Abstract
Coronavirus outbreak was a public health emergency. The surge of new confirmed cases and deaths was observed in developing countries due to the occurrence of new variants. However, factors associated with the duration of recovery among admitted patients remained uncertain. Therefore, we assessed factors associated with time to recovery from Covid-19 among hospitalized patients at the treatment center in South Central, Ethiopia. We employed a retrospective cross-sectional study among 422 patients hospitalized at Bokoji Hospital treatment center with Covid-19 from July 1, 2020, through October 30, 2021. Data were entered, coded, and analyzed using SPSS 26 version. We computed the survival probability using the Kaplan Meier method and determined factors associated with time to recovery using Cox regression analysis. Finally, the interpretation of adjusted hazard ratio (AHR) with 95% Confidence Interval (CI) and P-values less than 0.05 were declared as statistically significant. Our study found that the median time to recovery from Covid-19 infection of 13 days, with an IQR of 9–17 days. In multivariate Cox regression, ≥ 60 years old (AHR = 0.66; 95% CI: 0.49, 0.895), chronic pulmonary disease (AHR = 0.67; 95% CI: 0.455, 0.978), Male (AHR = 0.77; 95% CI: 0.611, 0.979), and being on Intranasal oxygen care (AHR = 0.56; 95% CI: 0.427–0.717) were significantly associated with time to recovery. Thus, health providers in treatment centers should give strict follow-up and priority for elders, patients with underlying diseases, and under supportive treatment during case management.
Keywords: Covid-19, Recovery time, Ethiopia, Coronavirus, South Central Ethiopia
Abbreviations: AIDS, Acquired Immune Deficiency Syndrome; AHR, Adjusted Hazard Ratio; CFR, Case Fatality Rate, CI, Confidence Interval; CHR, Crude Hazard Ratio; HIV, Human Immune Virus; LOS, Length of Stay; ICU, Intensive Care Unit; IQR, Interquartile Range; RT-PCR, Real-Time Polymerase Chain Reaction; HR, Hazard Ratio; SD, Standard Deviation; WHO, World Health Organization
1. Introduction
Covid-19 disease is a newly discovered infectious disease in the world [Bashirian et al., 2020]. The outbreak of Covid-19 began in Wuhan; China in December 2019 [Huang et al., 2020]. On 11 March 2020, the World Health Organization (WHO) declared the outbreak as a public health threat and a worldwide pandemic WHO, 2020. As of 3 November 2021, 247,472,724 confirmed cases, with 5012,337 deaths were reported to WHO globally. During this period, Africa reported 6092,498 confirmed cases, with 150,428 deaths WHO, 2021. Ethiopia reported the first confirmed case of this outbreak on 13 March 2020, in Addis Ababa. As of November 4, 2021, Ethiopia reported 366,424 confirmed cases, with 6509 deaths. The attack rate was estimated at 324.75 per 100 000 population, with a case fatality rate (CFR) of 1.78% [WHO, 2021, WHO, 2020]. Many Covid-19 infected people were asymptomatic or experienced mild symptoms and recovered without medical treatment [Cohen et al., 2020, Wu and McGoogan, 2020]. However, the severity of the disease ranges from asymptomatic to severe, with organ failure and death in some patients [Wiersinga et al., 2020]. The most common signs and symptoms of Covid-19 were fever, dry cough, diarrhea, and pneumonia in symptomatic patients [Huang et al., 2020, Young et al., 2020].
More than 75% of Covid-19 admitted patients need intranasal oxygen supplementation. The CFR among hospitalized patients varies by age, ranging from 0.3 per 1000 cases in age 5 to 17 years to 304.9 per 1000 cases among patients aged above 85 years old. However, treating hospitalized patients with Remdesivir improves the duration of viral clearances from 15 to 11 days [Alwafi et al., 2021]. The duration of viral clearance among admitted Covid-19 patients varies with populations’ age structure, presence of comorbidity, and quality of healthcare [van Gerwen et al., 2021, Bhandari et al., 2020]. For instance, the median length of stay (LOS) was 10 days in India, with the median time to recovery of 60 days [Bhandari et al., 2020]. Another study from the Indian setup also reported that the median LOS of 7 days among hospitalized Covid-19 patients [Thiruvengadam et al., 2021]. Moreover, the median LOS was 13 days, with a range of 10 to 18 days in China [Li et al., 2021]. On other hand, the median duration of viral clearance was 19 days in Addis Ababa (Abrahim et al., 2020) whereas the median time to recovery was 18 days in Western Ethiopia [T. Tolossa et al., 2021]. Studies from different settings revealed that being old-aged, female, having underlying diseases, presence of clinical manifestation during admission, low oxygen saturation, and neutrophil-lymphocyte ratio were associated with delayed recovery from Covid-19 [Alwafi et al., 2021, Thiruvengadam et al., 2021, T Tolossa et al., 2021, T. Tolossa et al., 2021, Liu et al., 2021, Wu et al., 2021, Cummings et al., 2020].
In developing countries, the occurrences of outbreaks increased the demand for hospital beds and supportive care medical equipment in public health facilities [Li et al., 2021]. Thus, determining the factors that delayed the recovery rate of admitted patients was essential in the planning of allocation of medical resources, improving the quality of healthcare, and designing effective interventions [Thiruvengadam et al., 2021]. Few studies assessed factors that affect the duration of recovery among Covid-19 patients admitted to public health facilities. However, the recovery rate of Covid-19 varies among patients and settings due to differences in risk factors. Thus, the absence of studies in our study area affects the decision-making of health providers to some extents. Therefore, this study determined factors associated with time to recovery among Covid-19 patients hospitalized at Bokoji hospital treatment center in South Central, Ethiopia.
2. Materials and methods
2.1. Study setting, design, and population
We conducted the study at Bokoji Hospital Covid-19 treatment center which is found in Arsi zone, South Central Ethiopia, with a 100-bed capacity. It is located 56 km from Asella, the zonal city of the Arsi zone. We used a retrospective cross-sectional study among Covid-19 patients discharged from the treatment center from July 1, 2020, to October 30, 2021. A total of 422 Covid-19 patients were followed for the clinical outcome; and the final date of follow-up was October 30, 2021. Covid-19 patients with incomplete medical records and deceased on arrival were excluded.
2.2. Data collection and quality management
Sociodemographic, clinical data such as status at admission, clinical signs and symptoms, comorbidities, place of treatment, length of stay, laboratory result, and final clinical outcome were extracted from medical records using data abstraction form. Health informatics professionals extracted the required data after one day of training. The completeness and consistency of the collected data was cross-checked by principal investigator on daily basis.
2.3. Study variables and operational definition
The primary dependent variable was time to recovery. The time was estimated in days and the interval from the date of hospitalization to the date of discharge was considered as the survival time. The final clinical outcome of patients under treatment was cured, death, discharged with consent after clinically improved, or transferred to the nearby treatment center for further management. Covid-19 patients were discharged from the treatment center after two consecutive negative real-time reverse transcriptase-polymerase chain reaction test (RT-PCR) tests or clinical improvement. If the patients were discharged after confirmed negative RT-PCR results, the patients had the event status and coded as “1″. Besides, cases were considered as censored if hospitalized Covid-19 patients died, were discharged with consent, or transferred out to the nearby treatment centers, and coded as “0″. We confirmed the outcome of patients by assessing the medical records of the patient which was approved by the physician. Sociodemographic factors, health-related factors, comorbidity conditions, clinical manifestation, and treatment-related factors were the independent variables.
2.4. Data analysis
Data were entered, coded, and analyzed using Statistical Package for Social Science (SPSS) version-26 Software. We computed mean or median, with standard deviations (SD) or Inter Quartile Range (IQR) for continuous variables. Categorical variables were summarized using frequencies and proportions. Survival curves were described using the Kaplan-Meier method and compared using the log-rank test. We used the Cox regression analysis model to determine factors associated with time to recovery. Variables with P-value less than 0.25 were transferred to multivariate Cox regression analysis, with P-value less than 0.05 were considered significantly associated with the Covid-19 recovery time.
3. Result
3.1. Covid-19 patient's sociodemographic and clinical characteristics
One hundred forty-one (33.4%) of the participants were in the age group 18–29 years old, with a mean age of 43 (SD: 19.22) years. Three hundred ninety-eight (94.3%) had Covid-19 signs and symptoms, with 82 (19.4%) were mild, 110 (26.1%) were moderate, 185 (43.8%) were severe and 21 (5%) were critical during admission. The most common observed comorbidities were Diabetic Mellitus (26.5%), hypertension (18%), and Chronic pulmonary disease (16.9%). Two hundred seventy-seven (69.6%) received intranasal oxygen care (Table 1 ).
Table 1.
Clinical and sociodemographic characteristics of Patients hospitalized with Covid-19 to Bokoji Hospital treatment center, South Central Ethiopia from July 1, 2020, to 30, October 2021.
| Clinical characteristics | Categories | Frequency (%) |
|---|---|---|
| Sex | Male | 244 (57.8) |
| Female | 178 (42.2) | |
| Resident | Rural | 160 (37.9) |
| Urban | 262 (62.1) | |
| Age (in years) | 18–29 | 141 (33.4) |
| 30–45 | 106 (25.1) | |
| 46–59 | 80 (19.0) | |
| ≥ 60 | 95 (22.5) | |
| Mean (SD) | 41 (21) | |
| Sign and symptom | yes | 398 (94.3) |
| No | 24 (5.7) | |
| Co-morbidity | Yes | 245 (58.1) |
| No | 177 (41.9) | |
| Status | Asymptomatic | 24 (5.7) |
| Mild | 82 (19.4) | |
| Moderate | 110 (26.1) | |
| Severe | 185 (43.8) | |
| Critical | 21 (5.0) | |
| Type of comorbidity | Hypertension | 62 (18.0) |
| Chronic cardiac disease | 37 (10.8) | |
| Chronic pulmonary disease | 58 (16.9) | |
| Asthma | 49 (14.2) | |
| Diabetic Mellitus | 91 (26.5) | |
| Chronic Kidney disease | 17 (4.9) | |
| Malignance | 15 (4.4) | |
| HIV/AIDS | 15 (4.4) | |
| Intranasal oxygen use | Yes | 277 (69.6) |
| No | 121 (30.4) | |
| Place of treatment | Ward only | 366 (86.7) |
| Intensive Care Unit (ICU) and Ward | 56 (13.3) |
3.2. Treatment outcome of Covid-19 patient hospitalized at the treatment center
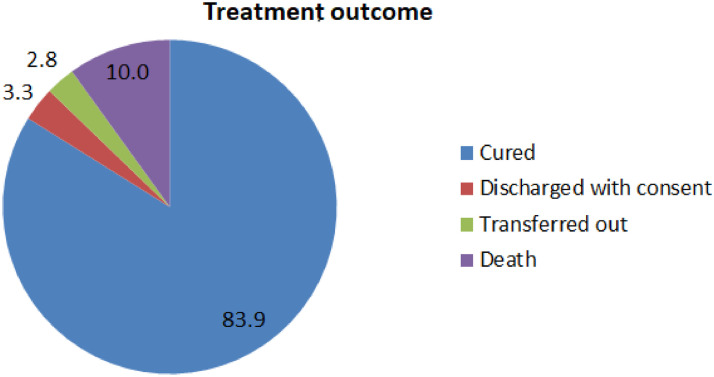
Out of 422 Covid-19 cases, 354 (83.8%) were cured and 14 (3.3%) were discharged with consent completed after clinical improvement. Besides, 12 (2.8%) were transferred out to a nearby treatment center for further management while 42 (10%) died in the treatment center (Fig 1 ).
Fig. 1.
Treatment outcome of Covid-19 patients admitted to Bokoji hospital treatment center, South Central Ethiopia from July 1, 2020, to October 30, 2021.
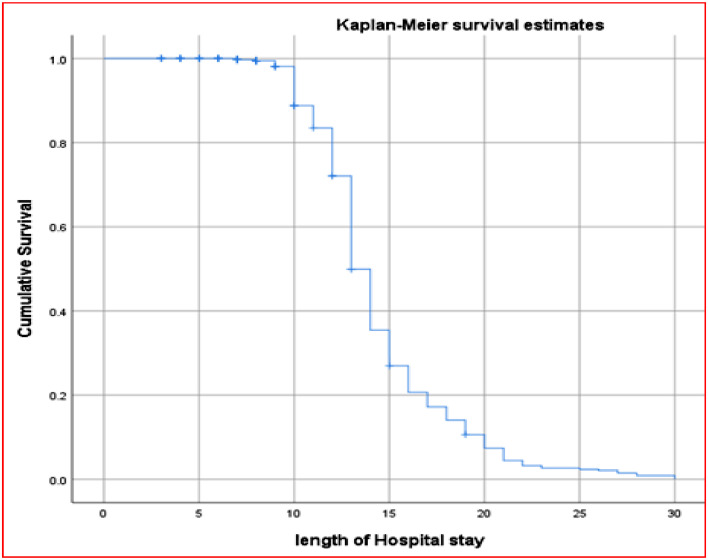
3.3. Time to recovery from Covid-19 infection among hospitalized patients
The median duration of viral clearance from Covid-19 infection was 13 days, with an IQR of 9–17 days (Fig 2 ). We used the Kaplan-Meier survivor functions curve to estimate the survival time and the differences in the duration of recovery rates between categories of individual variables. Covid-19 patients in worsening condition during admission received intranasal oxygen care, those from urban areas and ≥ 60 years old patients had a significantly longer duration of recovery from infection as compared to their counterparts. There was also a significant difference in the duration of viral clearance among male and female Covid-19 patients. However, a difference in the duration of recovery was not observed among patients treated at Ward or both (i.e. ICU and ward) (Table 2 ).
Fig. 2.
Kaplan-Meier survival probability curve among Covid-19 patients admitted to Bokoji hospital treatment center, South Central Ethiopia from July 1, 2020, to October 30, 2021.
Table 2.
Duration of recovery by sociodemographic and clinical characteristics of Covid 19 patients admitted to Bokoji Hospital treatment center, South Central Ethiopia from July 1, 2020, to October 30, 2021.
| Variable | Category | Duration of recovery in days Median (IQR) | P-value |
|---|---|---|---|
| Sex | Male | 14 (12–17) | 0.021 |
| Female | 13 (12–15) | ||
| Resident | Urban | 14(12–16) | 0.028 |
| Rural | 13(12–15) | ||
| Age (in years) | 18–29 | 13(12–14) | 0.002 |
| 30–45 | 14(13–16) | ||
| 46–59 | 14(13–17) | ||
| ≥ 60 | 14(13–17) | ||
| Intranasal oxygen use | Yes | 14(13–17) | 0.001 |
| No | 13(11–14) | ||
| Status at admission | No symptom/mild | 13(11–14) | 0.001 |
| Moderate | 13(12–15) | ||
| Severe/critical | 14(13–18) | ||
| Place of care | Ward only | 13(12–16) | 0.138 |
| ICU and Ward | 15(14–16) |
3.4. Factors associated with time to recovery among Covid 19 patients
In bivariate Cox regression analysis factors like residence, Age, sex, intranasal oxygen use, and different types of comorbidities were statistically associated with recovery time. Moreover, the age of patients, sex, intranasal oxygen use, and having the chronic pulmonary disease (CPD) were significantly associated with recovery time in multivariate Cox regression analysis. In multivariate Cox regression, the hazard ratio (HR) of recovery rate among Covid-19 patients were significantly lower among ≥ 60 years (AHR = 0.66; 95% CI: 0.49, 0.895), CPD (AHR = 0.67; 95% CI: 0.455, 0.978), Male (AHR = 0.77; 95% CI: 0.611, 0.979), and being on Intranasal oxygen (AHR = 0.56; 95% CI: 0.427–0.717) compared to their counterparts (Table 3 ).
Table 3.
Multivariate Cox regression analysis of recovery time among Covid-19 patients admitted to Bokoji Hospital treatment Center, South Central Ethiopia from July 1, 2020, to October 30, 2021.
| Categories | Recovered |
CHR (95%CI) | AHR (95%CI) | |
|---|---|---|---|---|
| Yes (%) | No (%) | |||
| Age (in years) | ||||
| 18–29 | 127 (90.1) | 14 (9.9) | 1 | 1 |
| 30- 45 | 84 (79.2) | 22 (20.8) | 0.71 (0.540, 0.942) | 0.76 (0.564, 1.017) |
| 46–59 | 67 (83.8) | 13 (16.2) | 0.70 (0.517, 0.936) | 0.73 (0.522, 1.017) |
| ≥ 60 | 76 (80.0) | 19 (20.0) | 0.66 (0.496, 0.881) | 0.66 (0.490, 0.895)* |
| Residence | ||||
| Rural | 140 (87.5) | 20 (12.5) | 1 | 1 |
| Urban | 214 (81.7) | 48 (18.3) | 0.82 (0.648, 0.998) | 0.83 (0.654, 1.058) |
| Sex | ||||
| Female | 151 (84.8) | 27 (15.2) | 1 | 1 |
| Male | 203 (83.2) | 41 (16.8) | 0.81 (0.649, 0.992) | 0.77 (0.611, 0.979)* |
| Hypertension | ||||
| Yes | 44 (71.0) | 18 (29.0) | 0.88 (0.639, 1.202) | 1.21 (0.841, 1.730) |
| No | 310 (86.1) | 50 (13.9) | 1 | 1 |
| Chronic cardiac disease | ||||
| Yes | 28 (75.7) | 9 (24.3) | 0.93 (0.631, 1.369) | 1.11 (0.728, 1.679) |
| No | 326 (84.7) | 59 (15.3) | 1 | 1 |
| Chronic pulmonary disease | ||||
| Yes | 34 (58.6) | 24 (41.4) | 0.58 (0.504, 0.825) | 0.67 (0.455, 0.978)* |
| No | 320 (87.9) | 44 (12.1) | 1 | 1 |
| Asthma | ||||
| Yes | 34 (69.4) | 15 (30.6) | 0.83 (0.578, 1.175) | 0.92 (0.635, 1.329) |
| No | 320 (85.8) | 53 (14.2) | 1 | 1 |
| Chronic Kidney disease | ||||
| Yes | 9 (52.9%) | 8 (47.1) | 1.24 (0.640, 2.408) | 1.16 (0.580, 2.310) |
| No | 345 (85.2) | 60 (14.8) | 1 | 1 |
| Malignance | ||||
| Yes | 10 (66.7) | 5 (33.3) | 1.10 (0.528, 1.985) | 1.49 (0.717, 3.106) |
| No | 344 (84.5) | 63 (15.5) | 1 | 1 |
| Diabetic Mellitus | ||||
| Yes | 73 (80.2) | 18 (19.8) | 1.10 (0.825, 1.385) | 1.22 (0.921, 1.606) |
| No | 281 (84.9) | 50 (15.1) | 1 | 1 |
| HIV/AIDS | ||||
| Yes | 7 (46.7) | 8 (53.3) | 1.60 (0.753, 3.377) | 1.33 (0.606, 2.936) |
| No | 347 (85.3) | 60 (14.7) | 1 | 1 |
| Intranasal oxygen use | ||||
| No | 117 (96.7) | 4 (3.3) | 1 | 1 |
| Yes | 213 (76.9) | 64 (23.1) | 0.57 (0.450, 0.711) | 0.56 (0.427, 0.717)* |
Note: *, P-values less than 0.05.
4. Discussion
The outbreak of Covid-19 emerged as a public health threat, with high CFR among old aged and patients with chronic illnesses [Algahtani et al., 2021, Greco et al., 2021]. The virus had a potency of spreading from asymptomatic and symptomatic carriers, with the average time of onset of signs and symptoms of five days. Around 97.5% of Covid-19 patients develop signs and symptoms within 11.5 days of acquiring infection [Wiersinga et al., 2020]. This study determined the time to recovery and its associated factors among Covid-19 patients hospitalized at Bokoji Hospital treatment center, South Central Ethiopia. Our study found that the median duration to recovery from Covid-19 infection of 13 days, with an IQR of 9–17 days. Recent findings from Hefei, China (17 days) [Guo et al., 2021], Vietnam (17 days) [Long et al., 2020], and India (10 days) [Bhandari et al., 2020] also reported the same median duration of viral shedding. However, the finding was lower than reports by Liu et al. from China (22 days) [Liu et al., 2020], Zhou et al. at Wuhan Pulmonary Hospital in China (20 days) [Zhou et al., 2020], Abrahim et al. from Addis Ababa, Ethiopia (19 days) (Abrahim et al., 2020), and Tolossa et al. from Western Ethiopia (18 days) [T. Tolossa et al., 2021] and higher than finding in Saudi Arabia (6 days) [Alwafi et al., 2021], India (7 days) [Thiruvengadam et al., 2021] and Pakistan (6 days) [Almas et al., 2021]. This discrepancy could be explained by differences in the quality of healthcare, medications utilized in the management of Covid-19 patients, disease severity, population structure, study setting, and period.
Moreover, patients with CPD had a 32% lower rate of recovery from Covid-19 infection compared to those without the disease. This is in line with finding in China [Wu et al., 2020, Wang et al., 2020, Shi et al., 2020], Pakistan [Almas et al., 2021], and Ethiopia [T Tolossa et al., 2021] that found patients with underlying diseases such as CPD were associated with a poor prognosis of Covid-19. This might be explained by the reduced immune system of patients with comorbidities to viral infection.
Sex of the patient was also significantly associated with the rate of recovery from Covid-19 infection. This is consistent with finding in China [Guo et al., 2021, Mi et al., 2020], Pakistan [Almas et al., 2021], South Korea [Byeon et al., 2021], and Addis Ababa (Abrahim et al., 2020) that reported a significant association between sex and Covid-19 patients' recovery rate from infection. Furthermore, patients with ≥ 60 years old had a 34% lower rate of recovery from Covid-19 compared to 18–29 years old individuals. The reports from studies in China [Liu et al., 2021, Wu et al., 2020], Korea [Das and Gopalan, 2020], Vietnam [Long et al., 2020, Thai et al., 2020], and Ethiopia [T. Tolossa et al., 2021] also revealed that old aged patients had lower recovery rates from Covid-19 infection as compared to young respondents. This might be due to the suppression of immunities against infection and the presence of different underlying conditions among old-aged individuals.
Our study also revealed that patients on intranasal oxygen care had a lower recovery rate compared to their counterparts. This is similar to reports from India [Thiruvengadam et al., 2021], Saudi Arabia [Alwafi et al., 2021], and China [Li et al., 2021, Hu et al., 2020] that revealed individuals with critical conditions (i.e. on supportive care treatment) had a lower rate of recovery compared to their counterparts. The most probably reason might be the majority of the patient receiving this supportive care was in worsening condition and had chronic illnesses that deteriorate their immunity status.
5. Limitations of the study
Our study had influenced by limitations related to retrospective study design and the use of secondary data sources. Consequently, essential variables that couldn't be recorded in patients’ medical records and had the potential of affecting the duration of the patient's recovery from Covid-19 infection were excluded.
6. Conclusion
Our study revealed that older age, male patients, being on intranasal oxygen supplementation and chronic pulmonary patients were significantly associated with prolonged recovery time from Covid-19 infection. Therefore, health providers in treatment centers should give strict follow-up and priority for elders, patients with chronic illnesses, and under supportive treatment during case management.
Declarations
Consent for publication: Not applicable
Availability of data and material: The datasets used or analyzed during this study were available from the corresponding author on reasonable request.
Competing interests: The authors declare that they have no competing interests.
Funding: NA
Authors’ contributions
AWK, GA, TK, and HEH designed and worked on the study protocols. GA, TK, HEH, and AK prepared data collection tools and trained the data collectors. AWK supervised the data collection process. AWK, GA, and HEH conducted data entry to SPPS. AWK, GA, and HEH analyzed the data, interpreted the result, and wrote the manuscript's draft and final version. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Arsi University, College of Health Sciences Research Ethics Review Board approved ethical clearance, and all methods were carried out in accordance with the University's relevant guidelines and regulations. Arsi University Institutional Review Board (IRB) waived the informed consent procedure for this study. Since the study was conducted through a review of medical records, consent to participate was waived. Individual patients were not harmed, and the data was used for this study.
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgments
We want to express our deepest gratitude to the Bokoji hospital administration and staff, particularly their data collection input. Our appreciation also goes to Mr. Mengesha Moges and Mr. Angasa Damissie for their sincere support during data collection.
References
- Abrahim S.A., Tessema M., Defar A., Hussen A., Ejeta E., Demoz G., Tereda A.B., Feleke A., Amare M., et al. Time to recovery and its predictors among adults hospitalized with COVID-19: A prospective cohort study in Ethiopia. PloS one. 2020;15(12) doi: 10.1371/journal.pone.0244269. In this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Algahtani F.D., Hassan S.-u.-N., Alsaif B., Zrieq R. Assessment of the quality of life during COVID-19 pandemic: a cross-sectional survey from the kingdom of saudi arabia. Int. J. Environ. Res. Public Health. 2021;18:847. doi: 10.3390/ijerph18030847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almas A., Mushtaq Z., Moller J. Acuity level of care as a predictor of case fatality and prolonged hospital stay in patients with COVID-19: a hospital-based observational follow-up study from Pakistan. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-045414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alwafi H., Naser A.Y., Qanash S., Brinji A.S., Ghazawi M.A., Alotaibi B., Alghamdi A., Alrhmani A., Fatehaldin R., Alelyani A. Predictors of length of hospital stay, mortality, and outcomes among hospitalised COVID-19 patients in Saudi Arabia: a cross-sectional study. J. Multidiscip. Healthc. 2021;14:839. doi: 10.2147/JMDH.S304788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashirian S., Jenabi E., Khazaei S., Barati M., Karimi-Shahanjarini A., Zareian S., Rezapur-Shahkolai F., Moeini B. Factors associated with preventive behaviours of COVID-19 among hospital staff in Iran in 2020: an application of the Protection Motivation Theory. J. Hosp. Infect. 2020;105:430–433. doi: 10.1016/j.jhin.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhandari S., Tak A., Singhal S., Shukla J., Shaktawat A.S., Gupta J., Patel B., Kakkar S., Dube A., Dia S. Patient flow dynamics in hospital systems during times of COVID-19: Cox proportional hazard regression analysis. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.585850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byeon K.H., Kim D.W., Kim J., Choi B.Y., Choi B., Cho K.D. Factors affecting the survival of early COVID-19 patients in South Korea: an observational study based on the Korean National Health Insurance big data. Int. J. Infect. Dis. 2021;105:588–594. doi: 10.1016/j.ijid.2021.02.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen P.A., Hall L.E., John J.N., Rapoport A.B. Elsevier; Mayo Clinic Proceedings: 2020. The Early Natural History of SARS-CoV-2 infection: Clinical Observations from an urban, Ambulatory COVID-19 Clinic; pp. 1124–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings M.J., Baldwin M.R., Abrams D., Jacobson S.D., Meyer B.J., Balough E.M., Aaron J.G., Claassen J., Rabbani L.E., Hastie J. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet North Am. Ed. 2020;395:1763–1770. doi: 10.1016/S0140-6736(20)31189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das A.K., Gopalan S.S. Epidemiology of COVID-19 and predictors of recovery in the Republic of Korea. Pulm. Med. 2020;2020 doi: 10.1155/2020/7291698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greco F., Altieri V.M., Esperto F., Mirone V., Scarpa R.M. Impact of COVID-19 pandemic on health-related quality of life in uro-oncologic patients: what should we wait for? Clin. Genitourin. Cancer. 2021;19:e63–e68. doi: 10.1016/j.clgc.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo A., Lu J., Tan H., Kuang Z., Luo Y., Yang T., Xu J., Yu J., Wen C., Shen A. Risk factors on admission associated with hospital length of stay in patients with COVID-19: a retrospective cohort study. Sci. Rep. 2021;11:1–7. doi: 10.1038/s41598-021-86853-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L., Chen S., Fu Y., Gao Z., Long H., Ren H.-w., Zuo Y., Wang J., Li H., Xu Q.-b. Risk factors associated with clinical outcomes in 323 coronavirus disease 2019 (COVID-19) hospitalized patients in Wuhan, China. Clin. Infect. Dis. 2020;71:2089–2098. doi: 10.1093/cid/ciaa539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet North Am. Ed. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li K., Zhang C., Qin L., Zang C., Li A., Sun J., Zhao Y., Feng Y., Zhang Y. A nomogram prediction of length of hospital stay in patients with COVID-19 pneumonia: a retrospective cohort study. Dis. Marker. 2021:2021. doi: 10.1155/2021/5598824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Zhou H., Zhou Y., Wu X., Zhao Y., Lu Y., Tan W., Yuan M., Ding X., Zou J. Risk factors associated with disease severity and length of hospital stay in COVID-19 patients. J. Infect. 2020;81:e95–e97. doi: 10.1016/j.jinf.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Zhang J.-.F., Ma H.-.N., Feng K., Chen Z.-.W., Yang L.-.S., Mei B., Zhang J.-.J. Clinical characteristics and factors associated with disease progression of mild to moderate COVID-19 patients in a Makeshift (Fangcang) hospital: a retrospective cohort study. Ther. Clin. Risk Manag. 2021;17:841. doi: 10.2147/TCRM.S314734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long K.Q., Hanh H.H., Hanh T.T.T., Van Minh H. Treatment for COVID-19 patients in Vietnam: analysis of time-to-recovery. Asian Pac. J. Trop. Med. 2020;13:397. [Google Scholar]
- Mi J., Zhong W., Huang C., Zhang W., Tan L., Ding L. Gender, age and comorbidities as the main prognostic factors in patients with COVID-19 pneumonia. Am. J. Transl. Res. 2020;12:6537. [PMC free article] [PubMed] [Google Scholar]
- Shi Q., Zhang X., Jiang F., Zhang X., Hu N., Bimu C., Feng J., Yan S., Guan Y., Xu D. Clinical characteristics and risk factors for mortality of COVID-19 patients with diabetes in Wuhan, China: a two-center, retrospective study. Diabetes Care. 2020;43:1382–1391. doi: 10.2337/dc20-0598. [DOI] [PubMed] [Google Scholar]
- Thai P.Q., Son D.T., Van H.T.H., Minh L.N., Hung L.X., Van Toan N., Hoat L.N., Luong D.H., Khue L.N., Khoa N.T. Factors associated with the duration of hospitalisation among COVID-19 patients in Vietnam: a survival analysis. Epidemiol. Infect. 2020;148 doi: 10.1017/S0950268820001259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiruvengadam G., Lakshmi M., Ramanujam R. A study of factors affecting the length of hospital stay of COVID-19 patients by Cox-proportional hazard model in a South Indian tertiary care hospital. J. Prim. Care Commun. Health. 2021;12 doi: 10.1177/21501327211000231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolossa T., Wakuma B., Seyoum G.D., Merdassa A.E., Getachew M., Fetensa G., Ayala D., Turi E. Time to recovery from COVID-19 and its predictors among patients admitted to treatment center of Wollega University Referral Hospital (WURH), Western Ethiopia: survival analysis of retrospective cohort study. PLoS One. 2021;16 doi: 10.1371/journal.pone.0252389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolossa T., Wakuma B., Seyoum Gebre D., Merdassa Atomssa E., Getachew M., Fetensa G., Ayala D., Turi E. Time to recovery from COVID-19 and its predictors among patients admitted to treatment center of Wollega University Referral Hospital (WURH), Western Ethiopia: survival analysis of retrospective cohort study. PLoS One. 2021;16 doi: 10.1371/journal.pone.0252389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Gerwen M., Alsen M., Little C., Barlow J., Genden E., Naymagon L., Tremblay D. Risk factors and outcomes of COVID-19 in New York City; a retrospective cohort study. J. Med. Virol. 2021;93:907–915. doi: 10.1002/jmv.26337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., He W., Yu X., Hu D., Bao M., Liu H., Zhou J., Jiang H. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J. Infect. 2020;80:639–645. doi: 10.1016/j.jinf.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiersinga W.J., Rhodes A., Cheng A.C., Peacock S.J., Prescott H.C. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;324:782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- Wu J., Li W., Shi X., Chen Z., Jiang B., Liu J., Wang D., Liu C., Meng Y., Cui L. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19) J. Intern. Med. 2020;288:128–138. doi: 10.1111/joim.13063. [DOI] [PubMed] [Google Scholar]
- Wu J., Mafham M., Mamas M.A., Rashid M., Kontopantelis E., Deanfield J.E., de Belder M.A., Gale C.P. Mayo Clinic Proceedings. Elsevier; 2021. Place and underlying cause of death during the COVID-19 pandemic: retrospective cohort study of 3.5 million deaths in England and Wales, 2014 to 2020; pp. 952–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO, 2021. Weekly Operational Update on COVID-19.
- WHO, 2020. The first case of covid-19 confirmed in Ethiopia.
- WHO, 2020. World Health Organization Director-General's Opening Remarks at the Media Briefing on COVID-19.
- Young B.E., Ong S.W.X., Kalimuddin S., Low J.G., Tan S.Y., Loh J., Ng O.-.T., Marimuthu K., Ang L.W., Mak T.M. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA. 2020;323:1488–1494. doi: 10.1001/jama.2020.3204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]