Abstract
Health 4.0 establishes a new promising vision for the healthcare industry. It creatively integrates and employ innovative technologies such as the Internet of Health Things (IoHT), medical Cyber-Physical Systems (medical CPS), health cloud, health fog, big data analytics, machine learning, blockchain, and smart algorithms. The goal is to deliver improved, value-added and cost-effective healthcare services to patients and enhance the effectiveness and efficiency or the healthcare industry. Health 4.0 (adapted from the Industry 4.0 principles) changes the healthcare business model to enhance the interactions across the healthcare clients (the patients), stakeholders, infrastructure, and value chain. This effectively will improve the quality, flexibility, productivity, cost-effectiveness, and reliability of healthcare services in addition to increasing patients’ satisfaction. However, building and utilizing healthcare applications that follow the Health 4.0 concept is a non-trivial and complex endeavor. In addition, advanced potential applications based on Health 4.0 capabilities are not yet being investigated. In this paper we define the main objectives of Health 4.0 and discuss advanced potential Health 4.0 applications. To have a clear understanding of these applications, we categorize them in 4 groups based on the primary beneficiary of these applications. Thus we have patient targeted applications, applications supporting healthcare professionals, resource management applications and high-level healthcare systems management applications. In addition, as we studied the different applications, we realized that these is a certain collection of services that these most of them need regardless of their goals or business context. Services supporting data collection and transfer, security and privacy, reliable operations are some examples. As a result we propose creating a service-oriented middleware framework to offers the common services to the applications developers and facilitate the integration of different services to build applications under the Health 4.0 umbrella.
Keywords: Health 40, Industry 40, healthcare systems, service-oriented middleware, service integration, health cloud, health fog, Internet of Health Things, medical cyber-physical systems, COVID-19
I. Introduction
The healthcare industry is facing several challenges including increasingly high costs of healthcare services, professionals, and equipment; shortages in skilled healthcare professionals [1]; rising demand for high-quality healthcare services [2], [3]; size and complexity of the healthcare value chain; the need for collaboration among healthcare providers and supporting industries and organizations [4]; and intense competition among healthcare providers [5]. These challenges are pushing healthcare providers towards considering the inclusion and use of new healthcare models based on innovative and cutting-edge information and communication technology (ICT) utilization. One sector already working on taking advantage of ICT advances is the industry sector using technologies like the internet of things (IoT), cyber-physical systems (CPS), and analytics to initiate the Industry 4.0 era [6]. The 4.0 is based on the historical progression of the industrial revolutions. Industry 1.0 (manual machining), Industry 2.0 (powered machining), Industry 3.0 (computerized machining) followed by the current start of Industry 4.0 taking us to the era of autonomous and smart industrial operations. Industry 4.0 aims to enhance operations, reduce costs and improve quality through optimization, industrial automation, and the use of intelligent services.
Another important sector to benefit from inheriting the Industry 4.0 principals is healthcare. Adapting Industry 4.0 principles for the healthcare industry created what is now known as Healthcare Industry 4.0, Healthcare 4.0, or Health 4.0 [7]–[11], in this paper we will use Health 4.0 to reference it. The 4.0 in Health 4.0 was inherited from its origin, Industry 4.0, and does not signify the existence of Health 3.0, 2.0 and 1.0 as the healthcare systems progressed differently from industrial systems. Health 4.0 can be defined as the implementation of integrated healthcare platforms with progressive virtualized, distributed and real-time healthcare services for patients, professionals and formal and informal care givers. It focuses on supporting, enabling and optimizing collaboration, coherence, and convergence to move healthcare services from being based on “empirical data” to “precision medicine” (i.e. personalized healthcare services) as one direction for enhancement. This aligns with the global shift from a hospital-based professional-oriented model to a distributed, patient-centered model [12]. Another direction involves enabling integration, sharing, and optimizing use of healthcare services resources, professionals and systems management for enhanced operations and reduced costs. Health 4.0 can be further extended to enhance all aspects in the healthcare system and its entire value chain. Worldwide spending on healthcare is anticipated to reach $18.28 trillion in 2040 [13], hence the need to utilize technologies and concepts presented by Industry 4.0 [14] to enhance effectiveness and efficiency in all directions.
The benefits of adopting Health 4.0 in the healthcare industry are numerous. These include improving the flexibility, scalability, reliability, agility, cost-effectiveness and quality of healthcare services and operations [8]. These features will enhance the healthcare system in many ways like integrating all these features to help improve national and global responses to pandemics like COVID-19 [15]. However, building and delivering healthcare applications that follow the concepts of Health 4.0 is very complex. Issues involved, like increased design complexity, verity of architectural choices, capabilities to support services and including security and privacy mechanisms are some examples. One approach to address these issues is to use an advanced service-oriented middleware (SOM) framework capable of integrating and utilizing advanced technologies such as cloud computing, edge/fog computing, IoT, IIoT (Industrial IoT), CPS and Big Data to relax some of the challenges of developing Health 4.0 applications. In addition, this framework can enhance current services and enable the introduction of new value-added Health 4.0 applications.
The main contributions of this paper are: (1) provide a better understanding of Health 4.0 objectives; (2) discuss and categorize different potential healthcare applications; and (3) introduce the main concepts that rationalize the SOM framework suitability to address these issues. Our work focuses on the design and features of the SOM platform and leaves implementation of healthcare services aspects as the follow-up for this work. There have been some efforts discussing the Health 4.0 vision, definition, market analysis and some of its capabilities and applications [7], [10], [11], [16]–[18]. However, we were not able to find comprehensive analysis of the main objectives of Health 4.0 and the different types of available and potential applications, or any work proposing holistic approaches using middleware to realize the real capabilities of Health 4.0. Therefore, in this paper, we first identify the main objectives of Health 4.0 and cover them under two main overarching objectives: improved efficiency and effectiveness and providing high-quality healthcare services. At the same time we implicitly include the ultimate financial objective of reducing costs. This can be inferred from the different possible enhancements, automation and streamlining of services using Health 4.0 technologies supported by a capable middleware framework. Then we provide an analysis of current and potential healthcare applications that can use Health 4.0 concepts. We categorized these in four groups: (1) applications for the patients; (2) applications supporting healthcare professionals’ work, (3) applications for resource management; and (4) high level and general healthcare system management applications. Applications in each category may overlap with other categories mainly due to the nature of healthcare services as they involve all resources and people in the system. In addition, most of these applications need specific features and functionalities that are common to all or a large subgroup of them. That led us to introduce middleware, in particular SOM, frameworks to help provide these common features for Health 4.0 applications.
The rest of the paper is organized as follows. Section II provides background information and discusses related work about Health 4.0 and about middleware as an enabling technology for healthcare systems. The main objectives of Health 4.0 are discussed in Section III and Section IV lists and discusses the categories of current and potential Health 4.0 applications. Section V introduces the concept of using SOM middleware to enable Health 4.0 and investigates the main requirements for such middleware to support implementing and operating Health 4.0 applications. Section VI concludes the paper and offers some remarks on future needs.
II. Background
The concepts of Health 4.0 and its general goals have been introduced in many different ways that in some cases could create a lot of misunderstanding of it. Here we will provide some background information about Health 4.0 to establish a base overview of the concept for the rest of the paper. We also provide a brief background about middleware as an enabling technology for healthcare applications. In both parts we include some examples of related work in the field.
A. Health 4.0 and its Main Technologies
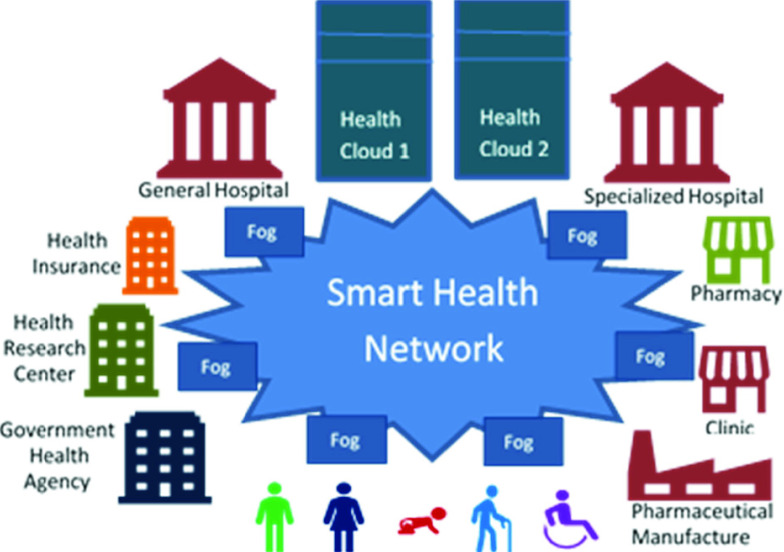
The evolution of the Healthcare utilization of ICT started with the Internet when information websites about public health and disease management were first introduced. This was followed by the emergence of electronic health records (EHR) and cloud-based and mobile-based interactive applications. The development of networked EHR systems, wearables and IoT integrated with data analytics came next. Today, we witness the emergence of Health 4.0 that brings together all these technologies coupled with real-time data collection; increased use of artificial intelligence (AI) and sophisticated analytical solutions facilitated by interactive virtual interfaces. The main principle of Health 4.0 is that by connecting patients, personal medical devices, hospitals, clinics, pharmaceutical and medical suppliers, and other healthcare-related components; healthcare providers are creating a smart health network along the entire healthcare value chain. This smart health network, as illustrated in Figure 1, changes healthcare service providing models and enables better and more effective interactions across the entire healthcare value chain.
FIGURE 1.
A smart health network utilizes ICT like medical CPS, IoT, health cloud, health fog, health data analytics, and communication.
The following is a brief overview of several ICT advancements that enable Health 4.0.
-
1.
Internet of Things (IoT). IoT connects medical devices in a network [19]. Examples include sensors to measure heart rate, body temperature, sleep behavior, and blood pressure; actuators like infusion pumps, alarms, and ventilators; and medical systems such as dialysis equipment, x-ray machines, and other diagnostic and treatment devices. This IoT is referred to as the internet of health things (IoHT).
-
2.
Internet of Services (IoS). When functionalities of medical and healthcare devices, systems, and organizations are provided as software services with well-defined interfaces over the Internet [20], they are referred to as IoS. The services on IoS (IoHS in healthcare) become the building blocks for new healthcare systems and to enable automation and collaboration.
-
3.
Medical Cyber-Physical Systems (medical CPS). Medical CPS are used to facilitate useful interactions between the cyber world (e.g. software and control signals) and the physical world (e.g. equipment and patients) by providing continuous health monitoring and treatment services [21]. Medical CPS use embedded feedback controls to monitor and react to specific conditions correctly. One example of medical CPS is Implantable Medical Devices (IMDs) [22] like deep brain simulators used to treat epilepsy, cardiac pacemakers used to regulate heart rate, and bio-instruments used to deal with bio-signals [23].
-
4.
Health Cloud. The cloud large scale infrastructure provides scalable and on-demand computation, data storage, and advanced software resources and services for healthcare applications [24]. Examples include storing EHRs, analyzing medical images, and monitoring a specific public health risk/trend. These applications require intensive computation and huge storage capabilities that the cloud can easily offer.
-
5.
Health Fog. Fog (or edge) nodes are usually used to smooth and enhance communication and integration between medical devices/systems and health clouds. Health fog can provide on-demand mini services for low latency interactive support, location awareness and mobility support [25].
-
6.
Health Big Data Analytics. Huge amount of data accumulate in healthcare systems over time. These become the input for decision making and future planning applications. Big data analytics offer advanced mechanisms to discover health trends, correlations, and insights from this data. This helps enhance healthcare services, systems, and treatment procedures; reduce healthcare costs; enhance healthcare services quality; and provide information to facilitate public health decisions and provide personalized treatments for individuals [26].
-
7.
Mobile Communication Networks (5G). 5G networking technology is promising to provide advanced features such as fast and low latency communication, smart management, and data capabilities. Using 5G will enhance the overall operations of healthcare systems, thus enabling the creation of many new and beneficial healthcare applications [27] and support for mobile health (M-health) applications [28].
-
8.
Blockchain. Healthcare services always entail collecting, storing and using sensitive data and classified information. They also require trustable operations and policies and adequate information for auditing and ensuring compliance. In addition, as healthcare systems extend to span several organizations or entities across the value chain, reliable and secure methods for creating contracts and agreements is necessary. Blockchain is one of the important and effective technologies to provide these services. With blockchain, secure and non-modifiable records can be stored and used for verification and security. The non-repudiation and transparency further ensure trustable contracts and clear agreements on collaboration rules and procedures. In addition it can provide mechanisms to achieve fairness in sharing data and protect the privacy of patients [29], [30].
Health 4.0 is based on six design principles [8], [10], [12], [31]: (1) Interoperability, the ability to connect different medical devices and systems; (2) Virtualization, the ability to create virtual/digital copies of different health devices, systems, and processes; (3) Decentralization, the ability of health systems to control themselves with suitable decisions; (4) Real-time Capability, the ability to actively gather and analyze health data to take the right action; (5) Service Oriented, the ability to create software services to interact with medical devices and systems; and (6) Modularity: the ability improve individual modules to meet new requirements and to reuse available modules to build new health/medical systems.
Recently, there is increasing interest in investigating Health 4.0 concepts, potential applications, and enabling techniques. The work in [7], [9]–[11], [16]–[18] discussed the main concept, fundamentals, principles opportunities and challenges of Health 4.0. Aceto et al. [32] reviewed utilizing IoT, big data, and cloud computing technologies for health 4.0. Mohamed and Al-Jaroodi [8] investigated the impact of Health 4.0 on healthcare system engineering. Several proposals for new applications leveraging Health 4.0 capabilities were also proposed. Thuemmler et al. [12] validated the suitability of Health 4.0 design principles for the diagnostics and therapy of asthma. Dubgorn et al. [33] discussed the advantages of following Health 4.0 concepts in engineering and implementing telemedicine systems. Sannino et al. [34] proposed a method that employs Health 4.0 capabilities to reduce the relative errors for estimating blood pressure values in a continuous, real-time, and noninvasive manner. Grigoriadis et al. [35], [36] investigated using Health 4.0 for precise mapping of multiple sclerosis symptoms over time to personalize care. In addition, Feussner et al. [37] proposed to use digitalization for surgeries, using Health 4.0 features (named Surgery 4.0), to improve outcomes and reduce costs.
Other efforts were dedicated for investigating different enabling techniques for Health 4.0. Kumari et al. [38] proposed a three-layer patient-driven health architecture for real-time data collection, processing, and transmission. Gupta et al. [39] proposed a tactile-internet-based telesurgery system for health 4.0. Mavrogiorgou et al. [40] proposed a unified method to guarantee end-to-end data and data sources quality for health 4.0. Yang et al. [41] investigated using robotic systems for homecare. Some researchers focused on security and privacy and/or using blockchain. Hathaliya and Tanwar [42] reviewed security and privacy issues in Health 4.0. Hathaliya et al. [43] and Tanwar et al. [44] proposed using blockchain to secure EHRs in Health 4.0. Hathaliya et al. [45] investigated utilizing blockchain for securing patients’ privacy and data for remote monitoring Health 4.0 applications. Gupta et al. [46] proposed a blockchain supported telesurgery framework for health 4.0. Bhattacharya et al. [47] developed a blockchain-based deep-learning service for health 4.0 applications. Qiu et al. [48] proposed a secure data sharing approach for medical CPS in Health 4.0. Finally, Chute and French [31] introduced a related concept of Care 4.0 focusing on trusted, integrated networks of organizations, people, and technologies to develop digital health and care services.
These efforts and several others are exploring the different capabilities and benefits of Health 4.0. Some address a very specific application and offer a solution. Others discuss specific features and propose mechanisms to design and implement them. As far as we got in our investigation, there are no holistic approaches for a framework with capabilities and services that facilitate the implementation and integration of many of the proposed solutions. We attempt to tackle this aspect in this paper by investigating how to make that possible.
B. Middleware as Enabling Technology for Healthcare Applications
A middleware is a software layer (or layers) that provides a set of services to enable the development, integration, and execution of distributed applications on distributed environments. It provides abstractions to enable the utilization and management of underling distributed and heterogeneous system components. Various middleware frameworks were developed and used for many distributed applications. One of these frameworks is Service-Oriented Middleware (SOM) [49] which enables interactions among distributed services and implementing distributed applications using the service-oriented architecture (SOA) [50]. SOM helps create more accessible and usable services to enable communication on heterogeneous systems with different operating systems and network protocols. Several specialized middleware platforms are designed with additional domain-specific features to facilitate the development, integration, and execution of distributed applications for the targeted domain. These specialized middleware frameworks provide value-added services designed specifically to relax common challenges facing applications in the targeted domain. Through our review of current solutions, we were not able to find works that attempt to provide a holistic solution to enable Health 4.0. Most of the work focus on creating or adapting middleware solutions tailored for a specific application in Healthcare.
There were also some efforts to utilize middleware approaches to support efficient solutions for specific challenges or certain applications in Health 4.0. Some examples include solutions to provide energy-efficiency for remote health monitoring [51]; enable e-health wireless sensor network (WSN) based systems [52]; enable ubiquitous individual health monitoring [53]; support mobile social networks in m-health [54]; enable utilizing smartphones and body sensor networks for health applications [55]; manage medical applications built on the HL7 standards [56]; guarantee synchronization of EHRs in dynamic and unreliable mobile situations [57]; enable health sensors interoperability [58]; and support IoT based healthcare [59], [60]. An interesting study of middleware approaches specifically for IoHT is presented in [61].
Moreover, some studies investigating and proposing utilizing SOA for healthcare are available. Some examples include using SOA to support home healthcare applications [62]; enable development of mobile personal health monitoring applications [63]; facilitate the integration of large-scale enterprise healthcare information systems [64]; support patient-centric care navigation system [65]; and enable online service composition for eHealth and medical systems within an integrated clinical situation [66]. In addition, some propose offering different health and healthcare resources as services using platforms like the health cloud. Examples are EHRs [67] and analysis of cell images [68]. Furthermore, SOA-based middleware platforms were developed for specific purposes like VIRTUS for e-health solutions [69]; ambient assisted living services at home [70]; Gal to support ambient assisted living by integrating sensors of a body area network (BAN) with environmental sensors to offer context to identified events [71]; and SANDS which offers clinical decision support service [72].
These efforts and several others show the importance of middleware as an enabling technology for healthcare systems. In our work we try to identify and describe how to arrive at a more comprehensive middleware framework for Health 4.0. This middleware we envision is an accessible, flexible, adaptive and expandable platform of services that can be used and integrated with specialized healthcare applications within the Health 4.0 context. It provides generic services that enable the development of a wide range of Healthcare applications at different scales. It helps integrate and utilize health clouds, health fogs, medical CPS, IoT and blockchain in addition to having the capability to include newly emerging technology. This middleware will also enable the incorporation of advanced services such as data analytics, intelligent decision making, machine learning, and virtualization tools.
III. Health 4.0 Objectives
The inclusion of Health 4.0 capabilities in healthcare will help achieve two main objectives: (1) high-quality healthcare services, and (2) improved efficiency and effectiveness, while keeping tabs on costs and resources utilization. In this section we dig deeper to expand these two objectives and discuss different Health 4.0 capabilities to achieve them. The research reviewed and presented in the previous section was the basis to formulating these objectives and organizing them. Health 4.0 offers various capabilities like fine grain data collection and management; enhanced sharing and collaboration opportunities across different healthcare services, resources, patients’ data, and healthcare professionals; increased accuracy in data analysis and needs forecasting; increased adoption of automation; and improved overall efficiency of the healthcare system. All of these capabilities, if utilized effectively, will help achieve both objectives.
-
1.Providing quality healthcare services for patients requires improving overall system effectiveness and performance, optimizing the utilization of resources, and using the system and tools to enhance the experiences of both the healthcare professionals and the patients. Examples of possible areas of change to achieve this objective include:
-
a.Improving patients’ services such as appointment scheduling, treatment protocols, health monitoring, and interactions with the healthcare professionals. This will create a better overall patient experience and improve satisfaction levels.
-
b.Improving healthcare staff, professionals and resources allocation and scheduling through more detailed analysis of current and historic operations and needs. This will allow better allocation of resources and personnel leading to improved personnel satisfaction and enhanced patients’ experiences.
-
c.Incorporating automated equipment and smart monitoring and decision-making services to enhance the efficiency and accuracy of services for the patients. As a result, it will be possible to decrease the reliance on humans for mundane or repetitive tasks, speed up many of the services offered, and reduce the possibilities of errors negatively affecting the patients.
-
d.Using detailed and comprehensive patient health records and keeping track of other factors (non-medical) that may be affecting their health will help the healthcare professionals create more personalized treatments and healthcare plans for each patient.
-
e.Analyzing current and historical data gathered about equipment and resources to set proactive maintenance schedules, perform preventive maintenance, and have better predictions of future needs. Thus, reducing service interruptions or delays and being ready to adjust quickly with changes in patients’ needs.
-
f.Enabling remote access to patients’ records, healthcare professionals and diagnostic tools. This will allow healthcare professionals to provide patients’ care in one place and reduce the delays or extra trips to different facilities for the needed services. In addition, this will enable more effective allocation and sharing of expensive or highly specialized resources, thus further improving patients’ access to these resources.
-
a.
-
2.Health 4.0 also aims to increase the effectiveness and efficiency of utilizing resources and operations for healthcare services. Examples to help achieve this objective include:
-
a.Enabling proactive maintenance using the constant monitoring and measurements to reduce costs of maintenance, improve equipment operational efficiency and reduce the number of failures leading to unscheduled repairs.
-
b.Providing the opportunity to analyze a patient’s complete health record over a long period of time to improve diagnostics and reduce the need for excessive tests and lab work and to also optimize medication use and frequency of visits.
-
c.Creating the ability to collectively gather infectious disease information across a large base of patients. This will help identify infection patterns, hot spots, and allow for better planning for resources needed to tackle the problem. This will help funnel the needed resources to the most affected areas as early as possible. In addition, it could help identify better ways to reduce infection rates and control the spread, which will reduce the pressure on the healthcare resources.
-
d.Providing a basis for analytics using collected data about patients that will allow for better understanding of common illnesses. This will help improve diagnostics, provide more insight about to correlations between certain illnesses and patients’ medical history, lifestyle and environment. As a result treatments, allocation of resources, estimates of necessary medications, will be optimized better operations and treatment protocols for these illnesses can be realized.
-
e.Facilitating the use of equipment supported by medical CPS and smart decision-making software will help automate various processes and reduce staffing needs. As a result, more efficient operations with lower error probabilities can be achieved and overall operational costs will be reduced.
-
f.Streamlining and automating different tasks personnel must perform for more efficient use of their services and better management of repetitive procedures.
-
g.Incorporating smart algorithms to create a knowledgebase for all sectors of the healthcare industry like insurers, pharmacies, hospitals, public health clinics and suppliers. This can be used by all of entities to investigate workflow, spending trends, redundancies, and operating procedures to design better and more efficient operations and protocols.
-
h.Creating optimized and more accurate operational procedures and policies based on collected data and identified problem areas and fine tuning workflow and value chain processes. As a result, resources and information will be always available to support interactive operations in the healthcare system.
-
i.Adding simulation environments using collected data about the healthcare system (e.g. digital twins or virtual environments). Simulations will help explore different possible approaches or procedures and assess or compare the feasibility and benefits of actions or procedures being considered before actually investing in them. Simulations can also help find current problems in the healthcare system.
-
j.Creating long term and strategic plans for resources utilization, acquisition, and distribution in addition to collaboration and support plans across all healthcare related industries. This includes facilities, equipment, materials and human resources to achieve timely and effective healthcare services for the whole system.
-
k.Enabling collaborative use and sharing of costly medical equipment and facilities across multiple healthcare providers to reduce operational costs and increase utilization of these resources. This will also reduce the need to move personnel and/or resources between facilities.
-
a.
IV. Health 4.0 Applications
There are different healthcare applications that have effectively used advanced ICT to achieve specific goals. In addition, there are various attempts to adopt Health 4.0 principles to further improve some of these applications. Designing and deploying applications within the larger context of Health 4.0 requires having a clear view of the capabilities and resources it offers. In addition to possessing the technical and strategic requirements to successfully develop and deploy them. The applications of Health 4.0 take advantage of all connected technologies, people, tools, equipment, and software to provide robust and high-quality healthcare services and optimized resources utilization. The following are possible Health 4.0 application areas that can support and optimize healthcare services. These are categorized in four groups of applications covering services for patients, for healthcare professionals, for resource management and for healthcare systems management. Currently available healthcare applications (some discussed in Section II) are examples that may support or fall under one or more of the identified categories. However, the discussion of the categories that follow offers an overview of the types and potential applications within each one.
A. Applications for Patients
Improving patent’s healthcare services quality and experience is essential for successful healthcare systems (after all they are the primary clients of these systems). Health 4.0 applications serving patients vary based on the goals of the applications; however, they are also related to and complement each other.
-
1.
Patient Management. Several applications are currently available for patients to find suitable care providers, schedule appointments, check in and fill medical forms, apply insurance benefits, order medications, and find self-care and wellness information. In Health 4.0, these applications and several others with similar functionalities can be integrated under one system umbrella. Patients will access the system, define their needs and the system will automatically walk them through all the necessary steps and seamlessly move the relevant data from their medical records among the different entities involved like doctors, nurses, laboratories, and pharmacies. This can also be taken further by integrating other systems and components that can help support these functionalities. For example, giving the system access to a patient’s smart devices to track health and activity changes, find suitable schedules on their calendar, remind patients of appointments or medications, push different updates and notifications to the patient’s devices, and notify the healthcare provider of anomalies or issues recurring with a patient.
-
2.Public Healthcare. Taking care of people and trying to minimize risks of developing illnesses, spreading infectious diseases, and the possibilities of developing chronic diseases is a complex task that involves people, facilities, equipment, material and information. Applications concerning preventive care, wellness programs, public health monitoring, and health campaigns can be part of Health 4.0.
-
a.Risk-Stratified Care. Patient care spans three stages: (1) primary prevention – healthy people at risk of developing chronic diseases; (2) secondary prevention – Patients having chronic disease, but keeping it under control; and (3) tertiary prevention – patients in advanced stages of chronic diseases or with significant complications. Health 4.0 applications can provide solutions to collect real-time information to track risk fluctuations and provide a complete historical view of developments based on the data collected. Doctors can devise different plans for patients based on their risk level, lifestyle, nutrition and medications. These applications can also be further enhanced to provide estimates of how a chronic disease will progress for each patient, for a community or for an entire nation.
-
b.Health Exposure Risk. Various context-aware services can be implemented in Health 4.0 to monitor a person’s mobility and activities, measure environmental exposure risks based on the person’s context, collect the person’s bio measures continuously, then use all of this is to identify the correlations between all factors and the person’s health. For example, changes in air quality can impact asthma patients and being able to know where exposure risks are high, the patient is guided to avoid them or if necessary given updates on their treatment to counter the effects quickly. Combining Health 4.0 data collection and analysis with available medical systems and patients personal monitoring devices will facilitate this type of operations, which can further improve the care patients get.
-
c.Health Behavior. Similar to monitoring people’s context, Health 4.0 infrastructure and applications using a verity of smart devices and sensors can continuously monitor everyday activities and behaviors. This offers the potentials to identify trends and use them to offer better advice for people to follow for a healthy and active lifestyle; improve people’s involvement in making decisions; provide ways to maintain accountability and better adherence to healthcare requirements; and keep track of general health conditions across different areas.
-
a.
-
3.
In-Patient Care. When a patient is admitted to a healthcare facility, several applications are possible to support the required processes. Currently most hospitals have digitized health records, programmable medical monitoring and treatment devices and various other applications helping in the process. A Health 4.0 view is being able to integrate all the services relevant to in-patient care so everyone and everything needed is directly and optimally accessible. For example, the application can admit the patient and immediately pull all available records on the patient, maybe even connect with other healthcare facilities to bring additional data. Then it will assign the necessary resources like a room or bed, doctors, and nursing and service staff. Another part of the application could connect with the dining services to specify dietary restrictions, thus allowing them to customize meals based on the patient’s condition and needs. Monitoring devices, event alerts, and medication schedules can also be managed through such applications. Applications can also allow for scheduling other possible tasks like alerts to collect lab samples, schedule and initiate surgery preparations, update visitation restrictions, etc. Finally, these applications can help in discharge processes by automatically sending prescriptions to the pharmacy, printing home care instructions, alerting care givers with updated instructions and requirements, and connecting to the patient’s smart devices to continue monitoring and advising after discharge.
-
4.
Home Care. In addition to traditional patients who need temporary home care (after surgery or injury), there is an increasing number of older adults that require home care due to age related issues. According to WHO (World Health Organization), chronic non-communicable diseases mostly affecting older people impose a great burden on healthcare systems. Creating capabilities to help these people prolong their independence, mobility and self-care capability at home is increasingly in demand. Integrating different types of services in Health 4.0 to support this goal is possible. An application can be built to monitor the patient at home, keep track of and reminds the patient of medication times, alert healthcare providers in case of emergencies, and connect the patient with the necessary healthcare providers and services. Bio measurement devices can also be integrated to create a clear and continuous view of the patient’s condition. This allows for more flexibility for the healthcare providers and can optimize the use of resources based on the different patients’ conditions. Health 4.0 applications can also connect to community care givers to keep track of patients within their area and ensure they are able to respond when needed. This could delay the need for dedicated in home care givers since medical needs are usually covered in short times. The collection of all this data and making it available to the healthcare providers cools also reduce the need for follow-up and visits and reduce the frequency of routine visits.
-
5.
Personalized Healthcare. This would be the ultimate achievement of Health 4.0 applications. Applications in all four previous categories are the basis for reaching the ultimate goal of healthcare – providing customized and personalized prevention and treatment plans for each patient. Integrating data collected in all areas and applying advance analysis and visualization techniques allow healthcare professionals to have more accurate assessments and provide very specific solutions for each case. For example, two patients suffering from heart disease but each one has other different medical conditions and live different lifestyles and maybe have different genetic inclinations for some diseases. Each one may require the same treatment for the heart disease, but most likely will need an overall different treatment plan to accommodate for the differences. In addition, this collective knowledge may result in better insights of what medications or treatments will work best for each patient, reduce possible negative impact of different treatments, and allow for dynamic adjustments in treatment based on overall changes.
B. Applications for Healthcare Professionals
People involved in the healthcare systems (other than the patients) and providing their services can benefit tremendously from Health 4.0 applications. These applications can help improve their working conditions, automate repetitive tasks, and include advanced and intelligent services to further enhance their work. Given that Health 4.0 applications gather, store and analyze tremendous amounts of data, it will be collecting the data about the personnel and how they perform their tasks as well. This data can leverage applications that streamline and optimize personnel management in different ways.
-
1.
Management. It is well known that managing healthcare personnel is a complicated task. Accounting for different types of doctors, varying levels of nursing staff, 24/7 work schedules, a vast collection of different equipment and resources and many other factors present a huge challenge for effective management. Applications leverage the collected data to help administrators evaluate operational procedures, personnel scheduling, resources allocation and patients’ treatments needs, to name a few examples, can be created and supported as part of Health 4.0. Analytics and decision-making techniques can be provided. In addition it is possible to build tools to review current operations and assess their effectiveness; forecast future needs; and explore possible future changes. Healthcare professionals can also be supported through analytics models for different diseases, patterns and trends of health issues, and support creating personalized treatment plans for their patients. Health 4.0 applications supporting the patients will also benefit their doctors and nurses as they will handle many of the trivial and mundane tasks and allow them to focus on the treatments.
-
2.
Scheduling. Excluding regular staff like clerks, custodians, and possibly administration, scheduling the professional healthcare personnel like doctors, surgeons, nurses, and therapists involve many factors that make it extremely difficult to reach an optimal schedule. In addition to the traditional factors like start and end time, location and vacations, it is also necessary to account for specialization, experience level, shifts, changes in demand, and required resources availability (e.g. hospital capacity, operating rooms, or the MRI scanners). Health 4.0 applications can be designed to pull data about the personnel, resources, demand levels and even historical data and use advanced scheduling algorithms to create optimized schedules, create contingency plans, and account for possible emergencies. This approach will help give the professionals better schedules, more predictable requirements, and improved work environment.
-
3.
Reducing “burnout”. Healthcare professionals are always under pressure to perform their jobs well and save lives. In addition, the high demand for and short supply of skilled healthcare professionals adds to the problem by forcing available professionals to take on more responsibilities. Furthermore, having to do many routine, repetitive and mechanical activities as part of their jobs further aggravates the problem. For example, many healthcare clinics require entering collected data during a patients visit digitally. As a result, you find nurses and doctors spending more time entering data than attending to the patients. All of this could easily lead to burnout, which negatively impacts the healthcare professionals performance and reduce their effectiveness. Health 4.0 applications to support healthcare professionals in terms of better scheduling, more access to needed resources, enhanced work processes and automated procedures will significantly reduce the load. Following up on the example, having doctors use dictation while they attend to a patient will minimize their time on the computer. Natural language processors, smart medical interpretation algorithms and intelligent capabilities can help create accurate digital versions of the dictated data and if necessary, someone, could review the final results at the end of the day for additional confirmation. In addition, personalized wellness features can be added as part of the Health 4.0 applications to guide them to better practices, enhanced efficiency and better management of personal and professional issues.
-
4.
Access to Resources. Healthcare personnel need a lot of resources to do their jobs. Most critical is the doctors and nurses who require consultation rooms, diagnostic devices, operating rooms, among many other resources. Assigning and granting access to some of these resources may require certain clearances or there may be a limited number of certain resources that will require scheduling. Consumables like protective gear, sanitizers, disposable diagnostic tools, etc. also need to be organized to ensure all personnel can get them when needed. Health 4.0 applications integrated with inventory control systems and resource utilization data can provide a better view of available resources and their use, optimize scheduling of shared resources, ensure continuous availability of supplies and consumables, and keep track of use, waste, and shortages to adjust procedures as needed. This can also help predict maintenance and replacement needs and reduce down times for large equipment. Keeping and analyzing all this data over time will also help identify critical over utilized resources, resources that are rarely used or abnormal patterns of use, which will help further optimize the processes and increase access to these resources.
-
5.
Collaboration. Several areas in healthcare systems require collaboration among personnel in the same facility, across facilities in the same system or with other systems and entities. Doctors need to consult with one another about some cases, they may need to consult with experts outside the facility as well. Administrators will need to exchange information or work together as they manage the different aspect in the system. They will also need to collaborate with other systems like producers and suppliers of medical equipment, transportation companies, pharmaceutical companies, insurance companies, suppliers of consumables, and possibly other healthcare facilities or systems. Adopting Health 4.0 will facilitate connectivity across all system components and can be designed to allow for links to other healthcare systems also using Health 4.0. Communication in and across systems will facilitate exchange of data, virtual meetings, online collaboration and many other group tasks.
-
6.
Remote Access. Many healthcare facilities are relatively small and do not own many of the advanced or expensive equipment. In addition, there are certain expertise and equipment that are unique to specific facilities. Having an easy and secure way to access and use such equipment will be a tremendous help to the requester and reap more benefits from this equipment. For example, one facility may have advanced and expensive tools for analyzing MRI results. Other facilities should be able to request using them to analyze their results. A business mode can also be developed to define use terms, costs, policies and management procedures. Health 4.0 connectivity can facilitate such remote access and tracking and costing tools. Including advanced methods like block chain can also help by providing ways to create usage agreements remotely, secure the data, and track all transactions.
C. Applications for Resource Management
Healthcare systems are usually huge and include hundreds (possibly thousands) of resources. These include physical infrastructures and their associated service units like HVAC, water, power, and fire alarm systems, in addition to furniture and other fixtures. We also have all medical components needed such as medical devices, laboratory and diagnostic equipment, surgical tools, sanitizing material, medications, treatment tools, protection instruments and material, and food. Moreover, all people working in the system and using the facilities and equipment to serve the patients are also resources. We can draw parallels between the applications of Health 4.0 related to the human resources (discussed in section IV-B), to physical resources here.
-
1.
Availability. Resources need to be always available when needed. Unfortunately there are many possibilities that can render some resources unavailable. For example, during emergencies like pandemics or natural disaster, hospital beds, life support equipment, medications, and even personnel will fall short. We have all witnessed this as the COVID-19 spread around the world causing shortages in hospital beds, ventilators and personal protection gear. In normal operating conditions, resources may also become unavailable due to failures, maintenance, reallocation, and misuse. Health 4.0 applications can help monitor, assess and redistribute resources based on needs and minimize unavailability periods.
-
2.
Allocation. Resources, especially large and shared ones, need to be allocated to the respective personnel for the procedures they use them for. Operating rooms, MRI scanners, X-Ray machines, and ICU equipment are shared throughout the system. There is a need for optimized allocation schedules that will increase utilization, reduce waiting time, and at the same time match the personnel scheduling and working needs. Health 4.0 applications can use usage data, personnel schedules, and patients’ records to create optimized allocation schedules for the resources.
-
3.
Connectivity. This is the most important enabler for Health 4.0 applications. Many of the applications we discussed require all components to be connected in some form (e.g. wired, wireless, Bluetooth, NFC, etc.). Equipping resources with connectivity capabilities will facilitate better use and detailed knowledge of these resources and their capabilities, status and usage history. This connectivity will allow Health 4.0 applications to collect and exchange data across components, transfer data to analysis modules, move records between facilities or across facilities, and allow measurement and monitoring devices to record their results automatically and continuously.
-
4.
Equipment Fault Management. In this context management refers to capabilities of assessing the utilization, conditions, and availability of healthcare equipment. The operational conditions of healthcare equipment are important to monitor to be able to address problems, anticipate failures and enhance maintenance and replacement processes. Constant monitoring and analysis of recorded data can help find possible failure risks, optimize maintenance procedures and schedules. In addition, close monitoring can help find faults quickly and adapt operations to minimize the effects of these failures. Moreover, this will help make the repairs or replacements earlier. Health 4.0 applications for this purpose are possible since we already collect all the necessary data in the system.
-
5.
Automation. Automating equipment, processes and the utilization of equipment will provide great benefits for the whole healthcare system as it will reduce the need for humans, provide traceable records of operations and transactions, and reduce the possibility of human errors. However, it is also a very difficult goal to achieve. Considering all the applications we already discussed, Health 4.0 services created of any of them will become a contributor to automation opportunities. A simple example, when one goes to see a doctor, a nurse comes in first to take the temperature, pulse, blood pressure and manually enter the data into the system. Here we can see that the blood pressure measurement instruments have been fully automated saving the nurse some time and reducing the skill level they need to have. Now, if these instruments (most of which has already been digitized) were capable of sharing the data with the main system and updating the appropriate records automatically, that will save a lot of time and expenses on the long run. This can be made possible with integration through Health 4.0 applications and devices. Consider another example, the embedded blood sugar measurement tool. It is already connected to the user’s smart phone and can provide readings any time anywhere and all readings are collected and stored. When adopting Health 4.0, this app can be connected to the user’s medical record and designed to provide periodic updates to the healthcare providers and alert them in case drastic changes occurred. Another area where automation can make a huge difference is in inventory control. Health 4.0 applications can provide many advanced and intelligent techniques to monitor and assess usage and inventory levels in addition to analyzing historical data and usage trends among many other factors to build automatic inventory management decisions.
D. Applications for Healthcare Systems Management
In this context we consider the different application areas supporting high level management, planning, control, decision making, and optimization. These are applications used to enhance the entire value chain in the healthcare system. Providing methods to streamline processes, automate some stages such as inventory control and insurance processes. In addition, applications to optimize transportation operations, warehousing and purchasing strategies can be applied. There is also the monitoring of resources utilization to adjust for errors, excess use, inappropriate distribution and many other aspects. Furthermore, Health 4.0 applications can be used to monitor the health of the infrastructures and equipment to discover problem areas early, optimize maintenance schedules, identify replacement needs, and create a better view of when and where updates or changes are needed. Once more, leveraging any or all of the applications discussed earlier is the key for successful adoption of effective Health 4.0 applications here. Many of the following points discuss the general view across the whole healthcare systems value chain; however, they also include many of the applications discussed earlier.
-
1.
Management. This represents an overarching perspective across the value chain to create optimized procedures, resource utilization schedules, personnel management, etc. Health 4.0 enables connectivity and interactions across multiple systems in different areas. Therefore, it makes it possible to negotiate contracts with suppliers, process insurance claims with insurance companies, enhance transportation and delivery schedules, and ensure all resources are available, in good condition and satisfy needs.
-
2.
Decision making. Health 4.0 applications can be extended to provide advanced analysis techniques, forecasting methods, and intelligent reporting and visualizations tools that collectively can help administrators make more informed decisions for the system. This type of knowledge can be used to also help identify future needs and plan for growth, changes in technology, and disaster management and recovery.
-
3.
Optimization. Similar to decision making, the data collected and the monitoring and tracking of all operations through Health 4.0 applications at all levels will provide ample data to analyze and evaluate current processes, find inefficiencies, and create leaner and highly optimized procedures and operational models. This may include relocation of resources, modified workforce numbers at different locations and possibly identifying more optimized distribution of services across different service locations.
-
4.
Automation. Similar to automating healthcare equipment and procedures within a facility, there are also a lot of benefits of automating value chain activities for the whole system. One example is automating reorders and delivery of consumables; automating processes for food supplies, meal preparation, and meal distribution to hospitals; and creating automatic schedules to ensure medications and medical supplies are always appropriately stocked. Moreover, automation can also help improve overall workflow across the different entities including suppliers, warehousing, transportation and insurers.
-
5.
Fault management. Another expanded area from fault management discussed for the resources above. In this case, we consider failures and problems at any area of the value chain such as delayed delivery, changes in supplier prices or sales conditions, compliance issues, and shortages in row material or supplies. Health 4.0 allows for more intimate integration of different supporting applications across the value chain. This creates a suitable environment to deploy fault detection, mitigation and correction techniques to enhance the overall effectiveness and efficiency of the whole healthcare system value chain.
-
6.
Disease and Disaster Response. There are many possibilities of events that can overwhelm the healthcare system and its value chain. A major natural disaster like a hurricane, earthquake or volcanic eruption will generate a large number of injuries that require healthcare. There are also deliberate actions that could lead to similar results like mass shootings and bombing in addition to possible accidental incidents at highly populated events like concerts and sports events. There are also infectious diseases that could start a pandemic and lead to hundreds or thousands of cases in a very short period of time. Healthcare facilities are usually designed to handle more than expected average capacity to accommodate unexpected increases in healthcare needs. However, high and fast increases in cases beyond the local healthcare facilities capabilities will be a huge problem. Health 4.0 can help in various ways. In a case where the increase in healthcare needs is localized (within a city, or even several adjacent cities, Health 4.0 applications can fall back on the available operational data, value chain status and divert resources to the affected areas from the nearest facilities. Some applications can also analyze and recreate schedules for personnel, allocation procedures for resources and initiate contacts with the different entities in the value chain to bring in the necessary resources. However, when the problem is widespread or possibly global like this current COVID-19 pandemic, simply rerouting resources may not be a good enough solution. More intelligent approaches are needed to estimate needs, find new sources, and possibly create connections with other industries to help. Here we can see more value of having a Health 4.0 infrastructure to provide the necessary data and the needed connections and collaboration to achieve best results.
E. Applications and Enabling Technologies Mapping
Different technologies play important roles in different Health 4.0 applications. For example, health fogs are used for applications that need to provide local processing, storage, and smooth communication with external systems. Data analytics is important for applications that involve decision making and long-term planning, while Blockchain supports secure access, privacy, secure ledgers and fair collaborations among different entities in healthcare. One important observation however is that IoS and health cloud technology are needed in almost all applications. The cloud in this context refers to the main healthcare system platform that could be available on public, hybrid, community, or private clouds. Thus it implicitly includes internal organization-owned systems and data centers. Therefore, it is absolutely necessary to ensure proper integration of the services in the system. In addition, IoS enables the registration, discovery, and integration of services representing any of the health system components such as IoT devices, Medical CPS services, fog-based services, and of course, cloud-based services in the main system.
Table 1 provides a summary that illustrates the relationships between key enabling technologies discussed in Section II and Health 4.0 applications listed and discussed in parts A. thru D. of this section. Generally, one could argue that all applications require practically all or almost all technologies listed. However, the nature of each application dictates some specific needs that must be satisfied and some that can be considered optional or peripheral. Therefore, in this table, we focused on identifying the key technologies essential for the corresponding type of applications. For example, health fog is usually necessary to provide localized small-scale storage or services to some IoT or CPS components that may need additional capabilities. For example, when considering something like scheduling resources, or personnel, the main systems on the cloud are capable of handling those tasks without fog support. However, dealing with multiple patient monitoring devices that need to collect and compare readings continuously, we possibly require support from local services executing on fog nodes to provide fast real-time analysis and responses. Another example is the need for IoT components. These can be present and used in most applications. However, they are only included for applications where they are considered the main enabling technology. For example, patient care applications will always need IoT since most monitoring and alert devices are IoT-based; yet applications like resource scheduling, appointment scheduling and professionals collaboration will mostly rely on other technologies like the cloud, data analytics, and/or Blockchain.
TABLE 1. A Summary of the Relationships Between Key Enabling Technologies and Health 4.0 Applications.
Enabling Technologies
 Health 4.0 Application (By Category) Health 4.0 Application (By Category) |
IoT | IoS | Medical CPS | Health Cloud | Health Fog | Data Analytic | 5G | Blockchain |
|---|---|---|---|---|---|---|---|---|
| Applications for patients | ||||||||
| Patient management | ✔ | ✔ | ✔ | |||||
| Patients/People care | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |
| In-Patient care | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| Home care | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |
| Personalized healthcare | ✔ | ✔ | ✔ | |||||
| Applications for healthcare professionals | ||||||||
| Management | ✔ | ✔ | ✔ | |||||
| Scheduling | ✔ | ✔ | ✔ | |||||
| Reducing “burnout” | ✔ | ✔ | ✔ | ✔ | ||||
| Access to resources | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |
| Collaboration | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| Remote access | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |
| Applications for resource mgt. | ||||||||
| Availability | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| Allocation | ✔ | ✔ | ✔ | ✔ | ||||
| Connectivity | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |
| Equipment fault management | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||
| Automation | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||
| Applications for healthcare systems mgt. | ||||||||
| Management | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| Decision making | ✔ | ✔ | ✔ | ✔ | ||||
| Optimization | ✔ | ✔ | ✔ | ✔ | ||||
| Automation | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| Fault management | ✔ | ✔ | ✔ | ✔ | ||||
| Disease and disaster response | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
F. Issues and Opportunities
Adopting Health 4.0 to achieve the two main objectives, efficiency and quality of healthcare, can help improve various areas in healthcare and create more value-added functionalities current systems cannot offer. There are different aspects in current healthcare systems that need to be tackled and improved for better adoption of Health 4.0. These may be considered challenges to the application of Health 4.0 and at the same time some provide good features and have the potential for more enhancements by adopting Health 4.0. Some examples of these issues include:
-
1.
Addressing the issues of fragmented and incompatible medical records and patients’ health data across multiple divisions within a single healthcare provider and across multiple providers.
-
2.
Providing ways to overcome the lack of standardized data representation models and interfaces across different applications in healthcare systems.
-
3.
Adding better ways for continuous and fine grain data collection in most areas of healthcare that can then be used for advanced analytics and decision making in addition to enabling more sophisticated value-added smart features.
-
4.
Including effective models to ensure data privacy and protection for everyone and everything involved including patients, staff, professionals, healthcare organizations and all entities in the healthcare systems value chain.
-
5.
Providing secure and effective methods for managing the sharing and exchange of medical records, health data, and organization information across multiple healthcare providers and related organizations that also address access policies and privacy issues.
-
6.
Introducing effective and efficient automation tools and monitoring services for healthcare records, procedures, and operations.
-
7.
Facilitating the integration of heterogeneous healthcare systems resources such as data, medical devices, smart devices, monitors, and control units with effective intelligent software services.
-
8.
Helping healthcare systems managers design and evaluate leaner processes with higher reliance on technology to achieve optimized operations and lower costs.
-
9.
Providing ways to analyze the use of resources and detailed operational expenditure to find more optimization methods that help improve resources utilization and sharing.
-
10.
Adding features and facilities to include intelligent techniques/algorithms for smart operations, enhanced forecasting and better visualization tools.
-
11.
Creating ways to allow for change and adoption of new technologies as they emerge and facilitating seamless integration of new devices, equipment and services.
-
12.
Providing effective secure collaborative techniques to facilitate different healthcare service providers and related industries to work together to streamline workflow, enhance the supply chain, find faults, identify trends, and predict future needs in the healthcare systems.
-
13.
Supporting the optimization and automation efforts for the healthcare systems value chain and enhancing the integration and management capabilities across the different entities.
G. Service Models and Health 4.0 Applications
Examining the main objectives of Health 4.0 in light of these possible gains, we can see some common needs in terms of data collection and management, system and service integration and collaboration. In addition, there are various common features and functionalities that most if not all applications need. These include robust network connectivity and services; data collection, management and analysis services; Access to heterogeneous resources both local and remote; security and privacy support; and facilities for data and resources sharing and collaboration needs.
Ideally, Health 4.0 applications will perform best if built from the ground up. This will ensure compatibility, interoperability, and standardized data representation and application interfaces. However, this will be expensive, complex and inefficient given that many areas in healthcare have been digitized and some also automated. Many individual applications are in place in different facilities and healthcare systems that are effective and suitable to be part of the Health 4.0 infrastructure and resources. Therefore, rebuilding a complete healthcare system in the Health 4.0 domain does not have to be done from scratch. Instead there is an immediate need to create a framework that can use available infrastructures and services, expand the features, optimized other features, and introduce new features as part of a complete integrated Health 4.0 application.
SOA is a suitable framework that can introduce service-oriented capabilities and middleware support. As apparent from the previous discussions, many Health 4.0 functionalities are or can be represented as services. These services offer specific functionalities and can be combined to effectively provide more under the SOA. However, the common functionalities across applications can be identified and separated in a middleware layer. This layer will offer different base features like security, connectivity, interoperability, and integration for the application-specific services to connect to and use as part of a Health 4.0 application. In addition, the use of middleware services can simplify the introduction of new services, extend the capabilities of the infrastructure, facilitate further integrations across multiple Health 4.0 applications and systems, and provide a base to support integration of healthcare systems with other supporting systems like manufacturing, transportation, suppliers, research facilities, to name a few. In the next section we introduce a service-oriented middleware framework to provide the necessary services for Health 4.0 applications.
Table 2 offers a summary that links the Health 4.0 applications with the objectives (Effectiveness and Quality) discussed in Section III and shows which ones each application listed satisfy. Here one can argue that all applications satisfy practically all objectives. However, in the table we highlight the objectives that are directly and significantly relevant to each application. In addition, we included references to some of the issues to address when designing Health 4.0 applications and middleware support services. Generally all challenges apply to any application targeted for healthcare. However, some have higher significance for some applications than others. For example, applications collecting and storing patients’ data in the system must pay very close attention to privacy issues, but applications managing maintenance schedules does not have the same urgency for privacy. In addition, the table provides a glimpse into the general areas in healthcare systems where adopting Health 4.0 could lower the costs.
TABLE 2. Connecting the Dots With Health 4.0.
| Application Category | Application Type | Quality Objective1 | Effectiveness and Efficiency Objective1 | Main Services for Support3 | Issues to address4 | Cost savings5, 6 |
|---|---|---|---|---|---|---|
| Applications for Patient | Patient management | a & d | g |
|
1, 2 & 4 |
|
| Patients/People care | a, c & d | b & d | ||||
| In-patient care | a, c & d | b & e | ||||
| Home care | d & f | g & i | ||||
| Personalized healthcare | a, d & f | b & e | ||||
| Applications for Healthcare Professionals | Management | a, b & f | f |
|
1, 2, 3, 4 & 10 |
|
| Scheduling | b | g, h & i | ||||
| Access to resources | a & f | G | ||||
| Collaboration | d & f | c, d, f & g | ||||
| Remote access | a, b & f | b, c & f | ||||
| Applications for Resource Management | Availability | a & b | a, e & g |
|
4, 5, 6, 6 & 11 |
|
| Allocation | b & f | e & g | ||||
| Connectivity | all2 | all2 | ||||
| Eqpt. fault management | c & e | a, e & f | ||||
| Automation | all | all | ||||
| Applications for Healthcare Systems Management | Management | a, b, e & f | c, f, e, g & h |
|
2, 3, 4, 5, 9, 10 & 11 |
|
| Decision making | all2 | all2 | ||||
| Optimization | all2 | all2 | ||||
| Automation | all2 | all2 | ||||
| Fault management | all2 | all2 | ||||
| Disease & Disaster Response | all2 | a, c, d, f, h & i |
Notes:
The objectives column uses the list of objectives discussed in Section III. The objectives mentioned are the ones that strongly relate to the application. Other objectives may also relate, but with less effects.
All means that this application affects all parts of an objective and none has more significant impact than the others.
Service support mentions some basic services needed to facilitate this type of applications.
Issues to address are listed in Section IV. Most relevant ones are listed.
Cost savings outline some ways these applications can save costs in the healthcare system.
-
a.Equipment: enhancing efficiency, optimizing scheduling and maintenance, sharing expensive equipment, optimizing patients’ diagnostics and treatment requirements, improving public health, and prolonging independence and delaying hospitalization or totally dependent home care for the elderly.
-
b.Healthcare professionals: optimizing scheduling, sharing experts, automating procedures and streamlining workflow will allow these professionals to focus on their primary jobs. This can also optimize other staffing needs and reduce the dependence on humans in various areas.
-
c.System: overall operational savings like reducing waste, optimizing supply chain, minimizing paperwork, using remote access, etc.
-
d.Patients: savings in healthcare systems costs should reflect into reductions of healthcare services costs for patients, reducing the need for continuous human support and monitoring, delaying the need for labor intensive and complicated home care.
V. Enabling Health 4.0 Using Middleware
Realizing Health 4.0 relies on various technologies and enabling services. The infrastructure is highly distributed, heterogeneous, and in many cases not interoperable. In addition, resources in this infrastructure may be as extensive and powerful as cloud nodes running complex and high-performance services and as very small and limited as a thermometer, and everything in between. Examples include health clouds, health fogs, medical CPS, IoT, robotics, sensors and many other devices and systems. Implementing Health 4.0 applications directly on the top of such heterogeneous distributed infrastructure is extremely difficult and will need huge efforts and time; thus, it will be an extremely costly process (if it is actually doable). The SOA offers a systematic model to help overcome some of the difficulties by realizing elements of the infrastructure and software components as services. At that level, we still need to deal with various common aspects needed for practically all Health 4.0 applications, hence the introduction of middleware (SOM in particular) into the mix. In this section, we will discuss our concept for SOM framework for Health 4.0 and the main requirements and support features (services) needed in this SOM framework to enable Health 4.0 applications.
A. SOM Framework
Offering an advanced middleware framework for Health 4.0 will enable the development, integration and execution of different Health 4.0 applications. In addition, it will make it simpler to integrate multiple healthcare applications with each other and with external related systems. This will reduce the complexity, effort needed, and cost of developing such applications. In addition, it will reduce the effort needed to test new applications as these applications will be built on top of functions that are already developed and tested with high quality standards. Furthermore, using middleware will also enable the integration of old/legacy healthcare systems with new ones, thus increasing the reuse of working software and components. This will enable healthcare information available in different healthcare applications to be used and exchanged smoothly among these integrated applications. Adding reliability features in the middleware will also help in enhancing the reliability and integrity of the execution of many distributed Health 4.0 applications. Other advanced functions such as security and management can be added and used to improve the operations of the Health 4.0 applications built on top of the middleware framework.
A middleware framework for Health 4.0 must enable the Health 4.0 design principles including interoperability, virtualization, decentralization, real-time capability, service orientation, and modularity (discussed in Section II). In addition, it must support utilizing the Health 4.0 enabling technologies such as IoT, IoS, medical CPS, health cloud, health fog, and blockchain (also discussed in Section II). Therefore, SOM (service-oriented middleware) is the most suitable type to use to design a SOM framework for Health 4.0 applications. Using the SOM framework is considered a practical approach to help relax some of the difficulties in developing distributed systems [73] in general. SOM, then, inherently support the design principles of Health 4.0 applications. However, generic SOM platforms are not well suited, as is, to support the specific needs of Health 4.0 applications.
The SOM framework for Health 4.0 can be presented with multiple layers as shown in Figure 2. It operates on top of the different technologies and infrastructure components in a healthcare system. These technologies provide services and functions for different purposes. These services can be integrated and utilized by the SOM framework directly if they are defined using web service standards or using adopters or wrappers that convert each function to a web service. It can utilize available services belonging to different technologies while adding other services to support the Health 4.0 applications. These added servicers are organized in three layers in the proposed SOM framework for Health 4.0 applications. The bottom layer consists the core services that integrate all available Health 4.0 technologies and provide other services with the required functionalities to be registered, discovered, and used. The middle layer is the SOM Value-Added Services layer, which consists of some advanced services to support different Health 4.0 applications such as security, fault-tolerance, and context-aware services. The top layer provides specialized and advanced services to support specific Health 4.0 applications. These services are usually needed by multiple Health 4.0 applications, but not general enough to include as services for all applications. One example is analytical services needed by diagnostics, supply chain, or disease tracking applications. Each of these analytics services will be tailored to the application to effectively and accurately perform the required analysis.
FIGURE 2.
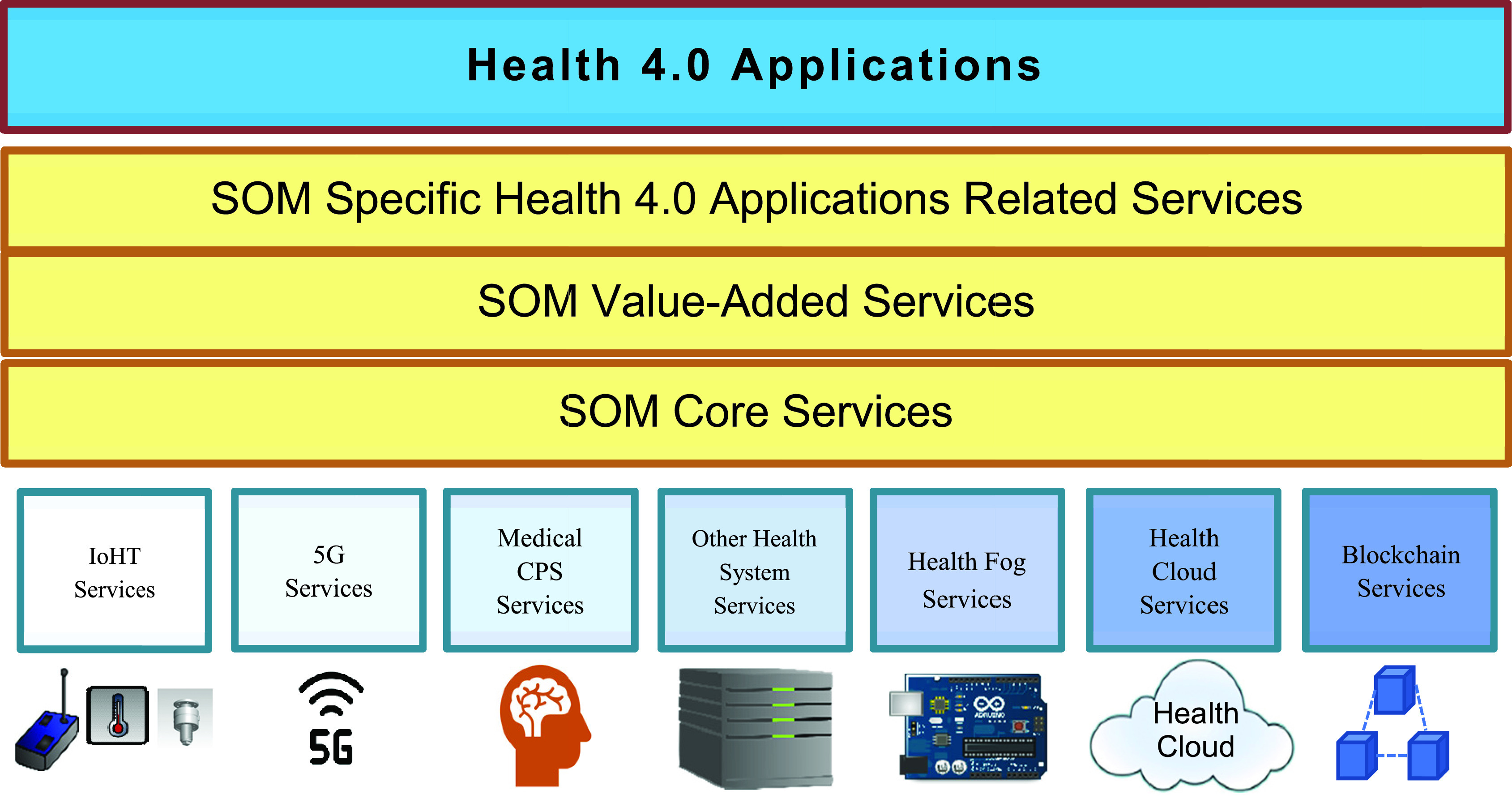
SOM integrates different healthcare services and supports Health 4.0 applications.
This layered and SOM approach allows for flexibility and dynamic adoption of new technologies and smooth transitions from one technology to another. It could easily start with only core services to enable base line Health 4.0 applications and expand as needed to incorporate other types of services as they appear. Finally, Health 4.0 applications are expected to evolve and increase with the advances of all the enabling technologies; the emergence of intelligent and optimized software services; and the need for new service models and healthcare facilities. The multiple layers in the SOM will provide these applications with the flexibility to introduce new services for their needs.
B. SOM Framework Support Services
Here we discuss and analyze some of the services needed in the SOM framework for Health 4.0 applications. These services will provide the required functionalities to support the different needs of these applications.
-
1.
Brokering. In this framework, all Health 4.0 components, systems, and software will be realized as services that collectively can implement full applications. These services need to be registered, advertised, and discovered to actually be useful. Brokering services in the SOM framework will provide these functions so that a service can register itself in a service repository [49]. The brokers also ensure that services are visible and available for use by any Health 4.0 application. In addition, the brokers will provide requesting services with the tools to discover available services in the repository and select the ones needed. Healthcare systems may be owned by a single entity (e.g. a single hospital system) or by multiple health entities (e.g. various hospitals, health clinics, homecare facilities, insurance companies, pharmaceutical companies, etc.). In this case each Healthcare system using the SOM framework will have its own broker, where the owner can define access and usage rules for its services. The broker will be responsible for enforcing these rules when integration and collaboration of services is needed across different entities to enable Health 4.0 applications across these systems. In a large multi-entity healthcare systems, there is a need to use a scalable structure for brokering services. This can be realized by creating a set of brokers organized in a hierarchical structure where lower level brokers are local brokers for an application or entity and brokers in the upper levels combine information about services available from the services managed by the local brokers below.
-
2.
Service Invocation. The SOM framework must provide services to enable services’ interactions through service invocation mechanisms. An application utilizing services will need to invoke some available services to achieve its goals. These services may be hosted locally within one machine or distributed among multiple hosts in the distributed environment. The invocation services are responsible for creating the correct invocation methods and integrating the requested services with the requesting application during run time. These mechanisms facilitate the integration of several services in various locations in the environment into complete Health 4.0 applications. Service invocation provides one approach for services to interact, it provides one-to-one interactions through request/response communication. In addition, it is considered a synchronous interaction that requires both the requested service and the requesting application to be in synch during the execution of the service.
-
3.
Decoupled Communication. There are several methods to achieve services interactions in a decoupled and asynchronous manner. Examples include notifications, emails, service queues, and workflow triggers, which all are based on the occurrence of an event that will trigger the communication. Event Notification is one of the most popular approaches that help avoid the shortfalls of synchronous service communication. This is very useful since many healthcare related activities need to be executed only when a specific condition is met (an event). These events represent operational or health conditions affecting the system, its users, or the patients. For example, an emergency procedure to activate a ventilator can be triggered by a drastic drop-in breathing rate of a patient or maybe it could be the activation of specific security actions when a user tries to access services beyond their clearances. These events do not have a specific time or pattern of occurrence. Therefore, it is important to be able to decouple the functionality, where we have services to watch for events happening and send notifications to the needed services to handle them. This requires communication mechanisms that provide efficient asynchronous one-to-one, one-to-many and many-to-many interactions. The SOM framework should provide event notification services using some form of publish/subscribe mechanism [74]. This can be supported through available infrastructure resources such as fog computing and 5G networks to provide services to support event notifications within the Health 4.0 system.
-
4.
Interoperability and Function Wrapping. Integration allows for effective utilization of available services in a system. However, when integrating different components and services it is common that many of these are incompatible or cannot communicate correctly as is. This is mainly due to the fact that not all devices, systems, and existing healthcare applications have standard and interoperable service interfaces. Therefore, the SOM framework should support features to help. Wrapper services that hide the original interfaces of a service and convert it to the interface used in another service is one example. Adapter services can modify or adjust certain interfaces to match other services without having to actually change the coding or design of these services. The SOM framework should include services of this type to allow for better integration and utilization of existing components and services.
-
5.
Real-Time Communication and Processing. In healthcare, it may be possible to wait to get the results of some lab test or to get a response from an insurance company regarding a claim. However, there are many activities and services that require constant monitoring, stream-based data analysis, and immediate activation of other services in response. If a patient’s heart monitor registers abnormal patterns or drastic change in heart rate, an immediate action is needed to resolve the issue before the patient dies. Similarly, systems monitoring environmental factors, homecare procedures and emergency response teams must all operate in real-time. There is no room for delays in these situations. The SOM framework needs to be capable of handling high volumes of data, analysis and event responses in real time. Services for real-time features can be implemented and made available in the SOM. It is also important to strategically utilize all available resources in the system like cloud computing with high performance capabilities, fast response processing on fog nodes, and fast and effective communication infrastructures like 5G.
-
6.
Virtualizations. The SOM framework should also include services to enable the visualization and virtualization of different healthcare processes implemented and operated using the SOM services. Creating a virtual copy or image of a system or part of a system relies on the availability of detailed and accurate data representing the system, its processes, infrastructure and operating environment. In addition, using services to provide dashboards and visualized models help identify trends, problems, and areas of improvements. The SOM framework services reside between the infrastructure and enabling technologies and the Health 4.0 applications. Therefore, it should be able to monitor, record and organize all data and operations in the system to facilitate the creation of the data visualizations and virtual simulations. Virtualization services are important for several purposes such as analyzing operations, simulating different scenarios, investigating problems, and comparing different methods of implementing new services [75], [76].
-
7.
Fault-Management. Heath 4.0 applications utilizing different technologies, components and capabilities, will experience failures in any of its parts. It is important to be able to manage failures in terms of early discovery, mitigation actions, counter measures, and recovery plans. This feature is covered at many levels in a system; however, application specific components and operations are usually not covered in the same ways. For example, the health cloud is designed to provide highly available services using transparent fault-management mechanisms that ensure the continuity and reliability of its services [77]. Several types of medical equipment have built-in fault management measures as well [78]. Other technologies such as fog computing, individual and small devices, and application specific services still lack such features, yet some are working on addressing this issue such as the work to introduce fault-tolerance for fog computing [79]. Therefore, it is necessary that the SOM framework include services to manage failures and support overall Health 4.0 applications fault tolerance beyond what is available.
-
8.
Scalability. Healthcare systems grow with the increase of population and average lifespan resulting in more elderly people in need of care. In addition, special circumstances could drastically increase demand on healthcare services. These are usually related to incidents leading to mass injuries or illnesses. Health 4.0 applications need to be capable of adjusting to match these changes in demand quickly, efficiently and without sacrificing performance or quality. The SOM framework can be equipped with services that will seamlessly facilitate this growth through different scaling capabilities. As the middleman, the middleware is aware of available resources and capabilities; therefore, resource management and optimization services can be implemented. In addition, the middleware should be capable of pulling additional resources to distribute the load to match the demand (i.e. horizontal scaling). IT should also support services to keep track of the status of applications and their execution stages and data so that they can migrate some or all to other larger resources (i.e. vertical scaling). Currently some technologies used in Health 4.0 applications such as health cloud are designed to be scalable, other technologies like health fog lack this feature. However, health fog nodes can be arranged in a more scalable fashion such as in a hierarchical structure [80] for better scalability. The SOM framework could include features to enable utilizing such structure to provide a base for scalable services [81].
-
9.
Security. Technologies and components integrated in Health 4.0 applications have varying levels of security. Some are resource-constrained like sensor devices and small control devices and cannot incorporate security mechanisms. Integrating these components that are also developed by different manufacturers with different operating standards in a Health 4.0 applications could create many security concerns [82]. To further complicate the issue, many devices and systems used are complex and generally protected when operating individually or as part of a well contained distributed system such as a Health 4.0 system serving a single healthcare facility. Once integrated further, these devices and systems become exposed to additional security threats from the networks and other components. One possible solution for this problem is to include security services as part of the SOM framework and make them available for these applications. These services can add security for unprotected components and secure connectivity and integration of system components. These could be advanced security services including encryption, authentication, access control, and firewall services. An investigation of security issues and an initial middleware-based solution are presented in [83].
-
10.
Privacy. Health 4.0 applications rely heavily on collecting data and creating knowledge. Usually it is expected that the application specific services will provide their own privacy protection features. However, there is a possibility to further support these by providing additional services as part of the SOM framework. For example, when certain sensing devices collect private data that do not particularly pertain to the application’s needs, the middleware can provide features to anonymize this data. Another example is services to obscure specific sensitive information during the data collection and transfer process. One relevant middleware-based approach for maintaining privacy of patients using IoHT devices when remotely sending their health data to cloud healthcare services is presented in [84], [85]. This approach uses personal gateways executing on fog nodes at the patients’ side. This approach can be implemented and provided as a service in the SOM framework.
-
11.
Mobility. Although the general conception is that healthcare devices and services are stationary or intermittently movable, there are many areas where mobile components are used. For example, a connected emergency medical transport (EMT) vehicle will move at significant speeds, but still needs to remain connected and active. Patients may be given portable monitoring devices as part of a medical CPS or need to connect their own smart devices as part of the system, thus requiring mobility support as well. Moreover, healthcare professionals are always on the move and defiantly need to stay connected and able to access the appropriate services when and where needed. Mobility support services need to be included in the SOM framework to create an inclusive environment for all mobile devices.
-
12.
Context-Awareness. The context in which a health 4.0 system and its components operate can be used to personalize services and provide context-specific versions of these services. Some reliable and automated healthcare services require knowledge of the context of their operations such as location, ambient conditions, current physical activity, and battery levels of medical devices for their effective operations [86]. This context can be utilized to extract more accurate information about the health condition of patients or the status of specific medical devices [87], [88]. This information can be used to provide better treatment for patients and manage and configure the medical devices. For example, if a physician is working with a patient, services pertaining to the patient’s needs and diagnostic services should be readily available for them. However, when the physician is in the operating room performing surgery, diagnostic services become less important, while services assisting in performing the procedure become more prominent. In addition, when a mobile component moves to a location with less reliable networks, the SOM framework could initiate services to stabilize the communication and buffer content. Furthermore, if a user or patient connects to the application from an unsecured network, these services could provide additional encryption and security services. The SOM framework must be flexible, reliable and capable of discovering and adapting to changing context quickly. There are some efforts to include support for context awareness in middleware to support specific healthcare scenarios such as personal smart health and elderly homecare [89]–[91].
-
13.
Collaboration. This is considered an advanced capability for Health 4.0 applications; however, it is increasingly growing in terms of needs and usage [92], [93]. Medical devices may need to connect and work with other devices to complete a task [94]. Healthcare professionals can make use of services that could help them discuss and exchange case information with colleagues or remote experts. Healthcare administration also require various levels of collaboration for managing resources, collaborating with other healthcare systems or value chain systems, and orchestrating healthcare processes in case of disasters or pandemics. The SOM framework can offer services supporting collaboration such as increasing the reliability of data exchange and integrity, providing tracking, securing transactions using new technologies like Blockchain, and offering services to support sophisticated online collaborations facilities.
C. SOM Services in an Example Application
To show the possibilities of how an SOM enabled Health 4.0 application will work, consider one implemented to monitor and personalize treatment for patients with chronic illnesses like diabetes or heart disease. We have a patient, physicians, nurses, nutritionists, medical labs, pharmacists, and insurance processing staff. In a comprehensive Health 4.0 system all of them need to exchange and use some data about the patient to offer complete and personalized services. Each one will have some localized or special services that will need support or data from services the others have. We need a platform that can support this connectivity and collaboration seamlessly among all participants. This platform will allow the patient to monitor and share daily health metrics collected by personal smart devices or monitors. The devices will collect the data on a regular basis and store them in some type of smart device the patient owns. The patient can also use the smart device to record nutrition information, medication times, activity levels, and possibly external environmental elements like humidity and pollution level. Health 4.0 services on the smart device will monitor this data and track changes; encrypt and send the data to the patient’s EHR; and issue alerts to the patient and/or the relevant healthcare units when necessary.
The services will run in the background continuously recording data and generating periodical reports and trends. If a problem or abnormal situation occurs these services will start designated procedures to respond. For example, if the heart rate gets elevated beyond a threshold for longer than a specified amount of time with no apparent reason a service triggers an alert to the patient to attend to the issue. If the condition persists, another service will send notifications to the nursing staff in the healthcare facility to follow up. Other services can intervene as needed to remedy the situation. Services to remind the patient to do daily tasks like eating, drinking water, moving, taking medications or performing a test can be integrated in this system. Services may also automatically initiate required procedures like setting up appointments to see the physician or do lab tests and services to secure a ride to the healthcare facility.
In an emergency, the patient’s services will start invoking more services to address the problem. It could start by an alert to the healthcare facility staff and a simultaneous transfer of the patient’s latest record from the patient’s device and the EHR from the main healthcare system to them. After evaluating the situation, the staff could trigger other services like dispatching an EMT to the patient, alerting designated emergency contacts, requesting specialized physicians, preparing for tests or other procedures, etc. If the patient is transported to a different healthcare facility (possibly a closer one), the system can request EHR transfer from the original facility. If the patient is admitted, then additional services will be triggered like assigning the room/bed, setting up medication and treatment schedules for the nurses on duty, providing nutrition requirements to the food services, and creating monitoring and treatment protocols.
Considering this example, we can see how a fully connected infrastructure of services will make this possible. In addition, many current applications offer some of the described tasks like appointment systems, EHRs, some types of monitoring and alert capabilities, among others. However, these applications are independent from each other and connecting them requires deliberate and explicit changes and a lot of redevelopment. The proposed SOM framework can offer its services to enable the integration of available services, streamline connectivity, and allow for the addition of new services. Examples of these enabling services include:
-
1.
Brokering services that allow services on the patients’ smart device and in the healthcare system to find and utilize the services they need such as the patient’s heart rate monitoring service activating the alert and data transfer services at the healthcare facility.
-
2.
Invocation services are needed to start the execution of the needed services either locally such as the service reading temperature can start the execution of temperature trend analysis service on the patient’s smart device, or remotely activating an alert service if the temperature read is too high.
-
3.
Decoupled Communication among services facilitate connected yet independent operations of different services for example a patient’s service activating a remote alert service does not have to get stuck waiting for a response, instead it could go back to do its other functions until a notification comes back for the request.
-
4.
Interoperability services that allow components to work together even if their original designs are not compatible. This helps different applications designed and developed by different entities (possibly at different times with different technologies) to understand each other and use the functions each provides.
-
5.
Real-time support services for access and utilization of services requiring fast responses. An example would be services that must alert the healthcare staff when a patient’s vital signs become abnormal or life threatening.
-
6.
Fault management services to ensure continuous highly available services throughout the system. You do not want your insulin pump to fail or malfunction while connected to a patient.
-
7.
Scalability services that ensure the ability of the application to remain stable and perform to standards even when the usage and demand grows significantly. Services handling patients at a hospital could be put under severe stress in a major disaster. Without scalability capabilities, these services could easily start to fail under this pressure.
-
8.
Security services to help fortify security measures in general and support integrating domain specific security services. This includes ensuring secure utilizations of devices and services across the whole system.
-
9.
Privacy support services to enable applications to implement and integrate their own privacy services. For example, ensuring safe delivery of patient data to their HER without risks of exposure.
-
10.
Mobility services that ensure a service will continue normal operations while in motion. EMT vehicles must remain connected to the healthcare provider to help with diagnosis and temporary treatment, while in transit.
-
11.
Context awareness services to help available services to act differently if their context changes. For example, if the patient has a fall detection service, it should recognize if the patient is walking at home or in the park versus being in a vehicle on a bumpy road.
-
12.
Collaboration services for entities and services to work together (both synchronously and asynchronously) using the same resources or data. For example, when a patient is transferred to a different facility, records, diagnostics information and historical data can be easily shared between facilities. This also allows physicians to share medical data and work together on the case remotely.
-
13.
Advanced virtualization and data services provide additional value-added features for more sophisticated customizable capabilities in different applications.
VI. Conclusion and Future Directions
Industry 4.0 in general aims to automate and autonomize the industry it targets. Health 4.0 is one area where industry 4.0 approaches are deemed extremely beneficial. Introducing smart, autonomous and enhanced healthcare services will greatly impact the quality and efficiency while reducing costs of healthcare. It delivers the ability to integrate healthcare organizations, care procedures, extensive amount of health data and use these to provide enhanced patient care, improved facilities and resources management, and effective cross-organizational collaboration. For example, considering the current pandemic of COVID-19, many of the efforts to combat it were supported heavily by technology, data analytics, tracking applications and medical research. If Health 4.0 was enabled across all these sectors and several others, everyone involved will be able to collaborate, share data and resources seamlessly. As a result, more solutions, vaccines, treatment protocols and protection plans would have been achieved, more informed decisions made, better public awareness and protection accomplished, and more effective approaches to solve the problem found faster and with a lot less resources and at lower costs.
We introduced the concept of SOM as an enabler to provide effective and efficient ways to implement and support Health 4.0 applications. It provides standard integration and access methods for available services. It also provides essential services to help applications find and use needed services. Moreover, it allows for better integration across different platforms. This facilitates developing a wide range of services and processes integrated under the Health 4.0 umbrella. It also allows applications to realize specific requirements for response times, quality of service, and security to mention a few.
In this paper we worked our way to demonstrate the advantages of SOM for Health 4.0 applications and demonstrate how it could offer a holistic approach to healthcare applications development and deployment as comprehensive Health 4.0 systems. We started by defining the main Health 4.0 objectives: enhancing the quality of healthcare services; and increasing efficiency and effectiveness with the intention of doing so at minimum cost. Then we took a close look at possible applications that collectively can form a comprehensive Health 4.0 healthcare system. These applications were organized in four categories for patients, healthcare professionals, resource management, and healthcare system management. This revealed the different issues and opportunities in realizing these applications and in particular helped identify several common features and functionalities they share. These features are ones that any or most healthcare applications will need to achieve effective integration and utilization of services, resources and components in the healthcare system. Therefore, we introduced the SOM framework to provide these services, support integration and facilitate building different healthcare applications.
The next step is to further analyze the requirements for effective Health 4.0 implementation, potential healthcare applications that can be introduced as part of such system. In addition, practical designs and implementations of the different services in the SOM framework are needed to provide the services effectively and efficiently. Ultimately efforts in this direction should come together to create healthcare applications on top of this SOM platform and seamlessly integrate current healthcare applications and systems under the Health 4.0 umbrella and achieve its objectives. There are also some aspects that we did not discuss on in this paper that will need to be closely examined in the context of Health 4.0. The main driver for the success of Health 4.0 is access to data and powerful ubiquitous resources. With this we face several extremely difficult issues like maintaining high levels of security, implementing and enforcing realistic and strong authentication and access control policies, and above all protecting the confidentiality and privacy of everyone involved. On top of all this we also must not forget ethics. Having this powerful system, access to incredibly important and private data, and high levels of control on how things are done raises a huge question mark on the ethics and ethical conduct of those using and managing such systems.
Biographies

Jameela Al-Jaroodi (Member, IEEE) received the Ph.D. degree in computer science from the University of Nebraska-Lincoln, Nebraska, USA, and the M.Ed. degree in higher education management from the University of Pittsburgh, Pittsburgh, PA, USA. She was a Research Assistant Professor with the Stevens Institute of Technology, Hoboken, NJ, USA. She was an Assistant Professor with United Arab Emirates University, United Arab Emirates. She was an Independent Researcher in computer and information technology. She is currently a Professor and a Coordinator of Software Engineering Concentration with the Department of Engineering, Robert Morris University, Moon, PA, USA. Her research interests include middleware, software engineering, security engineering, cyber-physical systems, smart systems, healthcare systems, distributed and cloud computing, UAVs, and wireless sensor networks.

Nader Mohamed (Member, IEEE) received the Ph.D. degree in computer science from the University of Nebraska-Lincoln, Lincoln, NE, USA. He was a Faculty Member with the Stevens Institute of Technology, Hoboken, NJ, USA, and United Arab Emirates University, Al Ain, United Arab Emirates. He has several years of industrial experience in information technology. He is currently a Professor of computer science and information systems with the California University of Pennsylvania, California, PA, USA. His current research interests include cybersecurity, middleware, Industry 4.0, cloud and fog computing, networking, healthcare systems, and cyber-physical systems.

Eman Abukhousa received the Ph.D. degree in information technology from United Arab Emirates University (UAEU). She is an experienced Health Information Technology (HIT) professional with over ten years of experience. She is also an expert in advising strategies for selections and implementations of health IT solutions with focus on achieving demonstrable clinical, operational, and financial benefits. She specializes in data-intensive solutions to support intelligent industries and smart enterprises of the future. She is currently the Department Head of New Media Technology at Modul University Dubai. She had a Postdoctoral Fellowship in the field of predictive analytics. She has played an instrumental role in the successful rollout of digital systems across multiple organizations in the Middle East as United Arab Emirates, Saudi Arabia, Oman, and Egypt. She has published several articles covering a wide range of topics, including data analytics, IT healthcare, smart learning, social and behavioral analysis technologies, industry digitalization, and others.
References
- [1].Kanchanachitra C., Lindelow M., Johnston T., Hanvoravongchai P., Lorenzo F. M., Huong N. L., Wilopo S. A., and Rosa J. F. D., “Human resources for health in southeast Asia: Shortages, distributional challenges, and international trade in health services,” Lancet, vol. 377, no. 9767, pp. 769–781, Feb. 2011. [DOI] [PubMed] [Google Scholar]
- [2].Akay M. and Tamura T., “Global healthcare: Advances and challenges [Scanning the Issue],” Proc. IEEE, vol. 103, no. 2, pp. 147–149, Feb. 2015. [Google Scholar]
- [3].Maphumulo W. T. and Bhengu B. R., “Challenges of quality improvement in the healthcare of South Africa post-apartheid: A critical review,” Curationis, vol. 42, no. 1, pp. 1–9, May 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Brewster A. L., Yuan C. T., Tan A. X., Tangoren C. G., and Curry L. A., “Collaboration in health care and social service networks for older adults,” Medical Care, vol. 57, no. 5, pp. 327–333, 2019. [DOI] [PubMed] [Google Scholar]
- [5].Douglas T. J. and Ryman J. A., “Understanding competitive advantage in the general hospital industry: Evaluating strategic competencies,” Strategic Manage. J., vol. 24, no. 4, pp. 333–347, 2003. [Google Scholar]
- [6].Lasi H., Fettke P., Kemper H. G., Feld T., and Hoffmann M., “Industry 4.0,” Bus. Inf. Syst. Eng., vol. 6, no. 4, pp. 239–242, 2014. [Google Scholar]
- [7].Thuemmler C. and Bai C., Eds., Health 4.0: How Virtualization and Big Data are Revolutionizing Healthcare. New York, NY, USA: Springer, 2017. [Google Scholar]
- [8].Mohamed N. and Al-Jaroodi J., “The impact of industry 4.0 on healthcare system engineering,” in Proc. IEEE Int. Syst. Conf. (SysCon), Apr. 2019, pp. 1–7. [Google Scholar]
- [9].AbuKhousa E., Mohamed N., and Al-Jaroodi J., “Health 4.0: Can healthcare industry get smarter?” in Proc. 13th Int. Symp. Tools Methods Competitive Eng. (TMCE), Dublin, Ireland, 2020. [Google Scholar]
- [10].Khelassi A., Estrela V. V., Monteiro A. C. B., França R. P., Iano Y., and Razmjooy N., “Health 4.0: Applications, management, technologies and review,” Med. Technol. J., vol. 2, no. 4, pp. 262–276, Jan. 2019. [Google Scholar]
- [11].Chanchaichujit J., Tan A., Meng F., and Eaimkhong S., “An introduction to healthcare 4.0,” in Healthcare 4. Singapore: Palgrave Pivot, 2019, pp. 1–15. [Google Scholar]
- [12].Thuemmler C. and Bai C., “Health 4.0: Application of industry 4.0 design principles in future asthma management,” in Health 4.0: How Virtualization Big Data are Revolutionizing Healthcare. Springer, 2017, pp. 23–37. [Google Scholar]
- [13].Dieleman J. L., Templin T., Sadat N., Reidy P., Chapin A., Foreman K., Haakenstad A., Evans T., Murray C. J. L., and Kurowski C., “National spending on health by source for 184 countries between 2013 and 2040,” Lancet, vol. 387, no. 10037, pp. 2521–2535, Jun. 2016. [DOI] [PubMed] [Google Scholar]
- [14].Hermann M., Pentek T., and Otto B., “Design principles for industrie 4.0 scenarios,” in Proc. 49th Hawaii Int. Conf. Syst. Sci. (HICSS), Jan. 2016, pp. 3928–3937. [Google Scholar]
- [15].Sampa M. B., Hoque M. R., Islam R., Nishikitani M., Nakashima N., Yokota F., Kikuchi K., Rahman M. M., Shah F., and Ahmed A., “Redesigning portable health clinic platform as a remote healthcare system to tackle COVID-19 pandemic situation in unreached communities,” Int. J. Environ. Res. Public Health, vol. 17, no. 13, p. 4709, Jun. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Wehde M., “Healthcare 4.0,” IEEE Eng. Manag. Rev., vol. 47, no. 3, pp. 24–28, Dec. 2019. [Google Scholar]
- [17].Jayaraman P. P., Forkan A. R. M., Morshed A., Haghighi P. D., and Kang Y. B., “Healthcare 4.0: A review of frontiers in digital health,” Wiley Interdiscipl. Rev. Data Mining Knowl. Discovery, vol. 10, no. 2, p. e1350, 2020. [Google Scholar]
- [18].Tortorella G. L., Fogliatto F. S., Vergara A. M. C., Vassolo R., and Sawhney R., “Healthcare 4.0: Trends, challenges and research directions,” Prod. Planning Control, vol. 31, no. 15, pp. 1245–1260, 2020. [Google Scholar]
- [19].Islam S. M. R., Kwak D., Kabir M. H., Hossain M., and Kwak K.-S., “The Internet of Things for health care: A comprehensive survey,” IEEE Access, vol. 3, pp. 678–708, 2015. [Google Scholar]
- [20].Cardoso J., Voigt K., and Winkler M., “Service engineering for the Internet of services,” in Proc. Int. Conf. Enterprise Inf. Syst. Berlin, Germany: Springer, 2008, pp. 15–27. [Google Scholar]
- [21].Lee I., Sokolsky O., Chen S., Hatcliff J., Jee E., Kim B., King A., Mullen-Fortino M., Park S., Roederer A., and Venkatasubramanian K. K., “Challenges and research directions in medical cyber–physical systems,” Proc. IEEE, vol. 100, no. 1, pp. 75–90, Jan. 2012. [Google Scholar]
- [22].Hansen J. A. and Hansen N. M., “A taxonomy of vulnerabilities in implantable medical devices,” in Proc. 2nd Annu. Workshop Secur. Privacy Med. Home-Care Syst., 2010, pp. 13–20. [Google Scholar]
- [23].Camara C., Peris-Lopez P., and Tapiador J. E., “Security and privacy issues in implantable medical devices: A comprehensive survey,” J. Biomed. Informat., vol. 55, pp. 272–289, Jun. 2015. [DOI] [PubMed] [Google Scholar]
- [24].AbuKhousa E., Mohamed N., and Al-Jaroodi J., “E-health cloud: Opportunities and challenges,” Future Internet, vol. 4, no. 3, pp. 621–645, Jul. 2012. [Google Scholar]
- [25].Ahmad M., Amin M. B., Hussain S., Kang B. H., Cheong T., and Lee S., “Health fog: A novel framework for health and wellness applications,” J. Supercomput., vol. 72, no. 10, pp. 3677–3695, Oct. 2016. [Google Scholar]
- [26].Raghupathi W. and Raghupathi V., “Big data analytics in healthcare: Promise and potential,” Health Inf. Sci. Syst., vol. 2, no. 1, p. 3, Dec. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].West D. M., “How 5G technology enables the health Internet of Things,” Brookings Center for Technol. Innovation., vol. 3, pp. 1–20, 2016. [Google Scholar]
- [28].de Mattos W. D. and Gondim P. R. L., “M-health solutions using 5G networks and M2M communications,” IT Prof., vol. 18, no. 3, pp. 24–29, May 2016. [Google Scholar]
- [29].Al-Jaroodi J. and Mohamed N., “Blockchain in industries: A survey,” IEEE Access, vol. 7, pp. 36500–36515, 2019. [Google Scholar]
- [30].Mohamed N. and Al-Jaroodi J., “Applying blockchain in industry 4.0 applications,” in Proc. IEEE 9th Annu. Comput. Commun. Workshop Conf. (CCWC), Jan. 2019, pp. 0852–0858. [Google Scholar]
- [31].Chute C. and French T., “Introducing care 4.0: An integrated care paradigm built on industry 4.0 capabilities,” Int. J. Environ. Res. Public Health, vol. 16, no. 12, p. 2247, Jun. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Aceto G., Persico V., and Pescapé A., “Industry 4.0 and health: Internet of Things, big data, and cloud computing for healthcare 4.0,” J. Ind. Inf. Integr., vol. 18, Jun. 2020, Art. no. 100129. [Google Scholar]
- [33].Dubgorn A., Kalinina O., Lyovina A., and Rotar O., “Foundation architecture of telemedicine system services based on health 4.0 concept,” in Proc. SHS Web Conf., vol. 44, 2018, p. 00032. [Google Scholar]
- [34].Sannino G., De Falco I., and Pietro G. D., “A continuous noninvasive arterial pressure (CNAP) approach for health 4.0 systems,” IEEE Trans. Ind. Informat., vol. 15, no. 1, pp. 498–506, Jan. 2019. [Google Scholar]
- [35].Grigoriadis N., Bakirtzis C., Politis C., Danas K., and Thuemmler C., “Health 4.0: The case of multiple sclerosis,” in Proc. IEEE 18th Int. Conf. e-Health Netw., Appl. Services (Healthcom), Sep. 2016, pp. 1–5. [Google Scholar]
- [36].Grigoriadis N., Bakirtzis C., Politis C., Danas K., Thuemmler C., and Lim A. K., “A health 4.0 based approach towards the management of multiple sclerosis,” in Health 4.0: How Virtualization Big Data are Revolutionizing Healthcare. Cham, Switzerland: Springer, 2017, pp. 205–218. [Google Scholar]
- [37].Feussner H., Ostler D., Kranzfelder M., Kohn N., Koller S., Wilhelm D., Thuemmler C., and Schneider A., Surgery 4.0. In Health 4.0: How Virtualization and Big Data are Revolutionizing Healthcare. Cham, Switzerland: Springer, 2017, pp. 91–107. [Google Scholar]
- [38].Kumari A., Tanwar S., Tyagi S., and Kumar N., “Fog computing for healthcare 4.0 environment: Opportunities and challenges,” Comput. Electr. Eng., vol. 72, pp. 1–13, Nov. 2018. [Google Scholar]
- [39].Gupta R., Tanwar S., Tyagi S., and Kumar N., “Tactile-Internet-based telesurgery system for healthcare 4.0: An architecture, research challenges, and future directions,” IEEE Netw., vol. 33, no. 6, pp. 22–29, Nov. 2019. [Google Scholar]
- [40].Mavrogiorgou A., Kiourtis A., Perakis K., Miltiadou D., Pitsios S., and Kyriazis D., “Analyzing data and data sources towards a unified approach for ensuring end-to-end data and data sources quality in healthcare 4.0,” Comput. Methods Programs Biomed., vol. 181, Nov. 2019, Art. no. 104967. [DOI] [PubMed] [Google Scholar]
- [41].Yang G., Pang Z., Deen M. J., Dong M., Zhang Y.-T., Lovell N., and Rahmani A. M., “Homecare robotic systems for healthcare 4.0: Visions and enabling technologies,” IEEE J. Biomed. Health Informat., vol. 24, no. 9, pp. 2535–2549, Sep. 2020. [DOI] [PubMed] [Google Scholar]
- [42].Hathaliya J. J. and Tanwar S., “An exhaustive survey on security and privacy issues in healthcare 4.0,” Comput. Commun., vol. 153, pp. 311–335, Mar. 2020. [Google Scholar]
- [43].Hathaliya J. J., Tanwar S., Tyagi S., and Kumar N., “Securing electronics healthcare records in healthcare 4.0: A biometric-based approach,” Comput. Electr. Eng., vol. 76, pp. 398–410, Jun. 2019. [Google Scholar]
- [44].Tanwar S., Parekh K., and Evans R., “Blockchain-based electronic healthcare record system for healthcare 4.0 applications,” J. Inf. Secur. Appl., vol. 50, Feb. 2020, Art. no. 102407. [Google Scholar]
- [45].Hathaliya J., Sharma P., Tanwar S., and Gupta R., “Blockchain-based remote patient monitoring in healthcare 4.0,” in Proc. IEEE 9th Int. Conf. Adv. Comput. (IACC), Dec. 2019, pp. 87–91. [Google Scholar]
- [46].Gupta R., Tanwar S., Tyagi S., Kumar N., Obaidat M. S., and Sadoun B., “HaBiTs: Blockchain-based telesurgery framework for healthcare 4.0,” in Proc. Int. Conf. Comput., Inf. Telecommun. Syst. (CITS), Aug. 2019, pp. 1–5. [Google Scholar]
- [47].Bhattacharya P., Tanwar S., Bodke U., Tyagi S., and Kumar N., “BinDaaS: Blockchain-based deep-learning as-a-service in healthcare 4.0 applications,” IEEE Trans. Netw. Sci. Eng., early access, Dec. 25, 2020, doi: 10.1109/TNSE.2019.2961932. [DOI]
- [48].Qiu H., Qiu M., Liu M., and Memmi G., “Secure health data sharing for medical cyber-physical systems for the healthcare 4.0,” IEEE J. Biomed. Health Informat., vol. 24, no. 9, pp. 2499–2505, Sep. 2020. [DOI] [PubMed] [Google Scholar]
- [49].Al-Jaroodi J. and Mohamed N., “Service-oriented middleware: A survey,” J. Netw. Comput. Appl., vol. 35, no. 1, pp. 211–220, 2012. [Google Scholar]
- [50].Sprott D. and Wilkes L., “Understanding service-oriented architecture,” The Archit. J., vol. 1, no. 1, pp. 10–17, 2004. [Google Scholar]
- [51].Roy Chowdhury A., Falchuk B., and Misra A., “MediAlly: A provenance-aware remote health monitoring middleware,” in Proc. IEEE Int. Conf. Pervas. Comput. Commun. (PerCom), Mar. 2010, pp. 125–134. [Google Scholar]
- [52].Boulmalf M., Belgana A., Sadiki T., Hussein S., Aouam T., and Harroud H., “A lightweight middleware for an e-health WSN based system using Android technology,” in Proc. Int. Conf. Multimedia Comput. Syst. (ICMCS), May 2012, pp. 551–556. [Google Scholar]
- [53].Carr D., O’Grady M. I., O’Hare G. M., and Collier R., “SIXTH: A middleware for supporting ubiquitous sensing in personal health monitoring,” in Proc. Int. Conf. Wireless Mobile Commun. Healthcare. Berlin, Germany: Springer, 2012, pp. 421–428. [Google Scholar]
- [54].Teles A., Pinheiro D., Gonçalves J., Batista R., Silva F., Pinheiro V., Haeusler E., and Endler M., “Mobilehealthnet: A middleware for mobile social networks in m-health,” in Proc. 3rd Int. Conf. Wireless Mobile Commun. Healthcare (MobiHealth), vol. 12, 2012, pp. 1–8. [Google Scholar]
- [55].Seeger C., Van Laerhoven K., and Buchmann A., “MyHealthAssistant: An event-driven middleware for multiple medical applications on a smartphone-mediated body sensor network,” IEEE J. Biomed. Health Informat., vol. 19, no. 2, pp. 752–760, Mar. 2015. [DOI] [PubMed] [Google Scholar]
- [56].Torres O. H. M. and Ricaurte J. A. B., “Application middleware for management of medical applications based on HL7 standards,” in Proc. Asia–Pacific Conf. Comput. Aided Syst. Eng. (APCASE), Jul. 2015, pp. 19–23. [Google Scholar]
- [57].Lomotey R. K., Nilson J., Mulder K., Wittmeier K., Schachter C., and Deters R., “Mobile medical data synchronization on cloud-powered middleware platform,” IEEE Trans. Services Comput., vol. 9, no. 5, pp. 757–770, Sep. 2016. [Google Scholar]
- [58].Georgi N., Corvol A., and Le Bouquin Jeannes R., “Middleware architecture for health sensors interoperability,” IEEE Access, vol. 6, pp. 26283–26291, 2018. [Google Scholar]
- [59].Bellagente P., Depari A., Ferrari P., Flammini A., Sisinni E., and Rinaldi S., “M3IoT-message-oriented middleware for M-health Internet of Things: Design and validation,” in Proc. IEEE Int. Instrum. Meas. Technol. Conf. (I2MTC), May 2018, pp. 1–6. [Google Scholar]
- [60].Mehedi A., Tokee A. H., Islam S., and Miah M. S. U., “IoT based healthcare middleware,” in Proc. Int. Conf. Comput. Adv., Jan. 2020, pp. 1–4. [Google Scholar]
- [61].Fersi G., “Study of middleware for Internet of healthcare things and their applications,” in The Impact of Digital Technologies on Public Health in Developed and Developing Countries, Jmaiel M., Mokhtari M., Abdulrazak B., Aloulou H., and Kallel S., Eds. (Lecture Notes in Computer Science), vol. 12157. Cham, Switzerland: Springer, 2020. [Google Scholar]
- [62].Avila K., Sanmartin P., Jabba D., and Jimeno M., “Applications based on service-oriented architecture (SOA) in the field of home healthcare,” Sensors, vol. 17, no. 8, p. 1703, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Ahlsén M., Asanin S., Kool P., Rosengren P., and Thestrup J., “Service-oriented middleware architecture for mobile personal health monitoring,” in Proc. Int. Conf. Wireless Mobile Commun. Healthcare. Berlin, Germany: Springer, 2011, pp. 305–312. [Google Scholar]
- [64].Hsieh S.-H., Hsieh S.-L., Cheng P.-H., and Lai F., “E-health and healthcare enterprise information system leveraging service-oriented architecture,” Telemedicine e-Health, vol. 18, no. 3, pp. 205–212, Apr. 2012. [DOI] [PubMed] [Google Scholar]
- [65].Bhandari G. and Snowdon A., “Design of a patient-centric, service-oriented health care navigation system for a local health integration network,” Behav. Inf. Technol., vol. 31, no. 3, pp. 275–285, Mar. 2012. [Google Scholar]
- [66].García-Valls M. and Touahria I., “On line service composition in the integrated clinical environment for eHealth and medical systems,” Sensors, vol. 17, no. 6, p. 1333, Jun. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Li J., “A service-oriented approach to interoperable and secure personal health record systems,” in Proc. IEEE Symp. Service-Oriented Syst. Eng. (SOSE), Apr. 2017, pp. 38–46. [Google Scholar]
- [68].Gamarra M., Zurek Z., Nieto W., Jimeno M., and Sierra D., “A service-oriented architecture for bioinformatics: An application in cell image analysis,” in Proc. World Conf. Inf. Syst. Technol. Cham, Switzerland: Springer, 2017, pp. 724–734. [Google Scholar]
- [69].Bazzani M., Conzon D., Scalera A., Spirito M. A., and Trainito C. I., “Enabling the IoT paradigm in E-health solutions through the VIRTUS middleware,” in Proc. IEEE 11th Int. Conf. Trust, Secur. Privacy Comput. Commun. (TrustCom), Jun. 2012, pp. 1954–1959. [Google Scholar]
- [70].Hein A., Eichelberg M., Nee O., Schulz A., Helmer A., and Lipprandt A., “A service oriented platform for health services and ambient assisted living,” in Proc. Int. Conf. Adv. Inf. Netw. Appl. Workshops (WAINA), May 2009, pp. 531–537. [Google Scholar]
- [71].Busching F., Bottazzi M., and Wolf L., “The GAL monitoring concept for distributed aal platforms,” in Proc. IEEE 14th Int. Conf. e-Health Netw., Appl. Services (Healthcom), Oct. 2012, pp. 466–469. [Google Scholar]
- [72].Wright A. and Sittig D. F., “SANDS: A service-oriented architecture for clinical decision support in a national health information network,” J. Biomed. Informat., vol. 41, no. 6, pp. 962–981, Dec. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Al-Jaroodi J. and Mohamed N., “Middleware is STILL everywhere!!!,” Concurrency Comput. Pract. Exper., vol. 24, no. 16, pp. 1919–1926, Nov. 2012. [Google Scholar]
- [74].Eugster P. T., Felber P. A., Guerraoui R., and Kermarrec A.-M., “The many faces of publish/subscribe,” ACM Comput. Surv., vol. 35, no. 2, pp. 114–131, Jun. 2003. [Google Scholar]
- [75].Tao F., Zhang M., Liu Y., and Nee A. Y. C., “Digital twin driven prognostics and health management for complex equipment,” CIRP Ann., vol. 67, no. 1, pp. 169–172, 2018. [Google Scholar]
- [76].Tao F., Zhang H., Liu A., and Nee A. Y., “Digital twin in industry: State-of-the-art,” IEEE Trans. Ind. Informat., vol. 15, no. 4, pp. 2405–2415, Apr. 2018. [Google Scholar]
- [77].Hasan M. and Goraya M. S., “Fault tolerance in cloud computing environment: A systematic survey,” Comput. Ind., vol. 99, pp. 156–172, Aug. 2018. [Google Scholar]
- [78].Flewwelling C. J., Easty A. C., Vicente K. J., and Cafazzo J. A., “The use of fault reporting of medical equipment to identify latent design flaws,” J. Biomed. Informat., vol. 51, pp. 80–85, Oct. 2014. [DOI] [PubMed] [Google Scholar]
- [79].Mohamed N., Al-Jaroodi J., and Jawhar I., “Towards fault tolerant fog computing for IoT-based smart city applications,” in Proc. IEEE 9th Annu. Comput. Commun. Workshop Conf. (CCWC), Jan. 2019, pp. 0752–0757. [Google Scholar]
- [80].Tang B., Chen Z., Hefferman G., Pei S., Wei T., He H., and Yang Q., “Incorporating intelligence in fog computing for big data analysis in smart cities,” IEEE Trans. Ind. Informat., vol. 13, no. 5, pp. 2140–2150, Oct. 2017. [Google Scholar]
- [81].Al-Jaroodi J. and Mohamed N., “PsCPS: A distributed platform for cloud and fog integrated smart cyber-physical systems,” IEEE Access, vol. 6, pp. 41432–41449, 2018. [Google Scholar]
- [82].Ray A. and Cleaveland R., “Security assurance cases for medical cyber-physical systems,” IEEE Des. Test. Comput., vol. 32, no. 5, pp. 56–65, Oct. 2015. [Google Scholar]
- [83].Mohamed N. and Al-Jaroodi J., “A middleware framework to address security issues in integrated multisystem applications,” in Proc. IEEE Int. Syst. Conf. (SysCon), Apr. 2019, pp. 1–6. [Google Scholar]
- [84].Elmisery A. M., Rho S., and Aborizka M., “A new computing environment for collective privacy protection from constrained healthcare devices to IoT cloud services,” Cluster Comput., vol. 22, no. S1, pp. 1611–1638, Jan. 2019. [Google Scholar]
- [85].Elmisery A. M., Rho S., and Botvich D., “A fog based middleware for automated compliance with OECD privacy principles in Internet of healthcare things,” IEEE Access, vol. 4, pp. 8418–8441, 2016. [Google Scholar]
- [86].Bricon-Souf N. and Newman C. R., “Context awareness in health care: A review,” Int. J. Med. Informat., vol. 76, no. 1, pp. 2–12, Jan. 2007. [DOI] [PubMed] [Google Scholar]
- [87].Viswanathan H., Chen B., and Pompili D., “Research challenges in computation, communication, and context awareness for ubiquitous healthcare,” IEEE Commun. Mag., vol. 50, no. 5, pp. 92–99, May 2012. [Google Scholar]
- [88].Tobon D. P., Falk T. H., and Maier M., “Context awareness in WBANs: A survey on medical and non-medical applications,” IEEE Wireless Commun., vol. 20, no. 4, pp. 30–37, Aug. 2013. [Google Scholar]
- [89].Sain M., Lee H., and Chung W. Y., “Designing context awareness middleware architecture for personal healthcare information system,” in Proc. 12th Int. Conf. Adv. Commun. Technol. (ICACT), vol. 2, Feb. 2010, pp. 1650–1654. [Google Scholar]
- [90].Roy N., Pallapa G., and Das S. K., “A middleware framework for ambiguous context mediation in smart healthcare application,” in Proc. 3rd IEEE Int. Conf. Wireless Mobile Comput., Netw. Commun. (WiMob), Oct. 2007, p. 72. [Google Scholar]
- [91].Pung H., Gu T., Xue W., Palmes P., Zhu J., Ng W., Tang C., and Chung N., “Context-aware middleware for pervasive elderly homecare,” IEEE J. Sel. Areas Commun., vol. 27, no. 4, pp. 510–524, May 2009. [Google Scholar]
- [92].Schot E., Tummers L., and Noordegraaf M., “Working on working together. A systematic review on how healthcare professionals contribute to interprofessional collaboration,” J. Interprofessional Care, vol. 34, no. 3, pp. 332–342, May 2020. [DOI] [PubMed] [Google Scholar]
- [93].Wong E. L.-Y., Yeoh E.-K., and Dong D., “Covid-19: Transforming healthcare will require collaboration and innovative policies,” Brit. Med. J., vol. 369, p. m2229, Jun. 2020. [DOI] [PubMed] [Google Scholar]
- [94].Jaleel A., Mahmood T., Hassan M. A., Bano G., and Khurshid S. K., “Towards medical data interoperability through collaboration of healthcare devices,” IEEE Access, vol. 8, pp. 132302–132319, 2020. [Google Scholar]