Abstract
This observational study assessed the achievement of treatment goals, as defined by the Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2004). These goals are: <140/80 mm Hg in elderly patients (65 years and older), <130/80 mm Hg in patients with diabetes or kidney disease, and <130/85 mm Hg in younger patients (younger than 65). From July 2006 to May 2007, 72 physician members of the Fukushima Hypertension Conference enrolled a total of 3320 patients from Fukushima Prefecture, Japan. The median age of the patients was 71 years and 46% were male. The success rate was 27% among patients with diabetes mellitus or renal disease, 30% among those younger than 65 years, and 66% among the elderly without the diseases. Factors significantly associated with an increased risk of failure to achieve goals were obesity, dyslipidemia, family histories of diabetes mellitus or hypertension, and number of antihypertensive drugs used. The presence of atherosclerotic complications decreased the risk. This study revealed low achievement rates, identified the importance of weight control and family histories, and indicated a need for better management to prevent complications.
According to the World Health Organization (WHO), 1 reported cardiovascular disease (CVD) was the most common cause of death worldwide in 2005, accounting for approximately 30% of all deaths, with the main causes of death among individuals 60 years and older being ischemic heart disease followed by cerebrovascular disease. 2 Prevention of CVD is emphasized in both developed and developing countries. 1 , 2 Hypertension affects approximately 1 billion people worldwide 3 and is estimated to account for 6% of deaths worldwide. 4 It is among the most important modifiable risk factors for CVD, and also the most common reason for outpatient office visits to physicians. 5
Hypertension management consists of several components, including the screening of elevated blood pressure (BP), lifestyle interventions and evaluation for pharmaceutical treatment, continued medical follow‐up, and adherence to treatment. 6 , 7 For several decades, many projects and studies have been conducted to clarify the factors associated with BP levels, 7 , 8 , 9 , 10 based on established treatment guidelines. 3 , 11 , 12 Major guidelines include the 2007 Guidelines for the Management of Arterial Hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC) (ESH/ESC 2007) 11 from Europe, the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) 3 from the United States, and the 2003 WHO/International Society of Hypertension (ISH) Statement on Management of Hypertension (WHO/ISH). 12 These reports have produced concise, evidence‐based manuals for the most effective and convenient therapy for hypertensive patients, although there are some differences between them regarding recommended first choice drugs and combinations of drugs. These guidelines provide clear and practical treatment algorithms, indicating goal BPs that take into consideration a patient’s risk factors: <130/80 mm Hg for patients with diabetes mellitus or chronic kidney disease and 140/90 mm Hg for those without the diseases. Intensive and strict BP control among hypertensive patients with diabetes mellitus and/or chronic kidney disease is emphasized, 3 , 11 , 13 because hypertension is a known risk factor for these outcomes. 13 Furthermore, diabetes mellitus often leads to atherosclerotic disorders 14 , 15 and chronic kidney disease, which is defined as either renal damage or decreased kidney function for 3 months or longer, 16 , 17 and causes CVD. 18 , 19
In Japan, the Japanese Society of Hypertension 20 first published the Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2000) in 2000, which was revised as JSH 2004 in 2004. The guidelines explain the measurement and clinical evaluation of BP as well as basic principals of treatment and lifestyle modification. It also indicates adequate BP goals according to individuals’ risk factors, which is similar to previously published guidelines. The average BPs of the Japanese population have decreased between 1961 and 1990 among both men (from 143.2/83.0 mm Hg to 134.3/82.9 mm Hg) and women (from 143.3/82.2 mm Hg to 128.4/77.6 mm Hg) aged 30 to 69 years. 21 During the same period, the incidence of stroke has significantly decreased in response to health promotion activities and introduction of new antihypertensive drugs. 20 , 21 , 22 Nevertheless, there are more than 30 million hypertensive patients in Japan, 23 and it is the second most common disease among those categorized within the metabolic syndrome. 24
Although a few studies reported robust achievement rates based on 140/90 mm Hg as a goal BP level, 25 , 26 , 27 there have been no reports from Japan assessing the rates toward individualized BP goals, and the present study was the first trial to evaluate these rates in a community. The aim of our study was to assess success rates in achieving treatment goals as defined by JSH 2004 in one prefecture in Japan. We will also explore the factors associated with these success rates, including patients’ and physicians’ characteristics.
Research Design and Methods
The present study was a prospective cohort study carried out in Fukushima Prefecture, Japan, from July 2006 to May 2007. Fukushima Prefecture is located in the northern region of Japan, with a population of about 2 million. From March to April 2006, we called physician‐members of the Fukushima Hypertension Conference to solicit participation in this study. The Fukushima Hypertension Conference was established in 1997 and there were 120 members as of April 2006.
Participants in our study had hypertension and had received antihypertensive medication for at least 3 months and visited a participating physician during the baseline survey period (July 2006). In the baseline survey, the physician enrolled the first 10 consecutive patients who were eligible and willing to participate in our study. 28 The enrollment continued until the total number of registered patients reached 50 for each physician. Even if the number of enrolled patients did not reach 50, the recruitment was stopped on the last day of July 2006. The research date was not announced to patients prior to the survey, and appointments for medical consultation were made according to their requests as usual. Enrolled patients were monitored for 1 year in 3‐month intervals.
In the baseline survey, the registered patient’s clinical data was copied from medical files to survey sheets. The data included the patient’s age, sex, height, weight, waist circumference, family histories (hypertension, diabetes mellitus, dyslipidemia, heart disease, stroke, renal disease, and premature CVD), alcohol consumption, current smoking habits, systolic and diastolic BPs, whether home BP measurement was instructed, duration of hypertension treatment, usage of antihypertensive drugs, and presence of metabolic disorders (diabetes mellitus, dyslipidemia), end‐organ damage, and CVDs (brain, heart, kidney, blood vessel, hypertensive, and diabetic retinopathy). The status of renal disease and diabetes mellitus was obtained from physician reports. In Japan, diabetes mellitus is defined based on the Japan Diabetes Society, Diabetes Treatment Guideline 2008–2009. 29 Renal disease is defined based on the Japanese Clinical Practice Guidebook for Diagnostic and Treatment of Chronic Kidney Disease. 16 As for methods to measure BP, we asked physicians to maintain their usual practices and report BP measurements on each day the patients were surveyed. Follow‐up surveys (October 2006, January 2007, and April 2007) collected hypertension‐related information. As for physicians’ characteristics, the following information was collected in the baseline survey: age, sex, place of employment, main specialty, number of hypertensive patients (per month), and measurer, timing, place, and method of BP measurement. The present report used data from the baseline survey and conducted analyses on achievement toward treatment goals and its associated factors.
All data were entered into a computer and analyzed using SPSS version 14 (SPSS Inc, Chicago, IL). We classified participants into 3 groups according to the JSH 2004: elderly patients 65 years and older without diabetes mellitus or renal disease, young or middle‐aged patients without diabetes mellitus or renal disease, and patients with diabetes mellitus or renal disease. The success rates were calculated following treatment goals for each group indicated in JSH 2004: <140/90 mm Hg for elderly patients without diabetes mellitus or renal disease, <130/80 mm Hg for patients with the diseases, and <130/85 mm Hg for young or middle‐aged patients without the diseases. For the analysis of factors associated with failure to achieve the treatment goals, we computed odds ratios (ORs) and 95% confidence intervals (CIs) for each item using univariate logistic regression. Significant factors in the univariate analysis (P<.05) were then entered into a multivariate logistic regression analysis.
With regard to the analysis of physicians’ characteristics and the success rates of their patients, we divided participating physicians into 2 groups using a median split of overall patient success rates (<45% vs ≥45%). The 2 groups were compared using the chi‐square test and Fisher exact test for categoric items and Mann–Whitney test for continuous items.
This survey was conducted according to the Ethical Guideline for Epidemiological Studies established by the Japanese government, 30 and work was performed in accordance with the Declaration of Helsinki of 1975 (revised in 2000). 31
Results
Seventy‐two of 120 members of the Fukushima Hypertension Conference enrolled patients into the study. In the baseline survey, 3358 hypertensive patients were initially registered. Of those registered, 38 patients were excluded due to missing data on BPs and nonmedication, and thus 3320 patients were entered into the present analysis. Median age of patients was 71 years (24–99 years) and the percentage of males was 46.1% (Table I). As for anthropometric measurements, median body mass index (BMI) was 24.3 (13.2–45.4), and median waist circumference was 87.6 cm (59.0–126.0 cm) for males and 85.0 cm (53.0–134.0 cm) for females. Among family histories, the prevalence of hypertension was most frequent (55.2%), followed by stroke (27.6%), diabetes mellitus (18.0%), and heart disease (15.3%). The prevalence of alcohol use (daily consumption) was 21.7%, and that of current smoking was 12.1%. The median systolic and diastolic BPs were 134 mm Hg (82–212 mm Hg) and 76 mm Hg (36–124 mm Hg), respectively. Sixty percent of patients were instructed to measure BPs at home, 43.6% of patients were treated by 1 antihypertensive drug, and the median duration of hypertension treatment was 8.0 years (0.5–60.0 years). The proportion of those with diabetes mellitus was 31.7% and that of dyslipidemia was 44.8%. Cardiovascular complications were reported in 21.5% of patients, neurological complications in 13.4%, and renal complications in 11.1%.
Table I.
Characteristics of Hypertensive Patients at Baseline
| Variables | Median (Range) or No. (%) |
|---|---|
| Age, y | 71 (24–99) |
| Male sex | 1524 (46.1) |
| Anthropometric measurements | |
| Body mass index | 24.3 (13.2–45.4) |
| Waist circumference, cm | |
| Male | 87.6 (59.0–126.0) |
| Female | 85.0 (53.0–134.0) |
| Family histories | |
| Hypertension | 1805 (55.2) |
| Stroke | 902 (27.6) |
| Diabetes mellitus | 589 (18.0) |
| Heart disease | 499 (15.3) |
| Dyslipidemia | 132 (4.0) |
| Renal disease | 123 (3.8) |
| Premature cardiovascular disease | 47 (1.4) |
| Alcohol consumption (daily) | 705 (21.7) |
| Current smoking | 392 (12.1) |
| Hypertension‐related factors | |
| Systolic blood pressure, mm Hg | 134 (82–212) |
| Diastolic blood pressure, mm Hg | 76 (36–124) |
| Instruction of home blood pressure measurement (yes) | 1969 (59.6) |
| Duration of hypertension treatment, y | 8.0 (0.5–60.0) |
| No. of antihypertensive drug used | |
| 1 | 1449 (43.6) |
| 2 | 1318 (39.7) |
| ≥3 | 553 (16.7) |
| Metabolic disorders | |
| Diabetes mellitus | 1050 (31.7) |
| Dyslipidemia | 1484 (44.8) |
| Organ damage/cardiovascular disease | |
| Heart | 713 (21.5) |
| Brain | 445 (13.4) |
| Kidney | 368 (11.1) |
| Peripheral vascular disease | 249 (7.5) |
| Hypertensive retinopathy | 150 (4.5) |
| Diabetic retinopathy | 176 (5.3) |
Table II shows various characteristics of the physicians assisting in this study. Seventy of 72 physicians completed the questionnaire. The proportion of males was 93.0% and median years after graduation from medical school was 24 years. The most frequent specialty among participating physicians was general internal medicine (n=35), followed by cardiology (n=17), gastroenterology (n=7), and endocrinology (n=7). The proportion of those working at hospitals was 52.9%, and 60.0% were located in urban areas (defined as cities with >100,000 residents). Median number of hypertensive patients per physician per month was 300. Eighty percent of physicians measured BPs by themselves, 82.9% during medical consultation, 82.9% in a consultation room, and 72.9% using mercury sphygmomanometer.
Table II.
Characteristics of Physicians Participating in the Survey
| Variables | Median (Range) or No. (%) |
|---|---|
| Male sex | 65 (93.0) |
| Years after graduation from medical university, y | 24 (8–44) |
| Main specialty | |
| General internal medicine | 34 (48.6) |
| Cardiology | 16 (22.9) |
| Gastroenterology | 7 (10.0) |
| Endocrinology | 7 (10.0) |
| Others | 6 (8.5) |
| Medical office | |
| Hospital | 37 (52.9) |
| Clinic | 33 (47.1) |
| Location of medical office (urbana) | |
| Urbana | 42 (60.0) |
| Rural | 28 (40.0) |
| Number of attending hypertension patients (No. per month) | 300 (15–1500) |
| Measurer of BP | |
| Physician | 56 (80.0) |
| Nurse | 8 (11.4) |
| Patient | 6 (8.6) |
| Timing of BP measurement | |
| During medical consultation | 58 (82.9) |
| Waiting time | 11 (15.7) |
| Others | 1 (1.4) |
| Place of BP measurement | |
| Consultation room | 58 (82.9) |
| Treatment room or waiting space | 11 (15.7) |
| Others | 1 (1.4) |
| Method of BP measure | 51 (72.9) |
| Mercury sphygmomanometer | 51 (72.9) |
| Automated sphygmomanometer | 19 (27.1) |
| No. of registered patients | 49.5 (14–51) |
| Achievement rate toward treatment goals | 43.9 (14.3–82.0) |
Abbreviation: BP, blood pressure. aUrban is defined as a city with a population of ≥100,000.
The median systolic and diastolic BPs were 134 mm Hg (84–190 mm Hg) and 75 mm Hg (36–120 mm Hg) for elderly without diabetes mellitus or renal disease, 132 mm Hg (100–180 mm Hg) and 80 mm Hg (43–106 mm Hg) for those younger than 65 years without the diseases, and 134 mm Hg (82–212 mm Hg) and 76 mm Hg (39–124 mm Hg) for those with the diseases. Success rates toward treatment goals (defined by JSH 2004) were 66.0% for the elderly without diabetes mellitus or renal disease, 30.4% for those younger than 65 years without the diseases, and 26.7% for those with the diseases (Table III). We conducted an additional analysis among those younger than 65 years without the diseases according to JNC 7 3 (<140/90 mm Hg), whose target BP level differs from JSH 2004, and found the success rate to be 65.9%.
Table III.
Median of Blood Pressure (BP) and Success Rates Toward Target BP Levels
| JSH 2004 Target BP Level, mm Hg | Median (Range) of Systolic and Diastolic BP, mm Hg | Success Rates, No. (%) | |
|---|---|---|---|
| Elderly patients without diabetes mellitus or renal disease (n=1518) | <140/90 | 134 (84–190)/75 (36–120) | 1002 (66.0) |
| Young or middle‐aged patients without diabetes mellitus or renal disease (n=583) | <130/85 | 132 (100–180)/80 (43–106) | 177 (30.4) |
| Patients with diabetes mellitus or renal disease (n=1212) | <130/80 | 134 (82–212)/76 (39–124) | 324 (26.7) |
Abbreviation: JSH 2004, Japanese Society of Hypertension Guidelines for the Management of Hypertension.
The Figure shows the number of antihypertensive drugs used. Monotherapy was most frequent among the elderly without diabetes mellitus or renal disease (47.7%), while bitherapy was most frequent among the patients with the diseases (40.9%). Median systolic and diastolic BPs were 132 mm Hg (82–190 mm Hg) and 77 mm Hg (36–120 mm Hg) among patients treated with monotherapy, 134 mm Hg (92–190 mm Hg) and 76 mm Hg (39–111 mm Hg) among those treated with bitherapy, and 135 mm Hg (96–212 mm Hg) and 76 mm Hg (41–124 mm Hg) among those treated with ≥3 drugs.
Figure.
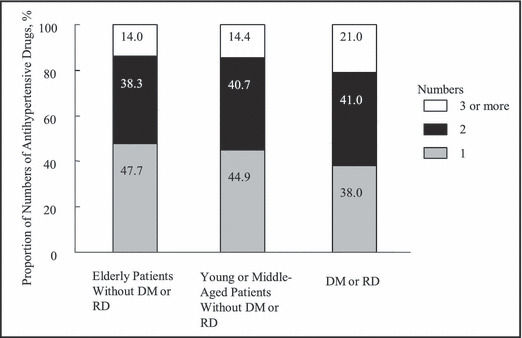
Numbers of antihypertensive drugs. DM indicates diabetes mellitus; RD, renal disease.
The multivariate analysis showed that the factors significantly associated with failure to achieve treatment goals were waist circumference of ≥85 cm for men and ≥90 cm for women (OR, 1.26; 95% CI, 1.01–1.57) and usage of ≥3 antihypertensive drugs (OR, 1.96; 95% CI, 1.42–2.71) for the elderly group without diabetes mellitus or renal disease (Table IVa). For young and middle‐aged patients without diabetes mellitus or renal disease, the significant factors were BMI ≥25 (OR, 1.74; 95% CI, 1.19–2.56), family history of hypertension (OR, 1.67; 95% CI, 1.14–2.45), cerebrovascular complication (OR, 0.33; 95% CI, 0.16–0.68), and hypertensive retinopathy (OR, 0.33; 95% CI, 0.12–0.91) (Table IVb). For patients with diabetes mellitus or renal disease, BMI ≥25 (OR, 1.34; 95% CI, 1.03–1.75), family history of diabetes mellitus (OR, 1.40; 95% CI, 1.04–1.87), dyslipidemia (OR, 1.41; 95% CI, 1.08–1.84), and cerebrovascular (OR, 0.62; 95% CI, 0.44–0.87) and vascular complications (OR, 0.48; 95% CI, 0.33–0.70) were significantly associated (Table IVc).
Table IV.
Association of Blood Pressure Achievement Failure
| Variables | No. (%) | Odds Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|---|
| (a) In elderly patients without diabetes mellitus or renal disease (multivariate logistic regression analyses) | ||||
| Waist circumference ≥85 cm for men, ≥90 for women | 620 (42.1) | 1.26 | 1.01–1.57 | <0.05 |
| No. of antihypertensive drugs used | ||||
| 1 | 461 (38.0) | 1.00 (Reference) | ||
| 2 | 496 (40.9) | 1.15 | 0.91–1.46 | |
| ≥3 | 255 (21.0) | 1.96 | 1.42–2.71 | <0.05 |
| (b) In young and middle‐aged patients without diabetes mellitus or renal disease (multivariate logistic regression analyses) | ||||
| Body mass index ≥25 | 241 (42.8) | 1.74 | 1.19–2.56 | <0.05 |
| Family history of hypertension (yes) | 378 (66.4) | 1.67 | 1.14–2.45 | <0.05 |
| Organ damage/cardiovascular disease | ||||
| Brain (yes) | 33 (5.7) | 0.33 | 0.16–0.68 | <0.05 |
| Hypertensive retinopathy (yes) | 17 (2.9) | 0.33 | 0.12–0.91 | <0.05 |
| (c) In patients with diabetes mellitus or renal disease (multivariate logistic regression analyses) | ||||
| Body mass index ≥25 | 582 (48.5) | 1.34 | 1.03–1.75 | <0.05 |
| Family history of diabetes mellitus (yes) | 379 (31.5) | 1.40 | 1.04–1.87 | <0.05 |
| Dyslipidemia (yes) | 656 (54.3) | 1.41 | 1.08–1.84 | <0.05 |
| Organ damage/cardiovascular disease | ||||
| Brain (yes) | 191 (15.8) | 0.62 | 0.44–0.87 | <0.05 |
| Blood vessel (yes) | 144 (11.9) | 0.48 | 0.33–0.70 | <0.05 |
Table V shows the differences in characteristics between 2 groups of physicians categorized by overall success rates of their patients. The proportion of elderly patients without diabetes mellitus or renal disease was higher among physicians with higher success rates.
Table V.
Physician Characteristics of Blood Pressure Achievement Rates Toward Treatment Goals
| Achievement Rate Median (Range) or No. (%)a | P Value | ||
|---|---|---|---|
| Variables | <45% (n=38) | ≤45% (n=32) | |
| Male sex | 35 (92.1) | 30 (93.8) | |
| Years after graduation from medical university | 24 (8–40) | 25 (11–44) | |
| Main specialty (internal medicine) | 37 (97.4)) | 29 (90.6) | |
| Medical office (hospital) | 23 (60.5) | 14 (43.8) | |
| Location of medical office (urbanb) | 25 (65.8) | 17 (53.1) | |
| Number of attending hypertension patients (for one month) | 300 (15–1500) | 300 (32–1200) | |
| Measurer of BP (physician) | 31 (81.6) | 25 (78.1) | |
| Timing of BP measurement (during medical consultation) | 32 (84.2) | 26 (81.3) | |
| Place of BP measurement (consultation room) | 32 (84.2) | 26 (81.3) | |
| Method of BP measure (mercury sphygmomanometer) | 28 (73.7) | 23 (71.9) | |
| Proportion of registered patients, % | |||
| Elderly patients without diabetes mellitus or renal disease | 42.8 (0.0–74.0) | 55.0 (0.0–84.0) | <0.01 |
| Young and middle‐aged patients without diabetes | 18.6 (0.0–60.0) | 13.3 (0.0–61.3) | |
| Patients with diabetes mellitus or renal disease | 29.2 (4.0–100) | 27.9 (2.0–100) | |
Abbreviation: BP, blood pressure. aThe chi‐square test and Fisher exact test for categoric items and Mann–Whitney test for continuous items were used to assess the significance. bUrban is defined as a city with a population of ≥100,000.
Discussion
This community‐based assessment of hypertension control among our patients in one prefecture in Japan showed excellent results with a median BP <140/90 mm Hg. Now given new target BP levels redefined by recent hypertension management guidelines, 3 , 11 , 20 we used the JSH 2004 to calculate the success rates among our patient population. Achievement rates were relatively pessimistic, especially among patients with diabetes mellitus or renal disease and those younger than 65 years without diseases based on JSH 2004, although median BPs showed excellent results of <140/90 mm Hg.
Other factors associated with failure to achieve treatment goals included BMI, waist circumference, family histories, dyslipidemia, and usage of ≥3 antihypertensive drugs increased the risk of achievement failure, while presence of complications was paradoxically associated with success rates.
The success rate of elderly patients without diabetes mellitus or renal disease in our study was substantially higher compared with those of young and middle‐aged patients. Likewise, a Japanese cross‐sectional study reported that achievement rate toward goal BP (defined as <140/90 mm Hg) was 17.0% in patients younger than 60 years while it was 40.6% for patients 60 to 69 years, 54.4% for patients 70 to 79 years, and 65% for patients 80 years and older. 32 In contrast, previous studies have reported advancing age as an independent predictor of inadequate BP control in the United States. 33 , 34 The discrepancies in achievement rates between the elderly and nonelderly in Japan and between the elderly in Japan and the United States could be explained in part by differences in health behaviors among the older generations. JNC 7 emphasizes the importance of the following 5 healthy lifestyles: weight reduction, improvement in dietary habits, dietary sodium restriction, increased physical activity, and appropriate alcohol consumption. 3 The proportions of those who exercise regularly, keep healthy weight, and do not smoke were higher in the elderly compared with the nonelderly according to a Japanese national survey. 35 In the United States, on the other hand, these proportions in the elderly are lower compared with the nonelderly. 36 , 37 Furthermore, BP level is correlated with cardiovascular mortality in the nonelderly, 10 which could result in a survivor effect causing a relatively elevated success rate among the Japanese elderly.
The study indicated that 2 markers of obesity, high BMI and waist circumference, were significantly associated with achievement failure among hypertensive patients with diabetes mellitus or renal disease, and young and middle‐aged patients without the diseases. Several studies have reported a high prevalence of hypertension among obese individuals compared with nonobese individuals. 38 , 39 , 40 The sympathetic nervous system, sodium retention/salt sensitivity, and insulin resistance are thought to be involved in the etiology of hypertension accompanied by obesity. 20 As previous research emphasized, 41 , 42 body weight control is thus considered one of the most important therapeutic strategies in JSH 2004, 20 JNC 7, 3 and ESH/ESC 2007. 12 In other words, obesity is an important risk factor of failure to achieve treatment goals 33 as indicated in our results.
It is well‐known that family histories of hypertension, 43 diabetes mellitus, 44 and dyslipidemia 45 are risk factors for hypertension. The number of these risk factors, as well as nonfavorable health behaviors, is associated with an increased incidence of hypertension and overall CVD severity. In Japan, family histories are usually recorded in standard medical files with other basic information and are checked in general clinical practice and routine health check‐ups.
Interestingly, we found a positive association between history of organ and vascular complications and achieving treatment goals. It may be possible that both patient and physician become more aware of the need to maintain goal BP levels, once organ and vascular complications present. Previous studies have reported a similar association between history of CVD and improved BP control, explained by increased patient compliance and/or more aggressive treatment. 46 , 47 Supporting this hypothesis, Street and colleagues 48 also reported that physicians seeing patients with a critical disease paid more attention to their clients than physicians seeing patients with less severe conditions. Furthermore, a lack of disease awareness has been pointed out as a patient‐related factor related to poor BP control. 49 Had patients been treated appropriately in the past, such a paradoxical result may not have been found, and presence of complications may have instead become a risk factor of inadequate BP control. Our results suggest the necessity of better management of hypertension prior to the onset of complications.
Using ≥2 drugs was a risk factor of achievement failure among our elderly patients without diabetes mellitus or renal disease. A previous report from the United States also showed that a multi‐drug regimen was an independent risk factor of poor BP control, 46 and patients whose BP is difficult to control are more likely to be treated with multiple drugs. Additional analyses of our study showed that a multiple antihypertensive drug therapy correlates with higher number of vascular and/or organ damage, longer duration of hypertension treatment, and a family history of hypertension. These findings suggest that resistance to treatment persists among the elderly without diabetes mellitus or renal disease, despite physician adherence to treatment guidelines. Further analysis of follow‐up data on change in antihypertensive drugs may provide additional insight on the relationship between different medications and BP control.
Limitations
Our study has some major limitations. First is a selection bias; the physicians who participated in our study were limited to members of the Fukushima Hypertension Conference, and participants were limited to hypertensive patients who visited these physicians. In addition, some important information on their characteristics and medical practices were not investigated, and the patient characteristics appeared as the only factor that differed significantly between 2 groups of physicians classified by their achievement levels. It is possible that participating members might be more aware about hypertension management compared with nonmembers. Success rates might become lower showing significant associations with physician’s characteristics once nonmembers are included. Secondly, this was a cross‐sectional analysis using baseline data, and causal relationships between success rates and the associated factors cannot be fully elucidated. Further analyses of follow‐up survey data are needed. Thirdly, other important factors, such as patient’s health behaviors, physicians’ treatment strategies, and their disease awareness were not obtained in our survey. The inclusion of additional factors in the multivariate analysis model might have modified our results.
Conclusions
The present study, which was conducted in one prefecture in Japan, revealed low achievement rates toward treatment goals among hypertensive patients regardless of physician characteristics, especially in groups with diabetes mellitus or renal disease and those younger than 65 years without the diseases. Analysis of associated factors indicated the importance of weight control, assessment of family history, and a need for better management before atherosclerotic complications appear.
Acknowledgments and disclosures: We thank physician members of the Fukushima Hypertension Conference for their excellent help in data collection, and the staff of the Department of Public Health, Fukushima Medical University School of Medicine, for data management. This study was funded by a Fukushima‐ken Igaku Shinkoukai (Fukushima Medical Foundation) grant (2006).
References
- 1. World Health Organization . Ten Statistical Highlights in Global Public Health. World Health Statistics 2006. http://www.who.int/whosis/whostat2006_10highlights.pdf. Accessed June 1, 2008. 2006. [Google Scholar]
- 2. World Health Organization . Global Health: Today’s Challenges. The World Health Report 2003. 2003. http://www.who.int/whr/2003/en/Chapter1‐en.pdf. Accessed June 1, 2008. [Google Scholar]
- 3. Chobanian AV, Bakris GL, Black HR, et al. National Heart, Lung, and Blood Institute Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 4. Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349:1436–1442. [DOI] [PubMed] [Google Scholar]
- 5. Cherry DK, Woodwell DA, Rechtsteiner EA. National Ambulatory Medical Care Survey: 2005 summary. Adv Data. 2007;387:1–39. [PubMed] [Google Scholar]
- 6. Whelton PK, He J, Appel LJ, et al. National High Blood Pressure Education Program Coordinating Committee. Primary prevention of hypertension: clinical and public health advisory from The National High Blood Pressure Education Program. JAMA. 2002;288:1882–1888. [DOI] [PubMed] [Google Scholar]
- 7. Mechanic D, McAlpine DD, Rosenthal M. Are patients’ office visits with physicians getting shorter? N Engl J Med. 2001;344:198–204. [DOI] [PubMed] [Google Scholar]
- 8. Kikuya M, Hozawa A, Ohokubo T, et al. Prognostic significance of blood pressure and heart rate variabilities: the Ohasama study. Hypertension. 2000;36:901–906. [DOI] [PubMed] [Google Scholar]
- 9. Stamler J, Stamler R, Neaton JD. Blood pressure, systolic and diastolic, and cardiovascular risks. US population data. Arch Intern Med. 1993;153:598–615. [DOI] [PubMed] [Google Scholar]
- 10. Flack JM, Neaton J, Grimm R Jr, et al. Blood pressure and mortality among men with prior myocardial infarction. Multiple Risk Factor Intervention Trial Research Group. Circulation. 1995;92:2437–2445. [DOI] [PubMed] [Google Scholar]
- 11. Mancia G, De Backer G, Dominiczak A, et al; Management of Arterial Hypertension of the European Society of Hypertension; European Society of Cardiology . 2007 Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25:1105–1187. [DOI] [PubMed] [Google Scholar]
- 12. Whitworth JA; World Health Organization, International Society of Hypertension Writing Group . 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21:1983–1992. [DOI] [PubMed] [Google Scholar]
- 13. National Kidney Foundation Kidney Disease Outcome and Quality Initiative (NKF/KDOQI) . K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004;43(5 suppl 1):S1–S290. [PubMed] [Google Scholar]
- 14. Almdal T, Scharling H, Jensen JS, et al. The independent effect of type 2 diabetes mellitus on ischemic heart disease, stroke, and death: a population‐based study of 13,000 men and women with 20 years of follow‐up. Arch Intern Med. 2004;164:1422–1426. [DOI] [PubMed] [Google Scholar]
- 15. Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000;321:412–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. The Japanese Society of Nephrology . Clinical Practice Guidebook for Diagnostic and Treatment of Chronic Kidney Disease. Tokyo: Tokyo Igakusya; 2007. (In Japanese). [Google Scholar]
- 17. Levey AS, Coresh J, Balk E, et al.; National Kidney Foundation . National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139:137–147. [DOI] [PubMed] [Google Scholar]
- 18. Go AS, Chertow GM, Fan D, et al. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. [DOI] [PubMed] [Google Scholar]
- 19. Deo R, Fyr CL, Fried LF, et al.; Health ABC study . Kidney dysfunction and fatal cardiovascular disease – an association independent of atherosclerotic events: results from the Health, Aging, and Body Composition (Health ABC) study. Am Heart J. 2008; 155:62–68. [DOI] [PubMed] [Google Scholar]
- 20. Japanese Society of Hypertension . Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2004). Hypertens Res. 2006;29(suppl):S1–S105. [DOI] [PubMed] [Google Scholar]
- 21. Kitamura A, Iso H, Iida M, et al. Trends in the incidence of coronary heart disease and stroke and the prevalence of cardiovascular risk factors among Japanese men from 1963 to 1994. Am J Med. 2002;112:104–109. [DOI] [PubMed] [Google Scholar]
- 22. Kubo M, Kiyohara Y, Kato I, et al. Trends in the incidence, mortality, and survival rate of cardiovascular disease in a Japanese community: the Hisayama study. Stroke. 2003;34:2349–2354. [DOI] [PubMed] [Google Scholar]
- 23. Ministry of Health and Welfare . 5th National Basic Survey for Circulatory Disease. http://www.mhlw.go.jp/toukei/saikin/hw/kenkou/jyunkan/jyunkan00/gaiyo.html. Accessed June 1, 2008. 2001. (In Japanese). [Google Scholar]
- 24. Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–1428. [DOI] [PubMed] [Google Scholar]
- 25. Spranger CB, Ries AJ, Berge CA, et al. Identifying gaps between guidelines and clinical practice in the evaluation and treatment of patients with hypertension. Am J Med. 2004;117:14–18. [DOI] [PubMed] [Google Scholar]
- 26. Singer GM, Izhar M, Black HR. Goal‐oriented hypertension management: translating clinical trials to practice. Hypertension. 2002;40:464–469. [DOI] [PubMed] [Google Scholar]
- 27. Osuga E, Tamachi H, Hayakawa H. Blood pressure control in outpatients with hypertension after the publication of the JSH 2000 guidelines. Jpn J Clin Pharmacol Ther. 2003;34:283–288 (In Japanese). [Google Scholar]
- 28. Phan TL, Elias C, Nguyen TL, et al. The prevalence of reproductive tract infections in Hue, Vietnam. Stud Fam Plann. 2002;33:217–226. [DOI] [PubMed] [Google Scholar]
- 29. Japan Diabetes Society . Diabetes Treatment Guideline 2008‐2009, Tokyo: Bunkodo; 2008. (In Japanese). [Google Scholar]
- 30. Ministry of Health, Labor and Welfare & Ministry of Education, Culture, Sports, Science and Technology . Ethical Guideline for Epidemiological Studies. http://www‐bm.mhlw.go.jp/general/seido/kousei/i‐kenkyu/ekigaku/0504sisin.html. Accessed June 1, 2008. 2007. (In Japanese). [Google Scholar]
- 31. Anonymous . World Medical Association Declaration of Helsinki. JAMA. 2000;284:3043–3045. [PubMed] [Google Scholar]
- 32. Yamamoto Y, Sonoyama K, Matsubara K, et al. The status of hypertension management in Japan in 2000. Hypertens Res. 2002;25:717–725. [DOI] [PubMed] [Google Scholar]
- 33. Lloyd‐Jones DM, Evans JC, Larson MG, et al. Differential control of systolic and diastolic blood pressure: factors associated with lack of blood pressure control in the community. Hypertension. 2000;36:594–599. [DOI] [PubMed] [Google Scholar]
- 34. Hyman DJ, Pavlik VN. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med. 2001;345:479–486. [DOI] [PubMed] [Google Scholar]
- 35. Public Health Division, Ministry of Health, Labor and Welfare . National Survey of Health and Nutrition. http://www.mhlw.go.jp/houdou/2007/05/h0516‐3a.html. Accessed June 1, 2008. 2007. (In Japanese). [Google Scholar]
- 36. Reeves MJ, Rafferty AP. Healthy lifestyle characteristics among adults in the United States, 2000. Arch Intern Med. 2005;165:854–857. [DOI] [PubMed] [Google Scholar]
- 37. Summary Health Statistics for U.S. Adults: National Health Interview Survey. 2006. http://www.cdc.gov/nchs/data/series/sr_10/sr10_235.pdf. Accessed June 1, 2008. [PubMed] [Google Scholar]
- 38. Brown CD, Higgins M, Donato KA, et al. Body mass index and the prevalence of hypertension and dyslipidemia. Obes Res. 2000;8:605–619. [DOI] [PubMed] [Google Scholar]
- 39. Wilsgaard T, Schirmer H, Arnesen E. Impact of body weight on blood pressure with a focus on sex differences: the Tromso Study, 1986‐1995. Arch Intern Med. 2000;160:2847–2853. [DOI] [PubMed] [Google Scholar]
- 40. Rosenbaum M, Leibel RL, Hirsch J. Obesity. N Engl J Med. 1997;337:396–407. [DOI] [PubMed] [Google Scholar]
- 41. Anonymous . Executive summary of the clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. Arch Intern Med. 1998;158:1855–1867. [DOI] [PubMed] [Google Scholar]
- 42. Kiernan M, Winkleby MA. Identifying patients for weight‐loss treatment: an empirical evaluation of the NHLBI obesity education initiative expert panel treatment recommendations. Arch Intern Med. 2000;160:2169–2176. [DOI] [PubMed] [Google Scholar]
- 43. Tozawa M, Oshiro S, Iseki C, et al. Multiple risk factor clustering of hypertension in a screened cohort. J Hypertens. 2000;18:1379–1385. [DOI] [PubMed] [Google Scholar]
- 44. Kannel WB, Wilson PW, Zhang TJ. The epidemiology of impaired glucose tolerance and hypertension. Am Heart J. 1991;121:1268–1273. [DOI] [PubMed] [Google Scholar]
- 45. Bønaa KH, Thelle DS. Association between blood pressure and serum lipids in a population. The Tromsø Study. Circulation. 1991;83:1305–1314. [DOI] [PubMed] [Google Scholar]
- 46. Knight EL, Bohn RL, Wang PS, et al. Predictors of uncontrolled hypertension in ambulatory patients. Hypertension. 2001;38:809–814. [DOI] [PubMed] [Google Scholar]
- 47. Di Bari M, Salti F, Nardi M, et al. Undertreatment of hypertension in community‐dwelling older adults: a drug‐utilization study in Dicomano, Italy. J Hypertens. 1999;17:1633–1640. [DOI] [PubMed] [Google Scholar]
- 48. Street RL Jr, Gordon HS, Ward MM, et al. Patient participation in medical consultations: why some patients are more involved than others. Med Care. 2005;43:960–969. [DOI] [PubMed] [Google Scholar]
- 49. Düsing R. Overcoming barriers to effective blood pressure control in patients with hypertension. Curr Med Res Opin. 2006;22:1545–1553. [DOI] [PubMed] [Google Scholar]


