Coronavirus disease-2019 (COVID-19) is among the greatest medical challenges, provoking pulmonary manifestations and cardiovascular consequences. In this study, we compared cardiac injury between patients with myocarditis and COVID-19 and those with myocarditis without COVID-19.
All consecutive patients (March 2020 to April 2021) who recovered from COVID-19 (confirmed on reverse-transcriptase polymerase chain reaction swab test) referred to 1 of 5 cardiovascular magnetic resonance (CMR) centers because of suspected myocarditis and cardiac symptoms were prospectively enrolled in the study group (n = 300). Afterward, a retrospective non-COVID-19 myocarditis (2018-2019) group was enrolled (n = 150). Patients with histories of myocardial infarction or coronary artery disease, significant valve diseases, congenital heart diseases, cardiomyopathy, or previous cardiac surgery were not included. The CMR images were acquired on 1.5-T systems (Optima MR450w [GE Healthcare], Magnetom Aera [Siemens], or Magnetom Avanto [Siemens]) with a dedicated phased-array cardiac coil or body matrix coil. The cardiac CMR studies were electrocardiographically gated, performed during a breath hold, and based on routine clinical protocols according to guidelines. The scanning protocol included: 1) functional sequences using conventional noncontrast multiplanar cine acquisitions (steady-state free precession); 2) edema imaging: T2-weighted triple inversion recovery (short-tau inversion recovery); and 3) viability imaging: late gadolinium enhancement (LGE) 10 to 15 minutes after contrast injection (0.1 mmol/kg body weight of Gadovist [Bayer]). The study was conducted in accordance with the principles of the Declaration of Helsinki and the local ethics committees (Medical Universities of Silesia and Gdansk).
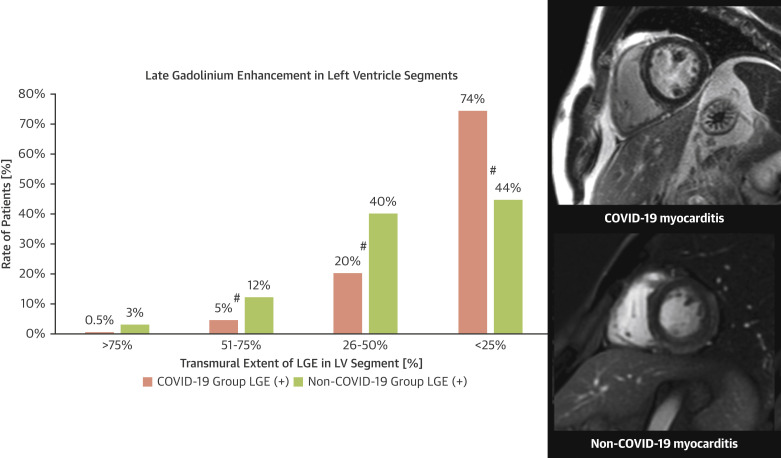
The COVID-19 study group included 300 patients who had COVID-19 a mean of 10.7 ± 4.8 weeks earlier. All studies were performed within 6 months of COVID-19 onset, and the clinical manifestation of infection was mostly moderate (83 patients required hospitalization). The COVID-19 group included slightly older patients (mean age 45.6 ± 12 years vs 42.8 ± 14 years; P = 0.03), with no other clinical differences compared with the non-COVID-19 group. Our study confirmed myocarditis-like LGE in 51% of post-COVID-19 patients, with no relation to primary symptoms or hospitalization during COVID-19. We found dilatation (8%) and moderate (5%) or severe (2%) systolic dysfunction of the left ventricle with mainly segmental (not global) wall motion abnormalities (14%). Most left ventricular (LV) segments (74.5%) showed a minor (<25%) transmural extent of LGE (Figure 1 ). Patients with COVID-19 and myocarditis showed a similar number of injured segments (4.2 ± 4.4 vs 4.3 ± 2.9; P = 0.82), smaller total LV LGE (7.2% ± 7.1% vs 9.66% ± 8.1%; P < 0.01), lower LV end-diastolic volume (149 ± 41 mL vs 166.8 ± 58 mL; P < 0.01), limited functional consequence (ejection fraction 59.5% ± 8.7% vs 55.6% ± 12.7%; P < 0.01) and a higher rate of pericarditis (15% vs 7%; P = 0.03) compared with non-COVID-19 myocarditis. Only wall motion score index (WMSI) showed weak predictive power for LV LGE (area under the curve [AUC]: 0.589; P < 0.001).
Figure 1.
LGE in the COVID-19 and Non-COVID-19 Groups
Transmural extent of late gadolinium enhancement (LGE) in left ventricular (LV) segments on cardiovascular magnetic resonance in patients with coronavirus disease-2019 (COVID-19) and non-COVID-19 myocarditis. #P < 0.05.
In this prospective multicenter study, we evaluated a large group of post-COVID-19 patients and showed prevalent myocardial injury, mostly with preserved LV systolic function. Clinical characteristics were not associated with the presence or severity of LGE or LV dysfunction. COVID-19-induced myocarditis showed a similar number of diseased LV segments but less severe LGE injury, lower rates of LV dysfunction, and more frequent pericarditis compared with the non-COVID-19 group.
A thorough search of published research confirmed that this is the first study to evaluate the differences between COVID-19 and non-COVID-19 myocarditis among patients sampled for clinical practice.
Our findings are consistent with the results of previous studies regarding positive CMR findings in COVID-19-related myocarditis, with small differences, which depend on the time and the severity of the disease (1, 2, 3). Puntmann et al (2) showed a higher rate of positive findings and myocardial inflammation on CMR (60%), irrespective of the clinical presentation or the time of acute COVID-19. However, a lower rate of post-COVID-19 myocardial injury (30%) was reported in 44 post-COVID-19 patients (3).
Hooper et al (4) reported an interesting large multicenter autopsy series of patients with COVID-19. As expected, patients had multiple pathological conditions, with acute myocardial dysfunction in 35%. Nevertheless, myocarditis was present in 6% of patients, which was the cause of death in only 4%. Our findings showing a high prevalence of LGE, but mild severity and minor functional consequences, are in line with the autopsy study. We also showed that LV wall motion abnormalities were found in only 16% of the COVID-19 study group. This suggests that echocardiographic screening misses a substantial number of COVID-19-related injuries on the basis of LV dysfunction and wall motion abnormalities, leading to wrong clinical conclusions.
The severity of the COVID-19-induced myocardial injury is smaller, and the rate of systolic dysfunction is lower and not dependent on clinical characteristics compared with non-COVID-19 myocarditis. Given the mean age of study patients, even mild residual myocardial injury plays a role in the progression to cardiomyopathy or heart failure. Regular follow-up of post-COVID-19 patients should verify the impact of residual injury on clinical outcomes.
Footnotes
This study was partially supported by the University Center of Maritime and Tropical Medicine (Gdynia, Poland) and the Medical University of Gdańsk (Gdańsk, Poland). The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Kotecha T., Knight D.S., Razvi Y., et al. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. Eur Heart J. 2021;42(19):1866–1878. doi: 10.1093/eurheartj/ehab075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Puntmann V.O., Carerj M.L., Wieters I., et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-2019) JAMA Cardiol. 2020;5(11):1265–1273. doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang H., Li R., Zhou Z., et al. Cardiac involvement in COVID-19 patients: mid-term follow up by cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2021;23:14–26. doi: 10.1186/s12968-021-00710-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hooper J.E., Padera R.F., Dolhnikoff M., et al. A postmortem portrait of the coronavirus disease 2019 (COVID-19) pandemic: a large multiinstitutional autopsy survey study. Arch Pathol Lab Med. 2021;145(5):529–535. doi: 10.5858/arpa.2020-0786-SA. [DOI] [PubMed] [Google Scholar]