Abstract
The authors assessed whether patient empowerment in the management of hypertension improved more with the practice of shared decision making (SDM) than by education programs. In a prospective controlled clinical study, 15 general practitioners in Nuremberg, Germany who were specially trained to conduct SDM consultations participated in a 12‐month study. Hypertensive patients (N=86) were included; N=40 were in the SDM group and N=46 were in the control group, if blood pressures were ≥135/85 mm Hg (self measurement) and patients had no signs of cardiovascular complications or severe hypertension. All participants in the SDM group and the control group were enrolled in an education program on hypertension in small groups. The SDM group participants also had 4 special consultations to share medical decisions. The main outcome measures were the effect of SDM on blood pressure control. After 1 year blood pressure had decreased in all participants: Δ−9.26±10.2 mm Hg/Δ−5.33±9.5 mm Hg in the SDM group (P<0.001) compared to Δ−6.0±11.8 mm Hg/Δ−3.0±8.3 mm Hg in the control group. There was no significant difference between the 2 groups. The study group practiced more SDM than controls, but blood pressure control was not significantly better. Patient empowerment by means of an education program in small groups and creating awareness of hypertensive disease helps to improve the outcome of hypertension treatment. SDM, however, did not improve management when compared to an education program, which is much easier to implement in general practice.
A growing number of randomized controlled studies suggest the efficacy of multidrug therapy in lowering blood pressure (BP) in hypertension 1 and in the prevention of related target organ damage, but this type of therapy is not pursued as aggressively as it should be. The percentage of hypertensive patients in developed countries whose BP is lowered to the extent suggested by various national and international guidelines 2 is still unsatisfactory. 3 Available antihypertensive drugs are likely effective; likely reasons for this lack of satisfactory results, therefore, may be secondary to the relative lack of symptoms in hypertension, the actual or feared side effects of the drugs, and the need for lifelong treatment of the disease. Patient expectations still often include the perception that taking a drug for a limited amount of time will cure a disease. 4 , 5 , 6 In this situation it seems reasonable—aside from the ethical demand—to let patients participate more than traditionally in the decisions made to treat their chronic illness. 7 , 8 A formal concept helping to achieve this goal is provided in the literature on shared decision making (SDM). 9 SDM in contrast to the paternalistic approach of physicians towards patients is said to involve patients in medical decisions and thus strengthen the autonomy of the patient. Operationalized criteria for physicians on how to share the process of medical decisions were established by Elwyn et al 10 , 11 (Table I).
Table I.
Stages and Competencies of Involving Patients in Health Care Decisions 11
| 1 | Implicit or explicit involvement of patients in decision‐making process |
| 2 | Explore ideas, fears, and expectations regarding possible treatments |
| 3 | Portrayal of equipoise and options |
| 4 | Identify preferred format and provide tailor‐made information |
| 5 | Checking process: understanding of information and reactions |
| 6 | Acceptance of process and decision‐making role preference |
| 7 | Make, discuss, or defer decision |
| 8 | Arrange follow‐up |
Such an approach has rarely been investigated with respect to its effects on biomedical outcome parameters like BP in hypertension where a lifelong involvement in the disease management is necessary. 12
Hence, we tested the hypothesis that arterial hypertension is more effectively lowered with the practice of SDM than by the mere implementation of education programs. Two groups participated in this study: one was to meet physicians who had undergone a special training program to develop communication skills necessary to practice SDM. In addition, they were enrolled in an education program for hypertensive patients since participation in the therapeutic process requires a certain standard of knowledge. A control group participated only in the education program to separate the effects of this program from the influence of the SDM consultations. The efficacy of this education program and its effects on BP lowering have been evaluated previously by our group. 13
Design and Methods
Eighty‐six hypertensive patients were enrolled in the study (Table II). Forty patients were recruited by the 15 study physicians who were trained in special communication skills for SDM. Forty‐six patients were recruited and allocated to the hypertension education program. Physicians of control patients were just informed about this patient empowerment.
Table II.
Characteristics of the Cohorts Studied
| Study Group | Control Group | |
|---|---|---|
| Number | 40 | 46 |
| Age (years) | 60.9±10.1 | 61.1±9.3 |
| Female/male | 67.5%/32.5% | 65%/35% |
| Blood pressure (mm Hg) | 145.4±11.7/86.6±8.2 | 144.9±11.1/86.1±9.8 |
| Known duration of hypertension (years) | 5.9±6.2 | 10.3±10.1 |
| Body mass index kg/m2 | 27.3±4.5 | 26.8±3.9 |
| Target organ damage | 26.0% | 23.9% |
| Cigarette smoking | 5.1% | 4.3 % |
Patients were selected for enrollment in the study as follows. Inclusion criteria: BP ≥135/85 mm Hg (average of at least 4 assessments according to self measurement); exclusion criteria: BP ≥160/110 mm Hg, history of stroke or myocardial infarction, antihypertensive therapy with 3 or more drugs, diabetes mellitus type 2, secondary hypertension, severe concomitant disease of any kind. The study was approved by the Ethics Commitee of the University of Erlangen‐Nuremberg, and written informed consent was obtained prior to study inclusion.
The SDM interventions were performed only by physicians who had undergone special communication training that was followed by regular supervision. 14 The trained physicians had regular SDM consultations with their patients following a fixed time schedule intended to make decisions on further treatment (1, 3, 6, and 12 months). Physicians of control patients did not take part in such a special communication program thereby avoiding any contamination with the SDM group. Subjects in both the SDM and control groups took part in the patient education program which consisted of 5 modules on the main topics of hypertension; these have been evaluated previously. 13
The quantitative evaluation mainly referred to BP decreases assessed by self‐measurements. Validated questionnaires were used to assess knowledge of hypertension (Hypertension Questionnaire 13 ), doctor–patient‐relationship (Patient Questionnaire, Difficult‐Doctor–Patient‐Relationship‐Questionnaire [DDPRQ] 15 ), and health related quality of life (Short Form 36‐Item Health Survey [SF‐36] 16 ), preference for SDM (Autonomy. Preference Index [API] 7 ), and the practice of SDM (Combined Outcome Measure for Risk Communication and Treatment Decision Making Effectiveness [COMRADE] 17 ). SDM was measured based on COMRADE, but an additional supplemental questionnaire was used to control for ceiling effects of COMRADE (support by the Institute for Medical Research Management and Biometrics, Nuremberg, Germany [IMEREM]): SDM was measured based on a sum score built from a factor analysis of COMRADE and an additional supplemental questionnaire to control for ceiling effects of COMRADE (support by IMEREM). Patients in the SDM and control group were monitored by self questionnaire and physicians’ records for the antihypertensive drugs actually taken.
Statistics
The primary objective was to analyze the changes in BP with respect to the practice of SDM during the observational period. A decrease of systolic BP by 5 mm Hg (standard deviation 11 mm Hg) in the SDM group was considered significant (α=0.05, β=0.80). Other comparisons were secondary: comparison of the BP changes between the 2 groups and subgroup analysis, such as patients with a high interest in SDM as compared to those with low interest in SDM classified by the median value of the API was also done. Analyses were performed using SPSS Software (Release 12.0; SPSS Inc., Chicago, IL) with paired and unpaired Student t‐test, analysis of variance (ANOVA), Spearman correlation, or further nonparametric tests where appropriate. Data are given as mean ± standard deviation. A P‐value <0.05 (2‐sided) was considered to be significant.
Results
Blood Pressure
The BP (self measurements by the patients) decreased from baseline after 1 year by −9.26±10.2 mm Hg/Δ−5.33±9.5 mm Hg in the SDM group and −6.0±11.8 mm Hg/Δ−3.0±8.3 mm Hg in the control group (systolic P=0.001 and P=0.002, respectively; diastolic P=0.001 and P=0.02, respectively). Thus, in both groups BP decreased (Figure 1) but there were no significant differences between the 2 groups (systolic P=0.24 and diastolic P=0.19, respectively).
Figure 1.
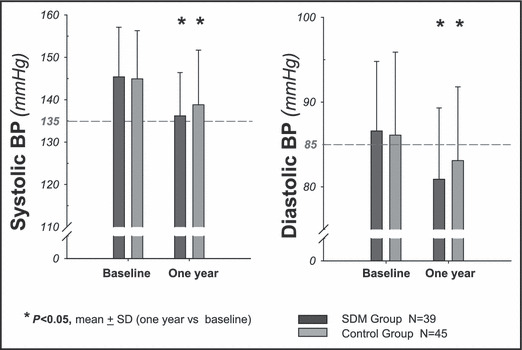
Systolic as well as diastolic blood pressure (BP) were lowered during the study to the same extent in patients practicing shared decision making (SDM) and in the patients enrolled in the education program on hypertension (baseline, after 1 year). SD indicates standard deviation.
Preference for SDM
The preference for SDM as assessed by the API (Figure 2) showed no differences between the SDM and control group at baseline (P=0.60) and did not change after 1 year (P=0.83).
Figure 2.
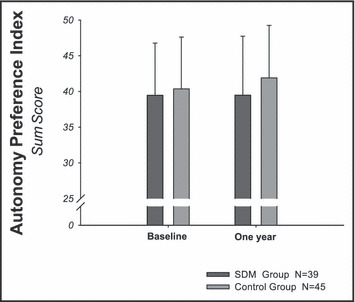
The results concerning blood pressure decreases cannot be attributed to a different desire for shared decision making (SDM) expressed at baseline in the 2 groups since the respective questionnaire (Autonomy Preference Index) revealed identical results at the beginning and after 1 year.
Shared Decision Making
The degree of SDM (Figure 3) was significantly higher in the SDM group at baseline and after 1 year visits. Both groups showed an increase in SDM (both P=0.001).
Figure 3.
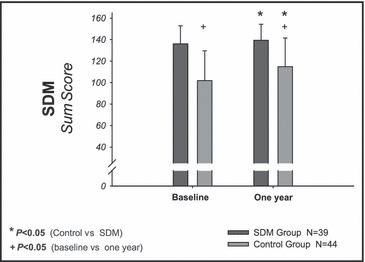
The results of the shared decision making (SDM) sum score on actually practiced SDM exhibited in both groups significantly increased, but the control group did not reach the score of the study group after 1 year.
In the SDM group, there was no correlation between BP decreases and the increase of SDM (systolic: r=0.15, P=0.19; diastolic: r=0.02, P=0.82).
Only in a subgroup analysis of patients with primarily a high interest in participating in medical decisions SDM patients with a great desire for SDM showed a correlation between an increase of SDM and decrease of systolic BP (r=−0.49, P=0.042) and diastolic (r=−0.524, P=0.043).
Knowledge of Hypertension
At baseline, control patients primarily exhibited a better knowledge about hypertensive issues than the study group (P=0.005). Only in the SDM group was there an increase in knowledge after 1 year (P=0.006). After 1 year both groups showed similar levels of knowledge.
Health‐Related Quality of Life
There were no differences between the 2 groups concerning health‐related quality of life measured with the 8 scales of SF‐36.
Doctor–Patient Relationship
Doctor–patient relationship as rated by patients was better in the SDM group than in the control group at the beginning of the study (P=0.0013) and after 1 year (P=0.0016). In the control group on the other hand, we observed an improvement in this respect (P=0.045) that did not occur in the SDM group (P=0.16).
Discussion
Our study demonstrates that patient empowerment by education programs in small groups alone improves BP control in addition to antihypertensive drug treatment. 13 , 18 SDM implemented in the treatment of hypertension was in general not found to exert additional BP lowering effects compared to the education program alone.
This is of interest for 2 reasons:
First, from the beginning the SDM group exhibited a greater degree of interest in SDM than the control group. This is in itself not unexpected since the patients could not be blinded concerning the allocation to either group or the aims of the study. Furthermore, we observed in both groups a similar increase in SDM; hence the SDM score was again higher in the SDM group after 1 year than in control patients.
Second, it turned out that baseline formal knowledge on matters relative to hypertension was significantly higher in the control group as compared to the SDM group. Thus, it might have been expected that a steeper increase in knowledge combined with a diligent implementation of SDM would favor a better outcome of BP control in the SDM group. Clearly, this was, in general, not the case.
These results suggest that neither better knowledge regarding hypertension 18 , 19 nor the intended modification of the decision‐making process as suggested by the SDM concept 11 was effective in altering the patients’ behavior and attitudes towards hypertension. A close relationship of a high degree of risk awareness and treatment with high control rates was, however, observed. 20 Which sociopsychological factors played a role in this group process cannot be conclusively answered from our study 21 but concomitant improvement of relationships between patient and doctor might also play a role. 22 Inclusion of patients in the control group improved the patient–doctor relationship; this can be considered a result of the patient empowerment.
One could argue that our group sizes were too small to draw conclusions. However, the results are relatively clear in favor of education programs themselves leading to patient empowerment; a substantial shift of the results is not likely with more patients enrolled. 11 , 23 In contrast, for the subgroup analyses we found a weak statistical result favoring the practice of SDM in patients with an initial great desire to be involved in decisions about their own treatment. This statistical correlation, however, was only found in the SDM group between systolic BP and the practice of SDM. Even if one argues that further research would provide parameters which could be of importance in patient selection for SDM and hypothetically influence outcomes, one problem remains: the size effect is low in light of the high need of resources to establish SDM.
The conclusion of our results favors the implementation of patient education programs for hypertensives thus empowering patients to participate in the control of their disease in times of economic constraints in many health care systems.
Disclosure: This work was supported by a Grant‐in‐Aid from the Federal Ministry of Health, Berlin, Germany to R.E. Schmieder. The authors’ work was independent of the funding institution. All authors agree that with respect to this paper there is no conflict of interest.
References
- 1. Cogolludo A, Perez‐Vizcaino F, Tamargo J. New insights in the pharmacological therapy of arterial hypertension. Curr Opin Nephrol Hypertens. 2005;14:423–427. [DOI] [PubMed] [Google Scholar]
- 2. Mancia G, De Backer G, Dominiczak A, et al. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25:1105–1187. [DOI] [PubMed] [Google Scholar]
- 3. Wolf‐Maier K, Cooper RS, Banegas JR, et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA. 2003;289:2363–2369. [DOI] [PubMed] [Google Scholar]
- 4. Ross SD, Akhras KS, Zhang S, et al. Discontinuation of antihypertensive drugs due to adverse events: a systematic review and meta‐analysis. Pharmacotherapy. 2001;21:940–953. [DOI] [PubMed] [Google Scholar]
- 5. Schroeder K, Fahey T, Ebrahim S. Interventions for improving adherence to treatment in patients with high blood pressure in ambulatory settings. Cochrane Database Syst Rev. 2004:CD004804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;60:301–312. [DOI] [PubMed] [Google Scholar]
- 7. Ende J, Kazis L, Ash A, et al. Measuring patients’ desire for autonomy: decision making and information‐seeking preferences among medical patients. J Gen Intern Med. 1989;4:23–30. [DOI] [PubMed] [Google Scholar]
- 8. Edwards A, Elwyn G, Hood K, et al. Patient‐based outcome results from a cluster randomized trial of shared decision making skill development and use of risk communication aids in general practice. Fam Pract. 2004;21:347–354. [DOI] [PubMed] [Google Scholar]
- 9. Elwyn G, Edwards A, Kinnersley P, et al. Shared decision making and the concept of equipoise: the competences of involving patients in healthcare choices. Br J Gen Pract. 2000;50:892–899. [PMC free article] [PubMed] [Google Scholar]
- 10. Elwyn G, Edwards A, Wensing M, et al. Shared decision making: developing the OPTION scale for measuring patient involvement. Qual Saf Health Care. 2003;12:93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Elwyn G, Edwards A, Mowle S, et al. Measuring the involvement of patients in shared decision‐making: a systematic review of instruments. Patient Educ Couns. 2001;43:5–22. [DOI] [PubMed] [Google Scholar]
- 12. Montgomery AA, Harding J, Fahey T. Shared decision making in hypertension: the impact of patient preferences on treatment choice. Fam Pract. 2001;18:309–313. [DOI] [PubMed] [Google Scholar]
- 13. Fleischmann EH, Friedrich A, Danzer E, et al. Intensive training of patients with hypertension is effective in modifying lifestyle risk factors. J Hum Hypertens. 2004;18:127–131. [DOI] [PubMed] [Google Scholar]
- 14. Deinzer A, Hegemann T, Veelken R, et al. [A model project on shared decision‐making in the treatment of arterial hypertension]. MMW Fortschr Med. 2004;146:48–50. [PubMed] [Google Scholar]
- 15. Hahn SR, Thompson KS, Wills TA, et al. The difficult doctor‐patient relationship: somatization, personality and psychopathology. J Clin Epidemiol. 1994;47:647–657. [DOI] [PubMed] [Google Scholar]
- 16. Alonso J, Ferrer M, Gandek B, et al. Health‐related quality of life associated with chronic conditions in eight countries: results from the International Quality of Life Assessment (IQOLA) Project. Qual Life Res. 2004;13:283–298. [DOI] [PubMed] [Google Scholar]
- 17. Edwards A, Elwyn G, Hood K, et al. The development of COMRADE – a patient‐based outcome measure to evaluate the effectiveness of risk communication and treatment decision making in consultations. Patient Educ Couns. 2003;50:311–322. [DOI] [PubMed] [Google Scholar]
- 18. Danzer E, Gallert K, Friedrich A, et al. [Results of an intensive training program for hypertension at the Institute for Preventive Medicine]. Dtsch Med Wochenschr. 2000;125:1385–1389. [DOI] [PubMed] [Google Scholar]
- 19. Danzer E, Gallert K, Henke J, et al. [Nurnberg Prevention Survey. “Prevention yes – but only when no effort is required”]. MMW Fortschr Med. 2000;142:46. [PubMed] [Google Scholar]
- 20. Moser M, Franklin SS. Hypertension management: results of a new national survey for the hypertension education foundation: Harris interactive. J Clin Hypertens (Greenwich). 2007;9:316–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kraetschmer N, Sharpe N, Urowitz S, et al. How does trust affect patient preferences for participation in decision‐making? Health Expect. 2004;7:317–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Roter DL, Stewart M, Putnam SM, et al. Communication patterns of primary care physicians. JAMA. 1997;277:350–356. [PubMed] [Google Scholar]
- 23. Snedecor GW, Cochran WG. Statistical Methods. Ames: Iowa State University Press; 1972. [Google Scholar]


