Abstract
J Clin Hypertens (Greenwich). 2010;12:40–46. © 2009 Wiley Periodicals, Inc.
Patient adherence to antihypertensive medication is vital to ensure the successful treatment of hypertension. Low levels of adherence to and persistence with prescribed therapy are major factors leading to the current poor rates of blood pressure control among patients with hypertension. There are many reasons for nonadherence to therapy including patient‐, physician‐, and therapy‐related factors. Poor tolerability has a detrimental effect on adherence, therefore reducing the apparent effectiveness of agents with dose‐dependent side effects. Various effective combination therapies are recommended by current guidelines, eg, β‐blocker plus calcium channel blocker (CCB), angiotensin receptor blocker (ARB) plus thiazide diuretic, angiotensin‐converting enzyme (ACE) inhibitor plus thiazide diuretic, CCB plus thiazide diuretic, ACE inhibitor plus CCB, and ARB plus CCB, and these have the potential to increase adherence to therapy by combining a favorable tolerability profile with once‐daily dosing.
Hypertension is a major risk factor for cardiovascular (CV) and cerebrovascular disease. However, only 37% of US patients with hypertension 1 and 12% to 36% of European patients with hypertension 2 achieve adequate blood pressure (BP) control. These suboptimal BP control rates contribute to the 7.1 million premature deaths attributed to hypertension per year. 3
Recent updates to the European Society of Hypertension (ESH) and European Society of Cardiology (ESC) guidelines acknowledge the poor hypertension control rates and endorse the use of combination therapy to improve BP control. 4 These guidelines state that the majority of patients will require combination therapy in order to achieve BP goals and a number of “preferred” 2‐agent combinations are endorsed (Figure 1). 4
Figure 1.
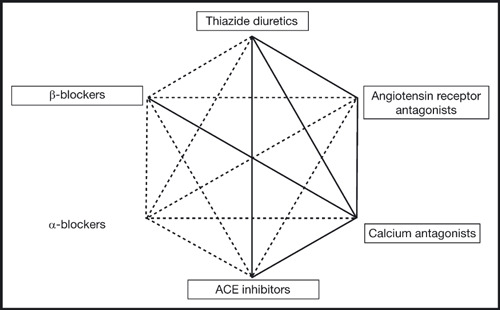
Possible combinations between some classes of antihypertensive drugs. The preferred combinations in the general hypertensive population are represented as thick lines. The frames indicate classes of agents proven to be beneficial in controlled intervention trials. ACE indicates angiotensin‐converting enzyme. Reproduced with permission from Mancia et al. 4
In addition to the development of new and potent combination options, the effectiveness of a drug treatment program is also dependent on the drug dose, the dosing interval, and the successful execution of the prescribed treatment program by the patient. Patient adherence (also known as compliance) to the prescribed therapeutic regimen is vital to ensure successful treatment of hypertension. 4 The aim of this review is to discuss the factors involved in regimen adherence and persistence and the benefits of good treatment adherence. Strategies to improve drug adherence, such as the use of fixed‐dose combinations, including the most recently developed involving an angiotensin receptor blocker (ARB) and a calcium channel blocker (CCB), 5 , 6 will also be considered.
Therapeutic Adherence is Multidimensional
Adherence to therapy is the extent to which a patient takes the medication as prescribed on a day‐to‐day basis. 7 Persistence is the extent to which a patient continues therapy for the duration of the disease. 7 Persistence is especially relevant in chronic conditions such as hypertension, in which patients may need to take medication for the rest of their lives.
Several factors contribute to therapeutic adherence, and here we will discuss patient‐, physician‐, and therapy‐related factors of regimen adherence (Figure 2). 7 , 8
Figure 2.
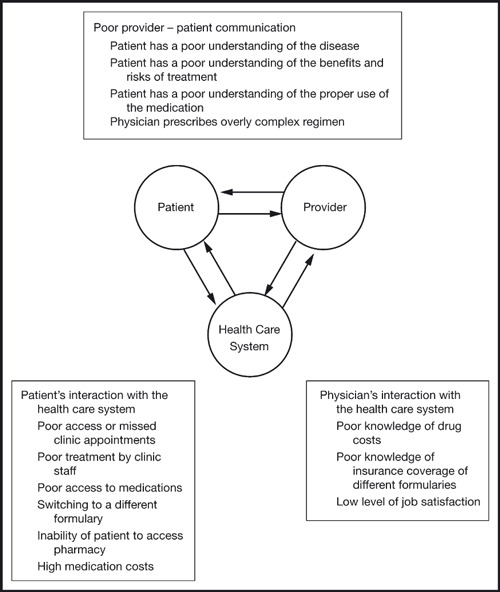
Factors specific to the patient, the provider, and the health care system interact to cause poor adherence. Reproduced with permission from Osterberg and Blaschke. 8
Patient‐Related Factors
The asymptomatic and chronic nature of hypertension affects both adherence and persistence because there are no symptoms to remind the patient of their condition and therefore they do not experience any adverse effects if they do not take their medication properly. In addition, an understanding of hypertension and the perception of the condition is another patient‐related factor that affects adherence. If patients are not aware of the chronic nature of the disease, or believe it is a trivial condition, they are less likely to adhere to and persist with prescribed therapy. Other patient‐related factors include demographic characteristics (eg, certain age groups are generally more adherent to therapy), socioeconomic status, and patient participation in therapy monitoring and disease management. 9 , 10
It has also been shown, in an analysis of 4783 patients prescribed antihypertensive therapy in 21 clinical studies of licensed drugs, that patients’ day‐to‐day dosing habits affect adherence. 11 Patients were more likely to take their medication if they normally took it in the morning than if they normally took it in the evening. Patients who took their medication at variable times during the day were the least likely to adhere to therapy. Moreover, there was a significant correlation between poor day‐to‐day adherence and poor long‐term persistence, with less than 20% of patients who adhered to therapy on fewer than 60% of days persisting with therapy after 1 year.
Physician‐Related Factors
The role of the physician in patient adherence and persistence is a critical one, 12 since physicians determine the prescribed regimen and often need to convince the patient of the need for treatment. Physician‐related factors that have been shown to affect adherence in hypertension include good patient‐physician relations, 13 willingness to treat hypertension aggressively (dose titration and combination therapy), and degree of knowledge of drug costs and insurance coverage of available formularies. 8
Therapy‐Related Factors
Regimen tolerability is a primary factor in treatment adherence. 10 Other important factors include regimen complexity and duration. 6 , 14
Persistence in Relation to Tolerability
The tolerability of an antihypertensive agent is a critical factor in determining adherence to treatment. Patient concerns regarding the nature and severity of side effects, especially at the start of therapy, are regarded as a major hindrance to adherence. 10 Because of this, physicians have to balance the benefit of therapy against the likelihood that patients will become nonadherent. Physicians may, therefore, sacrifice more effective BP control by selecting low‐dose formulations to avoid dose‐dependent side effects and improve adherence.
Persistence rates with hypertensive medications vary greatly. Indeed, in a 10‐year study of patients prescribed antihypertensive therapy, less than 60% of patients persisted with treatment after 2 years of treatment and only 39% were adherent to therapy for the full 10 years (Figure 3). 15 Considering the chronic nature of hypertension, this level of persistence is of great therapeutic concern.
Figure 3.
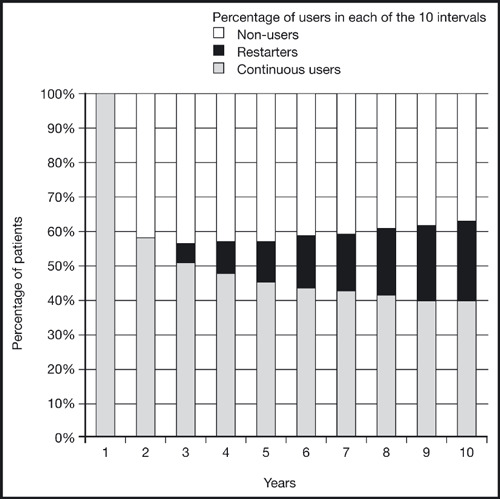
Patient adherence to antihypertensive therapy over a period of 10 years. Reproduced with permission from van Wijk and coworkers. 15
Because different classes of antihypertensive agents are associated with different tolerability profiles, attention should be paid to how these may affect adherence and persistence. It has been demonstrated, for example, that persistence rates from 12 to 48 months were higher in patients prescribed therapy with an ARB than for those prescribed other antihypertensive agents (Figure 4). 16
Figure 4.
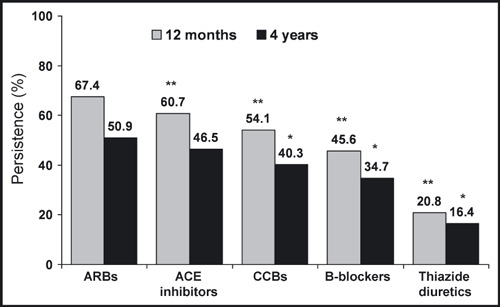
Persistence to antihypertensive drug classes over a 12‐month and 4‐year period. ARBs indicate angiotensin receptor blockers; ACE, angiotensin‐converting enzyme; CCBs, calcium channel blockers. *P<.05 vs ARBs. **P<.01 vs ARBs. 16 Figure reproduced with permission from Conlin et al. 16
Compared with other antihypertensive agents, ARBs are associated with a favorable tolerability profile even at twice the standard dose (Table I). 17 The recent Ongoing Telmisartan Alone and in Combination With Ramipril Global Endpoint Trial (ONTARGET) supported these findings by showing that the ARB telmisartan was as efficacious as the angiotensin‐converting enzyme (ACE) inhibitor ramipril in preventing adverse CV outcomes in high‐risk patients. Furthermore, telmisartan was associated with a lower incidence of angioedema, and a 4‐fold lower rate of discontinuation due to cough, compared with ramipril. 18 This favorable tolerability profile makes ARBs ideal candidates for combination therapy, since adherence and persistence are likely to be higher than with combinations involving other agents.
Table I.
Placebo‐Adjusted Proportion of Patients With ≥1 Side Effectsa in Patients Taking Thiazide Diuretics, β‐Blockers, ACE Inhibitors, ARBs, or CCBs in Randomized Trials
| Class of Drug | Placebo‐Adjusted Percentage of Patients With Symptoms (95% Confidence Interval) | ||
|---|---|---|---|
| Half Standard Dose | Standard Dose | Twice Standard Dose | |
| Thiazide diuretics | 2.0 (−2.2–6.3) | 9.9 (6.6–13.2) | 17.8 (11.5–24.2) |
| β‐Blockers | 5.5 (0.3–10.7) | 7.5 (4.0–10.9) | 9.4 (3.6–15.2) |
| ACE inhibitors | 3.9 (−3.7–11.6) | 3.9 (–0.5–8.3) | 3.9 (−0.2–8.0) |
| ARBs | −1.8 (−10.2–6.5) | 0 (−5.4–5.4) | 1.9 (−5.6–9.3) |
| CCBs | 1.6 (−3.5–6.7) | 8.3 (4.8–11.8) | 14.9 (9.8–20.1) |
Abbreviations: ACE, angiotensin‐converting enzyme; ARBs, angiotensin receptor blockers; CCB, calcium channel blockers. aExcluding headaches, which were more common with placebo. Amended with permission from Law et al. 17
Methods of Adherence Assessment
Several methods of adherence assessment are available. The most accurate methods are direct patient observation and electronic monitoring, although these are impractical and too expensive for use in the primary care setting and are therefore mainly used during clinical trials. 7
The most common forms of treatment adherence assessment are physician consultations and counting unused medications (pill count), with a pill usage in excess of 80% being used to define adherent patients. However, adherence rates may be overestimated with the pill count method if patients dispose of unused medications. Furthermore, as with self‐reported adherence (usually in the form of a daily diary card), pill counts provide no information on the actual time of dosing. 7 Pharmacy refill data can also be used to calculate adherence and has the benefit that large‐scale analyses can be performed; however, this method is dependant on complete pharmacy databases that capture all pharmacy refills. 7
Using these various methods of assessing adherence in hypertension, nonadherence rates have been estimated to range from 9% to 37% (Table II), 19 and in the primary health care setting, anywhere between 20% and 80% of patients can be considered “good compliers” with hypertensive therapy. 20 This broad variation between different studies not only reflects the different assessment methods that were used, but also differences between the study populations.
Table II.
The Proportion (%) of Patients Deemed to Be Noncompliant in Selected Studies That Used Specific Cutoffs for the Determination of Medication Compliance
| Study Reference | Compliance Measure | Monitoring Period, wk | Cutoff, % | Patients Below Cutoff, % |
|---|---|---|---|---|
| Mallion and coworkers 34 | Taking compliance | 4 | <80 | 17 |
| Waeber and coworkers 35 | Taking compliance | 12 | <80 | 34 |
| Weidler and coworkers 36 | Taking compliance | 18 | <80 | 29 |
| Waeber and coworkers 37 | Correct dosing | 4 | ≤80 | 9 |
| Vaur and coworkers 38 | Correct dosing | 4–6 | ≤80 | 37 |
Adapted with permission from Wetzels et al. 19
Benefits of Good Adherence
Good treatment adherence has several benefits for both the patient and the health care system, as it is associated with improved BP control, 20 reduced risk of adverse CV outcomes, 21 and reduced all‐cause and hypertension‐related costs. 22
Improvements in BP and Goal Rate Achievement
Adherence is directly linked to favorable outcomes in a variety of chronic conditions. Good adherence in patients with hypertension has been associated with a decrease in the risk of a poor therapeutic outcome and an increase in BP control. 20
In a database analysis of patients with hypertension who were receiving ARB‐based therapy, it was shown that reductions in both systolic BP (SBP) and diastolic BP (DBP) were significantly greater in patients who were therapeutically adherent and persistent than in those who were not. 21 This increased effectiveness of therapy in adherent and persistent patients also has a beneficial effect on goal rate achievement. 20
Reductions in CV Risk and Hospital Admissions
The goal of hypertension treatment is to prevent CV complications that arise from elevated BP. Since poor adherence to treatment negatively affects BP, it follows that adherence will also affect the long‐term outcomes of antihypertensive therapy. This has been demonstrated in a number of studies, in which patients who were adherent to therapeutic regimens had a lower predicted relative risk of adverse CV outcomes compared with those who were non‐adherent. 21 , 22
Cost Benefits to Health Care Payers
Poor therapeutic outcomes associated with low adherence rates to antihypertensive therapy increase the total cost to the health care system. This was demonstrated in an analysis of paid claims data, using 1994 prices, examining data for patients with hypertension who were persistent or nonpersistent with prescribed drug regimens. Although nonpersistent patients saved the health care system $281 per patient per year, they incurred an additional $873 in other health care expenses (P<.0001 vs adherent patients). 23 Furthermore, patients who are <60% adherent to their therapeutic regimens have been shown to incur significantly higher (P<.05) all‐cause and hypertension‐related medical costs, compared with patients who are >80% adherent. 22
With benefits to BP lowering, BP goal achievement rates, long‐term clinical outcomes, and health care provider costs, it is clear that an integrated strategy to ensure and maintain good patient adherence and persistence is a cornerstone of effective hypertension therapy.
Strategies to Improve Adherence
Many methods to improve patient adherence have been shown to be beneficial. Strategies that utilize combinations of these methods are likely to have the greatest impact as part of a multifaceted approach. Several studies have shown that improving patient‐awareness of hypertension can increase adherence to therapy. This can be achieved by making the patient more aware of their BP levels, increasing patient understanding of the asymptomatic but chronic nature of the disease, motivating patients to take their treatment, and medical education programs for both patients and physicians. 24 , 25 Further approaches for improving patient adherence are presented in Table III.
Table III.
Methods to Increase Patient Adherence to Medication
| Inform the patient of the risk of hypertension and the benefits of effective treatment. |
| Provide clear written and oral instructions about treatment. |
| Tailor the treatment regimens to the patient’s lifestyle and needs. |
| Simplify treatment by reducing, if possible, the number of daily medications. |
| Involve patient’s partner or family in information on disease and treatment. |
| Make use of self‐measurement of blood pressure at home and of behavioral strategies such as reminder systems. |
| Pay great attention to side effects (even if subtle) and be prepared to timely change drug doses or type if needed. |
| Dialogue with patient regarding adherence and be informed of his/her problems. |
| Provide reliable support system and affordable prices. |
| Use telemonitoring system. 39 |
Adapted with permission from Mancia et al. 4
Treatment Regimen–Based Methods for Improving Adherence
A major strategy in improving adherence involves selecting the most appropriate antihypertensive therapy. In addition to the efficacy of the drug, physicians should also consider the tolerability and pharmacokinetic profile of antihypertensive agents, where drugs with long half‐lives may minimize the effects of missing single doses. 8
Combination Therapy as a Strategy
As discussed above, the tolerability profile of an antihypertensive agent plays a major role in determining adherence among patients. This is particularly relevant since most patients will require dose escalation or combination therapy to achieve goal BP. Since some agents are associated with dose‐dependent increases in side effects (Table I), combination therapy is often preferable to high‐dose monotherapy because it can increase efficacy without substantially increasing the risk of side effects and, therefore, has the potential to increase adherence relative to high‐dose monotherapy. 17
Selecting the right antihypertensive agents for combination therapy can be a difficult decision and may differ by patient, depending on the contraindications for certain agents. The current European guidelines recommend 6 preferred combinations (β‐blocker plus CCB, ARB plus thiazide diuretic, ACE inhibitor plus thiazide diuretic, CCB plus thiazide diuretic, ACE inhibitor plus CCB, and ARB plus CCB; Figure 1), all of which are supported by clinical data. 4 However, it should be noted that the role of β‐blockers in some combinations has been questioned due to recent data demonstrating the dyslipidemic and diabetogenic effects of β‐blockers when combined with thiazide diuretics, relative to other combinations. 4
The combination of an ACE inhibitor or ARB with a CCB is also endorsed by the current UK guidelines, which recommend therapy with an ACE inhibitor or ARB in combination with either a CCB or a thiazide diuretic—the so‐called A+C or A+D approach. 26 While the combination of an ACE inhibitor with the thiazide diuretic hydrochlorothiazide (HCTZ) has been shown to be an effective and well‐tolerated combination, interestingly the recent large‐scale Avoiding Cardiovascular Events Through Combination Therapy in Patients Living With Systolic Hypertension (ACCOMPLISH) trial showed that initial combination treatment with an ACE inhibitor plus a CCB was superior to an ACE inhibitor plus a thiazide diuretic for reducing CV morbidity and mortality in high‐risk patients. 27 Furthermore, in terms of tolerability and the potential for increased compliance, ONTARGET demonstrated that an ARB was associated with fewer adverse events than an ACE inhibitor while achieving equivalent efficacy. 18 It is likely, therefore, that future guideline recommendations may go further in advocating specific combinations of antihypertensive agents to reflect these findings.
Clinical Data With Combination Therapy
The thiazide diuretic HCTZ has been shown to be an effective component of combination therapy in a number of clinical trials. The addition of HCTZ to an ARB (valsartan) results in improved BP control in approximately 70% of patients treated with an ARB alone, 28 with up‐titration of the HCTZ dose being associated with additional benefits in DBP control without impairing tolerability profiles. 29 The coadministration of the ACE inhibitor enalapril with HCTZ resulted in greater DBP control than with either component in monotherapy and had comparable efficacy as the combination of losartan/HCTZ 30 and the β‐blocker metoprolol in combination with HCTZ. 31
The latest fixed‐dose combination to be approved is the ARB/CCB combination of olmesartan plus amlodipine. 5 , 32 This combination has been shown to be more effective than monotherapy with either agent for both BP reductions and BP goal achievement rates, 5 , 32 , 33 with SBP and DBP reductions of up to 30.1 and 19.0 mm Hg, respectively, after 8 weeks of treatment. 5
In addition to the advantages in terms of efficacy, combination therapy with an ARB and a CCB has advantages over CCB monotherapy in terms of the tolerability profile. Amlodipine‐related peripheral edema is a dose‐dependent side effect that may reduce adherence to amlodipine therapy, especially at higher doses. However, the level of edema is reduced by addition of an ARB to a CCB, 5 , 6 , 32 through a mechanism that is likely to be due to the complementary pharmacologic profiles of the two agents. The reduction in the risk of peripheral edema with ARB/CCB combination therapy, relative to CCB monotherapy, has the potential to increase adherence to this regimen.
The Rationale for Fixed‐Dose Combination Therapy
In addition to the improved efficacy and better tolerability profile associated with combination therapy relative to monotherapy, fixed‐dose combination therapy has advantages over separate‐dose combination therapy in terms of adherence. 4 Fixed‐dose combination therapy reduces the daily pill burden and regimen complexity, both of which have been associated with nonadherence to antihypertensive therapy. 7 The fixed‐dose combination of an ARB with a CCB is a promising new step in hypertension management that has the potential to increase patient adherence in addition to providing good antihypertensive efficacy and a favorable tolerability profile.
Conclusions
Hypertension is a chronic condition that is frequently inadequately managed with current antihypertensive treatments. Poor patient adherence to prescribed therapy is a major factor involved in this therapeutic failure. Treatment‐related factors that can cause low levels of adherence in clinical practice are suboptimal treatment tolerability profile and/or a high pill burden. Fixed‐dose combination therapy is recommended by current hypertension treatment guidelines and has the potential to provide well‐tolerated and highly efficacious antihypertensive therapy with a low pill burden.
Acknowledgment and disclosure: The author would like to thank Jackie Campbell of Wolters Kluwer Health (Chester, UK) who provided medical writing assistance funded by Daiichi‐Sankyo.
References
- 1. Ong KL, Cheung BM, Man YB, et al. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. [DOI] [PubMed] [Google Scholar]
- 2. European Society of Hypertension Scientific Newsletter: Update on Hypertension Management, How well is hypertension controlled in Europe? http://www.eshonline.org/education/newsletter.htm. Accessed July 28, 2008.
- 3. WHO . The World Health Report 2002: Risks to Health 2002. Geneva: WHO; 2002. [Google Scholar]
- 4. Mancia G, De Backer G, Dominiczak A, et al. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25:1105–1187. [DOI] [PubMed] [Google Scholar]
- 5. Chrysant S, Melino M, Karki S, et al. The combination of olmesartan medoxomil and amlodipine besylate in controlling high blood pressure: COACH, a randomized, double‐blind, placebo‐controlled, 8‐week factorial efficacy and safety study. Clin Ther. 2008;30:587–604. [DOI] [PubMed] [Google Scholar]
- 6. Philipp T, Smith TR, Glazer R, et al. Two multicenter, 8‐week, randomized, double‐blind, placebo‐controlled, parallel‐group studies evaluating the efficacy and tolerability of amlodipine and valsartan in combination and as monotherapy in adult patients with mild to moderate essential hypertension. Clin Ther. 2007;294:563–580. [DOI] [PubMed] [Google Scholar]
- 7. Burnier M. Medication adherence and persistence as the cornerstone of effective antihypertensive therapy. Am J Hypertens. 2006;19:1190–1196. [DOI] [PubMed] [Google Scholar]
- 8. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. [DOI] [PubMed] [Google Scholar]
- 9. Burnier M, Schneider MP, Chiolero A, et al. Electronic compliance monitoring in resistant hypertension: the basis for rational therapeutic decisions. J Hypertens. 2001;19:335–341. [DOI] [PubMed] [Google Scholar]
- 10. Richardson MA, Simons‐Morton B, Annegers JF. Effect of perceived barriers on compliance with antihypertensive medication. Health Educ Q. 1993;20:489–503. [DOI] [PubMed] [Google Scholar]
- 11. Vrijens B, Vincze G, Kristanto P, et al. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ. 2008;336:1114–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. DiMatteo MR, Sherbourne CD, Hays RD, et al. Physicians’ characteristics influence patients’ adherence to medical treatment: results from the Medical Outcomes Study. Health Psychol. 1993;12:93–102. [DOI] [PubMed] [Google Scholar]
- 13. Caro JJ, Payne K. Real‐world effectiveness of antihypertensive drugs. CMAJ. 2000;162:190–191. [PMC free article] [PubMed] [Google Scholar]
- 14. Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23:1296–1310. [DOI] [PubMed] [Google Scholar]
- 15. Van Wijk BL, Klungel OH, Heerdink ER, et al. Rate and determinants of 10‐year persistence with antihypertensive drugs. J Hypertens. 2005;23:2101–2107. [DOI] [PubMed] [Google Scholar]
- 16. Conlin PR, Gerth WC, Fox J, et al. Four‐year persistence patterns among patients initiating therapy with the angiotensin II receptor antagonist losartan versus other antihypertensive drug classes. Clin Ther. 2001;23:1999–2010. [DOI] [PubMed] [Google Scholar]
- 17. Law MR, Wald NJ, Morris JK, et al. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326:1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yusuf S, Teo KK, Pogue J, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547–1559. [DOI] [PubMed] [Google Scholar]
- 19. Wetzels GE, Nelemans P, Schouten JS, et al. Facts and fiction of poor compliance as a cause of inadequate blood pressure control: a systematic review. J Hypertens. 2004;22:1849–1855. [DOI] [PubMed] [Google Scholar]
- 20. Weir MR, Maibach EW, Bakris GL, et al. Implications of a health lifestyle and medication analysis for improving hypertension control. Arch Intern Med. 2000;160:481–490. [DOI] [PubMed] [Google Scholar]
- 21. Halpern MT, Vincze G, Stewart WF, et al. Persistence with hypertension therapy and long‐term cardiovascular outcomes. J Hypertens. 2006;24(suppl 4):S182. [Google Scholar]
- 22. Sokol MC, McGuigan KA, Verbrugge RR, et al. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–530. [DOI] [PubMed] [Google Scholar]
- 23. McCombs JS, Nichol MB, Newman CM, et al. The costs of interrupting antihypertensive drug therapy in a Medicaid population. Med Care. 1994;32:214–226. [DOI] [PubMed] [Google Scholar]
- 24. Szirmai LA, Arnold C, Farsang C. Improving control of hypertension by an integrated approach – results of the ‘Manage it well!’ programme. J Hypertens. 2005;23:203–211. [DOI] [PubMed] [Google Scholar]
- 25. Heisler M. Actively engaging patients in treatment decision making and monitoring as a strategy to improve hypertension outcomes in diabetes mellitus. Circulation. 2008;117:1355–1357. [DOI] [PubMed] [Google Scholar]
- 26. Sever P. New hypertension guidelines from the National Institute for Health and Clinical Excellence and the British Hypertension Society. J Renin Angiotensin Aldosterone Syst. 2006;7(2):61–63. [DOI] [PubMed] [Google Scholar]
- 27. Jamerson K, Weber MA, Bakris GL, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high‐risk patients. N Engl J Med. 2008;359:2417–2428. [DOI] [PubMed] [Google Scholar]
- 28. Chrysant SG. Fixed combination therapy of hypertension: focus on valsartan/hydrochlorothiazide combination (Diovan/HCT). Expert Rev Cardiovasc Ther. 2003;1:335–343. [DOI] [PubMed] [Google Scholar]
- 29. Fuenfstueck R, Hempel RD, Ansari A, et al. Efficacy and safety of combination therapy using high‐ or low‐dose hydrochlorothiazide with valsartan or other Angiotensin‐receptor blockers. Adv Ther. 2005;22:263–277. [DOI] [PubMed] [Google Scholar]
- 30. Siddiqui MA, Plosker GL. Fixed‐dose combination enalapril/nitrendipine: a review of its use in mild‐to‐moderate hypertension. Drugs. 2004;64:1135–1148. [DOI] [PubMed] [Google Scholar]
- 31. Materson BJ, Reda DJ, Cushman WC, et al. Single‐drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. N Engl J Med. 1993;328:914–921. [DOI] [PubMed] [Google Scholar]
- 32. Volpe M, Brommer P, Haag U, et al. Efficacy and tolerability of olmesartan medoxomil combined with amlodipine in patients with moderate to severe hypertension after amlodipine monotherapy: a randomized, double‐blind, parallel‐group, multicentre study. Clin Drug Investig. 2009;29:11–25. [DOI] [PubMed] [Google Scholar]
- 33. Barrios V, Brommer P, Haag U, et al. Olmesartan medoxomil plus amlodipine increases efficacy in patients with moderate‐to‐severe hypertension after monotherapy. Clin Drug Investig. 2009;29:427–439. [DOI] [PubMed] [Google Scholar]
- 34. Mallion JM, Dutrey‐Dupagne C, Vaur L, et al. Benefits of electronic pillboxes in evaluating treatment compliance of patients with mild to moderate hypertension. J Hypertens. 1996;14:137–144. [PubMed] [Google Scholar]
- 35. Waeber B, Vetter W, Darioli R, et al. Improved blood pressure control by monitoring compliance with antihypertensive therapy. Int J Clin Pract. 1999;53:37–38. [PubMed] [Google Scholar]
- 36. Weidler D, Wallin JD, Cook E, et al. Transdermal clonidine as an adjunct to enalapril: an evaluation of efficacy and patient compliance. J Clin Pharmacol. 1992;32:444–449. [DOI] [PubMed] [Google Scholar]
- 37. Waeber B, Erne P, Saxenhofer H, et al. Use of drugs with more than a twenty‐four‐hour duration of action. J Hypertens Suppl. 1994;12:S67–S71. [PubMed] [Google Scholar]
- 38. Vaur L, Vaisse B, Genes N, et al. Use of electronic pill boxes to assess risk of poor treatment compliance: results of a large‐scale trial. Am J Hypertens. 1999; 12(4 Pt 1): 374–380. [DOI] [PubMed] [Google Scholar]
- 39. Antonicelli R, Testarmata P, Spazzafumo L, et al. Impact of telemonitoring at home on the management of elderly patients with congestive heart failure. J Telemed Telecare. 2008;14:300–305. [DOI] [PubMed] [Google Scholar]


