Abstract
Objective:
To determine if text message reminders regarding oral hygiene compliance have an influence on the level of compliance within an orthodontic population.
Materials and Methods:
In this prospective, randomized, controlled clinical trial, 42 orthodontic patients were assigned to a text message or control group. Parents of patients assigned to the text message group received a reminder text message one weekday each week. Oral hygiene compliance was measured using bleeding index (BI), modified gingival index (MGI), and plaque index (PI), and visual examination of white spot lesion (WSL) development at baseline (T0), two appointments after baseline (T1), and four appointments after baseline (T2).
Results:
BI, MGI, and PI scores were significantly lower in the text message group than in the control group at T2.
Conclusion:
A text message reminder system is effective for improving oral hygiene compliance in orthodontic patients.
Keywords: Oral hygiene, Text message, Orthodontics, Compliance
INTRODUCTION
Oral hygiene compliance is one of the most important factors controlled by the patient during orthodontic treatment. Previous studies have demonstrated a rapid decline in oral hygiene after the initial bonding, followed by an improvement by the fifth month of treatment.1 However, other studies have also shown that oral hygiene compliance is lowest at the end of orthodontic treatment, demonstrating the challenge in obtaining sustained and acceptable oral hygiene during therapy.2 Excessive plaque retention around brackets is the cause of WSL formation during orthodontic therapy.3 Inadequate pretreatment oral hygiene and poor oral hygiene during orthodontic therapy are associated with greater incidence and severity of WSLs.4 These undesired side effects can lead to unsatisfactory results or premature termination of orthodontic therapy.
Among factors that predict patients' compliance, only a limited number have been closely correlated to the demonstrated level of compliance.5 These factors include: a strong internal locus of control possessed by the patient, a strong interpersonal relationship between the orthodontist and patient, documentation of improvement in oral hygiene after detailed instruction, successful school performance by the patient, and positive parental attitudes toward treatment.1,5–7 However, only a few orthodontic studies have introduced interventions that could improve oral hygiene compliance, including reward systems and the use of the Hawthorne effect.6,8
In medicine and dentistry, active reminders have been reported to improve appointment attendance, adherence to medication schedules, and positive behavior changes.9–14 A 2009 systematic review of the influence of text messages on behavior changes in the medical field demonstrated positive behavior changes in 13 of the 14 studies that met the authors' inclusion criteria, including smoking cessation therapy, diabetes self-management, and anti-obesity behavior.11 In dentistry, postal, automated telephone, and text message reminders were effective in reducing appointment no-show rates.9,10,13,14 Additionally, text message follow-up sent from an orthodontic office following initial appliance placement resulted in lower levels of patient's self-reported pain.15 The influence of text message reminders on oral hygiene compliance has not been reported.
The aim of this study was to determine if there is a relationship between reminding patients of the importance of oral hygiene via weekly text message reminders sent to their parents/guardians and demonstrated oral hygiene compliance.
MATERIALS AND METHODS
For this prospective, randomized, clinical trial, approval was granted by the Virginia Commonwealth University Institutional Review Board. Subjects were required to be in active treatment at the VCU Department of Orthodontics with full fixed appliances in both arches, between the ages of 11 and 19, without any significant medical/dental history, and living full-time with a parent/guardian who owned a cellular telephone with text messaging services. Patients were excluded if they had health risks associated with periodontal probing or if their parents were not comfortable reading or speaking English.
During the consent/assent process, parents were notified that they would receive one text message each week for the duration of the study if their child was randomly assigned to the text message group. It was also made clear to them that their children would not receive study text messages. Additionally, parents and patients were made aware that their participation was voluntary and that they could freely withdraw at any time without any penalty or loss of benefits to which they were otherwise entitled.
At the start of treatment, all patients were given standardized oral hygiene instruction and received an oral hygiene kit that included a toothbrush, interproximal brush, floss, and mouthwash. In order to allow patients to adapt to oral hygiene with fixed appliances, they were not asked to enroll in this study until at least two appointments after bonding. At time point T0, baseline readings of the Ramfjord teeth (maxillary right first molar, maxillary left central incisor, maxillary left first premolar, mandibular left first molar, mandibular right central incisor, and mandibular right first premolar) were recorded for bleeding index (BI), modified gingival index (MGI), and plaque index (PI). A PDT Sensor Probe (Zila Pharmaceuticals, Fort Collins, Colo) was used to standardize periodontal probing force, and cheek retractors were placed to properly measure BI. At each time point, patients were permitted to brush upon arrival to their appointment with archwires and ligatures in place to eliminate bias related to appointment time.
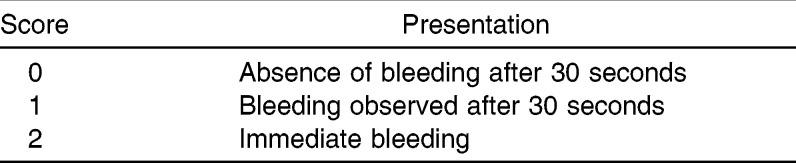
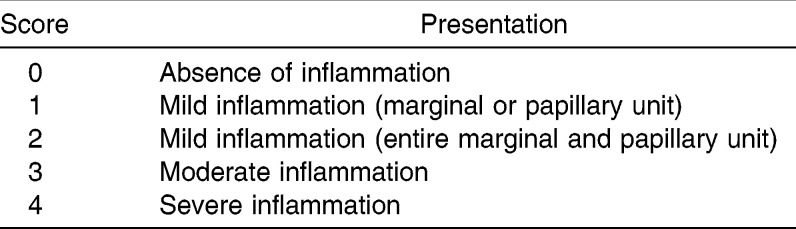
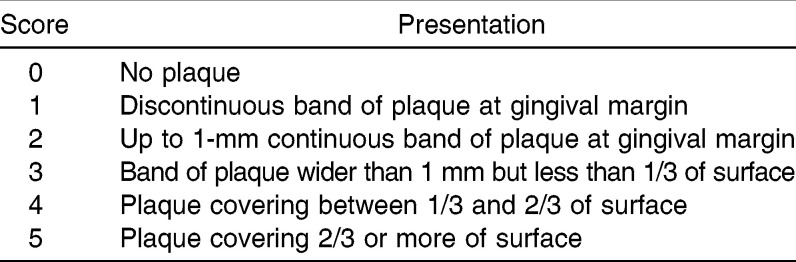
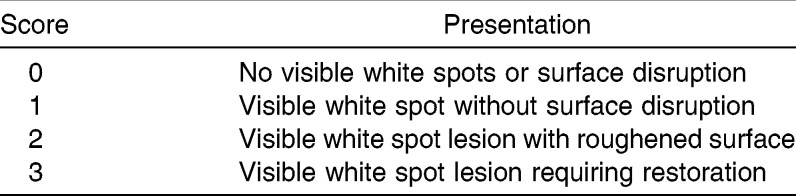
The BI was scored as described by Saxton and van der Ouderaa16 upon probing the mesio-buccal, direct buccal, and disto-buccal aspects of the gingival sulci of the Ramfjord teeth. BI scoring is described in Table 1.16 One MGI measurement of the buccal marginal gingiva for each Ramfjord tooth was scored as described in Table 2. One PI measurement was recorded for the buccal surface of each Ramfjord tooth according to the Turesky modification on the Quigley-Hein PI scoring system and is described in Table 3.17 Additionally, the presence of WSLs located on the buccal surface gingival to the archwire was examined visually on the maxillary and mandibular six anterior teeth after being air dried for 5 seconds. WSL scoring is described in Table 4.18
Table 1.
Bleeding Index (BI) Measurements
Table 2.
Modified Gingival Index (MGI) Measurements
Table 3.
Plaque Index (PI) Measurements
Table 4.
White Spot Lesion Measurements
Oral hygiene instruction and study measurements were performed by the same blinded examiner two appointments after baseline (T1) and four appointments after baseline (T2). The blinded examiner was calibrated for measurements by the VCU Department of Periodontics chief resident. After T2 study measurements were performed, patients were removed from study participation.
Subjects were randomly assigned to one of two groups, a text message or control group, using a block randomization protocol. One parent/guardian of each patient assigned to the text message group received a text message once weekly at 1715 hours from a cellular telephone that was only used for study text messages. Patients did not receive any direct text messages. Text messages were sent by one of the authors not involved in study measurements. The standardized text message was: “This is a message from the VCU Orthodontic Clinic reminding you that it is important to brush your teeth for 3 minutes after every meal or at least 3 times daily. Cleaning your teeth will help to keep them healthy and beautiful.” Parents/guardians of patients assigned to the control group did not receive study text messages.
Mean BI, MGI, and PI scores were compared between groups across three time points using repeated-measures mixed-model analysis of variance. WSLs were compared between groups across three time points using repeated-measures logistic regression after converting WSL into a No (score = 0) or Yes (score 1, 2, or 3). Because four measurements were compared, the significance level was set at P < .05/4 = 0.0125. SAS software was used for all calculations (SAS Institute Inc, Cary, NC).
RESULTS
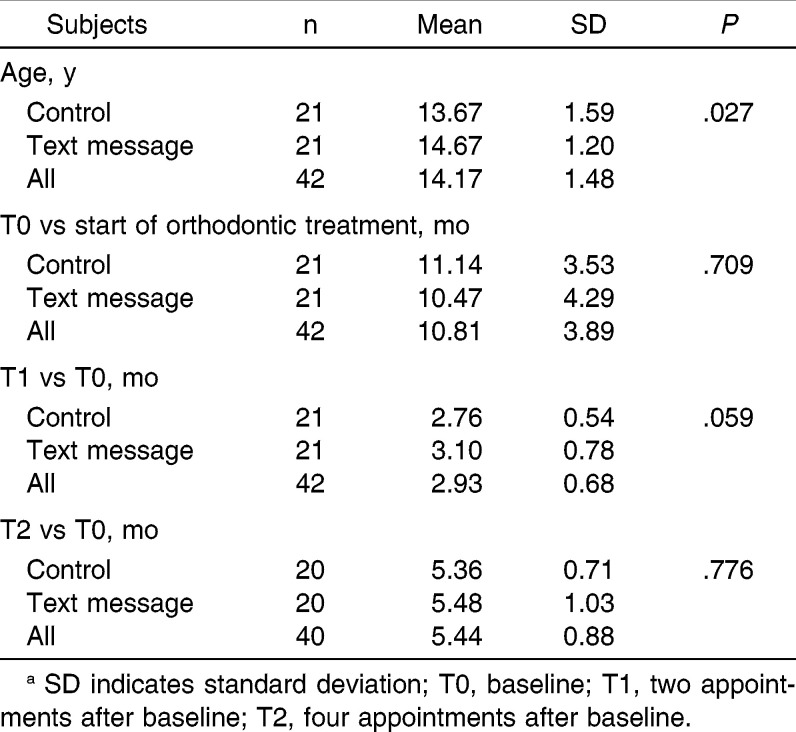
Of 45 consecutive patients that matched the inclusion/exclusion criteria, 42 patients and their parents consented to participate in the study. Following consent/assent, 42 subjects were randomly assigned to the text message or control group. Forty subjects completed all study measurements, as one subject from each group did not complete T2 evaluation because of inconsistent appointment attendance. Overall, there were 25 females and 17 males, with a mean age of 14.2 years, ranging from 11 to 18 years old. By chance alone, older subjects were assigned to the text message group (t-test P value = .027.) Table 5 shows a description of study participants in both groups. Subjects were enrolled an average of 10.81 months after bonding. T1 and T2 measurements were at two and four appointments after baseline, corresponding to a mean of 2.93 months and 5.44 months for these time points, respectively.
Table 5.
Description of Subjects in Each Groupa
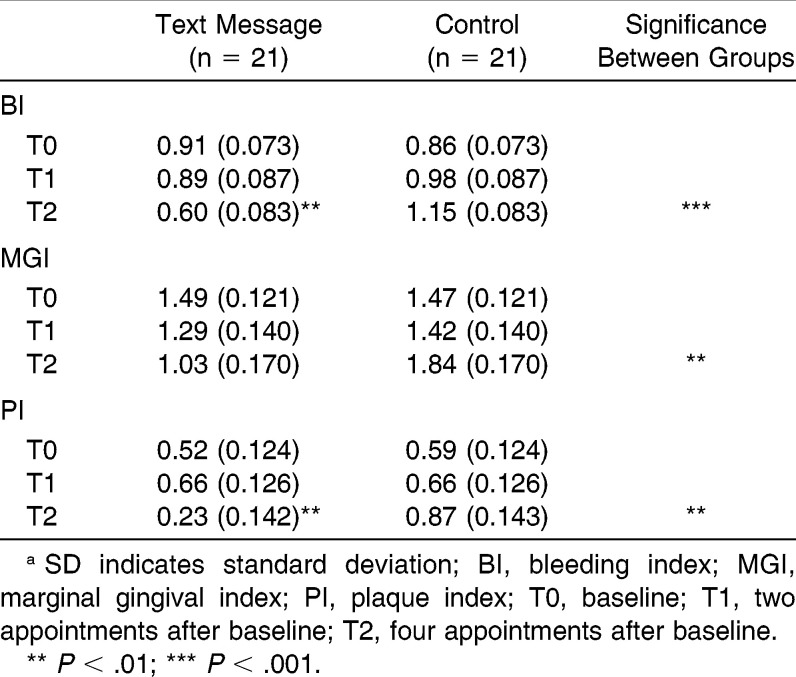
Table 6 shows BI, MGI, and PI scores for both groups at the three time points. There were no differences in scores between the groups at baseline (P > .5). Additionally, there were no baseline differences in these indices based on sex (P = .982) or age (P = .955). At T1, there were no BI, MGI, or PI differences between the groups. At T2, the text message group had significantly lower BI (P < .001), MGI (P = .002), and PI (P = .003) scores. None of these T2 differences were related to sex (P > .6) or age (P > .084). Within the groups, BI and PI improved over time in the text message group (P < .007) but did not change significantly within the control group.
Table 6.
Mean (SD) BI, MGI, and PI scores at T0, T1, and T2a
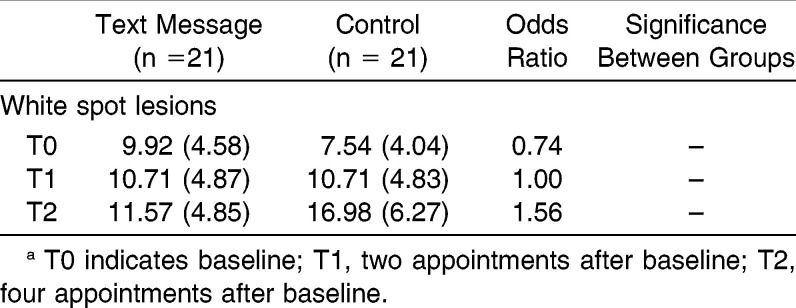
Table 7 shows the proportions of WSLs for each group and compares these proportions using odds ratios. There were no differences between the groups in prevalence of WSLs at any time point, and there were no significant changes within either group across the time points. The changes across time points in BI, MGI, PI, and proportions of WSLs are displayed in Figures 1–4, respectively.
Table 7.
Proportion of White Spot Lesions at T0, T1, and T2
Figure 1.
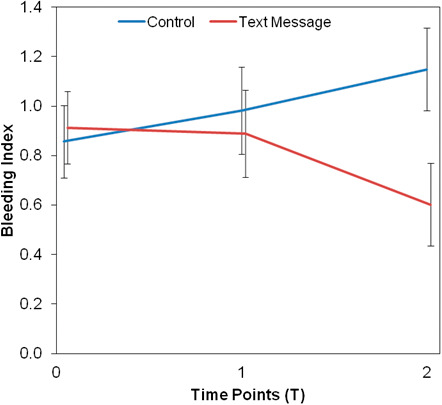
Treatment response for BI.
Figure 2.
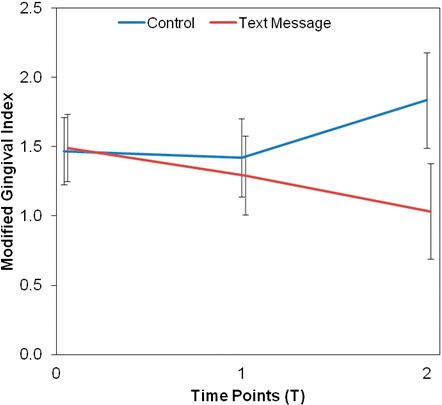
Treatment response for MGI.
Figure 3.
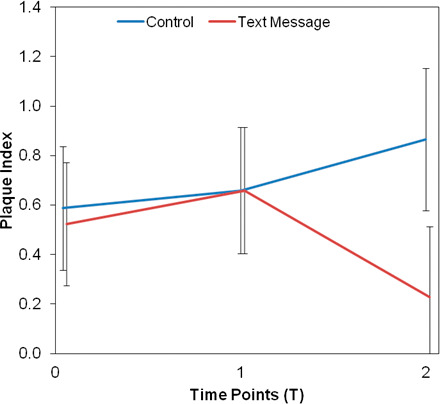
Treatment response for PI.
Figure 4.
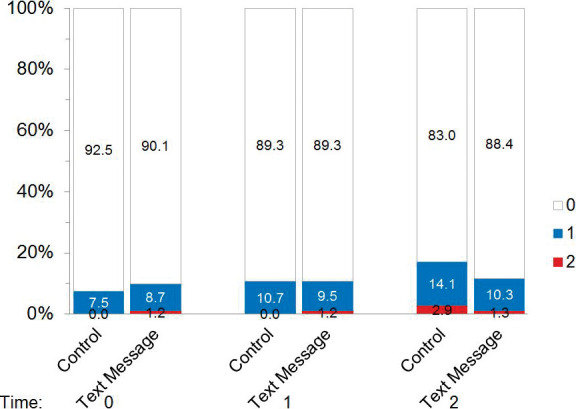
Summary of white spot lesions.
DISCUSSION
This study examined the effect of a weekly text message reminder emphasizing the importance of oral hygiene compliance that was sent to parents of patients. Outcome was assessed using BI, MGI, PI, and development of WSLs over time. The text message group demonstrated significantly lower BI, MGI, and PI scores at T2, which was four appointments or an average of 5.44 months after baseline (T0). According to the social psychology literature, it takes a median time of 66 days to turn a behavior into an automatic habit.19 This lag time in habit formation may explain why differences in oral hygiene measures were not seen at T1, which was two appointments after baseline.
BI is a strong indicator of oral hygiene compliance, as it has been shown to have high sensitivity and specificity in evaluating periodontal health.20,21 Additionally, MGI has shown high sensitivity for assessing resolution and progression of gingivitis.22 Studies have indicated that MGI and BI correlate well and should produce comparable results when used together in a clinical trial.22 Therefore, significantly lower BI and MGI scores in the text message group at T2 should be viewed as strong evidence of the effectiveness of the text messaging.
Although WSL development has been reported to occur in as little as 2 to 3 weeks after plaque accumulation in buccogingival areas of the teeth, in this 5.44-month clinical trial, significant differences in gingival health indices did not lead to significant differences in WSL development.23 Despite this, WSL development in the control group showed a trend toward increasing between T1 and T2. Therefore, studies measuring the development of WSLs should be conducted for longer than 6 months to determine when significant differences in oral hygiene will result in differences in WSL development.
Poor oral hygiene leading to the development of WSLs could have a negative impact on an orthodontic practice. Hamdan et al.24 reported that more than one-third of general dentists indicated that if one of their patients had severe WSLs after orthodontic treatment, it could have a negative effect on their perception of the treating orthodontist. This type of negative interaction with a general dentist could impact future referrals. In addition, WSLs have been a major cause of litigation for orthodontists, with juries awarding plaintiffs with up to $100,000 for past and future dental treatment and for past and future pain, suffering, and disfigurement.25 The professional and legal issues that WSLs could raise should strongly encourage practitioners to strive for impeccable oral hygiene compliance by their patients.
While the results of this study suggest that a text message reminder improves oral hygiene compliance, it is possible that its effectiveness was simply caused by the extra attention provided to the text message group. Sending messages to only the text message group may have maintained their awareness that they were in the study and influenced them to improve their oral hygiene. The control group, however, may have forgotten about study participation, allowing for a decline in their compliance. There is a need for future studies to determine whether the content of the text message or type of reminder system is important in improving oral hygiene compliance or if the extra attention provided to the text message group was the causative factor in oral hygiene-compliance improvement.
Directly text messaging parents of patients weekly to remind their children to maintain an impeccable oral hygiene protocol may not be that difficult to achieve in a private practice, because several orthodontic communication companies already provide text message automated-reminder services, and several Web-based text message programs are available free of charge. While these have traditionally been meant to remind patients to attend appointments, it seems reasonable that the text could be modified to serve other purposes. In addition, new applications for smart phones have been developed to remind patients to brush, floss, wear retainers, wear elastics, etc. Providing such a service will maintain good communication between the orthodontist and the patient and show that the orthodontist is concerned about each patient's well-being. Both of these orthodontist behaviors have proven to be important in influencing patient satisfaction and orthodontist-patient relationships.7 Additionally, the doctor's expression of concern about the well-being of the patient was also shown to be significant in predicting patient adherence to orthodontic treatment protocol.7 It is imperative, however, to be sure that parents and patients are aware of the frequency of communication so that it is not perceived as spam, which may negatively affect the orthodontist-patient relationship. The results of this study indicate that a text message reminder system is an effective means of improving oral hygiene compliance in orthodontic patients. Adding an active reminder system of the importance of impeccable oral hygiene should be strongly considered when implementing a protocol to improve oral hygiene compliance in orthodontic offices.
CONCLUSIONS
A text message reminder system explaining the importance of oral hygiene sent to parents of patients once weekly is an effective way to improve oral hygiene compliance in orthodontic patients over a 5.44-month period.
Orthodontists should add an active reminder system of the importance of oral hygiene compliance to their typical protocol during treatment.
REFERENCES
- 1.Al-Jewair T, Suri S. Predictors of adolescent compliance with oral hygiene instructions during two-arch multibracket fixed orthodontic treatment. Angle Orthod. 2011;81:525–531. doi: 10.2319/092010-547.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cantekin K, Celikoglu M, Karadas M, Yildirim H, Erdem A. Effects of orthodontic treatment with fixed appliances on oral health status: a comprehensive study. J Dent Sci. 2011;6:235–238. [Google Scholar]
- 3.Zachrisson BU, Zachrisson S. Caries incidence and oral hygiene during orthodontic treatment. Scand J Dent Res. 1971;79:394–401. doi: 10.1111/j.1600-0722.1971.tb02028.x. [DOI] [PubMed] [Google Scholar]
- 4.Chapman J, Roberts W, Eckert G, Kula K, Gonzalez-Cabezas C. Risk factors for incidence and severity of white spot lesions during treatment with fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2010;138:188–194. doi: 10.1016/j.ajodo.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 5.Sergel HG, Zentner A. Predicting patient compliance in orthodontic treatment. Semin Orthod. 2000;6:231–236. [Google Scholar]
- 6.Richter D, Nanda R. Effect of behavior modification on patient compliance in orthodontics. Angle Orthod. 1998;68:123–132. doi: 10.1043/0003-3219(1998)068<0123:EOBMOP>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Sinha P, Nanda R, McNeil D. Perceived orthodontist behaviors that predict patient satisfaction, orthodontist-patient relationship, and patient adherence in orthodontic treatment. Am J Orthod Dentofacial Orthop. 1996;110:370–377. doi: 10.1016/s0889-5406(96)70037-9. [DOI] [PubMed] [Google Scholar]
- 8.Feil P, Grauer J, Gadbury-Amyot C, Kula K, McCunniff M. Intentional use of the Hawthorne effect to improve oral hygiene compliance in orthodontic patients. J Dent Educ. 2002;66:1129–1135. [PubMed] [Google Scholar]
- 9.Almog D, Devires J, Borrelli J, Kopycka-Kedzierawski D. The reduction of broken appointment rates through an automated appointment confirmation system. J Dent Educ. 2003;67:1016–1022. [PubMed] [Google Scholar]
- 10.Roth J, Kula T, Claros A, Kula K. Effect of a computer-generated telephone reminder system on appointment attendance. Semin Orthod. 2004;10:190–193. [Google Scholar]
- 11.Fjeldsoe B, Marshall A, Miller Y. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med. 2009;36:165–173. doi: 10.1016/j.amepre.2008.09.040. [DOI] [PubMed] [Google Scholar]
- 12.Hussein W, Hasan K, Jaradat A. Effectiveness of mobile phone short-message service on diabetes mellitus management; the SMS-DM study. Diabetes Res Clin Pract. 2011;94:e24–e26. doi: 10.1016/j.diabres.2011.07.025. [DOI] [PubMed] [Google Scholar]
- 13.Can S, Marfarlane T, O'Brien K. The use of postal reminders to reduce non-attendance at an orthodontic clinic: a randomized controlled trial. Br Dent J. 2003;195:199–201. doi: 10.1038/sj.bdj.4810443. [DOI] [PubMed] [Google Scholar]
- 14.Foley J, O'Neill M. Use of mobile telephone short message service (SMS) as a reminder: the effect on patient attendance. Eur Arch Paediatr Dent. 2009;10:15–19. doi: 10.1007/BF03262661. [DOI] [PubMed] [Google Scholar]
- 15.Keith D, Rinchuse D, Kennedy M, Zullo T. Effect of text-message follow-up on patient's self-reported level of pain and anxiety. Angle Orthod. 2013;83:605–610. doi: 10.2319/091812-742.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saxton CA, van der Ouderaa FJ. The effect of a dentrifice containing zinc citrate and Triclosan on developing gingivitis. J Periodontal Res. 1989;24:75–80. doi: 10.1111/j.1600-0765.1989.tb00860.x. [DOI] [PubMed] [Google Scholar]
- 17.Quigley G, Hein JW. Comparative cleansing efficiency of manual and power brushing. J Am Dent Assoc. 1962;65:26–29. doi: 10.14219/jada.archive.1962.0184. [DOI] [PubMed] [Google Scholar]
- 18.Tufekci E, Dixon J, Gunsolley J, Lindauer S. Prevalence of white spot lesions during orthodontic treatment with fixed appliances. Angle Orthod. 2011;81:206–210. doi: 10.2319/051710-262.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lally P, Van Jaarsveld C, Potts H, Wardle J. How habits are formed: modelling habit formation in the real world. Eur J Soc Psychol. 2010;40:998–1009. [Google Scholar]
- 20.Lang NP, Adler R, Joss A, Nyman S. Absence of bleeding on probing. An indicator of periodontal stability. J Clin Periodontol. 1990;17:714–721. doi: 10.1111/j.1600-051x.1990.tb01059.x. [DOI] [PubMed] [Google Scholar]
- 21.De Souza PH, de Toledo BE, Rapp GE, Zuza EP, Neto CB, Mendes AJ. Reliability of bleeding and non-bleeding on probing to gingival histological features. J Int Acad Periodontol. 2003;5:71–76. [PubMed] [Google Scholar]
- 22.Barnett ML. Suitability of gingival indices for use in therapeutic trails. Is bleeding a sine qua non. J Clin Periodontol. 1996;23:582–586. doi: 10.1111/j.1600-051x.1996.tb01828.x. [DOI] [PubMed] [Google Scholar]
- 23.Lundstrom F, Krasse B. Caries incidence in orthodontic patients with high levels of Streptococcus mutans. Eur J Orthod. 1987;9:117–121. doi: 10.1093/ejo/9.2.117. [DOI] [PubMed] [Google Scholar]
- 24.Hamdan A, Maxfield B, Tufekci E, Shroff B, Lindauer S. Preventing and treating white-spot lesions associated with orthodontic treatment: a survey of general dentists and orthodontists. J Am Dent Assoc. 2012;143:777–783. doi: 10.14219/jada.archive.2012.0267. [DOI] [PubMed] [Google Scholar]
- 25.Machen D. Legal aspects of orthodontic practice: risk management concepts. Am J Orthod Dentofacial Orthop. 1991;100:93–94. [PubMed] [Google Scholar]