Abstract
Background
The COVID-19 pandemic has resulted in delays in presentation for other urgent medical conditions, including pediatric appendicitis. Several single-center studies have reported worse outcomes, but no state-level data is available. We aimed to determine the statewide effect of the COVID-19 pandemic on the presentation and management of pediatric appendicitis patients.
Materials and Methods
Patients < 18 years old with acute appendicitis at four tertiary pediatric hospitals in California between March 19, 2020 to September 19, 2020 (COVID-era) were compared to a pre-COVID cohort (March 19, 2019 to September 19, 2019). The primary outcome was the rate of perforated appendicitis. Secondary outcomes were symptom duration prior to presentation, and rates of non-operative management.
Results
Rates of perforated appendicitis were unchanged (40.4% of 592 patients pre-COVID versus 42.1% of 606 patients COVID-era, P = 0.17). The median symptom duration was 2 days in both cohorts (P = 0.90). Computed tomography (CT) use rose from 39.8% pre-COVID to 49.4% during COVID (P = 0.002). Non-operative management increased during the pandemic (8.8% pre-COVID versus 16.2% COVID-era, P < 0.0001). Hospital length of stay (LOS) was longer (2 days pre-COVID versus 3 days during COVID, P < 0.0001).
Conclusions
Pediatric perforated appendicitis rates did not rise during the first six months of the COVID-19 pandemic in California in this multicenter study, and there were no delays in presentation noted. There was a higher rate of CT scans, non-operative management, and longer hospital lengths of stay.
Keywords: Appendicitis, COVID-19, Appendectomy, Non-operative management
Introduction
The COVID-19 pandemic has posed a significant burden on an already resource-strained healthcare system. There is significant concern that fear of contracting COVID-19 has caused patients to avoid seeking healthcare for other conditions, leading to delays in presentation and subsequent treatment, with potentially worse outcomes. This has been studied in adult and pediatric cancer patients1 and in patients with emergency general surgical conditions such as appendicitis,2 finding delays in diagnosis and presentation at later stages of disease.
Several studies reported increased rates of perforated appendicitis in children during the COVID-19 pandemic.3, 4, 5 However, these studies were primarily single-center or single-city and investigated short time periods following the peak of the pandemic in March 2019, ranging from 1 to 3 months. As the pandemic continues, the lasting effect on the presentation and management of children with appendicitis is not well known. Additionally, statewide and nation-wide trends are unknown.
The objective of this study was to assess the effect of the COVID-19 pandemic and mandatory statewide Shelter in Place orders in California on the presentation and management of pediatric appendicitis over a 6 month period of time at multiple tertiary-care pediatric hospitals. We hypothesized that there would be increased rates of perforated appendicitis and delays in presentation following the Shelter in Place order compared to an identical time period one year earlier.
Methods
Study setting
Local institutional review board approval was obtained at each participating institution, and data use agreements for the sharing of de-identified data were approved. A waiver of informed consent was granted. All patients < 18 years old presenting with acute appendicitis from March 19, 2020 through September 19, 2020 were included in the COVID-era cohort. A historical cohort of patients presenting March 19, 2019 through September 19, 2019 was used for comparison (pre-COVID). The same dates one year prior were chosen to account for potential seasonal variability in appendicitis.6 The start date of March 19, 2020 was chosen as this was the date of the first Shelter-in-Place mandate issued by the state of California. Patients were identified by International Classification of Diseases (ICD) codes for acute appendicitis. Data were collected from four tertiary care pediatric hospitals around the state of California: University of California Davis in Sacramento, CA; Valley Children's Hospital in Madera, CA; University of California – Los Angeles Mattel Children's Hospital in Los Angeles, CA; and Harbor-UCLA Hospital in Torrance, CA, thus allowing for sampling of patients from Northern, Central and Southern California. Patients were excluded if they did not have acute appendicitis, if they were presenting for interval appendectomy, or if they had an appendectomy at an outside hospital and were transferred to a study center for ongoing management.
Data collection
Data was collected at each institution and entered in a de-identified manner into a Research Electronic Data Capture (REDCap) electronic database hosted at UC Davis. REDCap is a secure, web-based platform that supports data capture for research.7 , 8 Data collected included patient demographics, insurance status, transfer status, duration of symptoms prior to presentation, imaging results, initial white blood cell (WBC) count, diagnoses (acute non-perforated appendicitis or perforated appendicitis), management, post-operative complications including organ-space surgical site infections (SSI) and additional interventions needed, length of stay (LOS), as well as 30-day emergency department (ED) visits and readmissions.
Perforated appendicitis was determined by operative report description of a hole in the appendix for patients who underwent operative management; all other patients treated operatively for acute appendicitis were categorized as non-perforated, including suppurative and gangrenous appendicitis without a hole in the appendix. Patients treated with percutaneous abscess drainage were categorized as perforated appendicitis. Patients treated with antibiotics alone were categorized as perforated or non-perforated based on imaging reports; patients with an associated abscess were categorized as perforated. For transferred patients, the initial WBC from the referring institution was recorded, rather any repeat WBC results from the study institution, as patients may have received fluid resuscitation and antibiotics at the referring institution, thus resulting in a potentially improved WBC at the time of arrival to the study institution. Post-operative organ-space SSI was determined based on imaging showing a new or worsening intraabdominal abscess after surgical treatment.
Patient Management
Patient management was not pre-specified in this retrospective cohort study. Institutions continued to follow existing institutional guidelines for the treatment of pediatric appendicitis. In general, patients with acute non-perforated appendicitis are treated operatively at two of the institutions (UC Davis and Valley Children's Hospital), while non-operative management with antibiotics alone is offered as a treatment option for eligible patients at the other two institutions (UCLA and Harbor-UCLA). However, at all institutions, the decision to pursue non-operative management for non-perforated appendicitis is based upon a discussion between the surgical team and the family. The decision to operate for perforated appendicitis is typically based on duration of symptoms; those with perforated appendicitis and well-formed abscess are generally treated with non-operative management depending on duration of symptoms prior to presentation at all four institutions.
In the COVID-era cohort, at two institutions (UC Davis and Valley Children's Hospital), there was no intentional departmental shift to non-operative management during the COVID-era study period. At two institutions (UCLA and Harbor-UCLA), due to theoretical concern regarding aerosolization of COVID-19 particles, non-operative management was pursued when possible, regardless of the patient's COVID status.
Outcomes and Hypotheses
The primary outcome was the rate of perforated appendicitis, which we hypothesized would be higher in the COVID-era cohort than the pre-COVID cohort. Secondary outcomes included duration in symptoms prior to presentation to the hospital. We hypothesized that due to potential fear of exposure to COVID in the hospital or ED, patients may present after a longer duration of symptoms. We additionally hypothesized that non-operative management would be more common in the COVID-era cohort than the pre-COVID cohort, as hospital resources became increasingly strained. In cases of non-perforated appendicitis, treatment with antibiotics alone, for example, may have been an appealing choice to families as they may be able to complete the treatment course at home rather than in the hospital. Lastly, we hypothesized that post-operative outcomes, including complications such as SSI or need for additional interventions, and ED visits and readmissions would be higher in the COVID-era cohort.
Data Analysis
The COVID-era cohort was compared to the pre-COVID cohort. The rates of acute appendicitis cases in 2019 and 2020 were compared using Poisson regression analysis and are presented as percentage change with 95% confidence intervals (95% CI). With historical rates of perforated appendicitis in children of approximately 30%, a sample size of 172 patients would provide 80% power to detect a 10% increase in rates of perforated appendicitis. An additional sub-group analysis of patients with non-perforated versus perforated appendicitis was performed as outcomes frequently differ significantly. To determine if there were differential effects early in the pandemic compared to later, sub-group analyses of the first and last 3 months of the 6 month study period were performed. Finally, the main outcomes of perforated appendicitis rate and symptom duration prior to presentation were performed separately for each participating institution to ensure any hospital-level differences were captured.
Categorical data are presented as number and percentage and compared by chi-square test or Fisher's exact test where appropriate. Continuous data are presented as median and interquartile range and compared by Mann Whitney U test. Significance was set at P < 0.05. Analysis was conducted using SAS (SAS, version 9.45; SAS Institute Inc).
Results
Patient characteristics
Overall, there were 1198 pediatric patients with acute appendicitis included: 606 patients treated in the pre-COVID cohort and 592 patients in the COVID-era cohort (-2.3% change, 95% CI -12.8%, 9.5%, P = 0.69) (Table 1 ). Nearly one-half of patients presented as transfers from referring hospitals in both cohorts (43.9% pre-COVID versus 43.6% COVID-era, P = 0.91). The median symptom duration was similar (2 days in both, P = 0.90).
Table 1.
Comparison of patients with appendicitis before and during the COVID-19 pandemic, March 19-September 19.
| Variable | Pre-COVID (2019) n = 606 | During COVID (2020) n = 592 | P value |
|---|---|---|---|
| Hospital,n(%) | 0.008 | ||
| Valley Children's | 406 (67.0) | 436 (73.7) | |
| UC Davis | 104 (17.2) | 99 (16.7) | |
| UCLA | 63 (10.4) | 33 (5.6) | |
| Harbor-UCLA | 33 (5.5) | 24 (4.1) | |
| Race,n(%) | <0.0001 | ||
| White | 411 (67.8) | 467 (78.2) | |
| Black | 10 (1.7) | 14 (2.4) | |
| Asian | 23 (3.8) | 24 (4.0) | |
| Other or Unknown | 162 (26.7) | 92 (15.5) | |
| Age, years: median (IQR) | 10 (8-13) | 10 (7-13) | 0.84 |
| Male sex,n(%) | 375 (61.9) | 372 (62.8) | 0.73 |
| Insurance,n% | 0.62 | ||
| Public | 419 (69.1) | 424 (71.6) | |
| Private | 178 (29.4) | 161 (27.2) | |
| Other | 9 (1.5) | 7 (1.2) | |
| Symptom duration, days: median (IQR) | 2 (1-3) | 2 (1-3) | 0.90 |
| Initial WBC (x 103), median (IQR) | 15.5 (12.5-18.8) | 15.8 (12.6-18.8) | 0.57 |
| Imaging performed,n(%) | 0.002 | ||
| US only | 363 (59.9) | 315 (53.2) | |
| CT only | 158 (26.1) | 144 (24.3) | |
| US and CT | 83 (13.7) | 132 (22.3) | |
| Other | 2 (0.3) | 1 (0.2) | |
| Diagnosis,n(%) | 0.17 | ||
| Non-perforated | 361 (59.6) | 340 (57.4) | |
| Perforated | 245 (40.4) | 249 (42.1) | |
| Unable to determine | 0 (0) | 3 (0.5) | |
| Initial management,n(%) | <0.0001 | ||
| Operative | 553 (91.3) | 496 (83.8) | |
| Percutaneous drain | 24 (4.0) | 31 (5.2) | |
| Antibiotics alone | 29 (4.8) | 65 (11.0) | |
| Surgery on day of admission,n(%) | 447/553 (80.8) | 373/496 (75.2) | 0.03 |
| Surgical site infection,n(%) | 28/553 (5.1) | 14/496 (2.8) | 0.07 |
| Additional interventions | 27/606 (4.5) | 21/592 (3.6) | 0.42 |
| LOS, days: median (IQR) | 2 (1-4) | 3 (1-5) | <0.0001 |
| 30-day ED visits,n(%) | 40 (6.6) | 38 (6.4) | 0.90 |
| 30-day readmissions,n(%) | 17 (2.8) | 27 (4.6) | 0.11 |
CT = computed tomography; ED = Emergency Department; IQR = interquartile range; LOS = length of stay; US = ultrasound; WBC = white blood cell count; UC = University of California; UCLA = University of California Los Angeles.
Diagnosis and management
There was no difference in the rate of perforated appendicitis between groups (40.4% pre-COVID versus 42.1% COVID-era, P = 0.17). The proportion of children undergoing CT scans increased by 10% from 39.8% pre-COVID to 49.4% in the COVID-era cohort (P = 0.02). In the pre-COVID cohort, one patient underwent US and magnetic resonance imaging (MRI) and one patient underwent no imaging and was diagnosed by exam alone. One patient in the COVID-era cohort was diagnosed by MRI alone.
The rate of operative management was significantly lower in the COVID-era cohort (91.3% pre-COVID versus 83.8% COVID-era, P < 0.0001). In the COVID-era cohort, 16.2% of patients underwent non-operative management with either percutaneous drain or antibiotics alone, compared to 8.8% of patients in the pre-COVID cohort (P < 0.0001). Additionally, patients were less likely to undergo surgery on the day of admission in the COVID-era cohort (80.8% pre-COVID versus 75.2% COVID-era, P = 0.03).
Overall outcomes
LOS was longer in the COVID-era cohort (median 2 days pre-COVID versus 3 days COVID-era, P < 0.0001). Although there were fewer SSIs in the COVID-era cohort, this did not reach statistical significance (5.1% pre-COVID versus 2.8% COVID-era, P = 0.07). There was no difference in 30 day ED visits. Thirty-day readmissions were slightly higher in the COVID-era cohort, but this was not statistically significant (2.8% pre-COVID versus 4.6% COVID-era, P = 0.11).
Sub-group analysis of patients by perforated versus non-perforated appendicitis
There were 494 patients with perforated appendicitis: 245 in the pre-COVID cohort and 249 in the COVID-era cohort (Table 2 ). The median symptom duration prior to presentation was two days in each group (P = 0.38). There was a higher rate of non-operative management in the COVID-era cohort (15.1% pre-COVID versus 25.5% COVID-era, P = 0.002). Patients in the COVID-era cohort had a longer LOS (median 5 days pre-COVID versus 6 days COVID-era, P < 0.0001). There were no differences in SSIs, ED visits, or readmissions.
Table 2.
Comparison of pediatric patients with perforated appendicitis before and during the COVID-19 pandemic, March 19 – September 19.
| Variable | Pre-COVID (2019) n = 245 | During COVID (2020) n = 249 | P value |
|---|---|---|---|
| Hospital,n(%) | 0.12 | ||
| Valley Children's | 181 (73.9) | 203 (81.5) | |
| UC Davis | 43 (17.6) | 36 (14.5) | |
| UCLA | 14 (5.7) | 7 (2.8) | |
| Harbor-UCLA | 7 (2.9) | 3 (1.2) | |
| Race,n(%) | 0.004 | ||
| White | 179 (73.1) | 202 (81.1) | |
| Black | 6 (2.5) | 5 (2.0) | |
| Asian | 4 (1.6) | 12 (4.8) | |
| Other or Unknown | 56 (22.9) | 30 (12.5) | |
| Age, years: median (IQR) | 9 (6-13) | 9 (6-12) | 0.84 |
| Male sex,n(%) | 150 (61.2) | 156 (62.7) | 0.74 |
| Insurance,n(%) | 0.29 | ||
| Public | 176 (71.8) | 187 (75.1) | |
| Private | 67 (27.4) | 62 (24.9) | |
| Other | 2 (0.8) | 0 (0) | |
| Transfer,n(%) | 125 (51.0) | 126 (50.6) | 0.93 |
| Symptom duration, days: median (IQR) | 2 (1-4) | 2 (2-4) | 0.38 |
| Initial WBC (x 103), median (IQR) | 17.0 (14-21) | 16.6 (13.5-20.3) | 0.46 |
| Imaging performed,n(%) | 0.31 | ||
| US only | 133 (54.3) | 122 (49.0) | |
| CT only | 67 (27.4) | 64 (25.7) | |
| US and CT | 44 (18.0) | 62 (24.9) | |
| Other | 1 (0.4) | 1 (0.4) | |
| CT scan performed,n(%) | 111 (45.3) | 126 (50.6) | 0.24 |
| Initial management,n(%) | 0.002 | ||
| Operative | 208 (84.9) | 183 (73.5) | |
| Percutaneous drain | 24 (9.8) | 31 (12.5) | |
| Antibiotics alone | 13 (5.3) | 35 (14.1) | |
| Surgery on day of admission,n(%) | 166/208 (79.8) | 140/183 (76.5) | 0.43 |
| SSI,n(%) | 25/208 (12.0) | 13/183 (7.1) | 0.10 |
| Additional interventions,n(%) | 26/245 (10.6) | 20/249 (8.0) | 0.32 |
| LOS, days: median (IQR) | 5 (3-7) | 6 (4-8) | <0.0001 |
| 30-day ED visits,n(%) | 21 (8.6) | 23 (9.2) | 0.80 |
| 30-day readmissions,n(%) | 10 (4.1) | 16 (6.4) | 0.24 |
CT = computed tomography; ED = Emergency Department; IQR = interquartile range; LOS = length of stay; UC = University of California; UCLA = University of California Los Angeles; US = ultrasound; SSI = surgical site infection; WBC = white blood cell count.
When comparing patients with non-perforated acute appendicitis, there were again no significant differences in presenting characteristics (Table 3 ). The median symptom duration was one day in each group (P = 0.11). The use of CT in addition to US doubled (10.9% pre-COVID versus 20.6% COVID-era, P = 0.0003 for both). A slightly higher proportion of patients underwent non-operative management with antibiotics alone, but this did not reach statistical significance (4.4% pre-COVID versus 7.9% COVID-era, P = 0.05). Although the median LOS was one day for both cohorts, there was significantly increased variability in the interquartile ranges, with more patients having longer LOS in the COVID-era cohort (IQR 1-1 pre-COVID versus 1-2 COVID-era, P < 0.0001). There were no differences in SSIs, ED visits, or readmissions.
Table 3.
Comparison of pediatric patients with non-perforated acute appendicitis before and during the COVID-19 pandemic, March 19 – September 19.
| Variable | Pre-COVID (2019) n = 361 | During COVID (2020) n = 340 | P value |
|---|---|---|---|
| Hospital,n(%) | 0.07 | ||
| Valley Children's | 225 (62.3) | 230 (67.7) | |
| UC Davis | 61 (16.9) | 63 (18.5) | |
| UCLA | 49 (13.6) | 26 (7.7) | |
| Harbor-UCLA | 26 (7.2) | 21 (6.2) | |
| Race,n(%) | 0.001 | ||
| White | 232 (64.3) | 257 (75.6) | |
| Black | 4 (1.1) | 9 (2.7) | |
| Asian | 19 (5.3) | 12 (3.5) | |
| Other or Unknown | 106 (29.4) | 62 (18.2) | |
| Age, years: median (IQR) | 11 (8-14) | 11 (8-14) | 0.56 |
| Male sex,n(%) | 225 (62.3) | 213 (62.7) | 0.93 |
| Insurance,n(%) | 0.89 | ||
| Public | 243 (67.3) | 234 (68.8) | |
| Private | 111 (30.8) | 99 (29.1) | |
| Other | 7 (1.9) | 7 (2.1) | |
| Transfer,n(%) | 141 (39.1) | 131 (38.5) | 0.89 |
| Symptom duration, days: median (IQR) | 1 (1-2) | 1 (1-2) | 0.11 |
| Initial WBC (x 103), median (IQR) | 14.7 (11.7-17.2) | 15.3 (12.3-17.4) | 0.15 |
| Imaging performed,n(%) | 0.003 | ||
| US only | 230 (63.7) | 190 (55.9) | |
| CT only | 91 (25.2) | 80 (23.5) | |
| US and CT | 39 (10.9) | 70 (20.6) | |
| Exam only | 1 (0.3) | 0 (0) | |
| CT scan performed,n(%) | 130 (36.0) | 150 (44.1) | 0.03 |
| Initial management,n(%) | 0.05 | ||
| Operative | 345 (95.6) | 313 (92.1) | |
| Antibiotics alone | 16 (4.4) | 27 (7.9) | |
| Surgery on day of admission,n(%) | 281/345 (81.5) | 233/313 (74.4) | 0.03 |
| SSI,n(%) | 3/345 (0.9) | 1/313 (0.3) | 0.63 |
| Additional interventions,n(%) | 1/361 (0.3) | 0 (0) | 1.00 |
| LOS, days: median (IQR) | 1 (1-1) | 1 (1-2) | <0.0001 |
| 30-day ED visits,n(%) | 19 (5.3) | 14 (4.1) | 0.47 |
| 30-day readmissions,n(%) | 7 (1.9) | 10 (2.9) | 0.47 |
CT = computed tomography; ED = Emergency Department; IQR = interquartile range; LOS = length of stay; UC = University of California; UCLA = University of California Los Angeles; US = ultrasound; SSI = surgical site infection; WBC = white blood cell count.
Sub-group analysis by time
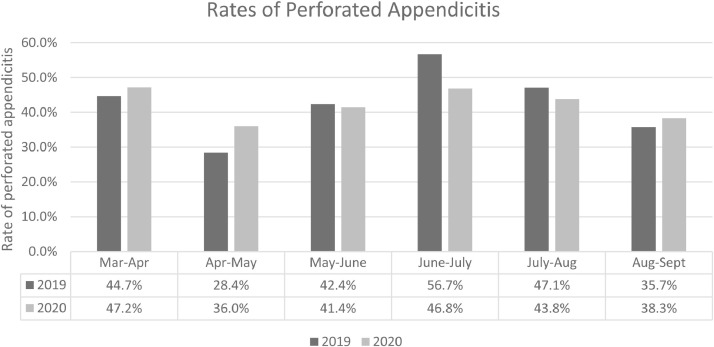
Analyzed by month, there was no significant difference in the primary outcome of rate of perforated appendicitis (Fig. 1 ). In the first three months (March to June) and latter three months (July-September), the rate of perforated appendicitis was similar between the two cohorts (March to June: 38.5% pre-COVID versus 41.3% COVID-era, P = 0.50; July-September: 45.8% pre-COVID versus 43.2% COVID-era, P = 0.52). To account for potential changing patterns of presentation and management over the evolving course of the pandemic, patients presenting in the first three months and latter three months of the study period were analyzed separately.
Fig. 1.
Rate of perforated appendicitis by month, pre-COVID (2019) versus COVID-era (2020). There were no statistically significant differences by month. P values as follows: March to April, P = 0.77; April to May, P = 0.29; May to June, P = 1.00; June to July, P = 0.67; July to August, P = 0.68; August to September, P = 0.77.
In the first three months following the Shelter in Place order (March 19 to June 18), there were similar overall numbers of patients presenting with acute appendicitis (283 pre-COVID and 289 during COVID) (Table 4 ). There were no differences between cohorts with the exception of increased utilization of CT scans, with 37.1% of patients in the pre-COVID cohort undergoing CT scan compared to 45.6% in the COVID-era cohort (P = 0.04). There was no difference in rates of operative management (90.8% pre-COVID versus 88.2% COVID-era, P = 0.59). Patients underwent surgery on the day of admission with equal rates in both cohorts (82%). There was no difference in SSIs, but there were lower rates of additional interventions in the COVID-era cohort. Additional interventions (n = 14) in the pre-COVID cohort included 6 drain placements into post-operative abscesses, 5 drain placements into recurrent abscesses following initial percutaneous drain placement, one abscess aspiration followed by surgery, one re-operation, and one failure of percutaneous drainage requiring appendectomy. In the COVID-era cohort, there were five additional interventions needed, all of which were drain placements. Four of the five were in post-operative abscesses, and one was in a patient who failed management with antibiotics alone. LOS was similar between groups (median 2 days in both, P = 0.42), and there were similar rates of ED visits and readmissions.
Table 4.
Comparison of pediatric patients with appendicitis before and during the COVID-19 pandemic, separated into first three-month period (March 19 – June 18) and second three-month period (June 19 – September 19).
| Variable | First Three Months March 19 – June 18 |
Second Three Months June 19 – September 19 |
||||
|---|---|---|---|---|---|---|
| Pre-COVID 2019 | During COVID 2020 | P value | Pre-COVID 2019 | During COVID 2020 |
P value | |
| n = 283 | n = 289 | n = 323 | n = 303 | |||
| Hospital,n(%) | 0.04 | 0.16 | ||||
| Valley Children's | 185 (65.4) | 207 (71.6) | 221 (68.4) | 229 (75.6) | ||
| UC Davis | 50 (17.7) | 56 (19.4) | 54 (16.7) | 43 (14.2) | ||
| UCLA | 32 (11.3) | 16 (5.5) | 31 (9.6) | 17 (5.6) | ||
| Harbor-UCLA | 16 (5.7) | 10 (3.5) | 17 (5.3) | 14 (4.6) | ||
| Race,n(%) | 0.36 | <0.0001 | ||||
| White | 206 (72.8) | 224 (77.5) | 205 (63.5) | 238 (78.6) | ||
| Black | 6 (2.1) | 9 (3.1) | 4 (1.2) | 5 (1.7) | ||
| Asian | 12 (4.2) | 11 (3.8) | 11 (3.4) | 13 (4.3) | ||
| Other or Unknown | 59 (20.9) | 45 (15.6) | 103 (31.9) | 47 (15.5) | ||
| Age, years: median (IQR) | 10.0 (8.0-14.0) | 10.0 (7.0-13.0) | 0.25 | 10 (7-13) | 10 (8-14) | 0.17 |
| Male sex,n (%) | 176 (62.2) | 183 (63.3) | 0.78 | 199 (61.6) | 189 (62.4) | 0.84 |
| Insurance,n(%) | 0.31 | 0.20 | ||||
| Public | 204 (72.1) | 206 (71.3) | 215 (66.6) | 218 (72.0) | ||
| Private | 73 (25.8) | 81 (28.0) | 105 (32.5) | 80 (26.4) | ||
| Other | 6 (2.1) | 2 (0.7) | 3 (0.9) | 5 (1.7) | ||
| Transfer,n(%) | 122 (43.1) | 127 (43.9) | 0.84 | 144 (44.6) | 131 (43.2) | 0.73 |
| Symptom duration, days: median (IQR) | 1 (1-2) | 2 (1-3) | 0.60 | 2 (1-3) | 2 (1-3) | 0.78 |
| Initial WBC (x 103), median (IQR) | 15.0 (12.5-18.5) | 16.1 (12.9-19.1) | 0.13 | 15.6 (12.4-18.9) | 15.5 (12.5-17.8) | 0.54 |
| Imaging performed,n(%) | 0.008 | 0.12 | ||||
| US only | 178 (62.9) | 157 (54.3) | 185 (57.3) | 158 (52.2) | ||
| CT only | 66 (23.3) | 63 (21.8) | 92 (28.5) | 81 (26.7) | ||
| US and CT | 39 (13.8) | 69 (23.9) | 44 (13.6) | 63 (20.8) | ||
| Other | 0 (0) | 0 (0) | 2 (0.6) | 1 (0.3) | ||
| CT scan performed,n(%) | 105 (37.1) | 132 (45.6) | 0.04 | 136 (42.1) | 144 (47.5) | 0.17 |
| Diagnosis,n(%) | 0.46 | 0.20 | ||||
| Non-perforated | 174 (61.5) | 169 (58.5) | 187 (57.9) | 171 (56.4) | ||
| Perforated | 109 (38.5) | 120 (41.5) | 136 (41.1) | 129 (42.6) | ||
| Unable to determine | 0 (0) | 0 (0) | 0 (0) | 3 (1.0) | ||
| Initial management,n(%) | 0.59 | <0.0001 | ||||
| Operative | 257 (90.8) | 255 (88.2) | 296 (91.6) | 241 (79.5) | ||
| Percutaneous drain | 13 (4.6) | 18 (6.2) | 11 (3.4) | 13 (4.3) | ||
| Antibiotics alone | 13 (4.6) | 16 (5.5) | 16 (5.0) | 49 (16.2) | ||
| Surgery on day of admission,n(%) | 210/257 (81.7) | 208/255 (81.6) | 0.99 | 237/296 (80.1) | 165/241 (68.5) | 0.002 |
| SSI,n(%) | 14/257 (5.5) | 6/255 (2.4) | 0.11 | 14/296 (4.7) | 8/241 (3.3) | 0.51 |
| Additional interventions,n(%) | 14/283 (5.0) | 5/289 (1.7) | 0.04 | 13/323 (4.0) | 16/303 (5.3) | 0.57 |
| LOS, days: median (IQR) | 2 (1-4) | 2 (1-5) | 0.42 | 2 (1-4) | 3 (2-6) | <0.0001 |
| 30-day ED visits,n(%) | 21 (7.4) | 15 (5.2) | 0.27 | 19 (5.9) | 23 (7.6) | 0.43 |
| 30-day readmissions,n(%) | 9 (3.2) | 13 (4.5) | 0.41 | 8 (2.5) | 14 (4.6) | 0.19 |
CT = computed tomography; ED = Emergency Department; IQR = interquartile range; LOS = length of stay; SSI = surgical site infection; UC = University of California; UCLA = University of California Los Angeles; US = ultrasound; WBC = white blood cell count.
In the second three months following the Shelter in Place order, patients’ presenting characteristics were similar (Table 4). There were significantly higher rates of non-operative management in the COVID-era cohort (8.4% pre-COVID versus 20.5% COVID-era, P < 0.0001). Additionally, patients undergoing operative intervention were significantly less likely to do so on the day of admission (80.1% pre-COVID versus 68.5% COVID-era, P = 0.002). Hospital LOS was longer in the COVID-era cohort (median 2 days pre-COVID versus 3 days COVID-era, P = 0.04), but there were no differences in SSIs, ED visits, or readmissions.
Hospital-level comparison
Lastly, the main outcomes were analyzed by hospital to account for any hospital-level variation (Table 5 ). There was no difference in the rate of perforated appendicitis at any participating institution when comparing pre-COVID cohorts to COVID-era cohorts. Duration of symptoms prior to presentation was similar in both cohorts at all institutions. Non-operative management increased at three of the four institutions, but only one was statistically significant.
Table 5.
Main outcomes analyzed by hospital.
| Hospital | Pre-COVID 2019 | During COVID 2020 | P value |
|---|---|---|---|
| Valley Children's | |||
| Perforated appendicitis, n (%) | 181/406 (44.6) | 203/433 (46.9) | 0.50 |
| Duration of symptoms, days: median (IQR) | 2 (1-3) | 2 (1-3) | 0.82 |
| Non-operative management, n (%) | 33/406 (8.1) | 74/433 (17.1) | 0.0001 |
| UC Davis | |||
| Perforated appendicitis, n (%) | 43/104 (41.4) | 36/99 (36.4) | 0.47 |
| Duration of symptoms, days: median (IQR) | 2 (1-3) | 2 (1-3) | 0.18 |
| Non-operative management, n (%) | 5/104 (4.8) | 10/99 (10.1) | 0.18 |
| UCLA | |||
| Perforated appendicitis, n (%) | 14/63 (22.2) | 7/33 (21.2) | 1.00 |
| Duration of symptoms, days: median (IQR) | 2 (1-2) | 1 (1-2) | 0.11 |
| Non-operative management, n (%) | 8/63 (12.7) | 7/33 (21.2) | 0.38 |
| Harbor-UCLA | |||
| Perforated appendicitis, n (%) | 7/33 (21.2) | 3/24 (12.5) | 0.49 |
| Duration of symptoms, days: median (IQR) | 2 (1-3) | 1 (1-2) | 0.05 |
| Non-operative management, n (%) | 7/33 (21.2) | 2/24 (8.3) | 0.28 |
Discussion
In this statewide, multicenter longitudinal study of pediatric patients with acute appendicitis during the COVID-19 pandemic, we found similar rates of perforated appendicitis pre-COVID and in the COVID-era cohorts. There did not appear to be a delay in presentation based on duration of symptoms prior to presentation, refuting our initial hypothesis. The use of CT imaging for diagnosis increased, particularly in the first half of the study period and for patients with non-perforated appendicitis. Non-operative management with percutaneous drainage or antibiotics alone became more common, primarily in the latter half of the study period. On sub-group analysis by diagnosis, non-operative management increased for both perforated and non-perforated appendicitis. The proportion of patients undergoing surgery on the day of admission decreased, especially in the latter half of the study period, and for non-perforated appendicitis. There was an increase in hospital LOS primarily in the second half of the study period, and most apparent among children with perforated appendicitis. Overall, there were no increases in post-operative complications including SSIs, 30 day ED visits, and readmissions.
Our findings differ from those published regarding rates of perforated appendicitis among children and adolescents during the COVID-19 pandemic, which have mostly found increased rates of perforation, thought to be due to delays in presentation. One study by Gerall et al evaluated rates of perforated appendicitis over three months from March 1 to May 31 of 2020, comparing to the same period in 2019, finding a significantly increased rate of perforation (41.7% versus 9.8% the year prior, P < 0.001) and a longer median symptom duration prior to presentation (2 versus 1 day).9 There was a much lower rate of operative management (75.0% versus 92.7%) during the pandemic. However, this was a single-center study of only 89 patients. Additionally, it was performed at a tertiary care children's hospital in New York City at the peak of the pandemic, a region hit particularly hard by COVID-19.10 A second single-center study from the New York metropolitan region of 55 pediatric patients with appendicitis from March 31 to May 3, 2020 compared outcomes to the same period in the three preceding years, finding similar rates of perforated appendicitis between cohorts.11 One study of 160 patients from Northern Virginia analyzed differences in outcomes over a similar time period (March 16 to June 7), compared to the same period in 2019, and found twice as many cases of perforated appendicitis during the pandemic (39% versus 19%, P = 0.009).5 In the first multicenter study of pediatric appendicitis outcomes during COVID, a total of 55 children treated at three NYC-area hospitals March 1 to May 7, 2020 were compared to 1291 patients treated over five years prior from January 1, 2014 to June 1, 20194. The perforation rate was significantly higher during the COVID era (45% versus 27%, P = 0.005), and patients presented after a longer symptom duration (3 versus 2 days, P = 0.001).
In contrast, we found no difference in perforation rates over a 6-month period at four major children's hospitals across the state of California in the six months following the first statewide Shelter in Place order. The spread of COVID-19 in California during the study period differs from that of the New York metropolitan region, which was hit particularly in the early months. During the study period, the peak of COVID-19 cases in California occurred in July to August 2020, with the highest reported new cases per day of approximately 12,000 cases on July 22, 2020. In contrary, the peak of the COVID-19 surge in the New York metropolitan area was early, in April 2020, with a peak of approximately 12,000 cases on April 4, 2020. In comparison, by July to August of 2020, new cases in New York City ranged from 500 to 800 per day.12 California was relatively spared in the beginning of the pandemic, although that has since changed, with the highest number of cases in the US being diagnosed in California at the time of this writing. However, the relatively few California cases in the first six months of the pandemic may partially explain our finding that children did not present after significant delays and did not have higher rates of perforated appendicitis.
Despite this, there were significant differences in patient management during the COVID-19 pandemic compared to the year prior. Although none of the included hospitals protocolized a change in the management of acute appendicitis during the pandemic, non-operative management by use of percutaneous drains or antibiotic treatment doubled over the 6 month period from 8.8% to 16.2%. On sub-group analysis by time, this change did not occur until June-September, at which point 20.5% of patients were undergoing non-operative management. Studies out of New York also reported a decrease in operative management during the COVID-19 pandemic of similar magnitude.9 In our study, this shift was noted in both patients with perforated and non-perforated appendicitis. Additionally, patients were less likely to undergo surgery on the day of admission, decreasing from 80.1% to 68.5% of patients during the latter half of the study period. The peak in cases in California during this study period occurred during the latter three months, which may partially explain the increase in non-operative management, lower proportion of patients undergoing surgery on the day of admission, and longer LOS. This may be due to strained hospital resources, or the waiting period between sending a required COVID-19 test prior to surgery and the results becoming available.
We found that CT imaging increased during the study period, which on sub-group analysis by diagnosis, remained significant only for non-perforated appendicitis. Additionally, on sub-group analysis by time for all patients, the increased utilization of CTs was significant only in the first three months of the pandemic. This has not been studied in prior publications on the effect of COVID-19 on pediatric patients with appendicitis. In children, ultrasound is the initial imaging modality of choice for the evaluation of abdominal pain, as it may provide a diagnosis while limiting exposure to ionizing radiation. Wide variations in the use of CT in diagnosing appendicitis in children have been reported, with lower rates at children's hospitals compared to referring hospitals.13 , 14 However, rates of transferred patients were similar in the pre-COVID and COVID-era cohorts included in this study, so the increase in CT utilization was not due to increased scanning by referring hospitals alone. We hypothesize that the reason for increased CT scan utilization in patients with acute non-perforated appendicitis may have been related to attempts to avoid hospitalization for serial abdominal exams to clinically ‘rule out’ acute appendicitis following an equivocal ultrasound study. This may be due to efforts to reduce hospital resource utilization in anticipation of COVID-19 surges, or to have a definitive diagnosis due to parental reluctance to be admitted for a clinical appendicitis rule-out. However, from medical record documentation we are not able to discern the underlying reason. Although patient-level cost data was not collected in this study, based on an average hospital charge of $266 per abdominal CT scan, the noted 10% increase in CT utilization in the COVID-era cohort was the equivalent of an additional 41 patients undergoing CT scans, with an associated total additional estimated cost of $10,906.
Lastly, we found that outcomes were largely unchanged during the study period, with the exception of LOS which was one day longer in the pandemic compared to the pre-COVID cohort. This was most notable during the latter half of the study period, and in patients with perforated appendicitis. Other studies have variably reported increased LOS9 or no changes compared to cases pre-COVID.4 There are several potential reasons for our noted increase in LOS. The previous finding of decreased rates of surgery on day of admission likely contributed to increases in LOS. Additionally, as the pandemic progressed, hospitals instituted mandatory COVID-19 tests on admission, and prior to any interventions under anesthesia. The increase in LOS is likely in part due to delays in treatment related to pending COVID-19 tests. As the average charge for a single day of a pediatric ward hospitalization is $12,202, an increase from a median LOS of two days to three days is associated with an additional potential $12,202 minimum of charges, not accounting for additional inpatient expenses such as medications and supplies needed in the course of a day of patient care. The economic impact of this increase is significant considering the prevalence of acute appendicitis in the pediatric population. Despite these differences, however, there were no significant changes in post-operative SSIs, ED visits, or readmissions during the COVID-era study period.
Our study has several limitations. The four hospitals included represent a diverse set of institutions, and management of appendicitis was not standardized across institutions. However, the primary outcomes of interest did not differ between hospitals as noted in Table 4. By performing this large multicenter study, we were able to analyze the effect of the COVID-19 pandemic on nearly 1,200 pediatric patients with acute appendicitis, a cohort several times larger than any previously reported. Although rates of COVID may vary within the state of California, Shelter in Place orders have generally been implemented in a statewide manner, impacting all Californians simultaneously, thus supporting a study of effects at multiple hospitals across the state rather than at an institutional or municipal level. It should be noted that not all pediatric hospitals in California were included, and thus these results may not be generalizable to the entire state. Cost data was not collected on a patient-level, but an average hospital charge for CT scans and inpatient hospital days is presented for context to provide an estimate of the potential excess costs associated with these findings. We did not collect data on COVID-19 testing for this cohort, which limits our ability to draw any conclusions about outcomes of COVID-positive patients. However, there is some data to suggest that children with COVID-19 infection have similar presentations and outcomes as those without.4 , 15 Lastly, as the COVID-19 pandemic continues to evolve, the presentation and management of pediatric patients with acute appendicitis may shift as well and should continue to be studied.
Conclusion
In this statewide multicenter longitudinal study of pediatric patients with acute appendicitis, there was no increase in rates of perforated appendicitis during the first six months of the COVID-19 pandemic. Use of CT imaging for diagnosis and rates of non-operative management rose during the study period, with delayed operative management compared to one year prior, which was associated with an overall increase in length of stay by one day. There were no increases in post-operative complications or ED visits. As the pandemic continues and even worsens in many parts of the country, the systems-wide effects on other acute medical and surgical conditions should continue to be studied to ensure care does not suffer.
Author Contributions
Drs. Theodorou, Beres, and Brown conceived of and designed the study. Drs. Theodorou, Nguyen, Castle, Faltermeier, and Tung performed data collection. Drs. Theodorou performed data analaysis. Drs. Theodorou, Beres, Nguyen, Castle, Faltermeier, Shekherdimian, Tung, DeUgarte, and Brown interpreted the data. Dr. Theodorou drafted the manuscript. Drs. Theodorou, Beres, Nguyen, Castle, Faltermeier, Shekherdimian, Tung, DeUgarte, and Brown critically revised the manuscript.
Acknowledgment
The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant number UL1 TR001860 for authors CT and EB The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Disclosure
None.
References
- 1.Wu JT, Daniel H, Glover MJ, Henry S, Wood D, Rubin DL. Changes in cancer management due to COVID-19 illness in patients with cancer in Northern California. JCO Oncol Pr. 2021;17:e377–e385. doi: 10.1200/OP.20.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kumaira Fonseca M, Trindade EN, Costa Filho OP, Nácul MP, Seabra AP. Impact of COVID-19 outbreak on the emergency presentation of acute appendicitis. Am Surg. 2020 doi: 10.1177/0003134820972098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee-Archer P, Blackall S, Campbell H, Boyd D, Patel B, McBride C. Increased incidence of complicated appendicitis during the COVID-19 pandemic. J Paediatr Child Health. 2020;56:1313–1314. doi: 10.1111/jpc.15058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fisher JC, Tomita SS, Ginsburg HB, Gordon A, Walker D, Kuenzler KA. Increase in pediatric perforated appendicitis in the New York City Metropolitan Region at the Epicenter of the COVID-19 outbreak. Ann Surg. 2020 doi: 10.1097/sla.0000000000004426. Publish Ah(Xx) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Place R, Lee J, Howell J. Rate of pediatric appendiceal perforation at a children's hospital during the COVID-19 pandemic compared with the previous year. JAMA Netw open. 2020;3 doi: 10.1001/jamanetworkopen.2020.27948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deng Y, Chang DC, Zhang Y, Webb J, Gabre-Kidan A, Abdullah F. Seasonal and day of the week variations of perforated appendicitis in US children. Pediatr Surg Int. 2010;26:691–696. doi: 10.1007/s00383-010-2628-z. [DOI] [PubMed] [Google Scholar]
- 7.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inf. 2019;95 doi: 10.1016/j.jbi.2019.103208.The. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gerall CD, DeFazio JF, Kahan AM, et al. Delayed presentation and sub-optimal outcomes of pediatric patients with acute appendicitis during the COVID-19 pandemic. J Pediatr Surg. 2020 doi: 10.1016/j.jpedsurg.2020.10.008. (Iii) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosenberg E, Dufort EM, Blog DS, Hall EW. COVID-19 testing, epidemic features, hospital outcomes, and household prevalence, New York-March 2020. Clin Infect Dis. 2020;5(71):1953–1959. doi: 10.1093/cid/ciaa549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kvasnovsky CL, Shi Y, Rich BS, et al. Limiting hospital resources for acute appendicitis in children: lessons learned from the U.S. epicenter of the COVID-19 pandemic. J Pediatr Surg. 2020:6–10. doi: 10.1016/j.jpedsurg.2020.06.024. (xxxx) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Allen Jordan, Almukhtar Sarah, Aufrichtig Aliza, Barnard Anne, Bloch Matthew, et al. Coronavirus in the U.S.: Latest Map and Case Count. New York Times. 2021 https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html.Published2020 Available at: [Accessed 6 February 2020] [Google Scholar]
- 13.Glass CC, Saito JM, Sidhwa F, et al. Diagnostic imaging practices for children with suspected appendicitis evaluated at definitive care hospitals and their associated referral centers. J Pediatr Surg. 2016;51:912–916. doi: 10.1016/j.jpedsurg.2016.02.055. [DOI] [PubMed] [Google Scholar]
- 14.Jones RE, Gee KM, Preston SC, Babb JL, Beres AL. Diagnostic utilization and accuracy of pediatric appendicitis imaging at adult and pediatric centers. J Surg Res. 2019;240:97–103. doi: 10.1016/j.jss.2019.02.047. [DOI] [PubMed] [Google Scholar]
- 15.Mehl SC, Loera JM, Shah SR, et al. Favorable postoperative outcomes for children with COVID-19 infection undergoing surgical intervention : Experience at a free-standing children’s hospital. J Pediatr Surg. 2021:1–8. doi: 10.1016/j.jpedsurg.2021.01.033. (xxxx) [DOI] [PMC free article] [PubMed] [Google Scholar]