Abstract
The authors explored whether the waist circumference (WC) cutoffs currently proposed to define abdominal obesity (AO) are associated with diabetes and cardiovascular disease (CVD) in Latin America. Primary care physicians in 12 countries were randomly chosen to measure WC and body mass index and record the presence of diabetes and CVD in all consecutive adult patients, consulting them on 2 prespecified half‐days. Overall, 70% of 9719 men, and 76% of 18,526 women had AO. Diabetes was reported in 10% of men and 9% of women and CVD in 9% of men and 7% of women. AO was significantly related with diabetes (age‐adjusted odds ratio, 1.63 for men and 2.86 for women) and with CVD (odds ratio, 1.41 for men and 1.62 for women). Obesity was also significantly related with diabetes and CVD. Strikingly, abdominal adiposity was very frequent in women with normal body mass index, suggesting that an evidence‐based definition of abdominal adiposity in Latin America is needed.
Obesity is becoming a serious health problem around the world, and its prevalence is increasing not only in the industrialized countries but also in developing countries where the rate of urbanization is high and lifestyle is changing toward greater caloric intake and lower physical activity. 1 Both obesity and overweight are associated with increased risk of diabetes, cardiovascular disease (CVD) and death. 1 , 2 , 3 , 4 Abdominal obesity (AO) is a strong risk factor for diabetes. 5 , 6 , 7 It is also an independent risk factor for acute coronary events, 8 and waist circumference (WC)—a surrogate measure of AO—has been found to be a strong predictor of mortality. 9 , 10 The multinational INTERHEART case‐control study confirmed the importance of AO as a potent risk factor for myocardial infarction in Latin America. 11
The International Diabetes Federation (IDF) published a worldwide definition of the metabolic syndrome in which AO became the main and obligatory component; they proposed ethnicity‐specific WC cutoffs. 12 For South and Central Americans, the recommendation was to use the South Asian values until more specific data were available, but it is not known whether these cutoffs for AO are associated with diabetes and CVD and appropriate to be used in addition to or replacement of body mass index (BMI) in primary care practice.
The International Day for Evaluation of Abdominal Adiposity (IDEA) 13 was a large international noninterventional cross‐sectional study evaluating WC measured by a standardized protocol in 168,000 primary care patients on 2 prespecified half‐days in 63 countries. This report describes the distribution of WC, overweight, and obesity in Latin America and Caribbean countries and evaluates whether WC, in addition to BMI, is a useful clinical marker.
Research Design and Methods
Twelve countries from Latin America and the Caribbean participated in the study: Argentina, Brazil, Chile, Colombia, Dominican Republic, Ecuador, Guatemala, Jamaica, Mexico, Peru, Trinidad and Tobago, and Venezuela. Primary care physicians (PCPs) were randomly selected in each country by geographic and administrative strata from an exhaustive list of active physicians, as reported previously. 13 Between May 9 and July 6, 2005, all consecutive patients aged 18 to 80 years who consulted these PCPs for any reason on 2 prespecified half‐days were invited to participate in the study. Women who were known to be pregnant were excluded. Ethics committee approval was obtained for each participating site, and each patient provided written informed consent.
Physicians recorded each patient’s age, sex, presence of known diabetes (type 1 or type 2), and known CVD (defined on the form as coronary heart disease, stroke, or revascularization). Disease status used a combination of the physician’s knowledge of the patient’s history, medical notes, and patient recall. The physicians were trained to measure WC in the standing position, midway between the lowest rib and the iliac crest. 14 Weight and height were measured and BMI calculated.
Statistical Analysis
Patient characteristics are described by means and SDs and by percentages and 95% confidence intervals (CIs). Age‐adjusted frequencies of obesity (BMI ≥30 kg/m2), of overweight (BMI, 25–30 kg/m2), of AO according to the IDF criteria (WC ≥90 cm for men and ≥80 cm for women) 12 and National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) criteria (>102/88 cm for men/women), 15 and of diabetes and CVD were calculated by country and by sex. Age‐adjusted odds ratios (ORs) for diabetes and CVD were calculated according to the BMI categories obesity and overweight and according to the NCEP ATP III– and IDF‐defined thresholds for WC. Further, age‐adjusted frequencies of diabetes and CVD were calculated according to sex‐specific WC and BMI categories using logistic regression in SAS PROC GENMOD (SAS Institute Inc., Cary, NC) with age as a continuous variable; trend tests were used to compare frequencies of diabetes and CVD across WC categories (<90, 90–102, and >102 cm for men and <80, 80–88, and >88 cm for women), within each BMI category (<25, 25–29.9, and ≥30 kg/m2), and similarly with BMI categories within each WC category. All statistical analyses used SAS statistical software (version 8.2; SAS Institute Inc., Cary, NC).
Results
Ninety‐nine percent of the patients agreed to participate, and 28,245 patients (9719 men and 18,526 women) had data available for age, anthropometric parameters, diabetes, and CVD. The mean (SD) age was 44.3 (15.4) and 44.0 (15.5) years for men and women, respectively, but varied among countries from 40.8 (13.9) and 40.3 (13.9) years in Mexico to 53.3 (16.6) and 54.0 (16.2) years in Argentina for men and women, respectively. The mean (SD) BMI varied from 26.4 (4.4) kg/m2 in Colombia to 28.6 (5.0) kg/m2 in Mexico for men and from 26.0 (5.0) kg/m2 in Peru to 28.7 (5.5) kg/m2 in Chile for women. The mean (SD) WC also varied widely from 93.4 (12.4) cm in Peru to 99.4 (13.5) cm in Argentina for men and from 86.2 (13.1) cm in Colombia to 91.6 (14.1) cm in Guatemala for women (Table I).
Table I.
Mean (SD) Age, BMI, and WC of Primary Care Patients in Latin America and the Caribbean by Sex and Country in the International Day for Evaluation of Abdominal Adiposity (IDEA) Study
| Country | No. | Age (Years) | BMI (kg/m2) | WC (cm) | ||||
|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | Men | Women | |
| Overall | 9719 | 18,526 | 44.3 (15.4) | 44.0 (15.5) | 27.8 (4.9) | 27.6 (5.7) | 96.4 (13.4) | 89.7 (13.8) |
| Argentina | 1098 | 1867 | 53.3 (16.6) | 54.0 (16.2) | 28.5 (4.8) | 27.4 (5.8) | 99.4 (13.5) | 90.5 (14.7) |
| Brazil | 1135 | 2140 | 45.3 (14.7) | 45.6 (15.3) | 27.4 (4.7) | 27.2 (5.7) | 96.5 (13.8) | 89.0 (13.6) |
| Chile | 449 | 935 | 45.0 (14.9) | 45.8 (14.8) | 28.1 (4.3) | 28.7 (5.5) | 95.8 (12.4) | 91.2 (14.1) |
| Colombia | 1169 | 2626 | 46.1 (16.0) | 45.0 (15.7) | 26.4 (4.4) | 26.2 (5.0) | 93.6 (12.8) | 86.2 (13.1) |
| Dominican Republic | 185 | 436 | 41.2 (13.8) | 41.0 (14.1) | 27.6 (5.9) | 27.3 (5.9) | 98.5 (18.4) | 90.5 (16.2) |
| Ecuador | 450 | 765 | 42.4 (14.7) | 42.8 (14.5) | 27.0 (4.4) | 27.4 (5.2) | 94.2 (11.5) | 88.0 (12.4) |
| Guatemala | 740 | 1447 | 42.5 (15.2) | 41.0 (15.3) | 27.5 (5.1) | 27.6 (5.4) | 97.1 (14.0) | 91.6 (14.1) |
| Jamaica | 182 | 385 | 48.4 (16.3) | 45.9 (17.2) | 27.1 (5.5) | 28.6 (5.8) | 92.1 (14.4) | 91.2 (13.7) |
| Mexico | 2900 | 4847 | 40.8 (13.9) | 40.3 (13.9) | 28.6 (5.0) | 28.7 (5.8) | 97.1 (13.4) | 90.7 (14.2) |
| Peru | 462 | 813 | 42.9 (14.8) | 41.5 (15.1) | 26.6 (4.5) | 26.0 (5.0) | 93.4 (12.4) | 86.7 (11.7) |
| Trinidad and Tobago | 198 | 396 | 45.2 (15.1) | 44.6 (16.7) | 27.5 (6.1) | 27.4 (6.0) | 95.5 (13.7) | 90.2 (13.4) |
| Venezuela | 751 | 1869 | 43.2 (14.5) | 43.5 (14.4) | 28.0 (4.7) | 28.0 (5.7) | 96.9 (12.2) | 90.9 (12.9) |
Abbreviations: BMI, body mass index; WC, waist circumference.
More than 60% of men and women were either overweight or obese (BMI ≥25 kg/m2). The frequency of overweight (BMI, 25–29.9 kg/m2) was strikingly higher in men (42.3%; 95% CI, 41.3–43.3%) than in women (35.0%; 95% CI, 34.3–35.7). In contrast, the frequency of obesity (BMI ≥30 kg/m2) was similar in both sexes (28.4% in men and 29.4% in women). There was a marked variation in the age‐adjusted frequency of obesity among countries, from <20% in Colombia and Peru for both men and women and in Ecuador for men to >30% in Mexico for men and women and in Chile, Dominican Republic, Jamaica, Trinidad and Tobago, and Venezuela for women. There was also some variation in the age‐adjusted frequency of overweight, from 31.1% in Trinidad and Tobago to 49.1% in Ecuador for men and from 37.9% in Ecuador to 38.0% in Guatemala for women.
The median and mean WC were almost identical for men (96.0 and 96.4 cm, respectively) and for women (89.0 and 89.7 cm, respectively) indicating a symmetric distribution. There was overall a 7‐cm difference between sexes, and this was consistent across countries (Table I; range, 4.6–8.0 cm), except in Jamaica where the WC was low in men and almost equal to women (<1‐cm difference). The WC tertiles for men (90 and 101 cm) were close to the cutoffs proposed by the IDF (≥90 cm) and the NCEP ATP III (>102 cm), respectively. In contrast, the tertiles for women (83 and 94 cm) were higher than the cutoffs proposed by the IDF (≥80 cm) and the NCEP ATP III (>88 cm), respectively.
According to the NCEP ATP III criteria (WC >102 cm for men and >88 cm for women), 29.3% (95% CI, 28.4–30.2) of men and 50.7% (95% CI, 49.9–51.4) of women had AO. With the IDF criteria proposed for Latin America (WC ≥90 for men and ≥80 cm for women), the frequency more than doubled in men (69.9%; 95 % CI, 69.0–70.9) and also increased in women (76.1%; 95% CI, 75.5–78.8) (1, 2). By the NCEP ATP III definition, the lowest age‐adjusted frequency of AO in men was seen in Jamaica (17.8%) and the highest in the Dominican Republic (35.8%); in women, the lowest was seen in Colombia (38.9%) and the highest in Guatemala (61.3%). A similar distribution among countries was seen using the IDF definition.
Figure 1.
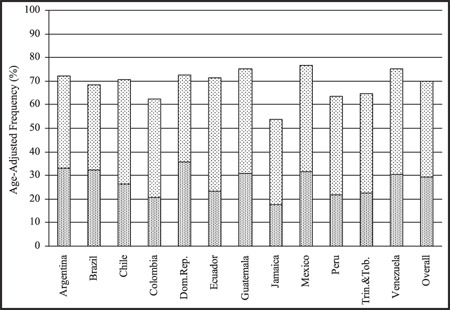
Age‐adjusted frequencies (%) of abdominal obesity in men using the International Diabetes Federation criteria (waist circumference ≥90 cm) and the National Cholesterol Education Program Adult Treatment Panel III criteria (waist circumference >102 cm) in the International Day for Evaluation of Abdominal Adiposity (IDEA) study.
Figure 2.
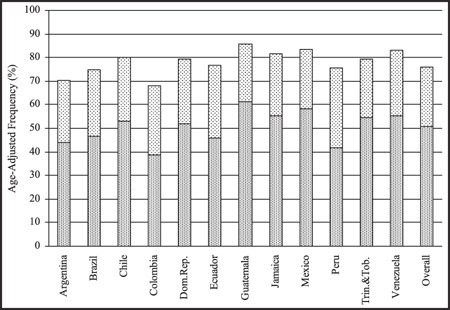
Age‐adjusted frequencies (%) of abdominal obesity in women using the International Diabetes Federation criteria (waist circumference ≥80 cm) and the National Cholesterol Education Program Adult Treatment Panel III criteria (waist circumference >88 cm) in the International Day for Evaluation of Abdominal Adiposity (IDEA) study.
In total, 25.4% (95% CI, 22.2–28.6) of men and 42.1% (95% CI, 40.3–43.9) of women with a normal BMI (<25 kg/m2) had AO by the IDF criteria, but the frequency varied across countries, in men from <20% in Chile, Colombia, and Jamaica to >35% in Guatemala and in women from <40% in Argentina, Chile, Colombia, Ecuador, and Jamaica to >50% in Guatemala. By the NCEP ATP III criteria, the frequency of AO was 1.5% in men and 10.7% in women with a normal BMI.
The age‐adjusted frequency of diabetes was significantly higher in men (9.5%; 95% CI, 8.9–10.1) than in women (8.5%; 95% CI, 8.1–8.9), but it varied across countries from <5% in Ecuador and Peru for men and women and in Argentina and Colombia for women to >10% in Jamaica for men and women and in Trinidad and Tobago for men. CVD rates were also significantly higher in men (8.6%; 95% CI, 8.0–9.2) than in women (7.2%; 95% CI, 6.9–7.6), and this frequency varied across countries from <4% in Peru and Colombia for men and women and in Trinidad and Tobago for women to >8% in Venezuela for men and women and in Brazil for men.
AO as well as obesity and overweight were significantly associated with the presence of diabetes in men and women (Table II). The frequency of diabetes increased across WC groups in each of the BMI classes for both men and women (at least P<.02 for trend) with one exception: men with a BMI <25 kg/m2 (P=.052). The inverse was not the case: for men, diabetes frequency increased with BMI only in those with WCs between 90 and 102 (P=.04); for the women, this was the case for the thinnest (WC <80 cm) and the largest (WC >88 cm) (P<.003 and P<.001). WC has a stronger role than BMI in diabetes, although in women in particular BMI provided useful predictive information as well.
Table II.
Age‐Adjusted ORs (95% Confidence Intervals) for CVD and Diabetes by BMI and WC Categories by Sex in the International Day for Evaluation of Abdominal Adiposity (IDEA) Study
| Age‐Adjusted ORs for CVD | Age‐Adjusted ORs for Diabetes | |||
|---|---|---|---|---|
| Men | Women | Men | Women | |
| BMI categories | ||||
| BMI <25 kg/m2 | 1 | 1 | 1 | 1 |
| BMI 25–29.9 kg/m2 | 1.04 (0.86–1.27) | 1.30 (1.11–1.53) | 1.20 (0.99–1.44) | 1.61 (1.39–1.88) |
| BMI ≥30 kg/m2 | 1.62 (1.35–1.96) | 2.06 (1.77–2.40) | 1.90 (1.57–2.29) | 2.77 (2.39–3.20) |
| WC categories, men/women | ||||
| WC ≥90/80 vs <90/80 cm | 1.41 (1.17–1.71) | 1.62 (1.36–1.93) | 1.63 (1.36–1.96) | 2.86 (2.35–3.49) |
| WC >102/88 vs ≤102/88 cm | 1.79 (1.54–2.08) | 1.55 (1.37–1.75) | 1.68 (1.46–1.94) | 2.53 (2.23–2.86) |
Abbreviations: BMI, body mass index; CVD, cardiovascular disease; OR, odds ratio; WC, waist circumference.
AO, by either definition, was also significantly associated with CVD in men and women (Table II). In women, the ORs were similar when either the NCEP ATP III or the IDF criteria were used to define AO: 1.55 (95% CI, 1.37–1.75) and 1.62 (95% CI, 1.36–1.93), respectively. In men, however, the NCEP ATP III criteria had a higher OR than the IDF criterea: 1.79 (95% CI, 1.54–2.08) and 1.41 (95% CI, 1.17–1.71) respectively. Obesity and overweight in comparison to normal weight (BMI <25 kg/m2) were significantly associated with CVD in women, but only obesity showed a significant association in men.
For men, trend tests showed that BMI class was not related to CVD in any of the 3 WC categories (<90, 90–102, >102 cm). In contrast, there was a significant trend for WC category within the overweight and obese (P<.0001 and P<.007, respectively). For women with a WC <80 cm and >88 cm, CVD increased over the 3 BMI classes (P<.01 and P<.0001, respectively); within BMI classes, WC groups were not significantly related to CVD. Thus, for CVD, WC appears more important than BMI for men, and the inverse appears true for women.
Conclusions
IDEA is the largest study to assess the frequency of adiposity in primary care patients worldwide. 16 The results from Latin America and the Caribbean region show that excess body weight is very frequent, since almost 70% of the primary care patients were overweight or obese. Abdominal adiposity, as measured by WC using the thresholds proposed by the IDF for our region (≥90/80 cm in men/women), was present in 70% of men and 76% of women.
The definition of AO proposed by the IDF for our region was based on preliminary observations that suggested that they were similar to those proposed by Asian studies. 17 , 18 However, the IDEA study has shown that the mean WC in the Latin American primary care population, 96.4 and 89.7 cm for men and women, respectively, is much larger than that in South and East Asia (86.4 and 89.3 cm, respectively, for men and 80.2 and 84.1 cm, respectively, for women). 16 There have been some attempts to establish the WC cutoff for the diagnosis of AO in Latin America by correlating WC with cardiovascular risk factors. 19 , 20 , 21 , 22 All studies found WC values between 83 and 91 cm for men and women. Although our study was not intended to clarify this issue, it is interesting to note that the overall frequency of AO by NCEP ATP III criteria in men was 29%, considerably lower than that by IDF criteria (70%), suggesting that the 102‐cm cutoff may underestimate the visceral adiposity found in Latin American and Caribbean men and that the IDF 90‐cm cutoff may be more appropriate. AO was significantly associated with the presence of diabetes and CVD in men. In contrast, in women the frequency of AO as defined by IDF criteria was very high (76%), and even in those with a normal BMI it was 42%, suggesting that the WC cutoff (80 cm) may be too low and overestimate the visceral adiposity found in Latin American and Caribbean women. AO was significantly associated in women with the presence of diabetes but not with CVD. Our findings support the need for a better definition of AO, particularly in women. Strategies need to be put in place to identify and treat obesity at the primary care level, where it is very frequent.
In this study, the frequency of known diabetes was high in comparison with data for the region, where the prevalence of diabetes for persons in the 20‐ to 79‐year age group is between 4.3% and 10.0% (mean, 6.1%); these frequencies included 30% to 50% of cases of diabetes that were not known. 23 Our observations may reflect the fact that diabetes is a frequent reason for attending primary care and emphasizes the need to identify AO in these patients as a main target for treatment, as well as being a means for identifying patients who should be screened for diabetes.
The ranking of frequencies of CVD in primary care are consistent with the few published data in the region. 24 The findings of IDEA, associating WC with any stage of diagnosed CVD, extend the findings from the INTERHEART case‐control study, which involved only myocardial infarction. 11 The mechanisms by which AO may lead to clinical disease are not clarified by the findings of the IDEA study. Two new large‐scale multinational studies have been initiated (INSPIRE ME and INSPIRE ME IAA) that will involve detailed profiling of risk factors and inflammatory biomarkers as well as computed tomography to quantify visceral fat. These studies will enable sex‐, region‐, and ethnicity‐specific definitions of WC thresholds to be established according to the visceral fat volume.
While the IDEA study was very large, care was taken by randomly selecting PCPs to ensure that primary care patients were representative within each geographic area of each country, with only 2 exclusion criteria: age younger than 18 or older than 80 years and pregnancy. The response rate was 99%, even though patients were not paid for participating. Our results cannot be extrapolated to the general population, only to the population consulting in primary care, and the differences between men and women and across countries may reflect different patterns of consultation and care provided at the primary level.
An important strength of the IDEA study was the uniform documentation and physician training to measure WC using a standardized approach. 13 In this study, we chose to use WC as a measure of AO because of the close correlation between WC and intra‐abdominal fat measured by computed tomography. 9 We chose not to measure the hip circumference and use the waist to hip ratio, as this would have required an additional measurement, taken more time, and been subject to more error. Our physician‐reported diagnosis is probably more reliable than patient‐reported diagnosis, which is used in many reports. 25 In our study, no diagnostic procedure was carried out for diabetes, and the IDEA questionnaire did not distinguish between type 1 and type 2 diabetes. As the majority of patients with diabetes (85%–95%) have type 2 diabetes, the observed relationships between diabetes and adiposity would be driven by type 2 diabetes.
The IDEA study has shown that the frequencies of adiposity are high in Latin America and the Caribbean and are associated with CVD and more closely with diabetes. Both BMI and WC should be routinely measured in primary care practice, particularly since the WC identified a high proportion of women with AO who had apparently “normal” weight. However, the thresholds for the definition of AO remain to be better determined in all populations and, in particular, in women from Latin America and the Caribbean region.
Acknowledgments
Acknowledgments and disclosures: The International Day for Evaluation of Abdominal Adiposity (IDEA) Steering Committee supervised the study conduct and design and the analysis and interpretation of data. PA and AR had primary responsibility for writing the paper, and all other authors critically reviewed the manuscript for important intellectual content. BB also validated the statistical analysis. Members of the IDEA Steering Committee were Beverley Balkau (France), Jean‐Pierre Després (Canada), Steven Haffner (Unites States), Phil Barter (Australia), Jean‐Pierre Bassand (France), John E. Deanfield (United Kingdom), Keith A. A. Fox (United Kingdom), Christine Massien (France), Alain‐Jean Richard (France), Sidney Smith (United States), Chee‐Eng Tan (Singapore), Luc Van Gaal (Belgium), and Hans‐Ulrich Wittchen (Germany). IDEA national coordinators and investigators were as follows: Argentina: J. Krauss; Brazil: A. Avezum; Chile: S. Kunstmann; Colombia: A. Ruiz; Dominican Republic, Jamaica, and Trinidad and Tobago: A. Gonzalez Medina; Ecuador: M. Pasquel; Guatemala: M. A. Rodas; Mexico: A. L. Esqueda; Peru: R. Gamboa; Venezuela: A. Perez Monteverde. The IDEA Steering Committee wishes to express their gratitude to the physicians who participated in the study, to Nadia Rolland, who managed the study; to Alain‐Jean Richard, who supervised the data analysis; and to Sandrine Brette, who provided statistical support. PA and AR are consultants to Sanofi Aventis. BB and SMH are consultants to Sanofi Aventis and have received honoraria for acting on the IDEA Steering Committee. CM is an employee of Sanofi Aventis. IDEA was funded by a grant from Sanofi Aventis.
References
- 1. Hossain P, Kawar B, El Nahas M. Obesity and diabetes in the developing world–a growing challenge. N Engl J Med. 2007;356:213–215. [DOI] [PubMed] [Google Scholar]
- 2. Haslam DW, James WPT. Obesity. Lancet. 2005;366:1197–1209. [DOI] [PubMed] [Google Scholar]
- 3. Caterson ID, Hubbard V, Bray GA, et al. American Heart Association: Prevention Conference VII: obesity, a worldwide epidemic related to heart disease and stroke: Group III: worldwide comorbidities of obesity. Circulation. 2004;110:e476–e483. [DOI] [PubMed] [Google Scholar]
- 4. Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. New Engl J Med. 2006;355:763–778. [DOI] [PubMed] [Google Scholar]
- 5. Wei M, Gaskill SP, Haffner SM, et al. Waist circumference as the best predictor of noninsulin dependent diabetes mellitus (NIDDM) compared to body mass index, waist/hip ratio and other anthropometric measurements in Mexican Americans: a 7‐year prospective study. Obes Res. 1997;5:16–23. [DOI] [PubMed] [Google Scholar]
- 6. Boyko EJ, Fujimoto WY, Leonetti DL, et al. Visceral adiposity and risk of type 2 diabetes: a prospective study among Japanese Americans. Diabetes Care. 2000;23:465–471. [DOI] [PubMed] [Google Scholar]
- 7. Wang Y, Rimm EB, Stampfer MJ, et al. Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am J Clin Nutr. 2005;81:555–563. [DOI] [PubMed] [Google Scholar]
- 8. Lakka HM, Lakka TA, Tuomilehto J, et al. Abdominal obesity is associated with increased risk of acute coronary events in men. Eur Heart J. 2002;23:706–713. [DOI] [PubMed] [Google Scholar]
- 9. Pouliot MC, Després JP, Lemieux S, et al. Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am J Cardiol. 1994;73:460–468. [DOI] [PubMed] [Google Scholar]
- 10. Bigaard J, Tjønneland A, Thomsen BL, et al. Waist circumference, BMI, smoking and mortality in middle‐aged men and women. Obes Res. 2003;11:895–903. [DOI] [PubMed] [Google Scholar]
- 11. Lanas F, Avezum A, Bautista LE, et al. Risk factors for acute myocardial infarction in Latin America: the INTERHEART Latin American study. Circulation. 2007;115: 1067–1074. [DOI] [PubMed] [Google Scholar]
- 12. Alberti KG, Zimmet P, Shaw J, et al. The metabolic syndrome–a new worldwide definition. Lancet. 2005;366: 1059–1062. [DOI] [PubMed] [Google Scholar]
- 13. Wittchen H‐U, Balkau B, Massien C, et al. International Day for the Evaluation of Abdominal Obesity (IDEA): rationale and design of a primary care study on the prevalence of abdominal obesity and associated factors in 63 countries. Eur Heart J Suppl. 2006;8(suppl B):B26–B33. [Google Scholar]
- 14. Seidell JC, Kahn HS, Williamson DF, et al. Report from a Centers for Disease Control and Prevention Workshop on use of adult anthropometry for public health and primary health care. Am J Clin Nutr. 2001;73:123–126. [DOI] [PubMed] [Google Scholar]
- 15. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults . Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285: 2486–2497. [DOI] [PubMed] [Google Scholar]
- 16. Balkau B, Deanfield JE, Despres JP, et al. International Day for the Evaluation of abdominal Obesity (IDEA): a study of waist circumference, cardiovascular disease and diabetes in 168 000 primary care patients in 63 countries. Circulation. 2007;116:1942–1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. WHO Western Pacific Region, IASO and IOFT . The Asia‐Pacific Perspective: redefining obesity and its treatment. Sydney, Australia: Health Communications Australia Pty Ltd, 2000. [Google Scholar]
- 18. Tan CE, Ma S, Wai D, et al. Can we apply the National Cholesterol Education Program Adult Treatment Panel definition of the metabolic syndrome to Asians? Diabetes Care. 2004;27:1182–1186. [DOI] [PubMed] [Google Scholar]
- 19. Berdasco A, Romero del Sol JM, Jimenez JM. Circunferencia de la cintura en adultos de Ciudad de la Habana como indicador de riesgo de morbilidad. Rev Cubana Aliment Nutr. 2002;16:48–53. [Google Scholar]
- 20. Sanchez‐Castillo CP, Velazquez‐Monroy O, Berber A, et al. Anthropometric cutoff points for predicting chronic diseases in the Mexican National Health Survey 2000. Obesity Res. 2003;11:442–451. [DOI] [PubMed] [Google Scholar]
- 21. Leite CC, Wajchenberg BL, Radominski R, et al. Intra‐abdominal thickness by ultrasonography to predict risk factors for cardiovascular disease and its correlation with anthropometric measurements. Metabolism. 2002;8:1034–1040. [DOI] [PubMed] [Google Scholar]
- 22. Perez M, Casas JP, Cubillos‐Garzon LA, et al. Using waist circumference as a screening tool to identify Colombian subjects at cardiovascular risk. Eur J Cardiovasc Prev Rehabil. 2003;10:328–335. [DOI] [PubMed] [Google Scholar]
- 23. Diabetes Atlas. Third edition. http://www.eatlas.idf.org. Accessed February 13, 2008. [Google Scholar]
- 24. Health Statistics from the Americas. 2007 edition. http://www.paho.org. Accessed February 13, 2008. [Google Scholar]
- 25. Carey VJ, Walters EE, Colditz GA, et al. Body fat distribution and risk of non‐insulin‐dependent diabetes mellitus in women. The Nurses’ Health Study. Am J Epidemiol. 1997;145:614–619. [DOI] [PubMed] [Google Scholar]


