Abstract
Background
The specific challenges experienced by the nursing and midwifery workforce in previous pandemics have exacerbated pre-existing professional and personal challenges, and triggered new issues. We aimed to determine the psychological impact of the COVID-19 pandemic on the UK nursing and midwifery workforce and identify potential factors associated with signs of post-traumatic stress disorder.
Methods
A United Kingdom national online survey was conducted at three time-points during the first wave of the COVID-19 pandemic between April and August 2020 (T1 and T2 during initial wave; T3 at three-months following the first wave). All members of the UK registered and unregistered nursing and midwifery workforce were eligible to participate. The survey was promoted via social media and through organisational email and newsletters.
The primary outcome was an Impact of Events Scale-Revised score indicative of a post-traumatic stress disorder diagnosis (defined using the cut-off score ≥33). Multivariable logistic regression modelling was used to assess the association between explanatory variables and post-traumatic stress disorder.
Results
We received 7840 eligible responses (T1- 2040; T2- 3638; T3- 2162). Overall, 91.6% participants were female, 77.2% were adult registered nurses, and 28.7% were redeployed during the pandemic.
An Impact of Events Scale-Revised score ≥33 (probable post-traumatic stress disorder) was observed in 44.6%, 37.1%, and 29.3% participants at T1, T2, and T3 respectively. At all three time-points, both personal and workplace factors were associated with probable post-traumatic stress disorder, although some specific associations changed over the course of the pandemic. Increased age was associated with reduced probable post-traumatic stress disorder at T1 and T2 (e.g. 41–50 years at T1 odds ratio (OR) 0.60, 95% confidence interval (CI) 0.42–0.86), but not at T3. Similarly, redeployment with inadequate/ no training was associated with increased probable post-traumatic stress disorder at T1 and T2, but not at T3 (T1 OR 1.37, 95% CI 1.06–1.77; T3 OR 1.17, 95% CI 0.89–1.55). A lack of confidence in infection prevention and control training was associated with increased probable post-traumatic stress disorder at all three time-points (e.g. T1 OR 1.48, 95% CI 1.11–1.97).
Conclusion
A negative psychological impact was evident 3-months following the first wave of the pandemic. Both personal and workplace are associated with adverse psychological effects linked to the COVID-19 pandemic.
These findings will inform how healthcare organisations should respond to staff wellbeing needs both during the current pandemic, and in planning for future pandemics.
Keywords: COVID-19, Nurses, Midwives, Pandemics, Post-traumatic stress disorders, Professional burnout, Psychological distress, Survey
What is already known
-
•
Nursing and midwifery workforce wellbeing is under strain due to staff shortages and high stress and burnout.
-
•
The nursing and midwifery workforce are at the forefront of the COVID-19 response.
-
•
In previous pandemics, the nursing and midwifery workforce has experienced worse psychological effects, compared with other healthcare professional groups.
What this paper adds
-
•
Almost 30% of survey respondents reported experiences indicative of a probable post-traumatic stress disorder diagnosis three-months after the first pandemic peak.
-
•
Key workplace-related factors were associated with adverse psychological effects, including redeployment to other clinical areas without adequate training and inadequate infection control training.
-
•
Healthcare organisations should urgently implement evidence-based strategies to support the wellbeing of members of the nursing and midwifery workforce affected by the pandemic, and develop robust workforce plans in preparation for future pandemics.
1. Introduction
The year 2020 was designated by the World Health Organization as International Year of the Nurse and Midwife (World Health Organization 2020b). This reflects the critical role nurses and midwives play in international health and social care delivery, policy and research. Underpinning this designation is a workforce already under significant pressure with high levels of attrition, ongoing recruitment challenges, and an ageing workforce (World Health Organization, 2020a). Across the world, a shortfall of 5.7 million nurses has been predicted by 2030 (World Health Organization, 2020a). In the United Kingdom (UK), the National Health Service (NHS) long-term plan included a commitment to improve staff recruitment and retention (National Health Service, 2019). However, this is against a backdrop of over 40,000 whole-time equivalent nursing vacancies and rates of dissatisfaction and plans to leave the profession in the UK that exceed many other European countries (Aiken et al., 2012; National Audit Office, 2020).
At the end of 2019, just prior to the start of the International Year of the Nurse and Midwife, the Severe Acute Respiratory Syndrome- Coronavirus 2 virus was first identified in China. The subsequent COVID-19 pandemic has both highlighted nurses’ and midwives’ essential role in healthcare delivery and served to exacerbate existing workforce challenges. The impact of COVID-19 on society has been well-documented, both as a direct result of the virus and indirectly through strategies (e.g., restrictions on travel and social gatherings; closure of workplaces and educational institutions) implemented to limit infection transmission (Douglas et al., 2020). In addition to these wider societal effects, nurses and midwives have faced the added challenge of healthcare provision in the context of lack of personal protective equipment, the rapid implementation of redeployment (move to a different clinical area to support the pandemic response), new ways of working, and vast numbers of high acuity patients (Fernandez et al., 2020; Liu et al., 2020; Maben and Bridges, 2020). Nurses and midwives have also faced the emotional challenge of high mortality rates, with 30.8% patients hospitalised with COVID-19 dying (Navaratnam et al., 2021). Observational studies highlight the increased risk of COVID-19 infection to frontline healthcare workers, such as nurses and midwives (Chou et al., 2020; Mutambudzi et al., 2020; Nguyen et al., 2020; Shah et al., 2020). The increased risk of infection may also extend to members of the healthcare worker's family (Shah et al., 2020). Reports have also highlighted the tragic loss of life due to COVID-19 infection amongst member of the nursing and midwifery workforce (Bandyopadhyay et al., 2020).
Early COVID-19 data from China and studies of previous pandemics and disease outbreaks have highlighted the potential effect of the pandemic on healthcare worker's mental health (Allan et al., 2020; Cabarkapa et al., 2020; De Kock et al., 2021; Fernandez et al., 2020; Stuijfzand et al., 2020). Some previous COVID-19 studies report worse psychological effects in nurses, compared with other healthcare workers (Allan et al., 2020; Cabarkapa et al., 2020). A recent systematic review of studies on mental health disorders in hospital-based healthcare workers in hospitals impacted by pandemics included 19 studies, of which most described the impact of the Severe Acute Respiratory Syndrome pandemic in Canada and South Asia (Allan et al., 2020). The review identified that post-traumatic stress, anxiety, and depression were common in healthcare workers during pandemics, with some concerning long-lasting effects.
This combination of pre-existing workforce challenges, rapid changes to professional life and ways of working, and risk of illness to both the individual and their family may have important and demonstrable psychological impacts on the UK nursing and midwifery workforce. On this basis, we identified the need to rapidly design and undertake research to understand the psychological impacts of the first wave of the COVID-19 pandemic on the UK nursing and midwifery workforce. This has been recognised as a key research priority by members of the public, mental health experts, and members of the nursing and midwifery workforce (Holmes et al., 2020; Manning et al., 2021). The aims of the study were to assess the mental health effects of the pandemic over time on the nursing workforce and identify the personal and workplace factors associated with wellbeing to inform the response to the current pandemic and support preparation for future pandemics.
2. Methods
A national longitudinal online survey study was conducted utilising a self-selecting sample of the UK nursing and midwifery workforce across three time-points to explore the self-reported personal psychological impact of the COVID-19 pandemic. The survey design and methodology drew on that developed for the COVID-19 emergency response assessment study (Roberts et al., 2021a; Roberts et al., 2020). This paper is reported in accordance with the Checklist for Reporting Results of Internet E-Surveys (Eysenbach, 2004).
2.1. Overview of survey
The survey was administered at three time-points (T1, T2, T3) through an online survey platform (Qualtrics, Provo, Utah, USA) and could be completed in approximately 10–15 min.
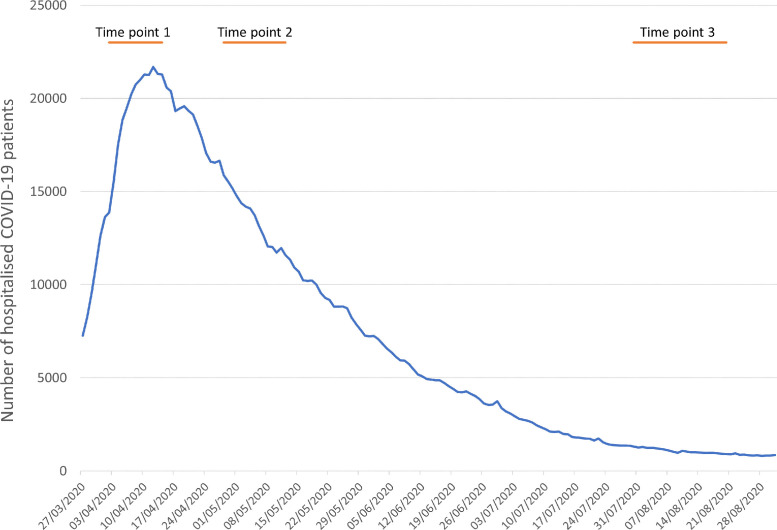
Our T1, T2, and T3 surveys were open for responses between 2nd and 14th April 2020, 28th April and 12th May 2020, and 30th July and 20th August 2020 respectively. During the first pandemic wave the number of hospitalised cases increased more rapidly than expected and then decreased more rapidly than expected. As such, both the highest number of hospitalised COVID-19 patients (21,686 on 12th April 2020) and number of deaths where COVID-19 was recorded on the death certificate (1457 on 8th April 2020) occurred during our T1 survey (UK Government, 2021). Fig. 1 shows our survey distribution time points in the context of the number of hospitalised patients across the UK. There was some regional variation in date of the peak and subsequent recovery trajectory (supplementary material, Fig. e1). Our T3 survey, issued three months after the T2 survey, was designed to reflect a COVID-19 recovery period.
Fig. 1.
Survey time-points in context of number of hospitalised cases across UK.
Survey questions covered six broad domains: participant demographics, professional characteristics, experience of work during the pandemic, personal impact of COVID-19, access to psychological support, and mental health and wellbeing outcomes (supplementary material table e1). Mental health and wellbeing outcomes were collected using validated tools, namely the impact of events-revised scale, Depression Anxiety Stress scales- 21 (DASS-21), Maslach Burnout Inventory (T3 survey only) and intention-to-leave scale (T3 survey only) (Antony et al., 1998; Chen et al., 2019; Creamer et al., 2003; Lovibond and Lovibond, 1996; Poghosyan et al., 2009; Weiss, 2006).
Questions were consistent across each survey, although minor changes were made to reflect emerging evidence as the pandemic progressed. In particular, we included ethnicity for our second and third survey to reflect evidence highlighting the disproportionate impact of COVID-19 on Black, Asian and minority ethnic populations (Ferrando-Vivas et al., 2021; Williamson et al., 2020).
2.2. Eligibility criteria
Study participation was open to all members of the nursing and midwifery workforce working in the UK. This included registered nurses and midwives, student nurses and midwives, healthcare assistants, nursing associates, and trainee nursing associates. Inclusion was not limited by employer type.
2.3. Survey promotion and distribution
Information about the survey and an internet link were widely distributed through social media (Twitter, Facebook). High-profile individuals in the UK nursing and midwifery community actively encouraged survey promotion by participants. In addition, survey information was included in emails distributed by key nursing and midwifery organisations (e.g., Royal College of Nursing) and the UK nursing and midwifery regulator (Nursing and Midwifery Council). The survey was also reported as a news story in mainstream journals Mitchell (2020). Access to the survey was open to any individual with the study internet address link. At both T2 and T3, we also directly emailed individuals that had completed our survey at a previous time-point and who had provided their email address and consented to use of their personal data for this purpose. A reminder email was sent approximately half-way through the survey period. No incentive was offered for completion.
Following T1 and T2 surveys, a brief summary of aggregated data was rapidly distributed so that findings could inform public policy. These summaries were featured by various news outlets including BBC News, and national newspapers (BBC News, 2020; Hackett, 2020; Toynbee, 2020).
2.4. Survey design
Survey questions were based on the author's expert subject knowledge, evidence from previous pandemics and disease outbreaks (e.g., Ebola, Severe Acute Respiratory Syndrome), other ongoing surveys, and emerging information about the COVID-19 pandemic (Roberts et al., 2020, Roberts et al., 2021b). The first page of the survey provided key information, including its purpose and length, and how we would manage personal data. We mandated completion of only the first two questions, which were used to confirm eligibility and record consent for study participation. Completion of subsequent questions was not mandated.
Adaptive questioning was used to filter questions that were not relevant based on preceding responses (e.g., questions about experience of redeployment were shown only to those individuals that were redeployed). We did not randomise the order of any part of the survey. In designing the survey, text entry was minimised and categorical responses were favoured. A survey back button allowed participants to review their answers as they progressed through the survey. The survey design was reviewed at each time-point to reflect emerging data and, where necessary, alter question grammatical tense to reflect the stage of the pandemic. For each survey version, the research team completed a draft of the survey using different response variations to ensure that the survey functioned as expected.
In the survey, we invited participants to provide their email address, and explicit agreement was sought to use this to: link information across surveys; inform the participant about surveys at subsequent time-points, and invite them to participate in future research. We did not limit responses by IP addresses as we anticipated that participants may complete the survey at their place of work or using a shared home internet router, such that a restriction might prevent completion by eligible colleagues or family members, who were also nurses.
2.5. Outcomes
The primary outcome was the prevalence of post-traumatic stress disorder, measured using the impact of events scale-revised at each time point (Creamer et al., 2003; Weiss, 2006). For each of the 22 items in the scale, participants were asked to rate the extent to which they had been distressed in relation to COVID-19 over the preceding 7-days. Based on previous research, we categorised a score of 33 or above as indicative of probable post-traumatic stress disorder (Creamer et al., 2003).
Secondary outcomes were depression, anxiety, stress, job satisfaction, burnout and the participant's intention to leave both their current role and healthcare, measured using validated tools (Antony et al., 1998; Chen et al., 2019; Lovibond and Lovibond, 1996; Poghosyan et al., 2009). A summary of outcome definitions and tools is included in the supplementary material (table e2). Outcomes were measured at each of the three time points, except for burnout and intention to leave which were captured at time-point three only to reflect the need to measure these concepts in a period of relative stability.
2.6. Statistical analysis
Data were downloaded directly from the survey hosting platform (Qualtrics, Provo, Utah, USA). Initial data processing and cleaning were undertaken using SPSS version 26 (IBM SPSS Statistics, Armonk, NY, USA). Imputation and modelling were undertaken using Stata version 16.1 (College Station, Texas, USA).
Our initial review of the three datasets identified 267 individuals that had completed the survey at all three time-points and 898 (216 at T1/T2; 154 at T1/T3; 528 at T2/T3) individuals completed the survey at two time-points. This is likely to be an underestimate of the true rate as we were only able to track responses where an individual had both provided a matching email address and had given permission to link data. Given the low frequency of completion at multiple time-points, we decided to treat each survey time-point as an independent sample in our primary analysis.
To be included in the analysis, we required participants to have completed one or more questions beyond the first two survey sections (professional characteristics and participant demographics), and to have completed at least one outcome measure (one of: impact of events scale-revised, Depression Anxiety Stress scales- 21, Maslach Burnout Inventory (T3 only) and intention-to-leave scale (T3 only)).
We identified duplicate responses through the recorded email address. Across T1, T2, and T3, we identified 310 duplicate responses. In most cases (93% duplicates), the first record was selected for inclusion. However, in a minority of cases (7%) where the first record contained little data or key outcomes (impact of events scale-revised, Depression Anxiety Stress scales- 21, and Maslach Burnout Inventory) were missing, we included the second response.
We observed data missingness across survey responses due to abandonment of the survey during completion and, presumed unintentional, omission of individual questions within the survey. Multiple imputation using the chained equations method was used to impute missing data. The imputation model included all variables used in the subsequent multivariable modelling plus other variables that were thought might predict either study outcomes or explanatory variables that we planned to model (supplementary material table e1) (Royston and White, 2011). Twenty imputed datasets were created using a method appropriate for data consisting of multiple psychometric scales (Plumpton et al., 2016). Based on the fraction of missing information measure from the multivariable models (T1- 0.098; T2- 0.133; T3- 0.121), 14 datasets were required to meet the criterion proposed by the UCLA Statistical Consulting Group (UCLA: Statistical Consulting Group).
All data variables, except for some outcomes, were categorical and are described using numbers and percentages. Our outcome measures included both those that provide an overall score and those that categorise individuals based on score cut-off values. For the former, we summarise data using the mean and 95% confidence interval or median and interquartile range, depending on data normality. The latter, we present as number and percentage in each category. We calculated Cronbach's α, mean scores and 95% confidence interval (CI) and Pearson correlations for the impact of events scale-revised and Depression Anxiety Stress scales- 21 sub-scales across time-points. For the Maslach Burnout Inventory, we calculated Cronbach's αfor sub-scales. We also explored the correlation between the impact of events scale-revised and Depression Anxiety Stress scales- 21 sub-scales, and the impact of pattern of response on impact of events scale-revised and Depression Anxiety Stress scales- 21.
We tested for equality across time. The type of test used depended on whether the variable had been imputed or not, and its measurement scale. For variables with two categories a logistic regression model was used and an ordinal regression model was used for three or more ordered categories. For variables with three or more categories with no natural order a multilogit model was used if the data had been imputed and the Pearson χ2 test if not. The logistic, multilogit and ordinal regression models fitted to imputed variables were tested for equality using a F statistic and the likelihood ratio statistic (χ2) for all other non-imputed variables. To improve readability, we combine some of the ordinal categories in the text for reporting, although the statistical test always relates to the original scale. A regression model was used to compute a F statistic for continuous variables although the degrees of freedom for imputed and non-imputed variables were calculated differently.
We fitted multivariable logistic regression models to individual imputed datasets, and then combined the results to obtain estimates of the association between key explanatory variables and an impact of events scale-revised score of 33 or more (probable post-traumatic stress disorder) (Creamer et al., 2003). We included variables based on clinical plausibility (supplementary material table e1), informed by previous literature, and developed individual models for each time-point. We measured the association between the explanatory variables and the dichotomous outcomes using odds ratios (OR) and 95% CI. For explanatory variables with three or more categories, we tested the overall effect for statistical significance using a F statistic. In a sensitivity analysis that was not defined a priori, we added a variable that categorised participant's pattern of response (e.g. those that only completed at a single time-point and those that completed at multiple time-points) to explore how this affected our model's findings.
2.7. Ethical approval
The study was approved by the University of Warwick Biomedical and Scientific Research Ethics Committee on 27th March 2020 (reference 101/19–20). Participants gave informed consent for participation through a checkbox at the start of the survey. All survey data were stored in accordance with national legislation and institutional policies.
3. Results
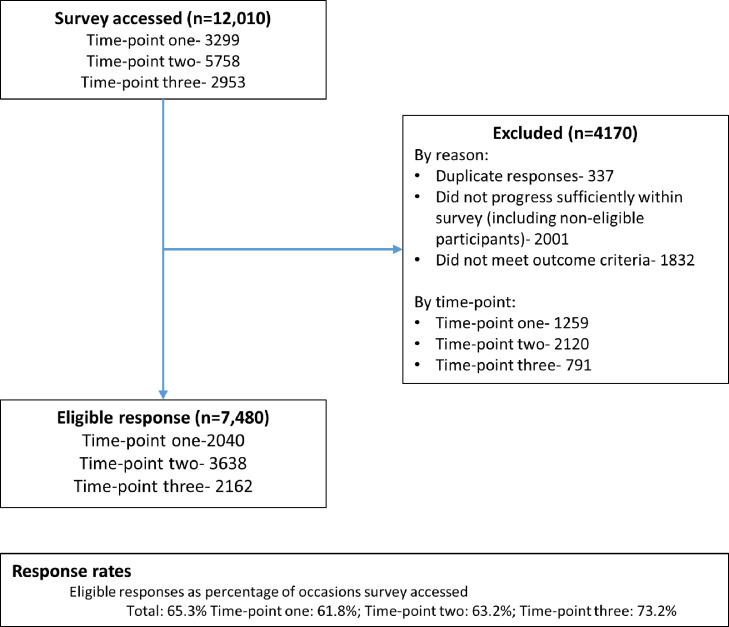
Across the three survey time-points, the survey was accessed on 12,010 occasions (3299 T1, 5758 T2, 2953 T3), of which we finally included 7840 responses (Fig. 2 ). The highest number of responses (n = 3638) was received at T2.
Fig. 2.
study flow chart.
3.1. Participant characteristics
Across all survey responses, most participants were female (T1 91.6%; T2 91.6%; T3 91.9%, p = 0.20, and of white ethnicity (T2 89.3%; T3 93.1%, p < 0.001). The most common age group was 51–60 years (T1 30.7%; T2 34.7%; T3 39.8%, p < 0.001). Professionally, the majority were adult registered nurses (T1 77.9%; T2 75.1%; T3 80.0%, p = 0.001). Table 1 summarises key personal and workplace variables, with the remainder summarised in table e3 (supplementary material).
Table 1.
Baseline characteristics.
| T1 (n = 2040) n(%) | T2 (n = 3638) n(%) | T3 (n = 2162) n(%) | P-value | ||
|---|---|---|---|---|---|
| Personal factors† | |||||
| Gender (mlogit) | F(4, 4.5e+08) = 1.50 | ||||
| Male | 160 (7.9) | 271 (7.5) | 166 (7.7) | ||
| Female | 1868 (91.6) | 3331 (91.6) | 1986 (91.9) | ||
| Other/prefer not to say | 12 (0.6) | 36 (1.0) | 10 (0.5) | p = 0.20 | |
| Age (years) (oreg) | F(2, 1.6e+07) = 39.48 | ||||
| 16–30 | 265 (13.0) | 381 (10.5) | 158 (7.3) | ||
| 31–40 | 406 (19.9) | 660 (18.1) | 321 (14.9) | ||
| 41–50 | 600 (29.4) | 1061 (29.2) | 620 (28.7) | ||
| 51–60 | 626 (30.7) | 1263 (34.7) | 860 (39.8) | ||
| 61 and over | 143 (7.0) | 273 (7.5) | 204 (9.4) | p<0.001 | |
| Ethnicity (mlogit) | F(3,336,836.6) = 9.43 | ||||
| White | 3248 (89.3) | 2012 (93.1) | |||
| Mixed/Multiple ethnic | 55 (1.5) | 35 (1.6) | |||
| Asian/Asian British | 126 (3.5) | 39 (1.8) | |||
| Black/African/Caribbean | 210 (5.8) | 76 (3.5) | p<0.001 | ||
| UK Region (mlogit) | F(20, 1.8e+08) = 4.58 | ||||
| South East | 322 (15.8) | 562 (15.4) | 326 (15.1) | ||
| South West | 220 (10.8) | 383 (10.5) | 234 (10.8) | ||
| London | 227 (11.1) | 526 (14.4) | 297 (13.7) | ||
| East Midlands | 214 (10.5) | 267 (7.3) | 173 (8.0) | ||
| East of England | 146 (7.2) | 276 (7.6) | 191 (8.9) | ||
| North West | 262 (12.9) | 380 (10.4) | 197 (9.1) | ||
| North East (including Yorkshire) | 126 (6.2) | 340 (9.4) | 227 (10.5) | ||
| West Midlands | 228 (11.2) | 311 (8.6) | 186 (8.6) | ||
| Scotland | 168 (8.3) | 345 (9.5) | 187 (8.7) | ||
| Wales | 86 (4.2) | 154 (4.2) | 108 (5.0) | ||
| Northern Ireland | 39 (1.9) | 96 (2.6) | 35 (1.6) | p<0.001 | |
| Professional qualification (mlogit) | F(12, 4.8e+07) = 2.84 | ||||
| RN - adult | 1589 (77.9) | 2732 (75.1) | 1730 (80.0) | ||
| RN - child | 109 (5.4) | 211 (5.8) | 111 (5.1) | ||
| RN- learning disability | 15 (0.7) | 52 (1.4) | 21 (1.0) | ||
| RN- mental health | 132 (6.5) | 284 (7.8) | 116 (5.4) | ||
| Midwife/Health visitor | 58 (2.9) | 96 (2.6) | 69 (3.2) | ||
| HCA/ Nursing associate/ trainee | 79 (3.9) | 140 (3.8) | 68 (3.2) | ||
| Student nurse/ midwife | 58 (2.8) | 122 (3.4) | 46 (2.1) | p<0.001 | |
| Caring responsibilities (mlogit) | F(4, 9.0e+07) = 2.99 | ||||
| Yes- sole carer | 223 (11.0) | 407 (11.2) | 205 (9.5) | ||
| Yes, but not sole carer | 774 (38.0) | 1270 (34.9) | 754 (34.9) | ||
| No | 1042 (51.1) | 1961 (53.9) | 1203 (55.7) | p = 0.018 | |
| WORKPLACE FACTORS† | |||||
| Health at risk due to clinical role (oreg) | F(1,15,516.5) = 31.77 | ||||
| Strongly disagree/disagree | 247 (12.1) | 568 (15.6) | |||
| Neither agree nor disagree | 279 (13.7) | 642 (17.6) | |||
| Strongly agree/agree | 1514 (74.2) | 2429 (66.8) | p<0.001 | ||
| Personal COVID-19 infection | – | ||||
| Yes - I had symptoms | 628 (29.0) | ||||
| Yes - did not have symptoms | 113 (5.2) | ||||
| No | 1421 (65.7) | – | |||
| Employed by NHS (lreg) | F(2, 2.3e+08) = 0.31 | ||||
| No | 470 (23.0) | 830 (22.8) | 512 (23.7) | ||
| Yes | 1570 (77.0) | 2808 (77.2) | 1650 (76.3) | p = 0.74 | |
| NHS pay banding (or equivalent) (mlogit) | F(2, 1.5e+06) = 14.39 | ||||
| Not banded | 38 (1.9) | 51 (1.4) | 20 (0.9) | ||
| HCA/ nursing associate | 103 (5.1) | 219 (6.0) | 99 (4.6) | ||
| Staff nurse | 567 (27.8) | 1106 (30.4) | 558 (25.8) | ||
| Senior staff nurse | 555 (27.2) | 1013 (27.9) | 620 (28.7) | ||
| Charge nurse | 446 (21.9) | 780 (21.5) | 547 (25.3) | ||
| Matron | 187 (9.1) | 281 (7.7) | 184 (8.5) | ||
| Senior nurse | 81 (4.0) | 100 (2.7) | 71 (3.3) | ||
| Very senior nurse | 64 (3.1) | 88 (2.4) | 62 (2.9) | p<0.001 | |
| Clinical speciality during pandemic (mlogit) | F(22, 1.4e+07) = 2.44 | ||||
| Acute/emergency hospital care | 547 (26.8) | 935 (25.7) | 511 (23.7) | ||
| Critical care/operating theatres | 324 (15.9) | 523 (14.4) | 338 (15.6) | ||
| Learning disabilities | 12 (0.6) | 26 (0.7) | 14 (0.7) | ||
| Mental health | 102 (5.0) | 253 (7.0) | 95 (4.4) | ||
| Midwifery/Paediatrics | 77 (3.8) | 129 (3.5) | 88 (4.1) | ||
| Palliative care | 49 (2.4) | 116 (3.2) | 64 (3.0) | ||
| Outpatients | 49 (2.4) | 98 (2.7) | 67 (3.1) | ||
| Care/nursing Home | 49 (2.4) | 119 (3.3) | 60 (2.8) | ||
| Community or primary care | 418 (20.5) | 742 (20.4) | 477 (22.1) | ||
| Education/ higher education | 41 (2.0) | 64 (1.8) | 46 (2.1) | ||
| Research | 79 (3.9) | 131 (3.6) | 123 (5.7) | ||
| Other | 292 (14.3) | 502 (13.8) | 276 (12.8) | p<0.001 | |
| Redeployment (mlogit) | F(4, 5.7e+06) = 7.17 | ||||
| Not redeployed | 1361 (66.8) | 2643 (72.7) | 1579 (73.1) | ||
| Redeployed - adequate training | 259 (12.7) | 368 (10.1) | 202 (9.4) | ||
| Redeployed - inadequate or no training | 419 (20.5) | 624 (17.2) | 380 (17.6) | p<0.001 | |
| Previously provided clinical care in pandemic (lreg) | F(2, 1.7e+07) = 1.92 | ||||
| Yes | 520 (25.5) | 963 (26.5) | 608 (28.1) | ||
| No | 1520 (74.5) | 2675 (73.5) | 1554 (71.9) | p = 0.15 | |
| Main role during the pandemic | – | ||||
| Direct clinical care | 1533 (70.9) | ||||
| Education | 78 (3.6) | ||||
| Research | 140 (6.5) | ||||
| Management/leadership | 236 (10.9) | ||||
| Unable to work | 63 (2.9) | ||||
| Other | 112 (5.2) | – | |||
| Correct PPE always available (oreg) | F(2, 1.1e+06) = 199.97 | ||||
| Strongly agree/agree | 795 (39.0) | 2192 (60.3) | 1468 (67.9) | ||
| Neither agree or disagree | 522 (25.6) | 782 (21.5) | 311 (14.4) | ||
| Disagree/strongly disagree | 724 (35.5) | 664 (18.3) | 384 (17.8) | p<0.001 | |
| Confidence in COVID-19 IPC training (mlogit) | F(2, 3.8e+06) = 72.76 | ||||
| Not confident at all/some not confident | 858 (42.1) | 1103 (30.3) | 532 (24.6) | ||
| Neither not confident nor confident | 346 (16.9) | 634 (17.4) | 295 (13.7) | ||
| Somewhat confident/very confident | 632 (31.0) | 1648 (45.3) | 1152 (53.3) | ||
| Not received training | 204 (10.0) | 254 (7.0) | 182 (8.4) | p<0.001 | |
| Prepared to provide care to COVID-19 patients (oreg) | F(2, 2.2e+06) = 75.79 | ||||
| Completely/somewhat unprepared | 1096 (53.7) | 1348 (37.1) | 916 (42.4) | ||
| Neither prepared nor unprepared | 237 (11.6) | 474 (13.0) | 292 (13.5) | ||
| Somewhat/very prepared | 707 (34.7) | 1816 (49.9) | 954 (44.1) | p<0.001 | |
| Care quality for non-COVID-19 (oreg) | F(2,57,974.0) = 35.09 | ||||
| Significantly/slightly worse than before | 1007 (49.3) | 1447 (39.8) | 1078 (49.9) | ||
| Same as before | 865 (42.4) | 1777 (48.8) | 867 (40.1) | ||
| Significantly/slightly better than before | 169 (8.3) | 414 (11.4) | 217 (10.1) | p<0.001 | |
| Mental health first aid training (lreg) | F(2, 5.9e+07) = 0.47 | ||||
| Yes | 396 (19.4) | 729 (20.0) | 446 (20.6) | ||
| No | 1644 (80.6) | 2909 (80.0) | 1716 (79.4) | p = 0.63 | |
HCA- healthcare assistant; IPC- infection prevention and control; PPE- personal protective equipment; RN- registered nurse.
All variables in table based on imputed dataset.
All variables collected at each of the three time-points except: ethnicity (not collected at time-point one); health at risk due to clinical role (not collected at time-point three); personal COVID-19 infection (not collected at time-points one/ two); main role during pandemic (not collected at time-points one/ two).
Statistical test obtained using: lreg = logistic regression, oreg = ordinal regression, mlogit = multinomial regression, PChi = Pearson Chi-squared.
†- The test statistic (where applicable) is shown adjacent to the variable name.
3.2. Personal and professional experiences of COVID-19
Across time-points, 28.7% (n = 2251) participants reported being redeployed in response to the pandemic (Table 1, table e3 supplementary material). Of these, 63.2% (n = 1422) reported that training to prepare for redeployment either did not occur or was inadequate.
Participants often (n = 3133, 40.0%) reported that they lacked confidence in infection prevention and control training, or that training had not been received, although this declined over time (T1 52.1%; T2 37.3%; T3 33.0%, p < 0.001). In total, 22.6% (n = 1772) disagreed or strongly disagreed that the correct personal protective equipment was always available, similarly this decreased across survey time-points (T1 35.5%; T2 18.3%; T3 17.8%, p < 0.001). Table 1 summarises these data across all time-points, with a breakdown by time-point included in the supplementary material.
At time-point three, 34.3% (n = 741) participants reported that they had experienced a COVID-19 infection. The clinical workplace was the most commonly identified source of infection (n = 477, 69.5%). Despite only 5.6% (n = 38) requiring hospital care, 35.2% (n = 241) reported that they had not fully recovered.
3.3. Primary outcome- Impact of events scale- -revised
An impact of events scale-revised score of 33 or above (probable post-traumatic stress disorder) was observed in 44.6% participants at time-point one, 37.1% participants at T2, and 29.3% participants at T3 (p < 0.001). The mean impact of events scale-revised score similarly decreased across time-points (T1 32.16, 95% CI 31.25–33.07; T2 28.11, 95% CI 27.43–28.79; T3 23.81, 95% CI 22.91–24.71, p < 0.001). Data are summarised in Table 2 and the supplementary material (table e4). Cronbach's α ranged from 0.89 to 0.94 across time-points and sub-scales (electronic supplement table e5).
Table 2.
Outcome data.
| T1 (n = 2040) | T2 (n = 3638) | T3 (n = 2162) | Test statistic/ p-value | ||
|---|---|---|---|---|---|
| Impact of events scale-revised | |||||
| Score cut-offs- n (%) | |||||
| ≥ 33 (probable PTSD) | 909(44.6) | 1350(37.1) | 634(29.3) | <0.001† | |
| ≥ 24 (PTSD clinical concern) | 1227 (60.2) | 1835 (50.4) | 897 (41.5) | <0.001† | |
| Total score- mean (95% CI) | 32.16 (31.25–33.07) |
28.11 (27.43–28.79) |
23.81 (22.91–24.71) |
F(2, 7521.1) = 81.95 p<0.001‡ | |
| DASS-21- n(%) | |||||
| Depression- severe/ extremely severe | 402 (19.7) | 727 (20.0) | 424 (19.6) | F(2,124,794.0) = 1.38, p = 0.25*,# | |
| Anxiety- severe/ extremely severe | 509 (25.0) | 792 (21.7) | 392 (18.1) | F(2,303,171.4) = 42.58, p<0.001*,# | |
| Stress- severe/ extremely severe | 421 (20.6) | 660 (18.1) | 379 (17.5) | F(2,223,990.2) = 9.30, p<0.001*, # | |
| Satisfaction with job- n(%) | |||||
| Very satisfied | 598 (29.3) | 991 (27.2) | 395 (18.3) | ||
| Somewhat satisfied | 819 (40.1) | 1475 (40.6) | 841 (38.9) | ||
| Average | 349 (17.1) | 667 (18.3) | 431 (19.9) | ||
| Somewhat unsatisfied | 176 (8.6) | 333 (9.2) | 323 (14.9) | ||
| Very unsatisfied | 98 (4.8) | 171 (4.7) | 172 (8.0) | F(2, 4.3e+07) = 68.10, p<0.001 | |
| Maslach burnout inventory- mean (95% CI) | |||||
| Emotional exhaustion | 26.48 (25.89–27.07) |
||||
| Depersonalization | 5.52 (5.27–5.78) |
||||
| Personal accomplishment | 34.64 (34.25–35.02) |
||||
| Level of intention to leave | |||||
| Current job- mean (95% CI) | 37.8 (36.3–39.4) | ||||
| Healthcare- mean (95% CI) | 28.6 (27.2–30.0) | ||||
*- p-value based on comparison across five categories: Normal; Mild; Moderate; Severe; Extremely severe.
CI- confidence interval; PTSD- post-traumatic stress disorder.
Statistical test obtained from † logistic regression model ‡ regression model # ordinal regression model.
3.4. Secondary outcomes
We observed decreases over time in the prevalence of severe and extremely severe anxiety and stress (e.g., severe/ extremely severe anxiety (T1 25.0%; T2 21.7%; T3 18.1%, p<0.001)). However, no changes were observed in prevalence of depression over time (T1 19.7%; T2 20.0%; 19.6%, p = 0.25). Job satisfaction declined across time-points with the lowest proportion reporting being very satisfied or somewhat satisfied with their job at T3 (T1 69.5%; T2 67.8%; 57.2%, p < 0.001). Cronbach's α ranged from 0.88 to 0.93 across time-points and sub-scales (electronic supplement table e5). There was a strong positive correlation between Depression Anxiety Stress scales- 21 sub-scales and impact of events scale-revised sub-scales across time-points (electronic supplement table e6).
At T3, mean scores for the Maslach Burnout Inventory scales of emotional exhaustion, depersonalization, and personal accomplishment were 26.48 (95% CI 25.89–27.07), 5.52
(95% CI 5.27–5.78), and 34.64 (95% CI 34.25–35.02) respectively. Cronbach's α ranged from 0.76 to 0.92 across sub-scales (electronic supplement table e5).The level of intention to leave was higher for an individual's current job (37.8, 95% CI 36.3–39.4) than it was for their intention to leave healthcare (28.6, 95% CI 27.2–30.0), although breakdown by response indicated polarised views with 26.1% having no plan to leave their current role, whilst 19.4% were giving high consideration to leaving with intermediate views having comparatively fewer responses (supplementary material (table e4).
3.5. Modelling of association between variables and probable post-traumatic stress disorder
In the multivariable logistic regression model (Table 3 ), factors were classified as personal (e.g., age, gender, caring responsibility) and workplace factors (e.g., clinical speciality, redeployment, personal protective equipment availability). For some factors, the low number of participants in a specific category means that our estimate of the association with the primary outcome is imprecise. Across time-points, we identified variability in the factors associated with our outcome of an impact of events scale-revised score of 33 or more.
Table 3.
Multivariable model of association between explanatory variables and probable PTSD.
|
T1 |
T2 |
T3 |
||||
|---|---|---|---|---|---|---|
| Odds ratio (95% CI) | P-value | Odds ratio (95% CI) | P-value | Odds ratio (95% CI) | P-value | |
| PERSONAL FACTORS | ||||||
| Gender | F(2, 1.7e+07) = 2.09, p = 0.12 | F(2, 1.9e+06) = 1.83, p = 0.16 | F(2,498,519.7)=1.38, p = 0.25 | |||
| Male (i) | 1.00 | 1.00 | 1.00 | |||
| Female | 1.41 (0.98–2.04) |
0.06 | 1.33 (0.99–1.77) |
0.056 | 0.75 (0.50–1.06) |
0.10 |
| Other/prefer not to say | 0.79 (0.21–2.96) |
0.73 | 1.29 (0.59–2.82) |
0.52 | 0.90 (0.21–3.79) |
0.88 |
| Age | F(4, 1.2e+06) = 6.91, p<0.001 | F(4, 2.2e+06) = 6.12, p<0.001 | F(4,67,237.7)=0.89, p = 0.47 | |||
| 16–30 (i) | 1.00 | 1.00 | 1.00 | |||
| 31–40 | 0.83 (0.58–1.20) |
0.33 | 0.89 (0.67–1.19) |
0.43 | 0.69 (0.43–1.09) |
0.11 |
| 41–50 | 0.60 (0.42–0.86) |
0.006 | 0.71 (0.53–0.93) |
0.015 | 0.75 (0.49–1.15 |
0.19 |
| 51–60 | 0.53 (0.37–0.75) |
<0.001 | 0.67 (0.51–0.88) |
0.004 | 0.74 (0.49–1.12) |
0.16 |
| 61 and over | 0.32 (0.19–0.53) |
<0.001 | 0.43 (0.29–0.63) |
<0.001 | 0.63 (0.38–1.06) |
0.083 |
| Ethnicity | F(3, 2,208,925.4) = 3.98, p = 0.008 | F(3,37,585.0)=0.24, p = 0.87 | ||||
| White (i) | 1.00 | 1.00 | ||||
| Mixed/Multiple ethnic | 1.36 (0.76–2.44) |
0.30 | 0.76 (0.35–1.65) |
0.48 | ||
| Asian/Asian British | 1.30 (0.86–1.96) |
0.21 | 1.07 (0.50–2.27) |
0.87 | ||
| Black/African/Caribbean | 1.72 (1.24–2.38) |
0.001 | 1.13 (0.64–1.98) |
0.68 | ||
| UK region | F(10, 998,003.8) = 1.41, p = 0.17 | F(10, 2.5e+06) = 1.34, p = 0.20 | F(10,146,571.6)=1.60, p = 0.099 | |||
| South East (i) | 1.00 | 1.00 | 1.00 | |||
| South West | 0.98 (0.67–1.44) |
0.91 | 0.92 (0.69–1.24) |
0.60 | 0.57 (0.37–0.87) |
0.010 |
| London | 1.28 (0.87–1.89) |
0.21 | 0.85 (0.64–1.12) |
0.24 | 0.89 (0.60–1.30) |
0.54 |
| East Midlands | 1.56 (1.06–2.31) |
0.025 | 0.80 (0.58–1.12) |
0.19 | 0.94 (0.61–1.46) |
0.78 |
| East of England | 1.02 (0.66–1.58 |
0.92 | 0.74 (0.53–1.03) |
0.077 | 0.99 (0.64–1.51) |
0.95 |
| North West | 0.88 (0.61- 1.26) |
0.48 | 0.98 (0.73–1.31) |
0.90 | 0.70 (0.46–1.08) |
0.11 |
| North East | 1.05 (0.67–1.66) |
0.82 | 0.91 (0.67–1.24) |
0.55 | 0.61 (0.40–0.94) |
0.024 |
| West Midlands | 1.39 (0.95–2.03 |
0.09 | 1.00 (0.73–1.37) |
0.99 | 0.88 (0.58–1.35) |
0.57 |
| Scotland | 1.07 (0.70–1.63 |
0.74 | 0.98 (0.72–1.33) |
0.90 | 0.72 (0.46–1.13) |
0.16 |
| Wales | 0.98 (0.58–1.66) |
0.94 | 0.58 (0.38–0.88) |
0.010 | 0.78 (0.47–1.31) |
0.35 |
| Northern Ireland | 1.72 (0.82–3.62) |
0.15 | 0.65 (0.40–1.07) |
0.09 | 1.66 (0.73–3.77) |
0.23 |
| Professional qualification | F(3, 27,417.4) = 2.12, p = 0.096 | F(3, 14,277.6) = 0.23, p = 0.87 | F(3,27,274.4)=0.29, p = 0.84 | |||
| RN-Adult nurse (i) | 1.00 | 1.00 | 1.00 | |||
| RN other/Midwives/HVs | 0.65 (0.45–0.94) |
0.023 | 1.07 (0.83–1.38) |
0.62 | 0.99 (0.67–1.48) |
0.98 |
| HCA/ nursing associate/ trainee | 0.36 (0.07–1.81) |
0.21 | 1.35 (0.42–4.27) |
0.61 | 0.47 (0.09–2.42) |
0.37 |
| Student nurse/ midwife | 0.43 (0.09–1.99) |
0.28 | 1.50 (0.46–4.88) |
0.50 | 0.59 (0.12–2.93) |
0.52 |
| Caring responsibilities | F(2, 301,685.9) = 3.84, p = 0.021 | F(2, 746,013.4) = 1.58, p = 0.21 | F(2,23,277.6)=3.97, p = 0.019 | |||
| Yes-sole carer | 1.51 (1.08–2.09) |
0.015 | 1.25 (0.98–1.59) |
0.076 | 1.58 (1.11–2.25) |
0.012 |
| Yes‑but not sole carer | 1.26 (1.01–1.58) |
0.041 | 1.05 (0.88–1.24) |
0.60 | 1.26 (0.99–1.59) |
0.056 |
| No (i) | 1.00 | 1.00 | 1.00 | |||
| WORKPLACE FACTORS | ||||||
| Health at risk due to clinical role | F(2, 10,572.7) = 5.91, p = 0.003 | F(2, 7886.3) = 16.10, p<0.001 | ||||
| Strongly disagree/disagree | 1.29 (0.86–1.96) |
0.22 | 1.34 (1.01–1.79) |
0.040 | ||
| Neither agree/ disagree (i) | 1.00 | 1.00 | ||||
| Strongly agree/agree | 1.68 (1.22–2.32) |
0.001 | 1.84 (1.47–2.31) |
<0.001 | ||
| Personal COVID-19 infection | F(2,2434.4)=7.55, p<0.001 | |||||
| Yes – symptomatic | 1.58 (1.25–2.00) |
<0.001 | ||||
| Yes- asymptomatic | 1.40 (0.87–2.25) |
0.17 | ||||
| No (i) | 1.00 | |||||
| Employed by NHS† | 1.37 (1.03–1.80) |
0.028 | 1.16 (0.94–1.42) |
0.17 | 0.89 (0.67–1.18) |
0.40 |
| NHS banding (or equivalent) | F(7, 108,131.0) = 1.32, p = 0.24 | F(7,,103,269.3) = 1.01, p = 0.42 | F(7,75,401.2)=1.28, p = 0.25 | |||
| Not banded | 2.78 (0.57–13.65) |
0.21 | 0.65 (0.19–2.23) |
0.49 | 0.57 (0.10–3.35) |
0.54 |
| HCA/ nursing associate | 2.80 (0.59–13.39) |
0.20 | 0.89 (0.29–2.75) |
0.84 | 1.60 (0.34–7.60) |
0.56 |
| Staff nurse (i) | 1.00 | 1.00 | 1.00 | |||
| Senior staff nurse | 0.88 (0.67–1.15) |
0.35 | 1.01 (0.83–1.22) |
0.95 | 0.91 (0.69–1.20) |
0.50 |
| Charge nurse | 0.73 (0.54–0.98) |
0.038 | 0.89 (0.72–1.11) |
0.31 | 0.75 (0.56–1.02) |
0.067 |
| Matron | 0.70 (0.47–1.05) |
0.087 | 0.72 (0.52–1.00) |
0.053 | 0.71 (0.46–1.09) |
0.12 |
| Senior nurse | 0.60 (0.34–1.06) |
0.078 | 0.93 (0.56–1.54) |
0.78 | 0.57 (0.29–1.14) |
0.11 |
| Very senior nurse | 0.71 (0.36–1.39) |
0.32 | 0.65 (0.36–1.17) |
0.15 | 0.57 (0.27–1.19) |
0.13 |
| Clinical speciality* | F(11, 586,562.0) = 1.31, p = 0.021 | F(11, 765,173.0) = 4.67, p<0.001 | F(11, 147,539.3)=1.70, p = 0.066 | |||
| Acute/emergency hospital care(i) | 1.00 | 1.00 | 1.00 | |||
| Critical care/operating theatres | 1.14 (0.79–1.64) |
0.50 | 1.51 (1.18–1.92) |
0.001 | 1.31 (0.94–1.82) |
0.11 |
| Learning disabilities | 0.83 (0.20–3.43) |
0.79 | 0.54 (0.20–1.41) |
0.21 | 0.67 (0.16–2.85) |
0.59 |
| Mental health | 0.78 (0.43–1.40) |
0.41 | 0.71 (0.48–1.04) |
0.075 | 0.85 (0.45–1.60) |
0.61 |
| Midwifery/Paediatrics | 0.76 (0.40–1.44) |
0.40 | 0.62 (0.39–1.01) |
0.056 | 0.47 (0.22–0.99) |
0.047 |
| Palliative care | 0.98 (0.48–2.01) |
0.95 | 1.02 (0.64–1.61) |
0.95 | 1.18 (0.62–2.22) |
0.61 |
| Outpatients | 0.85 (0.54–1.36) |
0.50 | 0.73 (0.45–1.18) |
0.20 | 0.78 (0.39–1.53) |
0.47 |
| Care/nursing Home | 1.12 (0.57–2.22) |
0.74 | 1.64 (1.03–2.60) |
0.036 | 1.39 (0.72–2.69) |
0.33 |
| Community or primary care | 0.93 (0.68–1.27) |
0.65 | 0.72 (0.57–0.91) |
0.006 | 0.73 (0.52–1.02) |
0.065 |
| Education/ higher education | 1.27 (0.69–2.32) |
0.45 | 0.82 (0.42–1.57) |
0.54 | 0.58 (0.26–1.31) |
0.19 |
| Research | 0.48 (0.30–0.76) |
0.002 | 0.71 (0.46–1.09) |
0.12 | 0.73 (0.43–1.23) |
0.23 |
| Other | 0.90 (0.65–1.26) |
0.55 | 0.70 (0.54–0.90) |
0.006 | 0.90 (0.62–1.30) |
0.57 |
| Redeployment | F(2, 379,222.6) = 4.09, p = 0.017 | F(2, 3.1e+06) = 7.76, p<0.001 | F(2,26,653.7)=1.25, p = 0.29 | |||
| Not redeployed (i) | 1.00 | 1.00 | 1.00 | |||
| Redeployed -adequate training | 0.85 (0.62–1.16) |
0.31 | 1.01 (0.78–1.31) |
0.93 | 0.84 (0.56–1.25) |
0.39 |
| Redeployed-inadequate/ no training | 1.37 (1.06–1.77) |
0.017 | 1.50 (1.22–1.84) |
<0.001 | 1.17 (0.89–1.55) |
0.26 |
| Previously provided clinical care in pandemic† | 1.10 (0.87–1.39) |
0.43 | 1.19 (1.00–1.41) |
0.047 | 1.44 (1.14–1.82) |
0.002 |
| Correct PPE always available | F(2, 148,518.3) = 6.84, p = 0.001 | F(2, 327,800.1) = 10.54, p<0.001 | F(2,38,969.5)=7.42, p<0.001 | |||
| Strongly agree/agree | 0.97 (0.74–1.28) |
0.84 | 0.82 (0.67–1.00) |
0.048 | 0.74 (0.54–1.01) |
0.056 |
| Neither agree/ disagree (i) | 1.00 | 1.00 | 1.00 | |||
| Disagree/strongly disagree | 1.49 (1.15–1.93) |
<0.001 | 1.34 (1.07–1.69) |
0.012 | 1.26 (0.88–1.80) |
0.20 |
| Confidence in COVID-19 IPC training | F(3, 264,019.8) = 3.98, p = 0.008 | F(3, 1.1e+06) = 11.45, p<0.001 | F(3,63,431.9)=3.35, p = 0.018 | |||
| Not confident at all/somewhat not confident | 1.48 (1.11–1.97) |
0.007 | 1.29 (1.03–1.61) |
0.024 | 1.51 (1.07–2.13) |
0.020 |
| Neither not confident/ confident (i) | 1.00 | 1.00 | 1.00 | |||
| Somewhat/ very confident | 0.96 (0.70–1.32) |
0.81 | 0.72 (0.57–0.90) |
0.004 | 1.09 (0.78–1.52) |
0.63 |
| Not received training | 1.23 (0.83–1.82) |
0.30 | 0.84 (0.60–1.17) |
0.30 | 1.65 (1.07–2.53) |
0.023 |
| Prepared to provide care to COVID-19 patients | F(2, 701,907.5) = 8.03, p<0.001 | F(2, 147,563.2) = 13.47, p<0.001 | F(2,21,028.1)=19.80, p<0.001 | |||
| Completely/somewhat unprepared | 1.60 (1.16–2.22) |
0.005 | 1.25 (0.98–1.59) |
0.066 | 1.32 (0.95–1.84) |
0.096 |
| Neither unprepared/ prepared (i) | 1.00 | 1.00 | 1.00 | |||
| Somewhat/very prepared | 1.01 (0.70–1.44) |
0.96 | 0.75 (0.59–0.96) |
0.024 | 0.56 (0.40–0.80) |
0.001 |
| Care quality for non-COVID-19 patients | F(2, 16,636.2) = 7.11, p<0.001 | F(2, 82,544.4) = 0.95, p = 0.39 | F(2,29,086.9)=3.37, p = 0.034 | |||
| Significantly/slightly worse | 1.47 (1.19–1.82) |
<0.001 | 1.12 (0.95–1.32) |
0.17 | 1.34 (1.07–1.69) |
0.012 |
| Same as before (i) | 1.00 | 1.00 | 1.00 | |||
| Significantly/slightly better | 0.98 (0.67–1.42) |
0.91 | 1.02 (0.79–1.31) |
0.88 | 1.30 (0.90–1.89) |
0.16 |
| Mental health first aid training† | 0.86 (0.66–1.12) |
0.26 | 0.87 (0.71–1.07) |
0.19 | 0.73 (0.54–0.97) |
0.031 |
| Psuedo R2 | 0.11 | 0.11 | 0.13 | |||
| C-Statistic (AUC) | 0.72 | 0.72 | 0.74 | |||
Note: the p-value for the overall effect of variables with three or more categories is shown in brackets in each row containing the variable name.
i- Index category. Where index category is not specified, the index category is a negative response.
† yes, compared with no.
*- Clinical speciality on 1st February 2020 used for time-point one; Clinical speciality during pandemic used for time-points two and three.
AUC- Area Under Curve; CI- confidence interval; IPC- Infection prevention and control; HCA- Healthcare assistant; HV- Health visitor; NHS- National health service; PPE- personal protective equipment; RN- Registered nurse.
3.6. Modelling- personal factors
For personal factors, compared with those aged 16–30, older participants were less likely to have an impact of events scale-revised score of 33 or more, although this was not statistically significant at T3 (e.g., age 51–60 T1 OR 0.53, 95% CI 0.37 – 0.75; T2 OR 0.67 95% CI 0.51 – 0.88; T3 OR 0.63 95% CI 0.38 – 1.06). Compared with white ethnicity, being of Black/ African/ Caribbean ethnicity was associated with impact of events scale-revised score of 33 or more at T2 (OR 1.72, 95% CI 1.24–2.38), but this association was not observed at T3 or for other ethnicities. A sole caring responsibility was associated with impact of events scale-revised score of 33 or more at T1 (OR 1.51, 95% CI 1.08–2.09) and T3 (OR 1.58, 95% CI 1.11–1.25), but not at T2 (OR 1.25, 95% CI 0.98–1.59). We did not find evidence of a clear association between gender, geographical region and professional qualification, and our outcome.
3.7. Modelling- workplace factors
For workplace factors, being employed by the NHS was associated with impact of events scale-revised score of 33 or more at T1 (OR 1.37, 95% CI 1.03–1.80), but not at subsequent time-points. Clinical speciality was not consistently associated with an impact of events scale-revised score of 33 or more, although at T2 working in critical/ operating theatres (OR 1.51, 95% CI 1.18–1.92) and working in a care/ nursing home (OR 1.64, 95% CI 1.03–2.60), compared with acute/ emergency hospital care, was associated with increased odds of impact of events scale-revised score of 33 or more.
Whilst redeployment with adequate training was not associated with impact of events scale-revised score of 33 or more, we identified an association between redeployment without training or inadequate training and impact of events scale-revised score of 33 or more at both T1 and T2 (e.g., T2 OR 1.50, 95% CI 1.22–1.84), but not at T3 (OR 1.17, 95% CI 0.89–1.55). A similar pattern was observed in relation to participants who disagreed or strongly disagreed that the correct personal protective equipment was always available (e.g., T2 OR 1.34, 95% CI 1.07–1.69; T3 OR 1.23, 95% CI 0.86–1.77). The only explanatory variable response associated with impact of events scale-revised score of 33 or more at all three time-points was being not (or somewhat not) confident in COVID-19 infection prevention and control training (T1 OR 1.48, 95% CI 1.11–1.97; T2 OR 1.29, 95% CI 1.03–1.61; T3 1.55, 95% CI 1.09–2.19). At T3, symptomatic COVID-19 infection was associated with impact of events scale-revised score of 33 or more (OR 1.56, 95% CI 1.23–1.98).
3.8. Modelling - participants pattern of response
For the outcomes of impact of impact of events scale-revised score of 33 or more and Depression Anxiety Stress scales- 21, results were broadly consistent with our primary analysis and across all response patterns (electronic supplement table e7 and table e8). The inclusion of a pattern of response variable in the multivariable models made little difference to the parameter estimates of other variables (electronic supplement Table e9).
4. Discussion
In this large national longitudinal survey study over the course of the first wave of the COVID-19 pandemic, we found that the UK nursing and midwifery workforce experienced a high prevalence of negative psychological effects, including severe stress, severe anxiety and high impact of events scale-revised scores, indicative of probable post-traumatic stress disorder. Prevalence of some psychological issues decreased following the first pandemic peak, but a significant proportion of participants continued to experience negative psychological effects during the pandemic recovery phase. Factors associated with an impact of events scale-revised score of 33 or more, indicative of probable post-traumatic stress disorder, varied across time-points. Personal factors including younger age and caring responsibilities were associated with increased distress, as were workplace factors such as availability of personal protective equipment and delivery of essential training. Workplace factors are potentially modifiable. Our results provide important information to support identification of at-risk staff and inform workforce support planning for future pandemics.
Our methodology and survey design drew on that developed for the COVID-19 Emergency Response Assessment study, which surveyed emergency medicine, intensive care, and anaesthetic doctors during the pandemic acceleration phase, peak phase, and one-month following the peak (Roberts et al., 2020, Roberts et al., 2021b). Collecting data across three time-points allowed us to explore changes in key psychological measures over the course the first wave of the pandemic, and into the recovery period. This contrasts with the majority of other studies of mental health in the context of a pandemic that have surveyed healthcare workers at only one single time-point, often with a focus on hospital-based healthcare staff (Ali et al., 2020; Chew et al., 2020, Dykes et al., 2021, Lai et al., 2020, Nickell et al., 2004, Wu et al., 2009, Zhu et al., 2020). Whilst such studies provide some helpful information about the impact of the pandemic, follow-up assessments are needed to understand the potential ongoing impact. A further limitation of many previous studies in this area is their focus on the hospital-based workforce, thereby missing the impact on those working in other areas, such as primary care and care homes.
As our experience shows, undertaking research in the context of a global pandemic, is challenging, particularly in mapping survey distribution to the unpredictable impact of the pandemic on society and the healthcare system. Despite rapidly developing the study protocol and survey tool, and expedited ethical review, our T1 survey coincided with the rapid increase in COVID-19 hospitalised cases in the UK and crossed the date on which the number of COVID-19 hospitalised patients peaked during the first wave (UK Government, 2021). This may, in part, explain the apparent improvement in wellbeing between T1 and T2, as individuals became more normalised to healthcare delivery in a pandemic, organisations began to improve their response (e.g., through improved availability of personal protective equipment) and overall healthcare system demand began to decline.
In our study, we reported a prevalence of probable post-traumatic stress disorder, based on an impact of events scale-revised score of 33 or more, of 45%, 37%, and 29% at T1, T2, and T3 respectively. As such, our observed rate was higher than that reported in many studies prior to the COVID-19 pandemic (Kinman et al., 2020). We identified similar patterns for the outcomes of stress and anxiety, whilst prevalence of depression did not change across survey time-points. Maslach burnout inventory scores indicated moderately high levels of emotional exhaustion, that exceeded population norms, and levels of depersonalisation and personal accomplishment that are in line with population norms (Maslach et al., 2018). Intention to leave showed polarised views with some individuals expressing a clear desire to leave both their current role and healthcare. There are likely important and complex relationships between these outcomes, such that the long-term trajectory of these conditions remains unclear.
Recent studies of post-traumatic stress disorder prevalence, which also used the impact of events scale-revised score and similar cut-off values, in healthcare workers in the context of COVID-19 have reported rates ranging from 12.6 to 29.8% during the pandemic peak (Dykes et al., 2021, Roberts et al., 2021a, Zhu et al., 2020). These data are consistent with a systematic review of 19 studies from both the COVID-19 pandemic and previous pandemics that reported a pooled prevalence of clinically important post-traumatic stress symptoms in healthcare workers in the acute pandemic phase of 23.4% (95% CI 16.3–31.2%), although heterogeneity was high (I2 = 96.2%) and seemingly driven by differences in population, the nature of the pandemic, and method of measuring post-traumatic stress (Allan et al., 2020).
The reason for the markedly higher prevalence of probable post-traumatic stress disorder in our study, compared with previous studies, is unclear. Previous studies have reported that post-traumatic stress disorder is more common in members of the nursing and midwifery workforce than other healthcare professions, although this finding is not consistent across all studies (Allan et al., 2020; Cabarkapa et al., 2020; Stuijfzand et al., 2020). Our study identified a variety of factors associated with probable post-traumatic stress disorder, and these factors changed across time-points. Key factors were linked to the organisational response to the pandemic (e.g., availability of personal protective equipment and training adequacy) highlighting the important role of employers in mitigating the impact of the pandemic on psychological wellbeing in the workforce. These factors may, in part, reflect the risk of contracting COVID-19 or the perceived health impact if the individual became infected. The factors identified are broadly consistent with those reported in a recent systematic review of 59 studies from a range of countries across four continents and a range of previous pandemics (Kisely et al., 2020). This supports the potential generalisability of our findings beyond the UK setting. However, some differences were noted. For example, we found that redeployment with adequate training was not associated with probable post-traumatic stress disorder, but an association was identified where redeployment occurred with inadequate or no training. This indicates the importance of planning adequate workforce preparation for future pandemics.
The observed decrease in negative psychological effects over the study period is consistent with previous studies with a longer follow-up period, although these same studies highlight that an important proportion of individuals will experience ongoing psychological effects (Allan et al., 2020; McAlonan et al., 2007; Stuijfzand et al., 2020; Wu et al., 2009). This has the potential to increase levels of sickness and staff attrition, and negatively affect patient safety (Dyrbye et al., 2019; Hall et al., 2016; Jun et al., 2021; Kinman et al., 2020). A further concern is that at T3, one-third reported having had a COVID-19 infection, of whom 35.2% reported that they had not yet fully recovered. Long-COVID is increasingly being recognised as an important health condition, with both physical and psychological effects (Greenhalgh et al., 2020; Taquet et al., 2021). As such, some individuals may require significant support to return to their previous work role, to avoid their potential loss to the health and social care workforce.
The key strength of our study is its large sample size with participants from all members of the nursing and midwifery workforce in a country that has been heavily impacted by COVID-19 (Bilinski and Emanuel, 2020; UK Government, 2021). In contrast to previous research, we chose not to limit our sample to a specific clinical area or specific members of the nursing and midwifery workforce (e.g. only registered nurses), thereby allowing us to produce findings that are relevant to the whole workforce.
Our study does, however, have some important limitations. Firstly, whilst we collected nearly 8000 eligible survey responses across the three time-points, or sample was self-selecting and represented a relatively small proportion of the UK's total nursing and midwifery workforce. There are around 400,000 members of the nursing and midwifery workforce directly employed by the NHS in England, but these data do not include the number of individuals working in other UK countries, or those not employed by the NHS, such as those working in social care (NHS Digital, 2018). As such, it is not possible to estimate our survey response rate. Recent data from the Nursing and Midwifery Council indicates that there 731,918 individuals on the professional register, although not of all of these individuals will be currently working and these data exclude the many non-registered members of the workforce, such as healthcare assistants (Nursing and Midwifery Council, 2021). The proportion of nursing and midwifery registrants identifying as female (89%) is similar to our sample (91.6%), whilst the proportion of non-white individuals is markedly higher (21.7%) than our sample (9.3%). We also observed low numbers of responses from healthcare assistants, who will typically receive lower salaries, despite our attempts to specifically target both non-registered individuals and Black, Asian and minority ethnicgroups through social media at T2 and T3. Given the significant negative impact of COVID-19 on these groups, we may have underestimated the true psychological impact on the total workforce (Ferrando-Vivas et al., 2021; Williamson et al., 2020). Secondly, we observed some differences in baseline characteristics across surveys. Whilst our modelling adjusted for known confounders, our findings across surveys may have been influenced by unmeasured confounders. Thirdly, our data linkage has some limitations. We allowed individuals to choose whether they supplied an email address and how we used their data (including permission to link data across surveys). In addition, at T2 and T3, we did not require participants to have completed one of the preceding surveys. As such, for analysis purposes, we decided to treat the three surveys as independent samples. However, where we explored the impact of pattern of response in sensitivity analyses, we found that findings were consistent with our primary analysis. Fourthly, we developed our survey rapidly and we sought to develop a tool that could be completed in 15–20 min. In developing our survey, we drew on the wider literature and expert knowledge to identify and prioritise questions, but it is possible that we may have missed additional factors associated with psychological wellbeing. Fifthly, whilst we used validated tools to assess psychological impacts, these tools cannot be used for the diagnosis of psychological conditions, but they may help identify individuals that may be at risk and benefit from further assessment and support. In particular, our definition of probable post-traumatic stress disorder did not fulfil all the necessary criteria (e.g., persistence of symptoms for over one-month and evidence of functional impairment) for a clinical diagnosis (Lancaster et al., 2016). Finally, our survey focussed on the first wave of the peak, such that the enduring impact of subsequent pandemic waves on psychological wellbeing is yet to be determined.
5. Conclusion
In this survey study, we observed a concerning prevalence of post-traumatic stress disorder, stress, and anxiety in members of the UK nursing and midwifery workforce during the first wave of the COVID-19 pandemic. Although prevalence decreased over time, even 3-months after the first surge, almost three in ten participants reported probable post-traumatic stress disorder. Our findings showed that both personal and workplace factors were associated with probable post-traumatic stress disorder, and may have acted as triggers. Key similarities with previous studies highlight the global relevance of our study findings.
Our findings should drive healthcare employers throughout the world to address shortcomings in their organisational response to COVID-19, and future health emergencies, to both prevent psychological issues developing and ensure that those affected receive timely high-quality evidence-based support during the pandemic and as needed thereafter.
CRediT authorship contribution statement
Keith Couper: Conceptualization, Methodology, Investigation, Writing – original draft, Writing – review & editing, Supervision, Project administration. Trevor Murrells: Conceptualization, Methodology, Formal analysis, Investigation, Writing – review & editing. Julie Sanders: Conceptualization, Methodology, Writing – review & editing, Funding acquisition. Janet E. Anderson: Conceptualization, Methodology, Investigation, Writing – review & editing. Holly Blake: Conceptualization, Methodology, Investigation, Writing – review & editing. Daniel Kelly: Conceptualization, Methodology, Investigation, Writing – review & editing. Bridie Kent: Conceptualization, Methodology, Investigation, Writing – review & editing. Jill Maben: Conceptualization, Methodology, Investigation, Writing – review & editing. Anne Marie Rafferty: Conceptualization, Methodology, Investigation, Writing – review & editing. Rachel M. Taylor: Conceptualization, Methodology, Investigation, Writing – review & editing. Ruth Harris: Conceptualization, Methodology, Investigation, Writing – review & editing.
Declaration of Competing Interest
None.
Acknowledgments
Funding
This work was supported by funding from The Burdett Trust for Nursing. The Burdett Trust for Nursing had no role in the design of the study, data collection, data analysis and interpretation, writing of the manuscript, or decision to publish.
RMT is a National Institute for Health Research (NIHR) Senior Nurse Research Leader, and receives funding through the NIHR PGfAR, HS&DR and UCLH Charity.
The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Acknowledgments
We are grateful to the Royal College of Nursing, Nursing and Midwifery Council, Council of Deans for Health, Florence Nightingale Foundation, Cavell Nurses’ Trust and all other individuals and organisations that supported survey dissemination.
We acknowledge the CERA (COVID-19 emergency response assessment) study team whose survey design informed our study.
Data availability
The datasets generated during and/or analysed during the current study may be made available by the corresponding author on reasonable request.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ijnurstu.2021.104155.
Appendix. Supplementary materials
References
- Aiken L.H., Sermeus W., Van den Heede K., Sloane D.M., Busse R., McKee M., Bruyneel L., Rafferty A.M., Griffiths P., Moreno-Casbas M.T., Tishelman C., Scott A., Brzostek T., Kinnunen J., Schwendimann R., Heinen M., Zikos D., Sjetne I.S., Smith H.L., Kutney-Lee A. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. 2012;344:e1717. doi: 10.1136/bmj.e1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali S., Maguire S., Marks E., Doyle M., Sheehy C. Psychological impact of the COVID-19 pandemic on healthcare workers at acute hospital settings in the South-East of Ireland: an observational cohort multicentre study. BMJ Open. 2020;10(12) doi: 10.1136/bmjopen-2020-042930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allan S.M., Bealey R., Birch J., Cushing T., Parke S., Sergi G., Bloomfield M., Meiser-Stedman R. The prevalence of common and stress-related mental health disorders in healthcare workers based in pandemic-affected hospitals: a rapid systematic review and meta-analysis. Eur. J. Psychotraumatol. 2020;11(1) doi: 10.1080/20008198.2020.1810903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antony M.M., Bieling P.J., Cox B.J., Enns M.W., Swinson R.P. Psychometric properties of the 42-item and 21-item versions of the depression anxiety stress scales in clinical groups and a community sample. Psychol. Assess. 1998;10(2):176–181. [Google Scholar]
- Bandyopadhyay S., Baticulon R.E., Kadhum M., Alser M., Ojuka D.K., Badereddin Y., Kamath A., Parepalli S.A., Brown G., Iharchane S., Gandino S., Markovic-Obiago Z., Scott S., Manirambona E., Machhada A., Aggarwal A., Benazaize L., Ibrahim M., Kim D., Tol I., Taylor E.H., Knighton A., Bbaale D., Jasim D., Alghoul H., Reddy H., Abuelgasim H., Saini K., Sigler A., Abuelgasim L., Moran-Romero M., Kumarendran M., Jamie N.A., Ali O., Sudarshan R., Dean R., Kisyova R., Kelzang S., Roche S., Ahsan T., Mohamed Y., Dube A.M., Gwini G.P., Gwokyala R., Brown R., Papon M.R.K.K., Li Z., Ruzats S.S., Charuvila S., Peter N., Khalidy K., Moyo N., Alser O., Solano A., Robles-Perez E., Tariq A., Gaddah M., Kolovos S., Muchemwa F.C., Saleh A., Gosman A., Pinedo-Villanueva R., Jani A., Khundkar R. Infection and mortality of healthcare workers worldwide from COVID-19: a systematic review. BMJ Global Health. 2020;5(12) doi: 10.1136/bmjgh-2020-003097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BBC News, 2020. Coronavirus: nurses' leaders urge 'care for those who caring'. [Available from: https://www.bbc.co.uk/news/health-53101331, accessed 8/02/2021]
- Bilinski A., Emanuel E.J. COVID-19 and excess all-cause mortality in the US and 18 comparison countries. JAMA. 2020;324(20):2100–2102. doi: 10.1001/jama.2020.20717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabarkapa S., Nadjidai S.E., Murgier J., Ng C.H. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: a rapid systematic review. Brain, Behav. Immun. - Health. 2020;8 doi: 10.1016/j.bbih.2020.100144. -100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y.-.C., Guo Y.-L.L., Chin W.-.S., Cheng N.-.Y., Ho J.-.J., Shiao J.S.-C. Patient-nurse ratio is related to nurses' intention to leave their job through mediating factors of burnout and job dissatisfaction. Int. J. Environ. Res. Public Health. 2019;16(23):4801. doi: 10.3390/ijerph16234801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew N.W.S., Lee G.K.H., Tan B.Y.Q., Jing M., Goh Y., Ngiam N.J.H., Yeo L.L.L., Ahmad A., Ahmed Khan F., Napolean Shanmugam G., Sharma A.K., Komalkumar R.N., Meenakshi P.V., Shah K., Patel B., Chan B.P.L., Sunny S., Chandra B., Ong J.J.Y., Paliwal P.R., Wong L.Y.H., Sagayanathan R., Chen J.T., Ying Ng A.Y., Teoh H.L., Tsivgoulis G., Ho C.S., Ho R.C., Sharma V.K. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou R., Dana T., Buckley D.I., Selph S., Fu R., Totten A.M. Epidemiology of and risk factors for coronavirus infection in health care workers: a living rapid review. Ann. Intern. Med. 2020;173(2):120–136. doi: 10.7326/M20-1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creamer M., Bell R., Failla S. Psychometric properties of the impact of event scale—revised. Behav. Res. Ther. 2003;41(12):1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- De Kock J.H., Latham H.A., Leslie S.J., Grindle M., Munoz S.-.A., Ellis L., Polson R., O'Malley C.M. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health. 2021;21(1):104. doi: 10.1186/s12889-020-10070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas M., Katikireddi S.V., Taulbut M., McKee M., McCartney G. Mitigating the wider health effects of covid-19 pandemic response. BMJ. 2020;369:m1557. doi: 10.1136/bmj.m1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dykes N., Johnson O., Bamford P. Assessing the psychological impact of COVID-19 on intensive care workers: a single-centre cross-sectional UK-based study. J. Intens. Care Soc. 2021 doi: 10.1177/1751143720983182. Epub ahead of print January 5, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyrbye L.N., Shanafelt T.D., Johnson P.O., Johnson L.A., Satele D., West C.P. A cross-sectional study exploring the relationship between burnout, absenteeism, and job performance among American nurses. BMC Nurs. 2019;18(1):57. doi: 10.1186/s12912-019-0382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-Surveys (CHERRIES) J. Med. Internet Res. 2004;6(3):e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez R., Lord H., Halcomb E., Moxham L., Middleton R., Alananzeh I., Ellwood L. Implications for COVID-19: a systematic review of nurses’ experiences of working in acute care hospital settings during a respiratory pandemic. Int. J. Nurs. Stud. 2020;111 doi: 10.1016/j.ijnurstu.2020.103637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrando-Vivas P., Doidge J., Thomas K., Gould D.W., Mouncey P., Shankar-Hari M., Young J.D., Rowan K.M., Harrison D.A., on behalf of the, I.C.-T. Prognostic factors for 30-day mortality in critically ill patients with coronavirus disease 2019: an observational cohort study. Crit. Care Med. 2021;49(1) doi: 10.1097/CCM.0000000000004740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh T., Knight M., A'Court C., Buxton M., Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020;370:m3026. doi: 10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- Hackett, K., 2020. Nursing Standard: COVID-19: redeployment training is non-existent or inadequate, nurses reveal. [Available from: https://rcni.com/nursing-standard/newsroom/news/covid-19-redeployment-training-non-existent-or-inadequate-nurses-reveal-160301 accessed 8/2/21]
- Hall L.H., Johnson J., Watt I., Tsipa A., O'Connor D.B. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS ONE. 2016;11(7) doi: 10.1371/journal.pone.0159015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jun J., Ojemeni M.M., Kalamani R., Tong J., Crecelius M.L. Relationship between nurse burnout, patient and organizational outcomes: systematic review. Int. J. Nurs. Stud. 2021;119 doi: 10.1016/j.ijnurstu.2021.103933. [DOI] [PubMed] [Google Scholar]
- Kinman, G., Teoh, K., Harriss, A., 2020. The Mental Health and Wellbeing of Nurses and Midwives in the United Kingdom. [Available from: https://www.som.org.uk/sites/som.org.uk/files/The_Mental_Health_and_Wellbeing_of_Nurses_and_Midwives_in_the_United_Kingdom.pdf, accessed 19/04/2021] [DOI] [PubMed]
- Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. -e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancaster C.L., Teeters J.B., Gros D.F., Back S.E. Posttraumatic stress disorder: overview of evidence-based assessment and treatment. J. Clin. Med. 2016;5(11):105. doi: 10.3390/jcm5110105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q., Luo D., Haase J.E., Guo Q., Wang X.Q., Liu S., Xia L., Liu Z., Yang J., Yang B.X. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. The Lancet Global Health. 2020;8(6):e790–e798. doi: 10.1016/S2214-109X(20)30204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond S.H., Lovibond P.F. Manual for the depression anxiety stress scales. Psychol. Found. Australia, Sydney. 1996 [Google Scholar]
- Maben J., Bridges J. Covid-19: supporting nurses' psychological and mental health. J Clin Nurs. 2020;29(15–16):2742–2750. doi: 10.1111/jocn.15307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning J.C., Bramley L., Coad J., Evans C., Evans K., Tinkler L., Cooper J. Priorities for research during the Coronavirus SARS-CoV-2 (COVID-19) pandemic and beyond: a survey of nurses, midwives and health visitors in the United Kingdom. J. Res.Nurs. 2021;26(5):442–454. doi: 10.1177/17449871211018737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslach C., Jackson S.E., Leiter M.P. Mind Garden; Menlo Park, CA: 2018. Maslach Burnout Inventory Manual. [Google Scholar]
- McAlonan G.M., Lee A.M., Cheung V., Cheung C., Tsang K.W., Sham P.C., Chua S.E., Wong J.G. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can. J. Psychiatry. 2007;52(4):241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- Mitchell, G., 2020. Nursing Times: nurses asked to share experiences of Covid-19 peak for major study. [Available from: https://www.nursingtimes.net/news/workforce/nurses-asked-to-share-experiences-of-covid-19-peak-for-major-study-29-04-2020/accessed 24/03/21].
- Mutambudzi M., Niedwiedz C., Macdonald E.B., Leyland A., Mair F., Anderson J., Celis-Morales C., Cleland J., Forbes J., Gill J., Hastie C., Ho F., Jani B., Mackay D.F., Nicholl B., O'Donnell C., Sattar N., Welsh P., Pell J.P., Katikireddi S.V., Demou E. Occupation and risk of severe COVID-19: prospective cohort study of 120 075 UK Biobank participants. Occupation. Environ. Med. Oemed-2020-106731. 2020 doi: 10.1136/oemed-2020-106731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Audit Office . 2020. The NHS Nursing Workforce.https://www.nao.org.uk/wp-content/uploads/2020/03/The-NHS-nursing-workforce.pdf [Available from: [9/02/2021]. Available from. accessed 9/02/21] [Google Scholar]
- National Health Service, 2019. The NHS Long Term Plan. [Available from: https://www.longtermplan.nhs.uk/wp-content/uploads/2019/01/nhs-long-term-plan.pdf accessed 31/01/2019].
- Navaratnam A.V., Gray W.K., Day J., Wendon J., Briggs T.W.R. Patient factors and temporal trends associated with COVID-19 in-hospital mortality in England: an observational study using administrative data. Lancet Respiratory Med. 2021 doi: 10.1016/S2213-2600(20)30579-8. Epub ahead of print February 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen L.H., Drew D.A., Graham M.S., Joshi A.D., Guo C.-.G., Ma W., Mehta R.S., Warner E.T., Sikavi D.R., Lo C.-.H., Kwon S., Song M., Mucci L.A., Stampfer M.J., Willett W.C., Eliassen A.H., Hart J.E., Chavarro J.E., Rich-Edwards J.W., Davies R., Capdevila J., Lee K.A., Lochlainn M.N., Varsavsky T., Sudre C.H., Cardoso M.J., Wolf J., Spector T.D., Ourselin S., Steves C.J., Chan A.T., Albert C.M., Andreotti G., Bala B., Balasubramanian B.A., Beane-Freeman L.E., Brownstein J.S., Bruinsma F.J., Coresh J., Costa R., Cowan A.N., Deka A., Deming-Halverson S.L., Elena Martinez M., Ernst M.E., Figueiredo J.C., Fortuna P., Franks P.W., Freeman L.B., Gardner C.D., Ghobrial I.M., Haiman C.A., Hall J.E., Kang J.H., Kirpach B., Koenen K.C., Kubzansky L.D., Lacey J.V., Jr, Le Marchand L., Lin X., Lutsey P., Marinac C.R., Martinez M.E., Milne R.L., Murray A.M., Nash D., Palmer J.R., Patel A.V., Pierce E., Robertson M.M., Rosenberg L., Sandler D.P., Schurman S.H., Sewalk K., Sharma S.V., Sidey-Gibbons C.J., Slevin L., Smoller J.W., Steves C.J., Tiirikainen M.I., Weiss S.T., Wilkens L.R., Zhang F. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHS Digital, 2018. Nurses, Midwives and Support staff by area, level, gender and age. [Available from: https://digital.nhs.uk/data-and-information/find-data-and-publications/supplementary-information/2018-supplementary-information-files/staff-numbers/nurses-midwives-and-support-staff-by-area-level-gender-and-age-january-18 accessed 13/09/2021].
- Nickell L.A., Crighton E.J., Tracy C.S., Al-Enazy H., Bolaji Y., Hanjrah S., Hussain A., Makhlouf S., Upshur R.E.G. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. Can. Med. Assoc. J. 2004;170(5):793–798. doi: 10.1503/cmaj.1031077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nursing and Midwifery Council, 2021. The NMC register: 1 April 2020 –31 March 2021. [Available from: https://www.nmc.org.uk/globalassets/sitedocuments/data-reports/annual-2021/0005b-nmc-register-2021-web.pdf accessed 16/08/2021].
- Plumpton C.O., Morris T., Hughes D.A., White I.R. Multiple imputation of multiple multi-item scales when a full imputation model is infeasible. BMC Res. Notes. 2016;9(1):45. doi: 10.1186/s13104-016-1853-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poghosyan L., Aiken L.H., Sloane D.M. Factor structure of the Maslach burnout inventory: an analysis of data from large scale cross-sectional surveys of nurses from eight countries. Int. J. Nurs. Stud. 2009;46(7):894–902. doi: 10.1016/j.ijnurstu.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts, T., Daniels, J., Hulme, W., Hirst, R., Horner, D., Lyttle, M.D., Samuel, K., Graham, B., Reynard, C., Barrett, M., Foley, J., Cronin, J., Umana, E., Carlton, E., Vinagre, J., 2021a. Psychological distress and trauma in doctors providing frontline care during the COVID-19 pandemic in the United Kingdom and Ireland: a prospective longitudinal survey cohort study. [Available from: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3760472 accessed 14th April 2021]. [DOI] [PMC free article] [PubMed]
- Roberts T., Daniels J., Hulme W., Hirst R., Horner D., Lyttle M.D., Samuel K., Graham B., Reynard C., Barrett M., Foley J., Cronin J., Umana E., Vinagre J., Carlton E., On behalf of the collaborators of TERN, R., PERUKI, ITERN, TRIC, and SATARN Psychological distress during the acceleration phase of the COVID-19 pandemic: a survey of doctors practising in emergency medicine, anaesthesia and intensive care medicine in the UK and Ireland. Emerg. Med. J. 2021 doi: 10.1136/emermed-2020-210438. Epub ahead of print April 10, 2021. [DOI] [PubMed] [Google Scholar]
- Roberts T., Daniels J., Hulme W., Horner D., Lyttle M.D., Samuel K., Graham B., Hirst R., Reynard C., Barrett M., Carlton E. COVID-19 emergency response assessment study: a prospective longitudinal survey of frontline doctors in the UK and Ireland: study protocol. BMJ Open. 2020;10(8) doi: 10.1136/bmjopen-2020-039851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royston, P., White, I.R., 2011. Multiple Imputation by Chained Equations (MICE): implementation in Stata. 2011 45 (4), 20.
- Shah A.S.V., Wood R., Gribben C., Caldwell D., Bishop J., Weir A., Kennedy S., Reid M., Smith-Palmer A., Goldberg D., McMenamin J., Fischbacher C., Robertson C., Hutchinson S., McKeigue P., Colhoun H., McAllister D.A. Risk of hospital admission with coronavirus disease 2019 in healthcare workers and their households: nationwide linkage cohort study. BMJ. 2020;371:m3582. doi: 10.1136/bmj.m3582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuijfzand S., Deforges C., Sandoz V., Sajin C.-.T., Jaques C., Elmers J., Horsch A. Psychological impact of an epidemic/pandemic on the mental health of healthcare professionals: a rapid review. BMC Public Health. 2020;20(1):1230. doi: 10.1186/s12889-020-09322-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taquet M., Geddes J.R., Husain M., Luciano S., Harrison P.J. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021;8(5):416–427. doi: 10.1016/S2215-0366(21)00084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toynbee, P., 2020. The Guardian: it's officially the year of the nurse – what better time to reverse 10 years of bad care? [Available from: https://www.theguardian.com/commentisfree/2020/apr/24/year-nurse-tories-10-years-bad-care-nhs-crisis accessed 8/2/21]
- UCLA: Statistical Consulting Group, Multiple imputation in stata. [Available from: https://stats.idre.ucla.edu/stata/seminars/mi_in_stata_pt1_new/ accessed 5/3/21].
- UK Government, 2021. Coronavirus (COVID-19) in the UK. [Available from: https://coronavirus.data.gov.uk/ accessed 5/2/21].
- Weiss D.S. In: Assessing Psychological Trauma and PTSD. Wilson J.P., Keane T.M., Guilford P., editors. The Guilford Press; New York; London: 2006. The impact of event scale- revised. [Google Scholar]
- Williamson E.J., Walker A.J., Bhaskaran K., Bacon S., Bates C., Morton C.E., Curtis H.J., Mehrkar A., Evans D., Inglesby P., Cockburn J., McDonald H.I., MacKenna B., Tomlinson L., Douglas I.J., Rentsch C.T., Mathur R., Wong A.Y.S., Grieve R., Harrison D., Forbes H., Schultze A., Croker R., Parry J., Hester F., Harper S., Perera R., Evans S.J.W., Smeeth L., Goldacre B. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2020a. State of the world's nursing 2020: investing in education, jobs and leadership. [Available from: https://apps.who.int/iris/rest/bitstreams/1274201/retrieve accessed 08/02/2020]
- World Health Organization, 2020b. Year of the Nurse and the Midwife 2020. [Available from: https://www.who.int/campaigns/year-of-the-nurse-and-the-midwife-2020 accessed 08/02/2021]
- Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z., Liu X., Fuller C.J., Susser E., Lu J., Hoven C.W. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Canadian J. Psychiatry. 2009;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Z., Xu S., Wang H., Liu Z., Wu J., Li G., Miao J., Zhang C., Yang Y., Sun W., Zhu S., Fan Y., Chen Y., Hu J., Liu J., Wang W. COVID-19 in Wuhan: sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers. EClinicalMedicine. 2020;24 doi: 10.1016/j.eclinm.2020.100443. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analysed during the current study may be made available by the corresponding author on reasonable request.