Abstract
J Clin Hypertens (Greenwich).
The Efectividad de un Programa de Intervención en el Control de la Presión Arterial de los Hipertensos en Riesgo de Desarrollar Insuficiencia Cardiaca (HEROIC) study was designed to assess whether an educational program for primary care physicians could improve blood pressure (BP) control in hypertensive patients at high risk for developing heart failure. The program contained a combination of educational training (live group sessions or online training) and information feedback. Two hundred twenty‐six physicians completed the program and provided valid data in 2489 patients before and 2168 after 1 year. There was a small but significant reduction of −1.1 mm Hg (P=.009) in systolic BP and a higher proportion of patients achieved their BP target (13.6% vs 15.6%, P=.055). Thus, the authors concluded that there was a slight improvement in BP control after the educational program, but this change was not sufficient to avoid development of heart failure. More complex and intensive programs are needed for this type of prevention.
High blood pressure (BP) is an important public health care problem. Evidence from randomized trials has shown that effective drug treatment reduces the risk of cardiovascular (CV) morbidity and mortality. However, there is ongoing concern that the benefits demonstrated by antihypertensive drugs in randomized trials are not usually implemented in everyday clinical practice. 1 Although BP control has progressively improved in the last years in Spain, only around 40% of hypertensive patients followed in primary care clinics (PC) are controlled. 2 , 3 , 4 , 5 , 6
Among the hypertension‐induced diseases, heart failure (HF) is a growing health problem worldwide. 7 , 8 Patients with HF face significant impairment in functional status, multiple hospital admissions, high mortality, multiple physical and psychological symptoms, and a diminished quality of life. 9 , 10 , 11 Although recent advances in therapy for HF have improved functional capacity and survival, control of risk factors, mainly high BP, 12 , 13 , 14 is crucial to halt HF development.
A recent observational study (Hipertensión e Insuficienca Cardiaca en Atención Primaria [HICAP] study) 15 with 6375 hypertensive patients attending PC showed that among patients not previously diagnosed with HF, 59.1% had a high risk of developing it. BP control, as well as the control of other CV risk factors, mainly diabetes mellitus and low‐density lipoprotein cholesterol, was clearly insufficient in these patients at risk for HF as compared with the remaining subjects.
How to improve the control rates of hypertension is a matter of debate. Educational programs directed at patients, at health professionals, or both; patient’s self‐monitoring; audits; health professional–led care; or appointment reminder systems have been evaluated. Their success has been variable, and it seems that only simultaneous multiple interventions could be useful to improve BP control. 16 , 17
The Efectividad de un Programa de Intervención en el Control de la Presión Arterial de los Hipertensos en Riesgo de Desarrollar Insuficiencia Cardiaca (HEROIC) study was designed to evaluate the effectiveness of an educational combined program addressed to PC physicians in order to improve BP control in their patients. The efficacy of the live vs the online training program is also evaluated.
Material and Methods
HEROIC was a prospective program of 10 months’ duration to evaluate the impact of an educational intervention on BP control in PC physicians. Four hundred PC physicians distributed throughout Spain were invited to participate. The study was approved by an independent Clinical Research Ethics Committee, and written informed consent was obtained from all of the recruited patients.
Study Population
Each of the PC physicians who entered the study collected information about their patients who fulfilled the criteria of having an established diagnosis of essential hypertension (systolic BP ≥140 mm Hg or diastolic BP ≥90 mm Hg, ≥130/80 mm Hg in diabetic patients, or patients under antihypertensive therapy), being followed for more than 1 year in primary health care centers, with a BP control visit in the last 6 months, and with a high risk profile for developing HF. The high risk profile for developing HF (stage A–B in the American College of Cardiology, American Heart Association [ACC‐AHA] HF guidelines 18 ) was defined as age ≥50 years plus another risk factor (diabetes, cardiomegaly on chest X‐ray, left ventricular hypertrophy in electrocardiogram, or previous coronary artery disease) or as age ≥70 years. 15
Patients were excluded if they had a previous diagnosis of HF or refused to participate in the study.
Physicians were asked to collect the required data during a single visit. Patient’s demographic and clinical characteristics were obtained by patient interview and medical record review. A specific case report form (CRF) was used to collect demographic (age and sex) and anthropometric data (weight, height, and waist circumference), associated CV risk factors, target organ damage, previous CV disease history, and current medications. Data from the last available laboratory test were also recorded (fasting glucose, creatinine, total cholesterol, high‐density lipoprotein cholesterol, low‐density lipoprotein cholesterol, triglycerides, and hemoglobin A1c (HbA1c) in diabetic patients).
BP was measured during the visit day on two separate occasions, in a seated position with calibrated mercury or automatic devices, after 5 minute rest. The average of the two measurements was recorded. BP was graded according to the European Society of Hypertension–European Society of Cardiology (ESH/ESC) 2003 guidelines. 19 Physicians were requested to indicate the BP they considered as the target for each patient. With the data provided by the investigators, a central assessment of risk stratification and BP target according to the ESH/ESC 2003 guidelines 19 was performed in each patient, and they were compared with that established by the physician.
BP was assumed to be well controlled according the ESH/ESC 2003 guidelines 19 if BP was <140/90mm Hg in patients with low or moderate CV risk, and when it was <130/80 mm Hg in high or very high CV risk patients. Data of BP control rates considering <140/90 mm Hg as the BP target in all patients, and control rates in diabetics patients (<130/80 mm Hg) were also determined.
The study was undertaken in 3 stages.
Stage I: Initial assessment of hypertension control rates in 10 consecutive hypertensive outpatients who attended the clinic of the selected physicians and fulfilled the inclusion criteria within 1 month (February, 2007).
Stage II: Intervention program. The intervention consisted of an 8 month‐long combined program that comprised an educational training and feedback of information.
Educational training was designed to increase physician awareness about the main clinical guidelines recommendations for the control and treatment of high BP. Specifically designed material was used during the training.
The educational training material was prepared by the scientific committee of the study consisting of 3 national experts in the CV field (a cardiologist, a hypertension specialist, and a primary care physician) with consultation with the 16 local experts responsible for the live group sessions. The material, slides kits, were provided to the trainers and were printed at the disposal of the physicians after the initial training.
This training could be realized by:
-
•
Live group sessions: during 2 months physicians could participate in one of the 16 one‐day sessions performed across Spain. Each of these trainings were directed by two trained local experts (a cardiologist and a primary care specialist).
-
•
Online training: during 2 months the same training material used in the live group sessions was available on the study Web page, with exclusive access for physicians participating in the study. Physicians who chose this educational training form had to complete an online evaluation test; only those who passed it could continue taking part in the study.
During the following 6 months all physicians received feedback of the results from the first cross‐sectional survey by a monthly message on their mobile phones. Physicians could also look up data from the initial results on the study Web page.
Stage III: Final assessment. Physicians that took part in the interventional program again collected data from 10 consecutive hypertensive patients who attended the clinic and fulfilled the same inclusion criteria as at Stage I (November 15 to December 15, 2007).
Statistical Analysis
The data management was performed in the MediClin Biometric Department; data were recorded into an Access 2002 database (Microsoft Corporation, Redmond, WA), with edit checks that guarantee an accurate recording of the data.
Statistical results were obtained by means of the statistical software SAS version 8.02 (SAS Institute Inc, Cary, NC) for Windows. For categorical variables, absolute frequencies and percentages were obtained; for continuous variables, mean ± standard deviation, median, percentiles 25th to 75th, and range were obtained. Confidence intervals at 95% level were also calculated.
A comparative analysis to establish differences between phase I and phase II was performed. Significance related to categorical variables was obtained through the chi‐squared test or the Fisher exact test. Significance related to phase and continuous variables was obtained through the Student’s t‐test or analysis of variance.
The degree of agreement between physician’s estimation and central assessment of CV was sought using Kappa index.
Results
A total of 375 physicians agreed to participate in the study, of whom 35 discontinued their participation and did not return the study CRFs. The Figure shows the flow of physicians and patients during the HEROIC study. Only physicians that completed the intervention program could collect data again during the 2º survey. As 266 physicians completed the intervention program, the expected number of patients in this second part of the study was 2660 patients. The number of patients included in the second survey was 2271 (87.3% of expected), with 2168 (83.3%) being suitable for the analysis. The final analyses were done only with data included by the 266 physicians that completed the intervention program: 2489 (96.7% of expected) valid data in the 1º survey and 2168 in the 2º survey (83.3% of expected).
Figure.
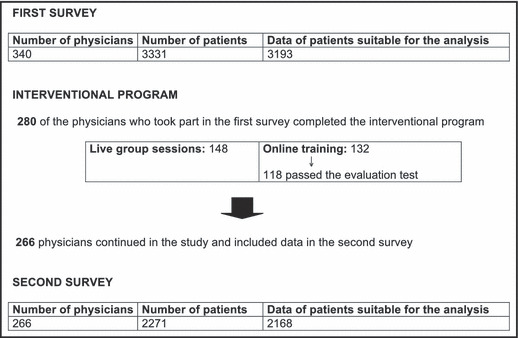
Flow of physicians and patients in the HEROIC study. See text for expansions of trial names.
The general characteristics of the study population are shown in Table I. In general, no significant differences were observed between the two surveys’ assessments. Mean age was about 69 years old, approximately 50% were males and most of them, nearly 80%, belong to high–very high CV risk groups in both surveys. Only a higher prevalence of left ventricular hypertrophy and ischemic heart disease in patients included in the second survey were observed, Table II.
Table I.
Characteristics of Patients Included in the Two Cross‐Sectional Surveys (Before and After the Intervention Program)
| 1º Survey Before Intervention | 2º Survey After Intervention | P Value | |
|---|---|---|---|
| Number of patients | 2489 | 2168 | |
| Age (mean, (95% CI) | 69 (68.7–69.4) | 69.3 (68.9–69.7) | .29 |
| Sex (% male) (%, 95% CI) | 50.5 (48.6–52.5) | 51.5 (49.4–53.6) | .52 |
| BMI (mean, 95% CI) | 29.5 (29.3–29.7) | 29.3 (29.1–29.5) | .18 |
| Waist circumference (mean, 95% CI) | 99.6 (99–100.2) | 100 (93.3–100.6) | .41 |
| CV risk factorsa (mean, 95% CI) | 3.8 (3.7–3.8) | 3.7 (3.7–3.8) | .14 |
| Age (men >55 years; women >65 years) (%, 95% CI) | 80.0 (78.4–81.6) | 80.2 (78.5–81.9) | .85 |
| Dyslipidemia (%, 95% CI) | 75.8 (74.1–77.5) | 75.11 (73.3–77.0) | .61 |
| Abdominal obesity (%, 95% CI) | 63.4 (61.3–65.4) | 64.0 (61.7–66.2) | .69 |
| Diabetes mellitus (%, 95% CI) | 45.3 (43.4–47.3) | 44.4 (42.3–46.5) | .51 |
| Smoking (%, 95% CI) | 13.3 (11.9–14.7) | 13.1 (11.6–14.6) | .32 |
| Family history of premature CV disease (%, 95% CI) | 11.1 (9.86–12.3) | 9.9 (8.62–11.1) | .17 |
| Subclinical organ damagea (%, 95% CI) | 41.9 (39.9–43.8) | 38.8 (36.7–40.9) | .03 |
| Microalbuminuria | 28.4 (25.7–31.0) | 29.5 (26.5–32.4) | .57 |
| Left ventricular hypertrophy | 31.4 (29.5–33.3) | 27.67 (25.7–29.6) | .007 |
| Slight increase in plasma creatinine | 7.63 (6.5–8.7) | 6.71 (5.6–7.8) | .24 |
| Establish CV or renal disease (%, 95% CI) | 36.4 (34.4–38.4) | 35.0 (32.8–37.1) | .33 |
| Ischemic cardiopathy | 18.3 (16.6–19.9) | 16.3 (14.6–17.9) | .09 |
| Peripheral artery disease | 8.9 (7.7–10.0) | 8.5 (7.3–9.7) | .68 |
| Cerebrovascular disease | 7.4 (6.3–8.5) | 7.1 (5.9–8.2) | .63 |
| Renal diseasea | 6.1 (5.1–7.1) | 6.7 (5.6–7.8) | .45 |
| Advanced retinopathy | 2.2 (1.6–2.8) | 2.0 (1.4–2.6) | .60 |
Abbreviations: BMI, body mass index; CI, confidence interval; CV, cardiovascular.
aAccording to the European Society of Hypertension–European Society of Cardiology 2003 guidelines.19 Dyslipidemia: total cholesterol >250 mg/dL, or low‐density lipoprotein cholesterol >155 mg/dL, or high‐density lipoprotein cholesterol <40 mg/dL in men and <48 mg/dL in women. Abdominal obesity: abdominal circumference (men ≥102 cm; women ≥88 cm). Family history of premature CV disease (at <55 years in men, <65 years in women). Left ventricular hypertrophy: electrocardiogram: Sokolow‐Lyons >38 mm; Cornell >2440 mm/ms; echocardiogram: left ventricular mass index (men ≥125 g/m2; women ≥110 g/m2). Microalbuminuria: 30–300 mg/24 h; albumin‐creatinine ratio (men ≥22 mg/g; women ≥31 mg/g). Slight elevation of serum creatinine concentration: men 1.3–1.5 mg/dL; women 1.2–1.4 mg/dL). Renal disease: proteinuria (>300 mg/24 h); or serum creatinine (men >1.5 mg/dL; women >1.4 mg/dL).
Table II.
Physician’s and Central Assessment of CVR According to the European Society of Hypertension–European Society of Cardiology 2003 Guidelines19
| Physician’s Estimations | Central Assessment | |
|---|---|---|
| 1º Survey before intervention (%, 95% CI) | ||
| Low CVR | 8.0 (6.85–9.08) | 5.0 (4.13–5.85) |
| Moderate CVR | 33.3 (31.4–35.2) | 14.5 (13.1–15.9) |
| High CVR | 42.5 (40.5–44.6) | 51.8 (49.9–53.8) |
| Very high CVR | 16.2 (14.7–17.7) | 28.7 (26.9–30.5) |
| 2º Survey after intervention (%, 95% CI) | ||
| Low CVR | 7.3 (6.15–8.44) | 6.2 (5.14–7.17) |
| Moderate CVR | 32.3 (30.3–34.4) | 14.5 (13.0–16.0) |
| High CVR | 45.7 (43.5–47.9) | 51.9 (49.8–54.0) |
| Very high CVR | 14.7 (13.1–16.2) | 27.5 (25.6–29.4) |
Abbreviations: CI, confidence interval; CVR, cardiovascular risk.
Physician’s Assessment of CV Risk
Central CV risk assessment and physician’s estimations of CV risk are presented in Table II. Physicians correctly classified 47.9% of the patients at the beginning and 45.6% at the end. There was a weak agreement between physicians’ estimations and central assessment of CV risk both at the beginning and at the end (Kappa index 0.3173 [95% confidence interval {CI}, 0.2896–0.3449] P< .0001 and 0.2715 [95% CI, 0.2412–0.3017], P< .0001, respectively).
BP Control
Table III summarizes BP data in both surveys. Mean systolic BP and pulse pressure were significantly lower in patients included after the intervention, and a lower proportion of patients in the second survey had grade 2–3 hypertension and isolated systolic hypertension. Likewise, there were also a higher proportion of patients that reached the BP target in the survey after intervention. The difference was close to achieving statistical significance when BP target was considered according to the CV added risk (13.6% in the survey before the intervention vs 15.6% in the survey after the intervention; P=.055).
Table III.
BP Findings in the Two Cross‐Sectional Surveys (Before and After the Intervention Program)
| 1º Survey Before Intervention | 2º Survey After Intervention | P Value | |
|---|---|---|---|
| Systolic BP (mean, 95% CI) | 144.4 (143.8–145.0) | 143.3 (142.7–143.9) | .009 |
| Diastolic BP (mean, 95% CI) | 83.3 (82.9–83.7) | 83.5 (83.1–83.9) | .50 |
| Pulse pressure (mean, 95% CI) | 61.1 (60.6–61.7) | 59.8 (59.2–60.3) | .0004 |
| Classification of BPa (%, 95% CI) | |||
| Optimal | 2.6 (2.0–3.2) | 2.7 (2.0–3.4) | .0348 |
| Normal | 9.5 (8.3–10.6) | 10.5 (9.2–11.8) | |
| High normal | 22.7 (21.0–24.3) | 23.4 (21.6–25.2) | |
| Grade 1 hypertension | 17.9 (16.4–19.4) | 21.0 (19.3–22.7) | |
| Grade 2 hypertension | 11.4 (10.1–12.6) | 10.1 (8.9–11.4) | |
| Grade 3 hypertension | 1.5 (1.0–2.0) | 1.3 (0.9–1.8) | |
| Isolated systolic hypertension | 34.4 (32.6–36.3) | 30.9 (28.9–32.8) | |
| BP control (%, 95% CI) | |||
| BP <140/90 mm Hg in all patients | 34.6 (32.7–36.5) | 36.5 (34.5–38.5) | .18 |
| Low CV risk | 94.3 (90.2–98.4) | 94.7 (90.9–98.5) | |
| Moderate CV risk | 37.7 (32.7–42.8) | 39.9 (33.9–44.8) | |
| High CV risk | 32.0 (29.5–34.6) | 34.0 (31.2–36.8) | |
| Very high | 27.3 (24.0–30.6) | 26.6 (23.0–30.1) | |
| According CV risk [low‐moderate risk <140/90 mm Hg; high‐very high risk <130/80 mm Hg] | 13.6 (12.3–15.0) | 15.6 (14.1–17.2) | .055 |
| Low CV risk | 94.3 (90.2–98.4) | 94.7 (90.9–98.5) | |
| Moderate CV risk | 37.7 (32.7–42.8) | 39.3 (33.9–44.8) | |
| High CV risk | 6.7 (5.4–8.1) | 7.9 (6.3–9.5) | |
| Very high | 0 | 0 | |
| BP findings in diabetics patients (%, 95% CI) | |||
| Systolic BP (mean, 95% CI) | 144.3 (143.4–145.2) | 142.7 (141.8–143.7) | .01 |
| Diastolic BP (mean, 95% CI) | 82.8 (82.2–83.3) | 82.9 (82.3–83.6) | .66 |
| Pulse pressure (mean, 95% CI) | 61.5 (60.7–62.3) | 59.8 (58.9–60.6) | .003 |
| BP <140/90 mm Hg | 35.8 (33.0–38.7) | 39.1 (36.0–42.2) | .12 |
| BP <130/80 mm Hg | 7.5 (6.00–9.10) | 10.6 (8.63–12.5) | .01 |
Abbreviations: BP, blood pressure; CI, confidence interval; CV, cardiovascular.
aAccording to the European Society of Hypertension–European Society of Cardiology 2003 guidelines.19
When analyzing whether there were differences in BP findings between physicians that chose live group sessions and online training as an educational training form, the data indicate that similar results were observed in both forms of educational training (Table IV).
Table IV.
BP Findings in the Two Cross‐Sectional Surveys (Before and After the Intervention Program) According to the Educational Training Realized by the Physicians
| 1º Survey Before Intervention | 2º Survey After Intervention | P Value | |
|---|---|---|---|
| BP control <140/90 mm Hg (%, 95% CI) | |||
| Online | 31.9 (29.1–34.7) | 34.0 (31.0–37.1) | .31 |
| Live sessions | 36.8 (34.2–39.3) | 38.4 (35.6–41.1) | .39 |
| According CV risk [low‐moderate risk <140/90 mm Hg; high‐very high risk <130/80 mm Hg] (%, 95% CI) | |||
| Online | 12.8 (10.8–14.8) | 15.1 (12.8–17.4) | .13 |
| Live sessions | 14.3 (12.5–16.2) | 16.1 (14.0–18.1) | .21 |
| BP <130/80 mm Hg in patients with diabetes mellitus (%, 95% CI) | |||
| Online | 6.3 (4.0–8.7) | 9.2 (6.3–12.1) | .12 |
| Live sessions | 8.3 (6.2–10.3) | 11.5 (8.9–14.2) | .053 |
Abbreviations: BP, blood pressure; CI, confidence interval; CV, cardiovascular.
The proportion of patients in whom the BP target established by the physician was concordant with that proposed by the ESH/ESC 2003 19 was higher in the survey realized after the intervention (18.6% in the survey before the intervention vs 22.1% after it; P=.003).
The mean number of antihypertensive drugs was 1.8 at the beginning, 40.0% of the patients on monotherapy, 40.3% on 2 drugs, 17.1% on 3 drugs, and the remainder on 4 or more drugs, Table V. At the end, more patients were treated with a higher number of drugs as compared to the beginning and also a higher proportion of patients were treated with combinations (60.0%, 2 or more drugs in the survey before the intervention vs 62.7% in the second survey; P=.02). Drug treatment is summarized in Table V. No differences in the kind of antihypertensive drugs used were observed.
Table V.
Treatment of Patients Included in the Two Cross‐Sectional Surveys (Before and After the Intervention Program)
| 1º Survey Before Intervention | 2º Survey After Intervention | P Value | |
|---|---|---|---|
| Antihypertensive medication (%, 95% CI) | |||
| % Patients with pharmacological treatment | 98.6 (98.2–99.1) | 99.3 (98.9–99.6) | .11 |
| Number of drugs (mean, 95% CI) | 1.8 (1.8–1.9) | 1.9 (1.8–1.9) | .13 |
| 1 Drug | 40.0 (38.1–41.9) | 37.3 (35.2–39.3) | .02 |
| 2 Drugs | 40.3 (38.3–42.2) | 43.3 (41.2–45.4) | |
| 3 Drugs | 17.1 (15.6–18.6) | 15.8 (14.3–17.3) | |
| ≥4 Drugs | 2.6 (2.0–3.2) | 3.6 (2.8–4.4) | |
| Diuretics | 48.6 (46.7–50.6) | 48.5 (46.4–50.6) | .95 |
| Thiazide | 35.5 (33.6–37.4) | 36.0 (34.0–38.0) | .69 |
| Loop | 10.6 (9.4–11.8) | 9.0 (7.8–10.2) | .08 |
| Spironolactone | 1.0 (0.6–1.3) | 1.2 (0.7–1.7) | .43 |
| β‐blockers | 14.6 (13.2–16.0) | 14.4 (13.0–15.9) | .88 |
| ACEI | 32.0 (30.1–33.8) | 30.8 (28.9–32.8) | .39 |
| ARB | 56.2 (54.2–58.1) | 61.0 (59.0–63.1) | .0008 |
| Calcium antagonists | 21.9 (20.3–23.5) | 24.1 (22.3–25.9) | .07 |
| Others | 6.9 (5.8–7.7) | 6.0 (4.9–6.8) | |
| Lipid lowering drugs (%, 95% CI) | |||
| % Patients with pharmacological treatment | 59.9 (57.9–61.8) | 59.9 (57.9–62.0) | .51 |
| Statins | 57.1 (55.1–59.0) | 56.7 (54.6–58.8) | .80 |
| Resin/ezetimibe | 3.2 (2.5–3.9) | 4.0 (3.2–4.8) | .14 |
| Fibrates | 2.8 (2.2–3.5) | 2.3 (1.6–2.9) | .20 |
| Diabetes treatment (%, 95% CI) | |||
| % Patients with pharmacological treatment | 86.8 (84.8–88.8) | 88.25 (86.2–90.3) | .58 |
| Oral antidiabetics | 67.0 (64.3–69.8) | 70.2 (67.3–73.1) | .30 |
| 1 Drug | 69.0 (65.7–72.3) | 74.4 (71.1–77.7) | |
| 2 Drugs | 31.0 (27.7–34.3) | 25.6 (22.3–28.9) | |
| Insulin | 9.8 (64.3–69.8) | 8.0 (6.29–9.72) | |
| Oral antidiabetics + insulin | 9.9 (8.18–11.7) | 10.1 (8.18–12.0) | |
| Other treatments (%, 95% CI) | |||
| Antiplatelet therapy | 43.2 (41.2–45.1) | 42.9 (40.8–45.0) | .84 |
Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; ARB, angiotensin receptor blocker; CI, confidence interval.
Findings in Patients With Diabetes Mellitus
A high number of patients were diabetics (approximately 45%), Table I. Among them, there was a statistically significantly higher proportion of diabetic patients that reached the BP target at the end (BP <130/80 mm Hg: 7.5% in the survey before the intervention vs 10.6% in the survey after the intervention; P=.01), Table III.
This group of diabetics was on a higher number of antihypertensive drugs and had a higher proportion of patients with 2 or more drugs as compared with the nondiabetic patients. No increment on drug consumption, however, was observed at the end of the study. Mean number (95% CI): 1.9 (1.9–2.0) in the first survey and 2.0 (1.9–2) in the second survey; P=.32. More than half (64.4%) were on 2 or more drugs in the first survey vs 65.8% in the second survey; P=.5.
Mean HbA1c was 7.0 (95% CI, 6.9–7.1) in patients included in both surveys. The proportion of patients with HbA1c <6.5% 20 were low and similar in both surveys (31.4% in the survey before the intervention vs 30.5% in the survey after the intervention; P=.66). The proportion of well controlled patients was higher in both surveys when HbA1c as <7% 21 was considered as control (49.6% before the intervention vs 48.8% after it; P=.73), Table IV.
Dyslipidemia Findings
Dyslipidemia was also very prevalent (≈75%) (Table I) and the control rates, according to the National Cholesterol Education Program Adult Treatment Panel III (NCEP‐ATP III) guidelines, 22 were low in both surveys (22.6% and 24.2%; P=.21). Statins were the most prescribed agents and no significant differences were seen in lipid‐lowering therapy between both surveys (Table V). Dyslipidemia control was lower in diabetic patients (19.9% in the survey before the intervention and 19.5% after the survey; P=.79).
Discussion
The present data from the HEROIC study show that most hypertensive patients at high risk for developing HF (near 80%) present a high or very high CV risk according to the ESH‐ESC 2003 19 and that PC physicians frequently make an incorrect risk stratification of these patients. In both surveys less than half of patients were correctly classified by their physicians and central assessment of CV risk showed higher percentages of patients with high or very high CV risk suggesting that physicians frequently underestimate the risk of their patients.
This problem has previously been shown in other studies in hypertensive patients followed in PC, where central assessment revealed that between 60.3% 23 and 64.5% 6 of the patients had a high or very high risk, but physicians estimated that only between 39.3% 6 and 40.5% 23 were at elevated CV risk.
The main reason for the differences detected between physicians and central assessment when comparing the risk stratification could most likely be due to the lack of recognition of the risk by the physicians. Despite a risk stratification table being provided in each CRF of HEROIC study and this issue being widely discussed during the educational training, the lack of recognition of the risk by the physicians seemed not to improve with the proposed intervention.
In the first survey, BP was well controlled (<140/90 mm Hg) in 34.6% of patients, but this percentage decreased to 13.6% when BP control was considered according to the CV risk (BP <130/80 mm Hg in patients with high or very high risk—near 80% of the HEROIC study patients). These figures are similar to previous data in PC in Spain, where although BP control has progressively improved in the last few years, present control rates are around 40% in the hypertensive general population, 2 , 3 , 4 , 5 , 6 and decreasing in patients with high or very high CV risk. 6 An incorrect estimation of the CV risk based on the physician’s perception may have significant implications in the clinical management of hypertensive patients and explain, at least in part, these low rates of BP control. If a patient is considered as being at moderate risk when the patient is actually at high risk, the BP target will be <140/90 mm Hg instead of <130/80 mm Hg as it should be.
A possible explanation for the underestimation of the CV risk of patients could be related to the fact that current guidelines are complex and recommend the evaluation of CV risk using diagnostic tests that are not always available in the PC. Because of this, risk stratification at this health care level is generally conducted by only evaluating the classic CV risk factors. However, several studies have indicated that the evaluation of CV risk is strongly influenced by the use of diagnostic tests aimed at detecting the presence of target organ lesion. 24 , 25 , 26 , 27 Although some of these tests are available for most PC physicians (eg, microalbuminuria evaluation), data from our study indicate that physicians do not use them in their routine evaluation of the CV risk (microalbuminuria data were only available in 45% of patients included in the first survey and 42% in the second). A CV risk stratification adapted to the diagnostic tests available in the PC could be useful to help physicians to add these diagnostic tests to the routine of their clinical practice and improve the estimation of patients’ risk. The better evaluation of risk will also help to provide a better determination of CV risk factors’ control targets and to discover the need to use specific drugs in each patient individually.
The HEROIC intervention has had a limited impact to improve BP. Mean systolic BP had a small but significant decrease of −1.1 mm Hg (−2.0, −0.3) and a higher proportion of patients achieved the BP target, specially when BP target was considered according to the CV added risk (13.6% vs 15.6%) and in the diabetic patients. These results could be explained because the proportion of patients in whom BP target established by the physician was coinciding with that proposed by the ESH/ESC guidelines 19 according their CV risk was higher after the intervention (18.6% vs 22.1%) and because the treatment seems to be more intensive after the intervention with a higher number of drugs and combinations (60.0% of patients with ≥2 drugs before the intervention vs 62.7% after the intervention).
The effect of this intervention is similar to previous experience based on educational activities. Recently, The Cochrane Collaboration 16 reviewed interventions used to improve control BP in hypertensive patients that were taking BP lowering medication in an ambulatory setting to determine their effectiveness. The interventions evaluated were: self‐monitoring; educational interventions directed at patients; educational interventions directed at the health professional; health professional (nurse and pharmacist)–led care; organizational interventions aimed to improve the care delivery; appointment reminder systems. The review concluded that an organized system of registration, recall, and regular review allied to a vigorous stepped care approach to antihypertensive treatment appears the most likely way to improve the high BP control. Randomized controlled trials (RCT) of educational interventions directed at patients or health professionals were heterogeneous but do not appear to be associated with a large net reduction in BP by themselves. Specifically, educational interventions directed towards the physicians (9 RCT) showed similar results to the HEROIC intervention (Table VI) since they were associated with a small reduction in systolic BP, pooled mean difference in systolic BP was −2.0 mm Hg, without a significant decrease in mean diastolic BP, whilst control of BP produced heterogeneous results (reported range 0.8–1.0).
Table VI.
Comparison of the Effect on Blood Pressure of the HEROIC Study Intervention and Educational Interventions Directed Toward the Physicians Reviewed by The Cochrane Collaboration16
| ΔSBP | ΔDBP | |
|---|---|---|
| Physician education (The Cochrane Review—9 RCT)16 | −2.03 [−3.45 to −0.62] | −0.43 [−1.12 to 0.27] |
| HEROIC | −1.1 [−2.0 to −0.3] | 0.2 [−0.4 to −0.8] |
Abbreviations: Δ, change; DBP, diastolic blood pressure, RCT, randomized controlled trials; SBP, systolic blood pressure. See text for expansions of trial names.
A small Spanish study 17 carried out in PC (one primary care health center as intervention group and another one as control group) a few years ago showed that a quality improvement intervention, designed for the medical and nursing staff, consisting of a combined program comprising audit, feedback, and training sessions about main hypertension clinical guidelines, resulted in a drop of 9.72 mm Hg in systolic BP and 3.84 mm Hg in diastolic BP, and an increased percentage of hypertensive patients with BP <140/90 mm Hg (from 37.5% to 68.8% in the intervention group without changes in control group).
Although the design of HEROIC and the Gómez‐Marcos et al. 17 study was similar (two cross‐sectional surveys, one before and the other after an interventional program), some important differences in the intervention proposed in these studies could explain, at least in part, the differences in BP results, and could show some of the limitations of the intervention proposed in HEROIC. While in HEROIC there was only one training session during 6 months, in the Gómez‐Marcos et al. 17 study there were 6 training sessions about main hypertension clinical guidelines plus another live session where a feedback and audit of the results of the first survey was done in order to improve the quality of assistance to hypertensive patients. In HEROIC, although all physicians received information about the main results on the 1º survey, these results were only suitable after the educational trainings were done and it was not possible to discuss how to implement specific activities to improve the current situation. In addition, the intervention in HEROIC was directed only at physicians, while in the other study, other health professionals in charge of hypertensive patients, such as nurses, were also involved. The inclusion of a control group in HEROIC as in the Gómez‐Marcos et al. 17 study could have also been useful to try to evaluate if the small differences between the surveys could be explained by other factors, including chance.
Concerning other CV risk factors’ control, results from HEROIC were similar to other studies 6 , 23 and indicate the low control rate of dyslipidemia and diabetes in hypertensive patients. The previously mentioned underestimation of the CV risk of these patients could be also associated with this fact. The intervention proposed in HEROIC was not associated with changes in the management and control of other CV risk factors.
In the HEROIC study, education training could be realized by live group sessions (selected by 55.6% of physicians) or online training (44.4% of physicians). There were no significant differences between the results observed in physicians that performed the live group sessions and those who chose online training as an educational training form.
The limitations of the intervention proposed in the HEROIC study have been previously commented upon. Although the cross‐sectional design of the study also has limitations, the fact that the HEROIC study aimed to evaluate the effectiveness of the proposed intervention under usual clinical practice conditions and that this was done in a wide sample of unselected and consecutively recruited patients collected by a large number of physicians throughout Spain, suggests that the results presumably reflect how an educational intervention could influence the clinical practice of physicians.
In summary, the results of the study suggest that after the intervention program proposed in this study a higher number of physicians establish as a BP target the values that guidelines recommend, and consequently the number of drugs used to treat hypertension was higher and a slight improvement in BP control was observed in the survey after the intervention. However, the proposed intervention has limitations that suggest that an intervention based mainly on an educational training is not enough to produce large reductions in BP. A more complex intervention combining several interventions (educational programs, audits, self‐monitoring, health professional–led care, appointment reminder systems, and so on) and involving not only physicians, but nurses and patients as well, could be the best way to improve BP control.
Acknowledgements: The authors acknowledge Eduardo Sobreviela of MediClin, Madrid, Spain, for his work on the statistical part of the study. The authors are grateful to all the primary care physicians who participated in this study providing the information requested. This study was sponsored by AstraZeneca Farmacéutica Spain, with the scientific support of the Spanish Society of Hypertension (SEH‐LELHA).
Disclosure: Beatriz De Rivas works as medical adviser in the cardiovascular medical department of AstraZeneca Farmacéutica Spain.
References
- 1. Burnier M. Blood pressure control and implementation of guidelines in clinical practice: can we fill the gap? J Hypertens. 2002;20:1251–1253. [DOI] [PubMed] [Google Scholar]
- 2. Barrios V, Escobar C, Calderón A, et al. Blood pressure and lipid goal attainment in the hypertensive population in the primary care setting in Spain. J Clin Hypertens (Greenwich). 2007;9:324–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Barrios V, Banegas JR, Ruilope LM, et al. Evolution of blood pressure control in Spain. J Hypertens. 2007;25:1975–1977. [DOI] [PubMed] [Google Scholar]
- 4. Llisterri Caro JL, Rodríguez Roca GC, Alonso Moreno JF, et al. Blood pressure control in Spanish hypertensive patients in primary health care centres. PRESCAP 2002 study. Med Clin (Barc). 2004;122:165–171. [DOI] [PubMed] [Google Scholar]
- 5. Llisterri Caro JL, Rodríguez Roca GC, Alonso Moreno JF, et al. Control of blood pressure in Spanish hypertensive population attended in primary health‐care. PRESCAP 2006 study. Med Clin (Barc). 2008;130:681–687. [DOI] [PubMed] [Google Scholar]
- 6. Márquez‐Contreras E, De Rivas Otero B, Divisón Garrote JA, et al. Are hypertensive patients managed in primary care well evaluated and controlled? HICAP Study [in Spanish] An Med Interna. 2007;24:312–316. [DOI] [PubMed] [Google Scholar]
- 7. Stewart S, MacIntyre K, Capewell S, et al. Heart failure and the aging population: an increasing burden in the 21st century? Heart. 2003;89:49–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Young JB. The global epidemiology of heart failure. Med Clin North Am 2004;88:1135–1143. [DOI] [PubMed] [Google Scholar]
- 9. Rodriguez‐Artalejo F, Banegas Banegas JR, Guallar‐Castillón P. Epidemiology of heart failure. Rev Esp Cardiolo. 2004;57:163–170. [PubMed] [Google Scholar]
- 10. Archana R, Gray D. The quality of life in chronic‐disease‐heart failure is as bad as it gets. Eur Heart J. 2002;23:1806–1808. [DOI] [PubMed] [Google Scholar]
- 11. De Rivas B, Permanyer‐Miralda G, Brotons C, et al. Health‐related quality of life in unselected outpatients with heart failure across Spain in two different health care levels. Magnitude and determinants of impairment: the INCA study. Qual Life Res. 2008;17:1229–1238. [DOI] [PubMed] [Google Scholar]
- 12. Lloyd‐Jones DM, Larson MG, Leip EP, et al. Lifetime risk for developing congestive heart failure. The Framingham Heart Study. Circulation. 2002;106:3068–3072. [DOI] [PubMed] [Google Scholar]
- 13. Moser M, Hebert PR. Prevention of disease progression, left ventricular hypertrophy and congestive heart failure in hypertension treatment trials. J Am Coll Cardiol. 1996;27:1214–1218. [DOI] [PubMed] [Google Scholar]
- 14. Kannel WB, D’Agostino RB, Silbershatz H, et al. Profile for estimating risk of heart failure. Arch Intern Med. 1999;159:1197–1204. [DOI] [PubMed] [Google Scholar]
- 15. De Rivas B, Divisón JA, Sobreviela E, et al. Prevalence and risk of developing heart failure in hypertensive patients managed in Spanish primary care centres. HICAP study. Rev Clin Esp. 2008;208:513–516. [DOI] [PubMed] [Google Scholar]
- 16. Fahey T, Schroeder K, Ebrahim S. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2006; (4):CD005182. [DOI] [PubMed] [Google Scholar]
- 17. Gómez‐Marcos MA, García‐Ortiz L, González‐Elena LJ, et al. Effectiveness of a quality improvement intervention in blood pressure control in primary care. Rev Clin Esp. 2006;206:428–434. [PubMed] [Google Scholar]
- 18. Hunt SA; American College of Cardiology; American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure) . ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol. 2005;46 (6):e1–e82. [DOI] [PubMed] [Google Scholar]
- 19. European Society of Hypertension‐European Society of Cardiology Guidelines Committee . European Society of Hypertension‐European Society of Cardiology guidelines for management of arterial hypertension. J Hypertens. 2003;21:1011–1053. [DOI] [PubMed] [Google Scholar]
- 20. Global guidelines for type 2 diabetes. International Diabetes Federation 2005. Disponible en: http://www.idf.org/webdata/docs/IDF%20GGT2D.pdf.
- 21. American Diabetes Association. Standards of medical care in diabetes‐‐2008 . Diabetes Care. 2008;31(suppl 1):S12–S54. [DOI] [PubMed] [Google Scholar]
- 22. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol In Adults . Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–2497. [DOI] [PubMed] [Google Scholar]
- 23. Barrios V, Escobar C, Calderón A, et al. Cardiovascular risk profile and risk stratification of the hypertensive population attended by general practitioners and specialists in Spain. The CONTROLRISK study. J Hum Hypertens. 2007;21:479–485. [DOI] [PubMed] [Google Scholar]
- 24. Luque M, De Rivas B, Alvarez B, et al. Influence of target organ lesion detection (assessment of microalbuminuria and echocardiogram) in cardiovascular risk stratification and treatment of untreated hypertensive patients. J Hum Hypertens. 2006;20:187–192. [DOI] [PubMed] [Google Scholar]
- 25. Viazzi F, Parodi D, Leoncini G, et al. Optimizing global risk evaluation in primary hypertension: the role of microalbuminuria and cardiovascular ultrasonography. J Hypertens. 2004;22 (5):907–913. [DOI] [PubMed] [Google Scholar]
- 26. Cerasola G, Mulè G, Nardi E, et al. Usefulness of microalbuminuria in cardiovascular risk stratification of essential hypertensive patients. Nephron Clin Pract. 2004;96:123–130. [DOI] [PubMed] [Google Scholar]
- 27. Martínez AM, Sancho T, Armada E, et al. Prevalence of left ventricular hypertrophy in patients with mild hypertension in primary care: impact of echocardiography on cardiovascular risk stratification. Am J Hypertens. 2003;16:556–563. [DOI] [PubMed] [Google Scholar]


