Abstract
MR Imaging is regarded as the gold standard for Image Gudied Adaptive Brachytherapy (IGABT) for cervical cancer. However, its wide applicability is limited by its availability, logistics and financial implications. Use of alternative imaging like CT and Ultrasound (US) for IGABT has been attempted. In order to arrive at a systematic, uniform and international approach for CT based definition and contouring of target structures, GEC ESTRO, IBS and ABS agreed to jointly develop such recommendations based on the concepts and terms as published in the ICRU Report 89.
The minimum requirements are clinical examination & documentation, CT or MR imaging at diagnosis and at a minimum, CT imaging with the applicator in place. The recommendations are based on (i) assessment of the GTV at diagnosis and at brachytherapy, (ii) categorizing the response to external radiation into different clinical remission patterns, (iii) defining various clinico-radiological environments and (iv) definition & delineation of a target on CT imaging at the time of brachytherapy with the applicator in situ. CT based target contouring recommendations based on 4 remission categories within 8 defined environments, aim at improving the contouring accuracy for IGABT using CT, US and MRI as available. For each clinico-radiological environment, there is an attempt to minimize the specific uncertainties in order to arrive at the best possible contouring accuracy.
Evaluating feasibility & reproducibility, to achieve a benchmark towards a gold standard MR IGABT and further clinical research including outcomes with CT Based IGABT will become the next steps.
Keywords: Cervical cancer brachytherapy recommendations, Cervical cancer, CT based contouring, IGABT, CT environments
Cervical cancer is the fourth most common cancer among women globally, with an estimated 579,200 new cases and 316,800 deaths worldwide in 2018 [1]. The incidence is higher in low-middle income (LMIC) or low income (LIC) countries settings accounting for 85% of locally advanced cervical cancer worldwide, in which sufficient resources for management, especially radiotherapy facilities, represents a major challenge [2].
Brachytherapy (BT) plays a pivotal role in the curative treatment of cervical cancer. In recent past, three-dimensional image guided adaptive brachytherapy (3D-IGABT) using magnetic resonance imaging (MRI) has evolved and is becoming increasingly wide-spread [3,4]. MRI based target-volume definition and dose optimization has resulted in improved clinical outcomes with reduced toxicities [4–7]. Although, MR imaging is superior in terms of target definition, its wide applicability is limited by its availability, logistics and financial implications. Hence, use of alternative imaging modalities including computerized tomography (CT) and ultrasonography (USG) for BT treatment planning has been explored [8,9].
With wide availability of CT scanners in radiation oncology departments and vast experience with its utilization in external beam radiation (EBRT) planning and treatment, CT is an attractive alternative option for 3D-IGABT planning. Also, various surveys report on CT utilization to be considerably higher than MR for planning of BT in cervical cancers [10–12]. Studies comparing target volume and dimensions on CT with MRI reveal that there is an overestimation of volume and width and an underestimation of height towards the uterus [8,13]. To refine CT based target definition, several attempts have been described using the clinico-radiological findings and anatomy related to the BT applicators [8,13,14]. Therefore, for wider acceptability and dissemination of image based brachytherapy, use of CT imaging becomes essential.
In addition, real-time trans-abdominal ultrasound (TAUS) or trans-rectal ultrasound (TRUS), which are easily accessible, portable and economical, have been utilized to facilitate applicator placement and avoid uterine perforation [15]. TAUS/TRUS during BT have also been used to assist in target definition and treatment planning [16,17].
Recently, CT based contouring guidelines have been reported by American and Japanese colleagues based on consensus guidelines for different clinical situations [18,19]. To overcome the uncertainties associated with the various clinico-radiological environments, recommendations for adapted target definitions and contouring on a CT with applicator in place have been developed. These are based on a uniform target concept [20,21] but take into account the specific uncertainties arising from the various clinic-radiological environments. These recommendations are meant to enable more accurate and homogenous target definition and contouring, reliable and reproducible prescription of dose and reporting of treatment in environments using CT with applicator in place for treatment planning.
Methodology
The need for CT based contouring recommendations for various environments, characterized by the availability of different imaging modalities at diagnosis and BT, were identified and discussed by GEC-ESTRO, IBS and ABS committees.
There was an agreement that such CT based recommendations for target and OAR delineation should use the terms and concepts defined in ICRU 89 based on the GEC-ESTRO recommendations [20,21] which have been clinically validated (RetroEMBRACE, EMBRACE). The gold standard approach for contouring remains clinical examination & documentation, and MRI at diagnosis (MRDG) and at BT (MRBT) with the applicator in place.
The major task was to define recommendations for CT based contouring with the minimum requirement being the availability of CT imaging at the time of BT with the applicator in place and this had to be adapted to and based on the gold standard MR approach. Two experts (Umesh Mahantshetty, Richard Poetter) were asked to set up this adaptation. Therefore, these two experts had to be widely experienced in the complexity of these different scenarios and the development and validation of such concepts. The task was to design a comprehensive systematic recommendation draft with adaptations accounting for the strengths and weaknesses of different clinical and imaging approaches based on broad clinical expert experience and scientific evidence as available. The uncertainties which are typical for specific approaches needed to be outlined and were accounted forin the recommendations. The overall aim was to provide a clinically safe procedure for CT based contouring in order to avoid misunderstandings in settings with limited imaging resources.
As a next step, a qualitative expert validation was carried out on the draft through two online workshops by a limited number of international experts experienced in the development, image based brachytherapy practice and representing different regions of the world. Modifications based on the discussions were integrated into the final recommendations.
The final draft was then reviewed by the committees of the societies involved (Gyn GEC-ESTRO, IBS, ABS). For ESTRO, the ACROP guideline committee approval process and procedures were followed.
Results
GTV assessment and CTV definition
Clinical and various imaging methods give rise to varying uncertainties in assessing and defining the GTV and CTV at diagnosis and at BT. Additionally, uncertainties in target definition and contouring are inherent to the CTV concept, as assumptions about microscopic tumor spread have to be made. These uncertainties are most pronounced in the assessment of the adaptive target (CTV-THR) and are regarded as major for CT, less with US, and least with MRI.
These uncertainties can be reduced to a considerable extent by multi -dimensional (“3D” documentation of the clinical examination and even more, by utilizing a revised scaled clinical diagram. Also, the protocols for various imaging modalities need to be defined appropriately to set the platform to define a target on CT at BT in various environments.
Clinical examination and documentation using a revised scaled clinical diagram and definition of Near Maximum Distance (NMD) for disease extension in each parametrium
There is a general agreement that in the modern imaging era, a thorough gynecologic examination leads to a precise assessment of locally advanced cervical cancer which is in general comparable to the precision of MRI assessment for cervical, parametrial and vaginal disease [4,20,22]. However, the value of gynecologic examination is very much operator dependent, with a major impact being clinical expertise. No robust data on precise estimates of inaccuracies are not readily available for locally advanced cervical cancer (LACC) [23]. All patients need to undergo a thorough bi-manual pelvic examination, including examination under anesthesia if required, and -documentation of the disease findings in all the dimensions (“3D”) using schematic diagrams with representative sagittal, coronal, transverse views (corresponding to volumetric imaging views) and a full speculum view documenting the cervix surface, fornices and the entire vagina. Such clinical drawings, emphasized and adopted in the Gyn GEC ESTRO Recommendations [21], were systematically utilized and validated within the EMBRACE - I study. (www.embracestudy.dk) (Supplementary material I i). These clinical diagrams were revised to include measurement scales in all directions, to show in a reliable and reproducible way, the dimensions of the GTV-Tinit and the GTV-Tres/CTV-THR precisely [24]. Secondly, to provide a straightforward tool for precise BT treatment planning, a new parameter was introduced for width assessment -“Near Maximum Distance” (NMD) which is a measurement of the lateral extension from the cervical canal (os) and needs to be specified for each parametrium (left and right) (Fig. 1 shows in detail the revised clinical diagram with tumor GTV-Tinit, GTV-Tres/CTV-THR dimensions to be documented in height, thickness and width including parametrial disease) [24]. There is a learning curve associated with documentation of NMD’s in clinical practice, especially in patients with large and extensive disease in the vagina.
Fig. 1.
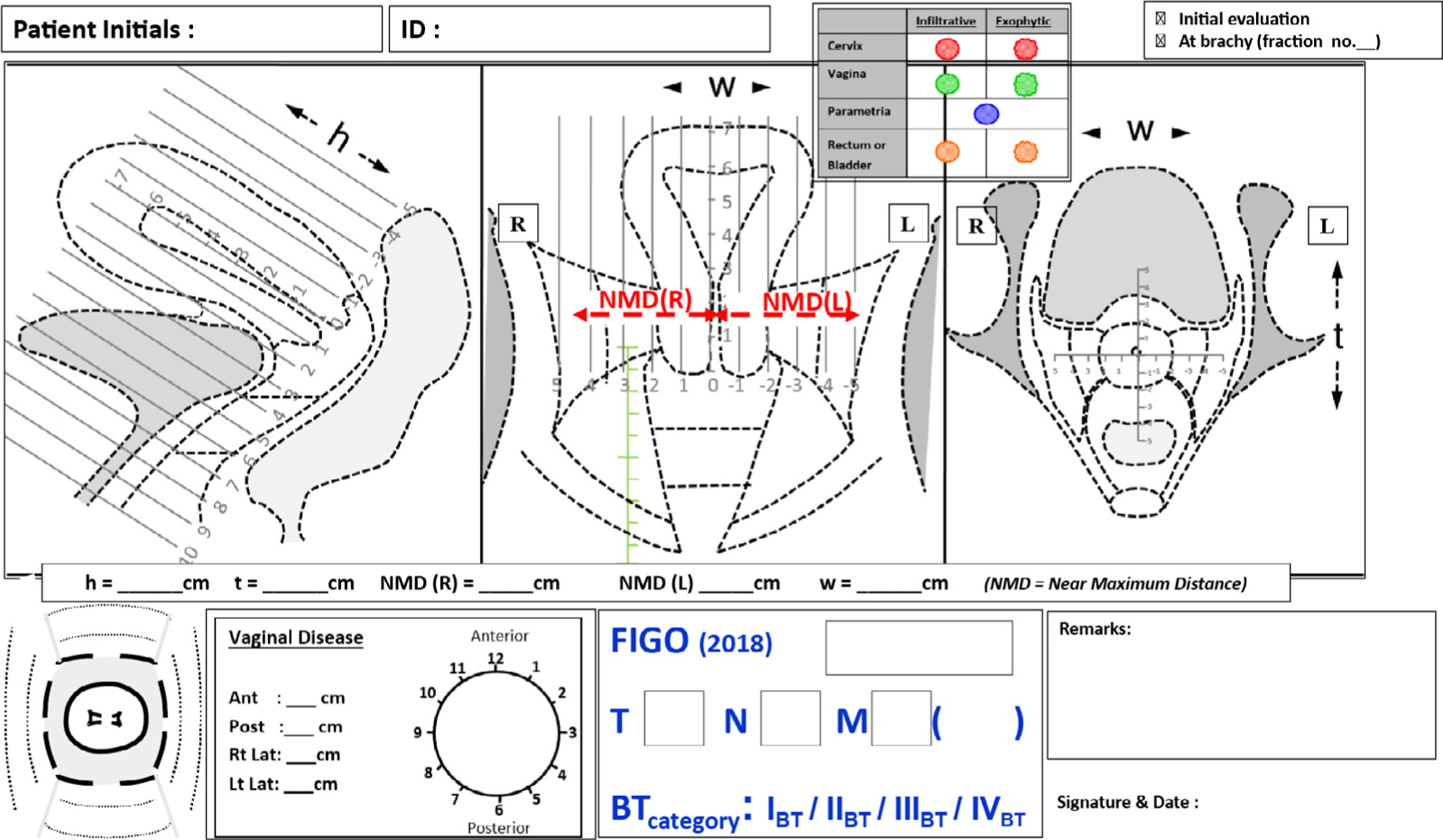
Revised clinical drawing with tumor GTV-Tinit, GTV-Tres/CTV-THR dimensions to be documented in terms of height, thickness and width including parametrial disease, near maximum distance (NMD), FIGO/TNM staging.
The right and left Near Maximum Distance (NMD) enables categorization and documentation of the response on either side of the utero-cervical canal. NMD’s can be defined in relation to the uterine tandem position at the time of BT (see section II). The NMD’s at diagnosis and at BT are therefore important for defining and contouring the CTV-THR in any clinico-radiological environment and to decide on the type of BT application (IC alone/IC + IS) and needle placement to be performed (Supplementary material I - ii).
Volumetric imaging
Major components for IGABT are the precise assessment of the shrinking tumor and the adaptive target volume definition. In the following paragraphs, different volumetric imaging methods are outlined with emphasis on their strengths, weaknesses, and limitations, including the uncertainties related to each imaging method.
MR imaging.
MRI, being the gold standard, is highly accurate for GTV and CTV assessment including the uterine cervix, parametria, uterine corpus, vagina and for organ wall involvement (bladder, rectum) [3]. Imaging accuracy is more pronounced at diagnosis when compared at the time of BT after chemoradiotherapy, due to tumor and tissue alterations induced through chemoradiotherapy This is in particular true for the assessment of the residual GTV (high signal intensity zone on T2) and the “gray zones” on T2 in the parametria in the region of the initial GTV, which are used for the definition of the CTVHR.
Pelvic MRI should be performed with a well-defined protocol including patient position, use of a pelvic coil, introduction of vaginal ultra-sound gel, bladder and rectal filling protocols and appropriate standard sequences as recommended by GEC –ESTRO [3]. During BT, an institutional bladder filling protocol should be defined. This is typically an empty bladder following catheter placement, followed by instillation of a small but consistent volume (20–50 ml) of fluid prior to both MR imaging and HDR treatment delivery (may not be applicable for PDR treatments). A minimum of T1 (as image localizer) and T2 weighted FRFSE non-contrast, axial, sagittal and coronal (para-axial/para-sagittal or para-coronal) sequences with 3–5 mm slice thickness, 0–2 mm spacing and 256 × 256 matrixes using 0.35–3 Tesla MR is preferred (Supplementary material I - iii).
The CTV-THR seems to be quite robust and reproducible whereas there is more inter-observer variation in assessment of the GTV-Tres and CTVIR. In a systematic study, 10 institutions who were actively recruiting patients in the EMBRACE I study participated in a contouring exercise for 6 patients with LACC. Reported volumetric conformity indices (>0.7) and inter – delineation distances (<4 mm) for CTVHR were significantly better as compared to GTV-Tres and CTVIR [22].
CT imaging.
In LACC, CT is not recognized as an appropriate method to assess GTV dimensions due to its limited soft tissue contrast and is clearly inferior to MRI [25]. An exception is disease limited to the cervix (T1b1), where CT assessment leads to comparable results (at diagnosis) to other imaging methods [22]. In addition, there is some expert experience that advanced disease, e.g. infiltration of pelvic wall, can be quite well recognized on CT [26]. Nevertheless, pelvic CT is recognized as an appropriate method to define the outer dimensions of the uterine cervix, corpus, parametria (essential components of target) and rectum, sigmoid and bladder (vagina) as OAR’s [8,18].
The CT Imaging protocol should be standardized. CT imaging has to be performed with 1–1.5 ml/kg body weight iodine based intravenous contrast administration after utilizing a uniform bladder filling protocol for BT as defined in the MR protocol. During the BT application, the bladder is kept nearly empty with an indwelling catheter. At the time of CT Imaging, the bladder is instilled with 20–50 ml fluid (mixture of 1 ml of Sodium-meglumine diatrizoate 76%) contrast and 20–50 ml of normal saline) to achieve adequate contrast for outer wall contouring. A similar protocol using dilute contrast (10–15 ml) may be instilled into the recto-sigmoid, in addition to the rectal tube to assist in delineation of the rectum and sigmoid. CT imaging using < 3 mm slice thickness should be performed, preferably include arterial/capillary phase to best define the pelvic anatomy. The bladder filling and other organ filling protocols during imaging is more applicable to HDR rather than PDR. The pelvic anatomical structures relevant to cervical cancer radiotherapy include, the primary tumor, cervical canal, cervix, vagina, uterine corpus, parametrium, pelvic vessels, uterine arteries, bladder, rectum and sigmoid.
In general CT alone should not be used for GTV assessment in LACC. In addition, uncertainties for target volume contouring are in general much more pronounced for CT compared with MRI and result in relatively larger target volumes [8,13,27].
Due to the significant dose gradients in BT, the impact of contouring uncertainties on dose reporting can be significant and may result in different CTV-T doses when reporting either MRI or CT based target definitions [28].
Trans-abdominal ultrasound (TAUS).
TAUS is a low-cost imaging modality widely available for gynecological evaluation. Its accuracy is comparable to MR imaging in staging of early-stage cervical cancer [25,29]. The advantages of US include good soft tissue contrast and dynamic real time imaging. With US, the outer and inner dimensions of the uterine cervix, corpus and vaginal wall can be defined precisely, but not the parametrium [9,16].
TAUS has been utilized during BT to guide the application and prevent perforations [30]. TAUS has also been used for assisting in defining the target confined to the uterus in image guided brachytherapy [9,16]. With TAUS and limited bladder filling (100–150 ml with normal saline), dimensions are determined at the level of cervix and uterine corpus, which have been used for dose prescription [9,16]. However, no complete volumetric imaging is performed due to sub-optimal evaluation of parametria for a comprehensive target volume definition.
The well-known limitations of TAUS include large interobserver variation, operator dependency, limited reproducibility, expertise and no standardized imaging documentation protocols.
Trans-rectal ultrasonography (TRUS).
TRUS has been used to define a target structure in relation to the cervical canal at the time of BT which corresponds to the target structure on MRI [31–33]. The reason is that the CTV-THR contains structures which appear dark (hypo-echoic) on the ultrasound image: residual GTV, cervical stroma, extra-cervical residual GTV and/or parametrial fibrotic pathologic tissue. Therefore, there is a significant contrast between the normal fatty parametrial tissue (bright) and the adjacent pathologic tissue (dark - hypo-echoic) which allows for defining and contouring the target.
TRUS using biplanar probes and acquisition of images at various levels of the cervical canal in relation to the anatomical structures such as the uterine vessels, external and internal os, and echoes from the involved and uninvolved parametrium, provide useful information to define the target more accurately compared to CT [33,34]. In-room intraoperative ultrasonography with a trans-rectal (5–7.5 MHz) probe can be used to guide and facilitate the application. The TRUS probe is usually covered with a sterile gel inside a plastic sheath and axial images can be acquired transrectally after the placement of the tandem into the utero-cervical canal. Scanning of the cervical region is done to identify the uterine arteries (assisted & confirmed by color doppler). From the level of these uterine vessels, a series of trans-axial images at 1 cm stepwise increments in an inferior direction can be obtained by retracting the TRUS probe sequentially. At least 3 trans-axial images at 1 cm intervals should be acquired to cover the entire cervical region namely, at the level of the crossing of the uterine artery (corresponds to the level of point A), and at 1 cm and 2 cm distal/below (corresponds to the level of external cervical os). On the axial images, the distances between the central canal and the outer margins of hypo-echoic (dark) regions (TRUS based NMD’s) can be utilized to guide the target contouring on the corresponding axial CT images [17,34]. This methodology with the use of TRUS is associated with a learning curve. For the assessment of CTV-THR, TRUS is within the intra-observer variability of MRI and superior to CT with good to excellent image quality [31,32,34].
TRUS combined with CT.
With the advantages of TRUS imaging in terms of evaluating and determining the GTV at diagnosis and the CTV-THR at BT, the information from TRUS can be extrapolated to CT to overcome the shortcomings of CTV contouring on CT alone. Hence it seems logical and straight forward to combine TRUS and CT to define and delineate the CTV-THR more efficiently and accurately and more applicable for 3D treatment planning [34].
The TRUS guided CTV-THR-CT on CT has been explored with different methodologies including adopting the TRUS based NMD’s dimensions on CT at BT. One study suggests that CT based target and OAR delineation utilizing MR at diagnosis and real time TRUS information during BT seems comparable to the gold standard MR based IGABT for cervical cancers [34]. Another study based on rigid co-registration of TRUS and CT Images shows that TRUS-CT substantially reduces the overestimation of the CTV-THR volume of CT alone and is only slightly larger than MRI based CTV-THR volumes [17,33].
Classification of clinical remission at the time of BT for CT based target contouring [35]
For CT based target contouring, it is essential to define at BT the tumor response to radio (chemo) therapy objectively in relation to the primary disease at diagnosis. When using CT as an exclusive imaging modality, the initial GTV and residual GTV at BT delineation is known to be less valid and reliable. Therefore, it is essential to use other modalities for GTV assessment such as clinical examination and ultrasound or MRI. Such assessment of the residual GTV and residual adjacent pathologic tissue should be related to specific relevant anatomical structures and categorized, e.g. as residual GTV with proximal or distal parametrial involvement. These anatomical structures can then be used on CT as reference structures and provide the framework for CTV-THR determination. The relevant tissues and organs for GTV response categorization can, in most cases, be defined on CT with sufficient accuracy: uterine cervix, parametria, vagina, uterine corpus, bladder wall, rectal wall. They can be subdivided according to geometrical and anatomical considerations which have been widely and successfully used in gynaecologic oncology. The residual involvement, as documented through clinical drawings +/− non CT based volumetric imaging (US, MRI), can therefore be delineated on CT in such well-defined parts of these tissues/organs: proximal/distal parametria, upper/mid/lower vagina, proximal/mid/distal uterine corpus. Some reduction of accuracy within such contouring a process is recognized compared to the gold standard MRI based target contouring. The clinical impact of such loss in accuracy is not well known at present (Supplementary material I - iv).
Therefore, such a categorical classification system indicating the spread of disease at diagnosis and at BT should serve as the essential basis for these CT based contouring recommendations. The comprehensive frame of this classification system are well recognized anatomical structures which are straightforward to be identified on CT and on other assessment methods (clinical, MRI, US).
The categorical classification system is is based on the involvement at diagnosis and at BT of the cervix, parametria, vagina, uterine corpus, bladder and rectum as detailed in Table 1.
Table 1.
Definition of four BT target categories according to assessment and restaging taking into account the pattern of residual disease at BT for CT based contouring of the adaptive CTV-THR-CT.
| Category of BT | Cervix | Parametrium | Vagina | Uterine corpus | bladder/rectum |
|---|---|---|---|---|---|
|
| |||||
| IBT | No residual disease | No residual disease | No residual disease | No residual disease | No residual wall/mucosa involvement |
| Or | Or | Or | |||
| Residual disease confined to cervix | Residual disease < 2 cm of upper vagina | Residual disease in proximal third of utero-cervical junction | |||
| IIBT | Significant residual disease | Proximal parametrial disease | Residual disease within upper one third | Residual disease not beyond mid corpus | No residual wall/mucosa involvement |
| IIIBT | Significant residual disease | Distal/upto pelvic wall parametrial disease | Residual disease in mid or lower third | Residual disease into distal corpus/Up to fundus | No residual wall/mucosa involvement |
| IVBT | Any residual disease | Proximal parametrial disease | Residual disease within upper one third | Residual disease not beyond mid corpus | Residual disease involving neighboring organ wall/ mucosa (bladder/ rectum) |
| Distal/upto pelvic wall parametrial disease | Residual disease in mid or lower third | Residual disease into distal corpus/Up to fundus | Residual disease involving neighboring organ wall/ mucosa (bladder/ rectum) | ||
Table 1 shows this categorization of patients depending on response and residual disease topography at the time of BT. Based on the spectrum of tumor response for any given anatomical structure of interest, a total of four distinct categories for CTV-THR definition at BT are outlined: IBT, IIBT, IIIBT, IVBT. These categories are analogous (not identical) to tumor staging at diagnosis and relevant for BT treatment planning. For each category, the width (NMDR/NMDL), the thickness and the height for the CTV-THR at the time of BT can then be defined efficiently, taking into account the different clinico-radiological environments and disease extensions both at diagnosis and at BT in the sub-structures which account for target volume definition and delineation (section III and IV). Some principles and further explanation for various categories is as shown in Supplementary material I – v.
Defining different clinico-radiological environments
The different clinico-radiological environments depend on the available imaging modalities which can be utilized at diagnosis and at BT. We suggest classifying these environments into four major categories. Each category can then be divided into 2 sub-categories - with or without real time TRUS - depending on the use of real time TRUS during BT application.
The minimum requirements for each category are
Clinical examination and documentation of disease findings including NMD’s at diagnosis and at BT using scaled schematic diagrams (I.1)
CT imaging at the time of BT with the applicator in place (I.2b).
The CT imaging at BT with the applicator in place serves as a volumetric imaging data set for targets and OARs contouring and BT treatment planning, aiming to arrive at a set of valid and reliable dose volume and dose point parameters.
Definition and delineation of target and OAR’s in different clinico-radiological environments
The GEC ESTRO/ICRU 89 recommendations for target definition follow the adaptive target concept which is based on MR Imaging and incorporation of the clinical and imaging findings at diagnosis and at BT [20].
The following recommendations for CT based contouring are adaptations based on the gold standard approach of MRI, clinical examination and account for the specific uncertainties for the various scenarios with the different imaging modalities available.
Definition of targets
Accurate identification of a primary tumor GTV-Tinit or residual GTV (GTV-Tresi) after external radiation, is in most cases, not possible for the CTBT environment. Hence, delineation of the GTV-Tresi based on CT findings only, is not recommended.
The high risk CTV at BT (CTV-THR) - consisting of the entire cervix, and presumed extra-cervical extensions in the regions of the parametrium, uterus and vagina - can be defined based on the classification of clinical remission (Table 1) and the use of defined anatomical structures and their subdivisions which are taken as a framework for CT based contouring (section II). Comprehensive information from clinical drawing documentation including NMD’s and vaginal extension is mandatory for defining the CTV-THR-CT in a CTDG – CTBT environment. The least uncertainty can be assumed if only the cervix has to be delineated as the CTV-THR-CT. Depending on other imaging modalities available (MRIDG, Pre-BT MRI, TRUS), uncertainties for CTV-THR contouring become less pronounced for assessing extra-cervical disease extensions of the CTVHR-CT.
The intermediate risk CTV may be generated with safety margins on the high risk CTV in various directions depending on the disease at diagnosis and should always be in line with the GEC ESTRO/ICRU 89 recommendations.
In summary, GTV delineation at BT on CT imaging is not recommended. However, GTV-Tresi-CT maybe defined on CT in (i) small residual tumors confined to the cervix if there is valid and reliable information from clinical examination and (ii) if Pre - BT MR (performed without BT applicator in place) information can be systematically adopted onto the CT at BT with the help of various anatomical landmarks. Fusion of various imaging sets is not recommended. The CTV-THR-CT can be defined on CT based on clinical documentation, clinical remission pattern and information from other imaging modalities as available.
Delineation of targets
The overall aim is to provide a clinically safe methodology for CT based contouring. Therefore, a systematic set of recommendations for width, height and thickness assessment of the CTV-THR-CT for the different environments is summarized and detailed in Tables 2–5, taking into account the uncertainties associated with the imaging methods available as outlined before (section I).
Table 2.
Width, Height and Thickness details for defining and delineating four categories of CTV-THR-CT based on CT at diagnosis and CT at BT (CTDG – CTBT Environment).
| Category of BT | Width | Height |
Thickness |
||
|---|---|---|---|---|---|
| Lateral | Superior | Inferior | Anterior | Posterior | |
|
| |||||
| IBT | Lateral boundaries of cervix | Lower two thirds of utero-cervical dimensions | Lower extent of cervical lip with vaginal applicator as surrogate | Outer surface of the cervix &/or uterus | Outer surface of the cervix &/or uterus |
| IIBT | Proximal parametrium defined by clinical and TRUS (if available) based NMD’s | Include appropriate length of vaginal wall defined by clinical examination and with/without guidance of markers implanted, maybe with safety margins, few mm longitudinal and up to 2 cm circumferential | To utilize TRUS based distances (if available) | To utilize TRUS based distances (if available) | |
| Additional 3–5 mm margins especially if the corresponding region of parametrium was involved at diagnosis | |||||
| IIIBT | Distal parametrium/upto lateral pelvic wall defined by clinical and TRUS based NMD’s | ||||
| Additional 3–5 mm margins especially if the corresponding region of parametrium was involved at diagnosis | |||||
| IVBT | Proximal /distal parametrium/upto lateral pelvic wall defined by clinical and TRUS based (if available) | In addition to outer surface of the cervix &/or uterus to include the bladder wall/mucosae involved with 2 cm margins at least. | In addition to outer surface of the cervix &/or uterus to include the rectal wall/mucosae involved with 2 cm margins at least. | ||
| NMD’s Additional 3–5 mm margins especially if the corresponding region of parametrium was involved at diagnosis | |||||
| To utilize TRUS based distances (if available) | To utilize TRUS based distances (if available) | ||||
Table 5.
Width, Height and Thickness details for defining and delineating four categories of CTV-THR-CT based on MR at diagnosis & Pre BT MR and CT at BT (MRIDG - Pre BT MRI and CTBT Environment).
| Cat of BT | Width | Height |
Thickness |
||
|---|---|---|---|---|---|
| Lateral | Superior | Inferior | Anterior | Posterior | |
|
| |||||
| IBT | Lateral boundaries of cervix | To review upper extent of disease on MR at diagnosis and Pre BT MR with respect to landmark anatomical structures eg. Uterine arteries, isthmus, distances from the surface of fundus etc. and extrapolate on CT at BT* * may not be applicable in enlarged uterine cavity due to fluid collection. |
Lower extent of cervical lip with vaginal applicator as surrogate | Outer surface of the cervix &/or uterus guided by Pre BT MR dimensions | Outer surface of the cervix &/or uterus guided by Pre BT MR dimensions |
| IIBT | Proximal parametrium defined by clinical/TRUS based NMD’s (if available) and guided by NMD’s on Pre-BT MR including gray zones | Review Pre-BT MR and include appropriate length of vaginal wall defined by clinical examination, with /without guidance of markers implanted and the Pre BT MR findings, with few mm safety margins longitudinal and circumferential. | |||
| To utilize TRUS based distances (if available) | To utilize TRUS based distances (if available) | ||||
| IIIBT | Distal parametrium defined by clinical/TRUS based NMD’s (if available) and guided by NMD’s on Pre-BT MR including gray zones | ||||
| IVBT | Proximal /distal parametrium/Up to lateral pelvic wall defined by clinical/TRUS based NMD’s (if available) and guided by NMD’s on Pre-BT MR including gray zones | In addition to outer surface of the cervix &/or uterus to include the bladder wall/mucosae involved with 2 cm margins at least guided by Pre BT MR findings To utilize TRUS based distances (if available) |
In addition to outer surface of the cervix &/or uterus to include the rectal wall/mucosae involved with 2 cm margins at least guided by Pre BT MR findings | ||
| To utilize TRUS based distances (if available) | |||||
1. Width:
The delineation of the width of the CTV-THR-CT on CT is the most challenging step. Width assessment is based on documentation of clinical remission patterns - especially for parametrial disease. The delineation is performed with the NMD’s (NMDR & NMDL) at diagnosis and at BT (in mm) within the various clinico-radiological environments on CT at BT.
CTDG - CTBT environment: (Table 2, Fig. 2)
Fig. 2.
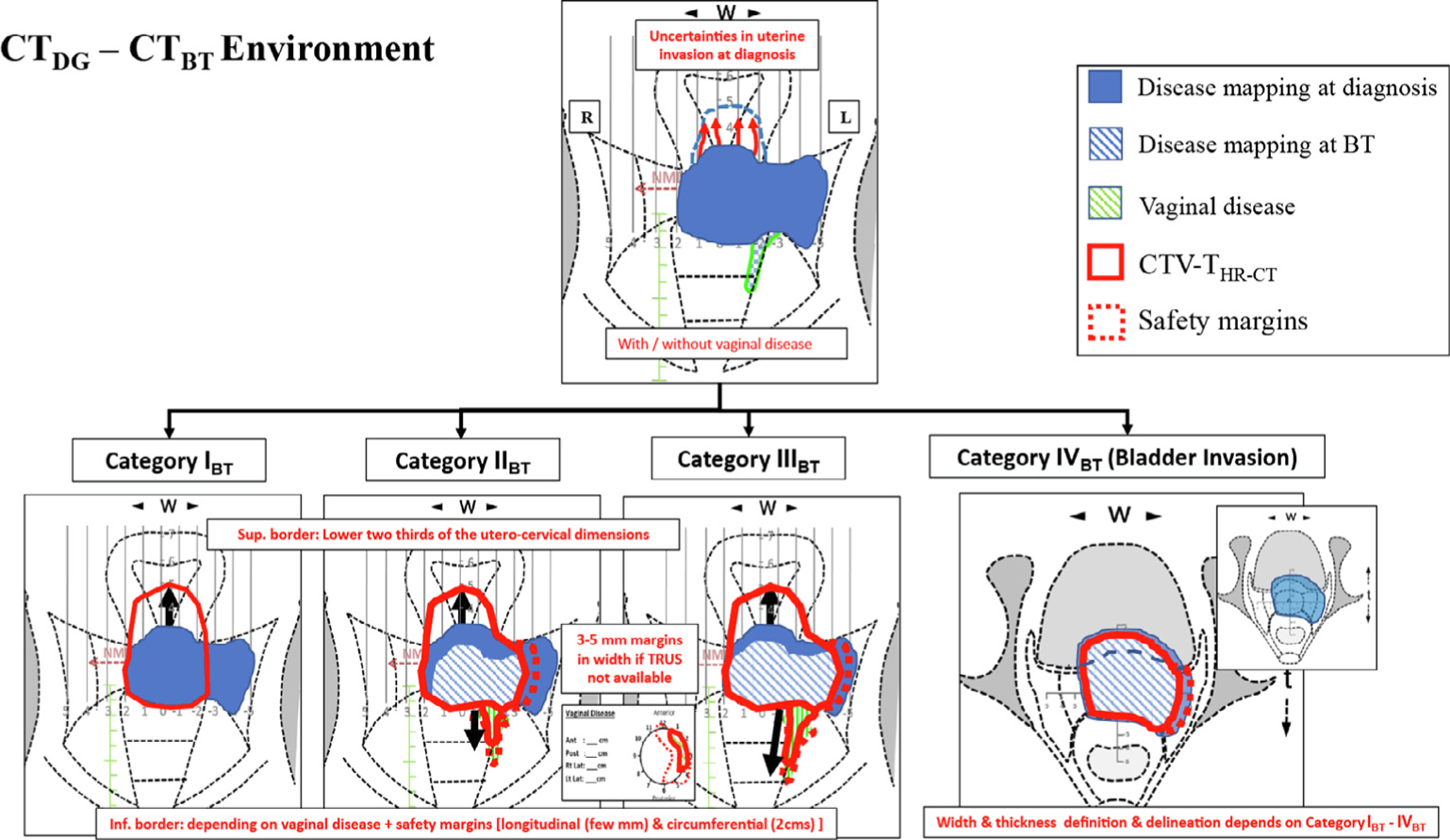
Schematic diagram showing definition of CTV- THR-CT for CTDG – CTBT Environment based on the disease at diagnosis (cervix and parametrium in blue fill & vaginal disease in green lines), residual disease at BT (blue oblique lines), CTV-THR (in red continuous lines) and safety margins (red dotted lines).
- CT only: The magnitude of uncertainty in delineation of the CTV-THR-CT width is large. These uncertainties can be reduced with the use of clinical NMD’s at diagnosis and at BT, with grouping of clinical remission patterns according to the parametrial residual pathological tissues using anatomical landmarks as reference structures (including lateral parametrial attachment, uterine vessels, etc.) on CT imaging with intravenous contrast.
Category I: In the group with no residual disease or residual disease confined to the cervix, the clinical outline of the cervix in the lateral direction, irrespective of abnormalities seen on CT imaging, should be delineated as the width.
Category II-IVBT: In the group with residual disease at the cervix and involvement of the parametrium, the NMD’s left and right at the time of BT become vital for definition of the width of the target in addition to the clinical findings of residual parametrial pathology as proximal or distal or lateral pelvic wall. The delineation may be generous and include additional margins of 3–5 mm to account for uncertainties, especially if the corresponding region of the parametrium was involved at diagnosis.
- Real time TRUS during BT application and CT: Apart from the above criteria, the configuration of the CTV-THR-CT and its lateral dimensions in relation to the central tandem (analog clinical NMD́s) can be depicted more precisely on TRUS imaging (TRUS NMD’s). This information can be used to delineate the width more accurately as compared to CT alone [34].
MRDG – CTBT environment: (Table 3, Fig. 3)
Table 3.
Width, Height and Thickness details for defining and delineating four categories of CTV-THR-CT based on MR at diagnosis and CT at brachytherapy (MRDG – CTBT Environment).
| Category of BT | Width | Height |
Thickness |
||
|---|---|---|---|---|---|
| Lateral | Superior | Inferior | Anterior | Posterior | |
|
| |||||
| IBT | Lateral boundaries of cervix | Lower extent of cervical lip with vaginal applicator as surrogate | |||
| IIBT | Proximal parametrium defined by clinical and TRUS based (if available) NMD’s | Maximum height of disease extent seen on MR at diagnosis. | Include appropriate length of vaginal wall defined by clinical examination and with /without guidance of markers implanted, maybe with safety margins, few mm longitudinal and circumferential | Outer surface of the cervix &/or uterus. | Outer surface of the cervix &/or uterus. |
| Width should not exceed the parametrial disease on MR at diagnosis | Guided by the upper extent of disease seen on MR at diagnosis. Distances from the outer surface of fundus to upper extent of disease to be utilized* * may not be applicable in enlarged uterine cavity due to fluid collection |
To utilize TRUS based distances (if available) | To utilize TRUS based distances (if available) | ||
| IIIBT | Distal parametrium/ upto lateral pelvic wall defined by clinical and TRUS based (if available) NMD’s | Length and circumference of vagina should not exceed vaginal disease on MR at diagnosis | |||
| Width should not exceed the parametrial disease on MR at diagnosis | |||||
| IVBT | Proximal /distal parametrium/Up to lateral pelvic wall defined by clinical and TRUS based (if available) NMD’s | In addition to outer surface of the cervix &/or uterus to include the bladder wall/mucosae involved with 2 cm margins at least. | In addition to Outer surface of the cervix &/or uterus to include the rectal wall/mucosae involved with 2 cm margins at least. | ||
| Width should not exceed the parametrial disease on MR at diagnosis | To utilize TRUS based distances (if available) | To utilize TRUS based distances (if available) | |||
Fig. 3.
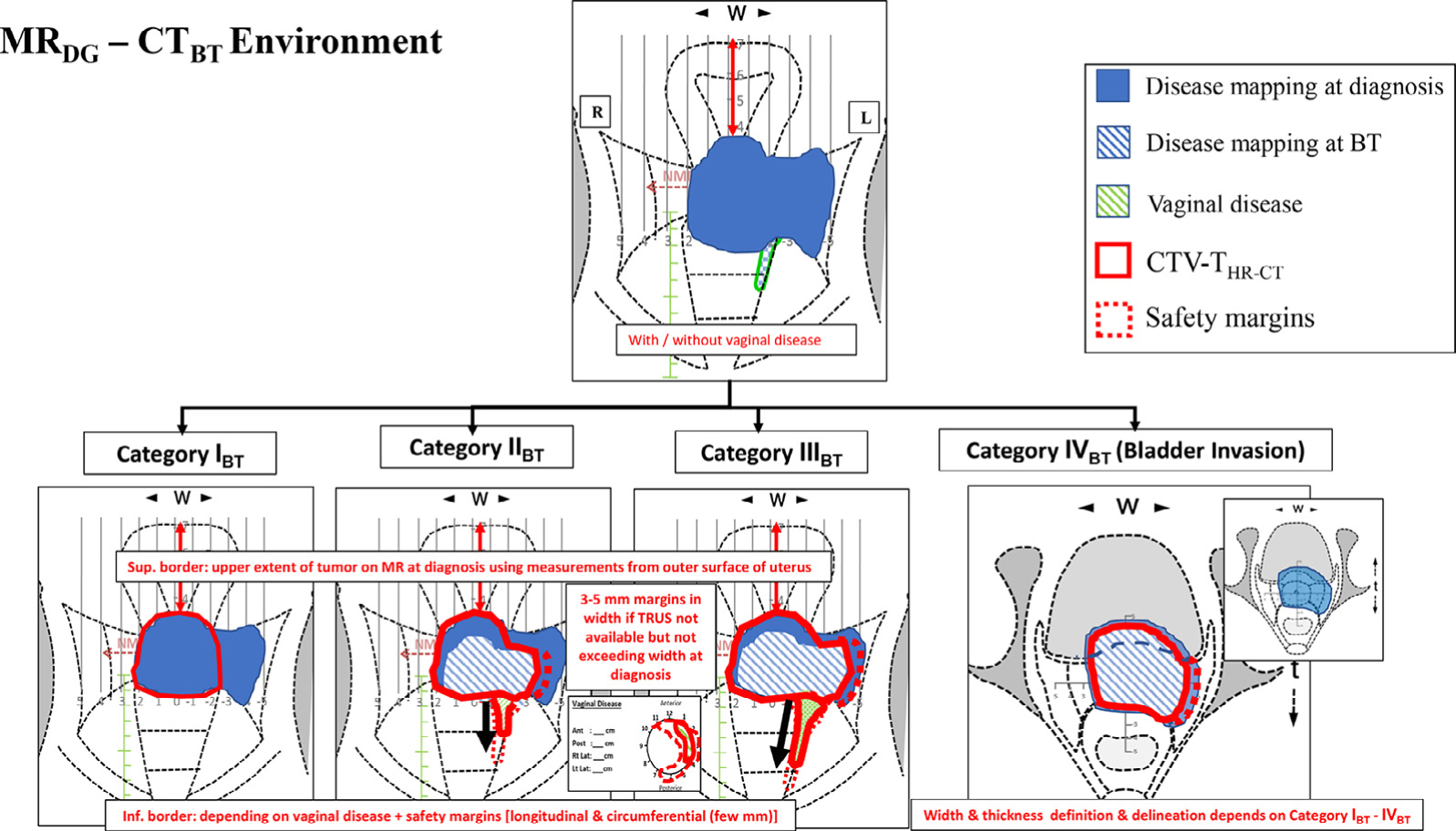
Schematic diagram showing definition of CTV- THR-CT for MRDG – CTBT Environment based on the disease at diagnosis (cervix and parametrium in blue fill & vaginal disease in green lines), residual disease at BT (blue oblique lines), CTV-THR (in red continuous lines) and safety margins (red dotted lines).
For this environment, apart from the details described in the CTDG - CTBT environment, the width of the CTV-THR is delineated taking into account the additional findings from the MRDG. The uncertainties are less as compared to the CTDG – CTBT approach with the width/NMD’s at CTBT not to exceed MRDG dimensions. Delineation of the CTV-THR-CT width should be accurate and should usually not include additional margins to account for uncertainties.
- CTBT only: Clinical NMD’s at diagnosis (including the MR findings) and at BT, grouping of clinical remission patterns using anatomical landmarks as reference structures on CT imaging with intravenous contrast, are used.
- Real time TRUS during BT application and CTBT: The configuration of the CTV-THR-CT and its lateral dimensions in relation to the central tandem can be depicted more precisely on TRUS imaging (TRUS NMD’s). This information leads to a more accurate width delineation. The accuracy of this approach is comparable to the MR IGABT gold standard approach [34].
CTDG- Pre BT MR/CTBT environment: (Table 4, Fig. 4)
Table 4.
Width, Height and Thickness details for defining and delineating four categories of CTV-THR-CT based on CT at diagnosis & Pre BT MR and CT at BT (CT - Pre BT MRI and CTBT Environment).
| Category of BT | Width | Height |
Thickness |
||
|---|---|---|---|---|---|
| Lateral | Superior | Inferior | Anterior | Posterior | |
|
| |||||
| IBT | Lateral boundaries of cervix | Lower extent of cervical lip with vaginal applicator as surrogate | Outer surface of the cervix &/or uterus guided by Pre BT MR dimensions | Outer surface of the cervix &/or uterus guided by Pre BT MR dimensions | |
| IIBT | Proximal parametrium defined by clinical/TRUS based NMD’s (if available) and guided by NMD’s on Pre-BT MR | Lower two thirds of utero-cervical dimensions | Include appropriate length of vaginal wall defined by clinical examination and with /without guidance of markers implanted and the Pre BT MR findings with few mm longitudinal and upto 2 cm circumferential safety margins | ||
| To utilize TRUS based distances (if available) | To utilize TRUS based distances (if available) | ||||
| IIIBT | Distal parametrium defined by clinical/TRUS based NMD’s (if available) and guided by NMD’s on Pre-BT MR$ | ||||
| IVBT | Proximal /distal parametrium/Up to lateral pelvic wall defined by clinical/TRUS based NMD’s (if available) and guided by NMD’s on Pre-BT MR. | Length and circumference of vagina should not exceed vaginal disease at diagnosis | In addition to outer surface of the cervix &/or uterus to include the bladder wall/mucosae involved with 2 cm margins at least guided by Pre BT MR findings To utilize TRUS based distances (if available) |
In addition to outer surface of the cervix &/or uterus to include the rectal wall/mucosae involved with 2 cm margins at least guided by Pre BT MR findings To utilize TRUS based distances (if available) |
|
Fig. 4.
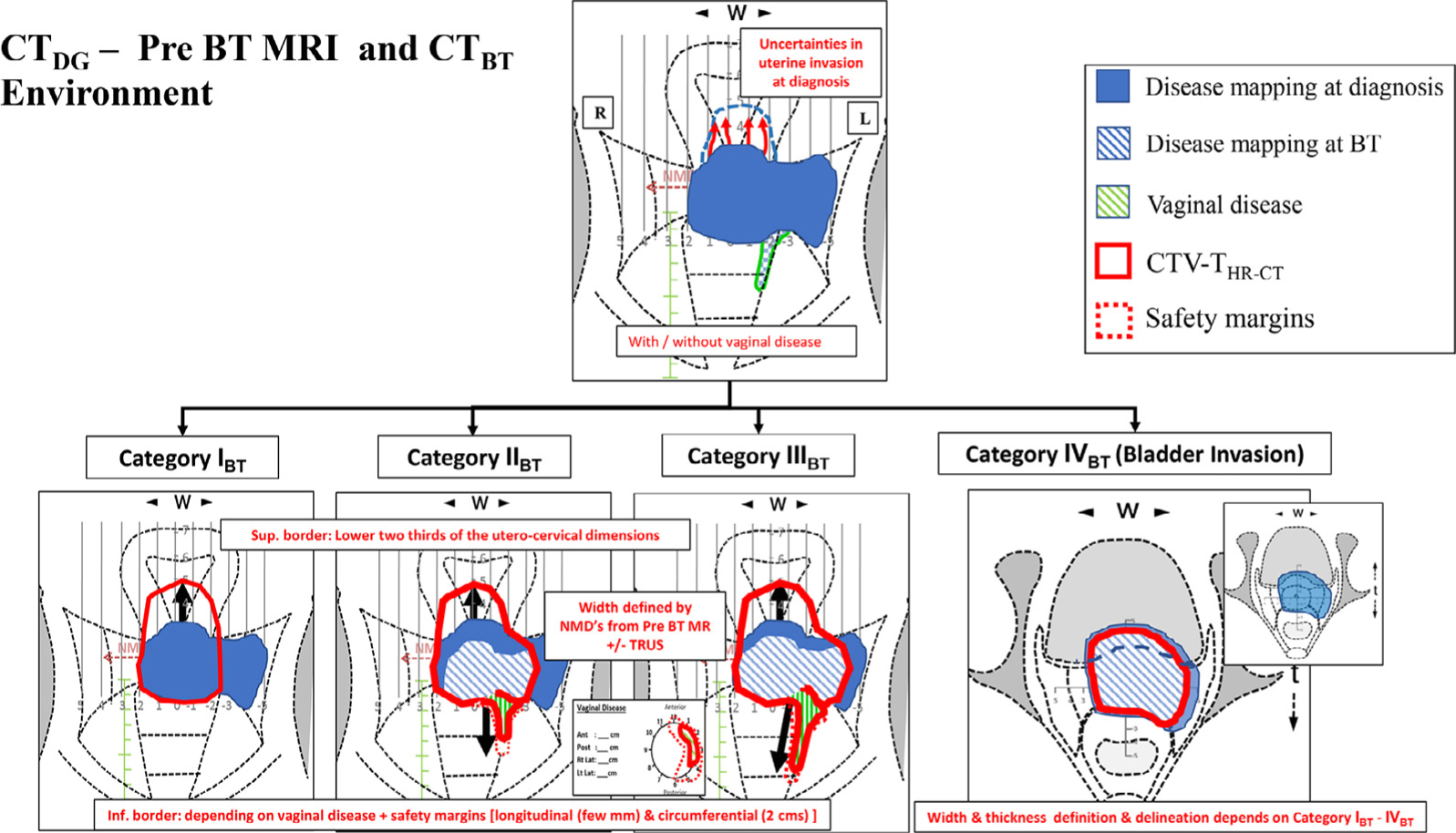
Schematic diagram showing definition of CTV- THR-CT for CTDG – Pre BT MRI and CTBT Environment. Based on the disease at diagnosis (cervix and parametrium in blue fill & vaginal disease in green lines), residual disease at BT (blue oblique lines), CTV-THR (in red continuous lines) and safety margins (red dotted lines).
This environment is similar to the MRDG - Pre BT MR and CTBT environment approach using clinical findings at diagnosis and MR findings done within a few days prior to the BT application (within 1 week). The MR findings of residual cervical tumor, residual or resolving pathological tissues in the parametrium (gray zones), vagina and corpus are systematically adopted onto the CT Imaging with the applicator in place to delineate the CTV-THR-CT.
- Pre BT MRI & CTBT Only: Clinical NMD’s at diagnosis and pre BT MR, response grouping and extrapolating the MR findings at BT with respect to anatomical landmarks onto CT imaging with intravenous contrast.
- Real time TRUS during BT application and CTBT: Apart from the above criteria, the dimensions on TRUS imaging is utilized to define the configuration of the CTV-THR-CT and the NMD’s more accurately.
MRDG - Pre BT MR/CTBT environment: (Table 5, Fig. 5)
Fig. 5.
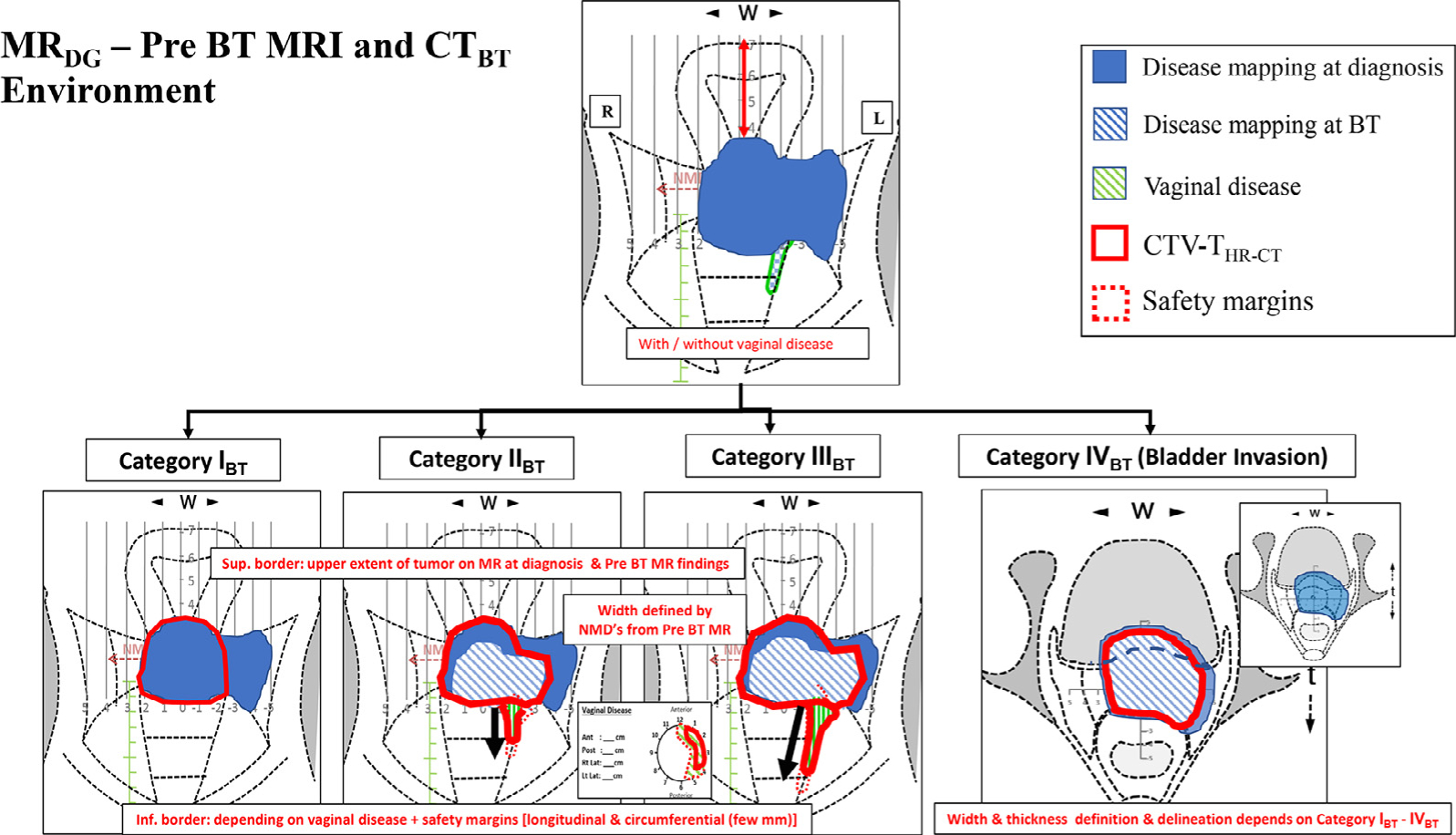
Schematic diagram showing definition of CTV- THR-CT for MRDG – Pre BT MRI and CTBT Environment based on the disease at diagnosis (cervix and parametrium in blue fill & vaginal disease in green lines), residual disease at BT (blue oblique lines), CTV-THR (in red continuous lines) and safety margins (red dotted lines).
This environment is similar to the gold standard approach using clinical and MR findings at diagnosis and at BT. The only difference is that the MRI for BT is done within few days prior to the BT application (within 1 week) and the MR findings of residual cervical tumor, residual or resolving pathological tissues in the parametrium (gray zones), vagina and corpus are systematically adopted onto the CT Imaging with the applicator in place to delineate the CTV-HRCT. This environment is also applicable for MR at diagnosis with MR at first BT and CT in subsequent fractions.
- CT only: Clinical NMD’s and MR at diagnosis and pre BT, response grouping and extrapolating MR findings at BT with respect to anatomical landmarks onto CT imaging with contrast.
- Real time TRUS during BT application and CTBT: Apart from the above criteria, the dimensions on TRUS imaging is utilized to define the configuration of the CTV-THR-CT and the NMD’s more accurate. The accuracy of this approach becomes comparable to the gold standard approach [17,34].
2. Height:
The inferior and superior margins are guided by the vaginal disease and uterine corpus invasion at diagnosis and at BT and the various imaging environments utilized
2.1. Inferior
- No vaginal involvement: vaginal applicator as surrogate [8].
- Vaginal involvement: Irrespective of various imaging environments, the delineation of the inferior extent in the presence of residual vaginal disease (upper, upper + mid, lower third) is straightforward. It should be guided by accurate examination and clinical documentation of vaginal & para-vaginal disease as detailed in the clinical drawings (Fig. 1). In addition, the inferior extent of the residual disease can be identified and delineated with the help of radio-opaque (CT/MR) markers placed during the BT application. Further to the remission classification (upper, upper + mid, lower third), in order to account for uncertainties, additional margins may be given of a few millimeters in inferior extent for all environments and up to 2 cm in circumferential extent for environments with CT at diagnosis. However, the length and circumference of vagina should not exceed the vaginal disease at diagnosis.
During BT planning, the uncertainties can be reduced further by careful attention to the vaginal loading during planning so that the immediate para-vaginal tissues in the upper 1.5 – 2 cm of vagina receive significant doses during the tandem-ovoid or tandem-ring intracavitary BT planning.
2.2. Superior
The assessment and definition of uterine corpus disease at diagnosis and residual pathological tissue at BT enables definition of the superior extent of the target and varies with different radiological environments and degree of uncertainties with larger margins in CTDG – CTBT and smaller for Pre BT MR – CTBT environments. Accurate assessment of the superior margins is not possible in CTDG – CTBT environment only, but becomes more accurate, if there is an MRI component in the environment. For CTDG – CTBT environment only, the lower two thirds of the overall cervico-uterine length should be taken as the minimum length for defining the length of the CTV-THR-CT [13]. For the Pre BT MR – CT environment, if the residual GTV is only within the cervix, a margin of 5–10 mm beyond the internal cervical os as the superior margin for CTV-THR-CT is defined.
- CTDG – CTBT : Lower two thirds of the utero-cervical dimensions [13].
- MRDG - CTBT : Upper extent of disease at diagnosis as the upper limit of the CTV-THR-CT.
- - CTDG – Pre BT MR and CTBT: Lower two thirds of the utero-cervical dimensions [13]
- MRDG – Pre BT MR and CTBT: To extrapolate the height from Pre BT MR to define the upper limit of the CTV-THR-CT.
In patients with residual disease in the parametrium, the superior extent of the CTV-THR-CT can be defined approximately 3–5 mm superior to the level of the uterine arteries.
During planning and optimization, a reduction in the tandem loading from the tandem tip end should be avoided in CT - CT environments and cautious in environments with only one MRI component, at diagnosis or at BT, to avoid underdosing poorly visualized residual uterine disease.
3. Thickness
The anterior and posterior margins of the CTV-THR essentially include the outer surface of the cervix in patients with no bladder or rectal wall/mucosa involvement. These surfaces anterior to the rectum and posterior to the bladder walls, respectively, are relatively easy to depict on CT imaging and are even more pronounced with the defined CT protocol for bladder and/or rectal contrast described in detail earlier.
Use of TRUS information at the time of BT to define the dimensions relative to the central tandem in the anterior and posterior directions, may assist further to refine the thickness of the CTV-THR-CT. However, there is a tendency for deformation and a decrease inthe measured thickness due to compression by placement of the TRUS probe. Any residual pathological tissue assessment and definition in rectal/bladder interfaces may assist further to define the thickness of the target, including (outer/inner) rectal/bladder wall infiltration if present. Depending on the imaging environment, the wall/mucosa of the involved organ with atleast 2 cm margins should be included in the target.
In summary, the definition of width and height of the CTV-THR-CT on CT imaging is a challenge and accounts for major uncertainties and inter-observer variations. However, these can be minimized in various clinic-radiological environments with objective evaluation, clinical documentation with revised clinical drawings, clinical remission patterns and various imaging findings. These are associated with a learning curve and various groups have reported its feasibility in different environments described above [13,17,34]. Also, during BT planning and plan evaluation, the high dose regions and prescription isodose may be conservative without a major compromise in the OAR doses.*
* synopsis for CT based contouring recommendations recipe for each environment has been summarized in Supplementary material II.
Organs-at-risk
For the OAR’s in gynecologic brachytherapy with hollow organs, the organ walls are the essential structures which need to be defined and contoured. For CT based OAR contouring, defined protocols for the depiction of the organ wall (eg contrast medium) and a reproducible organ filling status (preferably empty: rectosigmoid, bladder) are vital to minimize uncertainties. (as described in Section I).
The main OAR’s for routine CT based delineation include the rectum, bladder, sigmoid, bowel, while others like the anal canal, vagina, urethra are recommended only when target volume and dose distribution are in close proximity. The definition of OAR’s follows the anatomical boundaries and principles as detailed in ICRU 89 [20,33].
The ICRU bladder and rectal (now recto-vaginal) reference points in relation to the intracavitary brachytherapy application have to be reported irrespective of the imaging environments for BT planning, as they correlate with urinary, eg incontinence [36] and rectal eg. proctitis, fistula toxicities [37]. The recto-vaginal reference point as defined on radiographs or on volumetric images correlates with vaginal stenosis/shortening [38]. Additionally, other vaginal reference points suggested in ICRU 89 report have to be defined for the upper vagina (5 mm lateral from the applicator surface, ABS guidelines) and for the lower part of the vagina on radiographs or on volumetric images related to the level at the Posterior-Inferior Border of the Symphysis (PIBS and PIBS +/−2) [39,40].
For OAR’ volumes, in general, the organ walls have to be defined and delineated slice by slice on CT images. However, small wall thickness (in the range of millimeters), may cause substantial intra- and inter-observer variations. Such variations can result in significant uncertainties. Therefore, outer-wall contouring using only one line is recommended (ICRU 89) [20].
The assessment of small OAR volumes for brachytherapy planning and reporting (0.1 cm3 and 2 cm3) is applicable as recommended in ICRU 89/GEC-ESTRO Recommendations II [20,33]. For the rectum, a length of about 5 cm in the cranio-caudal direction or longer related to the vaginal sources needs to be delineated. The sigmoid colon, with specific focus on the areas adjacent to the uterus and target, should be clearly identified and contoured. Similarly, bowel loops have to be identified and areas (i.e., wall or organ volumes) near the uterus need to be contoured with their entire circumference. For the bladder, the entire bladder including the whole posterior, posterior-caudal (trigone), and posterior-cranial bladder wall should be delineated. For most of these parameters, in particular for the 2 cm3 volume, a strong correlation has been demonstrated to clinical morbidity endpoints (eg cystitis, proctitis, fistula, vaginal stenosis, diarrhea [36–41].
Discussion and future considerations
The recommendations on definition and delineation of the High risk CTV on CT at BT are based on clinical experience and published evidence on the value of commonly available imaging modalities, including clinical drawing documentation, MRI, CT and Ultrasound (section I). These recommendations are meant to enable more accurate and homogenous target definition and contouring, reliable and reproducible prescription of dose and reporting of treatment in environments using CT with applicator in place for treatment planning. These have been developed with a comprehensive approach of objective clinical examination and documentation of disease topography at diagnosis and at BT. A detailed CT Imaging protocol for CT based contouring is introduced, including intravenous contrast and organ filling & contrast prescription, with or without incorporation of real time TRUS during BT acquisition findings. Remission patterns of various components of disease spread are categorized (section II). Four different clinical environments are distinguished (section III). Based on the results of these three sections, a detailed definition for delineation of the CTV-THR-CT on CT is elaborated taking into account all dimensions (width, height and thickness) of the different components of disease spread.
It is well understood that these recommendations are adopted from the gold standard approach of MR IGABT, but are not identical, as they take into account more uncertainties for the different environments. For each environment there is an attempt to minimize the specific uncertainties with the use of revised clinical drawings, introduction of near maximum dstance/width (NMD), tailor the upper limit of target based on uterine infitration uncertainties. in order to arrive at the best possible contouring accuracy. Based on the prevailing clinical environment and availability of imaging modalities for radiotherapetutic management (minimum CT imaging), specific envirnoment may be implemented utilizing CT Imaging for target contouring and brachytherapy planning. The CT based contouring recommendations ready reckoned recipe for each environment is made available in Supplementary material II.
CT based target contouring within these different environments, is a major step towards improvement in the quality of contouring for BT treatment using alternate imaging modalitites. This is of special importance in LMIC’s and LIC’s settings where the cervical cancer burden is high with constant demand for high through-put and MRI at BT is rarely available.
The next steps include benchmarking of CT towards MRI based contouring, dissemination of these recommendations to high volume centers and evaluation of the feasibility and reproducibility of the recommendations in the environments as defined. These recommendations could serve as a uniform volumetric imaging based target prescription protocol for a larger part of the worldwide oncology community working in MRI resource constraint settings within different environments. The CT based contouring recommendations could then become a major step towards enabling adaptive 3D target prescription and improving target prescription homogeneity and quality of BT for cervical cancer in general, which will likely improve clinical outcome.
In addition, these recommendations should be used prospectively and systematically in an EMBRACE I analog prospective study to generate high level clinical evidence for different environments in various clinical settings in terms of target contouring, dose volume parameters (see upcoming treatment planning recommendations) and clinical outcomes (disease control and morbidity). Large multicentric patient cohorts and comparison with the published and upcoming literature on MR-IGABT could further enlighten the strengths and shortcomings of this CT based approach. Finally, this could then become an evidence-based approach for clinical practice change in large patient numbers with cervical cancer, especially in MRI resource constraint settings.
Supplementary Material
Acknowledgments
On behalf of all the authors we would like to thank ACROP Committee of ESTRO, Eralda Azizaj (ESTRO Coordinator) and the reviewers - J. Lindegaard, P. Hoskin, C. Haie Meder, B. Erickson and E. Zubizaretta for their help and support to finalize the recommendations.
Footnotes
Conflict of interest
None.
Disclaimer
ESTRO cannot endorse all statements or opinions made on the guidelines. Regardless of the vast professional knowledge and scientific expertise in the field of radiation oncology that ESTRO possesses, the Society cannot inspect all information to determine the truthfulness, accuracy, reliability, completeness or relevancy thereof. Under no circumstances will ESTRO be held liable for any decision taken or acted upon as a result of reliance on the content of the guidelines.
The component information of the guidelines is not intended or implied to be a substitute for professional medical advice or medical care. The advice of a medical professional should always be sought prior to commencing any form of medical treatment. To this end, all component information contained within the guidelines is done so for solely educational and scientific purposes. ESTRO and all of its staff, agents and members disclaim any and all warranties and representations with regards to the information contained on the guidelines. This includes any implied warranties and conditions that may be derived from the aforementioned guidelines.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.radonc.2021.05.010.
References
- [1].IARC/WHO. GLOBOCAN 2018: Estimated cancer incidence, mortality and prevalence worldwide in 2018. Cervical Cancer Fact Sheet. Available at: https://gco.iarc.fr/today/data/factsheets/cancers/23-Cervix-Uteri-fact-sheet.pdf. [Google Scholar]
- [2].Rodin D, Burger EA, Atun R, et al. Scale-up of radiotherapy for cervical cancer in the era of human papillomavirus vaccination in 118 countries: a model-based analysis of need and economic impact. Lancet Oncol 2019;20:915–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Dimopoulos JC, Petrow P, Tanderup K, Petric P, Berger D, Kirisits C, et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (IV): Basic principles and parameters for MR imaging within the frame of image based adaptive cervix cancer brachytherapy. Radiother Oncol 2012;103:113–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Haie-Meder C, Chargari C, Rey A, Dumas I, Morice P, Magne N. MRI-based low dose-rate brachytherapy experience in locally advanced cervical cancer patients initially treated by concomitant chemoradiotherapy. Radiother Oncol 2010;96:161–5. [DOI] [PubMed] [Google Scholar]
- [5].Pötter R, Georg P, Dimopoulos JC, Grimm M, Berger D, Nesvacil N, et al. Clinical outcome of protocol based image (MRI) guided adaptive brachytherapy combined with 3D conformal radiotherapy with or without chemotherapy in patients with locally advanced cervical cancer. Radiother Oncol 2011;100:116–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Mahantshetty U, Krishnatry R, Hande V, Jamema S, Ghadi Y, Engineer R, et al. Magnetic resonance image guided adaptive brachytherapy in locally advanced cervical cancer: an experience from a tertiary cancer center in a low and middle income countries setting. Int J Radiat Oncol Biol Phys 2017;99:608–17. [DOI] [PubMed] [Google Scholar]
- [7].Sturdza A, Pötter R, Fokdal LU, et al. Image guided brachytherapy in locally advanced cervical cancer: improved pelvic control and survival in RetroEMBRACE - A Multicenter cohort study. Radiother Oncol 2016;120:428–33. [DOI] [PubMed] [Google Scholar]
- [8].Viswanathan AN, Dimopoulos J, Kirisits C, Berger D, Pötter R. Computed tomography versus magnetic resonance imaging-based contouring in cervical cancer brachytherapy: results of a prospective trial and preliminary guidelines for standardized contours. Int J Radiat Oncol Biol Phys 2007;68:491–8. [DOI] [PubMed] [Google Scholar]
- [9].Mahantshetty U, Khanna N, Swamidas J, Engineer R, Thakur MH, Merchant NH, et al. Trans-abdominal ultrasound (US) and magnetic resonance imaging (MRI) correlation for conformal intracavitary brachytherapy in carcinoma of the uterine cervix. Radiother Oncol 2012;102:130–4. [DOI] [PubMed] [Google Scholar]
- [10].Phan T, Mula-Hussain L, Pavamani S, et al. The changing landscape of brachytherapy for cervical cancer: a Canadian practice survey. Curr Oncol 2015;22:356–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Grover S, Harkenrider MM, Cho LP, et al. Image guided cervical brachytherapy: 2014 survey of the American Brachytherapy Society. Int J Radiat Oncol Biol Phys 2016;94:598–604. [DOI] [PubMed] [Google Scholar]
- [12].Viswanathan AN, Creutzberg CL, Craighead P, et al. International brachytherapy practice patterns: a survey of the Gynecologic Cancer Intergroup (GCIG). Int J Radiat Oncol Biol Phys 2012;82:250–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Hegazy N, Potter R et al. High-risk clinical target volume delineation in CT-guided cervical cancer brachytherapy: impact of information from FIGO stage with or without systematic inclusion of 3D documentation of clinical gynecological examination. Acta Oncol 2013;52:1345–52. [DOI] [PubMed] [Google Scholar]
- [14].Eskander RN, Scanderbeg D, Saenz CC, Brown M, Yashar C. Comparison of computed tomography and magnetic resonance imaging in cervical cancer brachytherapy target and normal tissue contouring. Int J Gynecol Cancer 2010;20:47–53. [DOI] [PubMed] [Google Scholar]
- [15].Rao PB, Ghosh S. Routine use of ultrasound guided tandem placement in intracavitary brachytherapy for the treatment of cervical cancer-a South Indian institutional experience. J Contemp Brachytherapy 2015;7:352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Narayan K, van Dyk S, Bernshaw D, Khaw P, Mileshkin L, Kondalsamy-Chennakesavan S. Ultrasound guided conformal brachytherapy of cervix cancer: survival, patterns of failure, and late complications. J Gynecologic Oncology 2014;25:206–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Nesvacil N, Schmid MP, Pötter R, Kronreif G, Kirisits C. Combining transrectal ultrasound and CT for image-guided adaptive brachytherapy of cervical cancer: Proof of concept. Brachytherapy 2016;15:839–44. [DOI] [PubMed] [Google Scholar]
- [18].Viswanathan AN, Erickson B, Gaffney DK, Beriwal S, Bhatia SK, Burnett OL, et al. Comparison and consensus guidelines for delineation of clinical target volume for CT-and MR-based brachytherapy in locally advanced cervical cancer. Int J Radiat Oncol Biol Phys 2014;90:320–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ohno T, Wakatsuki M, Toita T, et al. Recommendations for high-risk clinical target volume definition with computed tomography for three-dimensional image-guided brachytherapy in cervical cancer patients. J Radiat Res 2017;58:341–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].International Commission on Radiation Units and Measurements. Prescribing, Recording, and Reporting Brachytherapy for Cancer of the Cervix (ICRU report 89). Bethesda: 2013. [Google Scholar]
- [21].Haie-Meder C, Pötter R, Van Limbergen E, B riot E, De Brabandere M, Dimopoulos J,, et al. Recommendations from Gynecological (GYN) GEC-ESTRO Working Group (I): Concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol 2005;74:235–45. [DOI] [PubMed] [Google Scholar]
- [22].Petrič P, Hudej R, Rogelj P, Blas M, Tanderup K, Fidarova E, et al. Uncertainties of target volume delineation in MRI guided adaptive brachytherapy of cervix cancer: a multi-institutional study. Radiother Oncol 2013;107:6–12. [DOI] [PubMed] [Google Scholar]
- [23].Knoth J, Potter R, Jürgenliemk-Schulz’s M et al. , Clinical and Imaging findings in cervical cancer and their impact on TNM and FIGO Staging- An Analysis from the EMBRACE study. Gyn Oncol 2020. (in press). [DOI] [PubMed] [Google Scholar]
- [24].Mahantshetty U, Gudi S, Singh R, et al. Indian Brachytherapy Society Guidelines for radiotherapeutic management of cervical cancer with special emphasis on high dose rate brachytherapy. J Contemp Brachytherapy 2019;11:293–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Hricak H, Gatsonis C, Chi DS, Amendola MA, et al. Role of imaging in pretreatment evaluation of early invasive cervical cancer: results of the intergroup study American College of Radiology Imaging Network 6651-Gynecologic Oncology Group 183. J Clin Oncol 2005;23:9329–37. [DOI] [PubMed] [Google Scholar]
- [26].Hricak H, Yu KK. Radiology in invasive cervical cancer. AJR Am J Roentgenol 1996;167:1101–8. [DOI] [PubMed] [Google Scholar]
- [27].Nesvacil N, Pötter R, Sturdza A, Hegazy N, et al. Adaptive image guided brachytherapy for cervical cancer: a combined MRI-/CT-planning technique with MRI only at first fraction. Radiother Oncol 2013;107:75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Hellebust TP, Tanderup K, Lervåg C, Fidarova E, Berger D, Malinen E, et al. Dosimetric impact of interobserver variability in MRI-based delineation for cervical cancer brachytherapy. Radiother Oncol 2013;107:13–9. [DOI] [PubMed] [Google Scholar]
- [29].Fischerova D, Cibula D, Stenhova H, et al. Transrectal ultrasound and magnetic resonance imaging in staging of early cervical cancer. Int J Gynecol Cancer 2008;18:766–72. [DOI] [PubMed] [Google Scholar]
- [30].Segedin B, Gugic J, Petric P. Uterine perforation - 5-year experience in 3-D image guided gynaecological brachytherapy at Institute of Oncology Ljubljana. Radiol Oncol. 2013. May 21;47(2):154–60. doi: 10.2478/raon-2013-0030. Print 2013 Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Schmid MP, Nesvacil N, Pötter R, Kronreif G, Kirisits C. Transrectal ultrasound for image-guided adaptive brachytherapy in cervix cancer-An alternative to MRI for target definition?. Radiother Oncol 2016;120:467–72. [DOI] [PubMed] [Google Scholar]
- [32].Schmid MP, Pötter R, Brader P, Kratochwil A, Goldner G, Kirchheiner K, et al. Feasibility of transrectal ultrasonography for assessment of cervical cancer. Strahlenther Onkol 2013;189:123–8. [DOI] [PubMed] [Google Scholar]
- [33].Pötter R, Federico M, Sturdza A, Fotina I, Hegazy N, Schmid M, et al. Value of magnetic resonance imaging without or with applicator in place for target definition in cervix cancer brachytherapy. Int J Radiat Oncol Biol Phys 2016;94:588–97. [DOI] [PubMed] [Google Scholar]
- [34].Mahantshetty U, Naga ChP, Khadanga CR, Gudi S, Chopra S, Gurram L, et al. A Prospective comparison of computed tomography with transrectal ultrasonography assistance and magnetic resonance imaging-based target-volume definition during image guided adaptive brachytherapy for cervical cancers. Int J Radiat Oncol Biol Phys 2018;7:30933–7. [DOI] [PubMed] [Google Scholar]
- [35].Jastaniyah N, Yoshida K, Tanderup K, et al. A volumetric analysis of GTVD and CTVHR as defined by the GEC ESTRO recommendations in FIGO stage IIB and IIIB cervical cancer patients treated with IGABT in a prospective multicentric trial (EMBRACE). Radiother Oncol 2016;120:404–11. [DOI] [PubMed] [Google Scholar]
- [36].Spampinato S, Tanderup K, Marinovskij E, et al. MRI-based contouring of functional sub-structures of the lower urinary tract in gynaecological radiotherapy. Radiother Oncol 2020;145:117–24. [DOI] [PubMed] [Google Scholar]
- [37].Mazeron R, Fokdal LU, Kirchheiner K. EMBRACE collaborative group, et al. , Dose-volume effect relationships for late rectal morbidity in patients treated with chemoradiation and MRI-guided adaptive brachytherapy for locally advanced cervical cancer: results from the prospective multicenter EMBRACE study. Radiother Oncol 2016;120:412–9. [DOI] [PubMed] [Google Scholar]
- [38].Kirchheiner K, Nout RA, Lindegaard JC, Haie-Meder C, Mahantshetty U, Segedin B, et al. EMBRACE Collaborative Group. Dose-effect relationship and risk factors for vaginal stenosis after definitive radio(chemo)therapy with image-guided brachytherapy for locally advanced cervical cancer in the EMBRACE study. Radiother Oncol 2016;118:160–6. [DOI] [PubMed] [Google Scholar]
- [39].Westerveld H, Pötter R, Berger D, Dankulchai P, Dörr W, Sora MC, et al. Vaginal dose point reporting in cervical cancer patients treated with combined 2D/3D external beam radiotherapy and 2D/3D brachytherapy. Radiother Oncol 2013;107:99–105. [DOI] [PubMed] [Google Scholar]
- [40].Westerveld H, de Leeuw A, Kirchheiner K, Dankulchai P, Oosterveld B, Oinam A, et al. EMBRACE Collaborative Group. Multicentre evaluation of a novel vaginal dose reporting method in 153 cervical cancer patients. Radiother Oncol 2016;120:420–7. [DOI] [PubMed] [Google Scholar]
- [41].Jensen NBK, Pötter R, Kirchheiner K. EMBRACE Collaborative Group, et al. , Bowel morbidity following radiochemotherapy and image-guided adaptive brachytherapy for cervical cancer: Physician- and patient reported outcome from the EMBRACE study. Radiother Oncol 2018;127:431–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


