Abstract
Delineating the association of age and cortical thickness in healthy individuals is critical given the association of cortical thickness with cognition and behavior. Previous research has shown that robust estimates of the association between age and brain morphometry require large‐scale studies. In response, we used cross‐sectional data from 17,075 individuals aged 3–90 years from the Enhancing Neuroimaging Genetics through Meta‐Analysis (ENIGMA) Consortium to infer age‐related changes in cortical thickness. We used fractional polynomial (FP) regression to quantify the association between age and cortical thickness, and we computed normalized growth centiles using the parametric Lambda, Mu, and Sigma method. Interindividual variability was estimated using meta‐analysis and one‐way analysis of variance. For most regions, their highest cortical thickness value was observed in childhood. Age and cortical thickness showed a negative association; the slope was steeper up to the third decade of life and more gradual thereafter; notable exceptions to this general pattern were entorhinal, temporopolar, and anterior cingulate cortices. Interindividual variability was largest in temporal and frontal regions across the lifespan. Age and its FP combinations explained up to 59% variance in cortical thickness. These results may form the basis of further investigation on normative deviation in cortical thickness and its significance for behavioral and cognitive outcomes.
Keywords: aging, cortical thickness, development, trajectories
We used cross‐sectional data from 17,075 individuals aged 3–90 years from the Enhancing Neuroimaging Genetics through Meta‐Analysis (ENIGMA) Consortium to infer age‐related changes in cortical thickness.

1. INTRODUCTION
In the last two decades, there has been a steady increase in the number of studies of age‐related changes in cerebral morphometry (Ducharme, et al., 2015; Good et al., 2001; Mutlu et al., 2013; Salat et al., 2004; Shaw et al., 2008; Storsve et al., 2014; Thambisetty et al., 2010; Wierenga, Langen, Oranje, & Durston, 2014) as a means to understand genetic and environmental influences on the human brain (Grasby, 2020; Modabbernia et al., 2020). Here we focus specifically on cortical thickness, as assessed using magnetic resonance imaging (MRI), as this measure has established associations with behavior and cognition in healthy populations (Goh et al., 2011; Schmitt et al., 2019; Shaw et al., 2006) and with disease mechanisms implicated in neuropsychiatric disorders (Boedhoe, et al., 2018; Hibar et al., 2018; Hoogman et al., 2019; Schmaal et al., 2017; Thompson et al., 2007; van Erp et al., 2018; van Rooij et al., 2018; Whelan et al., 2018).
Structural MRI is the most widely used neuroimaging method in research and clinical settings because of its excellent safety profile, ease of data acquisition and high patient acceptability. Thus, establishing the typical patterns of age‐related changes in cortical thickness as reference data could be a significant first step in the translational application of neuroimaging. The value of reference data is firmly established in medicine where deviations from an expected range are used to trigger further investigations or interventions. A classic example is the body mass index (BMI) which has been instrumental in informing about risk for relating to cardio‐metabolic outcomes (Aune et al., 2016).
There is significant uncertainty about the shape and interindividual variability of the association between age and cortical thickness. Prior studies have reported linear and nonlinear associations (e.g., Hedman, van Haren, Schnack, Kahn, & Hulshoff Pol, 2012; Mills et al., 2016) that may be influenced by sex (Paus, 2010; Raz, Ghisletta, Rodrigue, Kennedy, & Lindenberger, 2010; Wierenga et al., 2020). The present study harnessed the power of the Enhancing Neuroimaging Genetics through Meta‐Analysis (ENIGMA) Consortium, a multinational collaborative network of researchers organized into working groups, which conducts large‐scale analyses integrating data from over 250 institutions (Thompson et al., 2017; Thompson et al., 2020). Within ENIGMA, the focus of the Lifespan Working group is to delineate age‐associations in brain morphometric measures extracted from MRI images using standardized protocols and unified quality control procedures harmonized and validated across all participating sites. The ENIGMA Lifespan data set is the largest sample of healthy individuals available worldwide that offers the most comprehensive coverage of the human lifespan. This distinguishes the ENIGMA Lifespan data set from other imaging samples, such as the UK Biobank (http://www.ukbiobank.ac.uk) which includes individuals over 40 years of age. In the present study, we used MRI data from 17,075 healthy participants aged 3–90 years to infer age‐associated trajectories of cortical thickness. We also estimated regional interindividual variability in cortical thickness across the lifespan because it represents a major source of inter‐study variation (Raz et al., 2010; Wierenga et al., 2020). Based on prior literature, our initial hypotheses were that in most regions the relationship between age and thickness will follow an inverse U‐shape and will be influenced by sex.
2. MATERIALS AND METHODS
2.1. Study samples
De‐identified demographic and cortical thickness data from 83 worldwide samples (Figure 1) were pooled to create the data set analyzed in this study. For samples from longitudinal studies, only baseline MRI scans were considered. The pooled sample comprised 17,075 participants (52% female) aged 3–90 years; only participants with complete data were included (Table 1). All participants had been screened to exclude psychiatric disorders, medical and neurological morbidity and cognitive impairment. Information on the screening protocols and eligibility criteria is provided in Table S1.
FIGURE 1.
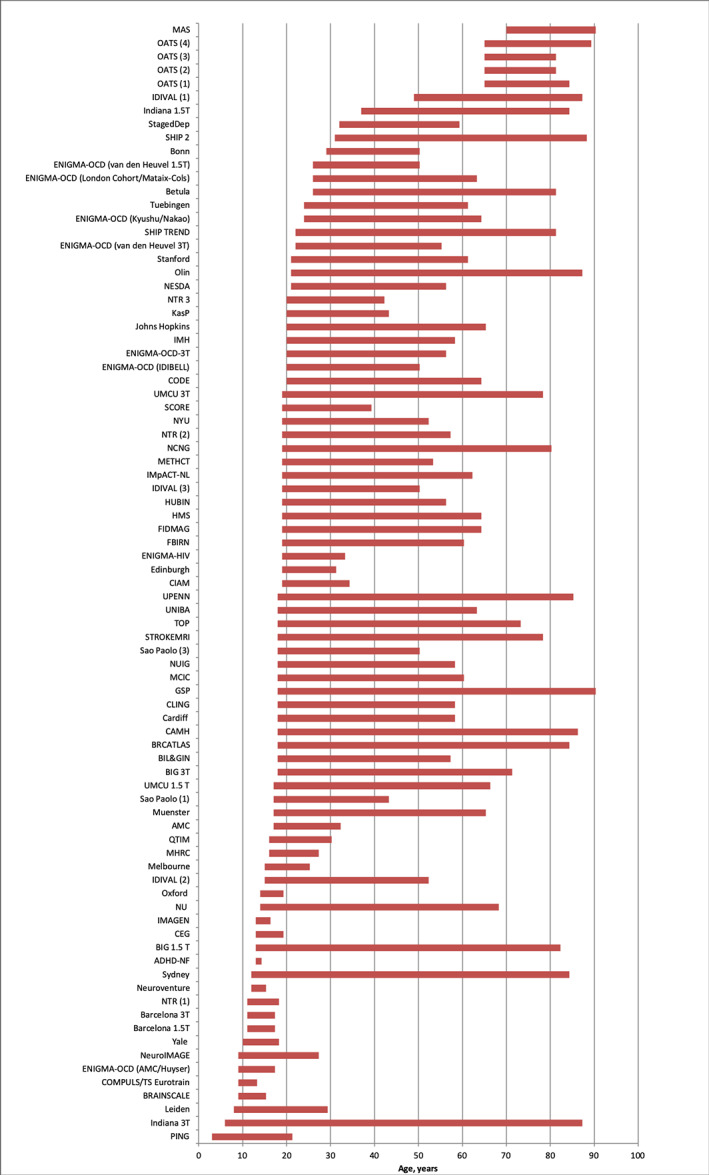
ENIGMA Lifespan samples. Abbreviations are explained in Table 1; further details of each sample are provided in the supplemental material
TABLE 1.
Characteristics of the included samples
| Sample | Age, mean, years | Age, SD, years | Age range | Sample N | Male N | Female N | |
|---|---|---|---|---|---|---|---|
| ADHD NF | 14 | 0.7 | 13 | 14 | 3 | 1 | 2 |
| AMC | 23 | 3.4 | 17 | 32 | 99 | 65 | 34 |
| Barcelona 1.5 T | 15 | 1.9 | 11 | 17 | 24 | 10 | 14 |
| Barcelona 3 T | 15 | 2.2 | 11 | 17 | 31 | 13 | 18 |
| Betula | 62 | 12.4 | 26 | 81 | 231 | 105 | 126 |
| BIG 1.5 T | 28 | 14.3 | 13 | 82 | 1,319 | 657 | 662 |
| BIG 3 T | 24 | 8.1 | 18 | 71 | 1,291 | 553 | 738 |
| BIL&GIN | 27 | 7.7 | 18 | 57 | 452 | 220 | 232 |
| Bonn | 39 | 6.5 | 29 | 50 | 175 | 175 | 0 |
| BRAINSCALE | 10 | 1.4 | 9 | 15 | 172 | 102 | 70 |
| BRCATLAS | 40 | 17.2 | 18 | 84 | 163 | 84 | 79 |
| CAMH | 44 | 19.3 | 18 | 86 | 141 | 72 | 69 |
| Cardiff | 26 | 7.8 | 18 | 58 | 265 | 78 | 187 |
| CEG | 16 | 1.8 | 13 | 19 | 31 | 31 | 0 |
| CIAM | 27 | 4.2 | 19 | 34 | 24 | 13 | 11 |
| CLING | 25 | 5.3 | 18 | 58 | 323 | 132 | 191 |
| CODE | 40 | 13.3 | 20 | 64 | 72 | 31 | 41 |
| COMPULS/TS Eurotrain | 11 | 1 | 9 | 13 | 42 | 29 | 13 |
| Edinburgh | 24 | 2.9 | 19 | 31 | 55 | 20 | 35 |
| ENIGMA‐HIV | 25 | 4.3 | 19 | 33 | 30 | 16 | 14 |
| ENIGMA‐OCD (AMC/Huyser) | 14 | 2.8 | 9 | 17 | 6 | 2 | 4 |
| ENIGMA‐OCD (IDIBELL) | 33 | 10.4 | 20 | 50 | 20 | 8 | 12 |
| ENIGMA‐OCD (Kyushu/Nakao) | 45 | 14.1 | 24 | 64 | 16 | 6 | 10 |
| ENIGMA‐OCD (London Cohort/Mataix‐Cols) | 38 | 11.6 | 26 | 63 | 10 | 2 | 8 |
| ENIGMA‐OCD (van den Heuvel 1.5 T) | 41 | 12.9 | 26 | 50 | 3 | 0 | 3 |
| ENIGMA‐OCD (van den Heuvel 3 T) | 36 | 10.9 | 22 | 55 | 8 | 4 | 4 |
| ENIGMA‐OCD‐3 T‐CONTROLS | 32 | 11 | 20 | 56 | 17 | 4 | 13 |
| FBIRN | 37 | 11.4 | 19 | 60 | 164 | 117 | 47 |
| FIDMAG | 38 | 10.1 | 19 | 64 | 123 | 54 | 69 |
| GSP | 27 | 16.5 | 18 | 90 | 2008 | 893 | 1,115 |
| HMS | 40 | 12.2 | 19 | 64 | 55 | 21 | 34 |
| HUBIN | 42 | 8.8 | 19 | 56 | 102 | 69 | 33 |
| IDIVAL (1) | 65 | 9.8 | 49 | 87 | 34 | 13 | 21 |
| IDIVAL (3) | 30 | 7.8 | 19 | 50 | 104 | 63 | 41 |
| IDIVAL(2) | 28 | 7.6 | 15 | 52 | 80 | 50 | 30 |
| IMAGEN | 14 | 0.4 | 13 | 16 | 1722 | 854 | 868 |
| IMH | 32 | 9.8 | 20 | 58 | 73 | 48 | 25 |
| IMpACT‐NL | 36 | 12.1 | 19 | 62 | 91 | 27 | 64 |
| Indiana 1.5 T | 62 | 11.7 | 37 | 84 | 49 | 9 | 40 |
| Indiana 3 T | 27 | 19.7 | 6 | 87 | 199 | 95 | 104 |
| Johns Hopkins | 44 | 12.5 | 20 | 65 | 85 | 42 | 43 |
| KaSP | 27 | 5.7 | 20 | 43 | 32 | 15 | 17 |
| Leiden | 17 | 4.8 | 8 | 29 | 572 | 279 | 293 |
| MAS | 79 | 4.7 | 70 | 90 | 385 | 176 | 209 |
| MCIC | 32 | 12.1 | 18 | 60 | 91 | 61 | 30 |
| Melbourne | 20 | 2.9 | 15 | 25 | 70 | 39 | 31 |
| METHCT | 27 | 6.5 | 19 | 53 | 39 | 29 | 10 |
| MHRC | 22 | 3.1 | 16 | 27 | 27 | 27 | 0 |
| Muenster | 35 | 12.1 | 17 | 65 | 744 | 323 | 421 |
| NCNG | 51 | 16.9 | 19 | 80 | 345 | 110 | 235 |
| NESDA | 40 | 9.7 | 21 | 56 | 65 | 23 | 42 |
| NeuroIMAGE | 17 | 3.4 | 9 | 27 | 252 | 115 | 137 |
| Neuroventure | 14 | 0.6 | 12 | 15 | 137 | 62 | 75 |
| NTR (1) | 15 | 1.4 | 11 | 18 | 37 | 14 | 23 |
| NTR (2) | 34 | 10.4 | 19 | 57 | 112 | 42 | 70 |
| NTR (3) | 30 | 5.9 | 20 | 42 | 29 | 11 | 18 |
| NU | 33 | 14.8 | 14 | 68 | 79 | 46 | 33 |
| NUIG | 36 | 11.5 | 18 | 58 | 92 | 53 | 39 |
| NYU | 31 | 8.7 | 19 | 52 | 51 | 31 | 20 |
| OATS (1) | 71 | 5.6 | 65 | 84 | 80 | 53 | 27 |
| OATS (2) | 69 | 5.1 | 65 | 81 | 13 | 7 | 6 |
| OATS (3) | 69 | 4 | 65 | 81 | 116 | 64 | 52 |
| OATS (4) | 70 | 4.7 | 65 | 89 | 90 | 63 | 27 |
| Olin | 36 | 13 | 21 | 87 | 582 | 231 | 351 |
| Oxford | 16 | 1.4 | 14 | 19 | 37 | 18 | 19 |
| PING | 12 | 4.8 | 3 | 21 | 431 | 223 | 208 |
| QTIM | 23 | 3.3 | 16 | 30 | 308 | 96 | 212 |
| Sao Paolo | 28 | 6.1 | 17 | 43 | 51 | 32 | 19 |
| Sao Paolo‐2 | 31 | 7.6 | 18 | 50 | 58 | 30 | 28 |
| SCORE | 25 | 4.3 | 19 | 39 | 44 | 17 | 27 |
| SHIP 2 | 55 | 12.3 | 31 | 88 | 306 | 172 | 134 |
| SHIP TREND | 50 | 13.7 | 22 | 81 | 628 | 355 | 273 |
| StagedDep | 48 | 8.1 | 32 | 59 | 23 | 7 | 16 |
| Stanford | 45 | 12.6 | 21 | 61 | 8 | 4 | 4 |
| STROKEMRI | 45 | 22.1 | 18 | 78 | 52 | 19 | 33 |
| Sydney | 39 | 22.1 | 12 | 84 | 157 | 65 | 92 |
| TOP | 35 | 9.9 | 18 | 73 | 303 | 159 | 144 |
| Tuebingen | 40 | 12.4 | 24 | 61 | 38 | 12 | 26 |
| UMCU 1.5 T | 33 | 12.5 | 17 | 66 | 278 | 158 | 120 |
| UMCU 3 T | 44 | 14 | 19 | 78 | 144 | 69 | 75 |
| UNIBA | 27 | 9.1 | 18 | 63 | 130 | 67 | 63 |
| UPENN | 37 | 13.1 | 18 | 85 | 115 | 42 | 73 |
| Yale | 14 | 2.7 | 10 | 18 | 12 | 5 | 7 |
| Total | 31 | 18.2 | 3 | 90 | 17,075 | 8,212 | 8,863 |
Abbreviations: ADHD‐NF, Attention Deficit Hyperactivity Disorder‐ Neurofeedback Study; AMC, Amsterdam Medisch Centrum; Basel, University of Basel; Barcelona, University of Barcelona; Betula, Swedish longitudinal study on aging, memory, and dementia; BIG, Brain Imaging Genetics; BIL&GIN, a multimodal multidimensional database for investigating hemispheric specialization; Bonn, University of Bonn; BrainSCALE, Brain Structure and Cognition: an Adolescence Longitudinal twin study; CAMH, Centre for Addiction and Mental Health; Cardiff, Cardiff University; CEG, Cognitive‐experimental and Genetic study of ADHD and Control Sibling Pairs; CIAM, Cortical Inhibition and Attentional Modulation study; CLiNG, Clinical Neuroscience Göttingen; CODE, formerly Cognitive Behavioral Analysis System of Psychotherapy (CBASP) study; Edinburgh, The University of Edinburgh; ENIGMA‐HIV, Enhancing NeuroImaging Genetics through Meta‐Analysis‐Human Immunodeficiency Virus Working Group; ENIGMA‐OCD, Enhancing NeuroImaging Genetics through Meta‐Analysis‐ Obsessive Compulsive Disorder Working Group; FBIRN, Function Biomedical Informatics Research Network; FIDMAG, Fundación para la Investigación y Docencia Maria Angustias Giménez; GSP, Brain Genomics Superstruct Project; HMS, Homburg Multidiagnosis Study; HUBIN, Human Brain Informatics; IDIVAL, Valdecilla Biomedical Research Institute; IMAGEN, the IMAGEN Consortium; IMH=Institute of Mental Health, Singapore; IMpACT, The International Multicentre persistent ADHD Genetics Collaboration; Indiana, Indiana University School of Medicine; Johns Hopkins, Johns Hopkins University; KaSP, The Karolinska Schizophrenia Project; Leiden, Leiden University; MAS, Memory and Aging Study; MCIC, MIND Clinical Imaging Consortium formed by the Mental Illness and Neuroscience Discovery (MIND) Institute now the Mind Research Network; Melbourne, University of Melbourne; Meth‐CT, study of methamphetamine users, University of Cape Town; MHRC, Mental Health Research Center; Muenster, Muenster University; NESDA, The Netherlands Study of Depression and Anxiety; NeuroIMAGE, Dutch part of the International Multicenter ADHD Genetics (IMAGE) study; Neuroventure: the imaging part of the Co‐Venture Trial funded by the Canadian Institutes of Health Research (CIHR); NCNG, Norwegian Cognitive NeuroGenetics sample; NTR, Netherlands Twin Register; NU, Northwestern University; NUIG, National University of Ireland Galway; NYU, New York University; OATS, Older Australian Twins Study; Olin, Olin Neuropsychiatric Research Center; Oxford, Oxford University; QTIM, Queensland Twin Imaging; Sao Paulo, University of Sao Paulo; SCORE, University of Basel Study; SHIP‐2 and SHIP TREND, Study of Health in Pomerania; Staged‐Dep, Stages of Depression Study; Stanford, Stanford University; StrokeMRI, Stroke Magnetic Resonance Imaging; Sydney, University of Sydney; TOP, Tematisk Område Psykoser (Thematically Organized Psychosis Research); TS‐EUROTRAIN, European‐Wide Investigation and Training Network on the Etiology and Pathophysiology of Gilles de la Tourette Syndrome; Tuebingen, University of Tuebingen; UMCU, Universitair Medisch Centrum Utrecht; UNIBA, University of Bari Aldo Moro; UPENN, University of Pennsylvania; Yale, Yale University.
2.2. Image acquisition and processing
Prior to pooling the data used in this study, researchers at each participating institution (a) used the ENIGMA MRI analysis protocols, which are based on FreeSurfer (http://surfer.nmr.mgh.harvard.edu), to compute the cortical thickness of 68 regions from high‐resolution T1‐weighted MRI brain scans collected at their site; (b) inspected all images by overlaying the cortical parcellations on the participants' anatomical scans and excluded improperly segmented scans; (c) identified outliers using five median absolute deviations (MAD) of the median value (additional details in the supplement). Information on scanner vendor, magnetic field strength, FreeSurfer version and acquisition parameters for each sample as provided by the participating institutions is detailed in Table S1.
2.3. Analysis of age‐related changes in cortical thickness
We modeled the effect of age on regional cortical thickness using higher order fractional polynomial (FP) regression analyses (Royston & Altman, 1994; Sauerbrei, Meier‐Hirmer, Benner, & Royston, 2006) implemented in STATA software version 14.0 (Stata Corp., College Station, TX). FP regression is one of the most flexible methods to study the effect of continuous variables on a response variable (Royston & Altman, 1994; Sauerbrei et al., 2006). FP allows for testing a broad family of shapes and multiple turning points while simultaneously providing a good fit at the extremes of the covariates (Royston & Altman, 1994). Prior to FP regression analysis, cortical thickness values were harmonized between sites using the ComBat method in R (Fortin et al., 2018). ComBat uses an empirical Bayes method to adjust for inter‐scanner variability in the data while preserving biological variability. As the effect of scanner was adjusted using ComBat, we only included sex as a covariate in the regression models. Additionally, standard errors were adjusted for the effect of scanner in the FP regression. We centered the data from each brain region so that the intercept of an FP was zero for all covariates. We used a predefined set of power terms (−2, −1, −0.5, 0.5, 1, 2, 3) and the natural logarithm function, and up to four power combinations to identify the best fitting model. FP for age was written as age(p1, p2, …p6)′β where p in age (p1, p2, …p6) refers to regular powers except age (0) which refers to ln(age). Powers can be repeated in FP; each time a power s repeated, it is multiplied by another ln(age). As an example:
494 models were trained for each region. Model comparison was performed using a partial F‐test and the lowest degree model with the smallest p‐value was selected as the optimal model. Following permutation, critical alpha value was set at .01 to decrease the probability of over‐fitting. The age at maximum cortical thickness for each cortical region was the maximum fitted value of the corresponding optimal FP model.
Further, we divided the data set into three age‐groups corresponding to early (3–29 years), middle (30–59 years) and late life (60–90 years). Within each age‐group, we calculated Pearson's correlation coefficient between age and regional cortical thickness. Finally, we used the cocor package in R to obtain P‐values for the differences in correlation coefficients between males and females in each age‐group.
2.4. Interindividual variation in cortical thickness
The residuals of the FP regression models for each cortical region were normally distributed. Using one‐way analysis of variance we extracted the residual variance around the optimal fitted FP regression model so as to identify age‐group differences in interindividual variation for each cortical region. Separately for each age‐group (t), we calculated the mean age‐related variance of each cortical region using where e 2 denotes the squared residual variance of that region around the best fitting FP regression line for each individual (i) of that age‐group, and n the number of observations in that age‐group. Because the square root of the squared residuals was positively skewed, we applied a natural logarithm transformation to the calculated variance. To account for multiple comparisons (68 regions assessed in three age‐groups), a Bonferroni adjusted p‐value of 0.0007 as chosen as a cut‐off for a significant F‐test. To confirm that the scanner effect did not drive the interindividual variability analyses, we also conducted a meta‐analysis of the SD of the regional cortical thickness in each age‐group, following previously validated methodology (Senior, et al., 2016). To test whether interindividual variability is a function of surface area (and possibly measurement error by FreeSurfer) we plotted the SD values of each region against their corresponding average surface area.
2.5. Centile values of cortical thickness
We calculated the centiles (0.4, 1, 2.5, 5, 10, 25, 50, 75, 90, 95, 97.5, 99, 99.6) for each regional cortical thickness measure by sex and hemisphere as normalized growth centiles using parametric Lambda (λ), Mu (μ), Sigma (σ) (LMS) method (Cole and Green, 1992) in the Generalized Additive Models for Location, Scale and Shape (GAMLSS) package in R (http://cran.r-project.org/web/packages/gamlss/index.html) (Rigby & Stasinopoulos, 2005; Stasinopoulos & Rigby, 2007). LMS is considered a powerful method for estimating centile curves based on the distribution of a response variable at each covariate value (in this case age). GAMLSS uses a penalized maximum likelihood function to estimate parameters of smoothness (effective degrees of freedom) which are then used to estimate the λ, μ, and σ parameters. The goodness of fit for these parameters in the GAMLSS algorithm is established by minimizing the Generalized Akaike Information Criterion (GAIC) index.
3. RESULTS
3.1. Association of age with cortical thickness
Figure 2 shows the shape of the association of age with cortical thickness in each lobe, while the corresponding information on all cortical regions is provided in File S1. For most regions, the highest value for cortical thickness was observed in childhood; age and cortical thickness showed a negative linear correlation, with the slope being steep until the third decade of life (Table S2). By contrast, the entorhinal and temporopolar cortices showed an inverse U‐shaped relation with age bilaterally while in the anterior cingulate cortex (ACC) showed an attenuated U‐shape. In general, age and its FP combinations explained up to 59% of the variance in mean cortical thickness (Table S2). Age explained the smallest proportion of the variance for entorhinal (1–2%) and temporopolar (2–3%) cortices but the largest proportion of variance for the superior frontal and precuneus gyri (50–52%).
FIGURE 2.
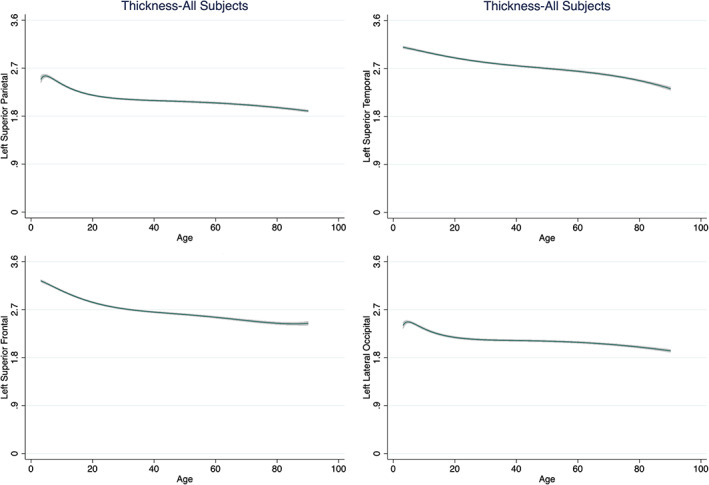
Illustrative Fractional Polynomial Plots for the association of age and cortical thickness. We present exemplars from each lobe as derived from fractional polynomial analyses of the entire data set. Details regarding the association of age and thickness for all cortical regions (for the entire data set and separately for males and females) are given in the supplementary material
We observed significant sex differences in the slopes of age‐related mean cortical thickness reduction in the middle‐life group (30–59 years) which were steeper for males (r = −.39 to −.38) than for females (r = −.27). In the early‐life group (3–29 years), the age‐related slopes for mean cortical thickness were not different between males (r = −.59) and females (r = −.56). Similarly, in the late‐life group (61–90 years) there were no meaningful sex differences (male: r‐range = −.30 to −.29; female: r‐range= = − .33 to −.31).
Further, sex differences were also noted at the regional level in the early‐ and middle‐life groups. In the early‐life group, the slope of the association between age and cortical thickness was steeper in males than in females in the bilateral cuneus, lateral occipital, lingual, superior parietal, postcentral, and paracentral, precuneus, and pericalcarine gyri (all p < .0007). In middle‐life age‐group, the slope was steeper in males than in females in the bilateral pars orbitalis and pars triangularis as well as left isthmus of the cingulate, pars opercularis, precuneus, rostral middle frontal, and supramarginal, and right fusiform, inferior temporal, inferior parietal, lateral occipital, lateral orbitofrontal, rostral anterior cingulate, superior frontal, supramarginal regions, and the insula (all p < .0002) (Figures 3 and S1, Table S3).
FIGURE 3.
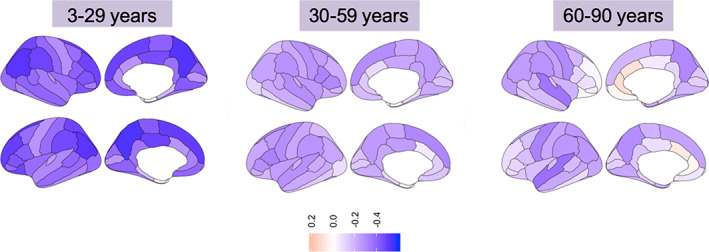
Correlation between age and cortical thickness across age‐groups. Left panel: early life age‐group (3–29 years); Middle panel: middle life age‐group (30–59 years); Right panel: late life age‐group (60–90 years). Blue hues = negative correlations; Red hues = positive correlations
3.2. Interindividual variation in cortical thickness
Across age‐groups (early, middle, and late life), interindividual variability in regional cortical thickness, as measured by pooled SD, was between 0.1 and 0.2 mm. Details are provided in Table S4, Figures 4 and S2. High interindividual variation was mainly confined bilaterally in the entorhinal, parahippocampal, transverse temporal, temporopolar, frontopolar, anterior cingulate and isthmus, and pars orbitalis regions. We confirmed the replicability of these findings in each age‐group by conducting meta‐analysis following the procedures set‐out by Senior et al. (2016).
FIGURE 4.
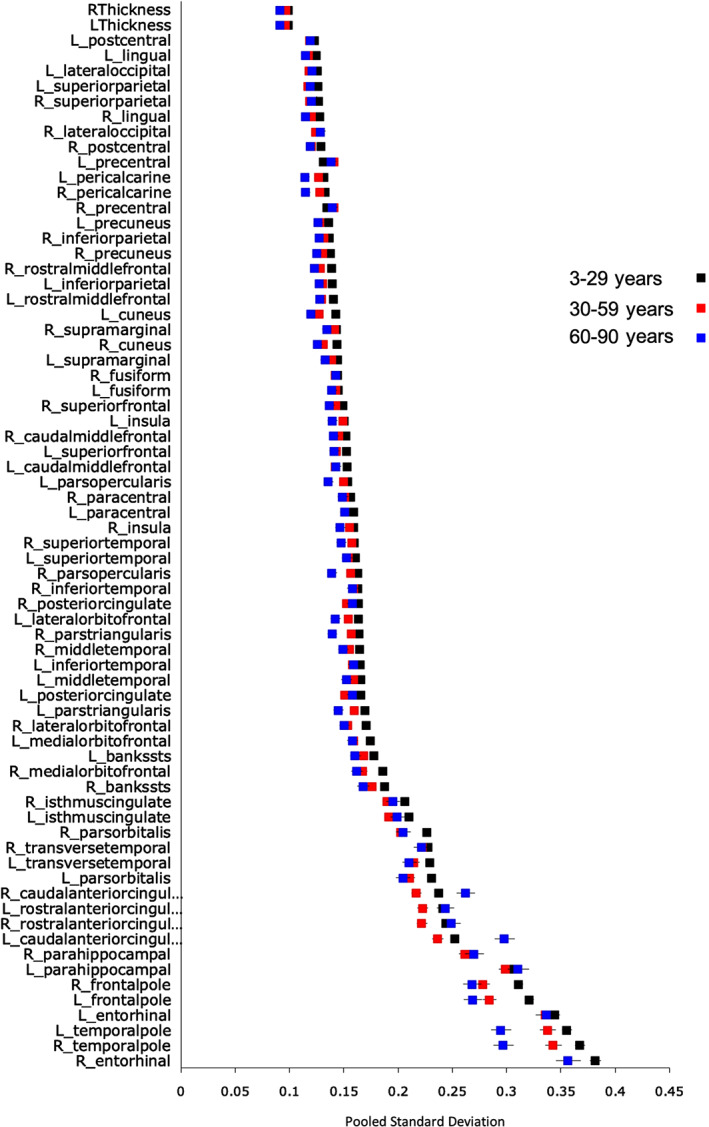
Interindividual variability in cortical thickness across the lifespan. The plot presents the pooled SD in regional cortical thickness values om the early, middle and late life age‐groups
Finally, we observed a nonlinear association between regional cortical surface area and interindividual variability with variability being typically higher in regions with smaller surface areas (Figure S3).
3.3. Centile curves of cortical thickness
Representative centiles curves for each lobe are presented in Figure 5. Centile values for the thickness of each cortical region, stratified by sex and hemisphere, are provided in Tables S5 to S7 and File S2.
FIGURE 5.
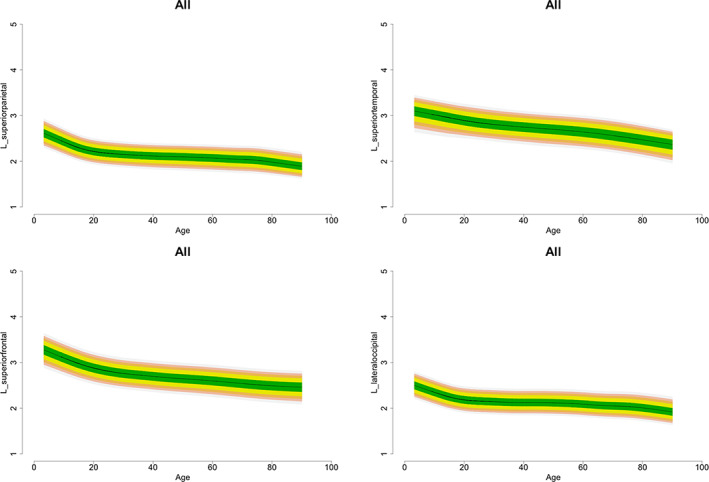
Illustrative normative centile curves of cortical thickness. We present exemplar sets of centile curves for each lobe as derived from LMS of the entire data set. Normative centile curves for all cortical regions (for the entire data set and separately for males and females) are given in the supplementary material
4. DISCUSSION
In the present study, we provide the most comprehensive characterization of the association between age and regional cortical thickness across the human lifespan based on multiple analytic methods (i.e., FP analysis, meta‐analysis and centile calculations) and the largest data set of cortical thickness measures available from healthy individuals aged 3 to 90 years. In addition to sample size, the study benefited from the standardized and validated protocols for data extraction and quality control that are shared by all ENIGMA sites and have supported all published ENIGMA structural MRI studies (Thompson et al., 2020).
Most regional cortical thickness measures reached their maximum value between 3 and 10 years of age, showed a steep decrease during the second and third decades of life and an attenuated or plateaued slope thereafter. This pattern was independent of the hemisphere and sex. A recent review (Walhovd, Fjell, Giedd, Dale, & Brown, 2017) has highlighted contradictions between studies that report an increase in cortical thickness during early childhood and studies that report a decrease in cortical thickness during the same period. The results from the current study help reconcile previous findings as they show that the median age at maximum thickness for most cortical regions is in the lower bound of the age‐range examined here. However, these findings must be considered in the context to the fewer data points available for those below the age of 10 years.
The general pattern of greater cortical thinning with advancing age was similar in both sexes. When participants were divided in early‐, middle‐ and late‐life groups, sex differences in the slope between age and cortical thickness was noted primarily for the mid‐life group. In this age‐group, which included individuals aged 30–59 years, the slope was steeper in males than in females. This sex‐difference has not been reported in other studies (Fjell et al., 2015; Raz et al., 2005; Raz et al., 2010; Storsve et al., 2014) which generally had smaller samples (<2000), shorter observation periods or examined age‐related trajectories of cortical thickness after the effect of sex was regressed‐out (e.g., Fjell et al., 2009). Although the sex‐differences reported here may be incidental, they resonate with findings of generally higher cognitive reserve in women as they enter later‐life (Mauvais‐Jarvis et al., 2020).
In the entorhinal and temporopolar cortex there were minimal age‐related changes until the seventh to eighth decades of life; thereafter both regions showed age‐related decrease in cortical thickness. Although the FreeSurfer estimation of cortical thickness in these regions is often considered suboptimal (compared with the rest of the brain), we note that our findings are consistent with a prior multicenter study of 1,660 healthy individuals (Hasan et al., 2016). Further, the current study supports results from the National Institutes of Health MRI study of 384 individuals that found no significant change in the bilateral entorhinal and medial temporopolar cortex between the ages of 4–22 years (Ducharme et al., 2016). A further study of 207 healthy adults aged 23–87 years also showed no significant cortical thinning in the entorhinal cortex until the sixth decade of life (Storsve et al., 2014). These observations suggest that the cortex of the entorhinal and temporopolar regions is largely preserved across the lifespan in healthy individuals. Both these regions contribute to episodic memory while the temporopolar region is also involved in semantic memory (Rolls, 2018). Degenerative changes of the temporopolar cortex have been reliably associated with semantic dementia, which is characterized by loss of conceptual knowledge about real‐world items (Hodges & Patterson, 2007). The integrity and resting metabolic rate of the temporopolar cortex decrease with age (Allen, Bruss, Brown, & Damasio, 2005; Eberling et al., 1995; Fjell et al., 2009), and lower perfusion rates in this region correlate with cognitive impairment in patients with Alzheimer's disease (AD) (Alegret et al., 2010). Entorhinal cortical thickness is a reliable marker of episodic memory performance (Schultz, Sommer, & Peters, 2012) and entorhinal cortex volume and metabolism are reduced in patients with AD and mild cognitive impairment (Dickerson et al., 2009; Zhou, Zhang, Zhao, Qian, & Dong, 2016). We therefore infer that “accelerated” entorhinal and temporopolar cortical thinning may be a marker of age‐related cognitive decline; as they grow older, individuals at risk of cognitive decline may show a gradual leftward shift in the distribution of the cortical thickness of these regions which coincides with the exponential age‐related increase in the incidence of AD in the later decades of life (Reitz & Mayeux, 2014).
The thickness of the ACC showed an attenuated U‐shaped association with age. This observation replicates an earlier finding in 178 healthy individuals aged 7–87 years (Sowell, et al., 2007). The U‐shaped age trajectory of ACC thickness might explain divergent findings in previous studies that have reported age‐related increases (Abe et al., 2008; Salat et al., 2004), age‐related reductions or no change (Brickman, Habeck, Zarahn, Flynn, & Stern, 2007; Ducharme et al., 2016; Good et al., 2001; Vaidya, Paradiso, Boles Ponto, McCormick, & Robinson, 2007).
A consistently higher degree of interindividual variation was observed in the most rostral frontal regions (frontopolar cortex and pars orbitalis), in the ACC and in several temporal regions (entorhinal, parahippocampal, temporopolar, and transverse temporal cortex). To some degree, greater variability in several of these regions may reflect measurement challenges associated with their small size (Figure S3). Nevertheless, the pattern observed suggests that greater interindividual variability may be a feature of proisocortical and periallocortical regions (in the cingulate and temporal cortices) that are anatomically connected to prefrontal isocortical regions, and particularly the frontopolar cortex. This prefrontal isocortical region is considered evolutionarily important based on its connectivity and function in humans and nonhuman primates (Ongür, Ferry, & Price, 2003; Semendeferi et al., 2011). The frontopolar region has several microstructural characteristics, such as a higher number and greater width of minicolumns and greater interneuron space, which are conducive to facilitating neuronal connectivity (Semendeferi et al., 2011). According to the popular “gateway” hypothesis, the lateral frontopolar cortex implements processing of external information (“stimulus‐oriented” processing) while the medial frontopolar cortex attends to self‐generated or maintained representations (“stimulus‐independent” processing) (Burgess, Dumontheil, & Gilbert, 2007). Stimulus‐oriented processing in the frontopolar cortex is focused on multitasking and goal‐directed planning while stimulus‐independent processing involves mainly metalizing and social cognition (Gilbert, Gonen‐Yaacovi, Benoit, Volle, & Burgess, 2010). The other regions (entorhinal, parahippocampal, cingulate, and temporopolar) with high interindividual variation in cortical thickness are periallocortical and proisocortical regions that are functionally connected to the medial frontopolar cortex (Gilbert et al., 2010; Moayedi, Salomons, Dunlop, Downar, & Davis, 2015). Notably, the periallocortex and proisocortex are considered transitional zones between the phylogenetically older allocortex and the more evolved isocortex. Specifically, the entorhinal cortex is perialiocortical (Insausti, Muñoz‐López, Insausti, & Artacho‐Pérula, 2017), the cingulate and parahippocampal cortices are proisocortical and the cortex of the temporopolar region is mixed (Blaizot et al., 2010; Petrides, Tomaiuolo, Yeterian, & Pandya, 2012). Considered together, these regions are core nodes of the default mode network (DMN; Raichle et al., 2001). At present, it is unclear whether this higher interindividual variation in the cortical thickness of the DMN nodes is associated with functional variation, but this is an important question for future studies.
The results presented here are based on the largest available brain MRI data set worldwide covering the human lifespan. However, none of the pooled samples in the current study was longitudinal. We fully appreciate that longitudinal studies are considered preferable to cross‐sectional designs when aiming to define age‐related brain morphometric trajectories. However, a longitudinal study of this size over nine decades of life is not feasible. In addition to problems with participant recruitment and retention, such a lengthy study would have involved changes in scanner types, magnetic field strengths, and acquisition protocols in line with necessary upgrades and technological advances. Nevertheless, it is possible to test the alignment between the results presented here and data from longitudinal cohorts, many of which are also available through the ENIGMA consortium. We consider this an important direction for follow‐up studies. We took several steps to mitigate against site effects. First, we ensured that we used age‐overlapping data sets throughout. Second, standardized analyses and quality control protocols were used to extract cortical thickness measures at all participating institutions. Third, we estimated and controlled for the contribution of site and scanner using ComBat prior to conducting our analysis. The validity of the findings reported here is reinforced by their alignment with the results from short‐term longitudinal studies of cortical thickness (Shaw et al., 2008; Storsve et al., 2014; Tamnes et al., 2010; Thambisetty et al., 2010; Wierenga et al., 2014). The generalizability of our findings for the older age‐group is qualified by our selection of individuals who appear to be aging successfully in terms of cognitive function and absence of significant medical morbidity. Nevertheless, despite the efforts to include only healthy older individuals, the observed pattern of brain aging may still be influenced by subclinical mental or medical conditions. For example, vascular risk factors (e.g., hypertension) are prevalent in older individuals and have been associated with decline in the age‐sensitive regions identified here (Raz et al., 2005). Thus, we cannot conclusively exclude the possibility that such factors may have contributed to our results. In addition, a wide range of factors have been associated with cortical morphology throughout the lifespan. Key among them are genetic factors (Grasby, 2020; Teeuw et al., 2019) and indices of socioeconomic status (Chan et al., 2018; Modabbernia et al., 2020; Ziegler et al., 2020) and possibly race (Zahodne et al., 2015). These factors were not modeled here as the relevant information was not collected in a systematic and harmonized fashion across contributing cohorts. It is therefore unclear to what extent they might have influenced the general pattern of age‐related associations with cortical thickness reported in the current study; qualifying their possible effects is a priority for future investigations. Cellular studies show that the number of neurons, the extent of dendritic arborization, and amount of glial support explain most of the variability in cortical thickness (la Fougère et al., 2011; Pelvig, Pakkenberg, Stark, & Pakkenberg, 2008; Terry, DeTeresa, & Hansen, 1987). MRI lacks the resolution to assess microstructural tissue properties but provides an estimate of cortical thickness based on the MR signal. Nevertheless, there is remarkable similarity between MRI‐derived thickness maps and postmortem data (Fischl & Dale, 2000). Finally, we present the centile curves to stimulate further research in developing normative reference values for neuroimaging phenotypes which should include investigation of measurement errors and reproducibility. In this context, the centile curves should not be used clinically or to make inferences about single individuals.
The findings of the current study suggest several avenues of further research. MRI‐derived measures of cortical thickness do not provide information on the mechanisms that underlie the observed age‐related associations. However, the results provided here could be used to study further factors that may lead to deviations in cortical thickness way from the expected age‐appropriate range. Additionally, the results of the current study provide a new avenue for investigating the functional correlates, either cognitive or behavioral, of age‐related changes and interindividual variation in regional cortical thickness.
In summary, using existing cross‐sectional data from 17,075 individuals we performed a large‐scale analysis to investigate the age‐related changes in cortical thickness. The size and age‐coverage of the analysis sample has the potential to inform about developmental and aging changes in cortical morphology and provide a foundation the study of factors that may lead to deviations from normative patterns.
CONFLICT OF INTERESTS
Hans Jörgen Grabe: Travel grants and speaker honoraria from Fresenius Medical Care, Neuraxpharm, Servier and Janssen Cilag; reseach funding from Fresenius Medical Care. Ole A Andreasen: Consultant to HealthLytix, speaker honorarium from Lundbeck. Anders M Dale: Founder and member of the Scientific Advisory Board CorTechs Labs, Inc where he holds equity; member of the Scientific Advisory of Human Longevity Inc; research grants with General Electric Healthcare.
Supporting information
Figure S1 Histogram of age‐distribution across all samples
Figure S2. Correlation between age and cortical thickness across age‐groups and stratified by sex
Figure S3. Meta‐analysis of pooled standard deviation stratified by sex
Figure S4. Pooled Standard deviation of cortical regions as a function of surface area
Table S1. Screening Process and Eligibility Criteria, Scanner, Image Acquisition Parameters and Image Segmentation Software
Table S2. Variance Explained by Age in fractional polynomial model
Table S3: Pearson's Correlation Coefficient between Age and Cortical Thickness
Table S4. Interindividual variations in cortical thickness
Table S5. Centile Values for Cortical Thickness
Table S6. Centile Values for Cortical Thickness in Males
Table S7. Centile Values for Cortical Thickness in Females
Appendix S1 Supporting Information.
Appendix S2 Supporting Information.
ACKNOWLEDGMENTS
This study presents independent research funded by multiple agencies. The funding sources had no role in the study design, data collection, analysis, and interpretation of the data. The views expressed in the manuscript are those of the authors and do not necessarily represent those of any of the funding agencies. Dr. Dima received funding from the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King's College London, the Psychiatry Research Trust and 2014 NARSAD Young Investigator Award. Dr. Frangou received support from the National Institutes of Health (R01 MH104284, R01 MH113619, R01 MH116147), the European Community's Seventh Framework Programme (FP7/2007‐2013) (grant agreement no 602450). This work was supported in part through the computational resources and staff expertise provided by Scientific Computing at the Icahn School of Medicine at Mount Sinai, USA. Dr. Agartz was supported by the Swedish Research Council (grant numbers: 521‐2014‐3487 and 2017‐00949). Dr. Alnæs was supported by the South Eastern Norway Regional Health Authority (grant number: 2019107). Dr. O Andreasen was supported by the Research Council of Norway (grant number: 223273) and South‐Eastern Norway Health Authority (grant number: 2017‐112). Dr. Cervenka was supported by the Swedish Research Council (grant number 523‐2014‐3467). Dr. Crespo‐Facorro was supported by the IDIVAL Neuroimaging Unit for imaging acquisition; Instituto de Salud Carlos III (grant numbers: PI020499, PI050427, PI060507, PI14/00639, and PI14/00918) and the Fundación Instituto de Investigación Marqués de Valdecilla (grant numbers: NCT0235832, NCT02534363, and API07/011). Dr. Gur was supported by the National Institute of Mental Health (grant numbers: R01MH042191 and R01MH117014). Dr. James was supported by the Medical Research Council (grant no G0500092). Dr. Saykin received support from U.S. National Institutes of Health grants R01 AG19771, P30 AG10133, and R01 CA101318. Dr. Thompson, Dr. Jahanshad, Dr. Wright, Dr. Medland, Dr. O Andreasen, Dr. Rinker, Dr. Schmaal, Dr. Veltam, Dr. van Erp, and D. P. H. were supported in part by a Consortium grant (U54EB020403 to P. M. T.) from the NIH Institutes contributing to the Big Data to Knowledge (BD2K) Initiative. FBIRN sample: Data collection and analysis was supported by the National Center for Research Resources at the National Institutes of Health (grant numbers: NIH 1U24 RR021992 (Function Biomedical Informatics Research Network) and NIH 1U24 RR025736‐01 (Biomedical Informatics Research Network Coordinating Center; http://www.birncommunity.org). FBIRN data were processed by the UCI High Performance Computing cluster supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1 TR000153. Brainscale: This work was supported by Nederlandse Organisatie voor Wetenschappelijk Onderzoek (NWO 51.02.061 to H.H., NWO 51.02.062 to D. B., NWO–NIHC Programs of excellence 433‐09‐220 to H.H., NWO‐MagW 480‐04‐004 to D. B., and NWO/SPI 56‐464‐14192 to D.B.); FP7 Ideas: European Research Council (ERC‐230374 to D. B.); and Universiteit Utrecht (High Potential Grant to H. H.). UMCU‐1.5T: This study is partially funded through the Geestkracht programme of the Dutch Health Research Council (Zon‐Mw, grant No 10‐000‐1001), and matching funds from participating pharmaceutical companies (Lundbeck, AstraZeneca, Eli Lilly, Janssen Cilag) and universities and mental health care organizations (Amsterdam: Academic Psychiatric Centre of the Academic Medical Center and the mental health institutions: GGZ Ingeest, Arkin, Dijk en Duin, GGZ Rivierduinen, Erasmus Medical Centre, GGZ Noord Holland Noord. Groningen: University Medical Center Groningen and the mental health institutions: Lentis, GGZ Friesland, GGZ Drenthe, Dimence, Mediant, GGNet Warnsveld, Yulius Dordrecht and Parnassia psycho‐medical center The Hague. Maastricht: Maastricht University Medical Centre and the mental health institutions: GGzE, GGZ Breburg, GGZ Oost‐Brabant, Vincent van Gogh voor Geestelijke Gezondheid, Mondriaan, Virenze riagg, Zuyderland GGZ, MET ggz, Universitair Centrum Sint‐Jozef Kortenberg, CAPRI University of Antwerp, PC Ziekeren Sint‐Truiden, PZ Sancta Maria Sint‐Truiden, GGZ Overpelt, OPZ Rekem. Utrecht: University Medical Center Utrecht and the mental health institutions Altrecht, GGZ Centraal and Delta.). UMCU‐3T: This study was supported by NIMH grant number: R01 MH090553 (to R. A. O.). The NIMH had no further role in study design, in the collection, analysis and interpretation of the data, in the writing of the report, and in the decision to submit the paper for publication. Netherlands Twin Register: Funding was obtained from the Netherlands Organization for Scientific Research (NWO) and The Netherlands Organization for Health Research and Development (ZonMW) grants 904‐61‐090, 985‐10‐002, 912‐10‐020, 904‐61‐193, 480‐04‐004, 463‐06‐001, 451‐04‐034, 400‐05‐717, 400‐07‐080, 31160008, 016‐115‐035, 481‐08‐011, 056‐32‐010, 911‐09‐032, 024.001.003, 480‐15‐001/674, Center for Medical Systems Biology (CSMB, NWO Genomics), Biobanking and Biomolecular Resources Research Infrastructure (BBMRI–NL, 184.021.007 and 184.033.111); Spinozapremie (NWO‐56‐464‐14192), and the Neuroscience Amsterdam research institute (former NCA). The BIG database, established in Nijmegen in 2007, is now part of Cognomics, a joint initiative by researchers of the Donders Centre for Cognitive Neuroimaging, the Human Genetics and Cognitive Neuroscience departments of the Radboud university medical centre, and the Max Planck Institute for Psycholinguistics. The Cognomics Initiative is supported by the participating departments and centres and by external grants, including grants from the Biobanking and Biomolecular Resources Research Infrastructure (Netherlands) (BBMRI‐NL) and the Hersenstichting Nederland. The authors also acknowledge grants supporting their work from the Netherlands Organization for Scientific Research (NWO), that is, the NWO Brain & Cognition Excellence Program (grant 433‐09‐229), the Vici Innovation Program (grant 016‐130‐669 to BF) and #91619115. Additional support is received from the European Community's Seventh Framework Programme (FP7/2007‐2013) under grant agreements no 602805 (Aggressotype), no 603016 (MATRICS), no 602450 (IMAGEMEND), and no 278948 (TACTICS), and from the European Community's Horizon 2020 Programme (H2020/2014‐2020) under grant agreements no 643051 (MiND) and no 667302 (CoCA). Betula sample: Data collection for the BETULA sample was supported by a grant from Knut and Alice Wallenberg Foundation (KAW); the Freesurfer segmentations were performed on resources provided by the Swedish National Infrastructure for Computing (SNIC) at HPC2N in Umeå, Sweden. Indiana sample: This sample was supported in part by grants to BCM from Siemens Medical Solutions, from the members of the Partnership for Pediatric Epilepsy Research, which includes the American Epilepsy Society, the Epilepsy Foundation, the Epilepsy Therapy Project, Fight Against Childhood Epilepsy and Seizures (F.A.C.E.S.), and Parents Against Childhood Epilepsy (P.A.C.E.), from the Indiana State Department of Health Spinal Cord and Brain Injury Fund Research Grant Program, and by a Project Development Team within the ICTSI NIH/NCRR Grant Number RR025761. MHRC study: It was supported in part by RFBR grant 20‐013‐00748. PING study: Data collection and sharing for the Pediatric Imaging, Neurocognition and Genetics (PING) Study (National Institutes of Health Grant RC2DA029475) were funded by the National Institute on Drug Abuse and the Eunice Kennedy Shriver National Institute of Child Health & Human Development. A full list of PING investigators is at http://pingstudy.ucsd.edu/investigators.html. QTIM sample: The authors are grateful to the twins for their generosity of time and willingness to participate in our study and thank the many research assistants, radiographers, and other staff at QIMR Berghofer Medical Research Institute and the Centre for Advanced Imaging, University of Queensland. QTIM was funded by the Australian National Health and Medical Research Council (Project Grants No. 496682 and 1009064) and US National Institute of Child Health and Human Development (RO1HD050735). Lachlan Strike was supported by a University of Queensland PhD scholarship. Study of Health in Pomerania (SHIP): this is part of the Community Medicine Research net (CMR) (http://www.medizin.uni-greifswald.de/icm) of the University Medicine Greifswald, which is supported by the German Federal State of Mecklenburg‐ West Pomerania. MRI scans in SHIP and SHIP‐TREND have been supported by a joint grant from Siemens Healthineers, Erlangen, Germany and the Federal State of Mecklenburg‐West Pomerania. This study was further supported by the DZHK (German Centre for Cardiovascular Research), the German Centre of Neurodegenerative Diseases (DZNE) and the EU‐JPND Funding for BRIDGET (FKZ:01ED1615). TOP study: this was supported by the European Community's Seventh Framework Programme (FP7/2007‐2013), grant agreement no 602450. The Southern and Eastern Norway Regional Health Authority supported Lars T. Westlye (grant no. 2014‐097) and STROKEMRI (grant no. 2013‐054). HUBIN sample: HUBIN was supported by the Swedish Research Council (K2007‐62X‐15077‐04‐1, K2008‐62P‐20597‐01‐3, K2010‐62X‐15078‐07‐2, K2012‐61X‐15078‐09‐3), the regional agreement on medical training and clinical research between Stockholm County Council, and the Karolinska Institutet, and the Knut and Alice Wallenberg Foundation. The BIG database: this was established in Nijmegen in 2007, is now part of Cognomics, a joint initiative by researchers of the Donders Centre for Cognitive Neuroimaging, the Human Genetics and Cognitive Neuroscience departments of the Radboud university medical centre, and the Max Planck Institute for Psycholinguistics. The Cognomics Initiative is supported by the participating departments and centers and by external grants, including grants from the Biobanking and Biomolecular Resources Research Infrastructure (Netherlands) (BBMRI‐NL) and the Hersenstichting Nederland. The authors also acknowledge grants supporting their work from the Netherlands Organization for Scientific Research (NWO), that is, the NWO Brain & Cognition Excellence Program (grant 433‐09‐229), the Vici Innovation Program (grant 016‐130‐669 to BF) and #91619115. Additional support is received from the European Community's Seventh Framework Programme (FP7/2007‐2013) under grant agreements no 602805 (Aggressotype), no 603016 (MATRICS), no 602450 (IMAGEMEND), and no 278948 (TACTICS), and from the European Community's Horizon 2020 Programme (H2020/2014‐2020) under grant agreements no 643051 (MiND) and no 667302 (CoCA).
APPENDIX A.
Göran Engberg, Department of Physiology and Pharmacology, Karolinska Institute, Sweden.
Sophie Erhardt, Department of Physiology and Pharmacology, Karolinska Institute, Sweden.
Lilly Schwieler, Department of Physiology and Pharmacology, Karolinska Institute, Sweden.
Funda Orhan, Department of Physiology and Pharmacology, Karolinska Institute, Sweden.
Anna Malmqvist, Department of Physiology and Pharmacology, Karolinska Institute, Sweden. Mikael Hedberg, Department of Physiology and Pharmacology, Karolinska Institute, Sweden.
Lars Farde, Department of Clinical Neuroscience, Center for Psychiatry Research, Karolinska Institutet, Sweden.
Simon Cervenka, Department of Clinical Neuroscience, Center for Psychiatry Research, Karolinska Institutet, Sweden.
Lena Flyckt, Department of Clinical Neuroscience, Center for Psychiatry Research, Karolinska Institutet, Sweden.
Karin Collste, Department of Clinical Neuroscience, Center for Psychiatry Research, Karolinska Institutet, Sweden.
Pauliina Ikonen, Department of Clinical Neuroscience, Center for Psychiatry Research, Karolinska Institutet, Sweden.
Fredrik Piehl, Neuroimmunology Unit, Department of Clinical Neuroscience, Karolinska Institutet, Sweden.
Ingrid Agartz, NORMENT, Division of Mental Health and Addiction, KG Jebsen Centre for Psychosis Research, University of Oslo and Department of Psychiatric Research, Diakonhjemmet Hospital, Norway; Center for Psychiatric Research, Department of Clinical Neuroscience, Karolinska Institutet, Sweden.
Frangou S, Modabbernia A, Williams SCR, et al. Cortical thickness across the lifespan: Data from 17,075 healthy individuals aged 3–90 years. Hum Brain Mapp. 2022;43:431–451. 10.1002/hbm.25364
Members of Karolinska Schizophrenia Project (KaSP) are given in Appendix.
Funding information European Community's Seventh Framework Programme, Grant/Award Numbers: 278948, 602450, 603016, 602805; US National Institute of Child Health and Human Development, Grant/Award Numbers: RO1HD050735, 1009064, 496682; QIMR Berghofer Medical Research Institute and the Centre for Advanced Imaging, University of Queensland; ICTSI NIH/NCRR, Grant/Award Number: RR025761; European Community's Horizon 2020 Programme, Grant/Award Numbers: 667302, 643051; Vici Innovation Program, Grant/Award Numbers: #91619115, 016‐130‐669; NWO Brain & Cognition Excellence Program, Grant/Award Number: 433‐09‐229; Biobanking and Biomolecular Resources Research Infrastructure (Netherlands) (BBMRI‐NL); Spinozapremie, Grant/Award Number: NWO‐56‐464‐14192; Biobanking and Biomolecular Resources Research Infrastructure, Grant/Award Numbers: 184.033.111, 184.021.007; Netherlands Organization for Health Research and Development (ZonMW), Grant/Award Numbers: 480‐15‐001/674, 024.001.003, 911‐09‐032, 056‐32‐010, 481‐08‐011, 016‐115‐035, 31160008, 400‐07‐080, 400‐05‐717, 451‐04‐034, 463‐06‐001, 480‐04‐004, 904‐61‐193, 912‐10‐020, 985‐10‐002, 904‐61‐090; NIMH, Grant/Award Number: R01 MH090553; Geestkracht programme of the Dutch Health Research Council, Grant/Award Number: 10‐000‐1001; FP7 Ideas: European Research Council; Nederlandse Organisatie voor Wetenschappelijk Onderzoek, Grant/Award Numbers: NWO/SPI 56‐464‐14192, NWO‐MagW 480‐04‐004, 433‐09‐220, NWO 51.02.062, NWO 51.02.061; National Center for Advancing Translational Sciences, National Institutes of Health, Grant/Award Number: UL1 TR000153; National Center for Research Resources; National Center for Research Resources at the National Institutes of Health, Grant/Award Numbers: NIH 1U24 RR025736‐01, NIH 1U24 RR021992; NIH Institutes contributing to the Big Data to Knowledge; U.S. National Institutes of Health, Grant/Award Numbers: R01 CA101318, P30 AG10133, R01 AG19771; Medical Research Council, Grant/Award Numbers: U54EB020403, G0500092; National Institute of Mental Health, Grant/Award Numbers: R01MH117014, R01MH042191; Fundación Instituto de Investigación Marqués de Valdecilla, Grant/Award Numbers: API07/011, NCT02534363, NCT0235832; Instituto de Salud Carlos III, Grant/Award Numbers: PI14/00918, PI14/00639, PI060507, PI050427, PI020499; Swedish Research Council, Grant/Award Numbers: 523‐2014‐3467, 2017‐00949, 521‐2014‐3487; South‐Eastern Norway Health Authority; the Research Council of Norway, Grant/Award Number: 223273; South Eastern Norway Regional Health Authority, Grant/Award Numbers: 2017‐112, 2019107; Icahn School of Medicine at Mount Sinai; Seventh Framework Programme (FP7/2007‐2013), Grant/Award Number: 602450; National Institutes of Health, Grant/Award Numbers: R01 MH116147, R01 MH113619, R01 MH104284; South London and Maudsley NHS Foundation Trust; the National Institute for Health Research (NIHR)
DATA AVAILABILITY STATEMENT
The ENIGMA Lifespan Working Group welcomes expression of interest from researchers in the field who wish to use the ENIGMA samples. Data sharing is possible subsequent to consent for the principal investigators of the contributing datasets. Requests should be directed to the corresponding authors.
REFERENCES
- Abe, O. , Yamasue, H. , Aoki, S. , Suga, M. , Yamada, H. , Kasai, K. , … Ohtomo, K. (2008). Aging in the CNS: Comparison of gray/white matter volume and diffusion tensor data. Neurobiology of Aging, 29(1), 102–116. 10.1016/j.neurobiolaging.2006.09.003 [DOI] [PubMed] [Google Scholar]
- Alegret, M. , Vinyes‐Junqué, G. , Boada, M. , Martínez‐Lage, P. , Cuberas, G. , Espinosa, A. , … Tárraga, L. (2010). Brain perfusion correlates of visuoperceptual deficits in mild cognitive impairment and mild Alzheimer's disease. Journal of Alzheimer's Disease, 21(2), 557–567. 10.3233/JAD-2010-091069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen, J. S. , Bruss, J. , Brown, C. K. , & Damasio, H. (2005). Normal neuroanatomical variation due to age: The major lobes and a parcellation of the temporal region. Neurobiology of Aging, 26(9), 1245–1260. 10.1016/j.neurobiolaging.2005.05.023 [DOI] [PubMed] [Google Scholar]
- Aune, D. , Sen, A. , Prasad, M. , Norat, T. , Janszky, I. , Tonstad, S. , … Vatten, L. J. (2016). BMI and all‐cause mortality: Systematic review and non‐linear dose‐response meta‐analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ, 353, i2156. 10.1136/bmj.i2156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaizot, X. , Mansilla, F. , Insausti, A. M. , Constans, J. M. , Salinas‐Alaman, A. , Pro‐Sistiaga, P. , … Insausti, R. (2010). The human parahippocampal region: I. temporal pole cytoarchitectonic and MRI correlation. Cerebral Cortex, 20(9), 2198–2212. 10.1093/cercor/bhp289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boedhoe, P. S. W. , Schmaal, L. , Abe, Y. , Alonso, P. , Ameis, S. H. , Anticevic, A. , … van den Heuvel, O. A. (2018). Cortical abnormalities associated with pediatric and adult obsessive‐compulsive disorder: Findings from the ENIGMA obsessive‐compulsive disorder working group. The American Journal of Psychiatry, 175(5), 453–462. 10.1176/appi.ajp.2017.17050485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brickman, A. M. , Habeck, C. , Zarahn, E. , Flynn, J. , & Stern, Y. (2007). Structural MRI covariance patterns associated with normal aging and neuropsychological functioning. Neurobiology of Aging, 28(2), 284–295. 10.1016/j.neurobiolaging.2005.12.016 [DOI] [PubMed] [Google Scholar]
- Burgess, P. W. , Dumontheil, I. , & Gilbert, S. J. (2007). The gateway hypothesis of rostral prefrontal cortex (area 10) function. Trends in Cognitive Sciences, 11(7), 290–298. 10.1016/j.tics.2007.05.004 [DOI] [PubMed] [Google Scholar]
- Chan, M. Y. , Na, J. , Agres, P. F. , Savalia, N. K. , Park, D. C. , & Wig, G. S. (2018). Socioeconomic status moderates age‐related differences in the brain's functional network organization and anatomy across the adult lifespan. Proceedings of the National Academy of Sciences of the United States of America, 115(22), E5144–E5153. 10.1073/pnas.1714021115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole, T. J. , & Green, P. J. (1992). Smoothing reference centile curves: the LMS method and penalized likelihood. Statistics in Medicine, 11(10), 1305–1319. 10.1002/sim.4780111005. [DOI] [PubMed] [Google Scholar]
- Dickerson, B. C. , Feczko, E. , Augustinack, J. C. , Pacheco, J. , Morris, J. C. , Fischl, B. , & Buckner, R. L. (2009). Differential effects of aging and Alzheimer's disease on medial temporal lobe cortical thickness and surface area. Neurobiology of Aging, 30(3), 432–440. 10.1016/j.neurobiolaging.2007.07.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ducharme, S. , Albaugh, M. D. , Nguyen, T. V. , Hudziak, J. J. , Mateos‐Pérez, J. M. , Labbe, A. , … Brain Development Cooperative Group . (2016). Trajectories of cortical thickness maturation in normal brain development‐the importance of quality control procedures. NeuroImage, 125, 267–279. 10.1016/j.neuroimage.2015.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eberling, J. L. , Nordahl, T. E. , Kusubov, N. , Reed, B. R. , Budinger, T. F. , & Jagust, W. J. (1995). Reduced temporal lobe glucose metabolism in aging. Journal of Neuroimaging, 5(3), 178–182. 10.1111/jon199553178 [DOI] [PubMed] [Google Scholar]
- Fischl, B. , & Dale, A. M. (2000). Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proceedings of the National Academy of Sciences of the United States of America, 97(20), 11050–11055. 10.1073/pnas.200033797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fjell, A. M. , Grydeland, H. , Krogsrud, S. K. , Amlien, I. , Rohani, D. A. , Ferschmann, L. , … Walhovd, K. B. (2015). Development and aging of cortical thickness correspond to genetic organization patterns. Proceedings of the National Academy of Sciences of the United States of America, 112(50), 15462–15467. 10.1073/pnas.1508831112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fjell, A. M. , Westlye, L. T. , Amlien, I. , Espeseth, T. , Reinvang, I. , Raz, N. , … Walhovd, K. B. (2009). High consistency of regional cortical thinning in aging across multiple samples. Cerebral Cortex, 19(9), 2001–2012. 10.1093/cercor/bhn232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortin, J. P. , Cullen, N. , Sheline, Y. I. , Taylor, W. D. , Aselcioglu, I. , Cook, P. A. , … Shinohara, R. T. (2018). Harmonization of cortical thickness measurements across scanners and sites. NeuroImage, 167, 104–120. 10.1016/j.neuroimage.2017.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert, S. J. , Gonen‐Yaacovi, G. , Benoit, R. G. , Volle, E. , & Burgess, P. W. (2010). Distinct functional connectivity associated with lateral versus medial rostral prefrontal cortex: A meta‐analysis. NeuroImage, 53(4), 1359–1367. 10.1016/j.neuroimage.2010.07.032 [DOI] [PubMed] [Google Scholar]
- Goh, S. , Bansal, R. , Xu, D. , Hao, X. , Liu, J. , & Peterson, B. S. (2011). Neuroanatomical correlates of intellectual ability across the life span. Developmental Cognitive Neuroscience, 1(3), 305–312. 10.1016/j.dcn.2011.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Good, C. D. , Johnsrude, I. S. , Ashburner, J. , Henson, R. N. A. , Friston, K. J. , & Frackowiak, R. S. J. (2001). A voxel‐based morphometric study of ageing in 465 normal adult human brains. NeuroImage, 14(1 Pt 1), 21–36. 10.1006/nimg.2001.0786 [DOI] [PubMed] [Google Scholar]
- Grasby, K. L. (2020). Enhancing NeuroImaging genetics through meta‐analysis consortium (ENIGMA)‐genetics working group. The genetic architecture of the human cerebral cortex. Science, 367(6484), eaay6690. 10.1126/science.aay6690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan, K. M. , Mwangi, B. , Cao, B. , Keser, Z. , Tustison, N. J. , Kochunov, P. , … Soares, J. (2016). Entorhinal cortex thickness across the human lifespan. Journal of Neuroimaging, 26(3), 278–282. 10.1111/jon.12297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedman, A. M. , van Haren, N. E. , Schnack, H. G. , Kahn, R. S. , & Hulshoff Pol, H. E. (2012). Human brain changes across the life span: A review of 56 longitudinal magnetic resonance imaging studies. Human Brain Mapping, 33(8), 1987–2002. 10.1002/hbm.21334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibar, D. P. , Westlye, L. T. , Doan, N. T. , Jahanshad, N. , Cheung, J. W. , Ching, C. R. K. , … Andreassen, O. A. (2018). Cortical abnormalities in bipolar disorder: An MRI analysis of 6503 individuals from the ENIGMA bipolar disorder working group. Molecular Psychiatry, 23(4), 932–942. 10.1038/mp.2017.73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodges, J. R. , & Patterson, K. (2007). Semantic dementia: a unique clinicopathological syndrome. Lancet Neurology, 6(11), 1004–1014. 10.1016/S1474-4422(07)70266-1 [DOI] [PubMed] [Google Scholar]
- Hoogman, M. , Muetzel, R. , Guimaraes, J. P. , Shumskaya, E. , Mennes, M. , Zwiers, M. P. , … Franke, B. (2019). Brain imaging of the cortex in ADHD: A coordinated analysis of large‐scale clinical and population‐based samples. The American Journal of Psychiatry, 176(7), 531–542. 10.1176/appi.ajp.2019.18091033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insausti, R. , Muñoz‐López, M. , Insausti, A. M. , & Artacho‐Pérula, E. (2017). The human Periallocortex: Layer pattern in Presubiculum, Parasubiculum and Entorhinal cortex. A review. Frontiers in Neuroanatomy, 11, 84. 10.3389/fnana.2017.00084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw, P. , Kabani, N. J. , Lerch, J. P. , Eckstrand, K. , Lenroot, R. , Gogtay, N. , … Wise, S. P. (2008). Neurodevelopmental trajectories of the human cerebral cortex. The Journal of Neuroscience, 28(14), 3586–3594. 10.1523/JNEUROSCI.5309-07.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- la Fougère, C. , Grant, S. , Kostikov, A. , Schirrmacher, R. , Gravel, P. , Schipper, H. M. , … Thiel, A. (2011). Where in‐vivo imaging meets cytoarchitectonics: The relationship between cortical thickness and neuronal density measured with high‐resolution [18F]flumazenil‐PET. NeuroImage, 56(3), 951–960. 10.1016/j.neuroimage.2010.11.015 [DOI] [PubMed] [Google Scholar]
- Mauvais‐Jarvis, F. , Bairey Merz, N. , Barnes, P. J. , Brinton, R. D. , Carrero, J. J. , DeMeo, D. L. , … Suzuki, A. (2020). Sex and gender: Modifiers of health, disease, and medicine. Lancet, 396(10250), 565–582. 10.1016/S0140-6736(20)31561-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills, K. L. , Goddings, A. L. , Herting, M. M. , Meuwese, R. , Blakemore, S. J. , Crone, E. A. , … Tamnes, C. K. (2016). Structural brain development between childhood and adulthood: Convergence across four longitudinal samples. NeuroImage, 141, 273–281. 10.1016/j.neuroimage.2016.07.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moayedi, M. , Salomons, T. V. , Dunlop, K. A. , Downar, J. , & Davis, K. D. (2015). Connectivity‐based parcellation of the human frontal polar cortex. Brain Structure & Function, 220(5), 2603–2616. 10.1007/s00429-014-0809-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modabbernia, A. , Reichenberg, A. , Ing, A. , Moser, D. A. , Doucet, G. E. , Artiges, E. , … Frangou, S. (2020). Linked patterns of biological and environmental covariation with brain structure in adolescence: A population‐based longitudinal study. Molecular Psychiatry. 10.1038/s41380-020-0757-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutlu, A. K. , Schneider, M. , Debbané, M. , Badoud, D. , Eliez, S. , & Schaer, M. (2013). Sex differences in thickness, and folding developments throughout the cortex. NeuroImage, 82, 200–207. 10.1016/j.neuroimage.2013.05.076 [DOI] [PubMed] [Google Scholar]
- Ongür, D. , Ferry, A. T. , & Price, J. L. (2003). Architectonic subdivision of the human orbital and medial prefrontal cortex. The Journal of Comparative Neurology, 460(3), 425–449. 10.1002/cne.10609 [DOI] [PubMed] [Google Scholar]
- Paus, T. (2010). Sex differences in the human brain: A developmental perspective. Progress in Brain Research, 186, 13–28. 10.1016/B978-0-444-53630-3.00002-6 [DOI] [PubMed] [Google Scholar]
- Pelvig, D. P. , Pakkenberg, H. , Stark, A. K. , & Pakkenberg, B. (2008). Neocortical glial cell numbers in human brains. Neurobiology of Aging, 29(11), 1754–1762. 10.1016/j.neurobiolaging.2007.04.013 [DOI] [PubMed] [Google Scholar]
- Petrides, M. , Tomaiuolo, F. , Yeterian, E. H. , & Pandya, D. N. (2012). The prefrontal cortex: Comparative architectonic organization in the human and the macaque monkey brains. Cortex, 48(1), 46–57. 10.1016/j.cortex.2011.07.002 [DOI] [PubMed] [Google Scholar]
- Raichle, M. E. , MacLeod, A. M. , Snyder, A. Z. , Powers, W. J. , Gusnard, D. A. , & Shulman, G. L. (2001). A default mode of brain function. Proceedings of the National Academy of Sciences of the United States of America, 98(2), 676–682. 10.1073/pnas.98.2.676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raz, N. , Ghisletta, P. , Rodrigue, K. M. , Kennedy, K. M. , & Lindenberger, U. (2010). Trajectories of brain aging in middle‐aged and older adults: Regional and individual differences. NeuroImage, 51(2), 501–511. 10.1016/j.neuroimage.2010.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raz, N. , Lindenberger, U. , Rodrigue, K. M. , Kennedy, K. M. , Head, D. , Williamson, A. , … Acker, J. D. (2005). Regional brain changes in aging healthy adults: General trends, individual differences and modifiers. Cerebral Cortex, 15(11), 1676–1689. 10.1093/cercor/bhi044 [DOI] [PubMed] [Google Scholar]
- Reitz, C. , & Mayeux, R. (2014). Alzheimer disease: Epidemiology, diagnostic criteria, risk factors and biomarkers. Biochemical Pharmacology, 88(4), 640–651. 10.1016/j.bcp.2013.12.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigby, R. A. , & Stasinopoulos, D. M. (2005). Generalized additive models for location, scale and shape. Applied Statistics, 54(3), 507–554. [Google Scholar]
- Rolls, E. T. (2018). The storage and recall of memories in the hippocampo‐cortical system. Cell and Tissue Research, 373(3), 577–604. 10.1007/s00441-017-2744-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royston, P. , & Altman, D. (1994). Regression using fractional polynomials of continuous covariates: Parsimonious parametric modelling. Applied Statistics, 43, 429–467. 10.2307/2986270 [DOI] [Google Scholar]
- Salat, D. H. , Buckner, R. L. , Snyder, A. Z. , Greve, D. N. , Desikan, R. S. , Busa, E. , … Fischl, B. (2004). Thinning of the cerebral cortex in aging. Cerebral Cortex, 14(7), 721–730. 10.1093/cercor/bhh032 [DOI] [PubMed] [Google Scholar]
- Sauerbrei, W. , Meier‐Hirmer, C. , Benner, A. , & Royston, P. (2006). Multivariable regression model building by using fractional polynomials: Description of SAS, STATA and R programs. Computational Statistics and Data Analysis, 50(12), 3464–3485. 10.1016/j.csda.2005.07.015 [DOI] [Google Scholar]
- Schmaal, L. , Hibar, D. P. , Sämann, P. G. , Hall, G. B. , Baune, B. T. , Jahanshad, N. , … Veltman, D. J. (2017). Cortical abnormalities in adults and adolescents with major depression based on brain scans from 20 cohorts worldwide in the ENIGMA major depressive disorder working group. Molecular Psychiatry, 22(6), 900–909. 10.1038/mp.2016.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitt, J. E. , Raznahan, A. , Clasen, L. S. , Wallace, G. L. , Pritikin, J. N. , Lee, N. R. , … Neale, M. C. (2019). The dynamic associations between cortical thickness and general intelligence are genetically mediated. Cerebral Cortex, 29(11), 4743–4752. 10.1093/cercor/bhz007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schultz, H. , Sommer, T. , & Peters, J. (2012). Direct evidence for domain‐sensitive functional subregions in human entorhinal cortex. The Journal of Neuroscience, 32(14), 4716–4723. 10.1523/JNEUROSCI.5126-11.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semendeferi, K. , Teffer, K. , Buxhoeveden, D. P. , Park, M. S. , Bludau, S. , Amunts, K. , … Buckwalter, J. (2011). Spatial organization of neurons in the frontal pole sets humans apart from great apes. Cerebral Cortex, 21(7), 1485–1497. 10.1093/cercor/bhq191 [DOI] [PubMed] [Google Scholar]
- Senior, A. M. , Grueber, C. E. , Kamiya, T. , Lagisz, M. , O'Dwyer, K. , Santos, E.S. , & Nakagawa, S. (2016). Heterogeneity in ecological and evolutionary meta‐analyses: its magnitude and implications. Ecology, 97(12), 3293–3299. 10.1002/ecy.1591. [DOI] [PubMed] [Google Scholar]
- Shaw, P. , Greenstein, D. , Lerch, J. , Clasen, L. , Lenroot, R. , Gogtay, N. , … Giedd, J. (2006). Intellectual ability and cortical development in children and adolescents. Nature, 440(7084), 676–679. 10.1038/nature04513 [DOI] [PubMed] [Google Scholar]
- Stasinopoulos, D. M. , & Rigby, R. A. (2007). Generalized additive models for location scale and shape (GAMLSS) in R. Journal of Statistical Software, 23(7), 1–46. 10.18637/jss.v023.i07 [DOI] [Google Scholar]
- Storsve, A. B. , Fjell, A. M. , Tamnes, C. K. , Westlye, L. T. , Overbye, K. , Aasland, H. W. , & Walhovd, K. B. (2014). Differential longitudinal changes in cortical thickness, surface area and volume across the adult life span: Regions of accelerating and decelerating change. The Journal of Neuroscience, 34(25), 8488–8498. 10.1523/JNEUROSCI.0391-14.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamnes, C. K. , Østby, Y. , Fjell, A. M. , Westlye, L. T. , Due‐Tønnessen, P. , & Walhovd, K. B. (2010). Brain maturation in adolescence and young adulthood: Regional age‐related changes in cortical thickness and white matter volume and microstructure. Cerebral Cortex, 20(3), 534–548. 10.1093/cercor/bhp118 [DOI] [PubMed] [Google Scholar]
- Teeuw, J. , Brouwer, R. M. , Koenis, M. M. G. , Swagerman, S. C. , Boomsma, D. I. , & Hulshoff Pol, H. E. (2019). Genetic influences on the development of cerebral cortical thickness during childhood and adolescence in a Dutch longitudinal twin sample: The Brainscale study. Cerebral Cortex, 29(3), 978–993. 10.1093/cercor/bhy005 [DOI] [PubMed] [Google Scholar]
- Terry, R. D. , DeTeresa, R. , & Hansen, L. A. (1987). Neocortical cell counts in normal human adult aging. Annals of Neurology, 21(6), 530–539. 10.1002/ana.410210603 [DOI] [PubMed] [Google Scholar]
- Thambisetty, M. , Wan, J. , Carass, A. , An, Y. , Prince, J. L. , & Resnick, S. M. (2010). Longitudinal changes in cortical thickness associated with normal aging. NeuroImage, 52(4), 1215–1223. 10.1016/j.neuroimage.2010.04.258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson, P. M. , Andreassen, O. A. , Arias‐Vasquez, A. , Bearden, C. E. , Boedhoe, P. S. , Brouwer, R. M. , … Ye, J. (2017). ENIGMA and the individual: Predicting factors that affect the brain in 35 countries worldwide. NeuroImage, 145(Pt B), 389–408. 10.1016/j.neuroimage.2015.11.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson, P. M. , Hayashi, K. M. , Dutton, R. A. , Chiang, M. C. , Leow, A. D. , Sowell, E. R. , … Toga, A. W. (2007). Tracking Alzheimer's disease. Annals of the New York Academy of Sciences, 1097, 183–214. 10.1196/annals.1379.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson, P. M. , Jahanshad, N. , Ching, C. R. K. , Salminen, L. E. , Thomopoulos, S. I. , Bright, J. , … Zelman, V. (2020). The ENIGMA consortium: Large‐scale collaborative analyses of neuroimaging and genetic data. Translational Psychiatry, 10(1), 100. 10.1038/s41398-020-0705-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaidya, J. G. , Paradiso, S. , Boles Ponto, L. L. , McCormick, L. M. , & Robinson, R. G. (2007). Aging, grey matter, and blood flow in the anterior cingulate cortex. NeuroImage, 37(4), 1346–1353. 10.1016/j.neuroimage.2007.06.015 [DOI] [PubMed] [Google Scholar]
- van Erp, T. G. , Walton, E. , Hibar, D. P. , Schmaal, L. , Jiang, W. , Glahn, D. C. , … Orhan, F. (2018). Cortical brain abnormalities in 4474 individuals with schizophrenia and 5098 control subjects via the enhancing Neuro imaging genetics through meta analysis (ENIGMA) consortium. Biological Psychiatry, 84(9), 644–654. 10.1016/j.biopsych.2018.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Rooij, D. , Anagnostou, E. , Arango, C. , Auzias, G. , Behrmann, M. , Busatto, G. F. , … Buitelaar, J. K. (2018). Cortical and subcortical brain Morphometry differences between patients with autism Spectrum disorder and healthy individuals across the lifespan: Results from the ENIGMA ASD working group. The American Journal of Psychiatry, 175(4), 359–369. 10.1176/appi.ajp.2017.17010100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walhovd, K. B. , Fjell, A. M. , Giedd, J. , Dale, A. M. , & Brown, T. T. (2017). Through thick and thin: A need to reconcile contradictory results on trajectories in human cortical development. Cerebral Cortex, 27(2), 1472–1481. 10.1093/cercor/bhv301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whelan, C. D. , Altmann, A. , Botía, J. A. , Jahanshad, N. , Hibar, D. P. , Absil, J. , … Sisodiya, S. M. (2018). Structural brain abnormalities in the common epilepsies assessed in a worldwide ENIGMA study. Brain, 141(2), 391–408. 10.1093/brain/awx341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wierenga, L. M. , Doucet, G. E. , Dima, D. , Agartz, I. , Aghajani, M. , Akudjedu, T. N. , … Tamnes, C. K. (2020). Greater male than female variability in regional brain structure across the lifespan. Human Brain Mapping. 10.1002/hbm.25204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wierenga, L. M. , Langen, M. , Oranje, B. , & Durston, S. (2014). Unique developmental trajectories of cortical thickness and surface area. NeuroImage, 87, 120–126. 10.1016/j.neuroimage.2013.11.010 [DOI] [PubMed] [Google Scholar]
- Zahodne, L. B. , Manly, J. J. , Narkhede, A. , Griffith, E. , DeCarli, C. , Schupf, N. , … Brickman, A. (2015). Structural MRI predictors of late‐life cognition differ across African Americans, Hispanics, and Whites. Current Alzheimer Research, 12(7), 632–639. 10.2174/1567205012666150530203214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, M. , Zhang, F. , Zhao, L. , Qian, J. , & Dong, C. (2016). Entorhinal cortex: A good biomarker of mild cognitive impairment and mild Alzheimer's disease. Reviews in the Neurosciences, 27(2), 185–195. 10.1515/revneuro-2015-0019 [DOI] [PubMed] [Google Scholar]
- Ziegler, G. , Moutoussis, M. , Hauser, T. U. , Fearon, P. , Bullmore, E. T. , Goodyer, I. M. , … Dolan, R. J. (2020). Childhood socio‐economic disadvantage predicts reduced myelin growth across adolescence and young adulthood. Human Brain Mapping, 41(12), 3392–3402. 10.1002/hbm.25024 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Histogram of age‐distribution across all samples
Figure S2. Correlation between age and cortical thickness across age‐groups and stratified by sex
Figure S3. Meta‐analysis of pooled standard deviation stratified by sex
Figure S4. Pooled Standard deviation of cortical regions as a function of surface area
Table S1. Screening Process and Eligibility Criteria, Scanner, Image Acquisition Parameters and Image Segmentation Software
Table S2. Variance Explained by Age in fractional polynomial model
Table S3: Pearson's Correlation Coefficient between Age and Cortical Thickness
Table S4. Interindividual variations in cortical thickness
Table S5. Centile Values for Cortical Thickness
Table S6. Centile Values for Cortical Thickness in Males
Table S7. Centile Values for Cortical Thickness in Females
Appendix S1 Supporting Information.
Appendix S2 Supporting Information.
Data Availability Statement
The ENIGMA Lifespan Working Group welcomes expression of interest from researchers in the field who wish to use the ENIGMA samples. Data sharing is possible subsequent to consent for the principal investigators of the contributing datasets. Requests should be directed to the corresponding authors.


