Abstract
Objective:
The novel coronavirus disease (COVID-19) has drastically impacted the provision of mental health services. Changes required of providers were substantial and could lead to increased burnout and, subsequently, increased turnover intentions. This study examined burnout experienced by mental health services providers in the context of COVID-19 and through the lens of the job demands-resources (JD-R) model. We examined the effects of work changes on burnout and subsequent turnover intentions, and how job and personal resources may have buffered the extent to which work changes due to COVID-19 impacted burnout.
Methods:
Service providers (n=93) from 6 community mental health centers (CMHCs) in one Midwestern state in the United States completed surveys as part of service contracts to implement evidence-based practices. Path analysis tested the unconditional indirect relations between work changes and turnover intentions through burnout. Moderated mediation determined whether the indirect effect of work changes on turnover intentions via burnout varied in strength by job and personal resources.
Results:
Work changes had a significant indirect effect on turnover intentions through burnout (=.140, 95% CI=.072, .217). This indirect effect varied as a function of two job resources, organizational trust and perceived organizational support.
Conclusions and Implications for Practice:
Burnout was relatively low only when work changes were low and job resources levels high. When work changes were high, burnout was similarly high across levels of job resources. To minimize burnout, organizations should limit task, setting, and team-related work changes to the extent possible.
Keywords: COVID-19, mental health services, burnout, job-demands resource model, moderated mediation
Introduction
The novel coronavirus disease (COVID-19) pandemic resulted in a quickly changing situation in a majority of countries (Shore et al., 2020) that necessitated adaptations to mental health service systems to limit the spread of the infection while also best addressing mental health needs (Moreno et al., 2020; Wind et al., 2020). Infection-control measures included screening patients, staff, and visitors for viral infection, limiting and/or eliminating in-person visits, reducing the number of outpatient appointments, adopting triage protocols that recommend treating only the most urgent issues, and restructuring caseloads to minimize contact among clients/patients (Moreno et al., 2020). Adaptations to facilitate access to services included the widespread use of telehealth, reinforced by changes to laws and legislation targeting confidentiality and privacy, and funding mechanisms (e.g., payment for services).
To respond to these changes, constant adaptation, flexibility, and problem solving is needed and can result in increased burnout amongst mental health services workers. The term “burnout” introduced by Freudenberger (1974) as a form of exhaustion among human services workers chronically exposed to the problems and emotional distress of their patients. Burnout has since been conceptualized more broadly and is defined in the 11th revision of the International Classification of Diseases (ICD-11) as a syndrome “resulting from chronic workplace stress that has not been successfully managed” (World Health Organization [WHO], 2019). Burnout is further characterized in the ICD-11 by three dimensions that include exhaustion, reduced professional efficacy, and increased mental distance from one’s job or feelings of cynicism or negativism about one’s job. Health service providers have greater experiences of workout than the general population (Shanafelt et al., 2012). Mental health workers might be particularly vulnerable to experiencing burnout as 21–67% report experiencing burnout across numerous studies (Morse et al., 2012). The consequences of burnout are vast. Employees who experience burnout often evidence impaired emotional and physical health (Stalker & Harvey, 2002; Acker 2010). Burnout is also correlated with reduced organizational commitment (Burke & Richardsen, 1993), increased absenteeism and turnover (Schwab et al., 1986; Smoot & Gonzales, 1995; Stalker & Harvey, 2002), and can also negatively impact the quality of care provided to patients and clients (Boyer & Bond, 1991; Carney et al., 1993; Hoag et al., 2007; Maslach & Pines, 1979). There is a clear need to focus attention on reducing burnout experienced by mental health services providers.
One of the most highly studied models of employee burnout is the job demands—resources (JD-R) model (Bakker & Demerouti, 2017; Bakker et al., 2005; Demerouti et al., 2001; Schaufeli & Bakker, 2004). In this model, all job characteristics are categorized as either job demands or job resources. Job demands are defined as “those physical, psychological, social, or organizational aspects of the job that require sustained physical and/or psychological effort and are therefore associated with certain physiological and/or psychological costs” (Bakker & Demerouti, 2017, p. 274), and job resources are defined as “those physical, psychological, social, or organizational aspects of the job that are functional in achieving work goals, reduce job demands and the associated physiological and psychological costs, or stimulate personal growth, learning, and development” (Bakker & Demerouti, 2017, p. 274). In addition to job resources, individuals also bring personal resources to the work environment; personal resources are defined as “the beliefs people hold regarding how much control they have over their environment” (Bakker & Demerouti, 2017, p. 275). Within JD-R, demands are conceptualized to be primarily responsible for strain outcomes, such as burnout and exhaustion. In contrast, resources are primarily responsible for work engagement, but also serve was buffers of the relationship between job demands and strain. In other words, individuals are better able to cope with the demands of their job when they have more resources at their disposal.
This study examines burnout experienced by mental health service providers in the context of the first four months of the COVID-19 pandemic, based on the JD-R framework. As noted previously, the changes required of providers were substantial, encompassing changes to their tasks, settings, and teams. Within the JD-R framework, such changes to the work context represent job demands that require high levels of effort and have extensive physiological and psychological costs. As a result, the extent to which providers had to adapt to such changes was expected to be associated with high levels of burnout and, subsequently, increased turnover intentions.
In addition to examining the outcomes of these work changes on strain and turnover-related outcomes, we also sought to examine what resources may buffer the extent to which work changes due to COVID-19 impacted burnout. We examined six resources in total, including three job resources and three personal resources. For job resources, we were particularly interested in those resources directly linked to leadership in order to provide practical steps that leaders could take to impact their subordinates’ coping and burnout. Thus, we assessed collective efficacy, organizational trust, and perceived organizational support. While self-efficacy represents an individual’s beliefs regarding the likelihood that a particular course of action or behavior can be carried out, collective efficacy applies this concept of efficacy to groups. Group members hold collective beliefs regarding the capability of the group as a whole, otherwise known as collective efficacy (Jex & Bliese, 1999). Employees’ trust in their organizations represent employees’ beliefs regarding the organization’s integrity, motives and intentions, behavioral consistency, openness, and discreteness (Gabarro & Athos, 1976; Robinson & Rousseau, 1994). Perceived organizational support is defined as employees’ global beliefs concerning the extent to which the organization values employees’ contributions and cares about their well-being (Eisenberger et al., 2002). We anticipated that when providers were confident in their team’s ability to cope with changes related to telehealth, when they trusted their organization to do the right thing and make decisions with integrity, and when they felt they had the support of the organization and its leadership, they would be better able to cope with the work changes related to COVID-19, and thus the impact of those changes on burnout would be diminished.
Within the JD-R framework, personal resources are often conceptualized in terms of efficacy and optimism (Bakker & Demerouti, 2017), and thus we focused on three individual constructs closely related to the transition to telehealth and to COVID-19: telehealth self-efficacy, beliefs regarding telehealth, and perceptions of personal risk. Telehealth self-efficacy is the extent to which the individual feels confident in their personal ability to make the transition to telehealth. Beliefs regarding telehealth are the extent to which providers held a positive view of telehealth and its usefulness for providing care. Finally, perceptions of personal risk assessed the level of vulnerability individuals felt to COVID-19 and their concern about infection. Linking back to the JD-R framework, we proposed each of these as contributing to a sense of control among providers in managing the crisis and the changes associated with it. In short, we expected that the more individuals were confident that they could transition to telehealth, held a positive outlook regarding the effects of telehealth on patient care, and felt less vulnerable to COVID-19 infection, the better they would be able to cope with the work changes in their jobs, diminishing the impact of those changes on burnout and turnover intentions.
Putting these pieces together, this study applies the JD-R framework to the COVID-19 crisis by examining the mediational relationship between COVID-19-related work changes on turnover intentions mediated through burnout. We hypothesized that providers coping with increased work changes would report higher levels of burnout, and subsequently also report increased turnover intentions. We also hypothesized that job resources and personal resources would buffer this mediational relationship, such that individuals reporting higher resource levels would report lower burnout associated with work changes due to COVID-19.
Method
Data were collected as part of an ongoing service contract to facilitate evidence-based practice implementation in a statewide mental health and addictions service system. CMHCs interested in participating responded to a request for funding announcement issued by the state mental health and addictions service system. Data were collected routinely over the course of this project to inform the identification and creation of strategies to facilitate successful evidence-based practice implementation. Ethics approval, and a waiver to consent, was obtained from the UC San Diego Human Research Protections Program (Protocol 200855).
Participants
Participants were direct outpatient, home-based, and school-based service providers (n=93, i.e., therapists, counselors) from 6 CMHCs across a Midwestern state in the US. CMHCs provided inpatient, outpatient, home-based, school, and community-based programs to clients of all ages in urban and rural areas across the state. The sample was mostly female (n=77; 83.7%), non-Hispanic (n=82; 89.1%), White (n=80; 87.0%), and average age was 42 years (sd=14.2 years). Most providers had completed master’s level education (n=66; 71.7%) and identified social work as their primary discipline (n=44; 47.8%). On average, providers reported having worked with their present agencies for 4.7 years (sd=7.7 years), and being in their current positions for 3.2 years (sd=5.9 years). Providers reported spending the greatest percentage of their work time in psychotherapy and/or counseling (=44.4%) and reported an average caseload of 51.9 (sd=39.3) clients per month. Administrative work (e.g., documentation, billing) (=18.1%) and case management (=11.8%) comprised the next greatest percentages of providers’ work time. See Table 1 for more provider demographics.
Table 1.
Provider demographics.
| Variable | n | % |
|
| ||
| Gender | ||
| Female | 77 | 82.8 |
|
| ||
| Male | 14 | 15.1 |
|
| ||
| Other | 1 | 1.1 |
|
| ||
| Missing | 1 | 1.1 |
| Race | ||
| White | 80 | 86.0 |
|
| ||
| Black or African American | 3 | 3.2 |
|
| ||
| Asian | 2 | 2.2 |
|
| ||
| American Indian/Alaska Native | 1 | 1.1 |
|
| ||
| More than one race | 6 | 6.5 |
|
| ||
| Missing | 1 | 1.1 |
| Ethnicity | ||
| Non-Hispanic | 82 | 88.2 |
|
| ||
| Hispanic | 10 | 10.8 |
|
| ||
| Missing | 1 | 1.1 |
| Highest level of Education | ||
| Some college | 1 | 1.1 |
|
| ||
| College graduate | 14 | 15.1 |
|
| ||
| Some graduate work | 5 | 5.4 |
|
| ||
| Master’s degree | 66 | 71.0 |
|
| ||
| PhD, MD, or equivalent | 6 | 6.5 |
|
| ||
| Missing | 1 | 1.1 |
| Primary Discipline | ||
| Drug/Alcohol Counseling | 13 | 14.0 |
|
| ||
| Social Work | 44 | 47.3 |
|
| ||
| Child Development | 2 | 2.2 |
|
| ||
| Marriage and Family Therapy | 2 | 2.2 |
|
| ||
| Psychology | 16 | 17.2 |
|
| ||
| Other | 15 | 16.1 |
|
| ||
| Missing | 1 | 1.1 |
| Providers per Agency | ||
| Agency 1 | 8 | 8.6 |
|
| ||
| Agency 2 | 15 | 16.1 |
|
| ||
| Agency 3 | 11 | 11.8 |
|
| ||
| Agency 4 | 14 | 15.1 |
|
| ||
| Agency 5 | 43 | 46.2 |
|
| ||
| Agency 6 | 2 | 2.2 |
|
| ||
| Variables | ||
|
| ||
| Age (years) | 41.7 ± 14.2 | |
| Years at present agency | 4.7±7.7 | |
| Years in present position | 3.2±5.9 | |
| Percentage of your work time doing the following... | ||
| Standardized assessments | 7.1±10.5 | |
|
| ||
| Case management | 11.8±18.4 | |
|
| ||
| Psychotherapy and/or counseling | 44.4±28.5 | |
|
| ||
| Administrative work (e.g., documentation, billing) | 18.1±11.9 | |
|
| ||
| Meeting with your supervisor | 7.2±10.5 | |
|
| ||
| Supervising others | 4.2±13.1 | |
|
| ||
| Travel | 2.1±5.0 | |
|
| ||
| Other | 5.1±14.5 | |
Procedures
CMHC providers completed surveys via the Qualtrics web-based platform on three occasions, Survey 1 in early March 2020, Survey 2 in late April/early May 2020, and Survey 3 in late June 2020. Response rates were 86%, 77%, and 75% for Surveys 1, 2, and 3, respectively. Between Surveys 1 and 3, a total of nine participants left their CMHCs, of which only five had completed an assessment prior to their turnover. Following Survey 1, an additional three participants opted out. Survey 1 included measures of participant demographics. Survey 2 included measures of work changes due to the COVID-19 outbreak and burnout. Survey 3 included a measure of turnover intentions. Thus, the present study is prospective, strengthening causal inferences. Additionally, Survey 2 examined job demands with measures of work place/organizational resources and personal resource.
Measures
Each of the measures that were utilized are described below. Unless otherwise stated, participants responded to items using a 5-point scale ranging from 1=“Strongly Disagree” to 5=“Strongly Agree.” When appropriate, the internal consistency of each measure was assessed for this sample using Cronbach’s α and is included in the description of each measure.
Work Changes Due to COVID-19.
Using a content validation approach, three distinct types of work changes were identified based on feedback from providers and their leaders. A single item was developed to capture each type of work change through an iterative process of item generation, discussion, and refinement until consensus on item wording was achieved. The resulting three items were as follows: “Because of COVID-19, my work tasks have changed”, “Because of COVID-19, my work setting has changed”, and “Because of COVID-19, my work team has changed.” Participants responded using a 5-point response scale ranging from 0=“Not at all” to 4=“Very great extent.” These items measured different types of changes that providers may have experienced, and together capture the aggregate level of work changes experienced by participants, consistent with a formative measurement approach (Coltman et al., 2008). The sum of all items was calculated to better understand the cumulative or summative impact of COVID-19 work changes on participants. Because the three items were developed to capture three distinct types of work changes and were not intended to represent a single underlying construct, internal consistency was not assessed (Coltman et al., 2008).
Burnout.
The Copenhagen Work Burnout Inventory is a measure developed to assess the extent to which participants have experienced emotional exhaustion and work-related frustration within the past two weeks (Kristensen et al., 2005). Although developed specifically to generalize to individuals outside of the human service work context, it was initially tested in a state psychiatric prison, social welfare offices, psychiatric inpatient facilities, and homecare services. In health care, this scale has demonstrated validity in predicting nurses’ job performance including medication administration errors (Montgomery et al., 2020). Participants responded to three items targeting work-related burnout using a 5-point scale ranging from 0=“Never” to 4=“Always.” Internal consistency for these items was high at α=.91.
Turnover Intentions.
The three-item turnover intention scale from the Michigan Organizational Assessment Questionnaire was used to assess participants’ intentions to leave their organization (Seashore et al., 1982). This commonly used scale of turnover intentions (Willness et al., 2007) has been used with nurses (Kath et al., 2012, Sagie & Krausz, 2003), used in large cross-cultural studies of role stress (Glazer & Beehr, 2005), and with community health service workers (Albrecht & Andreetta, 2011). Concurrent validity of this measure has been demonstrated through its significant negative relations with job satisfaction and organizational commitment (Windon et al., 2019). Internal consistency for these items was high at α=.89.
Job Resources.
The following three measures were used to assess job resources: collective efficacy, organizational trust, and perceived organizational support. Collective efficacy was assessed using three items adapted from Jex and Bliese (1999) to measure efficacy beliefs targeting the agency’s transition to telehealth. This measure has been used previously to examine the interaction effect of collective efficacy and job demands on psychological strain, job satisfaction, and organizational commitment (Jex & Bliese, 1999). It has demonstrated concurrent and discriminant validity with a stronger positive relation with leadership climate than individual self-efficacy and role clarity (Chen & Bliese, 2002). Internal consistency for this measure was moderately high at α=.76. The 7-item organizational trust scale was used to measure participants’ trust in their employers and the extent to which their employer has high integrity (Robinson & Rousseau, 1994). Three items are reverse scored, and the mean across all items is calculated to form an overall organizational trust score. Concurrent validity is supported by its positive relations with satisfaction, and negative relations with psychological contract violations and turnover (Robinson & Rousseau, 1994). Internal consistency for this measure was high at α=.92. The 3-item perceived organizational support scale was developed to assess the extent to which respondents believe help is available to them from their agency, that their agency cares about their well-being, and their agency shows concern for them (Eisenberger et al., 1986). Concurrent validity of this measure is strengthened by its significant negative correlation with absenteeism (Eisenberger et al., 1986) and significant positive correlation with perceived supervisor support (Eisenberger et al., 2002). Internal consistency for this measure was high at α=.93. Both the organizational trust scale and the perceived organizational support scale have been used in research examining their buffering effects on job performance and organizational citizenship behaviors (Bal et al., 2009).
Personal Resources.
The following three measures were used to assess personal resources: telehealth self-efficacy, beliefs regarding telehealth, and perceptions of personal risk. Telehealth self-efficacy was assessed using a 4-item scale adapted from a measure that assesses participant’s confidence, knowledge, understanding, and preparation to deliver therapy via telehealth (Lau & Brookman-Frazee, 2016; Kim et al., 2018). Internal consistency for this measure was high at α=.92. Telehealth beliefs were measured using a 5-item measure adapted from the University of Michigan’s Behavioral health Workforce Research Center to assess beliefs regarding the importance of telehealth from 329 behavioral health provider organizations representing all 50 states (Mace et al., 2018). Internal consistency for this measure was high at α=.85. Perceptions of personal risk was assessed using a 9-item measure adapted from Wu et al.’s (2009) measure assessing perceptions of personal risk around SARS. Items were adapted to assess participants perceived risk of being exposed to, and getting infected with, COVID-19. Internal consistency for this measure was high at α=.87.
Data Analysis
Descriptive statistics of each measure and corresponding items were assessed to explore the distributions and potential departures from normality and assumptions. Scale scores were mean centered and intraclass correlation coefficients (ICC(1)) were assessed to determine within clinic similarity in responses and whether controlling for unit level clustering was justified. Correlations between each measure were also examined. See Table 2 for descriptive statistics and ICC(1) values per scale and Table 3 for the correlation matrix. Examination of ICC(1) values revealed within clinic similarity in responses and support controlling for the clustering of participant responses by clinic (Bliese, 1998; LeBreton & Senter, 2008).
Table 2.
Survey scale descriptive statistics and intraclass correlation coefficients (ICC(1)).
| Minimum | Maximum | Mean | Std. Deviation | ICC(1) | |
|---|---|---|---|---|---|
| Work Changes | 2.00 | 12.00 | 8.69 | 2.36 | 0.11 |
| Burnout | 0.00 | 4.00 | 2.31 | 0.97 | 0.17 |
| Turnover Intentions | 1.00 | 5.00 | 2.73 | 1.19 | 0.08 |
| Collective Efficacy | 1.67 | 5.00 | 3.55 | 0.77 | 0.07 |
| Organizational Trust | 1.14 | 5.00 | 3.66 | 0.92 | 0.19 |
| Perceived Organizational Support | 1.00 | 5.00 | 3.66 | 1.00 | 0.11 |
| Telehealth Self-Efficacy | 1.00 | 5.00 | 3.68 | 0.85 | <0.005 |
| Telehealth Beliefs | 1.00 | 5.00 | 3.89 | 0.84 | <0.005 |
| Perceptions of Personal Risk | 0.00 | 4.00 | 1.41 | 0.83 | 0.12 |
Table 3.
Correlation matrix of turnover intentions, burnout, work changes, and job and personal resources.
| Turnover Intentions | Work Changes | Burnout | Collective Efficacy | Organizational Trust | Organizational Support | Telehealth Self-Efficacy | Telehealth Beliefs | |
|---|---|---|---|---|---|---|---|---|
| Work Changes | 0.186 | |||||||
| Burnout | .437** | .491** | ||||||
| Collective Efficacy | −.536** | −0.131 | −.343** | |||||
| Organizational Trust | −.666** | −.275** | −.365** | .556** | ||||
| Organizational Support | −.578** | −.241* | −.356** | .552** | .802** | |||
| Telehealth Self-Efficacy | −.235* | −.249* | −.377** | .578** | .318** | .351** | ||
| Telehealth Beliefs | −0.189 | 0.059 | −0.134 | .415** | .241* | .258* | .517** | |
| Personal Risk | .468** | .319** | .361** | −.337** | −.456** | −.395** | −0.015 | 0.049 |
p < .05
p < .01
We conducted path-analyses in Mplus Version 7.4 to test hypotheses regarding work changes, turnover intentions, and burnout. Analyses controlled for the clustering of providers’ data nested within teams/clinics as defined by having the same leader/supervisor using the cluster command. Additionally, because work place/organizational resources may vary as a function of CMHC and/or provider tenure at their CMHC, analyses also controlled for CMHC and years at the CMHC. Four participants had missing values for the predictor variables and were subsequently excluded from the analyses. Consistent with our hypotheses, the model specified direct paths from work changes to burnout (a1), burnout to turnover intentions (b1), and work changes to turnover intentions (c’). The model also specified unconditional indirect paths from work changes to turnover intentions via burnout. Figure 1 shows the proposed path-analysis model. Overall fit of the model was examined using a number of fit indices. The Bayesian information criterion (BIC) and sample-size adjusted BIC (ABIC) (Schwarz, 1978) are calculated from the log-likelihood of the model and the number of parameters in the model, and lower values suggest better model fit. The Akaike information criterion (AIC) (Akaike, 1981), assessed by the likelihood function accounting for estimated parameters, where smaller AIC values represent better model fit. Estimates of path coefficients corresponding with the direct and unconditional indirect effects were also assessed. The proportion of variance in each endogenous variable accounted for by the exogenous variable was assessed by examining R2.
Figure 1.
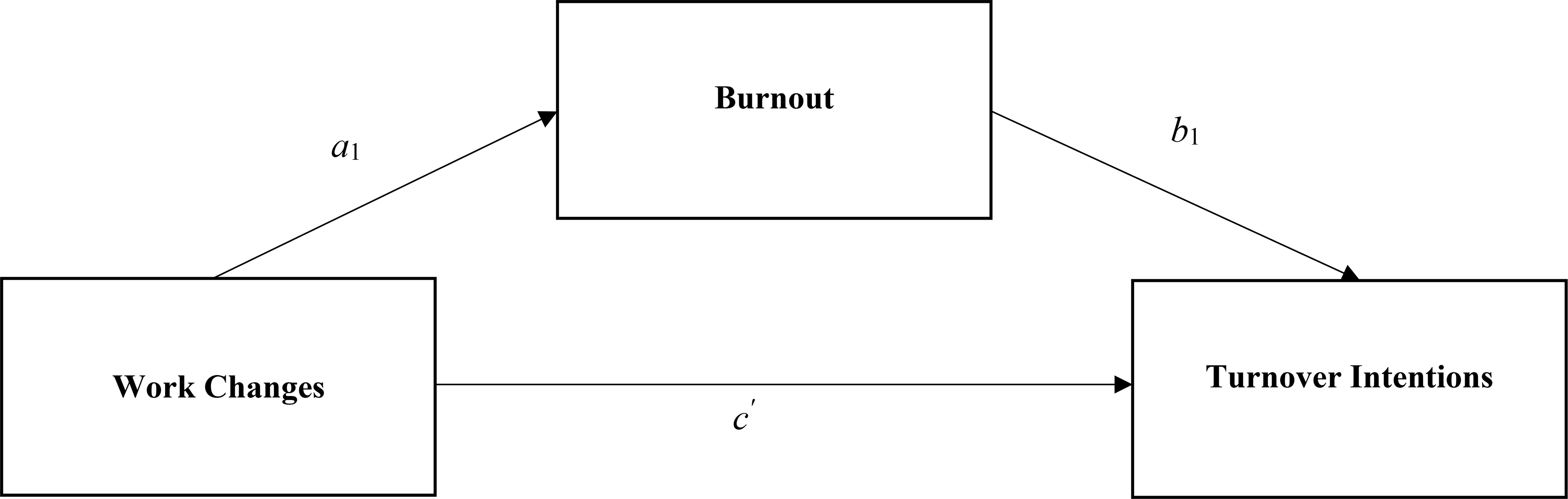
Path-analytic model testing the relations between work changes, burnout, and turnover intentions.
To determine whether the indirect effect of work changes on turnover intentions via burnout varied in strength as a function of work place/organizational resources and personal resources, a moderated mediation model was assessed. Specifically, the conditional indirect effect of the a1 path of the model in Figure 1 was tested with each job and personal resource included as moderating variables. Figure 2 shows this moderated mediation model. Similar to the unconditional model, overall model fit was examined using BIC, ABIC, and AIC fit indices and estimates of path coefficients corresponding with the direct and conditional indirect effect for this moderated mediation model were assessed.
Figure 2.
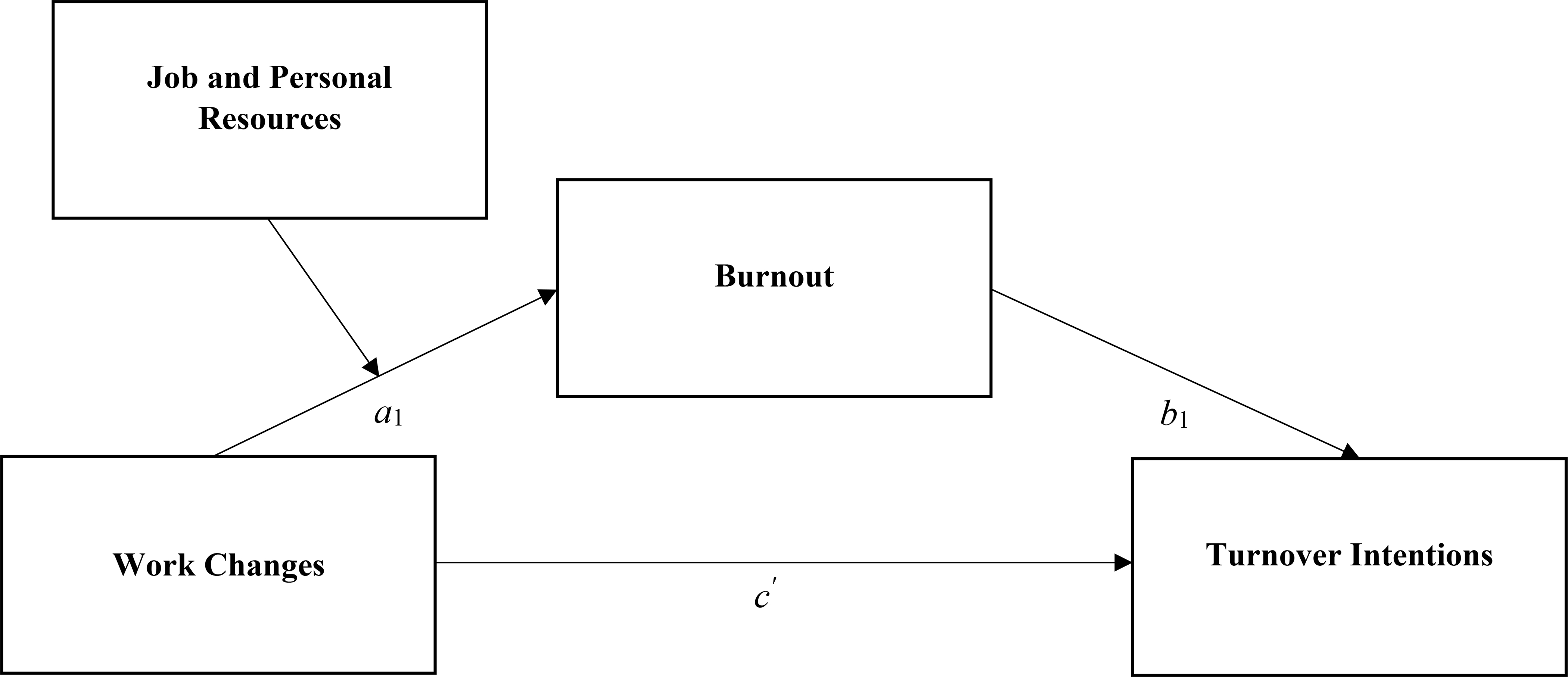
Moderated path-analytic model testing the relations between work changes, burnout, turnover intentions and job and personal resources.
Bootstrapping with k=1000 samples was used to test for the unconditional and conditional indirect effect of work changes to turnover intentions via burnout. Unconditional and conditional indirect effects are usually positively skewed and kurtotic; when using bootstrapping, no assumptions about the shape of the sampling distribution of the statistic are necessary for conducting inferential tests (Preacher et al., 2007). For hypothesis testing, the 95% confidence interval (CI) of the bootstrap values was examined; the unconditional and conditional indirect effects were rejected at α=.05 for cases wherein 0 lies outside of the CI.
For any cases wherein a conditional indirect effect was found, the interaction was subsequently explored by estimating the simple intercept and simple slope of the conditional regression of burnout on work changes at specified values of the moderator (the mean, one standard deviation above the mean, one standard deviation below the mean), and graphical representations of these relations were plotted using Rweb to aid in interpretability of the effects. Calculations of these simple intercepts and simple slopes were conducted using Preacher, Curran, and Bauer’s instructions and online calculator (Bauer & Curran, 2005; Curran et al., 2006; Preacher et al., 2006; Curren & Bauer, 2003).
Results
Unconditional Indirect Relations
The model testing the unconditional indirect relations from work changes to turnover intentions via the burnout mediating variable fit well (AIC=443.8, BIC=476.0, ABIC=434.9). The direct effect from burnout to turnover intentions was statistically significant (=.685, p <.001) and the direct effect from work changes to burnout was statistically significant (=.205, p < .001). The indirect effect from work changes to turnover intentions through burnout was statistically significant based on the bootstrapped CI not including zero (=.140, 95% CI=.072, .217). After accounting for indirect effects through burnout, the direct effect from work changes to turnover intentions was not statistically significant (=−.058, p=.260). Work changes accounted for 25% and 38% of the variance in burnout and turnover intentions (including both direct and indirect effect), respectively. Greater work change was positively associated with greater burnout, and greater reported burnout was positively associated with greater turnover intentions.
Conditional Indirect Relations
Six separate moderated mediation models were assessed to determine whether the direct path from work change to burnout (a1) was moderated by each job resource and personal resource. For all models, the extent to which the indirect effect of work changes on turnover intentions via burnout varied in strength as a function of each job resource and personal resource was tested.
Job Resources.
Three moderated mediation models determined whether the indirect effect of work changes on turnover intentions via burnout was moderated by collective efficacy, organizational trust, and perceived organizational support. The model exploring the moderating effect of collective efficacy fit better statistically than the unconditional model, as demonstrated by comparatively lower fit indices (AIC=437.1, BIC=474.3, ABIC=427.0). The direct effect from the work changes by collective efficacy interaction to burnout was not statistically significant (=.000, p=.998) and the indirect effect from work changes to turnover intentions through burnout was not moderated by collective efficacy as the bootstrapped CI included zero (=.000, 95% CI=−.062, .085).
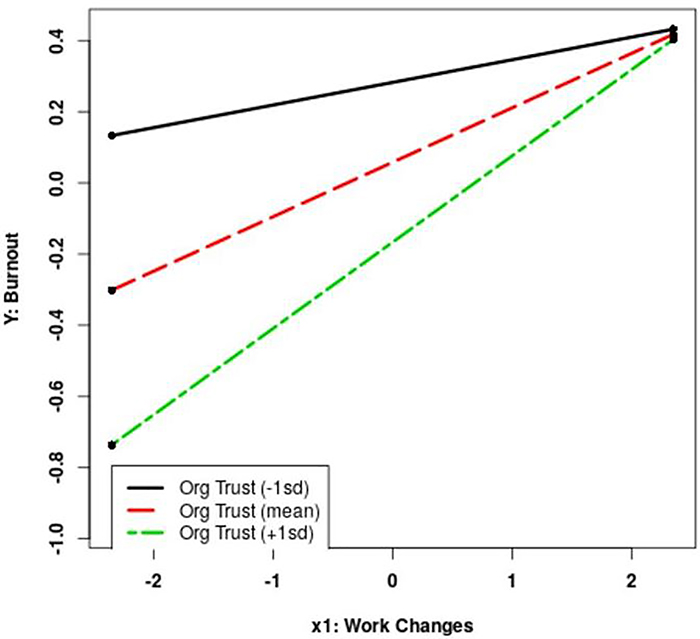
The model exploring the moderating effect of organizational trust fit better statistically than the unconditional model, as demonstrated by comparatively lower fit indices (AIC=434.9, BIC=472.1, ABIC=424.8). The direct effect from the work changes by organizational trust interaction to burnout was statistically significant (=.103, p=.002) and the indirect effect from work changes to turnover intentions through burnout was moderated by organizational trust based upon the bootstrapped CI not including zero (=.070, 95% CI=.022, .116). See Figure 3 for a graphical representation of the work changes by organizational trust interaction on burnout. When work changes were low, burnout differed as a function of organizational trust such that greater levels of organizational trust were associated with lesser levels of burnout. When work changes were great, burnout was similarly high across levels of organizational trust.
Figure 3.
Work changes on burnout by organizational trust.
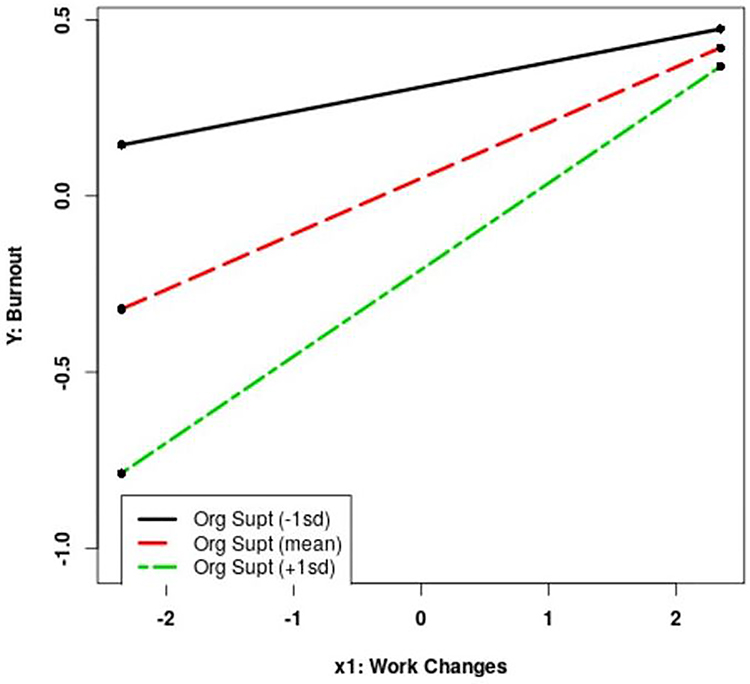
The model exploring the moderating effect of organizational support fit better statistically than the unconditional model, as demonstrated by comparatively lower fit indices (AIC=434.2, BIC=471.4, ABIC=424.1). The direct effect from the work changes by organizational support interaction to burnout was statistically significant (=.096, p=.002) and the indirect effect from work changes to turnover intentions through burnout was moderated by organizational support (=.066, 95% CI=.015, .100). See Figure 4 for a graphical representation of the work changes by organizational support interaction on burnout. Similar to the interaction between work changes and organizational trust, burnout differed as a function of organizational support when work changes were low such that higher levels of organizational support were associated with lesser levels of burnout. When work changes were higher, burnout was similarly high across levels of organizational support.
Figure 4.
Work changes on burnout by organizational support.
Personal resources.
Three moderated mediation models determined whether the indirect effect of work changes on turnover intentions via burnout was moderated by telehealth self-efficacy, beliefs regarding telehealth, and perceptions of personal risk. The model exploring the moderating effect of telehealth self-efficacy fit better statistically than the unconditional model, as demonstrated by mostly lower fit indices (AIC=439.1, BIC=476.2, ABIC=428.9). The direct effect from the work changes by telehealth self-efficacy interaction to burnout was not statistically significant (=−.020, p=.680) and the indirect effect from work changes to turnover intentions through burnout was not moderated by telehealth self-efficacy (=−.013, 95% CI=−.068, .083).
The model exploring the moderating effect of telehealth beliefs fit similarly to the unconditional model (AIC=443.7, BIC=480.8, ABIC=433.5). The direct effect from the work changes by telehealth beliefs interaction to burnout was not statistically significant (=−.032, p=.582) and the indirect effect from work changes to turnover intentions through burnout was not moderated by telehealth beliefs (=−.022, 95% CI=−.071, .082).
The model exploring the moderating effect of perceptions of personal risk fit better than the unconditional model, as demonstrated by lower fit indices (AIC=434.7, BIC=471.9, ABIC=424.5). The direct effect from the work changes by the perceptions of personal risk interaction to burnout was not statistically significant (=−.116, p=.066) and the indirect effect from work changes to turnover intentions through burnout was not moderated by perceptions of personal risk (=−.079, 95% CI=−.142, −.009).
Discussion
The goal of this prospective study was to test the effects of work changes in providing mental health services as a result of the COVID-19 pandemic crisis on burnout and turnover intentions in a sample of mental health service providers. Based on theory and research on the JD-R model (Bakker & Demerouti, 2017), we tested whether several job and personal resources buffered the effects of those work changes on burnout. Results provided clear support for the unconditional mediated model and our hypotheses that work changes would have a significant indirect effect on turnover intentions through burnout. In other words, providers experiencing more work changes in terms of their tasks, settings, and teams were more likely to report higher levels of burnout and were subsequently more likely to be considering leaving their current position six to eight weeks later.
The results for job and personal resources as buffers were mixed, and hypotheses regarding the nature of the moderated effects were partially supported. None of the personal resources significantly interacted with work changes to predict burnout. However, two of the job resources (organizational trust and perceived organizational support) did show significant interactions as well as significant conditional indirect effects. It was anticipated that these resources would buffer the relationship between work changes and burnout, such that the positive relationship between work changes and burnout would be weaker when higher levels of these resources were present. However, the results instead showed that the relationship between work changes and burnout was weakest when job resources in the form of organizational trust and perceived organizational support were high. This finding was a function of providers with low organizational trust and low perceived organizational support reporting relatively high levels of burnout, even when work changes were low. Similar levels of burnout were found when work changes were high and job resource levels were also high. Only when the levels of work changes were low and the job resource levels were high were burnout levels relatively low.
These results suggest that the personal and job resources assessed in this research could not overcome the negative effect of work changes on burnout and turnover intentions. This could be due to the extreme job and interpersonal stress that resulted from the COVID-19 pandemic and the very rapid shift to telehealth. Thus, it appears that extreme work changes had particularly pernicious effects on providers, and thus, such changes should be avoided if at all possible. At the very least, the organizational research literature suggests that ample preparation, particularly in the form of increased information availability (Dean, Brandes, & Dharwadkar, 1998; Reicher, Wanous, & Austin, 1997; Wanberg & Banas, 2000) and employee involvement in the change process (Morgan & Zeffane, 2003; Sagie & Kozlowski, 1994; Wanous, Reichers, & Austin, 2000) may be helpful. However, not all changes can be avoided or prepared for, such as the situation with a global pandemic like COVID-19. To the extent possible, minimizing work changes experienced by employees is ideal.
When work changes were low, burnout experienced amongst staff members differed as a function of organizational trust and organizational support. Organizations hoping to reduce burnout experienced amongst their staff members, and reduce subsequent turnover intentions, can aim to improve organizational trust and organizational support. A recent framework by Shanafelt et al. (2020) asserted behaviors organizations and leaders can engage in to increase support to health care professionals particularly during the COVID-19 pandemic. Such messages and actions that may be generalized beyond the COVID-19 pandemic include listening and recognizing the concerns of health care professionals, and communicating expressions of gratitude toward health care professionals. If change to employee work setting is necessary, organizations are encouraged to limit other work changes experienced by employees, such as work tasks and/or teams. Additionally, Crawford et al. (2010) found that work hindrances can increase burnout more so than work challenges. When work changes are unavoidable, the extent to which organizations can limit hindrances in the context of change may be the best approach.
There are several limitations to this study, as well as directions for future research. The sample size was not large, and thus the power to detect the unconditional indirect effects was limited. As a result, the resources that were not significant could still play a role in the outcomes of work changes on burnout and turnover intentions. Although turnover intentions was measured 6–8 weeks after the other measures, the remaining data were cross-sectional, and although the causal ordering of the variables is in line with past theory and research, more structured longitudinal designs in future research would be preferred. Due to the novel nature of this outbreak and the related work changes, some measures were created or adapted for this study and do not yet have published psychometrics. Additional work on these measures, particularly on the formative measurement of work changes, is needed. Future research should also consider additional resources not addressed in this study to better understand how management can support providers when work changes are unavoidable and necessary. This study did not address the process of changing “back to normal,” and although providers may welcome returning back to their original tasks, settings, and teams, they may also have a number of hesitations if such changes are initiated with too much haste. Thus, future research should consider how leaders can best manage that transition and best provide providers the flexibility and resources needed.
Conclusion
The COVID-19 outbreak has drastically impacted the way in which mental health services are provided. Rapid adaptation and flexibility were required of mental health service systems and providers to continue service provision while minimizing the risk of COVID-19 transmission. To mitigate the negative impact of work changes on burnout and subsequent turnover intentions, organizations are encouraged to strengthen organizational trust and organizational support.
Impact and Implications.
Mental health service providers experiencing more COVID-19 work changes were more likely to report high levels of burnout and to consider leaving their current position.
This relationship varied as a function of job resources such that burnout was relatively low only when work changes were low AND job resources were high.
To minimize burnout and turnover, organizations should limit the number and magnitude of work changes to the extent possible.
Acknowledgments
Funding: This project was supported in part by a professional service contract with a state Division of Mental Health and Addictions (DMHA; #0000000000000000000039342) and the National Institute of Drug Abuse R01DA049891.
Footnotes
Manuscript prepared for special issue on psychiatric rehabilitation service workers’ well-being in the Psychiatric Rehabilitation Journal.
References
- Acker GM, (2010). The challenges in providing services to clients with mental illness: managed care, burnout and somatic symptoms among social workers. Community Mental Health Journal, 46(6), 591–600. [DOI] [PubMed] [Google Scholar]
- Akaike H (1981). Likelihood of a model and information criteria. Journal of Econometrics, 16(1), 3–14. [Google Scholar]
- Albrecht SL, & Andreetta M (2011). The influence of empowering leadership, empowerment and engagement on affective commitment and turnover intentions in community health service workers. Leadership in Health Services, 24, 228–237. [Google Scholar]
- Bakker AB, & Demerouti E (2017). Job demands-resources theory: Taking stock and looking forward. Journal of Occupational Health Psychology, 22(3), 273–285. 10.1037/ocp0000056. [DOI] [PubMed] [Google Scholar]
- Bakker AB, Demerouti E, & Euwema M (2005). Job resources buffer the impact of job demands on burnout. Journal of Occupational Health Psychology, 10, 170–180. 10.1037/1076-8998.10.2.170 [DOI] [PubMed] [Google Scholar]
- Bal PM, Chiaburu DS, & Jansen PGW (2009). Psychological contract breach and work performance: Is social exchange a buffer or an intensifier? Journal of Managerial Psychology, 25(3), 252–273. [Google Scholar]
- Bauer DJ, & Curran PJ (2005). Probing interactions in fixed and multilevel regression: Inferential and graphical techniques. Multivariate Behavioral Research, 40, 373–400. [DOI] [PubMed] [Google Scholar]
- Bliese PD (1998). Group size, ICC values, and group-level correlations: A simulation. Organizational Research Methods, 1, 355–373. [Google Scholar]
- Boyer SL, & Bond G,R (1991). Does assertive community treatment reduce burnout? A comparison with traditional case management. Mental Health Services Research, 1(1), 31–45. [Google Scholar]
- Burke RJ, & Richardsen AM (1993) Psychological burnout in organizations. In Golembiewski RT (Ed.), Handbook of organizational behavior (pp. 327–368). New York: Marcel Dekker. [Google Scholar]
- Carney J, Donovan R, Yurdin M, & Starr R (1993) Incidence of burnout among New York City intensive case managers: Summary of findings. Psychosocial Rehabilitation Journal, 16(4), 25–38. [Google Scholar]
- Chen G, & Bliese PD (2002). The role of different levels of leadership in predicting self- and collective efficacy: Evidence for discontinuity. Journal of Applied Psychology, 87(93), 549–556. [DOI] [PubMed] [Google Scholar]
- Coltman T, Devinney TM, Midgley DF, & Venaik S (2008). Formative versus reflective measurement models: Two applications of formative measurement. Journal of Business Research, 61(12), 1250–1262. [Google Scholar]
- Crawford ER, LePine JA, & Rich BL (2010). Linking job demands and resources to employee engagement and burnout: A theoretical extension and meta-analytic test. Journal of Applied Psychology, 95(5), 834–848. [DOI] [PubMed] [Google Scholar]
- Curran P, & Bauer D (2003). Simple intercepts, simple slopes, and regions of significance in HLM 2-way interactions. Retrieved August 20, 2020, from http://www.quantpsy.org/interact/hlm2.htm.
- Curran PJ, Bauer DJ, & Willoughby MT (2006). Testing and probing interactions in hierarchical linear growth models. In Bergeman CS & Boker SM (Eds.), The Notre Dame Series on Quantitative Methodology, Volume 1: Methodological issues in aging research (pp. 99–129). Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Dean JW, Brandes P, & Dharwadkar R (1998). Organizational cynicism. Academy of Management Review, 23, 341–352. [Google Scholar]
- Demerouti E, Bakker AB, Nachreiner F, & Schaufeli WB (2001) The job demands-resources model of burnout. Journal of Applied Psychology, 56(3), 499–512. [PubMed] [Google Scholar]
- Demerouti E, & Euwema M (2005). Job resources buffer the impact of job demands on burnout. Journal of Occupational Health Psychology, 10, 170–80. 10.1037/1076-8998.10.2.170. [DOI] [PubMed] [Google Scholar]
- Eisenberger R, Huntington R, Hutchison S, & Sowa D (1986). Perceived organizational support. Journal of Applied Psychology, 71(3), 500–507. [Google Scholar]
- Eisenberger R, Stinglhamber F, Vandenberghe C, Sucharski IL, & Rhoades L (2002). Perceived supervisor support: Contributions to perceived organizational support and employee retention. Journal of Applied Psychology, 87, 565–573. [DOI] [PubMed] [Google Scholar]
- Freudenberger HJ (1974). Staff burnout. Journal of Social Issues, 30, 159–165. [Google Scholar]
- Gabarro JJ, Athos J (1976). Interpersonal relations and communications. Prentice Hall, New York. [Google Scholar]
- Glazer S, & Beehr TA (2005). Consistency of implications of three role stressors across four countries. Journal of Organizational Behavior: The International Journal of Industrial, Occupational and Organizational Psychology and Behavior, 26(5), 467–487. [Google Scholar]
- Hoge MA, Morris JA, Daniels AS, Stuart GW, Huey LY, & Adams N (2007). An action plan for behavioral health workforce development: A framework for discussion. Rockville, MD. [Google Scholar]
- Jex SM, Bliese PD (1999) Efficacy beliefs as a moderator of the impact of work-related stressors: A multilevel study. Journal of Applied Psychology, 84, 349–361. [DOI] [PubMed] [Google Scholar]
- Kath LM, Stichler JF, & Ehrhart MG (2012). Moderators of the negative outcomes of nurse manager stress. JONA: The Journal of Nursing Administration, 42(4), 215–221. [DOI] [PubMed] [Google Scholar]
- Kim JJ, Brookman-Frazee L, Gellatly R, Stadnick N, Barnett ML, & Lau AS (2018). Predictors of burnout among community therapists in the sustainment phase of a system-driven implementation of multiple evidence-based practices in children’s mental health. Professional Psychology: Research and Practice, 49, 131–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristensen TS, Borritz M, Villadsen E, & Christensen KB (2005). The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work & Stress, 19, 192–207. [Google Scholar]
- Lau AS, & Brookman-Frazee L (2016). The 4KEEPS study: Identifying predictors of sustainment of multiple practices fiscally mandated in children’s mental health services. Implementation Science, 11, 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBreton JM, & Senter JL (2008). Answers to 20 questions about interrater reliability and interrater agreement. Organizational Research Methods, 11(4), 815–852. 10.1177/1094428106296642. [DOI] [Google Scholar]
- Mace S, Boccanelli A, & Dormond M (2018). The use of telehealth within behavioral health settings: Utilization, opportunities, and challenges. University of Michigan School of Public Health. [Google Scholar]
- Maslach C, & Pines A (1979). Burnout, the loss of human caring. In Pines A & Maslach C (Eds.), Experiencing social psychology (pp. 246–252). New York: Random House. [Google Scholar]
- Montgomery AP, Azuero A, Baernholdt M, Loan LA, Miltner RS, Qu H, & Raju D (2020). Nurse burnout predicts self-reported medication administration errors in acute care hospitals. Journal for Healthcare Quality, Volume Publish Ahead of Print - Issue -doi: 10.1097/JHQ.0000000000000274. [DOI] [PubMed] [Google Scholar]
- Moreno C, Wykes T, & Galderisi S (2020). How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry, 7, 813–824, 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan D, & Zeffane R (2003). Employee involvement, organizational change, and trust in management. International Journal of Human Resource Management, 14(1), 55–75. [Google Scholar]
- Morse G, Salyers MP, Rollins AL, Monroe-DeVita M, & Pfahler C (2012). Burnout in mental health services: a review of the problem and its remediation. Administration and Policy in Mental Health, 39(5), 341–352. 10.1007/s10488-011-0352-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, & Hayes AF (2007). Addressing moderated mediation hypotheses: theory, methods, and prescriptions. Multivariate Behavioral Research, 42(1), 185–227. 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, & Bauer DJ (2006). Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31, 437–448. [Google Scholar]
- Reicher AE, Wanous JP, & Austin JT (1997). Understanding and managing cynicism about organizational change. Academy of Management Executive, 11(1), 48–59. [Google Scholar]
- Robinson SL, Rousseau DM (1994). Violating the psychological contract: Not the exception but the norm. Journal of Organizational Behavior, 15, 245–259. 10.1002/job.4030150306. [DOI] [Google Scholar]
- Sagie A, & Krausz M (2003). What aspects of the job have most effect on nurses?. Human Resource Management Journal, 13(1), 46–62. [Google Scholar]
- Schaufeli WB, Bakker AB (2004) Job demands, job resource, and their relationship with burnout and engagement: A multi-sample study. Journal of Organizational Behavior, 25, 293–315. 10.1002/job.248. [DOI] [Google Scholar]
- Schwab RL, Jackson SE, Schuler RS (1986). Educator burnout: Sources and consequences. Educational Research Quarterly, 10, 15–30. [Google Scholar]
- Schwarz G (1978). Estimating the dimension of a model. The Annals of Statistics, 6(2), 461–464. [Google Scholar]
- Sagie A, & Koslowsky M (1994). Organizational attitudes and behaviors as a function of participation in strategic and tactical change decisions: An application of path-goal theory. Journal of Organizational Behavior, 15(1), 37–47. [Google Scholar]
- Seashore SE, Lawler EE, Mirvis P, & Cammann C (1982). Observing and measuring organizational change: A guide to field practice. New York: Wiley. [Google Scholar]
- Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, West CP, Sloan J, & Oreskovich MR (2012). Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine, 172(18), 1377–1385. 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- Shanafelt TD, Ripp J & Trockel M (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. Journal of the American Medical Association, 323(21), 2133–2134. [DOI] [PubMed] [Google Scholar]
- Shore JH, Schneck CD, & Mishkind MC (2020) Telepsychiatry and the coronavirus disease 2019 pandemic—current and future outcomes of the rapid virtualization of psychiatric care. JAMA Psychiatry; published online May 12. 10.1001/jamapsychiatry.2020.1643. [DOI] [PubMed] [Google Scholar]
- Smoot SL, & Gonzales JL (1995). Cost-effective communication skills training for state hospital employees. Psychiatric Services, 46(8), 819–822. [DOI] [PubMed] [Google Scholar]
- Stalker C, & Harvey C (2002). Professional burnout: A review of theory, research, and prevention. Partnerships for Children and Families Project. Wilfrid Laurier University. [Google Scholar]
- Wanberg CR, & Banas JT (2000). Predictors and outcomes of openness to changes in a reorganizing workplace. Journal of Applied Psychology, 85(1), 132–142. [DOI] [PubMed] [Google Scholar]
- Wanous JP, Reichers AE, & Austin JT (2000). Cynicism about organizational change. Group and Organization Management, 25(2), 132–153. [Google Scholar]
- Willness CR, Steel P, & Lee K (2007). A meta-analysis of the antecedents and consequences of workplace sexual harassment. Personnel Psychology, 60(1), 127–162. [Google Scholar]
- Wind TR, Rijkeboer M, Andersson G, & Riper H (2020). The COVID-19 pandemic: The ‘black swan’ for mental health care and a turning point for e-health. Internet Interventions, 20, 100317. 10.1016/j.invent.2020.100317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windon SR, Cochran GR, Scheer SD, & Rodriguez MT (2019). Factors affecting turnover intention of Ohio State University extension program assistants. Journal of Agricultural Education, 60(3), 109–127. [Google Scholar]
- World Health Organization (2020). International statistical classification of diseases and related health problems (11th ed.). https://icd.who.int/. [Google Scholar]
- World Health Organization. (2019). QD 85 Burn-out. Retrieved August 29, 2020, from https://icd.who.int/browse11/l-m/en. [Google Scholar]
- Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, Liu X, Fuller CJ, Susser E, & Lu J (2009). The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. The Canadian Journal of Psychiatry, 54, 302–311. [DOI] [PMC free article] [PubMed] [Google Scholar]