Abstract
Trauma-focused cognitive behavioral therapy (TF-CBT) is an evidence-based intervention to treat Post-traumatic Stress Disorder among youth ages 3–18 years. In this pilot study, 31 clinicians in 13 urban public schools received TF-CBT training to improve access to a high-quality trauma treatment for youth in need. A mixed methods design was used to assess implementation barriers, facilitators and outcomes to examine initial feasibility, acceptability, and appropriateness of TF-CBT delivered in school settings. Although 70% of clinicians reported confidence in the evidence-base of TF-CBT and its potential to support their students who have a very high prevalence of lifetime trauma exposure, implementation practice outcomes suggest a wide range of TF-CBT use (Range = 0 to 11 students enrolled per clinician, Mean = 1.4 students) with 23 clinicians implementing the TF-CBT model with at least one case. Results point to the potential value of training school mental health clinicians in TF-CBT based on its compatibility with student needs. Yet, by connecting focus group results to top-rated barriers and facilitators, we identify several adjustments that should be made to improve intervention-setting fit in future studies. Specifically, school setting-specific intervention adaptations, school-tailored implementation support and thoughtful consideration of school-based clinicians’ roles and responsibilities are needed to enhance future implementation success.
Keywords: TF-CBT in schools, school-based trauma treatment, trauma-informed schools, TF-CBT implementation outcomes
Trauma exposure is common, with an estimated two-thirds of children experiencing at least one traumatic event and a smaller proportion of youth experiencing multiple traumas (Copeland, Keeler, Angold, & Costello, 2007; Saunders & Adams, 2014). Childhood trauma can lead to post-traumatic stress symptoms that interfere with functioning and growth, increasing risk for long-term outcomes including physical health problems (Goodwin & Stein, 2004; Kibler, 2009), substance use and psychological disorders (Carliner et al., 2016; Mandavia, Robinson, Bradley, Ressler, & Powers, 2016), poor school performance and unemployment (Goodman, Miller, & West-Olatunji, 2012), and decreased quality of life (Dye, 2018). Evidence-based treatments to reduce the negative impact of trauma exist, but access to care is low (Gillies et al., 2016). It is estimated that nearly 80% of youth aged 6–17 do not receive the mental health care they need (Kataoka, Zhang, & Wells, 2002). Schools are a logical location to offer trauma treatment, particularly to improve access to care. Many youth who access mental health services do so through schools and school-based treatments, which have been shown to reduce disparity in access to mental health services (Ali et al., 2019; Burns et al., 1995; Larson, Chapman, Spetz, & Brindis, 2017). Implementing behavioral health interventions within the school system differs from traditional clinical settings and requires special consideration and planning to be successful (Nadeem, Saldana, Chapman, & Schaper, 2018). Input from clinicians delivering the intervention is invaluable in addressing barriers and planning for successful dissemination.
Only a handful of trauma-focused early intervention (Tier 2) and treatment (Tier 3) approaches have been implemented and tested in schools and have primarily focused on group-based models (e.g., Cognitive Behavioral Intervention for Trauma in School, Bounce Back; Jaycox, Kataoka, Stein, Langley, & Wong, 2012; Langley, Gonzalez, Sugar, Solis, & Jaycox, 2015). In selecting a trauma-focused, evidence-based treatment model for this study, several factors were considered, weighing evidence of effectiveness and implementation feasibility. First, school district administrators were hesitant to utilize a group-based model due to concerns about implementation barriers (e.g., obtaining guardian consent for a cohort in a closed group model, coordinating student and clinician schedules, stigma). Focusing on individual models, Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) has the strongest evidence base for reducing trauma-related symptoms among youth across the developmental spectrum and representing diverse and under-resourced populations (NICE, 2018; de Arellano et al., 2014). Numerous randomized controlled trials have demonstrated effectiveness of TF-CBT compared to treatment as usual (de Arellano et al., 2014), and it is largely considered the “gold standard” approach for mental health intervention for youth posttraumatic stress.
Anchored in cognitive-behavioral theory and exposure-based principles, TF-CBT includes psychoeducation, coping strategies (relaxation, emotion identification and affective regulation, and cognitive coping), gradual exposure throughout treatment and specifically to a Trauma narrative written by the youth and caregiver participation. TF-CBT developers summarize components using the acronym PRACTICE, which stands for Psychoeducation and Parenting skills, Relaxation skills, Affective regulation skills, Cognitive coping skills, Trauma narrative and cognitive processing of traumatic events, In vivo mastery of trauma reminders, Conjoint parent-child sessions, and Enhancing safety and future development (Cohen, Mannarino, & Deblinger, 2012). TF-CBT is designed to reduce symptoms related to Post-Traumatic Stress Disorder for children and adolescents, but has also resulted in improved outcomes in child depression, child behavioral difficulties, parental support and parenting practices (Cohen, Deblinger, Mannarino, & Steer, 2004). Particularly pertinent to this study, TF-CBT is designed for delivery in 8–25 sessions in clinical settings with the creation of and exposure to the trauma narrative in the second phase of treatment, following initial coping skill acquisition. TF-CBT has been examined for its implementation feasibility in low-resource and community-based settings where access to trauma treatment is greatly needed (Murray et al., 2013).
Treatment developers and other scholars have advocated for the training and use of TF-CBT in schools (Rivera, 2012), with particular emphasis on the promising role of school psychologists to deliver TF-CBT in order to improve the quality and evidence-base of Tier 3 trauma treatment interventions available to students (Fitzgerald & Cohen, 2012; Little, Akin-Little & Gutierrez, 2009). However, the only published report we could locate in the peer-reviewed literature documenting school-based TF-CBT implementation and outcomes is that of Orengo-Aguayo and colleagues (2020). She and her team implemented TF-CBT in three low-resource settings, rural South Carolina, Puerto Rico and El Salvador. School staff were involved as stakeholders to develop the implementation plan and coordinate referrals to community providers. In at least one site, school psychologists were trained to implement TF-CBT and in several sites, mental health services were delivered on school campuses by community mental health providers. Although the implementation context and service delivery varied slightly for each setting depending on local needs, strengths and systems, TF-CBT was ultimately delivered to hundreds of students via telehealth or in person and pre-post trauma symptom reduction was large (d = 1.89 to 2.04). Another large-scale study was recently funded to examine TF-CBT implementation in schools, indicating federal investment and the importance of expanding the research base in this area (Lyon, Pullman, Dorsey, Levin, Gaias, Brewer, et al., in press).
Overall, TF-CBT holds promise for addressing trauma-related concerns in schools, but demonstrations of TF-CBT implementation in schools are still emerging and there is much to be learned about barriers and facilitators unique to the school context. Identifying context and intervention specific barriers and facilitators (i.e., “determinants of practice”) is a critical first step to inform intervention tailoring to optimize intervention-setting fit and ultimate implementation and sustainment of evidence-based practices in “real world” settings (Flottorp et al., 2013; Baker, Camosso- Stefinovic, Gillies, Shaw, Cheater, Flottorp, et al., 2015). To date, an in-depth examination of barriers, facilitators and implementation outcomes have not been well-established in the literature, particularly when TF-CBT is implemented among a multidisciplinary group of school-based mental health professionals in one school district.
The study team and their colleagues have been part of local TF-CBT implementation in schools. Specifically, the University of Maryland School Mental Health Program, in partnership with the Division of Child and Adolescent Psychiatry, had nearly a decade of prior experience providing TF-CBT training and ongoing consultation from a national TF-CBT trainer to their full-time clinicians and psychology predoctoral interns. This strategic opportunity to explicitly study TF-CBT implementation in schools was leveraged to better understand implementation barriers, facilitators and outcomes that have not been systematically examined in schools to date for this intervention.
Current Study
The current mixed methods pilot study was conducted to better understand implementation practices, determinants and outcomes of TF-CBT piloted in 13 urban public schools. Uncovering determinants of practice (i.e., barriers and facilitators) for TF-CBT in schools is the first step to selecting and later testing training, implementation, and support strategies which could increase TF-CBT treatment outcomes in other “real world” treatment settings.
Method
This study was conducted in the context of an evaluation of a multi-component approach to implementing a multi-tiered, trauma-informed framework to support student resilience in an urban school district. TF-CBT was the selected intervention for students who met criteria for PTSD when referred for mental health services and screened using the UCLA-PTSD Index. TF-CBT was implemented in 13 public schools in a large, urban district in the Mid-Atlantic region of the United States; schools were selected for implementation based on being part of a larger, multi-component initiative to improve trauma-sensitive school programming in three neighborhoods most proximal to city-wide civil unrest which garnered national attention and resulted in the Governor declaring a state of emergency. Together, these schools served approximately 4,629 students (which represents 5.5% of students in the entire district) and 97% students are non-Hispanic African-American (compared to 82% non-Hispanic African-American in the district). Of the 13 schools, 10 were traditional, general education public schools, two were charter, one was an alternative school. In addition, six were elementary, four were elementary/middle (grades Kindergarten through 8th), one was middle, one was middle/high, and one was high. However, all schools served students living in the neighborhoods in which they were located, which are characterized by extreme economic hardship (e.g., free and reduced price meal enrollment averages 83% in this district) and violent crime rates substantially above the national average.
Initial adoption and implementation of TF-CBT occurred in the 2017–2018 school year, with full implementation and the evaluation data reported in this paper occurring in the 2018–2019 school year. An initial informal needs assessment conducted with clinicians during TF-CBT training showed limited use of trauma-specific assessment or treatment; of 34 clinicians surveyed, only three (9%) reported using an evidence-based, trauma-focused model (e.g., Trauma-Focused Cognitive Behavioral Therapy or Cognitive Behavioral Intervention for Trauma in Schools). Most clinicians reported addressing trauma using evidence-based approaches such as cognitive behavioral therapy or various components of stress management (e.g., relaxation training, mindfulness, coping skills) that are not specific to trauma treatment. Further, only 7 of the 34 clinicians surveyed (32%) indicated that they had experience using an evidence-based assessment for trauma.
Participants
A total of 31 clinicians working in the 13 schools participated in this project (Table 1). Three of the initial 34 participants who were trained in TF-CBT did not continue to be employed by the school system or Expanded School Mental Health (ESMH) Programs. Participants identified primarily as female (N=27; 87%), White (N=20; 65%), Black/African-American (N=10; 32%) and non-Hispanic (N=27; 87%). Approximately one-third were school psychologists, one-third were school social workers, and one-third were ESMH clinicians (i.e., clinicians employed by a university or community organization contracted to provide mental health treatment services in the school). ESMH clinicians are typically licensed social workers, psychologists, and counselors. Schools generally have a school psychologist, school social worker, and ESMH clinician working at their school, but clinicians are assigned to 1–3 schools depending on their roles, responsibilities and funding. Clinicians had varying levels of experience providing mental health services within schools, with 48% having over 6 years of experience and 52% having 5 years or less of experience (see Table 1).
Table 1.
Clinician Demographic and Professional Characteristics
| n | % | ||
|---|---|---|---|
| Gender | Female | 27 | 87.10 |
| Male | 4 | 12.90 | |
| Race | White | 20 | 64.50 |
| Black/African American | 10 | 32.30 | |
| Asian or Asian Indian | 1 | 3.20 | |
| Ethnicity | Non-Hispanic | 27 | 87.10 |
| Hispanic | 3 | 9.10 | |
| Missing Data | 1 | 3.20 | |
| Role | School social worker | 10 | 32.25 |
| School psychologist | 9 | 29.00 | |
| ESMH clinician | 12 | 38.70 | |
| Years of Experience | 11 or more | 11 | 35.50 |
| 6 to 10 | 4 | 12.90 | |
| 2 to 5 | 10 | 32.30 | |
| Less than 2 | 6 | 19.40 |
All three school-employed mental health professional types have explicit expectations to provide individual counseling/therapy to children in their schools, with additional expectations by clinician type. Primary differences in the school-employed clinician groups are that 1) school psychologists conduct cognitive, social-emotional, and adaptive functioning assessments; 2) school social workers often link students and families with community supports such as housing assistance, food pantries, social services, and extracurricular activities; and, 3) school counselors are more likely to be placed in middle and high schools and have a heavy focus on college and career readiness. For more detailed information on school-employed clinician roles, see Padden and colleagues’ (2016) Venn diagram. ESMH providers augment service provision by school-employed staff to offer a fuller array of mental health promotion, prevention, and intervention. Like school-employed clinicians, ESMH clinicians can provide individual, family, and group counseling, teacher consultation, crisis intervention, and support schoolwide and classroom mental health promotion and prevention activities. ESMH clinicians participate on school mental health teams, provide professional development to school staff, and work predominantly with students in general education.
Procedures
Implementation
Clinicians received a two-day TF-CBT initial training prior to the start of the school year, a one-day booster training in January and consultation calls every other week throughout the school year. All training sessions and consultation calls were provided by a national TF-CBT trainer approved by TF-CBT developers based on completion of a 15-month TF-CBT Train-the-Trainer program (Hanson et al., 2014). Consultation calls lasted for one hour each, were in a small group format held at times recommended by clinicians and clinical supervisors to be as convenient as possible during the day and clinicians were invited to share specific prospective or current TF-CBT cases for expert and peer feedback. Clinicians who worked in the 13 public schools were encouraged to identify students potentially eligible for TF-CBT from their existing caseload and referrals. Clinicians received training in administering the UCLA-PTSD Reaction Index (Steinberg, Brymer, Decker, & Pynoos, 2004) to determine appropriateness of TF-CBT for each prospective student. Materials to support assessment and TF-CBT treatment implementation were provided in hard copies for school offices as well as online. Clinicians were not asked to change their current referral pathways or procedures. However, consultation calls focused on supporting all phases of implementation starting from engagement, trauma psychoeducation and providing rationale for TF-CBT as an exposure-based treatment.
Data Collection
Each month, clinicians received an email from the study team with a link to an online Qualtrics survey called the Monthly Practice Report (MPR) to report their TF-CBT practices. Clinicians were emailed by a study team member the first day of the month with a reminder to report prior-month data within ten (10) calendar days. Individual email reminders were sent up to three times to prompt completion and clinicians were offered the opportunity to retrospectively complete MPR from the prior month to “catch up” when needed. These reports took approximately 15 minutes to complete each month and retrospectively reported based on the clinicians’ personal case files and referral tracking.
A separate recruitment procedure and consent process was used for the follow-up clinician surveys and focus groups, which occurred together. A study team member emailed each clinician to invite them to participate in a voluntary, anonymous focus group to provide feedback about TF-CBT implementation at the end of the school year. Five focus groups were scheduled on one day at a central location, and clinicians were able to indicate their focus group time preference upon RSVP. At the beginning of each focus group, clinicians were provided the focus group protocol, consent information form, and project-end survey. A study team member read the study information form and provided opportunity to ask questions and/or decline participation. Prior to the start of the focus group, participants completed a brief project-end survey. Next, the focus group began with a report-out of top barriers and facilitators before opening the discussion for clinicians to share their experiences about TF-CBT implementation. Two facilitators conducted the group and an additional note taker was present. All focus groups were audio recorded, transcribed and checked for accuracy. All data collected were anonymous. Compensation of a $25 gift card was provided for focus group participation. Focus groups lasted one hour, including consent and the project-end survey administration. Focus groups were conducted on one day and clinicians could sign up to attend the group that best suited their schedule; most schools needed to send their clinicians at different times to ensure someone was on site for mental health coverage throughout the day.
Measures
Three measures were used for data collection: (1) Monthly Practice Reports (MPRs) during implementation, (2) a project-end survey, and (3) focus groups at the end of the project. Clinician practices were captured by MPRs and the project-end survey. Student needs for trauma treatment was also collected by the project-end survey. Implementation determinants (i.e., barriers and facilitators) were collected using the project-end survey and further examined via focus group data. Implementation outcomes were examined by focus group results.
Monthly Practice Reports
Each month during the project, clinicians received a link to an online Qualtrics survey asking them to report the number of students for whom they received referrals potentially related to trauma, number of students screened for trauma using the UCLA-PTSD checklist, and number of students eligible for, enrolled in, and who had completed TF-CBT. This survey was developed by the study team for the full implementation year to provide consistency in practice reporting across the 13 school buildings and 31 clinicians. MPR response rates ranged from 57–86% across months.
Project-End Survey
Clinicians who attended focus groups were asked to complete a 5- to 10-minute anonymous survey including information about demographic and professional characteristics, student trauma exposure and symptoms and their TF-CBT assessment and treatment practices. Clinicians were asked to estimate the percentage of their caseload during the past school year that 1) had experienced one or more lifetime traumas and 2) presented with trauma-related symptoms. The second part of the Project-End Clinician Survey was a Determinants of Practice Checklist used to 1) assess the relative salience of barriers and facilitators experienced by all clinicians to complement qualitative input during focus groups and 2) inform the focus group discussion by asking about determinants that were most frequently endorsed by the group. Clinicians indicated whether each of a list of 25 determinants drawn from prior literature had been a barrier, a facilitator, neither, or both in their experience using TF-CBT in a school setting. There are many methods to identify determinants, including mixed methods of a checklist and brainstorming or focus group (Krause et al., 2014). We selected a checklist developed by Flottorp and colleagues (2013) which was grouped by clinician, patient, systems, and innovation-specific factors. Two study team members independently rated each determinant for its application to the current project. Of the 57 determinants, coders both agreed to eliminate 31 and keep 18 (86% agreement). Coders’ decisions were discrepant on eight determinants; using a consensus process, an additional seven were retained for a total of 25 final determinants.
Focus Group Protocol
The focus group protocol asked clinicians to describe the barriers and facilitators experienced most frequently when implementing TF-CBT. This conversation was preceded by a report-out of the top barriers and facilitators endorsed on the Project-End Clinician Survey. The conversation was not limited to those determinants endorsed most frequently. Clinicians were also asked to comment on their recommendations for future implementation of TF-CBT in schools. Implementation outcomes such as perceived acceptability, appropriateness and feasibility were not explicitly queried but arose in the conversations and are reflected in the results.
Analyses
Quantitative data from the Monthly Practice Reports and Project-End Clinician Survey were examined descriptively due to the small sample size and single-implementation condition design. After data were checked for accuracy and cleaned, distributions, frequencies and measures of central tendency were examined.
Focus group data were analyzed by two study team members using grounded theory analysis (Charmaz, 2007). This included open or initial coding with all focus group data, followed by an iterative process of focus coding to develop, test, and refine the codebook with a smaller subset of focus group transcripts. First, each coder read through groups they did not facilitate to generate open codes and memos based on all focus groups. Next, the full list of open codes was reviewed and decisions were made about general coding rules, collapsing codes into focus codes, and adding sample quotes and descriptions to define and delineate codes. The resulting codebook was tested on one focus group transcript by both coders. Based on 93.8% inter-coder agreement on codes, the remaining four focus groups were divided for coding among the two coders. Memos were documented and discussed throughout the coding process and the final stage of theoretical coding was conducted with both coders’ review and discussion of themes or categories to summarize focus codes. Consistent with grounded theory, codes were grouped under broader theoretical categories or “themes” to synthesize the data for meaningful interpretation.
Our mixed methods analytic approach involved connecting top-rated determinants with focus group themes and codes to expand our understanding of the most frequently-experienced determinants among the sample. More specifically, we reviewed the five most frequently-rated barriers and facilitators and reexamined focus group findings to connect information learned across data sources and methods. Data were collected simultaneously with more weight or emphasis on qualitative data, which were connected to quantitative data to provide a more in-depth understanding of quantitative ratings. Our mixed methods approach can be described as having a “structure” of “quan + QUAL”, function of complementarity and process of connecting (Palinkas et al., 2011). Our initial and primary goal was to collect qualitative feedback to understand the implementation process, but due to the short amount of time allotted for focus groups (which required clinicians being excused from clinical duties at their school to participate), we opted to add the quantitative ratings of determinants to complement qualitative input received.
Results
Clinician-Reported Student Trauma Exposure and Symptoms
As shown in Table 2, 26 (84%) clinicians reported that 51% or more of the students on their caseload have experienced one or more lifetime traumas and 15 (48%) reported that 51% or more of the students on their caseload presented with symptoms related to trauma exposure. As would be expected, clinicians reported that more students had experienced trauma than showed symptoms related to trauma exposure. Clinician reports were consistent with documented rates of trauma exposure for students in this school district.
Table 2.
Clinician-Reported Student Trauma Exposure and Symptoms (N=31 Clinicians)
| Percent of students on my caseload… | …who have experienced at least one lifetime trauma. | ….who have symptoms related to trauma exposure. |
|---|---|---|
| 0–25% | 2 (6.5%) | 2 (6.5%) |
| 26–50% | 1 (3.2%) | 12 (38.7%) |
| 51–75% | 10 (32.3%) | 8 (25.8%) |
| 76–99% | 11 (35.5%) | 5 (16.1%) |
| All of them | 5 (16.1%) | 2 (6.5%) |
| I did not provide clinical services to youth last year* | 2 (6.5%) | 2 (6.5%) |
First-year clinicians
Clinician Practices
MPR data indicated that 116 students were referred for trauma-related concerns at the 13 participating schools. Of those, 47 (40.5%) were enrolled in TF-CBT. On average, clinicians reported receiving referrals for 3.14 students (Range = 0 to 22) and enrolling 1.37 students (Range = 0 to 11).
Reported use of trauma-specific assessment tools at follow-up was also fairly high, with 22 (71%) reporting having used at least one UCLA-PTSD Reaction Index in the past year. In contrast, reported rates of TF-CBT implementation were variable. Clinicians reported using any component of TF-CBT with two or three students on average (M=2.65, SD=3.17), but the range was wide (range = 0 to 15). Eight clinicians (25.8%) did not use any component of TF-CBT with any student and 21 (67.7%) reported not finishing the model with any student. As shown in Figure 1, most school-employed clinicians (N=19) reported using TF-CBT with zero to three students while ESMH clinicians (i.e., hired at outside community mental health agencies, N=12) reported a higher and more variable number. Post-hoc comparisons using an independent samples t-test showed that the number of students TF-CBT was used with varied significantly by clinician type when comparing ESMH and school-employed (t(12.35) = 3.14, 95% CI = 1.15, 6.27; p = .008). Specifically, ESMH providers reported using TF-CBT with more students (M=4.92, SD=3.96) when compared to school-employed providers (M=1.21, SD=1.23). However, even with equal variances not assumed, the significance of these results should be interpreted with caution as the distributions are non-normal (see Figure 1) and the sample size is small.
Figure 1.
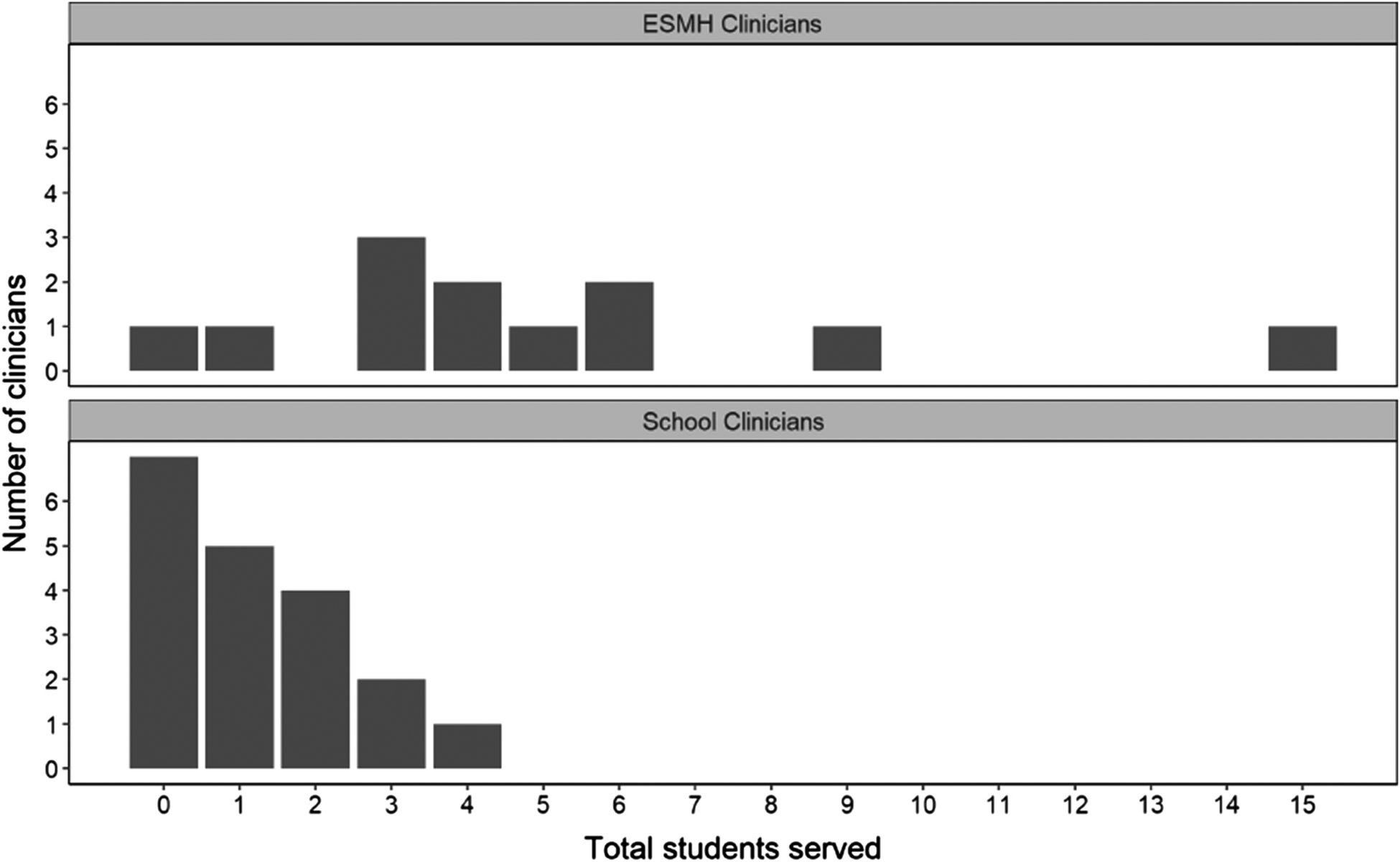
Distribution of Number of Students Served with TF-CBT by Clinician Type
Clinicians reported finishing the TF-CBT model with few students, (M=0.61, SD=1.05, range = 0 to 14). Similar between-group trends were observed, with ESMH clinician reports of finishing the model with more students on average (M = 1.25, SD = 1.36) than school-based clinician numbers (M = 0.21, SD = 0.53).
TF-CBT Implementation Barriers and Facilitators
A total of 27 clinicians completed the entire Determinants of Practice checklist on the Project-End Survey (four checklists were excluded due to missing data). Out of 25 possible options, clinicians reported an average of 5.89 barriers (Range = 0 to 18) and 7.93 facilitators (Range=0 to 18). A post-hoc analysis of N=27 clinicians with complete practices and determinants data revealed non-significant trends in the numbers of barriers and facilitators reported by “implementers” (use of TF-CBT with one or more student) as compared to “non-implementers”, though mean differences were in the expected directions with implementers endorsing more facilitators and non-implementers endorsing more barriers. Table 3 displays all determinants clinicians rated, and the number of clinicians who rated each as a facilitator, barrier, both or neither.
Table 3.
Determinants of Practice for TF-CBT Implemented in Schools
| Determinant | Definition | Facilitator N (%) | Barrier N (%) | Both N (%) | Neither N (%) |
|---|---|---|---|---|---|
| TF-CBT Factors | |||||
| 1. Quality of evidence | Level of confidence that TF-CBT is based in good science | 19 (70%) | 1 (4%) | 3 (11%) | 4 (15%) |
| 2. Strength of recommendation | Level of confidence that TF-CBT will help clients more than it hurts them | 19 (70%) | 1 (4%) | 5 (19%) | 2 (7%) |
| 3. Clarity | Clarity about who TF-CBT is for | 19 (70%) | 1 (4%) | 5 (19%) | 2 (7%) |
| 4. Cultural appropriateness | Level of fit between TF-CBT and students in this district | 6 (22%) | 5 (19%) | 16 (59%) | 0 |
| 5. Feasibility | Extent to which TF-CBT is practical in schools | 3 (11%) | 13 (48%) | 11 (41%) | 0 |
| 6. Compatibility | Level of fit between TF-CBT and other interventions I do with students | 14 (52%) | 5 (19%) | 8 (30%) | 0 |
| 7. Effort | Amount of effort required to implement TF-CBT | 3 (11%) | 14 (52%) | 9 (33%) | 1 (4%) |
| 8. Trialability | My ability to “try out” TF-CBT before really implementing (e.g., using PRAC skills with non-TF CBT students or practicing in training) | 14 (52%) | 4 (15%) | 3 (11%) | 6 (22%) |
| 9. Observability | Extent to which you can see and know other clinicians are implementing TF-CBT | 7 (26%) | 8 (30%) | 5 (19%) | 7 (26%) |
| Clinician Factors | |||||
| 10. Domain knowledge | Extent to which you already had expertise about trauma treatment before TF-CBT training | 13 (49%) | 4 (15%) | 4 (15%) | 6 (22%) |
| 11. Skills | Extent to which you have the skills you feel you need to actually implement TF-CBT | 13 (49%) | 6 (22%) | 6 (22%) | 2 (7%) |
| 12. Expected outcome** | Level of confidence that TF-CBT will work | 13 (50%) | 4 (15%) | 8 (31%) | 1 (4%) |
| 13. Learning style | How well TF-CBT training and consultation calls fit with my learning style | 8 (30%) | 8 (30%) | 8 (30%) | 3 (11%) |
| 14. Emotions | My emotional experience when providing trauma treatment | 6 (22%) | 3 (11%) | 8 (30%) | 10 (37%) |
| 15. Capacity to plan change | My capacity to make changes in my schedule to provide TF-CBT | 2 (7%) | 11 (41%) | 10 (37%) | 4 (15%) |
| Team Processes | |||||
| 16. Team processes | Extent to which your school team worked together on TF-CBT screening, enrollment and implementation | 4 (15%) | 13 (48%) | 3 (11%) | 7 (26%) |
| 17. Referral to enrollment processes | Processes for referring students, connecting to families, and screening students for TF-CBT enrollment | 5 (19%) | 14 (52%) | 6 (22%) | 2 (7%) |
| Client Factors | |||||
| 18. Student needs | How good of a fit TF-CBT was with student’s actual needs | 10 (37%) | 6 (22%) | 11 (41%) | 0 |
| 19. Student preferences** | How good of a fit TF-CBT was with student preferences | 6 (23%) | 9 (19%) | 10 (38%) | 1 (4%) |
| 20. Parent preferences | How good of a fit TF-CBT was with parent/guardian preferences | 1 (4%) | 12 (44%) | 10 (37%) | 4 (15%) |
| Organizational Factors | |||||
| 21. Capable leadership | Extent to which your supervisor or administrator supported your use of TF-CBT | 12 (44%) | 1 (4%) | 5 (19%) | 9 (33%) |
| 22. Priority | How important TF-CBT was compared to other new initiatives or requirements | 5 (19%) | 8 (30%) | 6 (22%) | 8 (30%) |
| 23. Monitoring and feedback** | Extent to which my supervisors or managers collected information on my progress with TF-CBT cases and provided feedback | 6 (23%) | 6 (23%) | 5 (19%) | 9 (19%) |
| Social, Political and Legal Factors | |||||
| 24. Payment/ reimbursement* | Extent to which students’ insurance or other funding sources covered TF-CBT | 5 (19%) | 0 | 1 (4%) | 21 (78%) |
| 25. Liability | Extent to which providing TF-CBT introduced a possible liability concern for you, your agency, school or district | 1 (4%) | 2 (7%) | 2 (7%) | 22 (81%) |
All factors are from the TICD Checklist (Flottorp et al., 2013) with the exception of “payment/reimbursement”, which was developed to represent “payer or funder policies” in the original checklist but more clearly named and defined for this study.
N=26 instead of 27 due to missing data from one participant on these items.
TF-CBT Implementation Focus Group Themes and Codes
In addition, clinicians provided in-depth feedback about the degree of acceptability and appropriateness of TF-CBT in schools based on their experiences. Qualitative themes were grouped as follows: 1) TF-CBT model and training, 2) school-based clinicians’ role with trauma treatment, 3) students and parents and 4) school environment (Table 5 for codes and frequencies within each theme). Each of these four themes are described below. Each theme describes various aspects of the implementation process, yet are inherently connected as they are all clinician-reported perspectives on a multi-level implementation effort. As displayed in Table 4, we connected the top five most frequently endorsed facilitators and barriers (described above) to the qualitative findings to expand our understanding of these determinants. Mixed methods findings are displayed in Table 4 and instances where focus group themes and codes connect to top barriers and facilitators are noted in text.
Table 5.
TF-CBT Implementation Focus Group Themes, Codes and Code Frequencies
| Theme | Code | Code Frequency* |
| TF-CBT model and training | ||
| Adaptations needed | 14 | |
| Clinician role | ||
| Office space | 2 | |
| Students and parents | ||
| Student and family characteristics and experiences | 17 | |
| School environment | ||
| Leadership and school staff support | 28 |
Code frequencies are provided to display the relative frequency with which codes arose during the focus groups to help the reader interpret which codes and themes were more or less emphasized in the codable content.
Table 4.
Mixed Methods Findings about TF-CBT Implementation in Schools
| Top 5 Determinants (Quantitative) | Connection to Focus Group Themes and Codes (Qualitative) | |
|---|---|---|
| Facilitators | Evidence-Base of TF-CBT | The training experience was appreciated by clinicians and reported as valuable to have TF-CBT as “part of the toolbox”. This could be because they viewed TF-CBT as evidence-based and having promise to help their students who clearly need it before and/or as a result of the training experience. |
| Strength / Promise of TF-CBT to help students | ||
| Clarity (who benefits most from TF-CBT) | ||
| Compatibility (fit with students) | High prevalence of trauma exposure among students and parents make trauma treatment a good fit. However, adaptations could improve fit and feasibility. | |
| Trialability | No clear connection to qualitative results. Clinicians may have rated this highly because they were able to “try out” TF-CBT during this implementation pilot. | |
| Barriers | Effort | School-based clinicians’ role with trauma treatment (i.e., lack of time, scope of practice) presented these barriers in the school context |
| Referral → Enrollment | ||
| Team Processes | ||
| Feasibility |
|
|
| Parent Preferences | Students and parents theme includes difficulty with parent engagement, consent and enrollment as well as how student and family characteristics and experiences may have influenced preferences for TF-CBT. |
Theme 1: TF-CBT Model and Training
Clinicians’ impressions of the TF-CBT model itself, including how appropriate this model is to be delivered in schools generally, adaptations they would have wanted, and their own experience with the 2-day training and biweekly consultation calls are discussed below.
TF-CBT Model: PRAC Skills vs Narrative.
The degree of appropriateness of the TF-CBT model was related to whether the clinician was referencing the psychoeducation, relaxation, affect modulation and cognitive coping (PRAC) skills (acknowledged as generally more appropriate) versus the trauma narrative (acknowledged as appropriate only for select students and under certain school setting conditions).1 Clinicians reported that the PRAC skills were generally helpful and fit well with the needs of their students and their workflow. For instance, one clinician who works in five schools reported delivering TF-CBT in a student’s home (in Spanish, using an online TF-CBT workbook) very slowly, from September until May. By May, they were just starting the trauma narrative and already his UCLA-PTSD scores had decreased from a 52 to 22. The coping skills were also applicable to students for whom trauma was not a focus of treatment. However, many more concerns about acceptability, feasibility and appropriateness of the trauma narrative were raised. Feedback about fit between the trauma narrative specifically and the school setting is embedded in other themes discussed below, but the overall concerns were related to the student’s level of readiness to report trauma and engage in exposure-based treatment, the school-based clinicians’ role to feasibly complete the narrative, and appropriateness of conducting exposure-based treatment in a school as compared to a clinic (away from the school setting and where a parent could be present). Student resistance to the narrative component was referenced in a couple of groups, which was an issue that clinicians often did not push but rather took as a sign that the narrative was not appropriate for the student, as illustrated by the following:
Focusing on the PRAC skills and psycho-education piece is helpful. All those practice skills were useful. I had two different kids who went through most of it but once we got the trauma narrative, they flipped out and would no longer come to my office. Doing that piece was too much for them.
Clinicians also expressed concerns about the appropriateness of trauma narrative sessions in schools such as, “How do we package the kids back up and send them back to take a test? I don’t think this is the right fit.”
A small handful of clinicians reported success with the trauma narrative. For instance, one clinician said:
In my experience, TF-CBT works, and it makes sense. The flow is really good. Kids really respond well to it, including the narrative. I would recommend, for elementary school children, creating storyboard narratives, drawing or acting it out with dolls. Just being flexible with meeting the kids where they are and being creative.
Other comments indicated clinician discomfort with using the narrative related to their concern that the school climate was not trauma-sensitive and would not be able to offer the support and safety students needed (both codes discussed below in clinician role and school climate and leadership). Related, clinicians in two focus groups raised concerns about the appropriateness of TF-CBT as a Tier 3 intervention when they felt their limited time is better spent consulting with teachers about the impact of trauma on learning and addressing larger school climate needs, particularly when trauma exposure is so widespread in this district. One clinician noted the importance of supporting school climate with their limited time:
Some schools are at different readiness levels with [trauma], most of our time and focus is on Tier 1 supports, so where is our time best served when it is already so limited? Is it best served with a handful of kids in hour long sessions, or is it best served addressing some of the larger climate issues that reach a larger number of students, and then refer out some of the trauma cases?
Another clinician stated the following:
So many of our kids are impacted by trauma in one way or another, so selecting a few of those kids was not using my skills in the most efficient way possible. I spent a lot of time working with grade levels and teachers and helping them understand trauma. This was a good way of looking at systems rather than doing intense therapy with just a few students.
Notably, clinician perspectives about the appropriateness of the TF-CBT model in schools is linked to other themes that emerged from the focus group data. For instance, the quote above illustrates that the appropriateness of the TF-CBT model is based on its fit with the implementers (i.e., school-based clinicians), their role in the school system, and larger systems factors such as the school environment.
Adaptations Needed.
Clinicians noted school-specific adaptations to the TF-CBT model that they would have wished for or recommend to improve the feasibility of TF-CBT; feasibility was rated as a top barrier to implementation (Table 4). Specifically, a slower pace of treatment and more flexibility with the model were the primary types of changes reportedly needed to make the TF-CBT model a better fit in schools. A slower pace was recommended for many reasons, from allowing the student more time to acquire PRAC skills before moving onto the trauma narrative to logistical considerations such as shorter sessions (20–30 minutes) and less frequent sessions (not weekly). Flexibility suggestions included involving other trusted adults such as teachers and mentors instead of or in addition to parents, being able to return to PRAC skills as needed later in the model and pausing to address immediate behavioral and/or safety concerns. One clinician acknowledged that the pace for PRAC skill acquisition is slower partly for student needs and related to her own skill development:
Treatment is supposed to be for four months but most of my students needed more time with the PRAC skills before ready for narrative because of chronic trauma and severe symptoms. I’ve done six or seven TF-CBT cases this year but started the majority of them last year. I didn’t want to rush through it and am doing no harm by slowing down the pace; TF-CBT is new to me. Now I could do it in six months to one school year.
Training Experience.
Clinicians routinely reported that the TF-CBT training was “helpful overall” not only for their TF-CBT cases but also to become “part of the tool box” because “the early part of TF-CBT is just CBT; you can use the skills with kids who aren’t experiencing trauma”. One clinician commented that the training helped her realize that trauma can underlie other externalizing behaviors. There was a general appreciation for the training and consultation support received, “I really enjoyed [trainer’s] training. She’s awesome. It felt good to be back in the trenches of training.” Another acknowledged how critical training and ongoing support is to implement TF-CBT in this setting, as follows:
I feel like I’ve had a lot of support and I think that’s very important for folks actually implementing it…I don’t know how we can work in inner city schools without having this support. People may not do the work if they don’t have that expectation and support there because it’s difficult. You have to be flexible, it’s challenging, and you might avoid it especially if you have trauma yourself you can be triggered.
The training experience was connected to several key facilitators of implementation, because clinicians valued training in this evidence-based practice that they perceived as having great promise to help students and match student needs (Table 4). It is unclear whether clinicians viewed TF-CBT as evidence-based with high potential to help students in need prior to the training, and these perceptions were part of their appreciation for TF-CBT training provided, or if those perceptions were a result of the training received. Either way, top facilitators of implementation were the evidence-base of TF-CBT, strength or promise of TF-CT to help students, and clarity about who could benefit most from TF-CBT (Table 4).
While the in-person trainings received very positive reviews, the bimonthly consultation calls received mixed reviews. While some said the phone calls make it easier to implement TF-CBT and offered useful strategies, others found the calls too long, and the accountability to have a situation or student in mind to present stressful. There were also logistical barriers to attending calls, such as having to pick a call time in the summer before school schedules were set and difficulty attending calls due to other duties. The logistics and pressure to present on the call likely contributed to the consultation call portion of the training experience being ranked highly as a feasibility barrier by participants at the end of implementation (Table 4).
Providing more information on school-specific implementation considerations was recommended, such as how to implement TF-CBT with a continuing case (as compared to with a new case which is more common for clinic-based providers who were also on the calls). This is not to say clinicians didn’t want ongoing support. On the contrary, they asked for options such as individual consultation or coaching with the trainer, dedicated time for planning, and additional physical materials (e.g., informational booklet about trauma and the treatment to share with parents in English and Spanish, PRAC skills game materials such as the feelings bingo game, a binder with all sessions, continuous access to online materials, and quick, concrete tips for clinicians to support students “in the moment” who are experiencing trauma symptoms daily in the school setting).
Theme 2: School-Based Clinicians’ Role with Trauma Treatment
Numerous aspects of the school-based mental health clinician’s role supporting students in their school were reported to impact the acceptability and feasibility of TF-CBT implementation. Of note, clinician’s specific disciplines as well as whether they were school-employed (e.g., school social worker or school psychologist) or community-employed school-based (e.g., ESMH) did influence each of the codes discussed below to some extent (and are noted accordingly in results) but overall, the barriers and facilitators experienced were shared by the entire group of participants.
Scope of Practice.
Clinicians generally acknowledged that “it’s important for school clinicians to be trauma-informed” and having a trauma intervention available in the school was valued. This is related, in part, to the appropriateness of the TF-CBT model to be delivered in schools, but is more specifically focused on the scope of practice for school-based mental health clinicians. For instance, one clinician noted, “When I look at these interventions, this is the only one specifically focusing on helping kids with their trauma. It’s a responsible thing. We have to do this. This is the one that’s going to help.” A school social worker commented that the TF-CBT training provided validation for her role to support trauma as a school social worker because it matches students’ needs. However, many school-based clinicians, particularly those who are school-employed, felt that treating trauma with a Tier 3 intervention was outside the scope of their practice. One clinician said, “I was trained as a school psychologist to not talk about those things, [thinking] ‘I don’t know if I can get into this trauma here’ and so we focus more on the present moment.” Some clinicians felt that the trauma treatment should be provided by a “neutral” or “outside” therapist who they could refer to and coordinate with because their dual roles as a “behavior therapist and a trauma therapist” is impractical, especially for school social workers. They felt it wouldn’t work “to be the trauma person and still tell them not to run in the hall”, for example. One community-employed clinician did acknowledge that the scope of practice and time allotment might make them more likely to be able to implement TF-CBT, as follows:
ESMHs have more capacity to provide TF CBT than school psychologists or guidance counselors. We had some flexibility and wiggle room. The [school-employed] clinicians had all their IEP kids and a full caseload.
Special Education Requirements and Documentation.
Several clinicians who were related service personnel (i.e., school psychologists or school social workers) reported challenges integrating TF-CBT into their priorities, requirements and documentation for working with students with special education classifications. One challenge was how to start TF-CBT with existing students with set Individualized Education Program goals, which the following quote highlights, “A tricky part of working trauma with special ed cases is that it is not always a natural fit. We would have students coming in from other schools who already have goals set. For some students, trauma is related to their underlying behavior. For others, it’s not.” Another comment mentions some confusion about how to address trauma as a focus for students with a mental health-related special education classification, as follows:
There was a lot of confusion because last year we talked about including [this project] into things that were already happening. There was confusion as to whether trauma was related to emotional disturbance eligibility or not.
However, other clinicians reported appreciating the opportunity to focus on trauma as an intervention target within special education, which the following quote illustrates:
For me, it was helpful, being a school social worker, to add to “are you in your seat, are you doing your homework, etc.” It gave me explicit permission to help work with the background reasons and what’s going on outside of school.
Lack of Time.
As a code, “lack of time” was the most frequently-coded concept throughout all the focus group notes and a lack of time code labelled, “TF-CBT is too much with existing responsibilities” was the only code that appeared in all five focus groups.
One of the existing responsibilities noted especially by school psychologists that kept them from being able to implement TF-CBT was psychoeducational testing. However, administrative and other non-clinical contacts were noted as required duties as well:
The main thing is that we just do so many other things. There are entire days when we are just in meetings. The second half of the year on Monday, Tuesday, and Wednesday have been all day meetings for several months. Then I stuff backpacks on Thursday and then I only have one day left and I haven’t seen my IEP kids yet.
All disciplines of clinicians cited limited time at their school sites in general and limited number of days of coverage at any school that made it challenging to enroll TF-CBT cases. For clinicians placed at a school as few as two days a week, it was noted that the administrators may choose to use their time for activities “that are not traditional social work; I plan school events, field trips, macro-style activities…the school …felt there were other ways to use our time.” There was a related concern expressed consistently that the mental health need among students exceeds their capacity in the time they have, and that TF-CBT referrals in addition to their “regular caseload” created waitlists and imposed extra burden and stress on their workflow at schools where they were expected to implement TF-CBT.
Recommendations for addressing this issue were to ensure protected time just for TF-CBT and/or having an additional therapist who is solely assigned to TF-CBT cases. The request for an additional therapist just for TF-CBT surfaced in the context of limited time, but also in the context of their very embedded role in the school that requires them to address a wide variety of student needs and have flexible, crisis-driven schedules when needed.
We battle with our time. Emergencies and crises come up that pull us all over the place. I might get called to another school I know nothing about to do an emergency petition.
This was the case for school-employed and community-employed clinicians, as follows:
We have so many crises all day long in the school. I’m being called during sessions and people knock on my door while I’m with students all the time…If you are a provider who is nice and likes to work within the school setting… who is amongst the school community, you will be pulled in different directions.
Discomfort with Trauma Treatment and Office Space.
In addition to frequent interruptions, concerns were expressed about the physical office environment including shared offices, lack of phone access and spaces not always feeling like a welcoming, supportive place to receive trauma treatment. Two illustrative quotes are as follows:
We don’t have access to private, decent, confidential locations- where we meet is so depressing. It breaks my heart to walk in and look at the room. I think “now let’s open this can of worms” in this space.
I am there twice a week without phone access. If I miss you on those days, we have to wait until next week.
The following quote illustrates how office space limitations and the clinicians’ role in terms of scope of practice may interact to influence the perceived acceptability and appropriateness of TF-CBT:
I only got to the trauma narrative with one client. I struggled with what to do with it after that. I felt like it should be burned. It comes from such a dark place for students. As school clinicians, I personally don’t think it belongs in what we do. We might have a locked space, but people are in and out all the time. We keep things as confidential as we can, but offices are shared. We are in a school, not a clinic.
This quote touches on the trauma narrative being outside scope of practice and not belonging in a school setting due to the physical space and confidentiality considerations. However, it also suggests that the clinician may have experienced some emotional discomfort completing the narrative with the student. Specific comments about clinician’s discomfort with trauma treatment were raised five times across all focus groups and seems to be related to scope of practice issues for these clinicians who may feel trauma treatment is beyond their role and/or comfort level.
Although reviews were mixed about how feasible TF-CBT was for clinicians’ roles in terms of scope of practice in school, consistent concerns about time constraints and office space are reflected in Table 4 as one aspect of overall feasibility barriers. More specifically, school-based clinicians’ role with trauma treatment in terms of limited time and concern related to scope of practice presented barriers to implement TF-CBT, referral to enrollment processes and team processes in the school context (Table 4).
Theme 3: Students and Parents
Clinicians discussed their experiences attempting to enroll students in TF-CBT and their perspectives on how appropriate TF-CBT was for a student based on student and parent factors. Parent preferences was a top barrier rated in the determinants checklist, and qualitative data within this theme suggests this was often related to difficulty with parent engagement, consent and enrollment, as well as how student and family characteristics and experiences may have negatively influenced preferences for and openness to TF-CBT (Table 4). However, clinicians also rated compatibility or fit with students as a primary implementation facilitator, which may be due to high prevalence of trauma exposure among students that was endorsed in the project-end survey as well as in focus groups when discussing students and parents (Table 4).
Parent Engagement, Consent and Enrollment.
The engagement, consent and enrollment processes are multifaceted; clinicians discussed logistical and perceptual barriers to treatment that families experienced. At some schools, there were not enough referrals because teachers were not aware that TF-CBT was available. However, the focus group team also heard that at other schools, TF-CBT referrals created waitlists, so this was a school-specific variation. Consent was difficult to obtain for hard-to-reach parents and for involved parents who were reticent to disclose their child’s trauma or perhaps had trauma histories themselves. In three focus groups, concerns about mandated reporting to child protective services were raised as a barrier to engaging students and families in treatment and to completing the trauma narrative.
Student and Family Characteristics and Experiences.
Clinicians expanded on the engagement, consent, and enrollment code by underscoring various student and family characteristics and experiences that influenced TF-CBT enrollment and implementation. For example, for students with attendance problems, homelessness or other housing instability, dropping out of school or not getting their basic needs met, there would be disruptions in treatment or enrollment and/or completion of TF-CBT might be nearly impossible. Many clinicians expressed concern about students they work with who are living in ongoing or chronic trauma, multigenerational trauma in the family, and unsafe living situations that make TF-CBT inappropriate. For example, one clinician stated:
I felt that TF-CBT was for one trauma and now the student is in a place where everything is safe now. That’s not the reality of the neighborhoods that we’re in. I can work on the historical traumas, but there are traumas happening at home in the moments we’re meeting.
Related to this point, clinicians identified that constant trauma exposure in the community resulted in some students and their families not recognizing the need for trauma treatment because it has become “normalized” and they don’t see it as a traumatic event.
Theme 4: School Environment
There were two primary factors related to the school environment that were reported to affect TF-CBT implementation, school climate and school leadership.
School Climate.
School climate and specifically, the degree to which the school was orderly, safe, supportive and overall trauma-informed. If the school environment was not trauma-informed (i.e., an atmosphere of “chaos”, poor behavioral management, students walking the halls, unsafe spaces), TF-CBT implementation was reported to be much less appropriate. This was particularly the case with respect to returning students to class after a narrative session. Related, clinicians recommended that more trauma-informed practices be provided to teachers and administrators as part of professional development and a whole-school approach to trauma-informed services and supports.
School Leadership.
School leadership, particularly administrators such as principals, were perceived to be invested in and supportive of the clinician’s ability to implement TF-CBT. Clinicians frequently noted that “teacher and principal buy-in about mental health is critical” as a foundation to identify and refer students and support the provision of services during instructional time if needed. One clinician said:
We need admin support for all of these things [including to] hire more staff to lessen the burden of responsibilities. This [TF-CBT] model is time intensive. If we want the value that comes from this, we need to invest the time. Staff are pulled in too many directions… We need [school administrators] on board to connect with families.
Of note, some clinicians provided examples where support in the school was strong and TF-CBT implementation was made a priority, which allowed the clinician to make time to implement, as follows:
Myself, my principal, and my supervisor made an agreement that some things can no longer be my priority so I can focus on TF-CBT. Without an agreement like this, I would get calls and be expected to take care of other things.
Discussion
This mixed methods study of 31 clinicians receiving TF-CBT training in 13 urban public schools was conducted to better understand implementation practices, facilitators and barriers and clinician recommendations to inform successful TF-CBT implementation in schools. The study relied on clinician self-reported quantitative survey and qualitative focus group data. Clinician self-reported practice findings are a common and informative strategy as a start to understanding implementation outcomes following evidence-based practice (EBP) training and consultation. Yet, as we found in this study, clinicians’ adoption and implementation of EBPs can vary following training and other supports, even when the EBP is well-suited to client needs and clinician training interests (Nadeem et al., 2018). Clinicians in this sample reported seeing many students with trauma on their caseload and very little experience with evidence-based assessment and/or treatment to address trauma specifically. In fact, the top facilitators of TF-CBT implementation were the evidence base of the practice, perceived promise of TF-CBT to help students, and the clarity about who would benefit among their students served. Moreover, clinicians generally appreciated the high-quality training in TF-CBT as some of the licensed, practicing school-based clinicians had not regularly received skills-based training and consultation supports through their organizations and/or school district. However, of those students referred, only 40% of potentially eligible students were enrolled in TF-CBT and although clinicians used TF-CBT with a couple of students each, on average, there was a wide range of students enrolled (0 to 15 students per clinician). Taken together, the variable use of TF-CBT among clinicians when: (1) the training and consultation was rated as highly useful, and (2) the practice is highly compatible with student needs and is evidence-based, points to more pressing questions such as: How did implementation work and why or why not was it successful?
Results of clinician focus groups shed light on the differences between clinician values and preferences for clinical practice, and actual implementation of EBPs in schools. Overall, the nature of school mental health clinicians’ role, responsibilities, and workflow are different than that of a traditional clinic-based provider in several ways that necessitate unique considerations and adaptations for TF-CBT implementation in schools. First, some logistical and structural service delivery aspects are quite different when providing mental health services in schools as compared to a traditional clinic; those that were particularly pertinent to TF-CBT feasibility and clinician effort in this study included office space, parent engagement, and session length. School-based clinicians, especially those in low-resource school settings, will likely benefit from organizational leadership and support to access a private, confidential, quiet and therapeutic space on the school campus to conduct TF-CBT sessions. Therapeutic tools and basic supplies for teaching coping skills (from crayons and markers to printers, laminating machines, games and toys) should be available. This may require flexible thinking as school building spaces are sometimes limited, shared, or ill-equipped as clinical spaces. Related, clinicians may also need support from school leaders, supervisors and/or school colleagues to minimize disruptions to their clinical space, particularly for trauma narrative sessions, whenever possible. We recommend clinicians work in partnership with their school colleagues, supervisor and school leadership to problem solve strategies including delivering narrative sessions when there is coverage from another mental health provider in the building, certain days/times of the week that can be uninterrupted, and/or ways for clinicians to signal when sessions that should not be interrupted are in progress. In terms of session length, the traditional 45–60 minute session in clinics is less feasible in schools when students are typically missing instructional time to receive services (Beidas, Edmunds, Marcus, & Kendall, 2012), so clear guidance about how to reduce session length for both PRAC skills and narrative sessions is likely important to promote feasible TF-CBT implementation in schools (Orengo-Aguayo et al., 2020).
In addition, clinicians reported that parent engagement, consent, enrollment, and preferences for TF-CBT were a top barrier for implementation. Although mental health treatment engagement issues including parent involvement are multidimensional (Becker, Boustani, Gellatly, & Chorpita, 2018; Guo, Kataoka, Bear, & Lau, 2014), students seen at school can be initially referred by someone other than their parent or guardian, and once enrolled, parents don’t need to transport their children to sessions. Although prior research indicates that school-based trauma treatment is far more accessible to families than clinic-based trauma treatment (Jaycox et al., 2010), school clinicians may need to take additional steps to establish and maintain a strong partnership with parents throughout the treatment process, as parent-child conjoint sessions are a key component of TF-CBT and parent involvement is optimal for child outcomes. School clinicians could likely benefit from targeted training and consultation support for the referral to enrollment process, as well as to enhance parent engagement in child trauma treatment to support coping, processing, and healing.
Also, we found that school mental health clinicians’ roles, responsibilities, and workflow should be considered in the context of TF-CBT implementation. Limited time to implement evidence-based practices is frequently cited by school mental health clinicians (Lyon et al., 2013), but our results suggest that contributing factors to “limited time” reported by clinicians needs to be unpacked. Although the school day itself is brief, clinician feedback suggests that the broader barrier is numerous responsibilities, a high demand on their time and competing priorities. We learned that school employed clinicians (i.e., school psychologists and social workers) may have less flexibility with their time, more non-clinical duties, and in some cases more barriers with supervisor and school administrator supports to deliver TF-CBT than community-employed mental health providers operating in the schools. This may or may not generalize to other school settings so warrants further exploration in other locales. In the case of this project, participation in the TF-CBT training experience was not optional and allocation of time and how this project impacted the current responsibilities of clinicians was minimally addressed, if at all. Principals agreed to participate in the study, which included releasing their mental health team for required trainings and ongoing consultation calls. However, allocation of time to deliver TF-CBT, or shifting other priorities to accommodate this, was inconsistently provided by administrators and not required for schools to participate in the project. Proactive evaluation of school clinician workload demands and competing priorities to problem solve how to support time management for TF-CBT – in partnership with clinicians, supervisors and administrators - should be considered in future implementation efforts. In addition, consideration of total mental health provider staffing (e.g., total full-time equivalents, days of coverage and number of providers), student body need for trauma treatment and other mental health provider roles and responsibilities could be examined at the school level to proactively assess staffing capacity for TF-CBT. Standard guidelines exist for mental health provider to student ratios by discipline (NASP, 2013), but there are no criteria for optimal mental health team coverage by student body size.
Nonetheless, prior research indicates that individual clinician motivation to implement an EBP is a predictor of implementation success (Beidas et al., 2012; Eiraldi, Wolk, Locke, & Beidas, 2015; Lyon et al., 2013). Therefore, making time for TF-CBT implementation in schools will require that it is valued and viewed as a priority by clinicians, supervisors and school leaders. When school leaders valued trauma interventions and the importance of dedicating time to their delivery by clinicians, there were opportunities to discuss and consider changes to tasks and responsibilities. It is important for administration (school and clinical supervisors) to be on the same page in clarifying clinicians’ roles and responsibilities related to evidence-bases trauma interventions. For example, how does trauma work fits within special education requirements and IEPs, how can it be integrated into treatment plans for students already receiving school-based services, and how can capacity issues be addressed, including limiting or eliminating time on non-clinical/administrative duties such as lunch, recess, and bus duty and other tasks that could be fulfilled by someone who is not a mental health clinician.
Related to school clinicians’ role, some school clinicians reported discomfort delivering trauma treatment. Specifically, focus group data indicate that overall, implementing PRAC skills was more natural to clinicians than the trauma narrative. Some clinicians were motivated to implement but reported concern delivering the trauma narrative portion, whereas others felt trauma treatment was outside their scope of practice entirely and/or did not feel trauma treatment should be delivered in schools. Several clinicians expressed concerns about the dilemma of wanting to work at the system level to help more students, questioning whether the significant time needed for individual treatment would take away from their ability to provide mental health promotion and prevention supports to a larger number of students. Mental health clinicians’ discomfort with or suboptimal delivery of exposure-based treatments is reflected in the literature (Deacon & Farrell, 2013; Zoellner et al., 2011), perhaps because it is emotionally challenging for the clinician and/or they have concern about exposure resulting in client distress. Ultimately, understanding individual clinicians’ readiness and motivation to implement TF-CBT, with the assurance they will receive appropriate support and encouragement to deliver an exposure-based treatment, is a critical factor when selecting clinicians to participate in resource-intensive training and consultation. The trauma narrative is a core component of TF-CBT and when implemented in other low-resource settings in the United States and globally, TF-CBT implementation strategy modifications have proven successful and recommended over changing or removing core components (Cohen, Mannarino, & Deblinger, 2012; Murray, et al., 2013; Orengo-Aguayo et al, 2020). Therefore, it is possible that with context-specific implementation strategies such as using consultation calls to discuss application of the narrative sessions in specialty settings (e.g., schools, telehealth), the TF-CBT model itself may not need to be changed. Yet, recent research on implementation of modular psychotherapy approaches including a trauma protocol with a narrative component has identified school clinicians’ discomfort with trauma narratives (see Corteselli et al., 2020). Therefore, it is reasonable to conclude that clinician acceptance and implementation of the trauma narrative specifically as an exposure-based treatment requires explicit attention in training and ongoing consultation for TF-CBT, perhaps especially in school settings. In summary, a tailored implementation approach for TF-CBT based on contextual determinants of the unique setting, providers and clients served appears necessary, but whether more substantial modifications are needed to the TF-CBT model itself is not yet clear and requires additional research.
Ultimately, training and ongoing consultation for TF-CBT that is tailored specifically to the school environment will likely support implementation with more cases. Topics such as obtaining consent from parents who may have limited contact with the school and/or have their own history of trauma, adapting sessions to school schedules, and/or returning a child to class after a difficult session may have helped increase the likelihood of successful TF-CBT implementation. Also, school leadership and administrative support are critical for EBP implementation in schools (Arnold et al., 2020; Langley, Nadeem, Kataoka, Stein, & Jaycox, 2010; Nadeem et al., 2018). For TF-CBT, these organizational factors are needed not only to address system-level issues such as access to clinical space and supporting the clinicians’ workflow to deliver TF-CBT, but also because when school leaders were invested, they were more likely to integrate trauma sensitive practices into the school building, offering a school environment that would be more supportive of youth, including youth receiving TF-CBT services.
Limitations
The results of this study should be interpreted in the context of several notable limitations. First, we encourage readers to consider the clinician demographics and professional characteristics of our relatively small sample of 31 clinicians to inform assumptions about potential generalizability of these findings to other clinician groups. However, within this small sample we were able to sample a relatively diverse cross-section of school mental health clinician roles and years of experience. Future studies with larger sample sizes of clinicians implementing TF-CBT in schools could examine additional factors that may predict implementation, such as caseload, school characteristics, grade bands served, or any other meaningful school-, clinician- or student- level variables. Second, we were limited to using self-reported TF-CBT practices submitted by clinicians which was difficult to overcome with more objective methods given the autonomy of school mental health clinicians to manage their own referrals, outreach, assessment and enrollment processes at their school sites. Future studies should ideally include a design element to validate clinician practice data. Third, focus group feedback is limited to our sample of clinicians with variable levels of implementation, including some clinicians who barely implemented the TF-CBT model due to barriers faced at the engagement and enrollment phase. As a result, our recommendations are primarily focused on how to overcome barriers. For instance, parent engagement difficulties were cited for the referral to enrollment process but due to variable to low implementation overall, we did not hear feedback about the feasibility of conjoint parent-child sessions in school which are part of the TF-CBT model. Therefore, the degree to which conjoin sessions occurred, or the feasibility of them in the school settings, is unknown to the research team and we recommend explicit inquiry of this in future TF-CBT implementation in schools. Also, qualitative feedback suggests that there was between-school variation in administrative and supervisory supports for TF-CBT implementation as a priority in the school. There was also variation in school culture and climate as some environments were perceived as so chaotic as to impact efficacy of TF-CBT. Due to the small numbers of clinicians within each school and the small number of schools, we were unable to quantitatively account for school-level effects on implementation.
Conclusion
TF-CBT is a relevant and promising intervention for delivery in school settings, but school-based implementation could benefit from specific adaptations, consultation and organizational supports to optimize its feasibility. Several adjustments were recommended to help optimize fit of TF-CBT in schools, including adaptations to the model itself, workflow adjustment for clinicians that would offer dedicated time for providing TF-CBT, specific consultation and coaching to engage parents, and consistent, unwavering support from their leadership team. Future implementation strategies for TF-CBT in schools could be selected based on determinants reported in this study as well as local determinants of practice assessed prior to implementation. Also, school-based mental health clinician roles and responsibilities and openness to delivering trauma treatment should be carefully considered when planning training and implementation. Finally, TF-CBT or any “Tier 3” or indicated treatment intervention will have optimal implementation in school buildings where students, clinicians, and/or teachers feel as though it is a safe, supportive and orderly school environment. TF-CBT implementation is only one component of a comprehensive, multi-tiered approach to a trauma-informed school setting (Chafouleas, Johnson, Overstreet, & Santos, 2016). Ultimately, the use of evidence-based trauma treatment delivered in schools is aligned with other trauma-informed practices throughout the school building and whole school safety planning activities which provide a strong foundation for building resilience through a positive culture and climate of student-centered supports.
Acknowledgements:
We are indebted to the schools and school mental health clinicians who participated in this study. We also thank Ms. Rebecca LaCosta and Ms. Marie Yuille for their assistance with study data collection and management, Ms. Kaylyn Garcia for her assistance preparing references and Ms. Vickie Beck for her contribution as a TF-CBT trainer.
Footnotes
After the first two focus groups, facilitators began probing for feedback on various components of the TF-CBT model to understand clinicians’ perspectives on acceptability and appropriateness of the trauma narrative specifically as compared to other parts of the TF-CBT model.
References
- Ali MM, West K, Teich JL, Lynch S, Mutter R, & Dubenitz J (2019). Utilization of Mental Health Services in Educational Setting by Adolescents in the United States. Journal of School Health, 89(5), 393–401. doi: 10.1111/josh.12753 [DOI] [PubMed] [Google Scholar]
- Arnold KT, Pollack Porter KM, Frattaroli S, Durham RE, Mmari K, Clary LK, & Mendelson T (2020). Factors that Influenced Adoption of a School-Based Trauma-Informed Universal Mental Health Intervention. Prevention Science. doi: 10.1007/s11121-020-01144-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker R, Camosso- Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S, … & Jaeger C (2015). Tailored interventions to address determinants of practice. Cochrane Database of Systematic Reviews, (4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker KD, Boustani M, Gellatly R, & Chorpita BF (2018). Forty years of engagement research in children’s mental health services: Multidimensional measurement and practice elements. Journal of Clinical Child & Adolescent Psychology, 47(1), 1–23. [DOI] [PubMed] [Google Scholar]
- Beidas RS, Edmunds JM, Marcus SC, & Kendall PC (2012). Training and consultation to promote implementation of an empirically supported treatment: A randomized trial. Psychiatric Services, 63(7), 660–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beidas RS, Mychailyszyn MP, Edmunds JM, Khanna MS, Downey MM, & Kendall PC (2012). Training School Mental Health Providers to Deliver Cognitive-Behavioral Therapy. School Mental Health, 4(4), 197–206. doi: 10.1007/s12310-012-9074-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns BJ, Costello EJ, Angold A, Tweed D, Stangl D, Farmer EM, & Erkanli A (1995). Children’s mental health service use across service sectors. Health affairs (Project Hope), 14(3), 147–159. [DOI] [PubMed] [Google Scholar]
- Carliner H, Keyes KM, McLaughlin KA, Meyers JL, Dunn EC, & Martins SS (2016). Childhood trauma and illicit drug use in adolescence: A population-based national comorbidity survey replication–adolescent supplement study. Journal of the American Academy of Child & Adolescent Psychiatry, 55(8), 701–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chafouleas SM, Johnson AH, Overstreet S, & Santos NM (2016). Toward a blueprint for trauma-informed service delivery in schools. School Mental Health, 8(1), 144–162. [Google Scholar]
- Cohen JA, Deblinger E, Mannarino AP, & Steer RA (2004). A multisite, randomized controlled trial for children with sexual abuse–related PTSD symptoms. Journal of the American Academy of Child & Adolescent Psychiatry, 43(4), 393–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, & Deblinger E (2012). Trauma-focused CBT for children and adolescents: Treatment applications: Guilford Press. [Google Scholar]
- Copeland WE, Keeler G, Angold A, & Costello EJ (2007). Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry, 64(5), 577–584. [DOI] [PubMed] [Google Scholar]
- Corteselli KA, Hollinsaid NL, Harmon SL, Bonadio FT, Westine M, Weisz JR, & Price MA (2020). School counselor perspectives on implementing a modular treatment for youth. Evidence-Based Practice in Child and Adolescent Mental Health, 5(3), 271–287. [Google Scholar]
- de Arellano MAR, Lyman DR, Jobe-Shields L, George P, Dougherty RH, Daniels AS, … Delphin-Rittmon ME (2014). Trauma-focused cognitive-behavioral therapy for children and adolescents: Assessing the evidence. Psychiatric Services, 65(5), 591–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deacon BJ, & Farrell NR (2013). Therapist barriers to the dissemination of exposure therapy Handbook of treating variants and complications in anxiety disorders (pp. 363–373): Springer. [Google Scholar]
- Dye H (2018). The impact and long-term effects of childhood trauma. Journal of Human Behavior in the Social Environment, 28(3), 381–392. [Google Scholar]
- Eiraldi R, Wolk CB, Locke J, & Beidas R (2015). Clearing hurdles: The challenges of implementation of mental health evidence-based practices in under-resourced schools. Advances in School Mental Health Promotion, 8(3), 124–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgerald MM, & Cohen JA (2012). Trauma-focused cognitive behavior therapy for school psychologists. Journal of Applied School Psychology, 28(3), 294–315. [Google Scholar]
- Flottorp SA, Oxman AD, Krause J, Musila NR, Wensing M, Godycki-Cwirko M, … Eccles MP (2013). A checklist for identifying determinants of practice: a systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implementation Science, 8, 35. doi: 10.1186/1748-5908-8-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillies D, Maiocchi L, Bhandari AP, Taylor F, Gray C, & O’Brien L (2016). Psychological therapies for children and adolescents exposed to trauma. Cochrane Database Syst Rev, 10, CD012371. doi: 10.1002/14651858.CD012371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman RD, Miller MD, & West-Olatunji CA (2012). Traumatic stress, socioeconomic status, and academic achievement among primary school students. Psychological Trauma: Theory, Research, Practice, and Policy, 4(3), 252. [Google Scholar]
- Goodwin RD, & Stein MB (2004). Association between childhood trauma and physical disorders among adults in the United States. Psychological Medicine, 34(3), 509–520. doi: 10.1017/s003329170300134x [DOI] [PubMed] [Google Scholar]
- Guo S, Kataoka SH, Bear L, & Lau AS (2014). Differences in school-based referrals for mental health care: Understanding racial/ethnic disparities between Asian American and Latino youth. School Mental Health, 6(1), 27–39. [Google Scholar]
- Hanson RF, Gros KS, Davidson TM, Barr S, Cohen J, Deblinger E, … Ruggiero KJ (2014). National trainers’ perspectives on challenges to implementation of an empirically-supported mental health treatment. Administration and Policy in Mental Health and Mental Health Services Research, 41(4), 522–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaycox LH, Cohen JA, Mannarino AP, Walker DW, Langley AK, Gegenheimer KL, … Schonlau M (2010). Children’s mental health care following Hurricane Katrina: A field trial of trauma- focused psychotherapies. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies, 23(2), 223–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaycox LH, Kataoka SH, Stein BD, Langley AK, & Wong M (2012). Cognitive behavioral intervention for trauma in schools. Journal of Applied School Psychology, 28(3), 239–255. [Google Scholar]
- Kataoka SH, Zhang L, & Wells KB (2002). Unmet need for mental health care among US children: Variation by ethnicity and insurance status. American Journal of Psychiatry, 159(9), 1548–1555. [DOI] [PubMed] [Google Scholar]
- Kibler JL (2009). Posttraumatic stress and cardiovascular disease risk. Journal of trauma & dissociation, 10(2), 135–150. [DOI] [PubMed] [Google Scholar]
- Langley AK, Gonzalez A, Sugar CA, Solis D, & Jaycox L (2015). Bounce back: Effectiveness of an elementary school-based intervention for multicultural children exposed to traumatic events. Journal of consulting and clinical psychology, 83(5), 853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langley AK, Nadeem E, Kataoka SH, Stein BD, & Jaycox LH (2010). Evidence-based mental health programs in schools: Barriers and facilitators of successful implementation. School Mental Health, 2(3), 105–113. doi: 10.1007/s12310-010-9038-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson S, Chapman S, Spetz J, & Brindis CD (2017). Chronic childhood trauma, mental health, academic achievement, and school- based health center mental health services. Journal of School Health, 87(9), 675–686. [DOI] [PubMed] [Google Scholar]
- Little SG, Akin- Little A, & Gutierrez G (2009). Children and traumatic events: Therapeutic techniques for psychologists working in the schools. Psychology in the Schools, 46(3), 199–205. [Google Scholar]
- Lyon AR, Ludwig K, Romano E, Leonard S, Stoep AV, & McCauley E (2013). “If it’s worth my time, i will make the time”: school-based providers’ decision-making about participating in an evidence-based psychotherapy consultation program. Administration and Policy Mental Health and Mental Health Services Research, 40(6), 467–481. doi: 10.1007/s10488-013-0494-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyon AR, Pullmann MD, Dorsey S, Levin C, Gaias LM, Brewer SK, Larson M, Corbin CM, Davis C, Muse I, Joshi M, Reyes R, Jungbluth NJ, Barrett R, Hong D, Gomez MD, & Cook CR (in press). Protocol for a Hybrid Type 2 Cluster Randomized Trial of Trauma-Focused Cognitive Behavioral Therapy and a Pragmatic Individual-Level Implementation Strategy. Implementation Science. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandavia A, Robinson GG, Bradley B, Ressler KJ, & Powers A (2016). Exposure to childhood abuse and later substance use: Indirect effects of emotion dysregulation and exposure to trauma. Journal of Traumatic Stress, 29(5), 422–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, Dorsey S, Skavenski S, Kasoma M, Imasiku M, Bolton P, … Cohen JA (2013). Identification, modification, and implementation of an evidence-based psychotherapy for children in a low-income country: the use of TF-CBT in Zambia. International Journal of Mental Health Systems, 7(1), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadeem E, Saldana L, Chapman J, & Schaper H (2018). A mixed methods study of the stages of implementation for an evidence-based trauma intervention in schools. Behavior therapy, 49(4), 509–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NASP. (2013). National Association of School Psychologist (NASP) Recommendations for Comprehensive School Safety Policies. Bethesda, MD. [Google Scholar]
- NICE. (2018). National Institute for Health and Care Excellence (NICE) Guidance: Post-traumatic stress disorder Management of PTSD in children, young people and adults. England. [Google Scholar]
- Orengo-Aguayo R, Stewart RW, Villalobos BT, Hernandez Rodriguez J, Dueweke AR, de Arellano MA, & Young J (2020). Listen, don’t tell: Partnership and adaptation to implement trauma-focused cognitive behavioral therapy in low-resourced settings. American Psychologist, 75(8), 1158. [DOI] [PubMed] [Google Scholar]
- Padden J, Ruiz R, Milburn R, & Lawrence-Webb C (2016). School Social Work, School Psychology, and School Counseling: A Venn Diagram of Services. Baltimore City Public Schools. Accessible as a teaming resource; in: http://www.theshapesystem.com [Google Scholar]
- Rivera S (2012). Schools. In Deblinger E, Cohen JA & Mannarino A (Eds.), Trauma-Focused CBT for Children and Adolescents: Treatment Applications. (pp. 29–48). The Guilford Press. [Google Scholar]
- Saunders BE, & Adams ZW (2014). Epidemiology of traumatic experiences in childhood. Child and Adolescent Psychiatric Clinics, 23(2), 167–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Decker KB, & Pynoos RS (2004). The University of California at Los Angeles post-traumatic stress disorder reaction index. Current psychiatry reports, 6(2), 96–100. [DOI] [PubMed] [Google Scholar]
- Zoellner LA, Feeny NC, Bittinger JN, Bedard-Gilligan MA, Slagle DM, Post LM, & Chen JA (2011). Teaching trauma-focused exposure therapy for PTSD: Critical clinical lessons for novice exposure therapists. Psychological Trauma: Theory, Research, Practice, and Policy, 3(3), 300. [DOI] [PMC free article] [PubMed] [Google Scholar]


