Abstract
To implement a nurse‐led protocol for the care of hypertension, 5 clinics were established in Yaounde (urban) and Bafut (rural) in Cameroon. International guidelines were adapted and 10 nurses were trained. The initial cohort of patients was referred from a field survey. The program proceeded for 26 months and 454 patients (45% urban) were registered in the clinics. Relative to urban participants, rural participants were more often women (59% vs 45%, P=.002) and less likely to have diabetes (7.2% vs 41.2%, P<.001). Between baseline and final visits, systolic and diastolic blood pressures dropped by 11.7 mm Hg (95% confidence interval, 8.9–14.4) and 7.8 (95% confidence interval, 5.9–9.6), respectively (P<.001). These changes were consistent in subgroups and after adjustment. Most dropouts occurred around the initial visit and among urban participants and nondiabetics. Nurse‐led clinics are effective for improving hypertension care in these settings and require implementation and validation through controlled trials.
Worldwide, nonoptimal blood pressure (BP) levels have been identified as a major contributor to the global burden of diseases. 1 In the year 2000, 12.8% of the total global deaths and 4.4% of the total global disability‐adjusted life‐years were attributable to systolic BP (SBP) levels >115 mm Hg. 2 The global population of individuals with hypertension was 972 millions in 2000, and is expected to increase to 60% by 2025. 3 By then, 71.2 to 76.0 million men and 75.0 to 79.1 million women with hypertension will be found in sub‐Saharan Africa (SSA). This will represent a nearly 50% increase relative to recent estimates. The prevalence of hypertension among adults in SSA varies consistently and has increased significantly over the past 2 to 3 decades. 4 Literature survey indicates that related complications and in particular stroke and heart failure are also becoming increasingly more common in this region. 5 , 6 , 7 Decades of research into prevention and control have convincingly demonstrated that sustained BP lowering significantly reduces the risk of BP‐related complications. 8 Guidelines have been developed and are regularly updated to assist the translation of the scientific evidence into actions that will ultimately reduce the burden of hypertension. The uptake of these guidelines in SSA and particularly at a primary health care level, where most patients are likely to seek care, is limited by the availability of adequate health care resources. In particular, the lack of physicians in most primary health care settings in SSA calls for new strategies to improve access to care for chronic conditions, such as hypertension, while caring for the still‐prevalent acute infectious diseases.
The overall aim of the Essential Non‐Communicable Diseases Health Intervention Project (ENHIP) was to contribute to strategies for the effective control and prevention of common noncommunicable diseases within SSA. 9 This program in Cameroon was implemented in the capital city (Yaounde) and in the rural health district of Bafut. At the same time, as part of ENHIP, nurse‐led protocol‐driven care was set up for the management of asthma, diabetes mellitus, epilepsy, and hypertension at primary health care levels. In this paper, we present the results relating to the management of hypertension within this program.
Patients and Methods
Setting, Study Design, and Participants: Baseline Information
Details on the purpose, design, and organization of the Cameroon Essential Noncommunicable Diseases Health Intervention Project (CENHIP) are available elsewhere. 9 Between November 1997 and March 1998, a baseline survey of a random sample of adults residing in the Biyem Assi (Yaounde) and Bafut health areas (Bafut) was conducted. 10 The aim of this survey was to determine the prevalence of hypertension and its related risk factors, to identify patients eligible for follow‐up in the clinics, and to sensitize populations to the growing importance of chronic diseases. Patients screened with hypertension were referred to 2 nurse‐led clinics specifically set up for this study in each setting (these patients are hereafter called survey patients). A third clinic was subsequently set up in the urban setting. Other patients were later attracted to the clinics or screened using opportunistic approaches during routine hospital activities (the patients are hereafter called new patients). Inclusion criteria were: (1) report of physician‐diagnosed hypertension in a patient currently treated or not, or (2) positive screening for hypertension (as defined below). Patients fulfilling these criteria were systematically recruited without any other selection process. Patients were included in the clinics from start (February 1998) to the end (January 2000) of the implementation process. Baseline information collected by trained nurses included sex, age, known duration of hypertension, and current medication. Ethical clearance was obtained from the national ethics committee, and the Ministry of Health of Cameroon authorized the study. Informed consent was obtained from patients before inclusion to the study. Local study site authorizations were obtained from the traditional rulers of the communities, subdivision officers, and health district medical officers. Documented informed consent and voluntary participation were obtained from the study participants.
Measurements and Definitions
BP was measured 3 times consecutively at rest using the right arm of a seated patient with a mercury sphygmomanometer. Phases 1 and 5 of Korotkoff sounds were used to indicate SBP and diastolic BP (DBP), respectively. The average of the second and third measurements were used to define hypertension as SBP ≥140 mm Hg and/or DBP ≥90 mm Hg. Weight (to the nearest kilogram) and height (to the nearest centimeter) were used to derive the body mass index (BMI) as weight/height×height in kg/m2. Fasting capillary blood glucose (FCBG) was also measured.
Clinical Algorithm
A clinical management algorithm was designed from international guidelines to assist BP evaluation and drug prescription. 11 , 12 It was also used by nurses to guide patient education. The algorithm used a stepwise approach to drug prescription and scaling (Figure 1). Medications locally available in the list of essential drugs were included in the algorithm. Treatment decisions were made on an individual basis according to the clinical circumstances of each patient. Medications were subsidized for rural participants and were extremely inexpensive in urban clinics compared with prices in conventional pharmacies. For instance 1 month’s treatment with hydrochlorothiazide cost rural patients $0.25 and urban patients $0.75. The same treatment would have usually cost about $2 in conventional pharmacies. Nurses were authorized to prescribe; however, physicians were also available to provide any needed advice. Nonpharmacologic measures targeted smoking, obesity, physical activity, alcohol consumption, and salt intake. The stepwise approach to drug treatment was implemented in 3 steps starting with thiazide diuretics unless contraindicated. This was usually hydrochlorothiazide 25 mg/d, increased to 50 mg. In the second step, a β‐blocker (usually propranolol) or a calcium channel blocker (usually nifedipine) was added to the diuretic. In the third step, methyldopa or nifedipine or propranolol (if not used in the second step) were added. Patients not controlled on a triple therapy were referred for follow‐up to a medical doctor.
Figure 1.
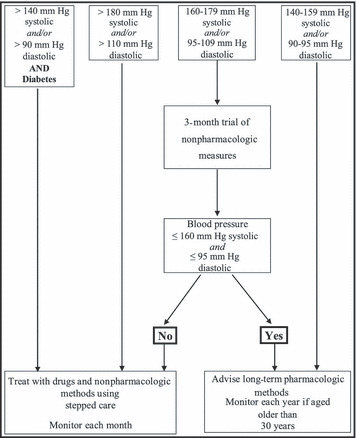
Flow chart summarizing the management of hypertension in the Essential Non‐Communicable Diseases Health Intervention Project (ENHIP) study.
Training and Retraining of Nurses
A training course was organized in each district prior to the baseline survey for risk factors and diseases. Two follow‐up sessions were thereafter organized 6 and 18 months later. This training was designed to standardize clinical practice among the nurses in charge of the clinics. Nurses had different qualifications but no previous experience in the management of chronic diseases. In addition, training was also provided to most other nurses in the health district to improve diagnosis and referral of cases to the pilot clinics and to facilitate the extension of the activities to the entire health district when the programs became effective. Initially designed using a typical medical school model, the lectures were progressively modified according to the feedback from the trainees. This feedback was obtained by 3 different methods: (1) precourse and postcourse evaluation, (2) report from trainees, and (3) rapid evaluation of the quality of care delivered in the pilot clinics by the trainees. In brief, the course aimed to achieve good training of primary health care workers for recognition of clinical presentation and risk factors of hypertension, accurate diagnosis, education of patients with hypertension, principles of management, record keeping, and referral scheme. Training methods included pre‐course assessment, formal lectures, demonstration, discussions, practical sessions, and post‐training evaluation. Practical sessions included simultaneous measurement of BP by trainees and trainers using a double‐headed stethoscope. Course facilitators were medical doctors (general practitioners and specialists) with experience in the field of chronic diseases and assisted in the follow‐up courses by the nurses in charge of the clinics. Courses were organized in one health facility of the district and each course ran for 3 consecutive days in the rural area and 6 half days in the urban area. Certificates of attendance were delivered to participants at the end of each training course.
Intervention and Follow‐Up
The first clinic visit (at least 30 minutes) offered the opportunity for baseline assessment as well as education of patients’ on risk factors. During subsequent visits, BP levels and weight were measured. Actions were taken following the treatment algorithm. Records were reviewed regularly and action undertaken to trace and track patients lost to follow‐up. Patient loss to follow‐up was defined as a failure for a patient to return to the clinic within 6 months of the last scheduled visit. The last clinic visit was used as the index for the outcome study in the clinic. The primary outcome of the study was any change in SBP and/or DBP levels between the final and baseline visit. Secondary outcomes included weight and FCBG changes and dropout rates.
Statistical Analyses
Comparison of baseline characteristics between the groups of participants was performed using Student t or chi‐square tests and equivalents as appropriate. Paired‐sample t test was used to assess the changes of continuous variables between baseline and final evaluation. General linear model (GLM) for repeated measures was used to assess the determinants of the changes in SBP and DBP during follow‐up. The models included age, sex, clinics of follow‐up, origin of patients (from the population‐based survey or attracted to the clinics), duration of follow‐up, and status of diabetes mellitus. These parameters were chosen a priori because they were believed to have potential impact in the outcomes of interest. Logistic regressions models were used to assess predictors of attrition during follow‐up. All analyses used SPSS version 14.0 (SPSS, Inc, Chicago, IL). A P value <.05 was considered significant.
Role of the Funding Source
The sponsors had no influence on design, analysis, or interpretation of results and took no part in the writing of this manuscript.
Results
Baseline Characteristics
At the end of the study, 454 patients were registered in the 5 rural and urban clinics. Of these participants, 204 (45%) were registered in the 3 urban clinics. Rural participants were more likely to be women (59.2% vs 44.6%, P<.002) and older (58.6 vs 53.8 years, P<.001), have higher mean levels of DBP (P<.026) and lower BMI (P<.001), and were less often diabetics (P<.001) compared with urban participants (Table I). More than half of participants were not from the baseline survey. New patients (as opposed to those from the survey) had lower DBP (P<.016) and higher BMI (P<.001) and were represented by more individuals with diabetes (33.5% vs 9.2%, P<.001). This was primarily due to the inclusion of patients from the third urban clinic, which was providing care mainly to people with diabetes. As expected, women displayed higher mean levels of BMI compared with men (P<.046), otherwise no significant difference was found among sex for BP and FCBG.
Table I.
Baseline Profile
| Variables | Rural (n=250) | Urban (n=204) | P Value |
|---|---|---|---|
| Clinics, No. | 2 | 3 | |
| Male sex, No. (%) | 102 (40.8) | 113 (55.4) | .002 |
| Age, y | 58.6 (11.4) | 53.8 (10.3) | <.001 |
| Origin, survey, No. (%) | 119 (47.6) | 87 (42.6) | .337 |
| Blood pressure, mm Hg | |||
| Systolic | 159.7 (24.1) | 155.9 (24.0) | .101 |
| Diastolic | 97.6 (14.2) | 94.5 (14.2) | .026 |
| Body mass index, kg/m2 | 23.9 (3.9) | 27.4 (5.7) | <.001 |
| Diabetes, No. (%) | 18 (7.2) | 84 (41.2) | <.001 |
| Fasting capillary glucose, mmol/La | 8.5 (4.8) | 10.4 (5.3) | .144 |
Values are expressed as mean (standard deviation) unless otherwise indicated. aFor participants with diabetes.
Follow‐Up
Of the participants registered at baseline, 351 (77.3%) had at least one subsequent visit. The number of patients lost to follow‐up after each clinic visit as a proportion of those who attended the relevant visit is summarized in Figure 2. The largest proportion of patients lost to follow‐up was recorded between baseline and the third clinic visit. In addition, being followed in the rural clinics, being new to the clinics, or having diabetes were associated with lower risk of loss to follow‐up (Table II). The median duration of follow‐up among those who attended at least one postbaseline visit (25th–75th percentiles) was 6 (3–9) months overall and 4 (2–8) and 8 (3–18) months in the urban and the rural setting, respectively. This duration ranged from <1 to 26 months, was longer in the rural compared with the urban setting (P<.001), was not significantly different in men and women, and was longer for participants from the survey (11 [3–21] months) compared with the new ones (4 [2–7] months) (P<.001). The number of patient‐months accumulated during follow‐up was 2844 overall and 1800 and 1044 patient‐months in rural and urban settings, respectively. The average number of nurse–patient contacts per month of follow‐up was 1.23 (standard deviation, 0.92) overall and 1.34 (1.07) in urban and 1.06 (0.71) in rural settings (P<.001).
Figure 2.
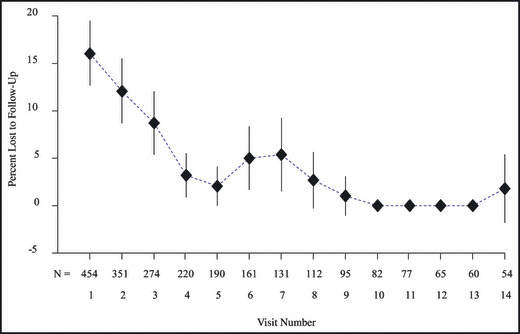
Distribution of participants lost to follow‐up by clinic visit. Diamonds represent the estimates (prevalence) and the vertical bars the 95% confidence interval. For each visit, the total number (N) of participants who attended is also shown. A linear interpolation line (broken line) has been superimposed to assist interpretation.
Table II.
Predictors of Loss to Follow‐Up
| Sex‐ and Age‐Adjusted | Multivariate (Backward Selection) | |||
|---|---|---|---|---|
| Variables | OR (95% CI) | P Value | OR (95% CI) | P Value |
| Sex (women vs men) | 0.83 (0.50–1.35) | .45 | – | – |
| Age (per year) | 0.99 (0.97–1.01) | .37 | – | – |
| Origin (new patient vs survey) | 0.16 (0.09–0.27) | <.001 | 0.018 (0.007–0.048) | <.0001 |
| Setting (rural vs urban) | 1.88 (1.1–3.23) | .02 | 0.42 (0.18–0.97) | .04 |
| Diabetes (yes vs no) | 0.35 (0.18–0.69) | .002 | 0.40 (0.14–1.14) | .08 |
| Follow‐up visits (per visit) | 0.68 (0.60–0.77) | <.0001 | 0.56 (0.48–0.67) | <.0001 |
Abbreviations: CI, confidence interval; OR, odds ratio.
Outcomes
The mean changes (95% confidence interval [CI]) in follow‐up parameters between final and baseline assessment visits were SBP −11.7 mm Hg (CI, −14.4 to −8.9 mm Hg; P<.001); DBP −7.8 mm Hg (CI, −9.7 to −5.9 mm Hg; P<.001); weight 0.4 kg (0.1–0.8 kg; P<.046); and fasting blood glucose −1.4 mmol/L (−2.6 to −0.6 mmol/L; P<.017). These changes persisted when analyses were stratified successively by study setting (Table III), sex, and origin of study participants (from the survey or new to the clinics). Although some P values did not reach the significant level, the direction of the effect never changed. The minimum SBP and DBP changes were recorded in participants with diabetes (Figure 3).
Table III.
Means Changes (95% Confidence Interval) in Variables Between Baseline and Final Visit
| Variables | Rural (n=176) | P Value | Urban (n=175) | P Value |
|---|---|---|---|---|
| Systolic blood pressure, mm Hg | 14.4 (10.5 to 18.3) | <.001 | 8.8 (4.9 to 12.7) | <.001 |
| Diastolic blood pressure, mm Hg | 12.1 (9.3 to 14.9) | <.001 | 3.2 (0.9 to 5.5) | .006 |
| Pulse rate, beats per min | −1.2 (−3.3 to 0.9) | .26 | −0.04 (−3.0 to 2.9) | .980 |
| Weight, kg | −1.0 (−1.5 to −0.4) | .001 | 0.3 (−0.1 to 0.9) | .161 |
| Fasting capillary glucose, mmol/La | 0.6 (−1.3 to 2.5) | .49 | 1.5 (0.2 to 2.8) | .02 |
aFor participants with diabetes at baseline.
Figure 3.
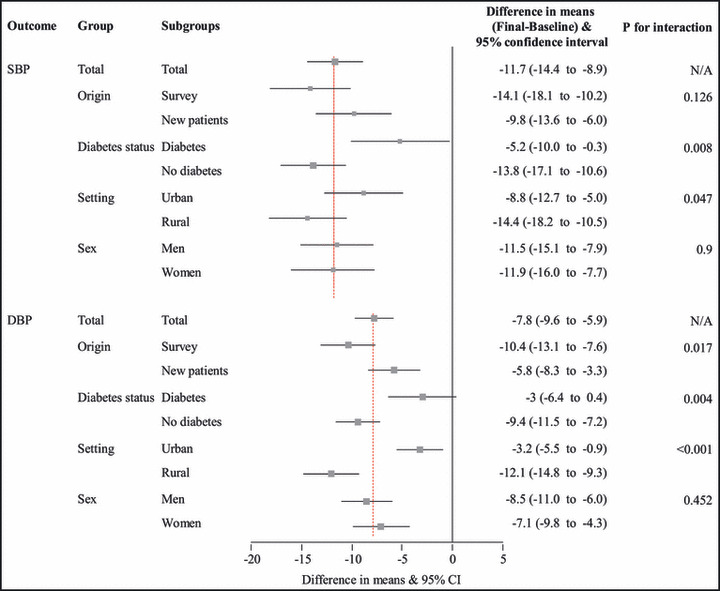
Forrest plot summarizing the mean changes in systolic blood pressure (SBP) and diastolic blood pressure (DBP) between final and baseline visits, overall and by subgroups. The squares represent the effect estimates (mean differences: final visit value – baseline visit value) and the horizontal lines the 95% confidence interval (CI) of the effect estimates. Sizes of the squares are proportional to the inverse of the variance. The broken vertical lines are for the overall estimates by blood pressure variable. N/A indicates not applicable.
The reductions in SBP and DBP were apparent from the second visit and were significantly sustained throughout follow‐up. This was observed for the overall cohort (Figure 4) and in subgroups defined by sex, setting, and the origin of the participants (all P for linear trend <.007). After adjustment for baseline age, duration of follow‐up, sex, setting of follow‐up, and origin of the patients, the mean difference in BP levels remained significant for the overall cohort: SBP (F=4.628, P<.03) and DBP (F=8.02, P<.005).
Figure 4.
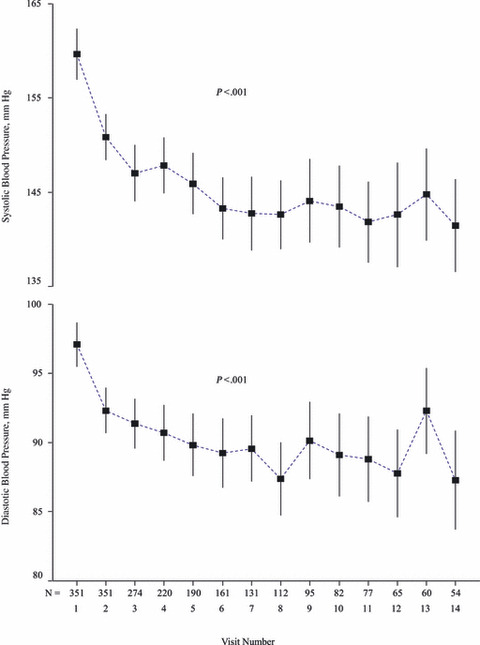
Trajectory of the average systolic (upper panel) and diastolic (lower panel) blood pressures during follow‐up for the overall cohort. Boxes represent the estimates (mean) and the vertical bars the 95% confidence interval. For each visit, the total number (N) of participants who attended is also shown. A linear interpolation line (broken line) has been superimposed to assist interpretation. The P values are for linear trend separately for systolic and diastolic blood pressure. The follow‐up was truncated at the 14th visit to account for the rapidly decreasing number of participants after this visit and the instability of the resulting estimates.
To test the robustness of our findings, additional analyses were performed including all the patients who participated in the study. Patients who attended the clinics once were given the values they had at the first visit for their second measure of SBP, DBP, weight, and FCBG. This led to some attenuation in the magnitude of parameter changes between final and baseline visit. However, changes remained significant and the directions of the effects were always similar. Average changes for the overall cohort were: SBP −9.1 mm Hg (−11.3 to −6.9 mm Hg; P<.001); DBP −6.1 mm Hg (−7.5 to −4.6 mm Hg; P<.001); weight 0.4 kg (0.1–0.7 kg; P<.018); and FCBG −1.3 mmol/L (−2.3 to −0.2 mmol/L; P<.017). Results within subgroups were also similar. After adjustment for baseline age, duration of follow‐up, sex, setting of follow‐up, and origin, the mean difference in BP levels remained: SBP (F=3.949, P<.05) and DBP (F=6.044, P<.014).
Discussion
The World Health Report 2008 advocates a shift back to primary health care so that access to care on a global scale may be improved. 13 This shift in care in developing countries of SSA must incorporate innovative strategies if access to care for chronic diseases in particular is to be scaled up. 14 This study has implemented and assessed the effectiveness of nurse‐led protocol‐driven care for hypertension at a primary health care level in rural and urban Cameroon. The program attracted many patients from the community and the intervention significantly reduced BP levels, with a mean reduction of 11.7 mm Hg for SBP and 7.8 mm Hg for DBP between baseline and final visits. The significant BP reduction was observed in all other subgroups of participants. Patients were likely to drop out of the program only in the initial period following their enrollment.
Nurse‐led care has been identified as a promising way of delivering care for hypertension, with the majority of randomized controlled trials conducted on this topic reporting an improvement in BP control. 15 In a 6‐month follow‐up randomized controlled trial in Toronto, regular care by physician was compared with worksite care by trained nurses. 16 Patients followed by nurses were more likely to be prescribed BP‐lowering treatment and to adhere to such medications, as well as reach targets for BP control. In another trial of similar duration in Mexico, 17 home‐delivered health promotion by nurses on top of usual care was associated with 3.31‐mm Hg (systolic) and 3.67‐mm Hg (diastolic) lower BP in the intervention group compared with the control group. More patients in the intervention group also achieved the predefined BP target of <160/90 mm Hg. Elsewhere, nurses and allied health personnel have also been used to assist physicians in the care of hypertension in various settings. 15 , 18 , 19 Evidence from SSA, however, remains very limited. 20
Changes in body weight were not significant in the overall population. This was primarily the result of a nonsignificant decrease among urban participants and a significant increase among the rural ones. There was no apparent explanation for this observed interaction. The less significant BP lowering achieved in participants with diabetes was likely a result of the difficult task of controlling BP in individuals with diabetes. In particular, average BP tended to be higher in such patients, many of whom would have required a combination of many BP‐lowering agents to achieve significant BP reduction. While such combinations are desirable in order to optimize BP control and increase health benefits, patients’ purchasing power was a major limitation to the intensity of the treatment in this study setting where health expenditure was funded by out‐of‐pocket money. The high proportion of individuals with diabetes among urban participants accounts at least in part for the less BP lowering achieved in the urban compared with the rural setting. In accordance with data from prospective observational studies and clinical trials, if sustained over time, the changes in BP observed in this study would translate into significant benefits in terms of reduction in the incidence of target organ damage and fatal outcomes. 8
Limitations
Limitations of this study include the large initial dropout rate, the unblinded assessment of end points, and the absence of a comparative arm. As such, to what extent some of the observed effect may be accounted for by a selective dropout of participants who were less likely to respond to the treatment, a systematic bias in BP assessment during follow‐up, and the “regression to the mean” phenomenon cannot be reliably assessed. The consistency of the findings between subgroups of participants, the varying duration between baseline and final visits between participants, and the magnitude of the observed changes in BP indicate, however, that the reductions in BP may be related to the intervention. Another limitation was our inability to assess the levels of other cardiovascular risk factors at baseline and monitor them during follow‐up, as well as assessing patients for target organ damage. Such measurement would have assisted in the choice and intensity of treatment and refined the analyses presented here but would not affect the conclusions of the study. Definition criteria for hypertension and treatment recommendations have changed since the time this study was conducted. The benefit of BP lowering is driven by the overall absolute risk of disease and the amount of BP lowering achieved, not the level of BP at which treatment is started. The conclusions of this study therefore remain valid.
Conclusions
A major advantage of this study was our ability to undertake such activity simultaneously in rural and urban areas, therefore providing evidence in support of the applicability of our approach in these settings with different characteristics and health needs. Increasing and improving access to care for hypertension is a particular concern in SSA. The present study has demonstrated that nurse‐led protocol‐driven hypertension care in rural and urban Cameroon achieved significant BP reduction in patients with known or newly diagnosed hypertension. The findings of this study have important implications for BP control policies in SSA if confirmed in other settings. We advocate validation of this approach in properly designed randomized controlled trials. Issues to be addressed by such studies could include how nurse‐delivered care for hypertension compares with that routinely provided by primary care physicians and how nurses can be efficiently used to improve the processes of care provided by primary care physicians. Long‐term follow‐up studies are also required to assess how such care affects hard clinical outcomes over time.
Acknowledgment and disclosure: We are grateful to Dr Sophia Zoungas for her comments on the final version of the manuscript. The ENHIP study was funded by the Department for International Development (DfID) of the UK Government through the University of Newcastle.
References
- 1. Ezzati M, Lopez AD, Rogers A, et al.; Comparative Risk Assessment Collaborating Group . Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–1360. [DOI] [PubMed] [Google Scholar]
- 2. Lawes CM, Vander Hoorn S, Law MR, et al. Blood pressure and the global burden of disease 2000. Part II: estimates of attributable burden. J Hypertens. 2006;24:423–430. [DOI] [PubMed] [Google Scholar]
- 3. Kearney PM, Whelton M, Reynolds K, et al. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. [DOI] [PubMed] [Google Scholar]
- 4. Addo J, Smeeth L, Leon DA. Hypertension in sub‐saharan Africa: a systematic review. Hypertension. 2007;50:1012–1018. [DOI] [PubMed] [Google Scholar]
- 5. Kengne AP, Dzudie A, Sobngwi E. Heart failure in sub‐Saharan Africa: a literature review with emphasis on individuals with diabetes. Vasc Health Risk Manag. 2008;4:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kengne AP, Anderson C. The neglected burden of stroke in sub‐Saharan Africa. Int J Stroke. 2006;1:180–190. [DOI] [PubMed] [Google Scholar]
- 7. Kengne AP, Awah PK. Classical cardiovascular risk factors and all‐cause mortality in rural Cameroon. QJM. 2009; 102:209–215. [DOI] [PubMed] [Google Scholar]
- 8. Turnbull F. Effects of different blood‐pressure‐lowering regimens on major cardiovascular events: results of prospectively‐designed overviews of randomised trials. Lancet. 2003;362:1527–1535. [DOI] [PubMed] [Google Scholar]
- 9. Unwin N, Mugusi F, Aspray T, et al. Tackling the emerging pandemic of non‐communicable diseases in sub‐Saharan Africa: the essential NCD health intervention project. Public Health. 1999;113:141–146. [PubMed] [Google Scholar]
- 10. Sobngwi E, Mbanya JC, Unwin NC, et al. Physical activity and its relationship with obesity, hypertension and diabetes in urban and rural Cameroon. Int J Obes Relat Metab Disord. 2002;26:1009–1016. [DOI] [PubMed] [Google Scholar]
- 11. O’Brien ET, Beevers DG, Marshall HS. ABC of Hypertension. 3rd ed. London, UK: BMJ Publishing Group; 1995. [Google Scholar]
- 12. Petrie J, O’Brien E, Littler W, et al. Recommendations on Blood Pressure Measurements. 2nd ed. London, UK: BMJ Publishing Group; 1990. [Google Scholar]
- 13. The World Health Organization . The World Health Report 2008: Primary Health Care Now More Than Ever. Geneva, Switzerland: WHO; 2008. [Google Scholar]
- 14. Beaglehole R, Epping‐Jordan J, Patel V, et al. Improving the prevention and management of chronic disease in low‐income and middle‐income countries: a priority for primary health care. Lancet. 2008;372:940–949. [DOI] [PubMed] [Google Scholar]
- 15. Fahey T, Schroeder K, Ebrahim S. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2006: CD005182. [DOI] [PubMed] [Google Scholar]
- 16. Logan AG, Milne BJ, Achber C, et al. Work‐site treatment of hypertension by specially trained nurses. A controlled trial. Lancet. 1979;2:1175–1178. [DOI] [PubMed] [Google Scholar]
- 17. Garcia‐Pena C, Thorogood M, Armstrong B, et al. Pragmatic randomized trial of home visits by a nurse to elderly people with hypertension in Mexico. Int J Epidemiol. 2001;30:1485–1491. [DOI] [PubMed] [Google Scholar]
- 18. McLean DL. Nurses managing high blood pressure in patients with diabetes in community pharmacies. Can J Cardiovasc Nurs. 2007;17:17–21. [PubMed] [Google Scholar]
- 19. Canzanello VJ, Jensen PL, Schwartz LL, et al. Improved blood pressure control with a physician‐nurse team and home blood pressure measurement. Mayo Clin Proc. 2005;80:31–36. [DOI] [PubMed] [Google Scholar]
- 20. Coleman R, Gill G, Wilkinson D. Noncommunicable disease management in resource‐poor settings: a primary care model from rural South Africa. Bull World Health Organ. 1998;76:633–640. [PMC free article] [PubMed] [Google Scholar]


