A 66‐year‐old man presented with a history of hypertension, dyslipidemia, and coronary artery disease. He had been taking different antihypertensive medications for 17 years. For the past 2 years, his regimen included amlodipine/olmesartan 10/40 every morning, metoprolol 25 mg every morning, and metoprolol 100 mg every night, as well as terazosin 2 mg every night. The patient has an automatic sphygmomanometer and checks his blood pressure (BP) regularly.
He went to Houston, Texas, for the Christmas holiday for 15 days and noticed that his BP was dropping, so he weaned himself off the BP medications in 2 days and finally stopped them altogether. In spite of that, his readings in Houston were systolic blood pressure (SBP), mean 106.07 mm Hg (ranging between 69 mm Hg and 148 mm Hg, standard deviation [SD] ±19.78); diastolic blood pressure (DBP), 66.53 (41 mm Hg and 98 mm Hg, SD ±15.27); and heart rate (HR), 92.63 beats per minute (67 and 112 beats per minute, SD ±9.84), which were monitored during a period of 15 days and 52 readings (Figure, Houston).
Figure.
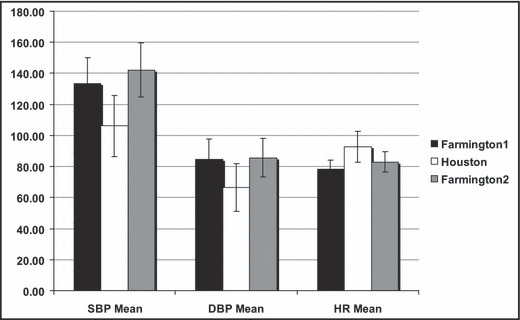
Bar graph comparing the mean systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) (with standard deviation) in Farmington, NM, before (Farmington1) and after going to Houston, TX, while taking medications (Farmington2), and in Houston, TX, while off medications (Houston).
His BP readings before his visit to Houston, while at home in Farmington, New Mexico, and while taking medications were SBP, 133.25 mm Hg (88 mm Hg and 152 mm Hg, SD ±16.86); DBP, 84.43 mm Hg (53 mm Hg and 104 mm Hg, SD ±13.04); and HR, 78.29 beats per minute (69 and 92 beats per minute, SD ±5.66), which were monitored during a period of 19 days and 48 readings prior to the trip to Houston (Figure, Farmington1).
After returning from Houston, his BP readings in Farmington, back on medications, were SBP, 142.05 mm Hg (101 mm Hg and 170 mm Hg, SD ±17.44); DBP, 85.66 mm Hg (52 mm Hg and 109 mm Hg, SD ±12.41); and HR, 82.97 beats per minute (67 and 102 beats per minute, SD ±6.69), which was monitored during a period of 14 days and 36 readings (Figure, Farmington2).
In summary, the BP was obviously noted to be more elevated in Farmington (even while taking the BP medications), compared with in Houston (while off the BP medications).
Farmington’s altitude is 5395 feet, and Houston’s is 55 feet above sea level. The temperatures in Farmington in the months of December and January range from a high of 42.0°F to 43.0°F and a low of 18.0°F to 19.0°F, and the barometric pressure is 30.00 in/Hg.
The temperatures in Houston in the months of December and January range from a high of 63.0°F to 65.0°F and a low of 43.0°F to 47.0°F, and the barometric pressure is 30.06 in/Hg. All other potential variables that could have affected the patient’s BP before, during, or after the trip, including level of stress, activity, lifestyle, or major dietary change, were discussed and excluded.
Discussion
Increased altitude introduces the additional factors of hypoxia, cold, wind, altitude sickness, dehydration, and stress associated with environmental change. 1 The pathophysiology of altitude‐related high BP is primarily related to hypoxia, compensatory hyperventilation, and low CO2 levels as a result of reduced bariatric pressure. A study by Wolfel and colleagues 2 demonstrated the association between acclimation of short‐term exposure to high‐altitude and sympathoadrenal activity. Cold‐induced diuresis with loss of blood volume causing hemoconcentration secondary polycythemia and increased blood viscosity, eventually contributing to the increased blood pressure, has been described. 3
Specific studies looking at cardiovascular risk associated with altitude‐related hypertension have not been accomplished. 3 Given the high prevalence of hypertension in the general population, it is a common medical condition that is often considered in this regard. Little information exists, however, to guide the management of this condition at high altitude. 4 The data regarding hypertension and its management at high altitude are very limited. Given the common nature of the problem and the increasing number of persons traveling to the mountains or even living in elevated areas, additional research is warranted to address these issues. 4
Conclusions
The available evidence suggests that BP rises to a modest extent in patients with mild to moderate hypertension upon acute ascent to high altitude, but there is no clear evidence of an increased risk of complications due to these increased pressures. There is, however, marked interindividual variability in BP responses at altitude. As a result, patients with poorly controlled or very labile hypertension should monitor their BP upon ascent to or descent from high altitude and travel with a plan for altering their medical regimen, preferably with help from their physician, in the event that marked or symptomatic BP changes occur.
Acknowledgments
Acknowledgments: I would like to thank Mr Richard Gibbons for his help in the statistical analysis and modifying of the graph bar for this manuscript.
References
- 1. Sizlan A, Ogur R, Ozer M, et al. Blood pressure changes in young male subjects exposed to a median altitude. Clin Auton Res. 2008;18:84–89. [DOI] [PubMed] [Google Scholar]
- 2. Wolfel EE, Selland MA, Mazzeo RS, et al. Systemic hypertension at 4,300 m is related to sympathoadrenal activity. J Appl Physiol. 1994;76:1643–1650. [DOI] [PubMed] [Google Scholar]
- 3. Handler J. Altitude‐related hypertension. J Clin Hypertens (Greenwich). 2009;11:161–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Luks AM. Should travelers with hypertension adjust their medications when traveling to high altitude? High Alt Med Biol. 2009;10:11–15. [DOI] [PubMed] [Google Scholar]


