Abstract
Background
The high mortality rate in Coronavirus Disease (COVID-19) patients is associated with their comorbid conditions. Therefore, it is important to identify risk factors associated with poor outcomes among COVID-19 patients. The aims of this study were to find out the comorbidities in case of death due to COVID-19.
Methods
The design of this study was a retrospective descriptive method with a confirmed COVID-19 patient on hospitalized at Dr. Wahidin Sudirohusodo Hospital from March to September 2020. Ethics Council recommendation number: 357/UN4.6.4.5.31/PP36/2020.
Results
A total of 454 patients were included of this study. 78 (17.18%) patients death due to COVID-19, consisting of 52 (66.67%) male and 26 (33.33%) female. Range of ages between 18 and 85 years. The highest mortality rate occurred in the age group ≥60 years (35; 51.47%), followed by the age group of 45–59 years (33; 48.53%), and the age group of <45 years (10; 12%). The prevalent comorbidity was hypertension (42.31%), cardiovascular disease (30.77%), diabetes (28.21%), chronic kidney disease (23.08%), malignancy (15.38%), obesity (15.38%), chronic liver disease (7.69%), chronic respiratory disease (6.41%), immune related disease (3.85%), and non-traumatic cerebral infarction (3.85%). 41 (52.56%) patients reported having two or more comorbidities, and 37 (47.44%) only has one comorbidity. Elevated neutrophil-to-lymphocyte ratio (NLR) ≥3.13 was seen in the majority of patients (68; 87.18%). The mean value of NLR was 20.94.
Conclusions
Hypertension, cardiovascular disease, and diabetes were the most common comorbidity in patients death due to COVID-19. More than half of the patients had two or more comorbidities.
Keywords: COVID-19, Comorbidities, Mortality
Introduction
On March 11, 2020, the World Health Organization declared the COVID-19 outbreak a pandemic.1 As of 09 September, the Government of Indonesia announced 203.342 confirmed cases of COVID-19 and 8.336 deaths.2 Data from China have indicated that older adults, particularly those with serious underlying health conditions, are at higher risk for severe COVID-19-associated illness and death than are younger persons. Although the majority of reported COVID-19 cases in China were mild (81%), approximately 80% of deaths occurred among adults aged ≥60 years.3 This first preliminary description of outcomes among patients with COVID-19 in the United States indicates that fatality was highest in persons aged ≥85, ranging from 10% to 27%, followed by 3% to 11% among persons aged 65–84 years.4
Over 180 countries have been affected by COVID-19, resulting in mass death worldwide. As cases evolve globally, it has been noted that persons with underlying chronic illnesses are more likely to contract the virus and become severely ill. Due to SARS CoV-2 being a relatively new virus, the data available is limited. However, patients with comorbidities have more deteriorating outcomes compared with patients without. COVID-19 patients with history of hypertension, obesity, chronic lung disease, diabetes, and cardiovascular disease have the worst prognosis and most often end up with deteriorating outcomes such as ARDS and pneumonia. Also, elderly patients in long-term care facilities, chronic kidney disease patients, and cancer patients are not only at risk for contracting the virus, but there is a significantly increased risk of death among these groups of patients.5
The high mortality rate in COVID-19 patients is associated with their comorbid conditions. Therefore, it is important to identify risk factors associated with poor outcomes among COVID-19 patients. The aims of this study were to find out the comorbidities in case of death due to COVID-19.
Methods
The design of this study was a retrospective descriptive method with the sampling technique in this study was carried out purposively on COVID-19 patients who entered and were treated at the WS Hospital from the period March to September 2020, total of 454 patients were included of this study. Ethical clearance from ethics committee Hasanuddin University, with number 357/UN4.6.4.5.31/PP36/2020.
Result
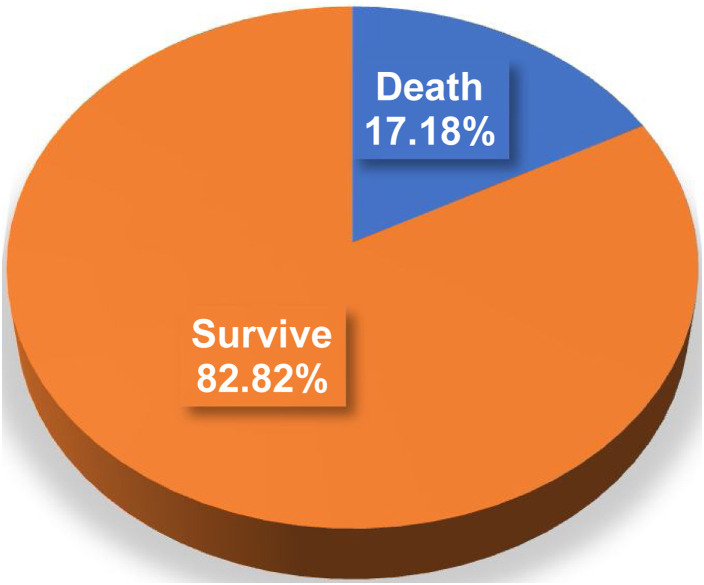
A total of 454 patients were included of this study, consisting of 225 (49.56%) male and 229 (50.44%) females. Among 78 (17.18%) patients had been reported death due to COVID-19 (Fig. 1 ).
Fig. 1.
Outcome of confirmed COVID-19 patients.
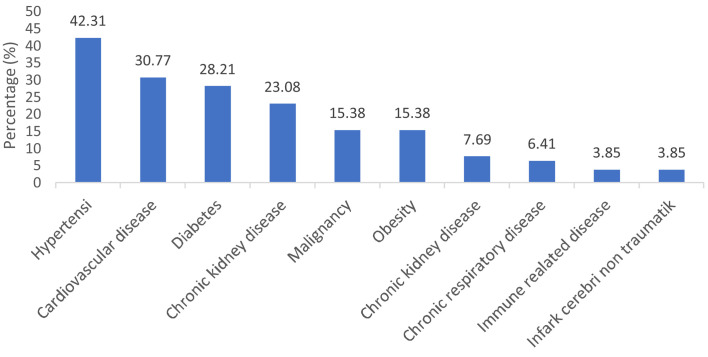
Two-thirds of them are male. Range of ages between 18 and 85 years with average 57 years. The highest mortality rate occurred in the age group ≥60 years (35; 51.47%), followed by the age group of 45–59 years (33; 48.53%), and the age group of <45 years (10; 12%). The most comorbidity was hypertension (42.31%), cardiovascular disease (30.77%), and diabetes (28.21%) (Fig. 2 ).
Fig. 2.
Comorbidities of patients death due to COVID-19.
Elevated NLR ≥3.13 was seen in the majority of patients (68; 87.18%) with the mean value of NLR was 20.94. Characteristic of patient is available in Table 1 .
Table 1.
Characteristics of patients death due to COVID-19.
| Characteristics | Total (n = 78) | Percentage (%) |
|---|---|---|
| Sex | ||
| Male | 52 | 66.67 |
| Female | 26 | 33.33 |
| Age | ||
| <45 | 10 | 12.82 |
| 45–59 | 33 | 48.53 |
| ≥60 | 35 | 51.47 |
| Comorbidity | ||
| Hypertension | 33 | 42.31 |
| Cardiovascular disease | 24 | 30.77 |
| Diabetes | 22 | 28.21 |
| Chronic kidney disease | 18 | 23.08 |
| Malignancy | 12 | 15.38 |
| Obesity | 12 | 15.38 |
| Chronic liver disease | 6 | 7.69 |
| Chronic respiratory disease | 5 | 6.41 |
| Immune related disease | 3 | 3.85 |
| Infark cerebri non traumatik | 3 | 3.85 |
| Number of comorbidities | ||
| 1 comorbidity | 37 | 47.44 |
| ≥2 comorbidities | 41 | 52.56 |
| NLR | ||
| <3.13 | 10 | 12.82 |
| ≥3.13 | 68 | 87.18 |
Discussion
In this study, the mortality rate was quite large, 17.18%. The high mortality rate indicates the severity of the disease and the presence of comorbid conditions. A high mortality rate was also reported in US. The study includes the first large case series of sequentially hospitalized patients with confirmed COVID-19 in the US. There were 21% of patients died, among patients who were discharged or died (n: 2634).6 In a retrospective cohort study from China, hospitalized patients were predominantly men with a median age of 56 years; 26% required intensive care unit (ICU) care, and there was a 28% mortality rate.7
The men's mortality rate was higher than for women (66.67% vs. 33.33%). The systematic literature review and meta-analysis by Ortolan et al., data pooling resulted in a significant association between male sex and mortality (OR = 1.81; 95% CI 1.25–2.62).8 Emerging evidence has suggested that ACE2 is a co-receptor for SARS-CoV-2 viral entry into the human cell that plays a significant role in the pathogenesis of this virus.9 A study has suggested that ACE2 expression was higher in Asian males.10 Other explanations to why men were associated with severe outcomes compared with women in response to COVID-19 infection may involve differences in immunologic reaction and the lack of protective effect of estrogen signaling seen in females.11
We found the highest mortality rate occurred in the age group ≥60 years (35; 51.47%). The condition of geriatric patients also increases the likelihood of a cytokine storm when exposed to COVID-19 because geriatrics have an immunosenescence condition (decreased immunity in old age).12 The presence of immunosenesscences in the elderly causes susceptibility to respiratory tract infections. This can occur due to reduced mucosal barrier, mucociliary clearance, immune response and the presence of respiratory inflammation against pathogenic microorganisms.13 Mucociliary clearance is reduced due to a decrease in the number and activity of cilia in the upper respiratory tract. It can also reduce the ability of the respiratory system to neutralize viral infections.14 Immune system dysfunction such as in the case of immunosenessence can cause susceptibility and severity of clinical manifestations of COVID-19 in the elderly population. This is caused by uncontrolled infection due to a weak immune system resulting in multi-organ failure, especially in organs or systems that have a lot of ACE2 such as the respiratory, cardiovascular, hepatic, and renal systems.15
Karyono DR and Wicaksana AL reported on their research that the mortality rate was higher among elderly patients with COVID-19 and COVID-19 patients with hypertension, diabetes, and other cardiovascular diseases.16 Leading comorbidities among COVID-19 deaths in NY, USA were hypertension (55.4%), diabetes (37.3%), hyperlipidemia (18.5%).5 A total of 5700 patients were included, the most common comorbidities were hypertension (3026, 56.6%), obesity (1737, 41.7%), and diabetes (1808, 33.8%).6 In this study, the most comorbidities were hypertension (42.31%), cardiovascular disease (30.77%) and diabetes (28.21%).
More than half of patients (52.56%) death due to COVID-19 had ≥2 comorbids and the rest had only one comorbid. Guan WJ et al. analyzed data from 1590 laboratory confirmed hospitalized patients from 575 hospitals in 31 provinces China. This study analyzed the composite end-points, which consisted of admission to an Intensive Care unit, invasive ventilation or death. Among laboratory confirmed cases of COVID-19, patients with any comorbidity yielded poorer clinical outcomes than those without. After adjusting for age and smoking status, COPD (HR (95% CI) 2.681 (1.424–5.048)), diabetes (1.59 (1.03–2.45)), hypertension (1.58 (1.07–2.32)) and malignancy (3.50 (1.60–7.64)) were risk factors of reaching the composite end-points. A greater number of comorbidities also correlated with poorer clinical outcomes. The hazard ratio (95% CI) was 1.79 (1.16–2.77) among patients with at least one comorbidity and 2.59 (1.61–4.17) among patients with two or more comorbidities.17
The data of 61 patients with confirmed COVID-19 were analyzed, the baseline characteristics of patients in the mild and severe groups were described and compared, and the dynamic changes of laboratory indexes and imaging were demonstrated. The independent risk factors affecting incidence of severe illness were screened. The results showed that NLR was the most significant factor affecting the severe illness incidence, and it had significant predictive value. Furthermore, according to the NLR and age stratification, the incidence of severe ill ones with NLR ≥3.13 and aged ≥50 years old was 50%, and 9.1% in age ≥50 and NLR < 3.13 patients.18
Conclusion
The mortality rate for hospitalized COVID-19 patients is 17.18%. Hipertension, cardiovascular disease, and diabetes were the most common comorbidity in patients death due to COVID-19. More than half of the patients had two or more comorbidities.
Conflicts of interest
The authors declare no conflict of interest.
Footnotes
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.
References
- 1.WHO. Coronavirus Disease 2019 Situation Report 51-11th March 2020. WHO Bull. 2020; 2019: 2633.
- 2.WHO Indonesia. Coronavirus Disease Situation Report World Health Organization. World Heal Organ. 2020; 19:1–17.
- 3.Hua W., Xiaofeng L., Zhenqiang B., et al. Consideration on the strategies during epidemic stage changing from emergency response to continuous prevention and control. Chinese J Endem. 2020;41:297–300. doi: 10.3760/cma.j.issn.0254-6450.2020.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Bialek S., Boundy E., Bowen V., et al. Severe outcomes among patients with coronavirus disease 2019 (COVID-19) — United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanyaolu A., Okorie C., Marinkovic A., et al. Comorbidity and its impact on patients with COVID-19. SN Compr Clin Med. 2020;2:1069–1076. doi: 10.1007/s42399-020-00363-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richardson S., Hirsch J.S., Narasimhan M., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA – J Am Med Assoc. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ortolan A., Lorenzin M., Felicetti M., et al. Does gender influence clinical expression and disease outcomes in COVID-19?. A systematic review and meta-analysis. Int J Infect Dis. 2020;99:496–504. doi: 10.1016/j.ijid.2020.07.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou P., Yang X.-L., Wang X.-G., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhao Y., Zhao Z., Wang Y., et al. Single-cell RNA expression profiling of ACE2, the receptor of SARS-CoV-2. Am J Respir Crit Care Med. 2020;202:756–759. doi: 10.1164/rccm.202001-0179LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Channappanavar R., Fett C., Mack M., et al. Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. J Immunol. 2017;198:4046–4053. doi: 10.4049/jimmunol.1601896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perhimpunan Dokter Paru Indonesia (PDPI) et al. Definisi Kasus dan Derajat Penyakit. Pedoman Tatalaksana COVID-19; 2020, 3–6.
- 13.Widya Wasityastuti, Andika Dhamarjati S.S. Immunosenescence and the susceptibility of the elderly to coronavirus disease 2019 (COVID-19) Expert Opin Ther Targets. 2020;40:199–202. [Google Scholar]
- 14.Abbas A.K., Lichtman A.H.P.S. 7th ed. Elsevier; Philadelphia: 2016. Basic immunology: functions and disorders of the immune system. [Google Scholar]
- 15.Patel A.B.V.A. COVID-19 and angiotensin-converting enzyme inhibitors and angiotensin receptor blockers. J Am Med Assoc. 2020;323:1769–1770. doi: 10.1001/jama.2020.4812. [DOI] [PubMed] [Google Scholar]
- 16.Karyono D.R., Wicaksana A.L. Current prevalence, characteristics, and comorbidities of patients with COVID-19 in Indonesia. J Community Empower Heal. 2020;3:77. [Google Scholar]
- 17.Guan W.J., Liang W.H., Zhao Y., et al. Comorbidity and its impact on 1,590 patients with Covid-19 in China: a nationwide analysis. Eur Respir J. 2020;55 doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu J., Liu Y., Xiang P., et al. Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J Transl Med. 2020;18 doi: 10.1186/s12967-020-02374-0. [DOI] [PMC free article] [PubMed] [Google Scholar]