Abstract
There has been much discussion and study about the role of continuing medical education (CME) in improving patient care. The authors describe the processes used to develop and implement a series of live, half‐day, highly interactive CME events that addressed knowledge, competency, and performance gaps in hypertension diagnosis and management in the primary care community and successfully changed physician behavior toward improved patient outcomes. Participation in an intensive, highly interactive, case‐based didactic program was significantly associated with an increase in clinician knowledge and competency in diagnosing and managing patients with hypertension. Participation was also associated with a high likelihood for practice change and making guideline‐driven and evidence‐based decisions to positively impact patient care. A greater portion of participants were able to identify the appropriate blood pressure goal and select the most appropriate pharmacotherapy regimen for specific patients. Quality of education index indicated that participants were 52% more likely to practice guideline‐driven and evidence‐based medicine than those who did not participate in the CME activity. J Clin Hypertens (Greenwich). 2011;13:97–105. © 2010 Wiley Periodicals, Inc.
The number of individuals affected by hypertension in the United States is steadily increasing as the population ages and the obesity epidemic continues. Currently, it is estimated that more than 74 million Americans have been diagnosed with hypertension, and approximately 53 million Americans have prehypertension. Over the next 10 to 15 years, the prevalence of hypertension is expected to increase, affecting more than 100 million Americans. 1 , 2 , 3 In reality, hypertension is a progressive cardiovascular (CV) syndrome that arises from complex and interrelated etiologies. Data from the Framingham Heart Study found that >80% of hypertensive patients (>140/90 mm Hg) have at least one metabolically linked CV risk factor. 4
Effective control of blood pressure (BP) with antihypertensive drug therapy has been associated with reductions in the incidence of heart failure (>50%), stroke (35%–40%), and myocardial infarction (20%–25%). 5 The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines provide an evidence‐based approach to the prevention and management of hypertension. The treatment goal is <140/90 mm Hg for individuals with no compelling conditions and <130/80 mm Hg in patients with diabetes or chronic kidney disease. The JNC 7 guidelines recommend treating all patients with stage 1 hypertension (systolic 140–159 mm Hg or diastolic 90–99 mm Hg) with either a thiazide diuretic, angiotensin‐converting enzyme (ACE) inhibitor, angiotensin receptor blocker (ARB), β‐blocker (BB), or calcium channel blocker (CCB) as monotherapy or, as felt necessary, with combination therapy. In patients with stage 2 hypertension (systolic ≥160 mm Hg or diastolic ≥100 mm Hg), however, where BP is 20/10 mm Hg above goal, it is recommended that one starts with a 2‐drug combination regimen, with one of the drugs being a thiazide‐type diuretic. 3
Despite target goal and treatment recommendations, approximately two thirds of hypertensive patients are not meeting BP goals defined by JNC 7. 6 Analysis of medical records from 6 community‐based hospitals revealed that overall adherence to JNC 7 guidelines was only 53.5%. Looking at factors that may have affected adherence, failure to promptly initiate/adjust therapy and follow‐up with patients who have uncontrolled BP was observed. 7 Clinical inertia has been discussed by other researchers and is a significant factor in poorly controlled BP. 8 , 9 , 10 , 11 In addition, discussion of lifestyle recommendations was infrequently documented by physicians, and this may reflect a missed opportunity to promote patient self‐management. 7
There has been much discussion and study regarding the role of continuing medical education (CME) in improving patient care. Theoretically, physicians who are educated about the latest advances in evidence‐based practice will make more informed treatment decisions, resulting in improved patient outcomes. 12 The literature suggests that the most effective strategies for educational design contain a multidimensional approach: rigorous and accurate assessment of need, use of active and varied learning approaches, and an evidence‐based curriculum that focuses on overcoming barriers to change. 13 Futhermore, a change in physician practice is more likely with interventions that are multifaceted, interactive, and consistent with the perceived needs of the learner. 14
In October 2009, we implemented a novel, live, highly intensive, case‐based educational initiative called STOP Hypertension NOW! Recognize & Manage Your High‐risk Patients. This CME initiative consisted of a series of 6 regional 4‐hour meetings designed to address existing knowledge and practice gaps in the management of hypertension. We describe the impact of this educational initiative on clinicians’ knowledge of hypertension treatment guidelines and competency in providing goal‐targeted therapy. Effectiveness of the educational activity was measured using a case‐based survey designed to assess whether the diagnostic and therapeutic choices of program participants were consistent with evidence‐based guidelines.
Methods
Design of the Educational Initiative
This CME activity was designed to address the Institute of Medicine competencies of providing patient‐centered care and employing evidence‐based practice. Developed by key opinion leaders in hypertension, this regional series was based on a core curriculum, with customization of each mini‐conference to highlight the unique challenges and statistics in a particular region.
This CME activity included 6 mini‐conferences held at various locations on the East Coast (Manhattan, NY; Pittsburgh, PA; Melville [Long Island], NY; Rochester, NY; Philadelphia, PA; and Princeton, NJ). The agenda of these mini‐conferences was divided into three 1‐hour teaching modules, respectively focusing on diagnosis and management, sex and ethnic disparities, hypertension in the elderly, and nonadherence to antihypertensive regimens. Each module included two 20‐minute didactic lectures, followed by a case study discussion. The format emphasized attendee‐faculty interaction during the lectures and the case study discussions and incorporated the use of an audience response system (ARS) and frequent question‐and‐answer sessions. This program was not part of a larger conference, and participation was completely voluntary.
The educational objectives for the live program were as follows:
-
•
Describe the effectiveness of various drug classes as they relate to different patient populations.
-
•
Cite the JNC 7 hypertension guideline recommendations for patients with compelling indications.
-
•
Explain benefits and limitations of the Framingham and Reynolds risk scores as they relate to cardiovascular risk assessment in women.
-
•
Discuss the rationale for hypertension disparities in African Americans and management considerations in this population.
-
•
Manage an elderly patient with isolated systolic hypertension.
-
•
Identify strategies to improve adherence to antihypertensive regimens.
Outcome Survey Instruments: Case Vignettes and Survey Questions
Evidence‐based case vignettes were developed to assess whether the diagnostic and therapeutic choices of participants were consistent with clinical evidence presented in the context of the educational activity. The case vignettes were also used to determine whether the practice choices of participants were different from those of nonparticipants. In addition, a series of key measurement indicators focusing on hypertension management were determined based on the learning objectives and educational content (Table I). Additional survey items were included to assess barriers to the optimal management of hypertension.
Table I.
Performance Indicators
| Case | Performance Indicator |
|---|---|
| Case 1: 38‐y‐old African American woman | |
| Presents for annual physical examination No medical history; no medications Family history remarkable for hypertension in parents and diabetes in two aunts Weight, 192 lb (body mass index, 29 kg/m2); blood pressure (BP), 158/92 mm Hg in right arm and 152/94 mm Hg in left arm; unremarkable cardiac examination Patient reports BPs of about 140/90 mm Hg (checks at grocery store) Next visit: BP, 150/95 mm Hg; glucose, 94 mg/dL; normal urine albumin/creatinine ratio | A patient with systolic BP 140–159 mm Hg or diastolic BP 90–99 mm Hg is classified in stage 1 hypertensiona The initial pharmacotherapy for a patient with stage 1 hypertension is a thiazide‐type diuretica |
| Case 2: 72‐y‐old Asian man | |
| 20‐y history of hypertension, untreated for approximately 10 y Retired, walks daily, eats traditional diet of rice and noodles 1 y ago: fasting glucose, 154 mg/dL; hemoglobin A1C, 7.4% Patient has gained 10 lb during past year On examination: BP, 182/84 mm Hg; heart rate, 86 beats per min, regular; soft systolic murmur | Patients with hypertension and comorbid diabetes or kidney disease have a lower BP goal and lower BP threshold for initial use of 2‐drug combinationsa The BP goal in a hypertensive patient (baseline BP <160/100 mm Hg) with comorbid diabetes is <130/80 mm Hga Combination pharmacotherapy should be initiated for a hypertensive and diabetic patient with a BP reading that is >20/10 mm Hg above goala Characteristics of hypertension in the elderly include increased systolic BP, pulse pressure, left ventricular hypertrophy, arterial stiffness, and elevated and total peripheral arterial resistance, as well as decreased cardiac output, pulse rate, renal blood flow, plasma renin activity, angiotensin II levels, arterial compliance, blood volume, and diastolic BPb |
| Case 3: 50‐y‐old Hispanic woman | |
| Presents after dentist noted BP elevation 10‐y history of hypertension Nonadherent with prescribed therapy Nonsmoker; family history of diabetes, stroke, congestive heart failure On examination: BP, 140/88 mm Hg in both arms; similar at previous visits Therapy with diuretic is initiated Patient starts diuretic, but is lost to follow‐up for 3 y; returns reporting dyspnea on exertion and mild edema Examination remarkable for few crackles over bases, mild edema; electrocardiography shows left ventricular hypertrophy; BP, 160/108 mm Hg; normal potassium level; creatinine, 1.5 mg/dL, with glomerular filtration rate <40 mL/min | The therapeutic goals in patients with hypertension and chronic kidney disease are to slow deterioration of renal function and prevent cardiovascular disease. Aggressive BP management with >2 drugs is recommended to reach a target BP value of <130/80 mm Hg. An angiotensin receptor blocker– or angiotensin‐converting enzyme inhibitor–based regimen is the preferred regimen for these patientsa |
| Case 4: 64‐y‐old African American man | |
| Presents after hospitalization for new cerebrovascular accident; experienced acute onset of dysarthria, which responded to thrombolytic therapy with near total recovery No medical history Quit smoking during hospitalization BP, 152/94 mm Hg; cholesterol, 254 mg/dL, low‐density lipoprotein cholesterol, 142 mg/dL; creatinine, 1.4 mg/dL; normal blood glucose | The ethnic group with the highest risk of hypertension and highest prevalence of stroke in 2005–2006 was African American womenc Combination therapy, including a renin‐angiotensin system–blocking agent, should be initiated in African American patients with hypertension (BP >145/90 mm Hg) who are at high cardiovascular riskd |
aFrom Chobanian et al.3 bFrom Black H. J Clin Hypertens (Greenwich). 2003;5:11–16. cLloyd‐Jones D et al.2 dFrom Douglas JG et al. Arch Intern Med. 2003;163:525–541.
Survey Distribution
Surveys were distributed to physicians who attended the CME program (participants) onsite, during participant registration, and then collected from the participants immediately after the educational activity. A total of 115 surveys were collected from participants, from which 50 surveys were randomly selected for further analysis. Surveys were also distributed to 50 primary care physicians who did not participate in the program (nonparticipants) via e‐mail. Answers to case study questions, current practice patterns, and perceived barriers to care were compared between participants and nonparticipants to assess differences in practice choices associated with program participation.
Statistical Analysis
Data were analyzed using SPSS version 17.0 (IBM Corporation, Somers, NY). For each question, data were first arrayed using frequencies. The differences between the mean evidence‐based responses of participants and nonparticipants were then analyzed using t tests. The difference between responses received by participants and nonparticipants was evaluated by determining the effect size, according to a previously published method by Colliver. 15 An effect size was calculated to determine the amount of difference between the evidence‐based responses of the participants and nonparticipants. Effect size is calculated using the Cohen’s d formula, and is expressed as a nonoverlap percentage or the percentage achieved by participants that was not reflected in the evidence‐based responses of nonparticipants. Any positive difference between the two groups where the content is relevant to the participants’ patient populations demonstrates an important potential educational impact. Significant differences were determined at P≤.10.
Results
Demographics
The average attendance for each program was 98 participants (total of 588); 67% of whom were physicians (MDs/DOs), 23% were nurses, and 10% were physician assistants. Table II provides complete demographic information for responding program participants, as well as for the 50 nonparticipants. Participants and nonparticipants were demographically similar in terms of medical degree, graduation year from medical school, specialty, major professional activity, practice location, and number of hypertensive patients seen per week.
Table II.
Demographics of Participants and Nonparticipants
| Participants | Nonparticipants | |||
|---|---|---|---|---|
| No. | Mean | No. | Mean | |
| Patients seen per week with hypertension | 43 | 38 | 50 | 35 |
| What year did you graduate from medical school? | 41 | 1982 | 47 | 1986 |
| No. | Percentage | No. | Percentage | |
| Degree | ||||
| MD/DO | 50 | 100.0 | 50 | 100.0 |
| Total respondents | 50 | 100.0 | 50 | 100.0 |
| Specialty | ||||
| Family practice | 28 | 56.0 | 28 | 56.0 |
| Internal medicine | 22 | 44.0 | 22 | 44.0 |
| Total respondents | 50 | 100.0 | 50 | 100.0 |
| Practice location | ||||
| Urban | 16 | 35.6 | 18 | 36.0 |
| Suburban | 21 | 46.7 | 20 | 40.0 |
| Rural | 8 | 17.8 | 12 | 24.0 |
| Total respondents | 45 | 100.0 | 50 | 100.0 |
| Present employment | ||||
| Solo practice | 21 | 46.7 | 19 | 38.0 |
| Group practice | 13 | 28.9 | 30 | 60.0 |
| Medical school | 1 | 2.2 | 0 | 0.0 |
| Nongovernment hospital | 3 | 6.7 | 1 | 2.0 |
| Government | 5 | 11.1 | 0 | 0.0 |
| Other | 2 | 4.4 | 0 | 0.0 |
| Total respondents | 45 | 100.0 | 50 | 100.0 |
| Major professional activity | ||||
| Direct patient care activities | 42 | 93.3 | 50 | 100.0 |
| Administrative activities | 1 | 2.2 | 0 | 0.0 |
| Medical education | 1 | 2.2 | 0 | 0.0 |
| Medical research | 0 | 0.0 | 0 | 0.0 |
| Other | 1 | 2.2 | 0 | 0.0 |
| Total respondents | 45 | 100.0 | 50 | 100.0 |
Survey Responses
Analysis and comparison of the survey results from participants and nonparticipants showed that participants chose evidence‐based answers more frequently than nonparticipants to questions related to JNC 7 guideline recommendations, appropriate antihypertensive therapy use in specific patients (those with compelling indications, elderly patients, and individuals at risk for stroke), and strategies to improve adherence to antihypertensive regimens. Participants also demonstrated a higher level of competency compared with nonparticipants.
JNC 7 Guidelines A similar number of participants and nonparticipants correctly classified the patient’s stage of hypertension when given a specific BP range. However, participants and nonparticipants differed in the response pattern to BP goal, with a significantly (P=.005) greater number of participants (78%) vs nonparticipants (51%) capable of selecting the appropriate BP goal for the specified patient (<130/80 mm Hg) (Figure 1).
Figure 1.
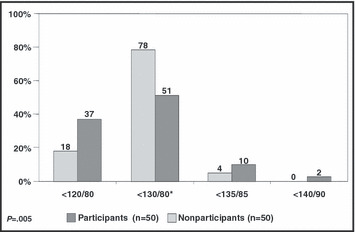
A significantly greater number of participants selected the appropriate blood pressure (BP) goal for a 72‐year‐old diabetic Asian man with a 20‐year history of hypertension compared with nonparticipants (case 2). *Appropriate BP goal for the specified patient.
Epidemiologic and Ethnic Disparities. A significantly (P<.001) greater number of participants (57%) was aware that African American women were more likely than another ethnic group/sex to experience a stroke event compared with nonparticipants (10%). Most nonparticipants (88%) selected “African American men” as having the highest prevalence of stroke.
Management of Hypertension in African Americans A similar proportion of participants and nonparticipants selected fasting glucose testing to help determine the best antihypertensive agent for an overweight African American woman with newly diagnosed hypertension and a family history of diabetes and hypertension. In addition, a similar number of participants and nonparticipants chose the most appropriate first‐line therapy for this patient, a thiazide diuretic. When asked to select the initial pharmacotherapy for an African American man who recently experienced a cerebrovascular accident, a significantly (P=.020) greater number of participants (53%) chose the more appropriate answer of a “RAS‐blocking agent plus a thiazide‐type diuretic or a CCB” compared with nonparticipants (30%). The majority of nonparticipants (36%) selected monotherapy with a RAS‐blocking agent as the most appropriate initial therapy for this patient.
Compelling Indications When asked to select the initial antihypertensive regimen for an elderly Asian man with severe systolic hypertension, diabetes, and recent weight gain (case 2), 84% of participants vs 52% of nonparticipants (P=.001) chose the most appropriate answer of combination therapy with an ACE inhibitor and a diuretic (Figure 2). The majority of participants (76%) and nonparticipants (70%) did not know which therapy was most appropriate to improve long‐term CV morbidity and mortality for a middle‐aged Hispanic woman with a history of hypertension and chronic kidney disease.
Figure 2.
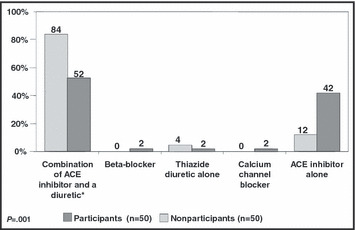
More participants chose the most appropriate initial antihypertensive regimen for a patient with severe systolic hypertension, diabetes, and recent weight gain compared with nonparticipants (case 2). *Most appropriate therapy for the specified patient. ACE indicates angiotensin‐converting enzyme.
Considerations in the Elderly A similar number of participants and nonparticipants identified increased pulse pressure as the characteristic of hypertension in the elderly (Figure 3).
Figure 3.
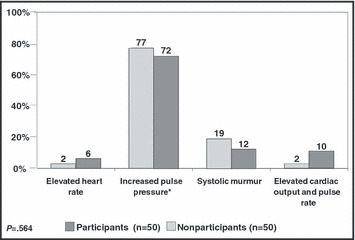
A similar number of participants and nonparticipants identified increased pulse pressure as the characteristic of hypertension in elderly patients (case 2). *Characteristic of hypertension in the elderly.
Medication Nonadherence In the management of a patient who did not take her antihypertensive medication as prescribed, a number of strategies to improve adherence were offered. A significantly greater number of participants vs nonparticipants agreed that a variety of options was necessary to improve adherence. Decreasing medication‐associated cost and providing language and literacy‐appropriate patient information were perceived as important factors by both groups. However, participants rated decreasing the complexity of the medical regimen (P=.001), selecting fixed‐dose combinations (P=.002), and maintaining contact with patient/family (P=.011) as strategies that were more likely to improve medication adherence compared with nonparticipants.
Barriers to Managing Hypertension The survey included a section on physicians’ perceived barriers in the management of hypertensive patients (Figure 4). Statistically significant differences were observed in the responses received from participants vs nonparticipants in the areas of patient adherence to the prescribed regimen (P=.015), patient adherence to lifestyle modifications (P=.095), and reluctance of physicians to intensify therapy despite uncontrolled BP (P=.037).
Figure 4.
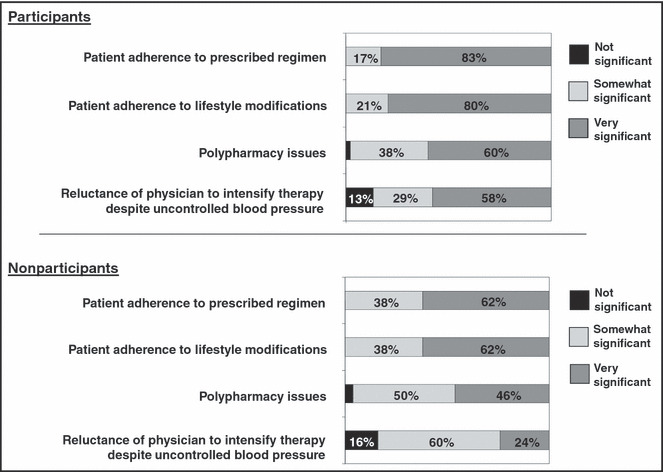
All barriers to managing hypertension were rated as being very significant by a considerably greater number of participants compared with nonparticipants.
Educational Impact of the Program
Calculated educational impact or the likelihood for a patient seen by physicians who participated in STOP Hypertension NOW! Recognize & Manage Your High‐risk Patients to receive evidence‐based care was 52%. Based on the average number of patients with hypertension seen weekly by the 588 health care providers who attended the educational activity, these data indicate that at least 22,304 hypertensive patients are 52% more likely to receive evidence‐based care than those seen by health care providers who did not participate in the activity. 15
Discussion
There is a growing need to better characterize the impact of CME on physician knowledge, competency, and practice performance, as well as patient outcomes. 16 We present data demonstrating that physicians who participated in STOP Hypertension NOW! Recognize & Manage Your High‐risk Patients acquired increased knowledge and competency in a variety of areas related to the management of hypertension. This CME activity was also associated with a projected increase in physician performance, as physicians who attended this educational activity are 52% more likely to provide evidence‐based medicine to their patients, as indicated by the education index. Areas that have been most affected by the received education include:
-
•
Recognizing BP goal based on JNC 7 guidelines for the management of hypertension.
-
•
Optimally treating BP in an elderly patient with severe systolic hypertension and diabetes or in a patient with a prior cerebrovascular accident.
-
•
Identifying the group of patients at the highest risk for stroke.
-
•
Optimally treating BP in a patient with stage 1 hypertension.
-
•
Initiating appropriate first‐line therapy for an African American patient with newly diagnosed hypertension.
-
•
Identifying strategies to improve adherence to antihypertensive medications.
Our outcomes methodology relies on the assessment of the responses to a series of case vignette questions from physicians who participated in a CME activity and comparison of these responses with those obtained from a comparable group of physicians who did not receive the same education. Greater emphasis on high‐level outcomes in literature discussing adult learning has challenged CME providers to find ways to accurately evaluate the impact of educational activities on physician competency and performance. The impact of physician education on patient outcomes is the ultimate end point. Assessing quality must ultimately rely on measures that are reliable, able to adequately control for case‐mix variation, and preferably inexpensive. Abstracted charting has been increasingly used, but data may be subject to recording bias because of time constraints on outpatient visits and limited possibility of adjustment for case‐mix variation, limiting direct comparisons of quality of care across different sites or delivery systems. 17 Recently, Walden and colleagues 18 used de‐identified claims data to evaluate change in physician ability to diagnose myelodysplastic syndromes as a result of attending an educational activity. While this methodology can accurately report impact on patient care, it is highly dependent on variable insurance reporting systems, which may delay or alter data collection. Case vignettes have gained considerable support for their value in predicting physician practice patterns. Results of recent research studies have demonstrated that case vignettes are a valid and comprehensive method for measuring a physician’s process of care in actual clinical practice, compared with chart review and standardized patients. In addition, case vignettes are more cost‐effective and less invasive than other means of measurement. 17 , 19
Studies have shown that educational formats can have variable effects on physician competency, performance, and ultimately patient care. 16 A 2007 meta‐analysis of more than 68,000 literature citations by the Agency for Healthcare Research and Quality demonstrated greater efficacy on short‐ and long‐term behaviors with live vs print media, interactive vs noninteractive techniques, and multimedia vs single media. 20 Performance improvement (PI) CME, approved by the American Medical Association, has recently come as an outstanding mean to impact physician practice by providing continuous learning and reinforcement on a timely basis. However, PI CME is a costly initiative and can impact a limited number of physicians at a given time. 21 The instructional approach used in the STOP Hypertension NOW! conference series is different than the traditional didactic presentations of many CME programs. These mini‐conferences were highly interactive, with the agenda broken into teaching modules. Each module emphasized faculty‐participant interactions via discussion of clinical practice preferences and responses to knowledge or competency‐based ARS questions and ample time for open discussion. Lectures were brief, focusing on data that were most applicable to practice. This format ensured that the presentations were short and crisp, with rapid changes in topic to avoid monotony and keep the audience alert and engaged, as emphasized in a variety of instructional models. Our approach allowed for approximately 600 physicians to receive the education, hence impacting the care of more than 22,000 patients.
We found that participants in our hypertension series became more knowledgeable regarding JNC 7 guideline recommendations and hypertension management strategies for a variety of patient populations. The impact of CME activities on physician knowledge is the most documented effect in the CME literature. For example, Bruno and colleagues 22 found that participation in a live peer‐to‐peer CME activity was effective for increasing pulmonologists’ knowledge on the diagnosis and management of idiopathic pulmonary fibrosis. Immediate learning evaluated by comparison of participant response patterns before and after a day‐and‐a‐half immersion course on sleep quality was reported by Dimor. 23
Results from our study also showed that program participation resulted in increased competency in recognizing patient BP goals, choosing the most appropriate therapy for specific patients based on guideline recommendations and efficacy studies and implementing ways to improve medication adherence. With shift in focus from increasing knowledge to increasing competency, the past few years have seen few data documenting the effect of CME on physician ability to provide the best health care. For example, Peterson and coworkers 24 showed that participation in a 2‐day course resulted in a significant increase in self‐assessed competency. Participants who reported substantial gains in competency were more likely than nonparticipants to make appropriate evidence‐based management decisions. In our study, the quality of education index of 52% suggested that increased physician competency will directly translate in an increased likelihood to provide evidence‐based and guideline‐driven health care. Improved physician performance leading to improved patient care and patient outcomes was reported after a CME program on pediatric asthma management. Compared with the control group, patients of physicians who attended the program on asthma management showed improvement in symptoms and health care utilization. 25
Our survey allowed for assessment of perceived barriers to the optimal management of hypertensive patients. It was found that low adherence to management strategies by patients and physician reluctance to intensify therapy (clinical inertia) were perceived as important barriers by both participant and nonparticipant groups. These findings highlight a need for education on these topics to empower care providers to successfully overcome these barriers and provide optimal care. We also found that participants’ awareness of the various barriers was greater than that of nonparticipants, demonstrating the efficacy of CME for increasing awareness and impacting physician ability to overcome barriers to optimal hypertension management.
Strengths and Limitations
While illustrating the potential impact of CME on patient care, our large effect size may have been affected by the methodology. In this study, participants completed the case vignette surveys directly after the program, thereby capturing immediate improvements in knowledge, competency, and intention to change practice behavior. Surveying participants weeks or months following an educational activity is favored as a mean for assessing long‐term retention, as well as to evaluate performance change that occurred after physicians return to practice. We chose to collect the completed survey immediately after the program to promote physician willingness to participate, but doing so may have increased the educational impact level. If the physicians had been surveyed after their return to practice, one would expect a different level of educational impact. Nevertheless, our data project an impact on physician behavior and strongly support the benefits of CME for improving the delivery of guideline‐recommended patient care.
Funding for the educational activity was provided by a pharmaceutical company, and one could question the objectivity of the content that was presented during the live programs or the objectivity of the data presented in this paper. In the current CME environment, a lack of objectivity is highly unlikely. CME providers are placed under strict scrutiny from the accredited bodies to provide certified CME that is fair balanced and free of commercial bias. Strict and specific processes, including development of content in absence of industry influence and peer review of the content, have been implemented to guarantee absence of commercial bias. In addition, we required that the steering committee members and faculty presenters disclose all financial relationships or affiliation with any commercial entity to the audience to ensure full transparency. Finally, random selection of the survey participants ensured the objectivity of the data reported in this study.
Conclusions
Participation in a half‐day, highly interactive CME activity is associated with increased physician knowledge in the management of hypertension, as well as increased likelihood for patients to receive evidence‐based care by the physicians who participated. Although additional data are needed to fully characterize the impact of CME, our data contribute to increase the current understanding of the effect of CME on physician knowledge, competency, and performance, and highlight the importance of CME in improving patient care.
Acknowledgments
Acknowledgments and disclosures : The STOP Hypertension NOW! Recognize & Manage Your High‐risk Patients meeting series was supported by an educational grant from Novartis Pharmaceuticals. Carole Drexel, PhD; Kathy Merlo, BA; Barry Watkins, PhD; Ben Whitfield, MA; Jay M. Katz, MA; Brad Pine, BA; Tom Sullivan, BS: nothing to disclose. Jan N. Basile, MD: grant/research support: NHLBI (ACCORD), NHLBI (SPRINT); consultant: Daiichi‐Sankyo, Forest, Novartis, Takeda; Speakers’ Bureau: AstraZeneca, Boehringer Ingelheim, Daiichi‐Sankyo, Forest, Novartis; major stock shareholder: none.
References
- 1. Lloyd‐Jones D, Adams R, Adams TR, et al. Heart disease and stroke statistics 2010 update: a report from the American Heart Association. Circulation. 2010;121:e46–e215. [DOI] [PubMed] [Google Scholar]
- 2. Lloyd‐Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics – 2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:e21–e181. [DOI] [PubMed] [Google Scholar]
- 3. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 Report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 4. Kannel WB. Risk stratification in hypertension: new insights from the Framingham Study. Am J Hypertens. 2000;13:3S–10S. [DOI] [PubMed] [Google Scholar]
- 5. Neal B, MacMahon S, Chapman N. Effects of ACE inhibitors, calcium antagonists, and other blood‐pressure‐lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists’ Collaboration. Lancet. 2000;356:1955–1964. [DOI] [PubMed] [Google Scholar]
- 6. Cushman WC, Basile J. Achieving blood pressure goals: why aren’t we? J Clin Hypertens. 2006;8:865–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ardery G, Carter BL, Milchak JL, et al. Explicit and implicit evaluation of physician adherence to hypertensive guidelines. J Clin Hypertens. 2007;9:113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Okonofua EC, Simpson KN, Jesri A, et al. Therapeutic inertia is an impediment to achieving the Healthy People 2010 blood pressure control goals. Hypertension. 2006;47:345–351. [DOI] [PubMed] [Google Scholar]
- 9. Berlowitz DR, Ash AS, Hickey EC, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339:1957–1963. [DOI] [PubMed] [Google Scholar]
- 10. Oliveria SA, Lapuerta P, McCarthy BD, et al. Physician‐related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162:413–420. [DOI] [PubMed] [Google Scholar]
- 11. Andrade SE, Gurwitz JH, Field TS, et al. Hypertension management: the care gap between clinical guidelines and clinical practice. Am J Manag Care. 2004;10:481–486. [PubMed] [Google Scholar]
- 12. Overstreet KM, Eidsvoog KE, Orsetti RF, et al. Educational interventions and outcomes – a literature review of CME regarding Institute of Medicine (IOM) competencies. CE Meas. 2006;1:17–26. [Google Scholar]
- 13. Davis D, Evans M, Jadad A, et al. The case for knowledge translation: shortening the journey from evidence to effect. BMJ. 2003;327:33–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Davis D, O’Brien MAT, Freemantle N, et al. Impact of formal continuing medical education. JAMA. 1999;282:867–874. [DOI] [PubMed] [Google Scholar]
- 15. Colliver JA. Call for greater emphasis on effect‐size measures in published articles in Teaching and Learning in Medicine . Teach Learn Med. 2002;14:206–210. [DOI] [PubMed] [Google Scholar]
- 16. Kahn N, Bagley B, Tyler S. Performance improvement CME: core of the new CME. AMA CPPD Report. 2007;22:1–3. [Google Scholar]
- 17. Peabody JW, Luck J, Glassman P, Dresselhaus TR, Lee M Comparison of vignettes, standardized patients, and chart abstraction: a prospective validation study of 3 methods for measuring quality. JAMA. 2000;283:1715–1722. [DOI] [PubMed] [Google Scholar]
- 18. Walden P, Dennison B, Hane C, et al. Administrative health data to assess performance in a myelodysplastic syndromes CME initiative. CE Meas. 2010;4:26–33. [Google Scholar]
- 19. Peabody JW, Luck J, Glassman P, et al. Measuring the quality of physician practice by using clinical vignettes: a prospective validation study. Ann Intern Med. 2004;141(10):771–780. [DOI] [PubMed] [Google Scholar]
- 20. Marinopoulos SS, Dorman T, Ratanawongsa N, et al. Effectiveness of Continuing Medical Education. Evidence Report/Technology Assessment No. 149 (Prepared by the Johns Hopkins Evidence‐based Practice Center, under Contract No. 290‐02‐0018.) AHRQ Publication No. 07‐E006. Rockville, MD: Agency for Healthcare Research and Quality. January 2007. [Google Scholar]
- 21. Stowell SA, Bongiorno Karcher R, Carter RD, et al. Outcomes measurement design for a performance improvement initiative in diabetes care. CE Meas. 2009;3:76–83. [Google Scholar]
- 22. Bruno TO, Miller S, Rand K, et al. Impact of a continuing medical education program on physician knowledge about idiopathic pulmonary fibrosis: analysis of an educational outcomes initiative. CE Meas. 2007;1:46–53. [Google Scholar]
- 23. Dimor M. Outcomes: using multiple measurements to determine effectiveness: a case report. CE Meas. 2008;2:35–36. [Google Scholar]
- 24. Peterson ED, Lulejian A, Laussucq S. Using perceived self‐efficacy to measure outcomes: evaluation of a two‐day course. CE Meas. 2007;1:59–64. [Google Scholar]
- 25. Cabana MD, Slish KK, Evans D, et al. Impact of physician asthma care education on patient outcomes. Pediatrics. 2006;117:2149–2157. [DOI] [PubMed] [Google Scholar]


