Abstract
Current treatment strategies for control of trauma-associated symptoms of Post Traumatic Stress Disorder (PTSD) have recently been updated by the Veterans Affairs (VA) and the Department of Defense (DoD, after over a decade of dedicated research. The most recent evidence is compelling that its use of trauma-focused therapies such as Cognitive Processing Therapy (CPT), Prolonged Exposure Therapy (PE), Eye Movement, Desensitization, and Restructuring (EMDR), and others with significant trauma focus are the current gold standard for treatment. Additional medication use may be of assistance in treatment of symptomology, with special avoidance of benzodiazepines or other sedative hypnotic medications which are causal of increased intrusive and dissociative symptoms over time.
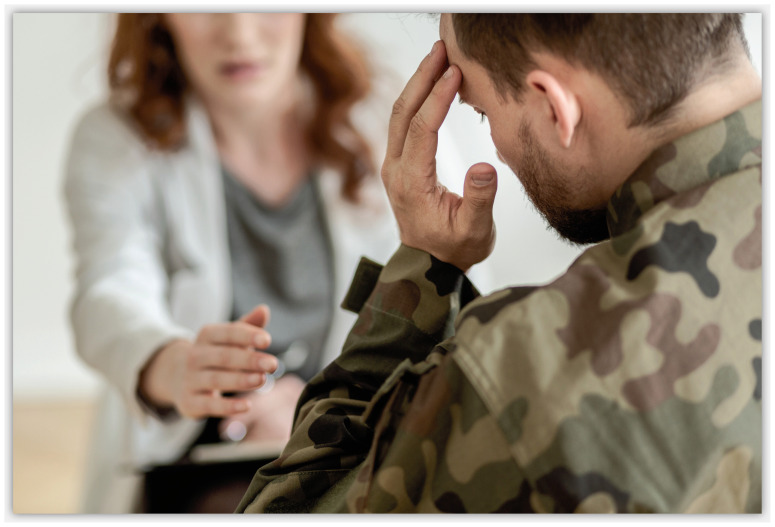
Introduction
In his early theories of the mind, Sigmund Freud hypothesized that the individual has stages of psychological development: that of forming an unconscious defense against pain and shock through the turning away from the triggers of unpleasure and finally the conscious disapproval of an impulse through use of judgement.1 Much of his early work focused on the traumatic shocks that his patients had endured through their lifetime; many of them through workplace accidents, loss of life or loved ones, involvement in war, and from sexual assault. Despite the efforts and work of many before and after him, those same traumatic experiences have historically elicited very similar reactions from those who have suffered through them and have so far, been difficult to appropriately treat. What we have known for some time is that trauma is no respecter of persons, status, or intellectual capacity, and that the after effects of trauma can significantly impair function in life.
The Modern Concept of Post-Traumatic Stress Disorder
The diagnosis of what is now accepted as Post Traumatic Stress Disorder (PTSD) has changed over the years as we have gained a better understanding of the stress response and its longer-term impact on the body and the brain. During the Seven Years War (1756–1763) a physician from Austria, one Joseph Auenbrugger, observed and documented symptoms in some troops such as excessive physical exhaustion, anger, and irritability (angst), and depressed mood. He termed the condition “nostalgia” after the soldiers being so homesick, and so far distant from that which they knew, that their personality and the core of who they were was significantly changed. In his 1761 book Inventum Novem he wrote:
“When young men who are still growing are forced to enter military service and thus lose all hope of returning safe and sound to their beloved homeland, they become sad, taciturn, listless, solitary, musing, full of sighs, and moans. Finally, these cease to pay attention and become indifferent to everything, which the maintenance of life requires of them. Neither medicaments, nor arguments, nor promises, nor threats of punishment are able to produce any improvement.” 2
The diagnosis of what is now accepted as Post Traumatic Stress Disorder (PTSD) has changed over the years as we have gained a better understanding of the stress response and its longer-term impact on the body and the brain.
Granted, the pharmacopeia of that generation was severely limited, ineffective for treatment of PTSD as it often included laudanum, strong spirits (such as rum and whiskey), and certain tinctures that were thought to improve the mood such as that of Saint Johns Wort, as well as other mild sedatives such as Chamomile and Valerian root. His observations though were valid, and matched those of the Greeks and Romans who also shared a history of documentation of similar symptoms among their returning troops.
While war and violent conflict among nations may be historically well documented as a cause of profound emotional changes, it is by sheer number alone the civilian population that will carry the numerical burden of PTSD. By far the most common causes in triggering traumatic events among the entire populace are motor vehicle collisions and assault (inclusive of sexual assault and rape). These trauma experiences are fairly common in childhood, with adolescents between the ages of 14–17 having a 28% lifetime prevalence of sexual victimization with 8% of girls in that age cohort with a history of an attempted or completed rape against them.3 Approximately 6–7% of the adult population in the United States will at some point during their lifetime, meet the criteria for a diagnosis of PTSD.4 Amongst the U.S. military veteran population the variance in studies has ranged from approximately 30% of the Vietnam era veterans to more recently 13–14% of veterans serving in the dual wars in Iraq and Afghanistan over the last 20 years.5,6
We also recognize that the self reporting of symptoms from these populations over the most recent conflicts is under represented due to fears of stigma and concerns over job loss, just as is speculated are the numbers from the general populace, who face the additional hurdle of potential lack of appropriate insurance coverage for appropriate albeit specialized treatments. Our primary care physicians are indeed ‘in the trenches’ so to speak when addressing mental health concerns of this same populace. Among the general population in 2010 approximately 20% of all primary care visits included treatment for mental health issues or diagnoses - making the primary care settings an important place to screen for and initiate mental health care.7 As all providers become more familiar with the diagnosis of PTSD and the current successful treatment options, educational barriers to initiation of care becomes less problematic – and those we serve can start care immediately while waiting on their referral to a mental health professional for continued care.
Over the last two decades a wealth of research has been conducted on PTSD, driven primarily by the rising suicide completion rates and daily impairment to military members with that diagnosis. Funded mainly by the U.S. Governmental agencies these projects over the years have added to the medical knowledge and understanding of the brain, human behavior, the effects of persistent stress on the hypothylamic-pituitaryadrenal axis system, stress change to the limbicamygdylar circuitry, as well as more effective treatment strategies. Past well thought of treatments have either passed the rigorous tests of double blind and placebo-controlled studies and continue in use, or did not – and have been discounted. The amount of research was a boon to the mental health community, who at the time of late 1990s had only 15 controlled trials on treatment for PTSD to draw from.8
The following decade brought great gains. A large meta-analysis in 2013 reviewed all available research on efficacy of treatments and interventions for PTSD, with a total of 112 non-duplicate studies included. This existing body of research was influential in the formation and updates to the VA and DoD clinical practice guidelines for assessment and treatment of PTSD in that same year.
Diagnosis
In 2013 the diagnosis itself received an update with the Diagnostic and Statistical Manual of Mental Disorders (DSM) – V and shifted from an anxiety disorder and into a new category of trauma associated disorders. This was in part done to provide an updated diagnosis representing the underlying pathology of the illness and to further differentiate it from anxiety and depressive disorders which it does share some symptomatology with. At present, to have a diagnosis of PTSD a person must have had a significant trauma exposure that has caused significant impairment to occupational and social function for greater than one month.
Symptoms must include one intrusive (recurrent, involuntary, distressing memories and/or dreams, dissociative reactions such as flashbacks, intense or prolonged psychological distress to triggers, or marked physiological reactions to triggers); one avoidance symptom (avoidance of memories, feelings, or thoughts of trauma or avoidance of external reminders of trauma); two negative alterations to cognition or mood related to the trauma (dissociate amnesia, negative beliefs of self or the world, persistent negative emotional state, anhedonia, feelings of detachment or estrangement from others, inability to experience positive emotions); two symptoms of marked alterations in arousal and reactivity (irritability or anger outbursts, reckless or self-destructive behaviors, hyper vigilance, exaggerated startle response, problems with concentration, sleep disturbance). A provider may specify if there are persistent dissociative symptoms such as depersonalization (feeling detached from oneself, as if observing from out of body) or derealization (feelings of the unreality of the environment). Because of the prevalence of childhood trauma and differences in the brain and personality development of children at that age, specific criteria for children ages 6 and younger are also detailed in the DSM-V.9
Non-Pharmacologic Treatment for PTSD
Shared Decision Making and Collaborative Care (Strong Recommendation for)
Both are important early interventions which have been shown to improve patient-centered care and treatment outcomes. Review of the relevant diagnosis along with treatment options with consistent use of decision aids with patients has been shown to improve clinical outcomes, enhance psychoeducation on the diagnosis of PTSD, and reduce ambivalence in regards to accepting the most efficacious treatment strategies.10 In particular for the collaborative care model (inclusive of telehealth modalities to improve access), a stepwise treatment approach in the primary care setting has been shown to increase patient compliance with treatment and to potentially reduce the possibility of the patient stopping medication or therapy treatment too early.11
Trauma-Focused Therapy as First Line Treatment for PTSD (Strong Recommendation for)
Prior to 2013 there was little evidence to suggest that there is a differentiation in treatment with pharmacotherapy versus psychotherapy. One of the larger changes to the updated clinical practice guidelines was to recommend therapy over medication for treatment of PTSD, to the recommendation now that manualized trauma focused therapies are the first line treatments. This change was a result of two large meta-analyses which did a head-to-head comparison between existing pharmacotherapy and manualized psychotherapy with a comparison of treatment outcomes. A manualized therapy is one in which the therapist or psychiatrist uses a guide manual to assist in care delivery, ensuring that all important trauma related topics are addressed. Use of a manual for trauma therapy is the gold standard for treatment delivery. It was noted in both that the psychotherapy alone presented a longer duration of symptom resolution with a reduction in risk of side effects from ongoing medication use amongst the studied patient populations.12
In conjunction with specific positive research supporting use of manualized, trauma-focused therapies such as PE, EMDR, and CPT have shown consistent reduction of symptoms of PTSD with completion of 12–16, 60 minute weekly sessions.13,14,15 While those three ‘main’ trauma therapies have been the foundation of trauma-focused therapy research, new subtypes of manualized focused therapy such as cognitive behavioral therapy for PTSD (CBT for PTSD), Narrative Exposure Therapy (NET) and Written Exposure have also shown evidence to support their use in treatment.16,17,18, 19 All of the therapies that have shown the greatest treatment benefit have been individual therapy, not group. Recent research also highlights that therapy through video call is as effective as in person and is a cost effective first line treatment strategy.20 Use of a manual to guide and structure therapy with a patient has been shown in the above, and many more studies to improve outcomes – both in terms of adherence to and attendance in the treatment program, and in improved symptom reduction over time as compared to therapy that does not use a manualized approach. It in no way limits the therapist or reduces their expertise—in fact it has been shown to enhance it by providing a scaffolding that addresses all core issues of trauma is a systematic way, and provides for evidence-based work for the patient in treatment outside of the treatment sessions. Of the newer researched therapies, written exposure therapy has been showing excellent benefit with good treatment retention. Especially for people whose learning style may be more tactile or experiential, it allows for the patient’s written narrative with additional cognitive therapy to be the mechanism for improvement, rather than a verbal repeated retelling as in Prolonged Exposure therapy.
The verbal with imagining retelling of the trauma experience as is performed in PE is effective, though described as difficulty at best, by the patient undergoing that type of therapy. Drop out rates from PE tend to be higher than that of other more cognitively-focused therapies such as CPT and EMDR. Written exposure therapy provides a mid point between the two with emerging data suggesting a much improved retention rate in therapy when compared to PE.
There is strong evidence for:
Individual, manualized trauma-focused psychotherapy, 12–20, 60-minute sessions weekly, as main and first line treatment for treatment of PTSD.
Cognitive Processing Therapy
Eye Movement Desensitization and Restructuring (
Written Exposure Therapy
Narrative Exposure Therapy
Prolonged Exposure
Any of the above therapies delivered through video teleconferencing (aka, virtual health)
Pharmacologic Treatment of PTSD
Pharmacotherapy as a Treatment for PTSD (Strong Recommendation for)
As based on the most relevant and recent research, the medications fluoxetine, venlafaxine, or paroxetine have shown the most benefit as monotherapy in treatment of posttraumatic stress disorder symptomology. The relative benefits of use of the selective serotonin reuptake inhibitors (SSRI) or selective norepinephrine reuptake inhibitors (SNRI) are that the side effect profiles are generally well tolerated. In clinical practice a psychiatrist will often switch to different SSRI or SNRI medications based on patient response, tolerability, or other issues of slow or rapid metabolism of those particular medications. Specifically, paroxetine is less prescribed as it tends to have greater anticholinergic side effect profiles than the other SSRIs and has an extremely short half-life often requiring twice daily dosing. Other medications such as des-venlafaxine and duloxetine are both acceptable alternatives, as is sertraline in the treatment of post traumatic stress disorder. Specifically noted Celexa and Lexapro in the research have a less significant impact on reduction of symptoms than these other medications.21
There is strong evidence for use of the following medications for treatment of PTSD:
Fluoxetine, initial dose 10–20mg daily, response range 20–80mg daily.
Paroxetine, initial dose 10–20mg daily, response range 20–50mg daily.
Sertraline, initial dose 25–50mg daily, response range 50–200mg daily.
Venlafaxine XR, initial dose 37.5mg daily, response range 75–225mg daily.
Augmentation Strategies (Weak or Insufficient Evidence for)
Augmentation strategies (Weak or Insufficient Evidence for)
Augmentation strategies for treatment resistant comorbid symptomology can be done in conjunction with a primary SSRI or SSRI. The most studied of these medications include the short half-life alpha adrenergic antagonist prazosin for the treatment of PTSD associated nightmares and hyper arousal response, though recent research concluded that there was only weak evidence for use in some studies even in this limited capacity. Typical dose ranges for prazosin range from 1–12mg usually nightly, though some individuals may respond well to a split dosing regimen with a smaller morning dose and larger even dose. Another augmentation medication with weak evidence for use is mirtazepine, dosed to target reduction of sleep latency, improvement of sleep duration, and augmentation of the primary SSRI or SNRI in anxiolytic effects. As a nightly anxiolytic this medication not only improves sleep architecture but may reduce anxiety symptoms in as early as two to three weeks which can be a remarkable benefit to those who do respond well to it—especially those not with PTSD but with Generalized Anxiety Disorder or Panic Disorder, with or without Agoraphobia. It is also important to note that all medications targeting reduction of anxiety symptoms tend to assist in reduction of the active anxiety components of PTSD rather than decreasing the avoidant and negative symptoms of post traumatic stress disorder. This again leaves therapy is the primary choice a first line treatments in that it can address all aspects of symptomology.
Weak or insufficient evidence for augmentation with:
Prazosin, for reduction of nightmares/hyper arousal symptoms
Mirtazapine, for augmentation with an SSRI or SNRI and sleep benefit for PTSD
PTSD Non-Advised Treatments
Given the amount of research conducted over the last two decades, and the interest in PTSD as a diagnosis due to the active military conflicts over that same time period, many medications have also been studied. Of particular note, benzodiazepines have been found to carry a ‘strong against’ use recommendation. In some studies that class of medications carries an ‘X’ recommendation as well due to evidence that they cause harm with long term use with a diagnosis of PTSD. This is thought to be due to the strong sedative, addictive, and dissociative properties of the benzodiazepines (sedative hypnotics) when used to attempt to treat a condition in which dissociation and hypnotic sedation fosters trauma reliving intrusive symptoms which in turn worsened avoidant symptoms of PTSD. That said, acute or emergent use of benzodiazepines for reduction of imminent risk aggression in an emergency room or inpatient setting, or to treat seizures or alcohol withdrawals is medically indicated and does not worsen outcome of PTSD symptoms. Other medications studied included all anti-convulsants, which are often used in psychiatry as mood stabilizers to treat both subtypes of bipolar disorder, and many typical and atypical antipsychotic medications which have been shown to be of benefit in treatment resistant major depressive disorders, in psychotic disorders such as schizophrenia, and also in bipolar disorders.
Additional procedures that have been effective in other areas of psychiatry were also well researched. While Electroconvulsive Therapy (ECT) and the newer repetitive transcranial magnetic stimulation (rTMS) are effective for treatment of severe major depressive disorder and bipolar disorders, there was no conclusive evidence that they effectively were able to reduce symptoms in PTSD as did on those primary mood disorders. Additional procedures showed benefit to a small subset of patients but those findings were not generalizable to a broad population base.
The following have been found to not be recommended for use in treatment of PTSD:
Risperidone, quetiapine, olanzapine, and other atypical antipsychotics
Divalproex, tiagabine, guanfacine, ketamine, hydorcortisone, D-cycloserine
Benzodiazepines (Causes harm)
Cannabis or cannabinoids
There was insufficient evidence to support use of the following procedures for treatment of PTSD:
Electroconvulsive Therapy Repetitive Transcranial Magnetic Stimulation
Hyperbaric Oxygen Therapy
Stellate Ganglion Block
Vagal Nerve Stimulation
Summary
There has been a wealth of new and updated research into PTSD and its treatment over the last 15 years. Out of the many treatments researched, the trauma-focused therapies, delivered individually, with use of a manual by the therapist showed the most benefit in treatment. While very effective the patient may be limited by access to a therapist who has been trained in trauma-focused therapy, who may not wish to use a manualized treatment approach, or by cost and/or insurance coverage. More research needs to be conducted to directly discover and address the reasons underlying the lack of broader availability of manualized trauma focused therapy by therapists. For those desiring such, or in the absence of good access to trauma focused therapy there is also strong evidence for use of SSRIs and SNRIs such as fluoxetine, paroxetine, sertraline, and venlafaxine, and at appropriate doses will assist with symptom reduction.
Footnotes
Christian Schrader, MD, is at Carl R. Darnall Army Medical Center Psychiatry Residency, Fort Hood, Texas. Abigail Ross, MS, is at the New York Institute of Technology College of Osteopathic Medicine, Old Westbury, New York.
References
- 1.Jones E. The Life and Work of Sigmund Freud. Vol. 1. New York: Basic Books; 1953. [Google Scholar]
- 2.Auenbrugger J. Inventum Novem 1761 [Google Scholar]
- 3.Finkelhor DTH. Violence, crime, and abuse exposure in a national sample of children and youth: an update. JAMA Pediatr. 2013 Jul;167(7):614–21. doi: 10.1001/jamapediatrics.2013.42. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RB. Lifetime revalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Achives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 5.Kulka RS. Trauma and the Vietnam War generation: Report of findings from the National Vietnam Veterans Readjustment Study. New York: Brunner/Mazel; 1990. [Google Scholar]
- 6.Tanielian T. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation; 2008. [Google Scholar]
- 7.CDC. National Ambulatory Medical Care Survey; 2010. [online, accessed 11/02/2021]. http://www.cdc.gov/nchs/ahcd.htm . [Google Scholar]
- 8.Van Etten ML, Taylor S. Comparative efficacy of treatment for posttraumatic stress disorder: a meta-analysis. Clin Psychol Rev. 1998;5:126–144. [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 10.Watts BV, Schnurr PP, Zayed M, Young-Xu Y, Stender P, Llewellyn-Thomas H. A randomized controlled clinical trial of a patient decision aid for posttraumatic stress disorder. Psychiatr Serv. 2015 Feb 1;66(2):149–154. doi: 10.1176/appi.ps.201400062. [DOI] [PubMed] [Google Scholar]
- 11.Engel CC, Jaycox LH, Freed MC, et al. Centrally assisted collaborative telecare for posttraumatic stress disorder and depression among military personnel attending primary care: A randomized clinical trial. JAMA internal medicine. 2016;176(7):948–956. doi: 10.1001/jamainternmed.2016.2402. [DOI] [PubMed] [Google Scholar]
- 12.Lee DJ, Schnitzlein CW, Wolf JP, Vythilingam M, Rasmusson AM, Hoge CW. Psychotherapy versus pharmacotherapy for posttraumatic stress disorder: Systemic review and meta-analyses to determine first-line treatments. Depress Anxiety. 2016 Sep;33(9):792–806. doi: 10.1002/da.22511. [DOI] [PubMed] [Google Scholar]
- 13.Foa EB, Hembree EA, Cahill SP, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. J Consult Clin Psychol. 2005 Oct;73(5):953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- 14.Rothbaum BO, Astin MC, Marsteller F. Prolonged exposure versus eye movement desensitization and reprocessing (EMDR) for PTSD rape victims. J Trauma Stress. 2005 Dec;18(6):607–616. doi: 10.1002/jts.20069. [DOI] [PubMed] [Google Scholar]
- 15.Ehlers A, Grey N, Wild J, et al. Implementation of cognitive therapy for PTSD in routine clinical care: Effectiveness and moderators of outcome in a consecutive sample. Behav Res Ther. 2013 Nov;51(11):742–752. doi: 10.1016/j.brat.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blanchard EB, Hickling EJ, Devineni T, et al. A controlled evaluation of cognitive behavioural therapy for posttraumatic stress in motor vehicle accident survivors. Behav Res Ther. 2003 Jan;41(1):79–96. doi: 10.1016/s0005-7967(01)00131-0. [DOI] [PubMed] [Google Scholar]
- 17.Sloan DM, Marx BP, Bovin MJ, Feinstein BA, Gallagher MW. Written exposure as an intervention for PTSD: A randomized clinical trial with motor vehicle accident survivors. Behav Res Ther. 2012 Oct;50(10):627–635. doi: 10.1016/j.brat.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stenmark H, Catani C, Neuner F, Elbert T, Holen A. Treating PTSD in refugees and asylum seekers within the general health care system. A randomized controlled multicenter study. Behav Res Ther. 2013 Oct;51(10):641–647. doi: 10.1016/j.brat.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 19.Sloan DM, Marx BP, Resick PA, Young-McCaughan S, Dondanville KA, Mintz J, Litz BT, Peterson AL STRONG STAR Consortium. Study design comparing written exposure therapy to cognitive processing therapy for PTSD among military service members: A noninferiority trial. Contemporary clinical trials communications. 2019;17:100507. doi: 10.1016/j.conctc.2019.100507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pande RL, Morris M, Peters A, Spettell CM, Feifer R, Gillis W. Leveraging remote behavioral health interventions to improve medical outcomes and reduce costs. Am J Manag Care. 2015;21(2):e141–151. [PubMed] [Google Scholar]
- 21.US Department of Veteran Affairs, Department of Defense. VA/DOD Clinical Practice Guideline for the Management of Posttraumatic Stress Disorder and Acute Stress Disorder. The Management of Posttraumatic Stress Disorder Work Group; 2017. pp. 1–200. [Google Scholar]