Abstract
Objectives
Prior studies have examined sleep during the coronavirus disease 2019 (COVID-19) pandemic, but have few compared sleep measured both during and prior to COVID. We examined the impact of the COVID-19 pandemic on subjective sleep quality in general and separately by gender and age (<50 vs. ≥50 years). Further, we compared sleep quality between those who did and did not follow quarantine orders.
Methods
This sample is from the Baependi Heart Study, a family-based cohort of adults in South-eastern Brazil. Longitudinal data were from 417 individuals who completed the Pittsburgh Sleep Quality Index (PSQI) twice: between January 2010 and September 2014 (pre-COVID) and during the COVID-19 stay-at-home order March-June, 2020. Cross-sectional analysis included 800 participants.
Results
Mean (±SD) PSQI scores were significantly higher during than before COVID-19 (5.7 ± 3.8 vs. 5.0 ± 3.3, p < .01). This increase was significant among women and among adults ≥50 years but not in men or younger adults. The significant increase in PSQI was only observed in those who quarantined during COVID-19 (5.9 ±3.7 vs. 5.2 ±3.4, p < .01) and not those who did not quarantine (5.0 ± 3.7 vs. 4.5 ± 3, p = .12). In cross-sectional analyses, individuals who quarantined had higher PSQI scores than nonquarantined individuals (6.1 ± 3.9 vs. 5.0 ± 3.5, p < .01). The quarantine status-dependent differences were significant for women (6.4 ± 4 vs. 5.2 ± 3.7, p < .01) and older adults (6.6 ± 0.1 vs. 5.5 ± 3.3, p = .04). Differences by quarantine status were attenuated after adjusting for age and gender.
Conclusions
Subjective sleep quality declined during the COVID-19 pandemic, particularly among women, older adults, and those compliant to quarantine orders.
Keywords: Coronavirus, insomnia, lockdown, SARS-CoV2, self-quarantine
Introduction
During the coronavirus (COVID-19) pandemic, governments across the world established preventive measures, such as self-isolation and stay-at-home or quarantine orders (hereafter referred to as “quarantine”) to combat the spread of the virus. Potential consequences of this confinement and the pandemic include restricted social interactions, concerns about the disease and the health of family and oneself, and potential economic impact on one's household or community. Quarantine can also limit physical activity due to the closure of gyms and the shift to remote schooling and work. It could also increase daily screen time, which could impair sleep by exposure to blue light.1 Lastly, since quarantine involves avoidance of non-essential social interaction and staying home, it may reduce sunlight exposure, which is an important regulator of circadian rhythms.2 All of these environmental, behavioral, and psychological factors could negatively impact sleep quality. Healthy sleep is associated with better overall health, including better immune function,3 , 4 and, consequently, worse sleep due to quarantine could weaken the immune response and increase the risk of COVID-19 infection and severity.5 Thus, if quarantine orders negatively impact sleep quality, this has implications for general health.
Impaired sleep has been associated with the pandemic in some cross-sectional studies from various countries, including China, Italy, Canada, France, and the United States.1 , 6, 7, 8, 9, 10, 11, 12, 13 Some studies examined changes in sleep quality from prior to and during the pandemic; however, the majority relied on retrospective reports of sleep quality,14, 15, 16, 17, 18, 19 which is subject to recall bias. A longitudinal approach enables comparisons of sleep quality measured both before and during the pandemic, but there have only been a few such studies. One study in the United States reported that sleep duration increased.20 Two studies assessed sleep quality right before (February 2020) and shortly after the pandemic began (late March or April 2020). One reported worse sleep quality during the pandemic,21 while the other study observed no significant change in sleep quality.22 Thus, these 3 longitudinal studies had inconsistent results.
Sleep quality is well known to vary by both age and gender. Women are more likely to develop insomnia symptoms than men and insomnia symptoms and sleep disturbances become more prevalent at older ages.23 If women or older adults are more susceptible to sleep disturbances in general, their sleep quality may be more vulnerable to the effects of quarantine and the pandemic. Some prior studies have reported gender differences in the association between the pandemic and sleep, including worse sleep among women compared to men.6 , 7 , 11 , 21 Two studies compared sleep during the pandemic between age groups, but they dichotomized age at 30 or 35 years of age,6 , 10 which is younger than the age at which sleep disturbances typically increase.
The aim of our study was to examine the impact of the COVID-19 pandemic on subjective sleep quality and to determine if sleep quality differed between those who followed quarantine orders and those who did not. Further, given established gender and age effects on sleep quality, we examined these associations separately for men and women and younger (<50 years) and older (≥50 years) adults. This study involved participants from the Baependi Heart Study (BHS), an ongoing, family-based cohort in the rural town, Baependi, Brazil. Participants completed an assessment of subjective sleep quality several years prior to the pandemic and again shortly after the quarantine order was established.
Participants and methods
Sample
This sample is from the BHS, an ongoing family-based cohort study that was established in 2005 to characterize the determinants of cardiovascular health. Probands were residents of Baependi, a small rural town with approximately 19,249 inhabitants in 2021 located in the state of Minas Gerais, Brazil.24 Nearly one-third of households are located in the rural area.24 The most recent Human Development Index in Baependi dates from 2010 and was lower than the national index (Human Development Index = 0.681 vs. 0.724).24 Residents of Baependi had a lower average monthly income than the national average (R$867 vs. R$1,202) and a lower proportion of children 6-16 years in school (96% vs. 97.2%); however, life expectancy was higher in Baependi than nationally (74.9 vs. 73.5 years).24 Participants in the BHS were recruited based on a random selection of district census and households. Once a residence within a district was selected, one resident aged 18 years or older was invited to participate in the study, followed by their first-degree relatives and then increasingly more distant relatives. At baseline in 2005, the study evaluated 1691 individuals across 95 families, and subsequent waves added new participants for a current sample of 3675 participants who have participated in the study. Recruitment process has been described previously.25 This study protocol conformed to international ethics standards based on the Declaration of Helsinki and was approved by the local ethics committee (Hospital das Clínicas – Universidade de São Paulo, Brazil). Participants gave informed consent at all assessment periods.
Cross-sectional sample
For the present study, there were 2 relevant data collection periods. Most recently, we recruited BHS participants between March 30 and June 29, 2020, which was during the quarantine order issued by the municipal government on March 23, 2020. During the quarantine order, which had no pre-established end date, residents were advised to leave their homes only for essential purposes, such as grocery shopping, pharmacy, doctor's appointments, etc. The use of masks was mandatory and those residents who were not compliant had to pay a fee. The essential businesses that remained open during lockdown had to follow sanitation protocols. Despite having only 3 cases and 0 deaths of COVID-19 at the time of data collection, the quarantine order was its most stringent in Baependi.26 On April 22, 2020, some of the restrictions were lifted in order to reopen retail stores. These businesses had to work at minimum capacity (25%) in addition to abidance by the sanitation protocols. All data collection took place during the quarantine order. Study participants completed a survey over the phone. All BHS participants were considered eligible for the telephone survey. We divided the full sample into 5 equal lists, one for each interviewer, who attempted calls in alphabetical order. Interviewers attempted to call 1800 participants, interviewed 872 participants and 800 participants provided complete data, which constituted the cross-sectional COVID-19 sample.
Longitudinal sample
The pre-COVID-19 data collection occurred between January 2010 and September 2014 when the participants in the BHS were interviewed in person. There were 1802 participants who completed Pittsburgh Sleep Quality Index (PSQI) during this period.27 There were 417 individuals who completed assessments at both time points and constitute the longitudinal sample. Mean age was similar (p = .32) in individuals at baseline who did not complete the COVID-19 follow up questionnaire (n = 1385; mean age = 44.8) compared to individuals who did (n = 417 mean age = 43.9) but the proportion of men in the follow-up COVID-19 sample (30%) was significantly lower (p < .01) than in the sample that did not (45%).
Assessments
PSQI
Participants completed the PSQI, which is a validated instrument to assess sleep quality.28 The PSQI is comprised of 7 components, each with scores ranging from 0 to 3. Total scores on the PSQI range from 0 to 21, and higher scores indicate worse sleep quality. The PSQI components are subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction.28 In addition, we examined responses to questions asking for usual bed time, wake time, time to fall asleep (sleep latency), and sleep duration. In addition, we derived time in bed (interval between bed and wake time) and sleep efficiency (sleep duration divided by time in bed).
Quarantine adherence
During the COVID-19 assessment, participants were asked whether they were complying with the quarantine order (yes/no).
Demographic information
As part of the main study, date of birth and gender were collected. In analyses stratified by age, we selected 50 years as the cut point because sleep disturbances become more common at older ages. A meta-analysis indicated a decline in sleep quality at middle-age, which spanned 40-60 years,29 and previous work with this cohort also indicated a deterioration of sleep quality in the age range of 41-60 years old.27 Further, we are stratifying based on age during COVID-19 because we are interested in how COVID-19 may have impacted sleep quality. Finally, since this is a family-based study, we adjusted for family structure, which quantifies degrees of relatedness among participants.
Statistical analysis
In the longitudinal sample, we compared the change in PSQI scores and sleep characteristics pre-COVID-19 to the COVID-19 pandemic period. We tested whether this within-subject change in the sleep measures was significant by using a linear regression with the “lmer” function in the lme4 package in R statistical computing environment. The change in sleep characteristic was considered the outcome and “time” (pre-COVID-19 and COVID-19) was the covariate while adjusting for the random term for the individual repeated measure and the family cluster. We also analyzed the influence of quarantine status on PSQI change by adding “quarantine” (yes/no) as a covariate in the model.
We performed stratified analyses of the above models to examine the association between PSQI and quarantine within gender and age. For that, we repeated the abovementioned analyses in subsamples of gender and age groups.
We examined these same associations in the cross-sectional sample to determine if they are consistent with our longitudinal analyses because we had a larger cross-sectional sample, which provides greater statistical power. In this cross-sectional sample, we tested the association between PSQI score and quarantine using a polygenic mixed model (PMM), using the “lmekin” package. We used the same procedure to test the association between each PSQI component and quarantine. Model 1 adjusted only for family structure and Model 2 adjusted for family structure, age (ranging from 20 to 89) and gender (men as the referent) by adding them as covariates. PMM is a linear mixed model that accounts for the family structure in the random term of the equation, so the interdependence of subjects is accounted for, by considering the degree of relationship within participants.30 We repeated these analyses stratified by age and gender. To correct for the multiple comparisons bias, we used the Bonferroni method and reported the adjusted p values for the cross-sectional analyses.
R software, Version 3.6.1, was used for all statistical analyses. The alpha level was set at 0.05.
Results
Descriptive characteristics of both the longitudinal and cross-sectional samples are available in Table 1 . The interval between pre-COVID-19 and COVID-19 assessments ranged from 5 to 10 years with a mean of 7.5 years.
Table 1.
Descriptive characteristics of cross-sectional and longitudinal samples
| Longitudinal | Cross-sectional | |
|---|---|---|
| N | 417 | 800 |
| Women (N, %) | 290 (70%) | 568 (71%) |
| Men (N, %) | 127 (30%) | 232 (29%) |
| Mean age (SD) | 44 (15) | 52 (16) |
| Younger adults (N, %) | 170 (41%) | 351 (44%) |
| Older adults (N, %) | 247 (59%) | 449 (56%) |
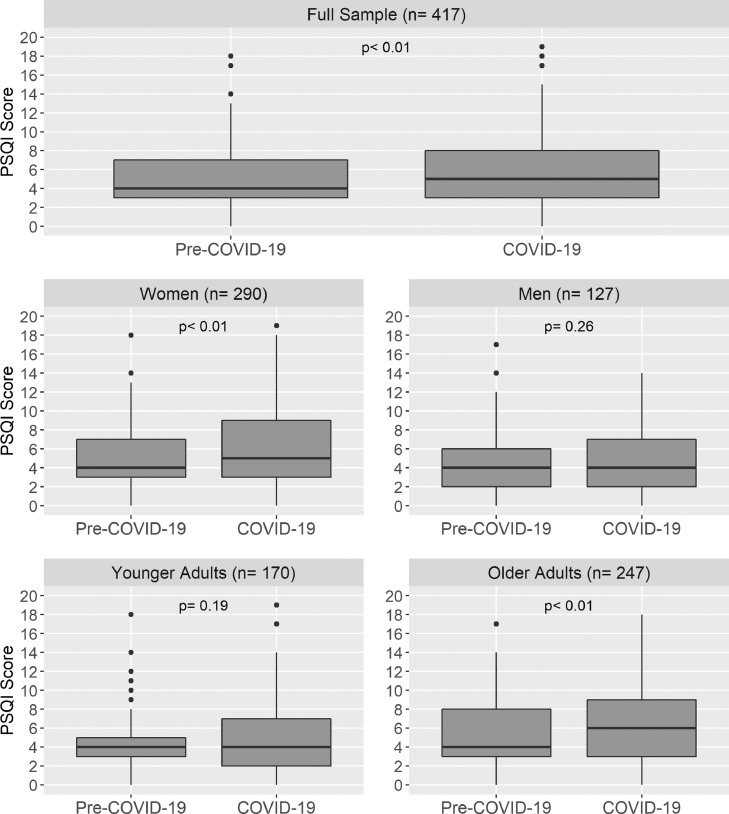
Mean PSQI score increased by approximately 0.7 points, which was a significant within-subject increase for the full longitudinal sample (Fig. 1 and Table 2 ). Stratified analysis demonstrated a significant increase in mean PSQI for women and older adults but not men and younger adults (Fig. 1 and Table 2). Bedtime did not change significantly between these time points but wake time was delayed by approximately 18 minutes and time in bed increased by approximately 24 minutes (Table 2). Sleep latency increased by about 7 minutes on average. Self-reported sleep duration did not increase and therefore sleep efficiency had a significant reduction of 6.3%. The same patterns were observed in women and older adults. However, among men, sleep latency did not increase and among younger adults, bedtime was delayed by approximately 24 minutes on average and sleep duration declined by about 18 minutes on average.
Fig. 1.
Mean Pittsburgh Sleep Quality Index (PSQI) scores pre-COVID-19 and during COVID-19 in the full sample and by gender and age group. p value indicates significance level of within-subject change adjusting for intra individual correlation and family cluster.
Table 2.
PSQI scores and sleep characteristics pre-COVID-19 and during COVID-19
| Pre-COVID-19 |
COVID-19 |
p valuea | |||
|---|---|---|---|---|---|
| mean | SD | mean | SD | ||
| Full sample (n = 417) | |||||
| PSQI score | 5 | 3.3 | 5.7 | 3.8 | <.01 |
| Bedtime (h) | 22.4 | 1.4 | 22.5 | 1.3 | .46 |
| Wake time (h) | 6.3 | 1.3 | 6.6 | 1.3 | <.01 |
| Time in bed (h) | 7.8 | 1.3 | 8.2 | 1.4 | <.01 |
| Sleep latency (min) | 22.4 | 29.4 | 29.7 | 35.2 | <.01 |
| Sleep duration (h) | 7.1 | 1.6 | 7 | 1.5 | .13 |
| Sleep efficiency (%) | 91.8 | 12.6 | 85.5 | 15.1 | <.01 |
| Women (n = 290) | |||||
| PSQI score | 5.2 | 3.31 | 5.98 | 3.86 | <.01 |
| Bedtime (h) | 22.37 | 1.06 | 22.43 | 1.2 | .81 |
| Wake time (h) | 6.34 | 1.22 | 6.72 | 1.23 | <.01 |
| Time in bed (h) | 7.86 | 1.21 | 8.29 | 1.46 | <.01 |
| Sleep latency (min) | 21.7 | 27.1 | 31.9 | 38.3 | <.01 |
| Sleep duration (h) | 7.13 | 1.6 | 7.01 | 1.51 | .27 |
| Sleep efficiency (%) | 91.86 | 12.04 | 85.31 | 15.41 | <.01 |
| Men (n = 127) | |||||
| PSQI score | 4.61 | 3.33 | 4.94 | 3.46 | .26 |
| Bedtime (h) | 22.35 | 1.29 | 22.57 | 1.34 | .39 |
| Wake time (h) | 6.09 | 1.34 | 6.46 | 1.43 | <.01 |
| Time in bed (h) | 7.57 | 1.4 | 7.89 | 1.32 | .02 |
| Sleep latency (min) | 24.1 | 34.2 | 24.6 | 26 | .78 |
| Sleep duration (h) | 6.98 | 1.46 | 6.8 | 1.47 | .25 |
| Sleep efficiency (%) | 91.66 | 12.9 | 86.22 | 14.51 | <.01 |
| Age < 50 years (n = 170) | |||||
| PSQI score | 4.42 | 2.99 | 4.82 | 3.61 | .19 |
| Bedtime (h) | 22.52 | 1.08 | 22.9 | 1.34 | <.01 |
| Wake time (h) | 6.78 | 1.38 | 6.95 | 1.32 | .16 |
| Time in bed (h) | 8.06 | 1.3 | 8.05 | 1.25 | .93 |
| Sleep latency (min) | 18.7 | 19.5 | 24.3 | 29.2 | .02 |
| Sleep duration (h) | 7.41 | 1.56 | 7.1 | 1.34 | .03 |
| Sleep efficiency (%) | 94.42 | 9.46 | 88.42 | 12.85 | <.01 |
| Age >= 50 years (n = 247) | |||||
| PSQI score | 5.43 | 3.47 | 6.23 | 3.77 | <.01 |
| Bedtime (h) | 22.26 | 1.15 | 22.18 | 1.2 | .14 |
| Wake time (h) | 5.91 | 1.04 | 6.43 | 1.24 | <.01 |
| Time in bed (h) | 7.6 | 1.24 | 8.25 | 1.54 | <.01 |
| Sleep latency (min) | 25 | 34.4 | 33.4 | 38.4 | <.01 |
| Sleep duration (h) | 6.87 | 1.52 | 6.84 | 1.6 | .8 |
| Sleep efficiency (%) | 90.18 | 14.02 | 83.63 | 16.27 | <.01 |
p value significance level was set at p < .05 and indicates within-subject change adjusting for intraindividual correlation and family cluster.
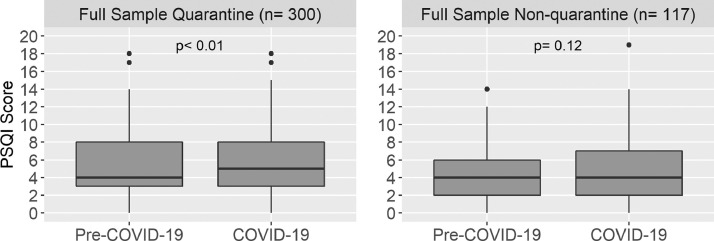
We examined whether the change in PSQI from pre-COVID-19 to during the pandemic differed between those who did and did not quarantine during COVID-19 (Fig. 2 and Supplemental Table 1). In the full sample, mean PSQI score increased significantly in those who quarantined during COVID-19 but not in those who did not quarantine. We also stratified these analyses by gender and age group (Supplemental Table 1 and Supplemental Fig. 1). There was a significant increase in PSQI score during COVID-19 among women who quarantined and among older adults who quarantined, but not among the other subgroups.
Fig. 2.
Mean Pittsburgh Sleep Quality Index (PSQI) scores pre-COVID-19 and during COVID-19 by quarantine status. p value indicates significance level of within-subject change adjusting for intra individual correlation and family cluster.
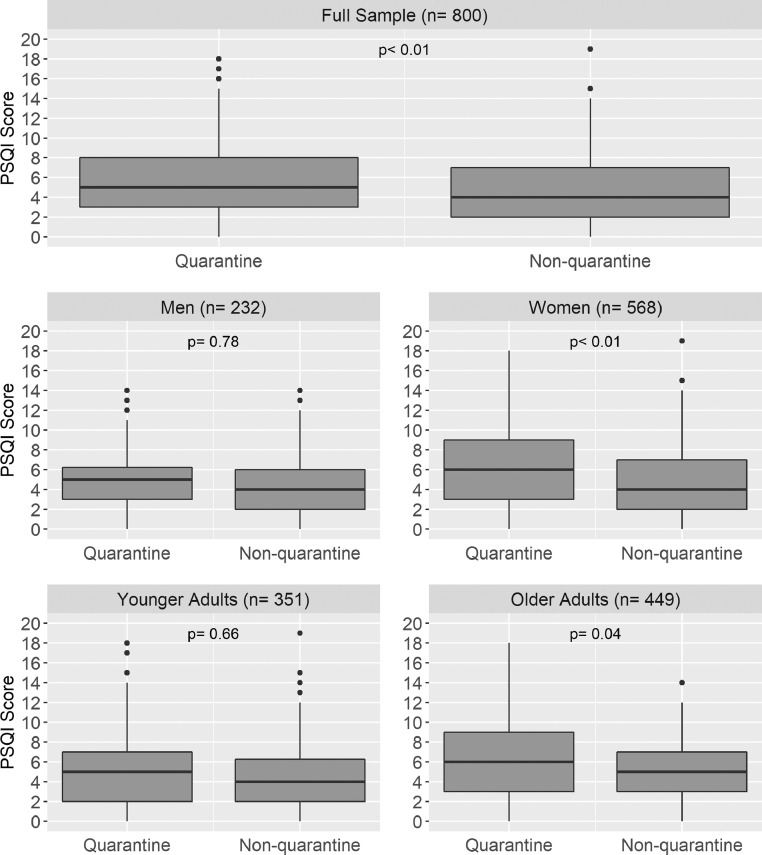
The cross-sectional associations between quarantine status and PSQI score are presented in Supplemental Table 2 and Fig. 3 . In the full cross-sectional sample, PSQI scores were higher among those who quarantined (p < .01). In the stratified analysis, PSQI scores were higher in women and older adults who quarantined during COVID-19 compared to those who did not. PSQI scores did not differ by quarantine status in men and young adults. When further adjusted for age and sex, the effect of quarantine status on mean PSQI score was attenuated (Supplemental Table 3) in the full sample (p = .30), women (p = .14) and in older adults (p = .28). Supplemental Table 4 presents comparisons of PSQI components by quarantine status. Sleep disturbances score was higher in quarantined individuals in the full sample. Quarantined individuals had increased sleep latency and sleep efficiency component scores than nonquarantined for the full sample and for women. Use of medication component score was higher in the quarantined group of the full sample, women and older adults. In Model II, the only component that remained significant was increased sleep latency for quarantined women and quarantined individuals in the full sample.
Fig. 3.
Mean Pittsburgh Sleep Quality Index (PSQI) scores by quarantine status in the full cross-sectional sample and by gender and age group. p value indicates significance level of the influence of quarantine status in PSQI scores adjusting for family structure.
Discussion
We observed a small but significant decline in subjective sleep quality during the pandemic compared to a previous assessment approximately 7.5 years prior. This is likely not just an effect of aging since we did not observe the decline in sleep quality in all subgroups; however, other sociocultural factors that changed over this time period may have impacted sleep quality, including economic and political factors.31 , 32 This decline appeared to be primarily among women and among adults 50 years or older. Further, during the COVID-19 pandemic, participants delayed their self-reported wake times resulting in an increased time in bed but not a longer sleep duration and sleep latency was slightly longer and sleep efficiency was reduced. In stratified analysis, a significant association between quarantine status and sleep quality was observed in women and older adults. The cross-sectional analysis, which had a larger sample size, was consistent with the longitudinal analysis and further suggested age and gender differences in these associations. Those who quarantined had a significantly higher PSQI score, and this was observed in women and older adults. The higher PSQI score in quarantined individuals coincided with a significantly worse sleep efficiency, higher sleep latency, and more use of sleep medication in the full sample and in women. In older adults, the use of medication was the only component to be significantly different between those who did and did not quarantine. Of note, the differences in PSQI are no longer significantly explained by quarantine status when adjusting for age and/or gender. Sleep latency was the only component that remained significantly different by quarantine status in the full sample and in women after adjustment for age and gender.
This is the first longitudinal study that investigated sleep during the pandemic in a Brazilian population. Several studies from around the world have examined sleep characteristics during COVID-19, but few studies compared COVID-19 sleep measures to data collected prior to COVID-19. Some studies attempted to compare sleep pre-COVID-19 using a retrospective recall design asking participants to describe their sleep currently and prior to the pandemic, which is prone to a recall bias.
In our study, individuals, particularly those who quarantined, women and older adults, perceived themselves as having worse sleep quality during the pandemic. Amongst other longitudinal studies using PSQI during the pandemic, 3 also reported worse sleep quality on the second follow-up.21 , 33 , 34 However, not all studies reported the same pattern, for example, Leone et al found no meaningful changes in PSQI score in the general Argentinian population.35 One study of 86 adults in the United States did not find a difference in PSQI between February and March of 2020.22 It is possible that, although the pandemic was not at its peak in the United States in February, it was still a potential cause of concern whereas COVID-19 was unknown at the time of the pre-COVID-19 PSQI assessment in Baependi in 2010-2014. The same argument could be applied to an Italian investigation that assessed 2701 adults and did not observe differences in PSQI between the third and the seventh week of lockdown.36 In this case, the first assessment included both the psychological distress of a potential infection and stringent measures of quarantine, limiting their exposure to important environmental sleep promoters.37 Therefore, the results from our study may have differed from the other longitudinal studies because our first assessment was obtained well before the COVID-19 pandemic began.
Despite differences in study designs, our study and others found that during the pandemic time in bed increased and wake time was delayed.16 , 21 , 35 , 38 Bedtime was not significantly different in our full sample, but, other studies observed delayed bedtimes.15 , 21 , 22 , 33 , 38 A delayed bed-time in young individuals was also described in other countries,20 , 35 which is consistent with our observation in the younger adults. This difference in sleep characteristics could be a reflection of a reduced mismatch between social cues and endogenous sleep timings. Freedom from social obligations increased the latitude to adjust timings to individual preferences.15 , 38 This is reflected in the younger adult group in Baependi who did delay bed times. However, residents of Baependi, in general, have a strong tendency towards morningness,39 which may explain why not all participants delayed their bedtime during the COVID-19 pandemic. Further, our sample is the only sample from a rural setting, as other studies enrolled either only urban residents or residents throughout a country, which would include a mix of urban and rural residents. Interestingly, Fu et al compared the rate of sleep problems between urban and rural residents of Wuhan during the pandemic.6 They found lower rates of sleep problems in rural residents, potentially due to the geographical distance from the center of the pandemic coupled with lower population density in rural areas.6 Thus, we speculate that our findings may be influenced by the rural setting of Baependi.
To our knowledge, no other report has compared sleep between those who did and did not adhere to quarantine orders. We observed that associations between quarantine and sleep quality were stronger in women and older adults. Women and older adults were also more likely to be quarantined. We speculate that this could be because women and older adults may have had found it easier to follow quarantine orders if women are more likely to work at home and older adults are more frequently retired than younger adults. Conversely, men and younger adults may have been compelled to continue occupational activities outside the home during the pandemic. An alternative hypothesis to the poorer sleep in women and older adults could be that they were more concerned about contracting COVID-19 than younger adults and men, and that contributed to both higher compliance to the quarantine order and to the poorer sleep quality. When we adjusted for age or gender in our comparisons, associations were attenuated, further emphasizing the importance of considering gender and age effects.
Prior literature included some conflicting reports regarding gender differences in sleep during the COVID-19 pandemic. Two studies in China and one in the United States reported no gender differences in PSQI scores1 , 10 , 12 and a meta-analysis that looked into the presence of sleep disturbances between men and women also reported that no significant differences were found during COVID-19.40 All studies that did report gender differences in sleep during the pandemic observed poorer sleep in women than men.6 , 7 , 11 , 17 Four longitudinal studies measured PSQI before and/or during the COVID-19 pandemic and 3 of them also observed the same pattern we did; women, but not men, had a significant increase in PSQI.21 , 33 , 36 The fourth study found no differences between genders.22 Despite COVID-19 being a worldwide phenomenon, its spread and the stringency measures adopted to combat the virus largely varied among countries. Given that, it is not surprising to find some inconsistencies in how much the pandemic affected the sleep of men and women, but publications to date strongly suggest poorer sleep in women than men during COVID. This finding is in line with the well-known fact that women are at increased risk of insomnia in general (not just during pandemics).41 We hypothesize that similar risk factors could lead to poorer sleep quality during the pandemic in women. Also, depression and anxiety can negatively impact sleep,42 , 43 and, a study investigating the comorbidity of depression and anxiety in Baependi, showed a significantly higher prevalence of both in women.44 The COVID-19 pandemic could exacerbate poor mental health, which could in turn impair sleep quality in women. From a sociocultural perspective, Baependi is a rural town where women are more frequently the primary caretaker of the household and children's education. Other studies showed that women encountered a work overload during the COVID-19 pandemic,6 , 36 which may have also occurred in Baependi because schools and daycare facilities were closed during this period, and this work overload may have played a role in the poorer sleep quality among women in this study.
In our sample, older adults had worse sleep quality during COVID-19 than prior to COVID-19, which was expected since sleep quality often deteriorates with age.23 Marelli et al33 reported that both workers (mean age = 37) and students (mean age = 22) from a university had a higher PSQI during COVID-19 compared to pre-COVID-19; however, the age difference in these 2 groups was not that large. Although we did not observe a significant change in sleep quality among younger adults, other studies indicate that the younger generation was affected by the pandemic, too.11 A comparison of 2 French cohorts reported a greater prevalence of trouble sleeping among young adults during COVID-19 than among the young adults prior to COVID-19. One possible contributor to poorer sleep among this age group could be that young people spent more time on social media reading about the pandemic, which could increase the preoccupation, awareness, and anxiety about infection.7 , 10 Since Baependi is a rural town, it is possible that younger adults have a different pattern of social media use than in metropolitan areas, thus, being more distant from the center of the pandemic could promote a sense of greater safety.6 Beck et al11 suggested that social distancing from peers, having precarious jobs with low income, or fear of schooling discontinuity are all vulnerabilities more specific to younger ages, which was hypothesized to be a few of the reasons for the worse sleep in youth.11 It is difficult, however, to compare differences in sleep quality during the pandemic based on age because cut-off points varied by study. Younger adults in our sample ranged from 20 to 49 years old and some of the posited reasons for worse sleep in young adults may not apply to this entire range (eg, school discontinuity). Other studies have observed higher PSQI scores among older adults compared to younger adults,6 , 13 which is consistent with our findings. In general, older individuals often have poorer general health and greater prevalence of chronic diseases,45 which could increase vulnerability to sleep disturbances. Older age is also associated with higher risk of severe COVID-19 symptoms or death, which can add an extra layer of concern, generating higher levels of stress, and contributing to poor sleep quality.14
The strengths of this study include the collection of PSQI both prior to and during the COVID-19 pandemic. Our work has limitations, however, that should be considered. We did not have objective measures of sleep, which would have provided more accurate measures of sleep duration and quality. The method of administration varied between time points because we were not allowed to do in-person interviews, but we cannot assess whether the administration format impacted the scores. In addition, there have been other changes in Brazil over this time period, including economic declines31 and political instability32; however, it is unclear if these factors could explain differences in sleep quality by quarantine status, gender, and age. There are additional potential confounders or mediators that we were not able to examine, including socioeconomic status, household size, and employment status, which could have impacted sleep and explain why individuals were or were not compliant to quarantine. We also had fewer men and younger adults, which may have limited power in subgroup analyses. Lastly, the interval between pre-COVID-19 and COVID-19 assessments varied among participants, but all pre-COVID-19 assessments occurred prior to the emergence of this virus in humans.
Conclusions
We found that subjective sleep quality declined during COVID-19 pandemic, particularly among those who followed quarantine orders, among women and among older adults. Reasons underlying these associations cannot be determined by our data, but could be related to psychosocial factors, such as anxiety or social isolation, as well as environmental factors, such as reduced activity or light exposure. The COVID-19 pandemic has affected health and well-being beyond the infection itself and these results demonstrate that sleep quality is one additional area that has been impacted.
Declaration of conflict of interest
The authors declare no conflict of interests.
Acknowledgments
This work is funded by NIH/NHLBI (R01HL141881) and by FAPESP (Fundação de Amparo à Pesquisa de São Paulo), grant number 2019/23078-1. We thank all participants of the Baependi Heart Study and the local staff for their dedication to this project even in difficult times during the pandemic.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.sleh.2021.11.007.
Appendix. Supplementary materials
References
- 1.Bigalke JA, Greenlund IM, Carter JR. Sex differences in self-report anxiety and sleep quality during COVID-19 stay-at-home orders. Biol Sex Differ. 2020;11(1):56. doi: 10.1186/s13293-020-00333-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bertrand L, Schröder C, Bourgin P, et al. Sleep and circadian rhythm characteristics in individuals from the general population during the French COVID-19 full lockdown. J Sleep Res. 2021:e13480. doi: 10.1111/jsr.13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prather AA, Janicki-Deverts D, Hall MH, Cohen S. Behaviorally assessed sleep and susceptibility to the common cold. Sleep. 2015;38(9):1353–1359. doi: 10.5665/sleep.4968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spiegel K, Sheridan JF, Van Cauter E. Effect of sleep deprivation on response to immunization. JAMA. 2002;288(12):1471–1472. doi: 10.1001/jama.288.12.1471-a. [DOI] [PubMed] [Google Scholar]
- 5.Gulia KK, Kumar VM. Importance of sleep for health and wellbeing amidst COVID-19 pandemic. Sleep Vigil. 2020;4:49–50. doi: 10.1007/s41782-020-00087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fu W, Wang C, Zou L, et al. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Transl Psychiatry. 2020;10(1):225. doi: 10.1038/s41398-020-00913-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gualano MR, Lo Moro G, Voglino G, Bert F, Siliquini R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Public Health. 2020;17(13) doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin LY, Wang J, Ou-Yang XY, et al. The immediate impact of the 2019 novel coronavirus (COVID-19) outbreak on subjective sleep status. Sleep Med. 2021;77:348–354. doi: 10.1016/j.sleep.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shillington KJ, Vanderloo LM, Burke SM, Ng V, Tucker P, Irwin JD. Not so sweet dreams: adults' quantity, quality, and disruptions of sleep during the initial stages of the COVID-19 pandemic. Sleep Med. 2021 doi: 10.1016/j.sleep.2021.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beck F, Léger D, Fressard L, Peretti-Watel P, Verger P. Covid-19 health crisis and lockdown associated with high level of sleep complaints and hypnotic uptake at the population level. J Sleep Res. 2021;30(1):e13119. doi: 10.1111/jsr.13119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jiang Z, Zhu P, Wang L, et al. Psychological distress and sleep quality of COVID-19 patients in Wuhan, a lockdown city as the epicenter of COVID-19. J Psychiatr Res. 2021;136:595–602. doi: 10.1016/j.jpsychires.2020.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou Y, Yang Y, Shi T, et al. Prevalence and demographic correlates of poor sleep quality among frontline health professionals in Liaoning Province, China during the COVID-19 outbreak. Front Psychiatry. 2020;11:520. doi: 10.3389/fpsyt.2020.00520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stanton R, To QG, Khalesi S, et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 2020;17(11) doi: 10.3390/ijerph17114065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blume C, Schmidt MH, Cajochen C. Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms. Curr Biol. 2020;30(14):R795–R797. doi: 10.1016/j.cub.2020.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cellini N, Canale N, Mioni G, Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020;29(4):e13074. doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yu BY, Yeung WF, Lam JC, et al. Prevalence of sleep disturbances during COVID-19 outbreak in an urban Chinese population: a cross-sectional study. Sleep Med. 2020;74:18–24. doi: 10.1016/j.sleep.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Majumdar P, Biswas A, Sahu S. COVID-19 pandemic and lockdown: cause of sleep disruption, depression, somatic pain, and increased screen exposure of office workers and students of India. Chronobiol Int. 2020;37(8):1191–1200. doi: 10.1080/07420528.2020.1786107. [DOI] [PubMed] [Google Scholar]
- 19.Roitblat Y, Burger J, Leit A, et al. Stay-at-home circumstances do not produce sleep disorders: an international survey during the COVID-19 pandemic. J Psychosom Res. 2020;139 doi: 10.1016/j.jpsychores.2020.110282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rezaei N, Grandner MA. Changes in sleep duration, timing, and variability during the COVID-19 pandemic: large-scale Fitbit data from 6 major US cities. Sleep Health. 2021;7(3):303–313. doi: 10.1016/j.sleh.2021.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Romero-Blanco C, Rodríguez-Almagro J, Onieva-Zafra MD, Parra-Fernández ML, Prado-Laguna MDC, Hernández-Martínez A. Sleep pattern changes in nursing students during the COVID-19 lockdown. Int J Environ Res Public Health. 2020;17(14) doi: 10.3390/ijerph17145222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gao C, Scullin MK. Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Med. 2020;73:1–10. doi: 10.1016/j.sleep.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 24.Census data. 2010. Available at: https://censo2010.ibge.gov.br. Accessed September 20, 2021.
- 25.Egan KJ, von Schantz M, Negrao AB, et al. Cohort profile: the Baependi Heart Study-a family-based, highly admixed cohort study in a rural Brazilian town. BMJ Open. 2016;6(10) doi: 10.1136/bmjopen-2016-011598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.da Saude M. COVID-19 no Brasil. 2021; Available at: https://qsprod.saude.gov.br/extensions/covid-19_html/covid-19_html.html. Accessed October 11, 2021.
- 27.Beijamini F, Knutson KL, Lorenzi-Filho G, et al. Timing and quality of sleep in a rural Brazilian family-based cohort, the Baependi Heart Study. Sci Rep. 2016;6:39283. doi: 10.1038/srep39283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 29.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27(7):1255–1273. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 30.de Andrade M, Amos CI, Thiel TJ. Methods to estimate genetic components of variance for quantitative traits in family studies. Genet Epidemiol. 1999;17(1):64–76. doi: 10.1002/(SICI)1098-2272(1999)17:1<64::AID-GEPI5>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 31.G1. 2020; Available at: https://g1.globo.com/economia/noticia/2021/03/03/pib-do-brasil-despenca-41percent-em-2020.ghtml. Accessed October 25, 2021.
- 32.Boschiero MN, Palamim CVC, Ortega MM, Mauch RM, Marson FAL. One year of coronavirus disease 2019 (COVID-19) in Brazil: a political and social overview. Ann Glob Health. 2021;87(1):44. doi: 10.5334/aogh.3182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marelli S, Castelnuovo A, Somma A, et al. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J Neurol. 2021;268(1):8–15. doi: 10.1007/s00415-020-10056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robillard R, Dion K, Pennestri MH, et al. Profiles of sleep changes during the COVID-19 pandemic: demographic, behavioural and psychological factors. J Sleep Res. 2021;30(1):e13231. doi: 10.1111/jsr.13231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leone MJ, Sigman M, Golombek DA. Effects of lockdown on human sleep and chronotype during the COVID-19 pandemic. Curr Biol. 2020;30(16):R930–R931. doi: 10.1016/j.cub.2020.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Salfi F, Lauriola M, Amicucci G, et al. Gender-related time course of sleep disturbances and psychological symptoms during the COVID-19 lockdown: a longitudinal study on the Italian population. Neurobiol Stress. 2020;13 doi: 10.1016/j.ynstr.2020.100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin YN, Liu ZR, Li SQ, et al. Burden of sleep disturbance during COVID-19 pandemic: a systematic review. Nat Sci Sleep. 2021;13:933–966. doi: 10.2147/NSS.S312037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wright KP, Jr., Linton SK, Withrow D, et al. Sleep in university students prior to and during COVID-19 stay-at-home orders. Curr Biol. 2020;30(14):R797–R798. doi: 10.1016/j.cub.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.von Schantz M, Taporoski TP, Horimoto AR, et al. Distribution and heritability of diurnal preference (chronotype) in a rural Brazilian family-based cohort, the Baependi study. Sci Rep. 2015;5:9214. doi: 10.1038/srep09214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Deng J, Zhou F, Hou W, et al. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;301 doi: 10.1016/j.psychres.2021.113863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang B, Wing YK. Sex differences in insomnia: a meta-analysis. Sleep. 2006;29(1):85–93. doi: 10.1093/sleep/29.1.85. [DOI] [PubMed] [Google Scholar]
- 42.Benca RM, Peterson MJ. Insomnia and depression. Sleep Med. 2008;9(suppl 1):S3–S9. doi: 10.1016/S1389-9457(08)70010-8. [DOI] [PubMed] [Google Scholar]
- 43.Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36(7):1059–1068. doi: 10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Taporoski TP, Negrão AB, Horimoto AR, et al. Shared genetic factors of anxiety and depression symptoms in a Brazilian family-based cohort, the Baependi Heart Study. PLoS One. 2015;10(12) doi: 10.1371/journal.pone.0144255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li J, Vitiello MV, Gooneratne NS. Sleep in normal aging. Sleep Med Clin. 2018;13(1):1–11. doi: 10.1016/j.jsmc.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.