Abstract
Biting midges of genus Culicoides (Diptera: Ceratopogonidae) are the vectors of several pathogenic arboviruses and parasites of humans and animals. Several reports have suggested that biting midges might be a potential vector of Leishmania parasites. In this study, we screened for Leishmania and Trypanosoma DNA in biting midges collected from near the home of a leishmaniasis patient in Lamphun province, northern Thailand by using UV-CDC light traps. The identification of biting midge species was based on morphological characters and confirmed using the Cytochrome C oxidase subunit I (COI) gene. The detection of Leishmania and Trypanosoma DNA was performed by amplifying the internal transcribed spacer 1 (ITS1) and small subunit ribosomal RNA (SSU rRNA) genes, respectively. All the amplified PCR amplicons were cloned and sequenced. The collected 223 biting midges belonged to seven species (Culicoides mahasarakhamense, C. guttifer, C. innoxius, C. sumatrae, C. huffi, C. oxystoma, and C. palpifer). The dominant species found in this study was C. mahasarakhamense (47.53%). Leishmania martiniquensis DNA was detected in three samples of 106 specimens of C. mahasarakhamense tested indicating a field infection rate of 2.83%, which is comparable to reported rates in local phlebotomines. Moreover, we also detected Trypanosoma sp. DNA in one sample of C. huffi. To our knowledge, this is the first molecular detection of L. martiniquensis in C. mahasarakhamense as well as the first detection of avian Trypanosoma in C. huffi. Blood meal analysis of engorged specimens of C. mahasarakhamense, C. guttifer, and C. huffi revealed that all specimens had fed on avian, however, further studies of the host ranges of Culicoides are needed to gain a better insight of potential vectors of emerging leishmaniasis. Clarification of the vectors of these parasites is also important to provide tools to establish effective disease prevention and control programs in Thailand.
Author summary
Culicoides are known to be vectors of several pathogens, including arboviruses and parasites. However, other investigations have demonstrated that Culicoides could be involved in the transmission of Leishmania and Trypanosoma parasites. Our studies demonstrated the first detection of L. martiniquensis in Culicoides mahasarakhamense and Trypanosoma sp., which is closely related to avian Trypanosome in C. huffi from an endemic area of leishmaniasis in northern Thailand. The finding of this work suggested that Culicoides biting midges are suspected to be the potential vector of L. martiniquensis and Trypanosoma parasites in Thailand.
Introduction
Culicoides Latreille are minute hematophagous insects belonging to the family Ceratopogonidae [1]. Several species play an important role in the transmission of arboviruses in domestic and wild ruminants, such as Bluetongue virus (BTV), Schmallenberg virus (SBV), African horse sickness virus (AHSV), Epizootic hemorrhagic disease virus (EHDV), and also in humans such as Oropouche virus (OROV) [2,3]. Apart from viruses, biting midges have been implicated as vectors of several protozoa such as Parahaemoproteus sp., Leucocytozoon sp., Hepatocytis, and filarial worms (Onchocerca cervicalis, Dipetalonema reconditum, Mansonella ozzardi, and M. perstans) [1,4]. Recent studies have demonstrated the capability of Leishmania and Trypanosoma parasites to develop in biting midges under laboratory conditions [5–9], suggesting they may also play a role in the transmission of these parasites in the field.
Leishmaniasis is a vector-borne disease that is caused by flagellated protozoa of the genus Leishmania. The disease is classified as a neglected tropical disease (NTDs) and is endemic in many parts of the world, especially in tropical and sub-tropical regions [10]. Twenty-one species have been described as affecting humans and these mostly belong to the subgenera Leishmania Ross 1903, Viannia Lainson & Shaw 1987 [11,12], and Mundinia Shaw, Camargo & Teixeira 2016 [13]. In Thailand, leishmaniasis is an emerging disease with the first autochthonous visceral leishmaniasis (VL) cases being reported in southern regions in 1996 [14]. The causative agents of autochthonous leishmaniasis in Thailand are Leishmania martiniquensis Desbois, Pratlong & Dedet 2014 [15,16] and L. orientalis Bate & Jariyapan 2018 (previously reported as "L. siamensis"), which both belong to L. subgenus Mundinia [17]. The disease has been reported in both immunocompetent and immunocompromised patients, especially in patients infected with human immunodeficiency virus (HIV) and is endemic in the southern, and the northern regions of the country [18].
The traditional vectors of Leishmania species are Phlebotomine sand flies (Diptera: Psychodidae), and initial attempts to identify the vectors of leishmaniasis in Thailand have focused on species of sand fly and detected L. martiniquensis in three species of Sergentomyia [18–21], and Phlebotomus stantoni [22].
Increasingly, however, ceratopogonid biting midges are being implicated in the transmission of Leishmania parasites. Becvar et al. [9] demonstrated that L. enriettii, L. macropodum, L. sp. strain GH5 from Ghana, L. orientalis, and four strains of L. martiniquensis (MAR1, Cu1, Cu2, and Aig1) successfully developed into metacyclic forms in the stomodeal valve (SV) of C. sonorensis. They additionally demonstrated transmission of L. sp. from Ghana, L. orientalis, and L. martiniquensis to mice by the bite of infected C. sonorensis. Dougall et al. [23] observed Leishmania metacyclic promastigotes in the midgut of two species of, Forcipomyia (Lasiohelea) midges in northern Australia. In addition, several reports have found Leishmania parasites in wild-collected Culicoides spp. [24–26].
Similarly, recent studies have implicated several species of Culicoides in the transmission of trypanosomes. Svobodová et al. [6] reported T. bennetii infection in wild-caught biting midges and demonstrated the development of T. avium and a species from the T. bennetii group in C. nubeculosus. Bernotiene et al. [8] were able to detect an unidentified species of Trypanosoma in 4 different species of Culicoides and T. avium in C. segnis; moreover, they also reported that T. everetti could develop in C. nubeculosus and C. impunctatus under laboratory conditions [8]. These reports suggest that biting midges may play a role in the transmission of these parasites which have traditionally been associated with tabanids, stable fly, tsetse flies, triatomine bugs, and sand flies [27–29].
Despite this mounting evidence, no investigations into the vectors of Leishmania and Trypanosoma parasites in Thailand have considered the potential role of biting midges. This study aims to assess the vector potential of Culicoides for Leishmania and Trypanosoma parasites in an endemic area in northern Thailand.
Materials and methods
Ethics statement
Experimental protocols of this study were approved by the animal research ethics committee of Chulalongkorn University Animal Care and Use Protocol (CU-ACUP), Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand (COA No. 019/2563).
Biting midge collection and morphological identification
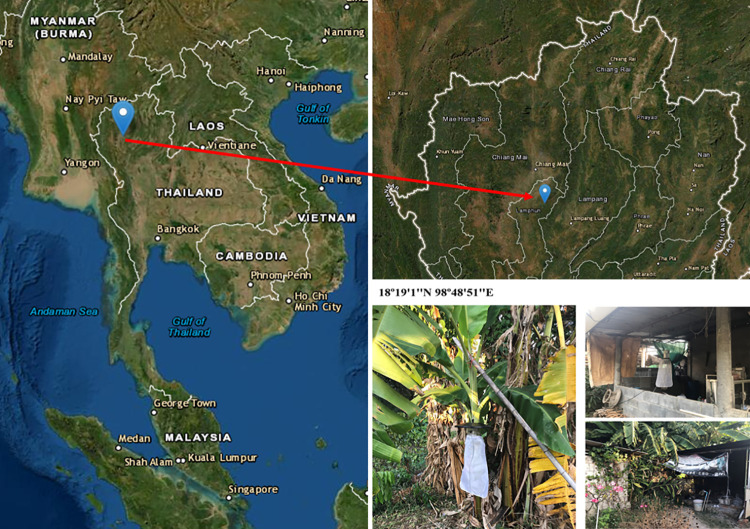
Biting midges were collected near the house of a leishmaniasis patient in Ban Hong district, Lamphun province, northern Thailand (18°19′1″N 98°48′51″E elevation 300 m) (Fig 1). The patient had AIDS associated with the clinical dissemination of cutaneous leishmaniasis. Biting midges were collected live from the house surroundings including chicken coops, stacks of firewood, and banana trees by using Center for Disease Control and Prevention (CDC) miniature light traps (25W bulb) with ultraviolet (UV) light between September 2019 and January 2020. Traps were operated from 6.00 pm to 6.00 am the following morning for two nights per month. All insects were anesthetized at -20°C for 30 min and transported to the laboratory. The female biting midges were examined under a stereomicroscope (Olympus, Tokyo, Japan), and separated from other insects based on morphological appearance. The samples were kept in liquid nitrogen and transported to the Vector Biology and Vector Borne Disease Research Unit, Department of Parasitology, Faculty of Medicine, Chulalongkorn University.
Fig 1. Map of northern Thailand showing the location of biting midge collection sites, including photographs of trap sites in Ban Hong district, Lamphun province, Thailand.
(map modified from public domain (https://earthexplorer.usgs.gov/) and photos taken by Padet siriyasatien, corresponding author.
For morphological identification, the head, wings, and genitalia were removed and mounted onto glass slides in a drop of sterilized normal saline and Hoyer’s medium before being examined under a compound microscope [30]. The remaining thorax and abdomen of biting midges were placed in a sterilized 1.5 ml microcentrifuge tube for DNA extraction. Female biting midges were identified using the keys and descriptions of Wirth and Hubert [31].
DNA extraction
Genomic DNA (gDNA) was extracted from thorax and abdomen of individual midges using a tissue DNA extraction kit (Invisorb Spin Tissue mini kit, STRATEC Molecular GmbH, Berlin, Germany) following the manufacturer’s instructions as modified by Srisuton et al. [21]. The quality of the obtained DNA concentrations of each sample was measured with Nanodrop 2000c (Thermo-Scientific, USA). The DNA sample was stored at -20°C until use in PCR investigation.
Molecular detection of Leishmania and Trypanosome parasites
The purified gDNA was used to detect Leishmania parasite DNA in conventional PCR with a primer set (LeF 5′-TCCGCCCGAAAGTTCACCGATA-3′ and LeR 5′-CCAAGTCATCCATCGCGACACG-3′) that targets the approximately 379 bp fragment of internal transcript spacer 1 (ITS1) region as previously described by Spanakos et al. [32]. PCR reactions were set at a total volume of 25 μl, containing 6 μl of gDNA, 10X PCR buffer, 25 mM of MgCl2 (Thermo Fisher Scientific, Walthman, MA, USA), 2.5 mM of dNTPs (GeneAll, Korea), 10 μM of each forward and reverse primer, and 1 unit of Taq DNA polymerase (Thermo Fisher Scientific, Walthman, MA, USA). The PCR cycles began with pre-denaturation at 95°C for 5 min, followed by 40 cycles of denaturation at 95°C for 1 min, annealing at 65°C for 1 min, extension at 72°C for 1 min. The final extension was performed at 72°C for 7 min.
In order to detect Trypanosoma DNA in biting midges, PCR amplification and reaction methods followed those of Srisuton et al. [21]. In this study, plasmid DNA containing ITS1 and SSU rRNA genes were used as positive controls in Leishmania and Trypanosoma detection respectively, and sterilized distilled water was used as a negative control.
Molecular identification of biting midges and blood meal analysis
The biting midge identifications were confirmed by analysis of the partial mitochondrial cytochrome C oxidase subunit I (COI) gene. The partial COI gene was amplified using the primers LCO1490 and HCO2198 [33] or C1-J-1718 and C1-N-2191 [34]. The PCR reaction and amplification profiles followed the protocols previously described in Harrup et al. [35] and Mathieu et al. [36]. Plasmid DNA containing COI gene of C. mahasarakhamense was used as the positive control and sterilized distilled water was used as a negative control.
The hosts of blood meals in engorged biting midges were identified by two PCR protocols for detection of mammal [37] and avian DNA [38]. Both PCR conditions were described in a previous study by Boonserm et al. [39].
Sequence analysis and phylogenetic construction
All positive PCR products were cloned into the pGEM-T Easy Vector (Promega, Mandison, WI, USA) followed the method described in Srisuton et al. [21], and the plasmid DNA was then isolated using the Invisorb Spin plasmid mini kit (STRATEC Molecular GmbH, Berlin, Germany) following the manufacturer’s instructions. The purified plasmid DNA was sequenced by the commercial service at Macrogen Inc., South Korea.
All sequences were truncated to obtain consensus sequences of each sample prior to alignment using the ClustalW multiple alignment program in BioEdit Sequence Alignment Editor Version 7.2.5 [40]. The consensus nucleotide sequences were compared to the previously published sequences in the GenBank database using the Basic Local Alignment Search Tool (BLAST) (https://blast.ncbi.nlm.nih.gov/Blast.cgi). Phylogenetic trees were constructed using the maximum likelihood method with 1000 bootstrap replications on Molecular Evolutionary Genetics Analysis software (MEGAX) [41].
Results
Biting midge species identification
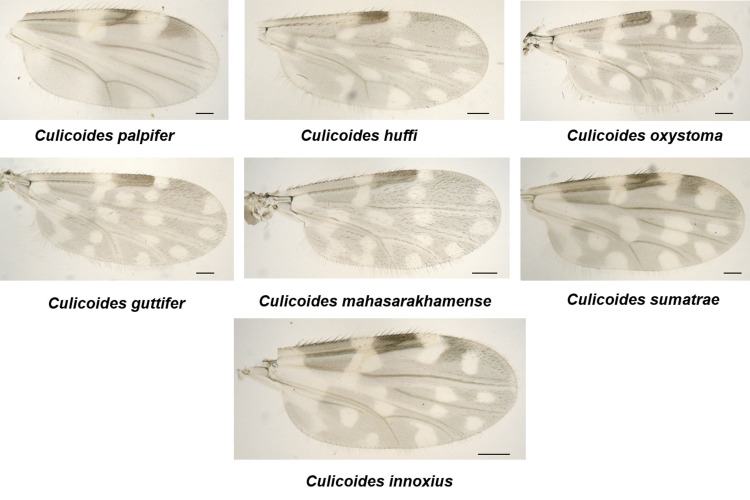
A total of 223 female biting midges belonging to seven species were captured and identified as Culicoides mahasarakhamense (47.53%), C. guttifer (22.87%), C. innoxius (12.56%), C. sumatrae (0.90%), C. huffi (9.42%), C. oxystoma (2.24%), and C. palpifer (4.48%) (Table 1). Fig 2 shows the wing patterns of representative specimens of these species.
Table 1. Number of biting midge species collected, tested, and found positive for DNA of Leishmania martiniquensis and Trypanosoma sp.
| Subgenus | Species identification | No. tested | ITS1-PCR | SSU rRNA-PCR |
|---|---|---|---|---|
| L. martiniquensis | Trypanosoma sp. | |||
| Meijerehelea | Culicoides mahasarakhamense | 106 | 3 | 0 |
| Culicoides guttifer | 51 | 0 | 0 | |
| Hoffmania | Culicoides innoxius | 28 | 0 | 0 |
| Culicoides sumatrae | 2 | 0 | 0 | |
| Clavipalpis group | Culicoides huffi | 21 | 0 | 1 |
| Remmia | Culicoides oxystoma | 5 | 0 | 0 |
| Trithecoides | Culicoides palpifer | 10 | 0 | 0 |
| Total | 223 | 3 | 1 | |
Fig 2. Photographs of representative specimens of the seven species of Culicoides found in this study, scale bar: 100 μm.
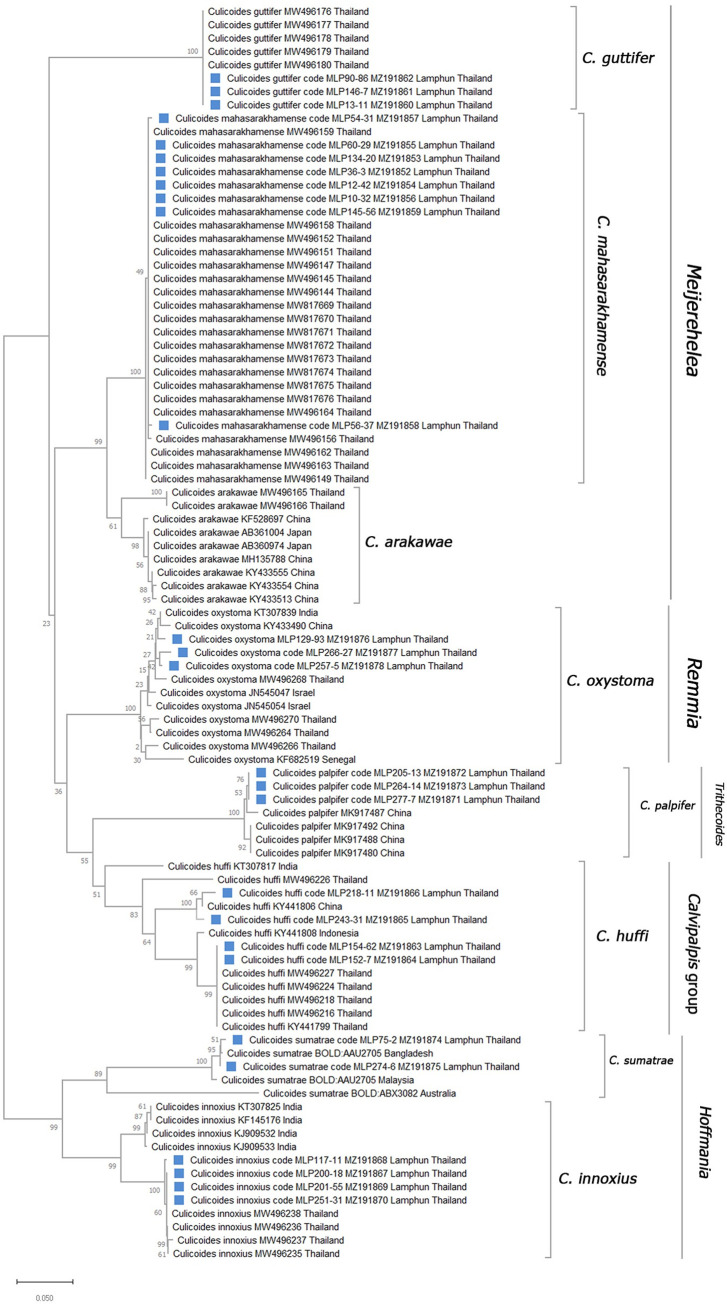
Of the 223 specimens tested for the presence of Leishmania and Trypanosoma parasites, the DNA of 27 were successfully used for COI amplification. These included 23 randomly selected to represent each morphologically identified species and the 4 specimens which were positive for parasite detection. The phylogenetic tree based on COI sequences was used to confirm the identifications of all specimens. The phylogenetic tree placed our specimens of C. mahasarakhamense, C. guttifer, C. innoxius, C. huffi, and C. oxystoma into clades with conspecific Culicoides species previously sequenced from Thailand (Fig 3). These sequences were submitted to the GenBank database under the GenBank accession numbers: MZ191852, MZ191853, MZ191854, MZ191855, MZ191856, MZ191857, MZ191858, and MZ191859 for C. mahasarakhamense; MZ191860, MZ191861, and MZ191862 for C. guttifer; MZ191863, MZ191864, MZ191865, and MZ191866 for C. huffi; MZ191867, MZ191868, MZ191869, and MZ191870 for C. innoxius; MZ191871, MZ191872, and MZ191873 for C. palpifer; MZ191874, and MZ191875 for C. sumatrae; MZ191876, MZ191877, and MZ191878 for C. oxystoma.
Fig 3. Maximum likelihood (ML) phylogenetic tree using the GTR+G+T model with 1,000 bootstrap replicates of partial COI sequences of Culicoides biting midges collected in this study and data from conspecific specimens available in GenBank database.
Detection of Leishmania, Trypanosoma, and host blood DNA in biting midges
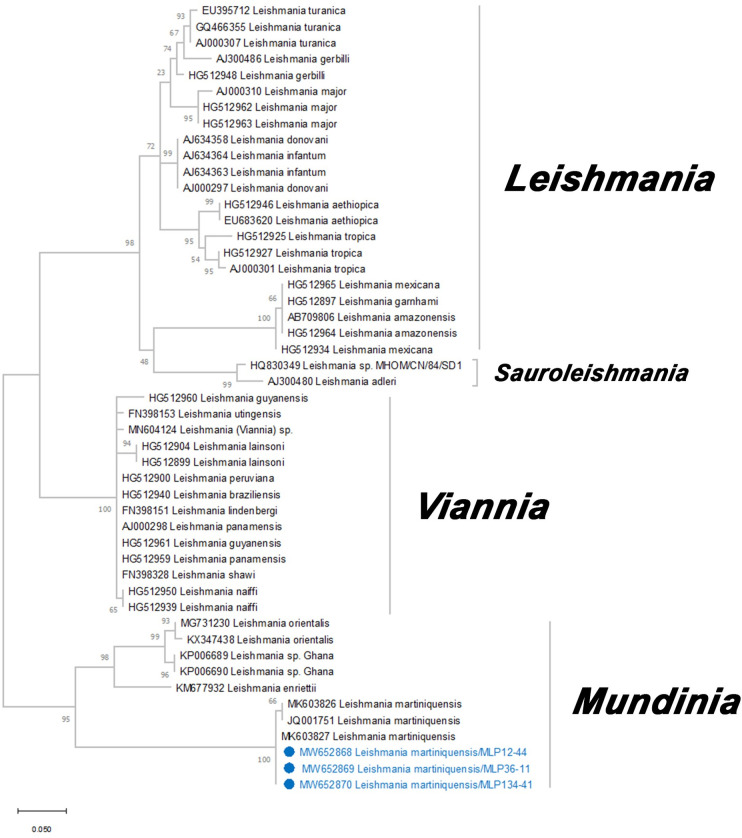
A total of 223 extracted DNA samples from biting midges were tested for the presence of Leishmania and Trypanosoma. Thirteen of these specimens contained a visible blood meal but no parasite DNA was detected in these specimens. Sequences from the ITS1-PCR amplification from 3 specimens of C. mahasarakhamense (MLP12-44, MLP36-11, and MLP134-41) were consistent with Leishmania DNA with nucleotide sequences of ITS1 gene of 379 bp in length. The BLAST results of these three ITS1 sequences showed a 100% similarity with L. martiniquensis sequence data from GenBank accession no. MK603827. This result was supported by the phylogenetic tree which showed that all three ITS1 sequences were clearly classified under L. martiniquensis with a bootstrap support value of 100% (Fig 4). The sequences of L. martiniquensis in this study were submitted to GenBank database (GenBank accession no. MW652868, MW652869, MW652870).
Fig 4. Maximum likelihood (ML) tree based on the K2+I model of nucleotide substitution of Leishmania spp. constructed from partial ITS1 gene sequences.
Bootstrap values are based on 1,000 replicates. Blue circles indicated samples that were obtained from this study.
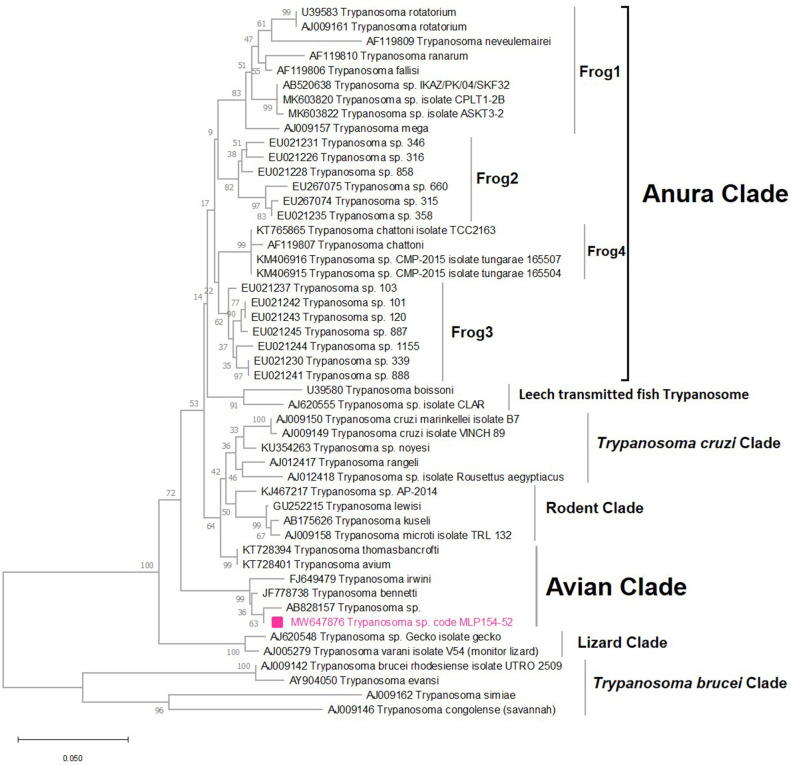
The conventional PCR specific to the SSU rRNA gene revealed a band of approximately 934 bp in one sample of C. huffi (MLP154-52). A BLAST result of this sequence demonstrated a 99.15% match with an unnamed species of Trypanosoma (GenBank accession no. AB828157) available in the GenBank database. These sequences were placed within a group of several clades formed by different species of Trypanosoma parasites including T. bennetti (GenBank accession no. JF778738), T. irwini (GenBank accession no. FJ649479), and the unnamed Trypanosoma sp. (GenBank accession no. AB828157) (Fig 5). The Trypanosome sequence obtained from this study was submitted to GenBank database under the GenBank accession number MW647876.
Fig 5. Maximum likelihood (ML) tree created using the TN93+G+I model with 1000 bootstrap replications from partial SSU rRNA sequences of Trypanosoma parasites from this study and reference sequences available in GenBank.
Sequences from this study are indicated with pink squares.
Host blood sources of engorged female specimens of C. mahasarakhamense (n = 4), C. guttifer (n = 2), and C. huffi (n = 7) were tested for the presence of host blood DNA. All of these specimens were found to contain avian DNA with no trace of mammalian DNA detected.
Discussion
This study is the first to investigate the potential role of biting midges as vectors of Leishmania or Trypanosoma in Asia. The detection of parasite DNA in field-collected midges satisfies one of the criteria for proving their status as vectors of these respective parasites but the remaining 3 criteria must be proven before a species can be categorized as a proven vector. These 4 criteria cited by Killick-Kendrick [42] are; (1) the vector will feed on man, and if the disease is zoonotic, the animal reservoir host; (2) it will support the development of the parasite after the infecting blood meal has been digested and voided; (3) parasites from wild-caught insects will be indistinguishable from isolates from vertebrate hosts; and (4) the insect will be able to transmit the parasite by bite.
One of these criteria requires an association between the vector, parasite, and reservoir host. For both of the protozoa detected in this study, however, the reservoir host is unclear although L. martiniquensis DNA was detected in black rats in one study in Thailand [20], and clinical symptoms noted in horses and cattle in Europe [43,44], and horses in North America [45]. There are no reports of leishmaniasis in cattle or horses in Thailand so it may be possible that these are dead-end rather than reservoir hosts. While there are records of the closely related species, C. arakawae, feeding on large mammals [46] there is no evidence of either C. arakawae or C. mahasarakhamense feeding on humans and this would need to be confirmed in C. mahasarakhamense if this species is to play an important role in the transmission of this parasite to humans.
Similarly, the trypanosome detected in C. huffi appears to be most closely related to species known to infect birds suggesting this species may also employ birds as reservoir hosts. The known host range of C. huffi is avian but this has only been reported in a single study [47] although our findings support this report. Additionally, the illustrations of Wirth & Hubert [31] indicate that the structure of the palpus and the number of sensilla coeloconica on the female antennae are consistent with a preference for feeding on birds [48–51].
Blood meal analysis from engorged female C. mahasarakhamense, C. guttifer, and C. huffi revealed that these specimens had all fed on avian hosts. In Thailand, Jomkumsing et al. [47] also found that the blood found in C. mahasarakhamense (reported as C. arakawae), C. guttifer, and C. huffi belonged to chickens. Presently, there is no evidence of Culicoides feeding on humans in Thailand although several species known to attack humans in other countries are present [31]. The potential vector status of Culicoides spp. for human diseases; however, indicates that further investigation of the host ranges of biting midges in Thailand is needed, especially in the endemic areas of leishmaniasis in the country.
The detection of L. martiniquensis in a species of biting midge provides further evidence that species of L. subgenus Mundinia are associated with this group of insects rather than solely dependant on Phlebotomine sand flies as are other subgenera of Leishmania [5,7,23]. L. martiniquensis DNA has been detected in four species of Sergentomyia gemmea, Se. barraudi, Se. khawi, and Ph. stantoni [18–22], suggesting that both midges and sandflies may potentially act as vectors of this parasite. The field infection rate of L. martiniquensis in C. mahasarakhamense detected in this study was 2.38% (3 positives from 106 tested) while that for Se. khawi and Ph. stantoni were a little higher at 5.41% and 12.5% [21,22], suggesting that C. mahasarakhamense may in fact play a similarly important role as Se. khawi and Ph. stantoni in the transmission of this parasite in Thailand. Field infection rates for the other 2 species of Sergentomyia found to harbor L. martiniquensis are difficult to assess as specimens were tested in pools rather than as individuals [18–20].
Similarly, the detection of a species of Trypanosoma in a biting midge supports previous reports that these insects may act as vectors of these parasites [6,8]. The field infection rate of Trypanosoma sp. in C. huffi detected here was 4.76% (1 positive in 21 tested) is which is comparable to rates found in other vectors for example black flies (2.13%) and sand flies (8.58%) but much lower than infection rates for triatomine bugs (55.2%) [21,52–54]. This suggests that C. huffi is potentially as important a vector as black flies and sand flies.
A total of 100 Culicoides species had been recorded in Thailand [55,56]. However, several of these species have been shown to contain cryptic species which are difficult to separate morphologically [48,55,57] so identification requires molecular analysis to clarify the cryptic species involved. Two such species are C. arakawae/ C. mahasarakhamense, and C. huffi making interpretation of the implications of these species as vectors difficult as it is unclear if published reports on the biology, distribution etc of these species refer to the cryptic species associated with these protozoa or to another of the cryptic species. Currently available information suggests that both C. mahasarakhamense and the haplotype of C. huffi found infected with Trypanosoma sp. are confined to Thailand. Should the distribution of either of these species be found to be more widely distributed in Asia then the distribution of their respective protozoa may be similarly widespread.
Analysis of COI barcodes proved a useful means of confirming identifications of 4 of the 7 species collected in this study. The ML tree analysis however indicates that our sequence data from specimens identified as C. innoxius, C. huffi, and C. palpifer differed to those reported by other workers suggesting of the presence of cryptic species. This is consistent with the findings of other studies in southeast Asia which have identified cryptic species amongst several taxa [47,57]. The COI sequence data provided here represent the first Thai data for C. sumatrae and C. palpifer.
Conclusion
This study is the first to report the detection of L. martiniquensis in C. mahasarakhamense and Trypanosoma sp. in C. huffi collected from a leishmaniasis endemic area in northern Thailand. Detection of both L. martiniquensis and Trypanosoma parasites in Culicoides biting midges suggests that they might be potential vectors of leishmaniasis and trypanosomiasis. Screening of wild-caught Culicoides biting midges for the presence of pathogens is a cost-effective method of identifying potential vectors which can then be targeted for more detailed laboratory studies to prove their vector competence. Knowledge of the vector is a key factor to assess the epidemiology of these diseases for better prevention and control measures in Thailand.
Data Availability
All data are in the manuscript.
Funding Statement
This research was supported by the Thailand Research Fund through the Royal Golden Jubilee Ph.D. Program (grant number PHD/0035/2561) to SS., the program Management Unit for Human Resources & Institutional Development, Research and Innovation (grant number B16F630071) to PS., Thailand Science Research Innovation (TSRI) (grant number FRB640001) to PS., Ratchadapisek Sompote Fund, Chulalongkorn University (grant number CU_GR_63_97_30_04) to PS., National Research Council of Thailand: CGEN (grant number N35A640452) to PS., and NIH/NIAID/CREID/07-049-7012-52338 to PS. The partial financial was supported from Research and Development Institute, Ramkhamhaeng University and TSRI fund (RU_64A112000009) to AT. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Mullen GR, Murphree CS, Biting midges (Ceratopogonidae). In: Mullen G.R., Durden L.A. (Eds.), Medical and Veterinary Entomology, 3rd edition. Elsevier, San Diego, CA, 2019. pp. 213–236. doi: 10.1111/mve.12352 [DOI] [Google Scholar]
- 2.Sakkas H, Bozidis P, Franks A, Papadopoulou C. Oropouche Fever: A Review. Viruses. 2018. Apr 4;10(4):175. doi: 10.3390/v10040175 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sick F, Beer M, Kampen H, Wernike K. Culicoides biting midges-underestimated vectors for arboviruses of public health and veterinary importance. Viruses. 2019. Apr 24;11(4):376. doi: 10.3390/v11040376 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prasad G, Bhatnagar PK. Acarines and insects of veterinary and medical importance. Bangalore: V National Training programme Centre of Advanced Studies, Department of Parasitology, Veterinary College; 2000. Culicoides: biology and transmission of viruses; pp. 34–38. [Google Scholar]
- 5.Seblova V, Sadlova J, Vojtkova B, Votypka J, Carpenter S, Bates PA, et al. The biting midge Culicoides sonorensis (Diptera: Ceratopogonidae) is capable of developing late stage infections of Leishmania enriettii. PLoS Negl Trop Dis. 2015. Sep 14;9(9):e0004060. doi: 10.1371/journal.pntd.0004060 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Svobodová M, Dolnik OV, Čepička I, Rádrová J. Biting midges (Ceratopogonidae) as vectors of avian trypanosomes. Parasit Vectors. 2017. May 8;10(1):224. doi: 10.1186/s13071-017-2158-9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chanmol W, Jariyapan N, Somboon P, Bates MD, Bates PA. Development of Leishmania orientalis in the sand fly Lutzomyia longipalpis (Diptera: Psychodidae) and the biting midge Culicoides soronensis (Diptera: Ceratopogonidae). Acta Trop. 2019. Nov;199:105157. doi: 10.1016/j.actatropica.2019.105157 Epub 2019 Sep 3. . [DOI] [PubMed] [Google Scholar]
- 8.Bernotienė R, Iezhova TA, Bukauskaitė D, Chagas CRF, Kazak M, Valkiūnas G. Development of Trypanosoma everetti in Culicoides biting midges. Acta Trop. 2020. Oct;210:105555. doi: 10.1016/j.actatropica.2020.105555 Epub 2020 May 28. . [DOI] [PubMed] [Google Scholar]
- 9.Becvar T, Vojtkova B, Siriyasatien P, Votypka J, Modry D, Jahn P, et al. Experimental transmission of Leishmania (Mundinia) parasites by biting midges (Diptera: Ceratopogonidae). PLoS Pathog. 2021. Jun 11;17(6):e1009654. doi: 10.1371/journal.ppat.1009654 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steverding D. The history of leishmaniasis. Parasit Vectors. 2017. Feb 15;10(1):82. doi: 10.1186/s13071-017-2028-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akhoundi M, Kuhls K, Cannet A, Votýpka J, Marty P, Delaunay P, et al. A historical overview of the classification, evolution, and dispersion of Leishmania parasites and sandflies. PLoS Negl Trop Dis. 2016. Mar 3;10(3):e0004349. doi: 10.1371/journal.pntd.0004349 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Akhoundi M, Downing T, Votýpka J, Kuhls K, Lukeš J, Cannet A, et al. Leishmania infections: Molecular targets and diagnosis. Mol Aspects Med. 2017. Oct;57:1–29. doi: 10.1016/j.mam.2016.11.012 Epub 2017 Jan 31. . [DOI] [PubMed] [Google Scholar]
- 13.Espinosa OA, Serrano MG, Camargo EP, Teixeira MMG, Shaw JJ. An appraisal of the taxonomy and nomenclature of trypanosomatids presently classified as Leishmania and Endotrypanum. Parasitology. 2018. Apr;145(4):430–442. doi: 10.1017/S0031182016002092 Epub 2016 Dec 15. . [DOI] [PubMed] [Google Scholar]
- 14.Thisyakorn U, Jongwutiwes S, Vanichsetakul P, Lertsapcharoen P. Visceral leishmaniasis: the first indigenous case report in Thailand. Trans R Soc Trop Med Hyg. 1999. Jan-Feb;93(1):23–24. doi: 10.1016/s0035-9203(99)90166-9 . [DOI] [PubMed] [Google Scholar]
- 15.Pothirat T, Tantiworawit A, Chaiwarith R, Jariyapan N, Wannasan A, Siriyasatien P, et al. First isolation of Leishmania from Northern Thailand: case report, identification as Leishmania martiniquensis and phylogenetic position within the Leishmania enriettii complex. PLoS Negl Trop Dis. 2014. Dec 4;8(12):e3339. doi: 10.1371/journal.pntd.0003339 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chiewchanvit S, Tovanabutra N, Jariyapan N, Bates MD, Mahanupab P, Chuamanochan M, et al. Chronic generalized fibrotic skin lesions from disseminated leishmaniasis caused by Leishmania martiniquensis in two patients from northern Thailand infected with HIV. Br J Dermatol. 2015. Sep;173(3):663–670. doi: 10.1111/bjd.13812 Epub 2015 Jun 1. . [DOI] [PubMed] [Google Scholar]
- 17.Jariyapan N, Daroontum T, Jaiwong K, Chanmol W, Intakhan N, Sor-Suwan S, et al. Leishmania (Mundinia) orientalis n. sp. (Trypanosomatidae), a parasite from Thailand responsible for localised cutaneous leishmaniasis. Parasit Vectors. 2018. Jun 18;11(1):351. doi: 10.1186/s13071-018-2908-3 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leelayoova S, Siripattanapipong S, Manomat J, Piyaraj P, Tan-Ariya P, Bualert L, et al. Leishmaniasis in Thailand: A review of causative agents and situations. Am J Trop Med Hyg. 2017. Mar;96(3):534–542. doi: 10.4269/ajtmh.16-0604 Epub 2017 Apr 6. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kanjanopas K, Siripattanapipong S, Ninsaeng U, Hitakarun A, Jitkaew S, Kaewtaphaya P, et al. Sergentomyia (Neophlebotomus) gemmea, a potential vector of Leishmania siamensis in southern Thailand. BMC Infect Dis. 2013. Jul 19;13:333. doi: 10.1186/1471-2334-13-333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chusri S, Thammapalo S, Silpapojakul K, Siriyasatien P. Animal reservoirs and potential vectors of Leishmania siamensis in southern Thailand. Southeast Asian J Trop Med Public Health. 2014. Jan;45(1):13–19. . [PubMed] [Google Scholar]
- 21.Srisuton P, Phumee A, Sunantaraporn S, Boonserm R, Sor-Suwan S, Brownell N, et al. Detection of Leishmania and Trypanosoma DNA in field-caught sand flies from endemic and non-endemic areas of leishmaniasis in southern Thailand. Insects. 2019. Aug 2;10(8):238. doi: 10.3390/insects10080238 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sriwongpan P, Nedsuwan S, Manomat J, Charoensakulchai S, Lacharojana K, Sankwan J, et al. Prevalence and associated risk factors of Leishmania infection among immunocompetent hosts, a community-based study in Chiang Rai, Thailand. PLoS Negl Trop Dis. 2021. Jul 12;15(7):e0009545. doi: 10.1371/journal.pntd.0009545 ; PMCID: PMC8297947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dougall AM, Alexander B, Holt DC, Harris T, Sultan AH, Bates PA, et al. Evidence incriminating midges (Diptera: Ceratopogonidae) as potential vectors of Leishmania in Australia. Int J Parasitol. 2011. Apr;41(5):571–579. doi: 10.1016/j.ijpara.2010.12.008 Epub 2011 Jan 18. . [DOI] [PubMed] [Google Scholar]
- 24.Slama D, Haouas N, Remadi L, Mezhoud H, Babba H, Chaker E. First detection of Leishmania infantum (Kinetoplastida: Trypanosomatidae) in Culicoides spp. (Diptera: Ceratopogonidae). Parasit Vectors. 2014. Jan 25;7:51. doi: 10.1186/1756-3305-7-51 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rebêlo JM, Rodrigues BL, Bandeira MD, Moraes JL, Fonteles RS, Pereira SR. Detection of Leishmania amazonensis and Leishmania braziliensis in Culicoides (Diptera, Ceratopogonidae) in an endemic area of cutaneous leishmaniasis in the Brazilian Amazonia. J Vector Ecol. 2016. Dec;41(2):303–308. doi: 10.1111/jvec.12227 . [DOI] [PubMed] [Google Scholar]
- 26.Ríos-Tostado JJ, Castillo-Ureta H, Torres-Montoya EH, Torres-Avendaño JI, Olimón-Andalón V, Romero-Higareda, et al. Molecular detection of Leishmania (L.) mexicana (Kinetoplastida: Trypanostomatidae) DNA in Culicoides furens (Diptera: Ceratopogonidae) from an area with autochthonous canine leishmaniasis in Northwestern Mexico. Acta Parasitol. 2021. Sep;66(3):1055–1058. doi: 10.1007/s11686-021-00335-1 Epub 2021 Feb 8. . [DOI] [PubMed] [Google Scholar]
- 27.Lukeš J, Butenko A, Hashimi H, Maslov DA, Votýpka J, Yurchenko V. Trypanosomatids are much more than just Trypanosomes: Clues from the expanded family tree. Trends Parasitol. 2018. Jun;34(6):466–480. doi: 10.1016/j.pt.2018.03.002 Epub 2018 Mar 28. . [DOI] [PubMed] [Google Scholar]
- 28.Desquesnes M, Dargantes A, Lai DH, Lun ZR, Holzmuller P, Jittapalapong S. Trypanosoma evansi and surra: a review and perspectives on transmission, epidemiology and control, impact, and zoonotic aspects. Biomed Res Int. 2013;2013:321237. doi: 10.1155/2013/321237 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wamwiri FN, Changasi RE. Tsetse flies (Glossina) as vectors of human African Trypanosomiasis: A review. Biomed Res Int. 2016;2016:6201350. doi: 10.1155/2016/6201350 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hadj-Henni L, De Meulemeester T, Mathieu B, Depaquit J, Augot D. Taxonomic assessment of Culicoides brunnicans, C. santonicus and C. vexans (Diptera: Ceratopogonidae) in France: Implications in systematics. Infect Genet Evol. 2015. Jul;33:324–331. doi: 10.1016/j.meegid.2015.05.024 . [DOI] [PubMed] [Google Scholar]
- 31.Wirth WW, Hubert AA. The Culicoides of Southeast Asia (Diptera: Ceratopogonidae). Memoirs of the American Entomological Institute, 1989;44:1–508. [Google Scholar]
- 32.Spanakos G, Piperaki ET, Menounos PG, Tegos N, Flemetakis A, Vakalis NC. Detection and species identification of Old World Leishmania in clinical samples using a PCR-based method. Trans R Soc Trop Med Hyg. 2008. Jan;102(1):46–53. doi: 10.1016/j.trstmh.2007.05.019 . [DOI] [PubMed] [Google Scholar]
- 33.Folmer O, Black M, Hoeh W, Lutz R, Vrijenhoek R. DNA primers for amplification of mitochondrial cytochrome c oxidase subunit I from diverse metazoan invertebrates. Mol Mar Biol Biotechnol. 1994. Oct;3(5):294–299. [PubMed] [Google Scholar]
- 34.Dallas JF, Cruickshank RH, Linton YM, Nolan DV, Patakakis M, Braverman Y, et al. Phylogenetic status and matrilineal structure of the biting midge, Culicoides imicola, in Portugal, Rhodes and Israel. Med Vet Entomol. 2003. Dec;17(4):379–387. doi: 10.1111/j.1365-2915.2003.00454.x . [DOI] [PubMed] [Google Scholar]
- 35.Harrup LE, Laban S, Purse BV, Reddy YK, Reddy YN, Byregowda SM, et al. DNA barcoding and surveillance sampling strategies for Culicoides biting midges (Diptera: Ceratopogonidae) in southern India. Parasit Vectors. 2016. Aug 22;9(1):461. doi: 10.1186/s13071-016-1722-z . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mathieu B, Garros C, Balenghien T, Candolfi E, Delécolle JC, Cêtre-Sossah C. A phylogenetic analysis of the biting midges belonging to Culicoides Latreille (Diptera: Ceratopogonidae) subgenus Avaritia using molecular data. Parasit Vectors. 2020. May 12;13(1):243. doi: 10.1186/s13071-020-04111-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kent RJ, Norris DE. Identification of mammalian blood meals in mosquitoes by a multiplexed polymerase chain reaction targeting cytochrome B. Am J Trop Med Hyg. 2005. Aug;73(2):336–342. ; PMCID: PMC4147110. [PMC free article] [PubMed] [Google Scholar]
- 38.Cicero C, Johnson NK. Speciation in sapsuckers (Sphyrapicus): III. Mitochondrial-DNA sequence divergence at the cytochrome-b locus. The Auk. 1995;112:547–563 [Google Scholar]
- 39.Boonserm R, Jantorn R, Phumee A, Sor-suwan S, Jariyapan N, Tiawsirisup S, et al. Identification of blood meal from field collected filarial vector mosquitoes, Armigeres subalbatus by multiplex PCR. Thai J Vet Med. 2019;49(2):155–160. [Google Scholar]
- 40.Hall TA. BioEdit: A user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucl Acids Symp Ser. 1999; 41:95–98. [Google Scholar]
- 41.Kumar S, Stecher G, Li M, Knyaz C, Tamura K. MEGA X: Molecular evolutionary genetics analysis across computing platforms. Mol Biol Evol. 2018. Jun 1;35(6):1547–1549. doi: 10.1093/molbev/msy096 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Killick-Kendrick R. The biology and control of phlebotomine sand flies. Clin Dermatol. 1999. May-Jun;17(3):279–289. doi: 10.1016/s0738-081x(99)00046-2 . [DOI] [PubMed] [Google Scholar]
- 43.Müller N, Welle M, Lobsiger L, Stoffel MH, Boghenbor KK, Hilbe M, et al. Occurrence of Leishmania sp. in cutaneous lesions of horses in Central Europe. Vet Parasitol. 2009. Dec 23;166(3–4):346–351. doi: 10.1016/j.vetpar.2009.09.001 . [DOI] [PubMed] [Google Scholar]
- 44.Lobsiger L, Müller N, Schweizer T, Frey CF, Wiederkehr D, Zumkehr B,et al. An autochthonous case of cutaneous bovine leishmaniasis in Switzerland. Vet Parasitol. 2010. May 11;169(3–4):408–414. doi: 10.1016/j.vetpar.2010.01.022 . [DOI] [PubMed] [Google Scholar]
- 45.Reuss SM, Dunbar MD, Calderwood Mays MB, Owen JL, Mallicote MF, Archer LL, et al. Autochthonous Leishmania siamensis in horse, Florida, USA. Emerg Infect Dis. 2012. Sep;18(9):1545–1547. doi: 10.3201/eid1809.120184 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kang CH, Yu HS. Seasonal abundance and host blood meal sources of the genus Culicoides (Diptera: Ceratopogonidae) from cattle and poultry farms in Kyeonggi Province, Korea., Korean J Entomol. 1991, 21:29–36. [Google Scholar]
- 47.Jomkumsing P, Surapinit A, Saengpara T, Pramual P. Genetic variation, DNA barcoding and blood meal identification of Culicoides Latreille biting midges (Diptera: Ceratopogonidae) in Thailand. Acta Trop. 2021. May;217:105866. doi: 10.1016/j.actatropica.2021.105866 . [DOI] [PubMed] [Google Scholar]
- 48.Rowley WA, Cornford, M. Scanning electron microscopy of the pit of the maxillary palp of selected species of Culicoides. Can J Zool, 1972;50(9):1207–1210. doi: 10.1139/z72-162 [DOI] [Google Scholar]
- 49.Braverman Y, Hulley PE. Relationship between the numbers and distribution of some antennal and palpal sense-organs and host preference in some Culicoides (Diptera: Ceratopogonidae) from southern Africa. J Med Entomol. 1979;15:419–424, doi: [DOI] [Google Scholar]
- 50.Isberg E, Hillbur Y, Ignell R. Comparative study of antennal and maxillary palp olfactory sensilla of female biting midges (Diptera: Ceratopogonidae: Culicoides) in the context of host preference and phylogeny. J Med Entomol. 2013. May;50(3):485–492. doi: 10.1603/me12235 . [DOI] [PubMed] [Google Scholar]
- 51.Purse BV, Carpenter S, Venter GJ, Bellis G, Mullens BA. Bionomics of temperate and tropical Culicoides midges: knowledge gaps and consequences for transmission of Culicoides-borne viruses. Annu Rev Entomol. 2015. Jan 7;60:373–392. doi: 10.1146/annurev-ento-010814-020614 . [DOI] [PubMed] [Google Scholar]
- 52.Thaijarern J, Tangkawanit U, Wongpakam K, Pramual P. Molecular detection of Trypanosoma (Kinetoplastida: Trypanosomatidae) in black flies (Diptera: Simuliidae) from Thailand. Acta Trop. 2019. Dec; 200:105196. doi: 10.1016/j.actatropica.2019.105196 . [DOI] [PubMed] [Google Scholar]
- 53.Phumee A, Tawatsin A, Thavara U, Pengsakul T, Thammapalo S, Depaquit J, et al. Detection of an unknown Trypanosoma DNA in a Phlebotomus stantoni (Diptera: Psychodidae) collected from southern Thailand and records of new sand flies with reinstatement of Sergentomyia hivernus Raynal & Gaschen, 1935 (Diptera: Psychodidae). J Med Entomol. 2017. Mar 1;54(2):429–434. doi: 10.1093/jme/tjw161 . [DOI] [PubMed] [Google Scholar]
- 54.Shender LA, Lewis MD, Rejmanek D, Mazet JA. Molecular diversity of Trypanosoma cruzi detected in the vector Triatoma protracta from California, USA. PLoS Negl Trop Dis. 2016. Jan 21;10(1):e0004291. doi: 10.1371/journal.pntd.0004291 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pramual P, Jomkumsing P, Piraonapicha K, Jumpato W. Integrative taxonomy uncovers a new Culicoides (Diptera: Ceratopogonidae) biting midge species from Thailand. Acta Trop. 2021. Aug;220:105941. doi: 10.1016/j.actatropica.2021.105941 . [DOI] [PubMed] [Google Scholar]
- 56.Thepparat A, Bellis G, Ketavan C, Ruangsittichai J, Sumruayphol S, Apiwathnasorn C. Ten species of Culicoides Latreille (Diptera: Ceratopogonidae) newly recorded from Thailand. Zootaxa. 2015. Oct 21;4033(1):48–56. doi: 10.11646/zootaxa.4033.1.2 . [DOI] [PubMed] [Google Scholar]
- 57.Gopurenko D, Bellis GA, Yanase T, Wardhana AH, Thepparat A, Wang J, et al. Integrative taxonomy to investigate species boundaries within Culicoides (Diptera: Ceratopogonidae): a case study using subgenus Avaritia from Australasia and Eastern Asia. Vet Ital. 2015. Oct-Dec;51(4):345–378. doi: 10.12834/VetIt.515.2463.2 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are in the manuscript.