Abstract
The authors sought to determine the prescribing practices of clinicians treating veterans with hypertension. A descriptive analysis was performed using a national pharmacy database of patients with a diagnosis of hypertension receiving antihypertensive medication in the fiscal years 2000 to 2006. Angiotensin‐converting enzyme inhibitors were the most frequently prescribed antihypertensive class, with utilization increasing from 56.0% in fiscal year 2000 to 63.2% of patients in 2006. Utilization of thiazide‐type diuretics increased from 31.9% of patients in fiscal year 2000 to 42.0% in 2006. When patient comorbidities were taken into consideration, 48.1% of patients defined as having uncomplicated hypertension had at least one prescription for a thiazide diuretic in fiscal year 2006. Utilization by monotherapy and combination therapy were also evaluated. The trends in utilization allowed for identification of areas in which a change in prescribing practices may improve blood pressure control and health outcomes in the Veterans Health Administration.
Hypertension remains a highly prevalent condition. According to the National Health and Nutrition Examination Survey (NHANES) data for 2001–2004, 25.3% of participants had a diagnosis of hypertension. 1 It has been estimated that >65 million Americans have blood pressure levels requiring therapy. 2 Within the Veterans Health Administration (VHA), in fiscal year (FY) 2006, there were 7.9 million veterans enrolled. with 5.5 million receiving health care services and 4.4 million receiving medications. 3 Of these enrollees, approximately 47% had a diagnosis of hypertension.
Despite data showing that elevated blood pressure is associated with an increased risk of vascular morbidity and mortality 4 , 5 and that treatment significantly reduces hypertension‐related morbidity and mortality, 6 , 7 , 8 it was reported in 2003 to 2004 that only 65.1% of patients with hypertension were being treated, 2 an increase of approximately 7% from 1999 to 2000. 2 , 9 A national survey in 2007 did, however, note that 90% of hypertensive patients were receiving some medication. 10 Although blood pressure awareness, treatment, and control are improving compared to previous reports, 2 , 9 , 11 there continues to be a need for improved blood pressure control. In the 2007 report, about 30% of patients who reported elevated blood pressure noted that their medication was not changed by their health care provider. 10
Treatment guidelines issued by the seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7, 2003) 11 and the VHA/Department of Defense (DoD) Clinical Practice Guideline on the Management of Hypertension in Primary Care (2004) 12 recommend a thiazide‐type diuretic as initial or concomitant therapy in most patients with hypertension. Agents from other antihypertensive classes may be considered based on patient comorbidities, treatment response, and the potential for adverse events.
The Department of Veterans Affairs (VA) VHA Hypertension Field Advisory Committee (FAC), a nationally appointed committee whose focus is to monitor, evaluate, and recommend best practices for treating hypertension in the VHA, in collaboration with the VHA Pharmacy Benefits Management (PBM) Services, sought to determine the trend in prescribing practices of clinicians treating veterans with hypertension in an effort to identify areas for improved blood pressure control and health outcomes. The Hypertension FAC also focused on the utilization of thiazide diuretics as monotherapy and in combination with other agents in specific hypertensive populations.
Methods
A descriptive analysis was performed with data obtained from the PBM and patient care databases for FYs 2000 to 2006. This project received approval by a VA investigational review board committee. The national PBM prescription database includes records of all pharmaceutical agents dispensed in the VA Medical Centers (VAMCs). The PBM database was checked for outpatients with at least 2 diagnoses of hypertension (by ICD‐9 code obtained from the VA National Patient Care Database [NCPD]) within each FY and receiving an active prescription for an antihypertensive medication. An active prescription was defined as at least one prescription for at least 90 days’ duration during the FY. The FY 2000 data consist of patients who were included in a PBM pilot study of the NPCD database to validate the accuracy of diagnostic coding as compared to the diagnostic information from the electronic medical record. The full administrative NPCD database was used for FY 2001 and 2002 and for 2004 through 2006. A representative sample was taken from the administrative NPCD database for FY 2003.
Patient utilization by antihypertensive drug class was broken down into thiazide‐type diuretics, angiotensin‐converting enzyme inhibitors (ACEIs), β‐adrenergic blockers (β‐blockers), calcium channel blockers (CCBs), α1‐adrenergic blockers (α‐blockers), angiotensin II receptor antagonists (also referred to as angiotensin II receptor blockers [ARBs]), loop and other diuretics, fixed‐dose combinations, and other (including central α‐agonists, direct vasodilators, and peripheral adrenergic inhibitors). Utilization was determined by evaluating the proportion of patients with a diagnosis of hypertension receiving antihypertensive medications by drug class and number of medications annually. As utilization of the fixed‐dose combination products including a thiazide‐type diuretic increased from FY 2000 to 2004, the data were reanalyzed for FY 2004 to include these patients as part of utilization in the respective drug classes. The patients on fixed‐dose combinations were also represented in the respective drug classes for FY 2005 and 2006.
In FY 2004, it was hypothesized that utilization may be influenced by patient comorbidities. Although we were not able to rerun previous evaluations, for FY 2004 to 2006, utilization was also evaluated by select patient comorbidities including benign prostatic hyperplasia (BPH), chronic heart failure (HF), diabetes mellitus (DM), and ischemic heart disease (IHD), as each of these was thought to have a potential influence on the selection of a particular antihypertensive drug class. Patients in each of these comorbidity cohorts were not mutually exclusive (ie, patients could be included in more than one comorbidity cohort). Data by comorbidity were also compared to those of patients without these specified diseases (ie, uncomplicated hypertension). Patient utilization by drug class prescribed as monotherapy as well as combination therapy and the percentage of patients on a thiazide diuretic as part of a 2‐drug or 3‐drug regimen were analyzed.
Results
The patient populations included by FY were as follows: FY 2000, 1,166,681; FY 2001, 1,464,068; FY 2002, 1,596,785; FY 2003, 1,005,393 (representative sample); FY 2004, 1,583,403; FY 2005, 1,607,630; and FY 2006, 1,619,824. Overall patient utilization of the various antihypertensive classes for FYs 2000 to 2006 are depicted in Figure 1 (note that data for FY 2003 represent a sample data set to determine whether using a sample would be comparable to the entire data set; although the trend appeared to be consistent with previous years, the full data set was used for the remainder of the annual evaluations).
Figure 1.
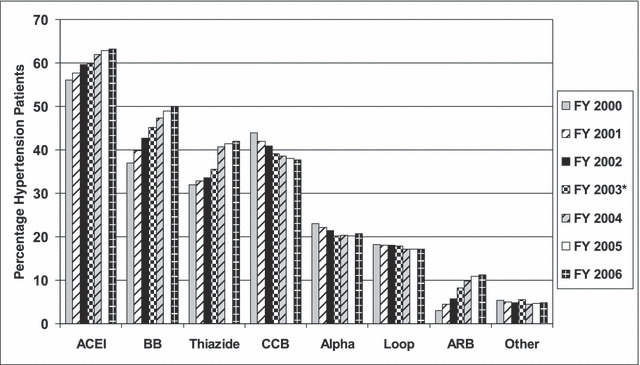
Veterans Health Administration patient utilization of antihypertensive medications by drug class (fiscal year [FY] 2000 to 2006). Drug classes include angiotensin‐converting enzyme inhibitors (ACEI); β‐adrenergic blockers (BB); thiazide diuretics (Thiazide); calcium channel blockers (CCB); α1‐adrenergic blockers (Alpha); loop plus other diuretics (Loop); angiotensin II receptor antagonists (ARB); and other (eg, clonidine, hydralazine, methyldopa, reserpine, and related medications). *Representative sample.
As shown in Figure 1, ACEIs were the most frequently prescribed antihypertensive class, with an increase from 56.0% in FY 2000 to 63.2% in FY 2006. In comparing data from FY 2000 to those from FY 2006, utilization of β‐blockers also steadily increased over the evaluation period from 37.0% to 49.9% of patients with hypertension, whereas CCBs decreased during this same time frame (from 44.0% to 37.6%). The percentage of patients receiving an α‐blocker decreased from FY 2000 to FY 2003, although the proportion remained at approximately 20% from FY 2003 to FY 2006. Utilization of ARBs increased from 3.0% in FY 2000 to 11.2% of patients with hypertension in FY 2006. Utilization of thiazide‐type diuretics increased from 31.9% in FY 2000 to 42.0% in FY 2006 (FY 2001, 32.8%; FY 2002, 33.5%; FY 2003, 35.5%; FY 2004, 40.7%; FY 2005, 41.4%). It should be noted that the data for thiazide‐type diuretic utilization during FY 2000 to FY 2003 do not include patients receiving fixed‐dose combination antihypertensive agents. Utilization of the fixed‐dose combinations increased from 0.2% in FY 2000, 0.4% in FY 2001, 0.9% in FY 2002, 1.7% in FY 2003, to 3.0% in FY 2004, at which time utilization of the fixed‐dose combinations were incorporated into the overall data set.
During FYs 2004 to 2006, patient data were also categorized by concomitant comorbidities (Figure 2 depicts data from FY 2006). During FY 2006, utilization of a thiazide diuretic was 48.1% in hypertensive patients without specified compelling indications but was lower when hypertension was associated with a comorbidity. In FY 2006, ACEIs were prescribed in approximately 73%, and β‐blockers and loop diuretics were each prescribed in more than 80% of patients with hypertension and concomitant HF. ACEIs were also widely prescribed in patients with IHD, and an ACEI was the most frequently prescribed therapy for patients with DM. Use of a β‐blocker increased from 76.3% of patients with IHD in FY 2004 to 78.1% in FY 2005 and 79.3% in FY 2006. In patients with concomitant HF, a β‐blocker was prescribed in 76.7% of patients in FY 2004, 80.4% in FY 2005, and 82.5% in FY 2006. When evaluating patients with uncomplicated hypertension (ie, patients who did not have one of the specified comorbidities), there was an increase in utilization of β‐blockers from 38.7% of patients in FY 2004 to 39.9% in FY 2005 and 40.6% in FY 2006. An α‐blocker was prescribed in >50% of patients with hypertension and concomitant BPH compared with 15.1% of patients with uncomplicated hypertension.
Figure 2.
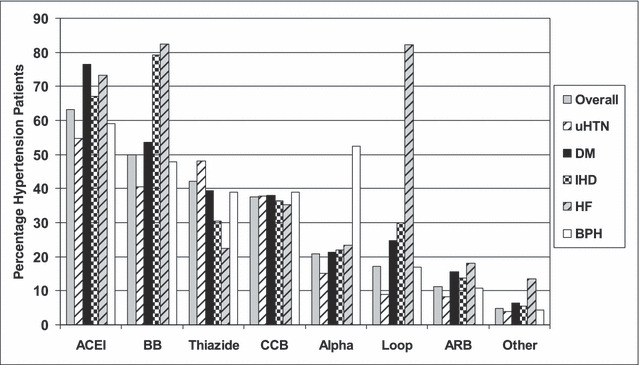
Veterans Health Administration patient utilization of antihypertensive medications by class and comorbidity (fiscal year 2006). Drug classes include angiotensin‐converting enzyme inhibitors (ACEI); β‐adrenergic blockers (BB); thiazide diuretics (Thiazide); calcium channel blockers (CCB); α1‐adrenergic blockers (Alpha); loop plus other diuretics (Loop); angiotensin II receptor antagonists (ARB); and other (eg, clonidine, hydralazine, methyldopa, reserpine, and related medications). Comorbidities include diabetes mellitus (DM), n=564,895; ischemic heart disease (IHD), n=347,417; heart failure (HF), n=72,741; benign prostatic hyperplasia (BPH), n=207,204; and uncomplicated hypertension (uHTN), n=720,268.
Utilization data by single agent (monotherapy) and combination therapy (≥2 agents) were also evaluated. From FY 2000 to FY 2006, the percentage of hypertensive patients treated with a single antihypertensive drug decreased from 32.0% to 22.6%, the percentage of those on 2 drugs decreased slightly from 35.0% to 33.0%, and the percentage of patients on 3 drugs increased from 22.0% to 26.2%; the percentage of patients receiving >3 drugs increased from 12.0% to 18.2%. During FY 2006, >77% of patients with hypertension were receiving ≥2 antihypertensive medications compared with 69% in FY 2000, and 44.4% were receiving ≥3 agents in FY 2006 compared with 34.0% in FY 2000.
Monotherapy data by drug class for FYs 2000 to 2006 are listed in Figure 3. During the evaluation period, utilization of a thiazide diuretic as monotherapy increased from 11.4% in FY 2000 to 14.0% in FY 2006. Monotherapy by drug class during FYs 2004 to 2006 was evaluated in all patients with hypertension as well as in patients with uncomplicated hypertension. For patients with uncomplicated hypertension receiving monotherapy in FY 2006, 34.2% received an ACEI, 19.8% a thiazide diuretic, 19.7% a β‐blocker, and 18.4% a CCB.
Figure 3.
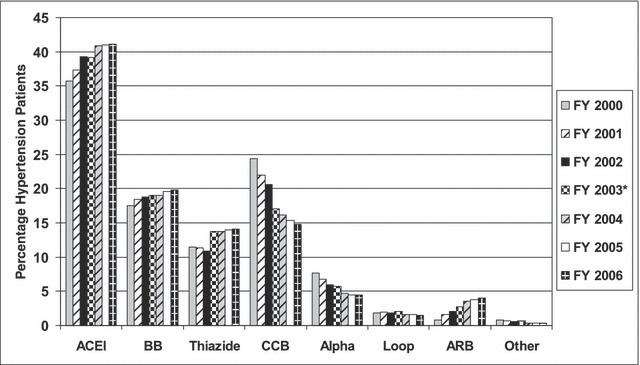
Veterans Health Administration patient utilization of antihypertensive monotherapy by drug class (fiscal year [FY] 2000 to 2006). Drug classes include angiotensin‐converting enzyme inhibitors (ACEI); β‐adrenergic blockers (BB); thiazide diuretics (Thiazide); calcium channel blockers (CCB); α1‐adrenergic blockers (Alpha); loop plus other diuretics (Loop); angiotensin II receptor antagonists (ARB); and other (eg, clonidine, hydralazine, methyldopa, reserpine, and related medications). *Representative sample.
In FY 2004, when the data were first evaluated by comorbidity, it was noted that an α‐blocker was prescribed as monotherapy in 3.8% of patients (n=8798) with uncomplicated hypertension. This decreased to 3.3% of patients (n=7098) in FY 2006. Of patients on combination therapy with 2 or 3 antihypertensive medications, a thiazide diuretic was prescribed in 40.2% and 53.9% of patients, respectively, during FY 2006, demonstrating an increase in utilization compared with FY 2000 (33.0% and 46.0%, respectively).
Discussion
Large national databases such as those available in the VHA provide a unique opportunity for monitoring prescription data of antihypertensive medications. These data may then be used by groups such as the Hypertension FAC and PBM to help guide policy and set goals for the management of hypertension.
We noted that utilization of thiazide‐type diuretics has increased in the veteran patient population with hypertension, with the largest increase from FY 2003 to FY 2004. Although not specifically evaluated in this analysis, this is thought to be due, in part, to the reporting of the primary results of the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) in 2002; the VA’s participation in ALLHAT, which included 70 VAMCs and >7000 veterans; and the recommendations of JNC 7 and the VHA/DoD Hypertension Clinical Practice Guidelines. In 1997, the JNC 6 recommended thiazide diuretics and β‐blockers as initial therapy. 13 In 2003, the JNC 7 recommended thiazide‐type diuretics for most patients with hypertension. 11 The VHA/DoD Hypertension Clinical Practice Guidelines were published in 1999 14 and then updated in 2004 12 with similar recommendations. Recommendations of the previous JNC V report (1993) included diuretics or β‐blockers as preferred initial antihypertensive therapy, although CCBs, ACEIs, α‐blockers, and α‐/β‐blockers were also considered appropriate for initial monotherapy. 15
During the past several years, outcomes trials evaluating the more recently approved antihypertensive classes (eg, ACEIs, CCBs, and ARBs) have been published. However, in several meta‐analyses, these drug classes have not been shown to be superior to thiazide‐type diuretics. 6 , 7 In addition to previous controlled clinical trials utilizing thiazide‐type diuretics, results of ALLHAT demonstrated that an α‐blocker, an ACEI, or a CCB as initial antihypertensive therapy was not superior to initial therapy with a thiazide‐type diuretic in preventing combined fatal coronary heart disease or nonfatal myocardial infarction. Treatment with the thiazide‐type diuretic did, however, result in a lower rate of combined cardiovascular disease, stroke, and heart failure compared with treatment with an α‐blocker or an ACEI and a lower rate of HF compared with treatment with a CCB. 16 , 17
Antihypertensive medication utilization within the VHA showed an initial increase in the use of ACEIs and CCBs, with a subsequent decrease in the use of CCBs and a shift toward utilization of thiazide diuretics and β‐blockers; this finding is similar but not entirely consistent with what has been seen in the private sector. 18 , 19 According to 2004 patient encounter data from a sample of office‐based physicians, utilization of an ACEI was highest, followed by that of a thiazide diuretic, a CCB, an ARB, and then a β‐blocker. 19 In addition to potential differences in patient comorbidities, the differences in utilization may be due, in part, to the implementation of national VHA/DoD Clinical Practice Guidelines and development of drug therapy criteria for use in VA facilities. The results of meta‐analyses evaluating β‐blockers in the treatment of hypertension did not appear to negatively affect utilization of this class during our period of evaluation. 20 , 21 As noted by Stafford and colleagues 19 the shift in utilization may reflect recommendations from clinical practice guidelines or evidence from published clinical trials, although not to the extent that would be anticipated.
In an effort to promote utilization of the thiazide diuretics and the possible added convenience for veterans, the Hypertension FAC recommended that fixed‐dose combination products including a thiazide diuretic be considered for addition to the VA national formulary. Two fixed‐dose combination products (atenolol/chlorthalidone and hydrochlorothiazide/lisinopril) were added in 2001. We also noted that there had been more than a 10‐fold increase in utilization of fixed‐dose combination antihypertensive agents in patients with hypertension in FY 2004 (the final time point at which data on fixed‐dose combination therapy were run separately) compared to FY 2000 (although the percentage of these was still fairly low).
There was a dramatic decrease in the utilization of monotherapy in the VHA, whereas more intense therapy with combinations of ≥3 antihypertensive agents increased over the evaluation period. According to the VHA data, <23% of patients with hypertension in FY 2006 were receiving 1 antihypertensive medication, and >44% of patients were receiving ≥3 antihypertensive medications. This decrease in monotherapy has been associated with improving blood pressure control rates in the VHA. 22 In the North American study sites of ALLHAT, approximately 63% of patients received ≥2 antihypertensive medications provided by the trial (the blinded initial therapy plus a β‐blocker, clonidine or reserpine as options for step 2 therapy, and hydralazine as step 3). 16 After 5 years, the blood pressure goal of <140/90 mm Hg was achieved in only 26% of study participants with a single antihypertensive agent and in only 49% using 1 or 2 agents. 23 Therefore, approximately half of patients required ≥3 drugs to achieve the blood pressure goal. A limitation of our data is that if one of the medications is discontinued in a patient previously receiving combination therapy with 2 medications, he or she is still counted as receiving both medications; thus, we may be slightly underestimating the number of patients on monotherapy.
Patients with comorbidities tended to receive combination therapy more often than patients with uncomplicated hypertension, although 70% of patients with uncomplicated hypertension also received combination therapy with ≥2 agents (PBM data on file), an indication that more intense therapy may lead to improved blood pressure control. 22 , 23 , 24 , 25 Despite this trend of utilizing combination therapy more often, providers frequently failed to include a thiazide diuretic as part of the antihypertensive regimen; a thiazide diuretic was prescribed in only 40.2% and 53.9% of patients who were receiving 2 and 3 antihypertensive medications, respectively, during FY 2006. This may provide one explanation for less than optimal blood pressure control, since regimens that include a thiazide‐type diuretic are more likely to control blood pressure than regimens without a thiazide. 26
We evaluated several comorbidities, specifically BPH, DM, HF, and IHD, as these disease states appeared to influence the selection of initial or concomitant therapy. As recommended in JNC 7, patients with HF or post–myocardial infarction have a compelling indication for treatment with an ACEI and/or a β‐blocker. In patients with DM, a diuretic, an ACEI, a β‐blocker, a CCB, or an ARB is recommended in JNC 7 as well as in the VHA/DoD Hypertension Clinical Practice Guidelines. 11 Although not listed as having a “compelling indication,”α‐blockers are indicated for patients with symptomatic BPH and are widely prescribed in patients with this diagnosis. As the majority of patients with hypertension will require >1 medication to control their blood pressure, the addition of a thiazide diuretic would be appropriate in most patients with concomitant diseases. Clinical trials demonstrating a benefit with a thiazide diuretic have often included patients with additional risk factors for coronary heart disease (eg, type 2 DM, previous myocardial infarction, left ventricular hypertrophy, low high‐density lipoprotein cholesterol, cigarette smoking), or other cardiovascular disease. 11 , 16 , 27
In addition to monitoring medication utilization, the PBM database has been used to identify potential medication safety concerns and to monitor the impact of interventions. One such project was a national effort to reduce utilization of short‐acting nifedipine for the treatment of hypertension. 28 During the evaluation of antihypertensive treatment in veteran patients with hypertension, the use of α‐blockers as monotherapy in patients with hypertension was also identified as a potential safety initiative although they are often considered for use in patients with symptomatic BPH. In fact, monotherapy with an α‐blocker is not recommended, as this treatment arm in ALLHAT was discontinued due to an increased risk of stroke and combined cardiovascular disease events and an increase in the risk of HF in patients treated with doxazosin compared with chlorthalidone. 17 , 29 According to the evaluation of the VHA antihypertensive medication utilization data in FY 2004, α‐blocker monotherapy represented 4.7% of the overall cohort. When the data were evaluated by comorbidity, it was noted that 3.8% of patients with uncomplicated hypertension (ie, without a diagnosis of BPH) were receiving an α‐blocker as monotherapy for the treatment of hypertension. As a result, an effort was undertaken to determine whether a change in antihypertensive regimen was warranted. Since implementation, there has been a decrease in 1700 patients being treated with an α‐blocker as monotherapy for the treatment of uncomplicated hypertension (PBM data on file).
The VHA experience with hypertension is similar to other national surveys. Of the nearly 8 million veterans enrolled in the VHA, approximately 47% have a diagnosis of hypertension. This figure is higher than the 25.3% of participants in NHANES (2001 to 2004), although it is comparable to the 45.8% and 58.5% of men aged 55 to 64 and 65 to 74 years, respectively. 1 The percentage of patients in the VHA being treated with an antihypertensive medication is comparable to data from NHANES. However, VHA blood pressure control is better than noted in NHANES. According to blood pressure control data from the VHA Office of Quality and Performance External Peer Review Program (ie, sample review of veteran patient medical records), approximately 67% of patients with hypertension sampled in the VHA had a blood pressure level <140/90 mm Hg during FY 2004 (73% when a blood pressure target of ≤140/90 mm Hg was used); this compared with 42% of patients during FY 2000. 24 Data from NHANES reported that approximately 37% of the overall survey population with hypertension had their blood pressure controlled (<140/90 mm Hg) during 2003 to 2004. 2 A trend toward more intensive antihypertensive therapy (ie, use of ≥3 medications) and an increase in the use of thiazide diuretics as described in the results may account for the improvement in blood pressure control over the past several years. 23 , 24 , 25 , 26 In the recent national Harris survey, >50% of hypertensive patients reported that their blood pressure was controlled. 10
Over time, the VHA data demonstrated a lower prescribing rate for thiazide diuretics than would be suggested by evidence from trials and guideline recommendations. More specifically, there has been only a modest increase in thiazide prescribing since 2004. Clinical trial evidence and clinical practice guideline recommendations impact prescribing practices, although the effect may be less than desired for a variety of reasons including differing recommendations from guidelines published outside the United States. In addition, evaluation of risk vs benefit to the patient based on potential adverse events or contraindications, provider or patient resistance to change, and the influence of marketing 19 , 30 may have an impact and require specific interventions to change prescribing practices. 24 , 31 , 32 , 33 There can also be a lag time in the development and approval of the VHA/DoD clinical practice guideline recommendations. To assist in implementation of the guideline recommendations, the VHA Office of Quality and Performance and other national groups within the VHA develop electronic clinical reminders, videotapes, and national performance measures. Implementation of these additional tools to educate clinicians and promote the guideline recommendations often require additional time to develop and disseminate, which may account, in part, for the less than expected and gradual change in therapy based on published recommendations. As a result, the VHA has recently completed a pilot‐phase nationwide performance measure program, more fully implemented for FY 2007, to encourage increased prescribing of thiazide diuretics in patients with uncomplicated hypertension. We suspect that this pilot program has already had some impact. Performance measures may prompt clinicians to improve thiazide use in patients with complicated hypertension (ie, those with compelling indications) who are already receiving appropriate medication for the specific comorbidity but who might benefit from the addition of a thiazide diuretic. We note that in Norway, implementation of a mandatory prescribing rule whereby a thiazide diuretic was the only drug class that would be reimbursed as initial therapy for uncomplicated hypertension increased thiazide diuretic use from approximately 10% to nearly 25% after the health care policy intervention. 31
The ability of the PBM database to evaluate prescribing practices within the VHA is unique in that the majority of veterans who seek care within the system receive all or most of their medications through the VA. Possible limitations to the accuracy of our database include the recent availability of medications outside the system at lower co‐payment rates. Thus, the true utilization rates of antihypertensive agents may not be captured, especially for lower‐cost generic agents or medications that can be obtained elsewhere over‐the‐counter. To deal with this potential limitation, the VHA has recently implemented a program to incorporate non‐VA medications into the patient’s electronic medication profile. This information was recently put into the national PBM database and has enhanced the accuracy of medication utilization reporting for some of the lower‐cost agents. Another limitation to our data was the use of comorbidities as entered by their ICD‐9 code; this is dependent on a number of factors including the accuracy of coding, the manual input of the diagnosis, and the program for data retrieval. In addition, we were unable to evaluate our data based on age, sex, or ethnic status or correlate medication use with reported adverse events. Adherence to the medication regimen was also not evaluated for this analysis, so it can only be documented that the prescription was written for and filled by the patient. However, there is no guarantee that the medication was actually taken as prescribed. This report should therefore be interpreted within the context of these limitations.
Conclusions
Based on recommendations of US clinical practice guidelines and evidence‐based recommendations published in the medical literature, thiazide‐type diuretics continue to be promoted for most patients with hypertension in the VHA. The prescription and patient databases allowed the VHA Hypertension FAC and PBM to document increased utilization of the thiazide diuretics in patients with hypertension. Trends in utilization provided the ability to evaluate adherence to therapeutic recommendations and allowed for identification of areas in which a change in prescribing practices might improve blood pressure control and health outcomes in the VHA.
Acknowledgments
Acknowledgements and disclosures: We would like to acknowledge the contributions of Sandra M. Walsh, MA,VAMC Memphis, Hypertension/Lipids Research Section, and Roxane Rusch, RN, BSN, MPA, clinical specialist for policy analysis and forecasting and VHA Office of the Assistant Deputy Under Secretary for Health for Policy and Planning, for their involvement on the Hypertension Field Advisory Committee. William C. Cushman, MD, has received grant/research support from Novartis Pharmaceuticals and Abbott Laboratories and is a consultant for and/or has received honoraria from AstraZeneca, Sanofi Aventis, Bristol‐Myers Squibb, Novartis Pharmaceuticals, Pfizer Inc, Daiichi Sankyo, Forest Laboratories, King Pharmaceuticals, Boehringer Ingelheim, Roche Pharmaceuticals, Calpis Company Ltd, Myogen, Inc, and Takeda Pharmaceutical Company Ltd. Jan Basile, MD, has received grant/research support from Boehringer Ingelheim and Novartis Pharmaceuticals and is on the speaker’s bureau for AstraZeneca, Boehringer Ingelheim, Daiichi Sankyo, Forest Laboratories, Merck, and Novartis Pharmaceuticals. Lois A. Katz, MD, has received grant/research support from Boehringer Ingelheim, Abbott Laboratories, and Kos Pharmaceuticals and honoraria from Novartis Pharmaceuticals. Dan R. Berlowitz, MD, has received grant/research support from Bristol‐Myers Squibb and Sanofi Aventis and honoraria from Bristol‐Myers Squibb. Vasilios Papademetriou, MD, has received grant/research support from AstraZeneca and honoraria from AstraZeneca and Novartis Pharmaceuticals.
References
- 1. National Center for Health Statistics . Health, United States, 2006. With Chartbook on Trends in the Health of Americans. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2006. Available at: http://www.cdc.gov/nchs/data/hus/hus06.pdf. Accessed June 6, 2007. [Google Scholar]
- 2. Ong KL, Cheung BM, Man YB, et al. Prevalence, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. [DOI] [PubMed] [Google Scholar]
- 3. Office of the Assistant Deputy Under Secretary for Health for Policy and Planning . VHA Enrollment, Patients and Expenditures. Washington, DC: U.S. Department of Veterans Affairs Intranet Site; 2007. Available at: http://vaww.va.gov/vhaopp/default.htm. Accessed June 6, 2007. [Google Scholar]
- 4. Lewington S, Clarke R, Qizilbash N, et al. Prospective Studies Collaboration. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2003;360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 5. MacMahon S, Peto R, Cutler J, et al. Blood pressure, stroke, and coronary heart disease: part 1, prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet. 1990;335:765–774. [DOI] [PubMed] [Google Scholar]
- 6. Psaty BM, Lumley T, Furberg CD, et al. Health outcomes associated with various antihypertensive therapies used as first‐line agents: a network meta‐analysis. JAMA. 2003;289:2534–2544. [DOI] [PubMed] [Google Scholar]
- 7. Blood Pressure Lowering Treatment Trialists’ Collaboration . Effects of different blood‐pressure‐lowering regimens on major cardiovascular events: results of prospectively‐designed overviews of randomized trials. Lancet. 2003;362:1527–1535. [DOI] [PubMed] [Google Scholar]
- 8. Staessen JA, Wang JG, Thijs L. Cardiovascular prevention and blood pressure reduction: a quantitative overview updated until March 2003. J Hypertens. 2003;21:1055–1076. [DOI] [PubMed] [Google Scholar]
- 9. Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206. [DOI] [PubMed] [Google Scholar]
- 10. Moser M, Franklin SS. Hypertension management: results of a new national survey for the Hypertension Education Foundation: Harris Interactive. J Clin Hypertens. 2007;9:316–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 12. VHA/DoD Clinical Practice Guideline for the Diagnosis and Management of Hypertension in the Primary Care Setting. Washington, DC: Office of Quality and Performance and the Veteran Affairs and Department of Defense Development Work Group, Veterans Health Administration, Department of Veterans Affairs; May 1999. Update 2004. [Google Scholar]
- 13. Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure and the National High Blood Pressure Education Program Coordinating Committee . The Sixth Report of the Joint National Committee on prevention, detection, evaluation and treatment of high blood pressure. Arch Intern Med. 1997;157:2413–2446. [DOI] [PubMed] [Google Scholar]
- 14. VHA/DoD Clinical Practice Guideline for the Diagnosis and Management of Hypertension in the Primary Care Setting. Washington, DC: Office of Quality and Performance and the Veteran Affairs and Department of Defense Development Work Group, Veterans Health Administration, Department of Veterans Affairs; 1999. [Google Scholar]
- 15. Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure . The Fifth Report of the Joint National Committee on detection, evaluation, and treatment of high blood pressure. Arch Intern Med. 1993;153:154–183. [PubMed] [Google Scholar]
- 16. The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group . Major outcomes in high‐risk hypertensive patients randomized to angiotensin‐converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288:2981–2997. [DOI] [PubMed] [Google Scholar]
- 17. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group . Diuretic versus alpha‐blocker as first‐step antihypertensive therapy. Final results from the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Hypertension. 2003;42:239–246. [DOI] [PubMed] [Google Scholar]
- 18. Ma J, Lee KV, Stafford RS. Changes in antihypertensive prescribing during US outpatient visits for uncomplicated hypertension between 1993 and 2004. Hypertension. 2006;48:846–852. [DOI] [PubMed] [Google Scholar]
- 19. Stafford RS, Monti V, Furberg CD, et al. Long‐term and short‐term changes in antihypertensive prescribing by office‐based physicians in the United States. Hypertension. 2006;48:213–218. [DOI] [PubMed] [Google Scholar]
- 20. Carlberg B, Samuelsson O, Lindholm LH. Atenolol in hypertension: is it a wise choice? Lancet. 2004;364:1684–1689. [DOI] [PubMed] [Google Scholar]
- 21. Lindholm LH, Carlberg B, Samuelsson O. Should β blockers remain first choice in the treatment of primary hypertension? A meta‐analysis. Lancet. 2005;366:1545–1553. [DOI] [PubMed] [Google Scholar]
- 22. Berlowitz DR, Cushman WC, Glassman P. Hypertension in adults across age groups. JAMA. 2005;294:2970–2971; author reply 2971–2972. [DOI] [PubMed] [Google Scholar]
- 23. Cushman WC, Ford CE, Cutler JA, et al. Success and predictors of blood pressure control in diverse North American settings: the antihypertensive and lipid‐lowering treatment to prevent heart attack trial (ALLHAT). J Clin Hypertens. 2002;4:393–404. [DOI] [PubMed] [Google Scholar]
- 24. Berlowitz DR, Ash AS, Hickey EC, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339:1957–1963. [DOI] [PubMed] [Google Scholar]
- 25. Wang YR, Alexander GC, Stafford RS. Outpatient hypertension treatment, treatment intensification, and control in Western Europe and the United States. Arch Intern Med. 2007;167:141–147. [DOI] [PubMed] [Google Scholar]
- 26. Materson BJ, Reda DJ, Cushman WC, et al. Results of combination anti‐hypertensive therapy after failure of each of the components. Department of Veterans Affairs Cooperative Study Group on Anti‐hypertensive Agents. J Hum Hypertens. 1995;9:791–796. [PubMed] [Google Scholar]
- 27. Whelton PK, Barzilay J, Cushman WC, et al. Clinical outcomes in antihypertensive treatment of type 2 diabetes, impaired fasting glucose concentration, and normoglycemia: Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2005;165:1401–1409. [DOI] [PubMed] [Google Scholar]
- 28. Furmaga EM, Glassman PA, Cunningham FE, et al. Reducing the use of short‐acting nifedipine by hypertensives using a pharmaceutical database. In: Henriksen K, Battles JB, Marks ES, Lewin DI, eds Advances in Patient Safety: From Research to Implementation. Vol. 3, Implementation Issues. AHRQ Publication No. 05‐0021‐3. Rockville, MD: Agency for Healthcare Research and Quality; 2005:277–289. [PubMed] [Google Scholar]
- 29. The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group . Major cardiovascular events in hypertensive patients randomized to doxazosin vs chlorthalidone: the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2000;283:1967–1975. [PubMed] [Google Scholar]
- 30. Lopez J, Meier J, Cunningham F, et al. Antihypertensive medication use in the Department of Veterans Affairs. Am J Hypertens. 2004;17:1095–1099. [DOI] [PubMed] [Google Scholar]
- 31. Fretheim A, Håvelsrud K, MacLennan G, et al. (2007) The effects of mandatory prescribing of thiazides for newly treated, uncomplicated hypertension: interrupted time‐series analysis. PLoS Med. 4: e232. doi: 10.1371/journal.pmed.0040232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jha AK, Perlin JB, Kizer KW, et al. Effect of the transformation of the Veterans Health Care System on the quality of care. N Engl J Med. 2003;348:2218–2227. [DOI] [PubMed] [Google Scholar]
- 33. Roumie CL, Elasy TA, Greevy R, et al. Improving blood pressure control through provider education, provider alerts, and patient education. Ann Intern Med. 2006;145:165–175. [DOI] [PubMed] [Google Scholar]


