Abstract
J Clin Hypertens (Greenwich).
This study compared the prevalence of high‐risk cardiovascular (CV) conditions, antihypertensive medication treatment patterns, and demographic and clinical characteristics associated with blood pressure (BP) goal attainment between elderly (65 years and older) and nonelderly (younger than 65 years) adults with hypertension. Retrospective cohort study was conducted using an electronic medical record database among patients receiving at least 1 antihypertensive medication. CV risk profiles were assessed by International Classification of Diseases, 9th Revision diagnosis codes. Treatment patterns were assessed by the number of antihypertensive medications prescribed. BP goal attainment was determined by the mean of the last 2 BP readings during 1 year of follow‐up. Logistic regression estimated the odds of achieving BP goal. There were 61,355 nonelderly (mean age, 51.8 years) and 47,796 elderly (mean age, 73.2 years) patients in the study. Elderly patients had statistically significant higher levels of isolated systolic hypertension and complicated hypertension. Elderly patients had statistically significant higher levels of prescribing patterns characterized by multiple antihypertensive medications but statistically significant lower levels of BP goal attainment. Age 65 years and older, African American race, body mass index ≥30, and the presence of complicated hypertension were found to be statistically significant factors contributing to a lower likelihood of BP goal attainment. Despite aggressive antihypertensive treatment, elderly patients are less likely to achieve BP goals. J Clin Hypertens (Greenwich). 2010;12:935–944. © 2010 Wiley Periodicals, Inc.
Hypertension, broadly defined as blood pressure (BP) ≥140/90 mm Hg, affects approximately 73 million people in the United States, and there is a 90% lifetime risk of developing hypertension for persons 55 years and older. 1 Hypertension is the most common chronic condition for which Americans visit a doctor and it is increasing in prevalence as the population ages and body mass indices (BMIs) increase. 2 The World Health Organization states that hypertension is the most common attributable cause of preventable death in developed countries. 2 Among individuals with hypertension, 61.4% are receiving antihypertensive treatment and about 35% have controlled hypertension; therefore, as many as 65% of hypertensive patients do not attain adequate BP control. 1
Many antihypertensive agents are available to allow effective reduction of high BP and its associated complications for all ages. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC 7) and other literature recommends that elevated BP be reduced to <140/90 mm Hg (or <130/80 mm Hg for patients with diabetes and chronic kidney disease) and that most patients with hypertension require ≥2 antihypertensive medications to achieve target BP. It is now recognized that multiple‐mechanism therapy results in greater BP reduction than is seen with single‐mechanism components. 3 , 4 , 5 , 6 , 7 JNC 7 also acknowledges that hypertension commonly occurs in more than two thirds of adults older than 65 years. Treatment recommendations in the elderly population should follow the same principles as for the general population, with the only caution that lower starting doses may be necessary to avoid adverse events. As in the general population, standard doses and multiple therapies are needed to attain BP goals. Previous research has found that elderly patients with hypertension are treated less aggressively than their younger counterparts and have lower rates of BP control. 8 , 9
This study was undertaken to assess whether elderly patients with hypertension have different underlying clinical characteristics than nonelderly patients with hypertension that may explain variations in antihypertensive therapy and BP goal attainment. Therefore, the objectives of this study are: (1) to describe the prevalence of high‐risk CV conditions among adults with hypertension, comparing patients 65 years and older with those younger than 65 years; (2) to describe the antihypertensive medication use and BP goal attainment among those with stage I and II hypertension, comparing patients 65 years and older with those younger than 65 years; and (3) to assess those factors associated with BP goal attainment. The data source for this study was an electronic medical record (EMR) database of patients seeking care and treatment in the outpatient setting.
Methods
Data Source
This study used data from GE Centricity (GE Healthcare, GE Healthcare IT, Princeton, NJ) a de‐identified Health Insurance Portability and Accountability Act of 1996 (HIPPA)–compliant EMR database. At the time of the study (2007), the EMR contained data on more than 8.9 million patients. The GE EMR database is comprised of data submitted by more than 70 consortium member institutions located in more than 40 states. Consortium members represent a variety of practice types, ranging from solo practitioners to community clinics, academic medical centers, and large integrated delivery networks. Approximately, two thirds of the participating clinicians identify themselves as primary care physicians. The dataset is comprised of submitted longitudinal patient data and includes but is not limited to demographic information; payment type (commercial, Medicare, Medicaid, self‐pay, and unrecognized payment type); enrollment dates; vital signs; laboratory orders and results; medication list entries and prescriptions; International Classification of Diseases, 9th Revision, (ICD‐9) Clinical Modification (ICD‐99‐CM) diagnosis codes; and Current Procedure Terminology Version 4 (CPT‐4), indicating the type of procedure if provided.
Study Design and Inclusion Criteria
We conducted a retrospective cohort study using the EMR database. The study period ranged from January 1, 2004, through December 31, 2007. All adult patients with diagnosed primary/essential hypertension (ICD‐9: 401.xx, 402.xx, 403.xx, 404.xx) who received at least 1 antihypertensive prescription between December 1, 2005, and November 30, 2006 (index period), and were longitudinally enrolled in the EMR database for at least 13 months after (follow‐up period) and 23 months prior (screening period) to the index date were selected. The index date was defined as the date of hypertension diagnosis or the date of antihypertensive prescription, whichever was earlier during the index period. Presence of the high‐risk clinical conditions for coronary heart disease (CHD) according to JNC 7 was assessed during the screening period (23 months prior to the index date except for myocardial infarction, which was assessed during 13 months prior to the index date) (Table 1). Patients were followed 12 months after the index date for treatment patterns and BP goal attainment. Patients would have to be at goal for both systolic BP (SBP) and diastolic BP (DBP) measurements to be considered at goal during follow‐up. Pharmacotherapy was evaluated according to JNC 7 guideline (Table 2).
Table I.
Clinical Conditions With High CHD Riska
| clinical condition | description |
|---|---|
| Type II diabetes | Considered as a CHD risk‐equivalent condition (ICD‐9: 250.xx) |
| Cerebrovascular disease | ICD‐9: 430.xx‐434.xx, 435.9x, and 436.xx–438.xx |
| Heart disease | ICD‐9: 402.xx, 410.xx, 411.xx, 413.xx, 414.xx, and 428.xx |
| Kidney disease | ICD‐9: 403.xx and 585.xx |
| Peripheral vascular disease | ICD‐9: 440.2x, 443.xx, and444.2x |
Abbreviations: CHD, coronary heart disease; ICD‐9, International Classification of Diseases, Ninth Revision. aHigh CHD risk: Patients with essential hypertension (ICD‐9: 401.xx) and ≥2 risk factors (from the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure guidelines), 6 including age and sex (men >55 y and women >65 y); smoking; dyslipidemia (low‐density lipoprotein ≥160 mm Hg; high‐density lipoprotein [HDL] <40 mm Hg for men, HDL <50 mm Hg for women; triglycerides [TGs] ≥150 mg/dL, total cholesterol ≥240 mg/dL); metabolic syndrome (abdominal obesity: baseline waist circumference >40 in for men and >35 in for women; fasting glucose ≥110 mg/dL, high TGs (≥150 mg/dL); low HDL cholesterol (<40 mg/dL for men and <50 mg/dL for women); obesity (≥30 kg/m2).
Table II.
Management of Blood Pressure for Adults 18 Years or Older With Compelling Indications according to JNC 7 Guidelines
| compelling indication | first‐line antihypertensive drugs | no. of drugs recommended |
|---|---|---|
| Heart disease | ||
| Stable angina pectoris | BBs or CCBs | ≥2 drugs |
| Acute coronary syndromes (unstable angina or myocardial infarction) | BBs or ACEIs | ≥2 drugs |
| Post–myocardial infarction | ACEIs or BBs or aldosterone antagonists | ≥2 drugs |
| Heart failure | ACEIs or BBs or ARBs or aldosterone blockers in combination with diuretics | ≥2 drugs |
| Diabetes | Combinations of ≥2 drugs with thiazide‐type diuretics, BBs, ACEIs, ARBs, and CCBs to achieve the target goal of <130/80 mm Hg | ≥2 drugs |
| Kidney disease | Often with ≥3 drugs to reach target BP values of <130/80 mm Hg with ACEIs or ARBs in a combination with diuretics or BBs | ≥3 drugs |
| Cerebrovascular disease (recurrent stroke prevention) | Combination of an ACEI and thiazide‐type diuretic | ≥2 drugs |
Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; ARB, angiotensin receptor blocker; BB, β‐blocker; CCB, calcium channel blocker; JNC 7, the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.
Variable Definition
Hypertension. Patients were categorized by their index BP levels as normal (SBP <120 mm Hg and DBP <80 mm Hg), prehypertension (120–139 mm Hg SBP or 80–89 mm Hg DBP), stage 1 hypertension (140–159 mm Hg SBP or 90–99 mm Hg DBP) and stage 2 hypertension (SBP ≥160 mm Hg or DBP ≥100 mm Hg), isolated systolic hypertension (SBP >140 mm Hg in the presence of normal DBP [<80 mm Hg]), and the presence of comorbid conditions as defined in Table 1.
Goal Attainment. The mean of the last 2 BP values obtained during evaluation period was used to assess clinical goal attainment. Patients not at goal at baseline (either BP >140/90 mm Hg or >130/80 for patients with diabetes or chronic kidney disease) were defined as attaining BP goal if both their last BP readings during the evaluation period were at goal.
Treatment Pattern. Medication prescribing was determined by first‐line antihypertensive regimen and number of prescribed antihypertensive drugs during follow‐up, as suggested by JNC 7 guidelines on pharmacologic treatment in patients without compelling indications (uncomplicated hypertension) and with compelling indications (complicated hypertension). 3 According to JNC 7, the following are considered compelling indications: stable angina pectoris, unstable angina, myocardial infarction, heart failure, diabetes, kidney disease, and cerebrovascular disease.
Statistical Analysis
All analyses were stratified into two cohorts based on age at index date: nonelderly age younger than 65 years, and elderly 65 years and older. Descriptive analyses were conducted to assess the CV risk profile, treatment pattern, and BP goal attainment between elderly and nonelderly patients and were compared using chi‐square tests for proportions and t test for means. Distribution of baseline CV risk factors, BP, and follow‐up BP were also compared between groups. Factors associated with BP goal attainment were assessed using multivariate logistic regression analyses. The logistic regressions estimated the odds of achieving BP goals by age, sex, race, baseline BP, dyslipidemia, baseline BMI, smoking status, number of antihypertensive medications, initial drugs prescribed, with or without comorbidities, and number of comorbidities. All statistical analysis was performed at a significance level of .05 using STATA v.10 (StataCorp, College Station, TX).
This project was reviewed and approved by the University of Utah institutional review board.
Results
Baseline Characteristics
There were 109,151 adult hypertensive patients in the dataset that met the inclusion and exclusion criteria. The nonelderly cohort consisted of 61,355 patients and the elderly cohort consisted of 47,796 patients (Figure). Characteristics of the study population are shown in Table 3. The mean age of the nonelderly cohort was 51.8 years. (standard deviation [SD]: 9.01), while the elderly cohort was 73.2 years (SD: 4.57). The elderly cohort had a significantly greater proportion of women compared with the other group (60.5% vs 53.8%, P<.0001; respectively).
Figure.
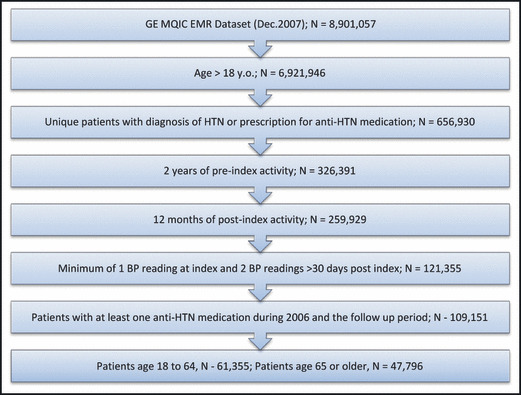
Identification of study population. EMR indicates electronic medical record; y.o., years old; HTN, hypertension; BP, blood pressure.
Table III.
Baseline Characteristics by Age
| variable | age <65 (n=61,355) | age≥65(n=47,796) | P value | ||
|---|---|---|---|---|---|
| mean/% | SD | mean/% | SD | ||
| Age | 51.83 | 9.01 | 73.17 | 4.57 | <.001 |
| Sex | |||||
| Female | 53.83 | 60.51 | <.001 | ||
| Male | 46.17 | 39.49 | |||
| Race | |||||
| Caucasian | 35.39 | 35.40 | <.001 | ||
| African American | 7.62 | 4.31 | |||
| Hispanic | 1.60 | 1.49 | |||
| Other (Asian/Indian) | 1.16 | 0.68 | |||
| Unknown | 54.23 | 58.12 | |||
| Smoking | |||||
| Never smoking | 38.59 | 37.99 | <.001 | ||
| Former | 25.55 | 34.47 | |||
| Current | 17.30 | 6.80 | |||
| Unknown | 18.56 | 20.75 | |||
| Clinical parameters | |||||
| Baseline BP | |||||
| Systolic BP | 136.48 | 8.83 | 138.70 | 20.03 | <.001 |
| Diastolic BP | 82.91 | 11.85 | 75.38 | 11.05 | <.001 |
| Follow‐up BP | |||||
| Systolic BP | 131.12 | 14.07 | 133.99 | 15.23 | <.001 |
| Diastolic BP | 79.64 | 8.92 | 73.23 | 8.86 | <.001 |
| Body mass index | |||||
| <30 | 36.54 | 59.72 | <.001 | ||
| ≥30 | 63.46 | 40.28 | |||
| Uncomplicated hypertension | 43.44 | 25.69 | 0.061 | ||
| Normal | 4.89 | 2.87 | |||
| Prehypertension | 16.34 | 9.96 | |||
| Stage 1 | 14.01 | 8.25 | |||
| Stage 2 | 8.21 | 4.60 | |||
| Isolated systolic hypertension | 7.34 | 9.63 | <.001 | ||
| Complicated hypertension | 56.56 | 74.31 | .791 | ||
| Normal | 6.86 | 9.12 | |||
| Prehypertension | 22.26 | 29.39 | |||
| Stage 1 | 18.25 | 23.88 | |||
| Stage 2 | 9.19 | 11.92 | |||
| Isolated systolic hypertension | 11.83 | 27.78 | <.001 | ||
| Comorbid conditions | |||||
| Dyslipidemia | 51.81 | 47.32 | <.001 | ||
| Diabetes | 12.80 | 11.66 | <.001 | ||
| Cerebrovascular disease | 1.40 | 4.58 | <.001 | ||
| Kidney disease | 1.09 | 2.85 | <.001 | ||
| Heart disease | 5.27 | 12.44 | <.001 | ||
| Peripheral vascular disease | 0.90 | 2.42 | <.001 | ||
| Coronary heart disease | 48.22 | 64.24 | <.001 | ||
| No. of comorbidities | |||||
| 0 | 43.44 | 25.69 | <.001 | ||
| 1 | 44.11 | 52.28 | |||
| 2 | 11.84 | 20.44 | |||
| ≥3 | 0.61 | 1.58 | |||
Abbreviations: BP, blood pressure; SD, standard deviation.
Consistent with the characteristics of hypertension in the elderly, isolated systolic hypertension (ISH) and the presence of comorbid conditions were more prevalent in the elderly cohort, with the exceptions of dyslipidemia (elderly 47.32% vs nonelderly 51.81%; P<.001) and diabetes (elderly 11.66% vs nonelderly 12.80%; P<0.001). ISH was significantly increased in the elderly population for both uncomplicated hypertension (elderly 9.63% vs nonelderly 7.34%; P<.001) and complicated hypertension (elderly 27.78% vs nonelderly 11.83%; P<.001). All other comorbid conditions (including cerebrovascular disease [elderly 4.58% vs nonelderly 1.40%; P<.001], kidney disease [elderly 2.85% vs nonelderly 1.09; P<.001], heart disease [elderly 12.44% vs 5.27%; P<.001], peripheral vascular disease [elderly 2.42% vs nonelderly 0.90%; P<.001], and high CHD risk [elderly 64.24% vs nonelderly 48.22%; P<.001]) were all present at a statistically significant higher level in the elderly vs nonelderly cohort. In addition, the number of comorbidities (either 1, 2, or ≥3) present in the two groups was statistically significantly higher in the elderly cohort. Overall, the elderly cohort had higher prevalence of CV risk conditions than the nonelderly cohort.
Prevalence of ISH
IV, V further illustrate the common occurrence of ISH in the elderly population. Table 4 compares the baseline mean SBP and DBP for the elderly and nonelderly cohorts by hypertension stage and presence of comorbidities. Again, consistent with the characteristic of ISH prevalence in the elderly, the elderly cohort had a statistically significant higher SBP at baseline across all categories with the exception of renal disease, which did not achieve statistical significance. In addition, DBP at baseline for the elderly cohort was statistically significantly lower across all categories as compared with the nonelderly cohort. Further, with the exception of stage 2 hypertension (in both the uncomplicated and complicated hypertension groups) and high CHD risk, the elderly had a mean DBP at baseline that was normal (<80 mm Hg) in all other categories, while the nonelderly cohort had a mean DBP at baseline that was indicative of prehypertension (>80 mm Hg).
Table IV.
Mean Baseline BP by Age and High‐Risk Cardiovascular Conditions
| condition (age <65 y; ≥65 y) | baseline systolic BP (SD) | baseline diastolic BP (SD) | ||||||
|---|---|---|---|---|---|---|---|---|
| total | <65 | ≥65 | P value a | total | <65 | ≥65 | P value a | |
| Uncomplicated hypertension (n=26,653; 12,280) | 137.69 (19.56) | 136.79 (19.07) | 139.64 (20.44) | .000 | 81.43 (12.28) | 83.96 (11.98) | 75.95 (11.08) | .000 |
| Stage 1 hypertension (n=8594; 3945) | 144.01 (8.23) | 142.98 (8.78) | 146.25 (6.33) | .000 | 84.38 (9.34) | 87.28 (7.73) | 78.05 (9.43) | .000 |
| Stage 2 hypertension (n=5034; 2200) | 165.39 (16.38) | 162.75 (16.67) | 171.43 (13.92) | .000 | 94.65 (12.64) | 98.65 (10.46) | 85.51 (12.43) | .000 |
| Complicated hypertension (n=34,702; 35,516) | 137.33 (19.30) | 136.25 (18.63) | 138.38 (19.87) | .000 | 78.60 (11.88) | 82.10 (11.69) | 75.18 (11.04) | .000 |
| Stage 1 hypertension (n=11,200; 11,413) | 144.91 (7.46) | 143.71 (8.21) | 146.09 (6.44) | .000 | 81.60 (9.78) | 85.50 (8.36) | 77.77 (9.57) | .000 |
| Stage 2 hypertension (n=5636; 5695) | 167.05 (14.92) | 163.68 (15.53) | 170.38 (13.48) | .000 | 90.58 (13.34) | 96.58 (11.53) | 84.65 (12.31) | .000 |
| Diabetes (n=3454; 2623) | 151.80 (14.51) | 150.63 (14.69) | 153.33 (14.13) | .000 | 83.23 (11.87) | 86.85 (11.17) | 78.46 (11.05) | .000 |
| Cerebrovascular disease (n=399; 1071) | 154.59 (15.40) | 151.68 (14.83) | 155.67 (15.48) | .000 | 81.37 (11.96) | 86.88 (11.66) | 79.32 (11.42) | .000 |
| Heart disease (n=1242; 2356) | 152.81 (15.21) | 150.86 (15.16) | 153.84 (15.13) | .000 | 81.58 (11.93) | 87.47 (11.53) | 78.48 (10.94) | .000 |
| Renal disease (n=331; 639) | 153.72 (15.58) | 153.32 (17.09) | 153.92 (14.76) | .574 | 80.96 (12.29) | 87.31 (11.55) | 77.67 (11.33) | .000 |
| Peripheral vascular disease (n=253; 538) | 153.37 (14.84) | 151.65 (14.38) | 154.18 (15.00) | .025 | 80.11 (12.02) | 86.21 (11.74) | 77.24 (11.05) | .000 |
| High CHD risk (n=14,686; 14,996) | 152.23 (14.79) | 150.31 (14.55) | 154.12 (14.77) | .000 | 84.83 (11.83) | 89.47 (10.79) | 80.29 (11.02) | .000 |
Abbreviations: BP, blood pressure; CHD, coronary heart disease; SD, standard deviation. a P value shows whether patients younger than 65 years and patients 65 years and younger are statistically different.
Table V.
Mean Blood Pressure During Follow‐Up
| condition (age <65 y; ≥65 y) | post–systolic BPa (SD) | post–diastolic BPa (SD) | ||||||
|---|---|---|---|---|---|---|---|---|
| total | <65 | ≥65 | P value b | total | <65 | ≥65 | P value b | |
| Uncomplicated hypertension (n=26,653; 12,280) | 131.86 (14.36) | 130.75 (13.82) | 134.27 (15.18) | .000 | 78.21 (9.34) | 80.35 (8.80) | 73.55 (8.75) | .000 |
| Stage 1 hypertension (n=8594; 3945) | 134.57 (12.95) | 133.45 (12.54) | 137.01 (13.50) | .000 | 79.50 (8.96) | 81.80 (8.18) | 74.49 (8.54) | .000 |
| Stage 2 hypertension (n=5034; 2200) | 140.58 (16.46) | 138.91 (16.08) | 144.41 (16.61) | .000 | 82.51 (10.47) | 85.20 (9.60) | 76.34 (9.74) | .000 |
| Complicated hypertension (n=34,702; 35,516) | 132.66 (14.81) | 131.40 (14.25) | 133.89 (15.24) | .000 | 76.07 (9.42) | 79.09 (8.98) | 73.13 (8.89) | .000 |
| Stage 1 hypertension (n=11,200; 11,413) | 135.80 (13.29) | 134.45 (12.79) | 137.14 (13.63) | .000 | 77.26 (9.15) | 80.42 (8.46) | 74.16 (8.74) | .000 |
| Stage 2 hypertension (n=5636; 5695) | 142.62 (16.97) | 140.80 (16.71) | 144.41 (17.03) | .000 | 80.02 (10.80) | 84.12 (10.20) | 75.97 (9.81) | .000 |
| Diabetes (n=3454; 2623) | 138.15 (15.38) | 137.21 (15.32) | 139.38 (15.39) | .000 | 77.29 (10.00) | 80.17 (9.60) | 73.50 (9.24) | .000 |
| Cerebrovascular disease (n=399; 1071) | 137.96 (15.70) | 134.39 (13.77) | 139.27 (16.17) | .000 | 74.97 (9.59) | 79.70 (8.70) | 73.21 (9.32) | .000 |
| Heart disease (n=1242; 2356) | 137.95 (15.91) | 136.82 (15.68) | 138.54 (15.99) | .002 | 75.62 (9.93) | 80.22 (10.03) | 73.19 (8.98) | .000 |
| Renal disease (n=331; 639) | 138.31 (17.54) | 138.20 (19.72) | 138.36 (16.31) | .894 | 74.91 (10.50) | 79.80 (11.40) | 72.37 (9.02) | .000 |
| Peripheral vascular disease (n=253; 538) | 137.82 (15.09) | 136.58 (15.01) | 138.41 (15.10) | .112 | 74.55 (9.95) | 79.76 (9.21) | 72.10 (9.32) | .000 |
| Coronary disease (n=14,686; 14,996) | 138.14 (14.81) | 136.51 (14.39) | 139.74 (15.04) | .000 | 78.41 (9.72) | 81.84 (9.13) | 75.06 (9.08) | .000 |
Abbreviation: SD, standard deviation. aPost–blood pressure (BP) is a mean value of the last 2 BP readings after index date. b P value shows whether patients younger than 65 years and patients 65 years and older are statistically different.
At the end of the follow‐up period, the pattern of elevated SBP in the elderly as compared with the nonelderly population and decreased DBP was still present (Table 5). SBP levels at follow‐up were statistically significantly higher in the elderly population in all categories with the exception of renal disease and peripheral vascular disease, which did not achieve statistical significance. DBP levels were statistically significantly lower in all categories for the elderly as compared with the nonelderly cohort.
Treatment Pattern
At baseline, the most commonly prescribed medication class in both the nonelderly and elderly groups were angiotensin‐converting enzyme inhibitors (ACEIs) (26.8% vs 22.9%, respectively). Diuretics (14.1% nonelderly vs 10.6% elderly) were the next most commonly prescribed medication in both cohorts, followed by angiotensin receptor blockers (ARBs) (7.2% nonelderly vs 8.3% elderly). Among the combination therapies, ACEI/diuretic (9.7% nonelderly vs 7.2% elderly) was the most commonly seen combination, followed by the ARB/diuretic combination (8.1% nonelderly vs 6.8% elderly). Overall, the distribution of the medication classes at baseline for the two populations appeared similar.
Table 6 compares treatment pattern and BP goal attainment rates between both cohorts among patients categorized as having stage 1 or stage 2 hypertension at baseline. Treatment patterns in the study population were assessed by the number of prescribed medications for patients with or without compelling indications. Across all categories, elderly patients were more likely to be treated with a greater number of medications than nonelderly patients. The elderly population was more likely to be prescribed additional antihypertensive therapies and less likely to discontinue antihypertensive therapies. The proportion of elderly patients with add‐on antihypertensive therapy was significantly higher than the nonelderly patients (47.11% vs 36.84%, respectively; P value <.001). In addition, a higher proportion of nonelderly patients discontinued antihypertensive therapies than the elderly (27.44% vs 25.91%, respectively; P value <.001).
Table VI.
Antihypertensive Treatment Utilizationa and BP Goal Attainment Rate During Follow‐Up by Age Among Patients With Stage 1 or Stage 2 Hypertension
| treatment utilization | BP goal attainment | |||||
|---|---|---|---|---|---|---|
| age <65 (n=30,464), % | age≥65 (n=23,253), % | P value | age <65 (n=30,464), % | age≥65 (n=23,253), % | P value | |
| Uncomplicated hypertension | 89.20 | 91.51 | .000 | 58.29 | 52.97 | .000 |
| Stage 1 hypertension | 100 | 100 | 1.000 | 64.88 | 59.52 | .000 |
| Stage 2 hypertension | 70.76 | 76.27 | .000 | 47.04 | 41.23 | .000 |
| Complicated hypertension | 69.38 | 76.06 | .000 | 56.90 | 51.89 | .000 |
| Stage 1 | 67.33 | 75.05 | .000 | 63.43 | 57.73 | .000 |
| Stage 2 | 77.63 | 81.00 | .000 | 43.93 | 40.19 | .000 |
| Complication conditions | ||||||
| Diabetes | 65.51 | 75.27 | 0.000 | 13.20 | 15.14 | 0.007 |
| Cerebrovascular disease | 73.81 | 78.21 | 0.068 | 58.10 | 50.85 | 0.011 |
| Heart disease | 73.87 | 75.28 | 0.339 | 54.90 | 51.61 | 0.053 |
| Renal disease | 63.92 | 72.97 | 0.000 | 17.26 | 18.09 | 0.691 |
| Peripheral vascular disease | 74.44 | 77.60 | 0.315 | 59.63 | 53.23 | 0.082 |
| High CHD risk | 70.69 | 77.82 | 0.000 | 51.44 | 47.34 | 0.000 |
Abbreviations: BP, blood pressure; CHD, coronary heart disease. aProportion of patients treated with ≥2 antihypertensive medications over 13 months of follow‐up.
BP Goal Attainment
Among patients with uncomplicated hypertension, nonelderly patients achieved greater proportions of BP goal attainment than elderly patients (58.3% vs 53.0%, respectively; P<.0001) (Table 6). This result of greater BP goal attainment in the younger population with uncomplicated hypertension was consistent in both the stage 1 and stage 2 hypertensive populations. Complicated hypertension also displayed similar results (nonelderly 56.9% vs elderly 51.9%; P<.0001). Interestingly, nonelderly patients with diabetes achieved lower rates of BP control than the elderly cohort (13.2% vs 15.1%; P=.007). The results for goal attainment in the heart disease, renal disease, and peripheral vascular disease groups did not achieve statistical significance.
Resistant hypertension was defined as BP that remained above BP goal despite patients being treated with ≥3 antihypertensive drugs, of which 1 drug was a diuretic. 10 Among all populations in the study dataset (n=109,151), 8.04% exhibited resistant hypertension. Among elderly patients (n=47,796), 8.5% exhibited resistant hypertension, while 7.7% of nonelderly (n=61,355) exhibited resistant hypertension (P value <.001).
Multivariate Analysis of BP Goal Attainment by Age
To study factors associated with BP goal attainment in hypertensive patients, logistic regression models were used (Table 7). Of the total population (N=109,151), there were 53,717 patients with stages 1 and 2 hypertension (55,434 were excluded with normal BP or prehypertension). Patients with “race” and “smoking status” reported as unknown were excluded from the regression analysis (n=34,660), because the result of “unknown race” or “unknown smoking status” being a factor associated with BP goal attainment was not interpretable. Finally, there were 363 patients excluded with missing BP or BMI values. Therefore, the sample for logistic regression models was 18,694 patients, of which 7477 were elderly and 11,217 were nonelderly.
Table VII.
Multivariate Analysis of BP Goal Attainment Among Hypertensive Patients During Follow‐Up Adjusting for Confounding Factors (n=18,694)
| variable | odds ratio | 95%confidence interval | |
|---|---|---|---|
| Nonelderly patients | Reference | ||
| Elderly patients (≥65 y) | 0.83a | 0.77 | 0.90 |
| Sex | |||
| Male | Reference | ||
| Female | 1.05 | 0.98 | 1.11 |
| Race | |||
| Caucasian | Reference | ||
| African American | 0.67a | 0.62 | 0.73 |
| Hispanic | 1.09 | 0.93 | 1.28 |
| Others | 1.04 | 0.84 | 1.30 |
| Baseline BP | |||
| Systolic BP | 0.98a | 0.98 | 0.98 |
| Diastolic BP | 1.04a | 1.04 | 1.04 |
| Dyslipidemia | 1.03 | 0.96 | 1.11 |
| BMI at baseline | |||
| Nonobese (<30 kg/m²) | Reference | ||
| Obese (≥30 kg/m²) | 0.84a | 0.78 | 0.90 |
| Smoking status at baseline | |||
| Never smoked | Reference | ||
| Former smoker | 1.06 | 0.99 | 1.14 |
| Current smoker | 0.95 | 0.87 | 1.04 |
| Complicated hypertension | 0.79a | 0.72 | 0.94 |
| Treated with multiple antihypertensive medications | 1.00 | 0.93 | 1.08 |
| Initial prescription medication | |||
| Fixed‐dose Combination | Reference | ||
| ACEI | 0.93 | 0.86 | 1.01 |
| ARB | 0.92 | 0.83 | 1.02 |
| BB | 1.04 | 0.91 | 1.19 |
| CCB | 1.06 | 0.87 | 1.29 |
| Diuretics | 1.25a | 1.13 | 1.39 |
Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; ARB, angiotensin receptor blocker; BB, β‐blocker; BMI, body mass index, BP, blood pressure; CCB, calcium channel blocker. a P<.001
Among demographic factors, increasing age and African American race were found to negatively impact BP goal attainment. Using the nonelderly population as the reference group, the elderly population was 17% more likely to not achieve (95% confidence interval [CI], 0.77–0.90) BP goal. Using Caucasian race as the reference group, African Americans had an odds ratio [OR] of 0.67 (95% CI, 0.62–0.73) for BP goal achievement. Patients with elevated SBP at baseline were less likely to achieve goal (OR, 0.98; 95% CI, 0.98–0.98), while patients with elevated DBP at baseline were more likely to achieve goal (OR, 1.04; 95% CI, 1.04–1.04). Obese patients, defined as those with a BMI ≥30 kg/m2 at baseline (reference group nonobese patients <30 kg/m2), were less likely to achieve BP goal (OR, 0.84; 95% CI, 0.78–0.90). Patients categorized as having complicated hypertension (hypertension with ≥1 compelling indications including stable angina pectoris, unstable angina, myocardial infarction, heart failure, diabetes, kidney disease, and cerebrovascular disease) were also less likely to achieve BP goals (OR, 0.79; 95% CI, 0.72–0.94). Among the initially prescribed medications for hypertension, the use of diuretics (reference group: any fixed‐dose combination) was associated with an increased likelihood of achieving BP goal (OR, 1.25; 95% CI, 1.13–1.39).
Discussion
This study examined the CV risk profile and the status of hypertension management among both elderly and nonelderly patients in primary care practices in the United States using the GE Medical Quality Improvement Consortium (MQIC) EMR database. In addition, the study also investigated the factors associated with BP goal attainment in the entire study population.
As has been reported in the literature, elderly patients with hypertension tend to have greater numbers of comorbid conditions, higher levels of ISH, and lower levels of BP goal attainment. This study found that relative to patients older than 65 years, elderly patients (those 65 years and older) have statistically significant higher levels of comorbid conditions, particularly those diagnoses considered compelling indications as per JNC 7 guidelines that are indicative of high coronary heart disease risk. As shown in Table 3, this was consistent for all diagnoses in the elderly except for dyslipidemia and diabetes. All other diagnoses were found to be more prevalent in the elderly population. These findings are consistent with an elderly population having a higher CV risk profile than nonelderly patients. This study also examined the presence of ISH in both the elderly and nonelderly patients. As shown in Table 3, both the uncomplicated hypertension and complicated hypertension patient populations exhibited statistically significant higher levels of ISH in the elderly compared with the nonelderly. Further, Table 4, shows that this characteristic of the elderly, ie, the presence of ISH, was consistently present across all high‐risk CV conditions. All of these results, taken together, are consistent with a higher CV risk profile in the elderly and are indicative of the increased difficulty in treating elderly patients to BP goals.
This study also examined hypertension management as evidenced by physician‐prescribing patterns and comparison to recommendations from JNC 7 for management of BP in adult patients. This study found that elderly patients were more likely to be treated with multiple antihypertensive medications than younger patients (Table 6). For those diagnoses that are considered to be compelling indications, the elderly population was found to have consistently higher levels of treatment with multiple medications than the nonelderly, although not all were found to be statistically significant. These results suggest that there may be subtle differences in the management of elderly and nonelderly hypertension patients. Table 6 also illustrates the levels of BP goal attainment across the various elderly and nonelderly populations. Although older patients were more likely to receive multiple antihypertensive medications, the rate of BP goal attainment was consistently lower than their younger counterparts in various hypertension categories and high‐risk CV comorbidities, except for diabetes. Patients with diabetes (13.2% nonelderly vs 15.14% in the elderly; P=.007) and renal disease (17.3% nonelderly vs 18.1% elderly; P=.691) had the lowest levels of BP goal attainment among all patients with compelling indications.
Previous research has suggested that elderly hypertension patients are treated less aggressively than their younger counterparts. This study found that elderly patients were more likely to be treated with multiple medications than nonelderly patients. Treatment with multiple antihypertensive medications is important but it is probably not the only measure of treatment intensity. If aggressive treatment is defined not solely by number of medications but also by the dosage strengths of the medications prescribed, we were unable to discern any differences. One limitation of the EMR database is the lack of dosing information. The starting dose of a medication is typically given; however, dose titrations are rarely reported in the database, making it difficult to determine whether elderly and nonelderly patients receive comparable doses. Similarly, since medications are recorded in the database by physician orders and patient medication history, actual utilization of medications (including patient compliance) is not known.
Multivariate analyses of BP goal attainment (Table 7) confirm that elderly patients have a statistically significant lower likelihood of achieving goal than nonelderly patients. In addition, the analysis found that the presence of complicated hypertension was a statistically significant factor that contributes to lower goal attainment levels. Given the higher levels of comorbid conditions in the elderly, these results are consistent with previous research demonstrating higher CV risk profile in the elderly and lower levels of goal attainment. Obesity was also found to be a statistically significant factor contributing to lower goal attainment levels. A large number of patients (34,660 of 53,717 patients with stages 1 and 2 hypertension) were excluded from the regression analysis because race and smoking status were reported as unknown. When the regression analyses were run with those patients included, the results were similar to those reported in Table 7, with the only difference being that patients with unknown race or unknown smoking status were more likely to achieve goal.
Conclusions
This study examined the treatment of patients with hypertension in the primary care setting by retrospective analysis of an EMR database. Our results were consistent with previously published findings that elderly patients with hypertension have a higher prevalence of ISH, a greater number of comorbidities, and lower levels of BP goal attainment than nonelderly patients with hypertension. Obesity, a modifiable lifestyle factor, was associated with lower levels of BP goal attainment. Both elderly and nonelderly diabetic and renal disease patients were found to have very low levels of BP goal attainment. In contrast to other published literature, our study did not find evidence for less aggressive management of elderly patients relative to nonelderly patients. Our results suggest that elderly patients are actually treated more aggressively than nonelderly patients based on the number of antihypertensive medications prescribed. Despite this, providers would be well advised to treat elderly patients even more aggressively, since the levels of BP goal attainment for the elderly are consistently lower than that for the nonelderly.
References
- 1. Rosamond W, Flegal K, Furie K. Heart Disease and Stroke Statistics 2008 Update: a Report From the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117:e25–e146. [DOI] [PubMed] [Google Scholar]
- 2. Elliot WJ. Management of hypertension in the very elderly patient. Hypertension. 2004;44:800–804. [DOI] [PubMed] [Google Scholar]
- 3. Chobanian AV, Bakras GL, Black HR. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–1252. [DOI] [PubMed] [Google Scholar]
- 4. Materson BJ, Reda DJ, Cushman WC. Single‐drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. N Engl J Med. 1993;328(13):914–921. [DOI] [PubMed] [Google Scholar]
- 5. Bakris GL, Williams M, Dworkin L. Preserving renal function in adults with hypertension and diabetes: a consensus approach. National Kidney Foundation Hypertension and Diabetes Executive Committees Working Group. Am J Kidney Dis. 2000;36(3):S220–S227. [DOI] [PubMed] [Google Scholar]
- 6. Milani RV. Reaching for aggressive blood pressure goals: role of angiotensin receptor blockade in combination therapy. Am J Manag Care. 2005;11(suppl 7):S220–S227. [PubMed] [Google Scholar]
- 7. Sica DA. Rationale for fixed‐dose combinations in the treatment of hypertension: the cycle repeats. Drugs. 2002;62(3):443–462. [DOI] [PubMed] [Google Scholar]
- 8. Gradman AH, Morsy M. Hypertension in the elderly. Cardiology Review. 2006 (September). Available at: http://www.cardiologyreviewonline.com/issues/articles/2006‐09_07.asp.
- 9. Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment and control of hypertension in the United States, 1988–2000. JAMA. 2003;290(22):199–206. [DOI] [PubMed] [Google Scholar]
- 10. Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403–1419. [DOI] [PubMed] [Google Scholar]


