelength of 412 nm, using a Synergy H1 hybrid reader (BioTek). The GSH levels were quantified against a corresponding standard curve.
RT-qPCR.
The expression levels of acrA, acrB, and tolC were compared between the wild-type strain and mutant strains via RT-qPCR. All bacterial cells were grown in LB broth to the mid-log phase (OD600, ∼0.8). Total RNA was isolated using an RNeasy kit (Qiagen, Germany), and cDNA was synthesized with a ReverTra Ace qPCR kit (Toyobo) according to the manufacturer’s instructions. Quantification of gene expression levels was performed using real-time qPCR analysis on a 7900HT sequence-detection system (ABI, USA) with ABI Power SYBR green PCR master mix. The primers were designed and synthesized by the Shanghai Biotechnology Corporation. We used the comparative cycle threshold (CT) value method for RT-PCR in this study; the resulting CT values were normalized using gapA as the reference gene, and the final relative gene expression level was normalized using the wild-type strain (23). Detailed information about the primers is given in Table S9 of the supplemental material.
Quantification of intracellular TMP levels in E. coli via liquid chromatography-mass spectrometry.
The bacterial intracellular TMP levels were estimated using liquid chromatography-mass spectrometry (LC-MS), and intracellular TMP quantification from E. coli was performed as previously described (30). In brief, all tested E. coli strains were grown in LB broth to the mid-log phase (OD600 ∼0.8), washed once with fresh LB broth, diluted to an OD600 of approximately 0.2, and then challenged with 1 mg/L of TMP. After incubation at 37°C on a shaker (200 rpm) for 30 min, 10 mL of each culture was collected for metabolic quenching. For each sample, a double volume of 60% cold methanol was added, and cellular pellets were collected by centrifugation (1800 g for 10 min) for the subsequent extraction of metabolites. The cellular pellets were resuspended in 1 mL 80% cold methanol, and three rounds of freeze-thawing were performed to maximize the extraction of intracellular metabolites. The samples extracted from intracellular fractions were then subjected to LC-MS analysis, and the TMP reference standard was obtained against the appropriate concentration level. The details of these methods are provided in Table S8 and in the supplemental material for LC-MS. The TMP levels within the intracellular extracts were inferred against the standard curve, and the intracellular concentration levels were normalized to the OD600 readings taken from the original bacterial cultures.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by the Strategic Priority Research Program of the Chinese Academy of Sciences (grant number XDB29020000).
We thank LetPub for linguistic assistance during the preparation of the manuscript.
Footnotes
Supplemental material is available online only.
Contributor Information
Jiaoyu Deng, Email: dengjy@wh.iov.cn.
Hui Wang, Peking University People’s Hospital.
REFERENCES
- 1.Bermingham A, Derrick JP. 2002. The folic acid biosynthesis pathway in bacteria: evaluation of potential for antibacterial drug discovery. Bioessays 24:637–648. doi: 10.1002/bies.10114. [DOI] [PubMed] [Google Scholar]
- 2.Kwon YK, Lu W, Melamud E, Khanam N, Bognar A, Rabinowitz JD. 2008. A domino effect in antifolate drug action in Escherichia coli. Nat Chem Biol 4:602–608. doi: 10.1038/nchembio.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huovinen P, Sundstrom L, Swedberg G, Skold O. 1995. Trimethoprim and sulfonamide resistance. Antimicrob Agents Chemother 39:279–289. doi: 10.1128/AAC.39.2.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galano A, Alvarez-Idaboy JR. 2011. Glutathione: mechanism and kinetics of its non-enzymatic defense action against free radicals. RSC Adv Advances 1:1763. doi: 10.1039/c1ra00474c. [DOI] [Google Scholar]
- 5.Kalinina EV, Chernov NN, Novichkova MD. 2014. Role of glutathione, glutathione transferase, and glutaredoxin in regulation of redox-dependent processes. Biochemistry (Mosc) 79:1562–1583. doi: 10.1134/S0006297914130082. [DOI] [PubMed] [Google Scholar]
- 6.Smirnova G, Muzyka N, Oktyabrsky O. 2012. Transmembrane glutathione cycling in growing Escherichia coli cells. Microbiol Res 167:166–172. doi: 10.1016/j.micres.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 7.Carmel-Harel O, Storz G. 2000. Roles of the glutathione- and thioredoxin-dependent reduction systems in the Escherichia coli and Saccharomyces cerevisiae responses to oxidative stress. Annu Rev Microbiol 54:439–461. doi: 10.1146/annurev.micro.54.1.439. [DOI] [PubMed] [Google Scholar]
- 8.Suzuki H, Koyanagi T, Izuka S, Onishi A, Kumagai H. 2005. The yliA, -B, -C, and -D genes of Escherichia coli K-12 encode a novel glutathione importer with an ATP-binding cassette. J Bacteriol 187:5861–5867. doi: 10.1128/JB.187.17.5861-5867.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goswami M, Mangoli SH, Jawali N. 2006. Involvement of reactive oxygen species in the action of ciprofloxacin against Escherichia coli. Antimicrob Agents Chemother 50:949–954. doi: 10.1128/AAC.50.3.949-954.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goswami M, Jawali N. 2007. Glutathione-mediated augmentation of beta-lactam antibacterial activity against Escherichia coli. J Antimicrob Chemother 60:184–185. doi: 10.1093/jac/dkm121. [DOI] [PubMed] [Google Scholar]
- 11.Goswami M, Mangoli SH, Jawali N. 2007. Effects of glutathione and ascorbic acid on streptomycin sensitivity of Escherichia coli. Antimicrob Agents Chemother 51:1119–1122. doi: 10.1128/AAC.00779-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dhamdhere G, Krishnamoorthy G, Zgurskaya HI. 2010. Interplay between drug efflux and antioxidants in Escherichia coli resistance to antibiotics. Antimicrob Agents Chemother 54:5366–5368. doi: 10.1128/AAC.00719-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goswami M, Jawali N. 2016. Glutathione-mediated reversal of streptomycin susceptibility is refractory to the status of glutathione-S-transferase (gst) or translational fidelity of Escherichia coli. J Glob Antimicrob Resist 7:59–60. doi: 10.1016/j.jgar.2016.07.009. [DOI] [PubMed] [Google Scholar]
- 14.Weston N, Sharma P, Ricci V, Piddock LJV. 2018. Regulation of the AcrAB-TolC efflux pump in Enterobacteriaceae. Res Microbiol 169:425–431. doi: 10.1016/j.resmic.2017.10.005. [DOI] [PubMed] [Google Scholar]
- 15.Nikaido H, Zgurskaya HI. 2001. AcrAB and related multidrug efflux pumps of Escherichia coli. J Mol Microbiol Biotechnol 3:215–218. [PubMed] [Google Scholar]
- 16.Aono R, Tsukagoshi N, Yamamoto M. 1998. Involvement of outer membrane protein TolC, a possible member of the mar-sox regulon, in maintenance and improvement of organic solvent tolerance of Escherichia coli K-12. J Bacteriol 180:938–944. doi: 10.1128/JB.180.4.938-944.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Perez A, Poza M, Aranda J, Latasa C, Medrano FJ, Tomas M, Romero A, Lasa I, Bou G. 2012. Effect of transcriptional activators SoxS, RobA, and RamA on expression of multidrug efflux pump AcrAB-TolC in Enterobacter cloacae. Antimicrob Agents Chemother 56:6256–6266. doi: 10.1128/AAC.01085-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenberg EY, Bertenthal D, Nilles ML, Bertrand KP, Nikaido H. 2003. Bile salts and fatty acids induce the expression of Escherichia coli AcrAB multidrug efflux pump through their interaction with Rob regulatory protein. Mol Microbiol 48:1609–1619. doi: 10.1046/j.1365-2958.2003.03531.x. [DOI] [PubMed] [Google Scholar]
- 19.Lopatkin AJ, Bening SC, Manson AL, Stokes JM, Kohanski MA, Badran AH, Earl AM, Cheney NJ, Yang JH, Collins JJ. 2021. Clinically relevant mutations in core metabolic genes confer antibiotic resistance. Science 371:eaba0862. doi: 10.1126/science.aba0862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pittman MS, Robinson HC, Poole RK. 2005. A bacterial glutathione transporter (Escherichia coli CydDC) exports reductant to the periplasm. J Biol Chem 280:32254–32261. doi: 10.1074/jbc.M503075200. [DOI] [PubMed] [Google Scholar]
- 21.Smirnova GV, Tyulenev AV, Muzyka NG, Oktyabrsky ON. 2020. Study of the relationship between extracellular superoxide and glutathione production in batch cultures of Escherichia coli. Res Microbiol 171:301–310. doi: 10.1016/j.resmic.2020.07.004. [DOI] [PubMed] [Google Scholar]
- 22.Goswami M, Jawali N. 2010. N-acetylcysteine-mediated modulation of bacterial antibiotic susceptibility. Antimicrob Agents Chemother 54:3529–3530. doi: 10.1128/AAC.00710-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goswami M, Subramanian M, Kumar R, Jass J, Jawali N. 2016. Involvement of antibiotic efflux machinery in glutathione-mediated decreased ciprofloxacin activity in Escherichia coli. Antimicrob Agents Chemother 60:4369–4374. doi: 10.1128/AAC.00414-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holyoake LV, Hunt S, Sanguinetti G, Cook GM, Howard MJ, Rowe ML, Poole RK, Shepherd M. 2016. CydDC-mediated reductant export in Escherichia coli controls the transcriptional wiring of energy metabolism and combats nitrosative stress. Biochem J 473:693–701. doi: 10.1042/BJ20150536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Delaunay-Moisan A, Ponsero A, Toledano MB. 2017. Reexamining the function of glutathione in oxidative protein folding and secretion. Antioxid Redox Signal 27:1178–1199. doi: 10.1089/ars.2017.7148. [DOI] [PubMed] [Google Scholar]
- 26.Duval V, Lister IM. 2013. MarA, SoxS and Rob of Escherichia coli—global regulators of multidrug resistance, virulence and stress response. Int J Biotechnol Wellness Ind 2:101–124. doi: 10.6000/1927-3037.2013.02.03.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Merdanovic M, Clausen T, Kaiser M, Huber R, Ehrmann M. 2011. Protein quality control in the bacterial periplasm. Annu Rev Microbiol 65:149–168. doi: 10.1146/annurev-micro-090110-102925. [DOI] [PubMed] [Google Scholar]
- 28.Huang H, Sun Y, Yuan L, Pan Y, Gao Y, Ma C, Hu G. 2016. Regulation of the two-component regulator CpxR on aminoglycosides and beta-lactams resistance in Salmonella enterica serovar Typhimurium. Front Microbiol 7:604. doi: 10.3389/fmicb.2016.00604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baba T, Mori H. 2008. The construction of systematic in-frame, single-gene knockout mutant collection in Escherichia coli K-12. Methods Mol Biol 416:171–181. doi: 10.1007/978-1-59745-321-9_11. [DOI] [PubMed] [Google Scholar]
- 30.AlRabiah H, Allwood JW, Correa E, Xu Y, Goodacre R. 2018. pH plays a role in the mode of action of trimethoprim on Escherichia coli. PLoS One 13:e0200272. doi: 10.1371/journal.pone.0200272. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material. Download SPECTRUM00743-21_Supp_1_seq4.pdf, PDF file, 0.3 MB (345.9KB, pdf)
Supplemental material. Download SPECTRUM00743-21_Supp_2_seq5.xlsx, XLSX file, 0.03 MB (27.9KB, xlsx)