Abstract
J Clin Hypertens (Greenwich). 2010;12:757‐764. © 2010 Wiley Periodicals, Inc.
Nonadherence and poor or no persistence in taking antihypertensive medications results in uncontrolled high blood pressure, poor clinical outcomes, and preventable health care costs. Factors associated with nonadherence are multilevel and relate not only to the patient, but also to the provider, health care system, health care organization, and community. National guideline committees have called for more aggressive approaches to implement strategies known to improve adherence and technologies known to enable changes at the systems level, including improved communication among providers and patients. Improvements in adherence and persistence are likely to be achieved by supporting patient self‐management, a team approach to patient care, technology‐supported office practice systems, better methods to measure adherence, and less clinical inertia. Integrating high blood pressure control into health care policies that emphasize and improve prevention and management of chronic illness remains a challenge. Four strategies are proposed: focusing on clinical outcomes; empowering informed, activated patients; developing prepared proactive practice teams; and advocating for health care policy reform. With hypertension remaining the most common reason for office visits, the time is now.
To achieve and maintain blood pressure (BP) control, two gaps must be closed: (1) between effective interventions in research studies and what clinicians do in practice, and (2) between what clinicians in their offices recommend to patients and what patients do at home and in their communities. Closing these gaps will require implementing health care practices and systems that guarantee continuity of care as well as integrate technology to support clinicians’ decision‐making and patients’ self‐management.
The Scope of the Problem
The most recent US survey data, obtained from randomly selected households, show that high BP awareness, treatment, and control rates have improved from 69%, 53%, and 26%, respectively, at the time of the 1988 to 1994 Nutrition Health and Examination Survey to 76%, 65%, and 37% between 2003 to 2004. 11 In a recent Harris Interactive survey, more than two thirds of patients with hypertension said they are aware of their high BP and are in care and 90% were on treatment. 37 Two major requirements for high BP control that are problematic include: (1) lack of effective provider response to uncontrolled BP, and (2) insufficient patient adherence to treatment recommendations. Despite the greater availability of effective antihypertensive agents, 65% of patients with hypertension receive the indicated care 28 and only 50% of patients for whom drug treatment is initiated persist on treatment 1 year later. 61
Terminology, definitions, and understanding of the behavioral aspects of high BP control have changed over time. The term compliance has been defined as “the extent to which the patient’s behavior coincides with the clinical prescription,” implying that the patient defaults by not following health care providers’ advice. 18 Concordance refers to the process of discussion between health care professionals and patients to reach agreement about the treatment plan and the patient’s use of prescribed medicines. The term adherence, which is widely used now, refers to a complex interplay among patient, provider, and health care system: “a behavioral process, strongly influenced by the environment in which patients live, health care providers practice, and health care systems deliver care.” Adherence assumes that a patient has the knowledge, motivation, skills, and resources required to follow the recommendations of a health care professional. 32 More recently, World Health Organization (WHO) 49 defined adherence as “the extent to which a person’s behaviour—taking medication, following a diet, and/or executing lifestyle changes—corresponds with agreed recommendations from a health care provider.” The term persistence refers to the length of time during which the patient continues to be engaged with the prescribed dosing regimen.
Adherence and persistence are intrinsically linked. In a landmark study, Vrijens and colleagues 61 analyzed dosing histories of 4783 patients with hypertension using electronic monitoring (Figure 1). They divided adherence into 2 main components: discontinuation of treatment and poor execution of the dosing regimen. At 1 year, only 50% of patients were persistent with their prescribed antihypertensive regimen, and nonexecution, the proportion of doses omitted on each day of treatment, was 10% (Figure 1). Although much of the research on compliance cites rates as low as 50%, reports of treated populations describe compliance rates of 70% to 80% in uncontrolled populations and slightly higher rates in controlled populations. Thus, the challenge is for clinicians to tailor the regimen to obtain and maintain optimal levels of BP control and address the importance of adherence and persistence in patients on drug therapy.
Figure 1.
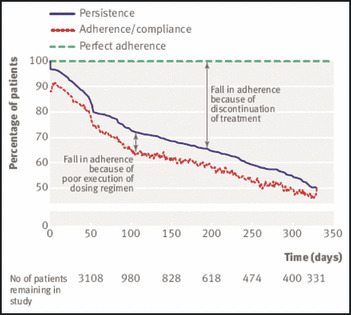
Time course of adherence/compliance parameters (execution, persistence). From Vrijens and colleagues. 61
The consequences of nonadherence are serious because of the resulting poor clinical outcomes and preventable health care costs. Results from a meta‐analysis by DiMatteo and colleagues 13 showed a 27% difference in clinical outcome between patients with low vs high adherence. Cherry and colleagues 7 assessed the benefit of “ideal” over “typical” adherence in patients with hypertension and hyperlipidemia and found a nearly double relative risk (13.3 vs 25 events per 100 patient‐years over 3 years) of myocardial infarction, angina, and stroke in patients who showed no adherence vs those who showed ideal adherence.
The factors that contribute to insufficient adherence and persistence with taking antihypertensive medications are multilevel and extend beyond patient and provider levels. 32 The WHO, 49 in a 2003 report on long‐term adherence, identified 5 important sets of factors: social and economic factors, condition‐related factors, therapy‐related factors, patient‐related factors, and health care system/health care team–related factors. The importance of the latter set of factors is undervalued. For well‐intentioned clinicians and patients to achieve and maintain BP control over years it is critical to consider the health care organizations and delivery systems within which clinicians practice and the communities within which patients live. 29 , 32 For instance, wide variability exists in view of access to care among health care systems. A recent Commonwealth survey 51 showed that cost‐related medication nonadherence ranged from 3% in the Netherlands to 43% in the United States.
Scientific Background
The scientific evidence to support the preceding statement of the problem comes from epidemiology, clinical trials, behavioral science and health services research, and systematic reviews. The original VA trial, the first to show the efficacy of oral medication to lower BP and reduce fatal complications of uncontrolled hypertension, was conducted in a hospital setting where a nursing staff initially directly administered antihypertensive medications to patients. After discharge, compliance was assessed by pill counts and a urine marker. 60 Subsequent trials, such as the Multiple Risk Factor Intervention Trial (MRFIT), the Hypertension Detection and Follow‐up Program (HDFP), the Systolic Hypertension in the Elderly Program (SHEP), and more recently the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), illustrated that improvements in BP control and patient outcomes could be achieved in ambulatory care and community settings with good, if not perfect, adherence to medication recommendations and BP control rates. 1 , 20 , 21 , 38 , 54 , 57
Early studies of interventions to improve BP control focused on patient and provider education. 15 , 20 , 21 , 54 The initial assumption was that increasing patient knowledge of the importance of controlling high BP would lead to improved adherence and persistence. However, patient attitudes, beliefs, and social support, in addition to behavioral strategies to tailor and simplify the regimen, and prompt and remind the patient to take the medication as prescribed, were also shown to contribute to improved BP control. Importantly, forgetting, ie, not remembering, has been found to be the most common reason for patients not taking medication. 18 , 59 Other barriers to BP control such as cost of care and medication, lack of insurance and transportation, convenience, and comorbidities including depression, also contribute to medication nonadherence and lack of persistence. 14 , 15 , 23 , 62
From the late 1960s, continuing medical education and high BP practice guidelines focused on the role of the physician in diagnosis, evaluation, and treatment, particularly in the selection of appropriate pharmacologic classes and agents. In 1972, the National Institutes of Health National Heart, Lung, and Blood Institute established the National High Blood Pressure Education Program (NHBPEP) to work with professional societies and voluntary health organizations to improve high BP diagnosis, treatment, and control. The NHBPEP Coordinating Committee membership grew to 39 national professional, public, and voluntary health organizations including the American Heart Association, the American Society of Hypertension (ASH), and 7 federal agencies. In 1976, the NHBPEP Coordinating Committee began to publish a series of consensus guidelines entitled the Report of the Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure. 8 The eighth report is now being written. The NHBPEP also conducted national campaigns to increase public awareness of high BP and the importance of screening, follow‐up, and treatment to goal BP. 46 In parallel, and continuing today, professional societies and/or pharmaceutical companies develop their own guidelines often focusing on subpopulations of patients, such as the patient with hypertension and diabetes (ASH), or Calls to Action 2 , 43 to motivate renewed attention to controlling high BP and preventing its complications.
The early JNC reports primarily focused on the physician’s role in the workup of hypertension and selection of the appropriate pharmaceutical agent(s) with which to initiate therapy. Little information was provided on how to improve physicians’ and other health professionals’ counseling skills to help patients improve adherence and persistence. Also little information was provided on how to optimize practice and office arrangements and organization or on how to improve overall care processes to achieve optimal BP control. The importance of psychosocial and behavioral aspects of the patient’s role in entering and remaining in care and achieving the desired treatment outcome, while not substantively addressed in the JNC reports, was addressed in several articles and reports published by the NHBPEP. An important early example, Critical Patient Behavior for Blood Pressure Control: Guidelines for Professionals, published in 1979, emphasized that “the patient is in charge,” and recommended that clinicians help patients to: (1) achieve goal BP, (2) take medication as recommended, (3) monitor progress toward goal BP, and (4) resolve problems blocking progress toward goal. 65 Subsequent evidence showed that the quality of the patient‐provider relationship, including the way health care providers communicate and build trust with patients, related to favorable adherence patterns among chronically ill patients. 9 , 22 , 44 , 45 , 56 The risk for nonadherence is 19% higher in patients whose physician communicates poorly compared with patients whose physician communicates well. 66 The term physician inertia, used to describe poor adherence to guidelines by providers in the presence of uncontrolled BP on repeated return visits, has been shown to significantly contribute to suboptimal BP control rates in treated patients. 3 , 47 An additional cornerstone that contributes to improved adherence and persistence is the extent to which patients actively participate in self‐monitoring of their BP and clinicians provide feedback to them. 43
Adherence should be monitored as an important clinical parameter. The importance of new methods to increase valid and reliable measurement of adherence beyond self‐report and pill counts has been long recognized as a challenge. 26 , 36 , 58 While these methods are feasible and affordable they are flawed by recall bias, social desirability of response, and single‐point estimation. The accurate assessment of medication taking has been improved by the introduction of computerized records of pharmacy prescription refills and electronic monitoring, which provides evidence of dynamics of medication‐taking behavior such as drug holidays. 42 Urquhart found that based on unobtrusive electronic medication monitoring patients could be divided into 6 groups based on their medication‐taking behaviors: One sixth execute the regimen with strict punctuality; one sixth take all prescribed doses but have some fluctuations in dose timing, one sixth omit a single day’s dose with fluctuations in dose timing, one sixth have a drug holiday (the sequential omission of 3 or more day’s doses) 3 to 4 times per year, one sixth have a drug holiday monthly or more often with frequent omissions of 1 to 2 day’s doses, and one sixth take few or no doses while maintaining the appearance of satisfactory adherence. 58 The ability to categorize patient behaviors, understand the pharmacokinetics of drug absorption, and pharmionics, which includes failure of medicines to be taken in appropriate doses and timing adds to our understanding of nonadherence, nonabsorption, and nonresponse. The use of this categorization, however, is limited to individuals that were part of drug studies primarily in Europe. Further testing is needed to determine the value of categorizing individuals into these 6 groups and implementing effective tailored interventions.
Assessing adherence and executing adherence‐enhancing interventions requires health care providers to be trained in these skills. An internet poll on Medscape in conjunction with the paper by Cherry and colleagues 7 asked: “How confident are you that you are up‐to‐date in the most effective strategies for reducing treatment nonadherence among patients with hypertension and hyperlipidemia?” Twenty percent of the respondents stated not at all confident, 59% somewhat confident, 17% confident, and only 2% very confident. 16 This and other research provides evidence of the importance of providers developing skills to effectively communicate and counsel patients, such as: (1) providing clear, direct messages about the importance of adherence behaviors; (2) including patients in decisions regarding treatment goals and related strategies; and (3) incorporating behavioral strategies such as listening actively, tailoring strategies to each patient, anticipating and discussing potential barriers to adherence, and working with the patient to develop multidimensional strategies to overcome them. 19 , 32 , 40 , 48 , 49 The principles of motivational interviewing 35 have been shown to facilitate a communication style that fosters a collaborative partnership with the patient and supports self‐management.
An increasing number of systematic reviews of evidence‐based interventions to improve medication adherence have been published including Cochrane systematic reviews. 19 , 27 , 50 , 53 , 64 The Schedlbauer review evaluated the efficacy of computerized drug alerts and prompts on clinicians’ prescribing behavior and found that most (23 of 27) improved prescribing behavior and/or reduced error rates. The Haynes review identified 18,867 citations, of which 1020 met criteria for assessment of both adherence and clinical outcome. Of these, 82 met all review criteria testing 93 unconfounded interventions. Twelve studies were of hypertension. The effectiveness of interventions was found in general conditions in 83 randomized clinical trials (RCTs) with 36 (43%) showing improved adherence and 32 (38.6% or 89% of hypertension trials) improved clinical outcomes. Schroeder and colleagues 52 , 53 found 58 RCTs on hypertension with 19 (37%) showing improved adherence and 13 of 43 (30%) showing improved clinical outcomes. However, these studies lacked homogeneity in measurement of adherence, the population sampled, setting, intervention, duration of study, and consideration of regimens. Nonetheless, the characteristics of effective adherence interventions summarized by the reviews include: (1) simplification of the regimen; (2) information and education; (3) intensified care (monitoring, telephone follow‐up, reminders, home visits, social support, computer‐aided counseling and packaging); (4) group sessions; and (5) complex interventions (behavioral training, worksite and pharmacy‐based programs, and combinations of strategies).
For more than 30 years, numerous studies have provided increasing and consistent evidence that changing systems of care positively impacts outcomes. More specifically, the safety and efficacy of alternative and/or complimentary models of care, particularly nurse‐run clinics, nurse case management, a team approach to care, and pharmacy‐based counseling and other community‐based monitoring and care sites have shown documented benefits in improving BP control most often through closer follow‐up of individuals and closer adherence to guidelines. These models of care have resulted in a decrease in drug interactions, improvement in adherence, and lower patient costs. Restructuring the health care delivery system to include and reimburse these models of care is likely to improve adherence and BP control. 6 , 10 , 12 , 33 , 34
Until recently, few studies examined the impact of practice and office arrangements and organization of how office practices are managed on achievement of BP control. In 1996, Ockene and colleagues 39 demonstrated that fostering effective communication with the patient, and documenting and responding to patient progress toward goals, improved patients’ medication adherence. Specifically, they demonstrated the value of providers who develop the skills to assess adherence at each visit and use reminder systems to ensure reliable identification and follow‐up of the patients’ status. This work demonstrated the need for health care organizations to invest in care systems designed to support patient self‐management within a chronic illness care model. Health services research studies, including those documenting the effect of system‐level interventions to reduce health disparities, are providing needed empirical evidence about organizational strategies to improve outcomes. Many require information technology applications, electronic medical records, and personal health records to facilitate better systems’ approaches to care. Studies examining the delivery of care, and the extent to which guidelines are implemented and outcomes are achieved, especially among ethnic and minority groups, have become prevalent. 3 , 4 , 17 , 24 , 25 , 30 , 31 , 41 , 55
In the past decade, as national policy attention has increasingly been paid to the need to improve the safety and quality of care and patient outcomes, health services research has grown in importance. Figure 2 illustrates Wagner and colleagues’ model of productive interactions that improve functional and clinical outcomes. 5 The following recommendations are made to advance progress toward this end.
Figure 2.
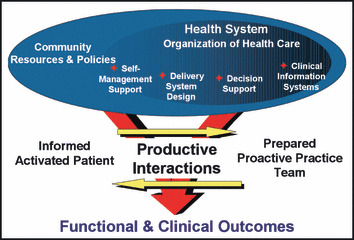
Interventions that improve outcomes. From Wagner and colleagues. 63
Practical Considerations and Recommendations
There is clear potential to improve clinical outcomes by improving adherence and persistence with appropriate antihypertensive medications. It is essential that 4 strategies to maintain high BP control be integrated into effective health care policies that emphasize and improve prevention and management of chronic illness. (see Table)
Table.
Practical Considerations and Recommendations for Adherence
| Focus on clinical outcomes |
| Initiate medications according to national guidelines |
| Keep the regimen simple: once‐/twice‐a‐day dosing |
| Re‐evaluate all uncontrolled blood pressures (BPs) |
| Communicate with patients about taking medications as directed |
| Encourage self‐monitoring of BP |
| Use technologies (eg, e‐mail) to monitor progress and maintenance of goal BP’s |
| Empower informed activated patients |
| Assess patient knowledge, skills, behaviors, confidence and barriers to adherence |
| Encourage problem‐solving and behavior change interventions |
| Urge the use of pill boxes for daily use |
| Help patients develop a system for refilling prescriptions |
| Implement a team approach |
| Implement a collaborative model based on a team approach |
| Apply office practice policies and procedures to improve BP control |
| Support self‐management and problem prevention |
| Advocate for health policy reform |
| Elevate medication adherence as a critical healthcare issue |
| Develop policies to support prevention and chronic illness management including self‐management |
| Structure/finance healthcare that stimulates behavioral aspects of care in communities |
| Seek regulatory changes to improve the use of home BP monitors |
Focus on the Clinical Outcomes
-
•
Initiate medication according to national guidelines, modifying as indicated for patient characteristics (including ability to pay) and adjust the regimen until goal BP is achieved.
-
•
Stress the importance of maintaining goal BP over time—a lifetime.
-
•
Keep the regimen as simple as possible with once‐ or twice‐daily dosing.
-
•
Re‐evaluate uncontrolled BP and review all treatment options with the patient.
-
•
Monitor adherence as an important clinical parameter.
-
•
Communicate consistently and proactively with patients about the importance of their taking the medication as recommended.
-
•
Encourage self‐monitoring of BP.
-
•
Use e‐mail and other technologies to stay in touch with patients and provide feedback on progress toward and maintenance of goal BP.
Empower Informed, Activated Patients
-
•
Emphasize the patient’s central role in caring for themselves.
-
•
Assess patient’s knowledge, skills, behaviors, confidence, and barriers to adherence.
-
•
Help patients identify and resolve problems that interfere with maintaining BP control.
-
•
Encourage effective behavior change interventions and assure collaborative care‐planning and problem‐solving.
-
•
Strongly urge patients to use a pill box to organize all daily and weekly medications, as the most common reason for not taking medication is forgetting due to being distracted by daily hassles and disruption of daily routines.
-
•
Help patients implement an effective strategy for refilling prescriptions before running out of medication.
-
•
Monitor the cost of medications and patients’ ability to pay for them.
Implement a Team Approach
-
•
Provide collaborative care, based on close cooperation among patients, physicians, nurses, pharmacists, and allied health professionals within a chronic illness management paradigm. 5
-
•
Implement a team approach to delivering evidence‐based care that is patient‐centered and assist patients with self‐management.
-
•
Develop office practice policies and procedures that use technology to improve communication, documentation, and tracking of BPs.
-
•
Be proactive to rapidly and efficiently incorporate technology in clinical practice systems (ie, prompts, algorithms, and screening and follow‐up for specific actions such as missed appointments).
-
•
Support self‐management and problem prevention as part of a chronic illness management model.
Advocate for Health Policy Reform
Advocate for policies and regulations to: (1) elevate awareness that medication adherence is a critical health care issue; (2) develop and integrate policies that support prevention and chronic illness management including patient self‐management and adherence to medication regimens; (3) support the structure and finance of health care that stimulates interest in behavioral aspects of care in communities; (4) seek regulatory changes to remove roadblocks for patient self‐management such as the use of home BP monitors and reimbursement for monitoring such data; and (5) evaluate strategies to increase provider and patient adherence to evidence‐based guidelines, such as pay‐for‐performance and self‐monitoring.
Acknowledgments
Acknowledgments and disclosures: This article was reviewed by David J. Hyman, MD, MPH, and Donald E. Morisky, ScD, MSPH, ScM. The American Society of Hypertension Writing Group Steering Committee: Barry J. Materson, MD, MBA, Chair; Henry R. Black, MD; Joseph L. Izzo, Jr, MD; Suzanne Oparil, MD; and Michael A. Weber, MD. Nancy H. Miller is a consultant for Boehringer Ingelheim and AstraZeneca. Martha Hill, RN, PhD and Sabina DeGeest, RN, PhD have nothing to disclose.
References
- 1. The ALLHAT officers and coordinators for the ALLHAT Collaborative Research Group . Major outcomes in high‐risk hypertensives patients randomized to angiotensin‐converting enzymes inhibitor or calcium‐channel blocker versus diuretic: the Antihypertensive and Lipid‐lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002; 288: 2981–2997. [DOI] [PubMed] [Google Scholar]
- 2. Bakris G, Hill M, Mancia G, et al. Achieving blood pressure control goals globally: five core actions for health‐care professionals. A world‐wide call to action. J Hum Hypertens. 2008;22:63–70. [DOI] [PubMed] [Google Scholar]
- 3. Berlowitz DR, Aash AS, Hickey EC, et al. Infrequent management of blood pressure in a hypertensive population. N Engl J Med. 1998;339:1957–1963. [DOI] [PubMed] [Google Scholar]
- 4. Bramley TJ, Gerbino PP, Nightengale BS, Frech‐Tamas F. Relationship of blood pressure control to adherence with antihypertensive monotherapy in 13 managed care organization. J Manag Care Pharm. 2006;12:239–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002;288(15):1909–1914. [DOI] [PubMed] [Google Scholar]
- 6. Carter BL, Zillich AJ, Elliott WJ. How pharmacists can assist physicians with controlling BP. J Clin Hypertens. 2003;5:31–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cherry SB, Benner JS, Hussein Ma, et al. The clinical and economic burden of nonadherence with antihypertensive and lipid‐lowering therapy in hypertensive patients. Value Health. 2009;12:489–497. [DOI] [PubMed] [Google Scholar]
- 8. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on prevention, detection, evaluation and treatment of high blood pressure. Hypertension. 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 9. Cooper LA. A 41‐year‐old African American man with poorly controlled hypertension: review of patient and physician factors related to hypertension treatment adherence. JAMA. 2009;301(12):1260–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Curzio JL, Beevers M. The role of nurses in hypertension care and research. J Hum Hypertens. 1997;11:541–550. [DOI] [PubMed] [Google Scholar]
- 11. Cutler JA, Sorlie PD, Wolz M, et al. Trends in hypertension prevalence, awareness, treatment and control rates in the United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–827. [DOI] [PubMed] [Google Scholar]
- 12. Dennison C, Post WS, Kim MT, et al. Underserved urban African American men: hypertension trial outcomes and mortality during 5 years. Am J Hypertens. 2007;20:164–171. [DOI] [PubMed] [Google Scholar]
- 13. DiMatteo MR, Giordani PJ, Lepper HS, et al. Patient adherence and medical treatment outcomes: a meta‐analysis. Med Care. 2002;40:794–811. [DOI] [PubMed] [Google Scholar]
- 14. Dunbar‐Jacobs J, Dwyer K, Dunning R. Compliance with antihypertensive regimen: a review of the research in the 1980s. Ann Behav Med. 1991;3:31–39. [Google Scholar]
- 15. Hill MN. Strategies for patient education. Clinical Exp Hypertens. 1989;11:1187–1201. [DOI] [PubMed] [Google Scholar]
- 16. Foody J. Medication adherence: America’s other drug problem. Available at: http://www.medscape.com/viewarticle/549907.
- 17. Fung V, Huang J, Brand R, et al. Hypertension treatment in a medicare population: adherence and SBP control. Clin Ther. 2007;29:972–984. [DOI] [PubMed] [Google Scholar]
- 18. Haynes RB, Taylor DW, Sackert DL, eds. Compliance in Health Care. Baltimore, MD: Johns Hopkins University Press; 1979. [Google Scholar]
- 19. Haynes RB, Ackloo E, Sahota N, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008; (2):CD000011. Brief record. [DOI] [PubMed] [Google Scholar]
- 20. Hypertension Detection and Follow‐up Program Cooperative Group . Five year findings of the Hypertension Detection and Follow‐up Program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. JAMA. 1979;242:2562–2571. [PubMed] [Google Scholar]
- 21. Hypertension Detection and Follow‐up Program Cooperative Group . Five year findings of the Hypertension Detection and Follow‐up Program. II. Mortality by race‐sex and age. JAMA. 1979;242:2572–2577. [DOI] [PubMed] [Google Scholar]
- 22. Heisler M, Wagner TH, Piette JD. Patient strategies to cope with high prescription medication costs: who is cutting back on necessities, increasing debt, or underusing medications? J Behav Med. 2005;28:43–51. [DOI] [PubMed] [Google Scholar]
- 23. Hill MN, Bone LR, Levine DM. Community outreach. In: Oparil S, Weber M, eds. Hypertension, 2nd edn. Philadelphia, PA: Elsevier Saunders; 2005:423–429. [Google Scholar]
- 24. Hyman DJ, Pavlik VN. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med. 2001;345:479–486. [DOI] [PubMed] [Google Scholar]
- 25. Hyman DJ, Pavlik VN. Poor hypertension control: let’s stop blaming patients. Cleve Clin J Med. 2002;69:793–799. [DOI] [PubMed] [Google Scholar]
- 26. Kim MT, Hill MN, Bone LR, et al. Development and testing of the Hill‐Bone Compliance to High Blood Pressure Therapy Scale. Prog Cardiovasc Nurs. 2000;15:90–96. [DOI] [PubMed] [Google Scholar]
- 27. Kripalani Yao X, Haynes B. Interventions to enhance medication adherence in chronic medical conditions. A systematic review. Arch Intern Med. 2007;167:540–550. [DOI] [PubMed] [Google Scholar]
- 28. McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. [DOI] [PubMed] [Google Scholar]
- 29. McLeroy KR, Bibeau D, Steckler A, et al. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. [DOI] [PubMed] [Google Scholar]
- 30. Milchak JL, Carter BL, Ardery G, et al. Development of explicit criteria to measure adherence to hypertension guidelines. J Hum Hypertens. 2006;20:426–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Milchak JL, Carter BL, James PA, et al. Physician adherence to JNC 7 guidelines and blood pressure control. Am J Hypertens. 2005;18:190A–190A. [Google Scholar]
- 32. Miller NH, Hill MN, Kottke T, et al. The multilevel compliance challenge: Recommendations for a call to action. Circulation. 1997;95:1085–1090. [DOI] [PubMed] [Google Scholar]
- 33. Miller NH, Hill MN. Non‐physician providers and the Management of Hypertension. In: Izzo JL, Black HR, eds. Hypertension Primer, 3rd ed. Dallas, TX: American Heart Association; 2003:399–401. [Google Scholar]
- 34. Miller NH, Hill MN. Nursing clinics in the management of hypertension. In Oparil S, Weber M, eds. Hypertension, 2nd edn. Philadephia, PA: Elsevier Saunders; 2005:416–422. [Google Scholar]
- 35. Miller WR, Rollnick S. Motivational Interviewing Preparing People for Change, 2nd edn. New York, NY: The Guilford Press; 2002. [Google Scholar]
- 36. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self‐reported measure of medication adherence. Med Care. 1986;24:67–74. [DOI] [PubMed] [Google Scholar]
- 37. Moser M, Franklin SS. Hypertension management: results of a new national survey for the hypertension education foundation: Harris interactive. J Clin Hypertens. 2007;5:316–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Multiple Risk Factor Intervention Trial Research Group . Multiple risk factor intervention trial: risk factor changes and mortality results. JAMA. 1982;248:1465–1477. [PubMed] [Google Scholar]
- 39. Ockene IS, Hebert JR, Ockene JK, et al. Effect of training and a structured office practice on physician‐delivered nutrition counseling: the Worcester‐Area trial for counseling on hyperlipidemia (WATCH). Am J Prev Med. 1996;12:252–258. [PubMed] [Google Scholar]
- 40. Ockene IS, Hayman LL, Pasternack RC, et al. Task force #4 – adherence issues and behavior changes: achieving a long‐term solution. 33rd Bethesda Conference. J Am Coll Cardiol. 2002;40(4):630–640. [DOI] [PubMed] [Google Scholar]
- 41. Oliveria SA, Chen RS, McCarthy BD, et al. Hypertension knowledge, awareness, and attitudes in a hypertension population. J Gen Intern Med. 2005;20(3):219–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. [DOI] [PubMed] [Google Scholar]
- 43. Pickering TP, Houston Miller N, Ogedegbe G, et al. Call to action on use and reimbursement for home blood pressure monitoring. A joint statement by the American Heart Association, American Diabetes Association, and the Preventive Cardiovascular Nurses Association. Hypertension. 2008;52:1–9. [DOI] [PubMed] [Google Scholar]
- 44. Piette JD, Heisler M, Horne R, et al. A conceptually based approach to understanding chronically ill patients’ response to medication cost pressures. Soc Sci Med. 2006;62:846–857. [DOI] [PubMed] [Google Scholar]
- 45. Piette JD, Heisler M, Krein S, et al. The role of the patient‐physician trust in moderating medication nonadherence due to cost pressures. Arch Intern Med. 2005;165:1749–1755. [DOI] [PubMed] [Google Scholar]
- 46. Roccella EJ. The National High Blood Pressure Education Program. In: Oparil S, Weber M, eds. Hypertension, 2nd ed. Philadelphia, PA: Elsevier Saunders; 2005:7–15. [Google Scholar]
- 47. Rose AJ, Berlowitz DR, Orner MB, et al. Understanding uncontrolled hypertension: is it the patient or provider? J Clin Hypertens. 2007;12:937–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Dennison CR, Miller NH. Adherence to antihypertensive therapy. In: Izzo JL, Sica DA, Black HR, eds. Hypertension Primer: The Essentials of High Blood Pressure, 4th ed. Pennsylvania: Lippincott Williams & Wilkins: 2008:413–417. [Google Scholar]
- 49. Sabate E, et al. Adherence to Long‐Term Therapies: Evidence for Action. Geneva, Switzerland: World Health Organization; 2003. [PubMed] [Google Scholar]
- 50. Schedlbauer A, Prasad V, Mulvaney C, et al. What evidence supports the use of computerized alerts and prompts to improve clinicians’ prescribing behavior? J Am Med Inform Assoc. 2009;16(4):531–538. Epub 2009 Apr 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Schoen C, Osborn R, Doty MM, et al. A survey of primary care physicians in eleven countries, 2009: perspectives on care, costs, and experiences. Health Aff (Millwood). 2009;28(6):w1171–w1173. Epub 2009 Nov 2. [DOI] [PubMed] [Google Scholar]
- 52. Fahey T, Schroeder K, Ebrahim S. Interventions used to improve blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2006;(2):CD005182. Review. [DOI] [PubMed]
- 53. Schroeder K, Fahey T, Ebrahim S. Interventions for improving adherence to treatment in patients with high blood pressure in ambulatory settings. Cochrane Database Syst Rev. 2004; (2):CD004804. Review [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. SHEP Cooperative Research Group . Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. JAMA. 1991;265:3255–3264. [PubMed] [Google Scholar]
- 55. Singer GM, Izhar M, Black HR. Goal‐oriented hypertension management: translating clinical trials to practice. Hypertension. 2002;40:464–469. [DOI] [PubMed] [Google Scholar]
- 56. Stewart M, Brown JB, Boon H, et al. Evidence on patient‐doctor communication. Cancer Prev Control. 1999;3:25–30. [PubMed] [Google Scholar]
- 57. The Trials of Hypertension Prevention Collaborative Research Group . The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels. Results of the Trials of Hypertension Prevention, Phase I. JAMA. 1992;267:1213–1220. [DOI] [PubMed] [Google Scholar]
- 58. Urquhart J. The odds of the three nons when an aptly prescribed medicine isn’t working: noncompliance, non‐absorption, non‐response. Br J Clin Pharmacol. 2002;54:212–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Vawter L, Tong X, Gemilyan M, et al. Barriers to antihypertensive medication adherence among adults – United States, 2005. J Clin Hypertens (Greenwich). 2008;10(12):922–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Veterans Administration Cooperative Study Group on Antihypertensive Agents . Effects of treatment on morbidity in hypertension: results in patients with diastolic blood pressures averaging 115 through 129 mm Hg. JAMA. 1967;202(11):1028–1034. [PubMed] [Google Scholar]
- 61. Vrijens B, Vincze G, Kristano P, et al. Adherence to prescribed anti‐hypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ. 2008;336:1114–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Wagner TH, Heisler M, Piette JD. Prescription drug co‐payments and cost‐related medication underuse. Health Econ Policy Law. 2008;3:51–67. [DOI] [PubMed] [Google Scholar]
- 63. Wagner EH, Davis C, Schaefer J, et al. A survey of leading chronic disease management programs: are they consistent with the literature? Manag Care Q. 1999;7(3):56–66. [PubMed] [Google Scholar]
- 64. Wetzels GE, et al. Facts and fiction of poor compliance as a cause of inadequate blood pressure control: a systematic review. J Hypertens. 2004;10:1849–1855. [DOI] [PubMed] [Google Scholar]
- 65. Working Group to Define Critical Patient Behaviors in High Blood Pressure Control (National High Blood Pressure Education Program, National Heart, Lung, and Blood Institute) . Patient behavior for blood pressure control. JAMA. 1979;241(23):2534–2537. [DOI] [PubMed] [Google Scholar]
- 66. Zolnierek KB, DiMatteo MR. Physician communication and patient adherence to treatment: a meta‐analysis. Med Care. 2009;47(8):826–834. [DOI] [PMC free article] [PubMed] [Google Scholar]


