Abstract
Adrenal venous sampling (AVS) remains controversial in the management of primary aldosteronism. Retrospective chart review was conducted at the Hospital of the University of Pennsylvania from July 2001 to September 2007. A total of 113 patients underwent AVS, 16 patients were excluded as records were unavailable. Among 97 remaining patients, 61 had unilateral disease and 57 underwent unilateral adrenalectomy. Blood pressure (BP) improved significantly with less antihypertensive medication requirement. Among those with different BP responses to adrenalectomy (cure, improvement, or no change), a higher number of preoperative antihypertensive medications was associated with persistent hypertension (P = .03). There were no significant differences in age (P = .14), duration of hypertension (P = .60), family history of hypertension (P = .68), or serum creatinine (P = .34). When AVS shows lateralization, age, duration of hypertension, family history, or renal dysfunction did not predict BP response to adrenalectomy. Results suggest that these factors should not preclude AVS and subsequent adrenalectomy. Further studies are indicated to confirm these findings.
Primary aldosteronism (PA) is increasingly recognized as an important cause of secondary hypertension. 1 , 2 PA not only causes refractory hypertension but is also associated with a higher cardiovascular morbidity irrespective of blood pressure (BP). 3 Recent data suggests that the prevalence of PA is higher than previously thought. A large prospective study reported that the prevalence of PA was 11% in newly diagnosed hypertensives 4 and as high as 38% in suspicious cases. 5
There are several subtypes of PA; aldosterone‐producing adenoma (APA), unilateral adrenal hyperplasia (UAH), 6 bilateral adrenal hyperplasia (BAH), and other rare causes. Unilateral disease (APA and UAH) is often treated with adrenalectomy with variable improvements in BP after adrenalectomy. Bilateral disease (BAH) is usually treated with multiple antihypertensive medications including aldosterone antagonists. 1
Adrenal venous sampling (AVS) distinguishes unilateral from bilateral disease. 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 It is, however, technically challenging and not used in all centers or only in select cases in some centers. 11 , 12 , 14 Whether AVS is always necessary and whether it changes clinical management has been debated. 11 , 12 , 14 In our program, we routinely confirm suspicious or diagnostic biochemical findings of increased aldosterone activity with AVS before undertaking adrenalectomy in patients who are willing to undergo surgery. The purpose of this study is to review clinical outcomes of patients who underwent AVS and examine the predictors of outcomes.
Methods
This is a retrospective chart review. Patients undergoing AVS studies at the Hospital of the University of Pennsylvania from July 2001 to September 2007 were identified from the radiology database, from which 22 cases were previously published. 13 The following data were collected: age, sex, race, duration of hypertension, serum creatinine, family history of hypertension in first‐degree relatives, plasma aldosterone concentration (PAC; in ng/dL), plasma renin activity (PRA; in ng/mL/h), PAC to PRA ratio, imaging studies of the adrenal glands, side of adrenal mass, results of AVS, pathologic findings of the surgical specimen, BP and the number of antihypertensive medications, serum potassium and potassium supplementation preoperatively and postoperatively, and the duration of follow‐up at the last available BP reading. To prevent confusion, we used the term hyperplasia for pathologic findings and bilateral adrenal mass for imaging findings. Direct renin levels or 24‐hour urine aldosterone was used for the diagnosis of PA in 9 and 1 patients, respectively. These data were excluded from the analysis of PAC, PRA, and PAC/PRA ratio. Saline loading was not routinely performed. Before the measurement of PAC and PRA or AVS, aldosterone antagonists (spironolactone and eplerenone) were held but other antihypertensive agents were continued. 15 , 16 , 17 For patients referred from outside practice, the referral letters were examined to obtain the necessary information. AVS was performed as described previously. 13 Briefly, the adrenal veins were catheterized via the percutaneous femoral vein approach. Blood samples were obtained from the inferior vena cava (IVC) and bilateral adrenal veins for the measurement of cortisol and aldosterone. For simultaneous technique, after baseline sampling, 0.25 mg of cosyntropin was administered as a bolus followed by 0.25 mg in 5 mL of normal saline solution infused over 10 to 15 minutes. For sequential technique, continuous infusion of cosyntropin was administered (0.25 mg in 500 mL of normal saline, 100 mL/h, beginning 1 hour before the sampling and throughout the procedure). For simultaneous technique, poststimulation values were used for analysis. Selectivity index (SI) was defined by a ratio of cortisol level in each adrenal vein compared with that in the IVC. Adequate sampling was determined by SI >5. 10 Lateralization index (LI) was defined by ipsilateral aldosterone to cortisol ratio (A/C ratio [ng/dL per g/dL]) over contralateral A/C ratio. AVS results are interpreted as follows: lateralization if LI >4 and no lateralization if LI <4. 10 , 13 , 18 The change in BP after adrenalectomy was defined as follows: cure when BP was <140/90 mm Hg without antihypertensive medications; improvement when systolic BP (SBP) decreased by >10 mm Hg with the same number of drugs or SBP remained within 10 mm Hg of difference from preoperative value with fewer antihypertensives; no change when the same number of antihypertensives was required to keep BP within 10 mm Hg of difference from preoperative value or BP increased by >10 mm Hg with fewer medications; worsening when more medications were required to control BP or BP increased with the same number of medications.
The protocol and the permission to waive written informed consents were approved by the institutional review board at the University of Pennsylvania.
Statistical Analysis
Continuous variables are expressed as mean followed by standard deviation. Continuous variables were compared by Student t test or analysis of variance (ANOVA) and categoric variables by chi‐square test using SPSS version 16.0 (SPSS Inc, Chicago, IL). A P value <.05 was considered statistically significant.
Results
Results of AVS
There were 127 studies of AVS performed on 113 patients from July 2001 to September 2007. In 114 studies AVS was performed by using a sequential technique, and in 13 studies AVS was performed using a simultaneous technique. The results were as follows: LI ≥4 in 61 (48%) and LI <4 in 54 (42%). In 10 studies, SI was <5. In 1 case, the blood sample was lost by the laboratory and in another case, the left renal vein was occluded and the procedure was voluntarily terminated. Excluding these 2 cases, the successful sampling (SI >5) was obtained in 115 of 125 cases (92%). Among them, SI was >10 in 112 cases (90%). In 12 patients, AVS was repeated twice (6 due to inadequate sampling, 6 due to borderline LI). In one patient, AVS was repeated 3 times due to technical difficulties and loss of the blood sample.
Patients’ Characteristics With Adrenalectomy and Without Adrenalectomy
Among 113 patients who had AVS, medical records were available for review in 97 patients. There were no significant differences in demographics (age, sex, and race) of the 16 patients without medical records and 97 with medical records (data not shown). The imaging findings and AVS results for these 97 patients are shown in Table I. There were 5 patients with equivocal AVS results. In these 5 cases, LIs were 2.7, 2.89, 3.18, 3.5, and 3.86. The decision for adrenalectomy was made due to the contralateral suppression of A/C ratio that was used for the criteria for lateralization in some studies. 7 , 8 In the last case, an LI of 3.86 was felt to be close enough for the cutoff of 4. Fifty‐six patients with lateralization and 5 patients with equivocal AVS results were considered to have unilateral disease. Among them, 3 were lost to follow‐up and 1 refused adrenalectomy. Thus, a total of 57 patients underwent adrenalectomy (details of patient flow are shown in Figure 1).
Table I.
Imaging Findings and AVS Results for 97 Patients With Medical Records
| No. | |
|---|---|
| Imaging | |
| Right adrenal mass | 26 |
| Left adrenal mass | 52 |
| Bilateral adrenal mass | 8 |
| No adrenal mass | 10 |
| Data not available | 1 |
| AVS | |
| Lateralization | |
| To the right | 30 |
| To the left | 26 |
| Equivocal (see text) | 5 |
| No lateralization | 36 |
Abbreviation: AVS, adrenal venous sampling.
Figure 1.
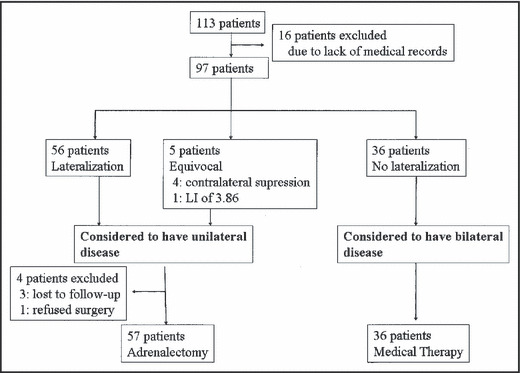
Details of 113 patients who underwent adrenal venous sampling. LI indicates lateralization index.
The characteristics of patients with different AVS results and response to surgery are summarized in Table II. All but 4 (all in the nonlateralized group) had PAC >15 ng/dL and PAC/PRA >20, which are consistent with the recent guidelines published by the Endocrine Society for screening for PA. 18 There was no significant difference in demographics, duration of hypertension, serum creatinine, family history of hypertension, PAC, size of mass, or severity of hypertension between those who underwent adrenalectomy and those who did not (data not shown). Patients who underwent adrenalectomy required significantly more potassium supplementation preoperatively compared with those who did not have surgery (24±40 vs 6.4±14.4 mEq; P=.02). They also had significantly lower PRA (0.33±0.30 vs 0.54±0.60 ng/mL/h; P=.02) and higher PAC/PRA ratio (199±130 vs 112±93 ng/dL per ng/mL/h; P=.002). When PAC and PRA were tested, 34% were taking an angiotensin‐converting enzyme inhibitor (ACEI) and 30% were taking an angiotensin receptor blocker (ARB).
Table II.
Clinical Characteristics of Groups According to AVS Findings
| Lateralization (n=56) | Equivocal (n=5) | No Lateralization (n=36) | |
|---|---|---|---|
| Imaging | |||
| Right adrenal mass | 19 | 2 | 5 |
| Left adrenal mass | 27 | 3 | 22 |
| Bilateral adrenal mass | 5 | 0 | 3 |
| No mass | 4 | 0 | 6 |
| Data not available | 1 | 0 | 0 |
| Contralateral suppression in AVS | 53 | 4 | 2 |
| Pathology | |||
| Adenoma | 40 | 4 | |
| Hyperplasia | 9 | 0 | |
| Hyperplasia with dominant adenoma | 2 | 1 | |
| Data not available | 1 | 0 | |
| No surgery | 4 | 0 | |
| Response to surgery | |||
| SBP, mm Hg | |||
| Preoperative | 148.0 (22.2) | 146.8 (29.0) | |
| Postoperative | 133.2 (19.3) | 147.0 (34.0) | |
| DBP, mm Hg | |||
| Preoperative | 87.7 (11.7) | 88.4 (16.7) | |
| Postoperative | 81.3 (10.6) | 86.0 (10.2) | |
| Hypertensive medications, No. | |||
| Preoperative | 3.4 (1.7) | 4.8 (0.5) | |
| Postoperative | 1.2 (1.1) | 1.4 (1.1) | |
| Serum potassium, mmol/L | |||
| Preoperative | 3.6 (0.6) | 3.7 (0.6) | |
| Postoperative | 4.0 (0.7) | 4.1 (0.5) | |
| Potassium supplement, mEq/d | |||
| Preoperative | 23.1 (40.2) | 35 (34) | |
| Postoperative | 1.5 (6.7) | 0 | |
Abbreviations: AVS, adrenal venous sampling; DBP, diastolic blood pressure; SBP, systolic blood pressure. Values are expressed as mean (standard deviation).
Clinical Outcomes of Unilateral Adrenalectomy
Clinical outcomes of unilateral adrenalectomy are summarized in Table II. BP improved significantly with fewer antihypertensive medications required (148±23/88±12 mm Hg with 3.5±1.7 medications preoperatively and 134±21/82±11 mm Hg with 1.2±1.1 medications postoperatively) (n=57). The duration of follow‐up was 9.4±15.8 months from the time of surgery. Serum potassium also significantly increased with less potassium supplementation. None of the patients were taking aldosterone antagonists or potassium‐sparing diuretics postoperatively. The improvement in hypertension was persistent up to 4 years (Figure 2). After adrenalectomy, hypertension was cured in 12 (21%), improved in 39 (68%), unchanged in 5 (9%), and worsened in 1 (2%). Overall, 89% of patients had either cure or improvement in BP control. In 1 patient, the number of antihypertensive medications was increased with no change in BP but it was indicated for worsening heart failure rather than for worsening hypertension. In comparison, 36 patients without lateralization showed significant improvement in BP at the last visit (132±14/ 83±10 mm Hg [P<.001 compared with initial visit]) but no change in the requirement of number of medications (3.5±1.4 [P=.75]) (duration of follow‐up was 35±21 months). Among them, 14 were taking spironolactone, 4 taking eplerenone, and 4 taking amiloride. Other patients were referred back to the referring physicians and therefore we do not have the data available on their use of aldosterone antagonists after AVS. None of these patients had a cure of hypertension during the follow‐up period.
Figure 2.
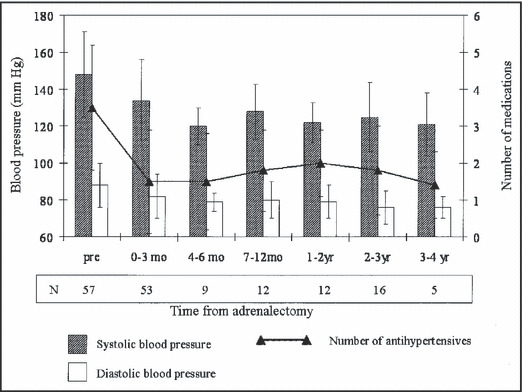
Change in blood pressure after adrenalectomy.
The characteristics of patients with different outcomes in BP control were summarized in Table III. Patients with persistent hypertension tended to be older, although this was not statistically significant. There was no significant difference in sex, race, duration of hypertension, serum creatinine, PAC, PRA, PAC/PRA ratio, LI by AVS, or preoperative BP. The requirement of more medication preoperatively was significantly associated with persistent hypertension. There was equivalent improvement in BP in adenoma and hyperplasia groups (data not shown). For 9 patients with hyperplasia, BP improved from 156.7±18.1/86.9±6.7 mm Hg to 135.8±14.9/82.9±8.5 mm Hg. Serum potassium increased from 3.6±0.7 mmol/L to 4.0±0.4 mmol/L. Potassium supplementation decreased from 20±42.8 mEq/d to 2.5±7.1 mEq/d.
Table III.
Characteristics of Patients With Different Blood Pressure Outcome
| Cure (n=12) | Improvement (n=39) | No Change (n=5) | P Valuea | |
|---|---|---|---|---|
| Age | 47.3 (5.7) | 50.9 (11.0) | 56.6 (8.3) | .14 |
| Sex (male:female) | 6:6 | 23:16 | 4:1 | .52 |
| Race | ||||
| White | 7 | 22 | 3 | .83 |
| African American | 2 | 7 | 0 | |
| Asian | 1 | 1 | 0 | |
| Unknown | 2 | 9 | 2 | |
| Duration of HTN, y | 14.4 (10.7) (n=8) | 12.7 (9.7) (n=33) | 12.5 (5.0) (n=4) | .60 |
| Serum creatinine, μmol/L and mg/dL | 79.6 (17.7) and 0.9 (0.2) (n=12) | 106.1 (61.9) and 1.2 (0.7) (n=39) | 79.6 (26.5) and 0.9 (0.3) (n=5) | .34 |
| Family history of HTN in first‐degree relative, % | 75 (6 of 8) | 63 (17 of 27) | 50 (2 of 4) | .68 |
| PAC, ng/dL | 47.6 (28.6) (n=7) | 41.1 (27.2) (n=29) | 31.1 (13.7) (n=4) | .78 |
| PRA, ng/mL/h | 0.45 (0.46) (n=7) | 0.31 (0.40) (n=29) | 0.24 (0.13) (n=4) | .28 |
| PAC/PRA, ng/dL per ng/mL/h | 164 (120) (n=7) | 211 (140) (n=29) | 158 (99) (n=4) | .70 |
| LI by AVS | 19.4 (16.8) (n=12) | 17.1 (15.2) (n=39) | 13.1 (17.2) (n=5) | .71 |
| Pathological findings | ||||
| Adenoma | 7 | 32 | 4 | .46 |
| Hyperplasia | 3 | 5 | 1 | |
| Hyperplasia with dominant adenoma | 1 | 2 | 0 | |
| Unknown | 1 | 0 | 0 | |
| Preoperative | ||||
| SBP, mm Hg | 140 (18) | 153 (23) | 128 (15) | .08 |
| DBP, mm Hg | 87 (9) | 89 (13) | 79 (13) | .13 |
| Antihypertensive medications, No. | 2.4 (1.3) | 3.9 (1.6) | 3.1 (2.2) | .03 |
| Antihypertensive medications, units | 1.8 (1.0) | 3.3 (1.6) | 3.1 (3.2) | .03 |
Abbreviations: AVS, adrenal venous sampling; DBP, diastolic blood pressure; HTN, hypertension; LI, lateralization index; PAC, plasma aldosterone concentration; PRA, plasma renin activity; SBP, systolic blood pressure. a P values for categoric variables are by chi‐square test and P values for continuous variables are by analysis of variance.
AVS Results and Clinical Outcomes in Patients With Lateralization
We hypothesized that a higher LI would predict better BP response after adrenalectomy. As shown in Table IV, there was no difference in BP response to adrenalectomy in patients with LI > or <10. We also used cutoff values of 5, 13, 15, 20, and 25 and there was still no significant difference (data not shown).
Table IV.
Characteristics of AVS Results and Clinical Outcomes in Patients With Lateralization
| LI <10 (n=26) | LI ≥10 (n=31) | P Valuea | |
|---|---|---|---|
| Preoperative | |||
| SBP, mm Hg | 146 (28) | 149 (17) | .62 |
| DBP, mm Hg | 87 (14) | 88 (10) | .75 |
| Antihypertensive medications, No. | 3.8 (1.6) | 3.3 (1.7) | .32 |
| Antihypertensive medications, units | 3.2 (1.9) | 2.8 (1.5) | .37 |
| Postoperative | |||
| SBP, mm Hg | 134 (23) | 135 (20) | .91 |
| DBP, mm Hg | 81 (9) | 82 (12) | .56 |
| Antihypertensive medications, No. | 1.5 (1.2) | 1.1 (1.0) | .18 |
| Antihypertensive medications, units | 0.9 (0.8) | 0.7 (1.0) | .58 |
Abbreviations: AVS, adrenal venous sampling; DBP, diastolic blood pressure; LI, lateralization index; SBP, systolic blood pressure. a P values by t test.
Discussion
Adrenal venous sampling is the gold standard test to differentiate unilateral from bilateral disease in patients with PA; however, it is technically difficult with a variable success rate. It has been debated whether it should be performed in all patients with PA or just in select cases. Also, there have been controversies over the use of cosyntropin stimulation and its interpretation.
In this single‐center experience, AVS was performed in all patients with PA and it was successfully achieved in 92%. In previous studies, the success rate ranged from 42% 12 to 95%. 10
Rossi and colleagues 19 , 20 evaluated whether cosyntropin stimulation improves the selectivity and lateralization of AVS. They concluded that it improves selectivity but increases false‐negative results for lateralization. In other studies, the use of cosyntropin was reported to improve the accuracy of interpretation. 12 , 13
Adequate sampling and lateralization have been variably defined by an SI of 1.1 to 5 (7–14) and an LI >2 to 5 (7–14), respectively. Rossi and colleagues 9 claim that an SI of 1.1 is sufficient and an LI of 2 gives the best sensitivity and specificity. Cosyntropin stimulation was not used in their study. An SI of 5 is accepted in most studies using cosyntropin stimulation. 8 , 10 , 13 Doppman and colleagues 7 demonstrated that an LI of 5 carries a positive predictive value of 0.96 and a negative predictive value of 1.00 for APA using pathological findings as a gold standard. In another study, Young and colleagues 10 demonstrated that an LI of 4 had a 95.2% sensitivity and 100% specificity for unilateral disease. In their study, they distinguished APA, UAH, and BAH using the combination of AVS, pathological findings, postoperative urinary aldosterone excretion, and the clinical course.
We used an SI ≥5 (most of the adrenalectomy patients had an SI ≥10) and an LI ≥4 as cutoff points with the use of cosyntropin stimulation. Recent guidelines from the Endocrine Society 18 pointed out that “many groups advocate the use of continuous cosyntropin infusion during AVS” although it did not make any discrete recommendation for or against its use. The guideline also mentioned that an SI ≥10 and an LI ≥4 have been used for the criteria for selective catheterization and for unilateral disease, respectively, with cosyntropin stimulation. The use of cosyntropin stimulation and the selection of cutoff points of SI and LI in our center are based on most accepted current clinical practice in accordance with guidelines by the Endocrine Society.
Hypokalemia was more severe in patients with lateralization as noted previously, when comparing patients who had lateralization and no lateralization. 5 , 9 Patients with lateralization had more suppression of PRA but no difference in PAC. This differed from previous reports, 5 , 9 which reported higher PAC but similar PRA. The reason for the difference is unclear. We also showed that there was significant difference in the presence of contralateral suppression of A/C ratio (contralateral A/C ratio less than that of IVC) in patients with lateralization compared with those without lateralization. This was also reported by Young and colleagues, 10 but in our study the difference was more pronounced (93% vs 6%, respectively, in our study and 94% vs 32%, respectively, in their study).
Fifty‐seven patients underwent unilateral adrenalectomy. Their BP improved significantly with significantly fewer antihypertensive medications. Overall, 89% of patients had achieved some benefit in BP control after adrenalectomy. This is comparable to previous studies. 21 , 22 , 23 , 24 , 25 , 26 It is well‐known that hypertension can persist after adrenalectomy in PA. The factors associated with persistence of hypertension are variably listed as age, longer duration of hypertension, higher PAC, family history of hypertension in a first‐degree relative, the number of antihypertensive medications before adrenalectomy, and serum creatinine level. 21 , 22 , 23 , 24 , 25 , 26 In these studies, patients were considered to have APA preoperatively depending on the presence of an adrenal mass on imaging studies. AVS was not always performed and often done only in select cases. In our study, compared with previous studies, 21 , 22 , 23 , 24 , 25 , 26 the patients’ mean age was higher (mean age in 40s in previous studies vs in early 50s in our study), duration of hypertension longer (<10 years in previous studies compared with >10 years in our study), and the number of antihypertensive medications taken before adrenalectomy was higher (mean number of antihypertensives of 2 or 3 in previous studies compared with >3 in our study). All of these are risk factors for a poor response to adrenalectomy. Nevertheless, we had comparable improvement in BP control. In our study, the number of antihypertensives required preoperatively was associated with persistent hypertension postoperatively but not age, duration of hypertension, family history, preoperative PAC, or serum creatinine. This suggests that older patients with a long history of hypertension may still benefit from unilateral adrenalectomy if AVS shows lateralization. It also raises the possibility that in previous studies that did not use AVS, they may have misclassified BAH with nonfunctional adenoma as APA. In general, patients with BAH are older. 1 Since older age is associated with longer duration of hypertension and higher creatinine, these may have caused an apparent association with persistent hypertension in their studies.
We also report that 16% of patients who showed lateralization by AVS had pathological findings of adrenal hyperplasia, suggestive of UAH. This is much higher than a previously reported prevalence of <2%. 10 There was no significant difference in the improvement of BP in adenoma and hyperplasia groups, suggesting that this was not due to a misclassification by AVS. UAH might have been underrepresented in previous studies that did not routinely use AVS.
We further examined whether the LI in AVS predicts the BP response from unilateral adrenalectomy. Higher LI did not predict BP response. This suggests that patients with lateralization (LI ≥4) will experience similar benefit from unilateral adrenalectomy.
Limitations
There are several limitations to our study. This is a retrospective single‐center study in a tertiary referral center. Because the sample size is relatively small, we cannot completely exclude the possibility that the absence of association with age, duration of hypertension, and family history may be due to a type 2 error. There could also be a referral bias. Since patients were referred for AVS from multiple practices, there was no standardized criterion for the referral to evaluate a possible diagnosis of PA and a salt‐loading test was not routinely performed. However, more than half of the patients were taking an ACEI or an ARB when PAC and PRA were measured. It is reported that a captopril suppression test is as effective as a salt‐loading test. 27 The continued use of an ACEI or ARB may have served as an equivalent of a suppression test. ACEIs and ARBs affect aldosterone and renin secretion and there is a theoretic concern that their use may confuse the interpretation of PAC/PRA. However, previous studies reported that PAC/PRA can still be interpreted with the use of antihypertensive agents other than aldosterone antagonists. 15 , 16 , 17 The American Heart Association Scientific Statement supported these findings. It only mandates the cessation of aldosterone antagonists before the measurement of PAC and PRA for the screening of PA. 28
We cannot rule out the possibility that patients without lateralization by AVS could have possibly benefited from adrenalectomy. It would have been informative if there were patients whose AVS suggested bilateral disease but who underwent adrenalectomy due to other reasons (such as significant adrenal enlargement over time) and whether we could compare the clinical outcomes of these patients with patients whose AVS showed lateralization. However, we did not find such a case in our series. Although the cure of hypokalemia without aldosterone antagonists or potassium‐sparing diuretics strongly suggests a biochemical cure of PA, postoperative PAC and PRA were not available. Thus we cannot definitively correlate the change in BP with biochemical cure of PA.
Conclusions
We report the clinical outcomes of patients with PA who underwent AVS. BP improved persistently with significantly fewer antihypertensive medications. Older age, duration of hypertension, and family history were not associated with persistent hypertension for patients with lateralization by AVS in our experience. Our data suggest that long duration of hypertension or family history should not necessarily exclude patients from having adrenalectomy. Additional studies are needed to confirm our findings.
References
- 1. Mattsson C, Young WF. Primary aldosteronism: diagnostic and treatment strategies. Nat Clin Pract Nephrol. 2006;2:198–208. [DOI] [PubMed] [Google Scholar]
- 2. Mantero F, Mattarello MJ, Albiger NME. Detecting and treating primary aldosteronism. Exp Clin Endocrinol Diabetes. 2007;115:171–174. [DOI] [PubMed] [Google Scholar]
- 3. Milliez P, Girerd X, Plouin PF, et al. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;45:1243–1248. [DOI] [PubMed] [Google Scholar]
- 4. Rossi GP, Bernini G, Caliumi C, et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol. 2006;48:2293–2300. [DOI] [PubMed] [Google Scholar]
- 5. Giacchetti G, Ronconi V, Lucarelli G, et al. Analysis of screening and confirmatory tests in the diagnosis of primary aldosteronism: need for a standardized protocol. J Hypertens. 2006;24:737–745. [DOI] [PubMed] [Google Scholar]
- 6. Goh BK, Tan YH, Chang KT, et al. Primary hyperaldosteronism secondary to unilateral adrenal hyperplasia: an unusual cause of surgically correctable hypertension. A review of 30 cases. World J Surg. 2007;31:72–79. [DOI] [PubMed] [Google Scholar]
- 7. Doppman JL, Gill JR, Miller DL, et al. Distinction between hyperaldosteronism due to bilateral hyperplasia and unilateral aldosteronoma: reliability of CT. Radiology. 1992;184:677–682. [DOI] [PubMed] [Google Scholar]
- 8. Phillips JL, Walther MM, Pezzullo JC, et al. Predictive value of preoperative tests in discriminating bilateral adrenal hyperplasia from an aldosterone‐producing adrenal adenoma. J Clin Endocrinol Metab. 2000;85:4526–4533. [DOI] [PubMed] [Google Scholar]
- 9. Rossi GP, Sacchetto A, Chiesura‐Corona M, et al. Identification of the etiology of primary alsdosteronism with adrenal vein sampling in patients with equivocal computed tomography and magnetic resonance findings: results in 104 consecutive cases. J Clin Endocrinol Metab. 2001;86:1083–1090. [DOI] [PubMed] [Google Scholar]
- 10. Young WF, Stanson AW, Thompson GB, et al. Role for adrenal venous sampling in primary aldosteronism. Surgery. 2004;136:1227–1235. [DOI] [PubMed] [Google Scholar]
- 11. Tan YY, Ogilvie JB, Triponez F, et al. Selective use of adrenal venous sampling in the lateralization of aldosterone‐producing adenomas. World J Surg. 2006;30:879–885. [DOI] [PubMed] [Google Scholar]
- 12. Harvey A, Kline G, Pasieka JL. Adrenal venous sampling in primary hyperaldosteronism: comparison of radiographic with biochemical success and the clinical decision‐making with “less than ideal” testing. Surgery. 2006;140:847–855. [DOI] [PubMed] [Google Scholar]
- 13. Carr CE, Cope C, Cohen DL, et al. Comparison of sequential versus simultaneous methods of adrenal venous sampling. J Vasc Interv Radiol. 2004;15:1245–1250. [DOI] [PubMed] [Google Scholar]
- 14. Zarnegar R, Bloom AI, Lee J, et al. Is adrenal venous sampling necessary in all patients with hyperaldosteronism before adrenalectomy? J Vasc Interv Radiol. 2008;19:66–71. [DOI] [PubMed] [Google Scholar]
- 15. Gallay BJ, Ahmad S, Xu L, et al. Screening for primary aldosteronism without discontinuing hypertensive medications: plasma aldosterone‐renin ratio. Am J Kidney Dis. 2001;37:699–705. [DOI] [PubMed] [Google Scholar]
- 16. Nishizaka MK, Pratt‐Ubunama M, Zaman MA, et al. Validity of plasma aldosterone‐to‐renin activity in African American and white subjects with resistant hypertension. Am J Hypertens. 2005;18:805–812. [DOI] [PubMed] [Google Scholar]
- 17. Schwartz GL, Turner ST. Screening for primary aldosteronism in essential hypertension: diagnostic accuracy of the ratio of plasma aldosterone concentration to plasma renin activity. Clin Chem. 2005;51:386–394. [DOI] [PubMed] [Google Scholar]
- 18. Funder JW, Carey RM, Fardella C, et al. Case detection, diagnosis and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2008;93:3266–3281. [DOI] [PubMed] [Google Scholar]
- 19. Rossi GP, Ganzalori C, Miotto D, et al. Dynamic testing with adrenocorticotropic hormone does not improve lateralization of aldosterone oversecretion in primary aldosteronism patients. J Hypertens. 2006;24:371–379. [DOI] [PubMed] [Google Scholar]
- 20. Rossi GP, Pitter G, Bernante P, et al. Adrenal vein sampling for primary aldosteronism: assessment of selectivity and lateralization of aldosterone excess baseline and after adrenocorticotropic hormone (ACTH) stimulation. J Hypertens. 2008;26:989–997. [DOI] [PubMed] [Google Scholar]
- 21. Sawka AM, Young WF, Thompson GB, et al. Primary aldosteronism: factors associated with normalization of blood pressure after surgery. Ann Intern Med. 2001;135:258–261. [DOI] [PubMed] [Google Scholar]
- 22. Horita Y, Inenaga T, Nakahama H, et al. Cause of residual hypertension after adrenalectomy in patients with primary aldosteronism. Am J Kidney Dis. 2001;37:884–889. [DOI] [PubMed] [Google Scholar]
- 23. Sywak M, Pasieka JL. Long‐term follow‐up and cost benefit of adrenalectomy in patients with primary hyperaldosteronism. Br J Surg. 2002;89:1587–1593. [DOI] [PubMed] [Google Scholar]
- 24. Fukudome Y, Fujii K, Arima H, et al. Discriminating factors for recurrent hypertension in patients with primary aldosteronism after adrenalectomy. Hypertens Res. 2002;25:11–18. [DOI] [PubMed] [Google Scholar]
- 25. Meyer A, Brabant G, Behrend M. Long‐term follow‐up after adrenalectomy for primary aldosteronism. World J Surg. 2005;29:155–159. [DOI] [PubMed] [Google Scholar]
- 26. Tsujihata M, Nonomura N, Tsujimura A, et al. Laparoscopic adrenalectomy for primary hyperaldosteronism: clinical experience with 60 cases. J Endocrinol. 2006;20:262–265. [DOI] [PubMed] [Google Scholar]
- 27. Rossi GP, Belfiore A, Bernini G, et al. Comparison of the captoril and saline infusion test for excluding aldosterone‐producing adenoma. Hypertension. 2007;50:424–431. [DOI] [PubMed] [Google Scholar]
- 28. Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure research. Hypertension. 2008;51:1403–1419. [DOI] [PubMed] [Google Scholar]


