ABSTRACT
Background
The coronavirus disease 2019 (COVID-19) pandemic profoundly affected food systems including food security. Understanding how the COVID-19 pandemic impacted food security is important to provide support and identify long-term impacts and needs.
Objective
The National Food Access and COVID research Team (NFACT) was formed to assess food security over different US study sites throughout the pandemic, using common instruments and measurements. This study presents results from 18 study sites across 15 states and nationally over the first year of the COVID-19 pandemic.
Methods
A validated survey instrument was developed and implemented in whole or part through an online survey of adults across the sites throughout the first year of the pandemic, representing 22 separate surveys. Sampling methods for each study site were convenience, representative, or high-risk targeted. Food security was measured using the USDA 6-item module. Food security prevalence was analyzed using ANOVA by sampling method to assess statistically significant differences.
Results
Respondents (n = 27,168) indicate higher prevalence of food insecurity (low or very low food security) since the COVID-19 pandemic, compared with before the pandemic. In nearly all study sites, there is a higher prevalence of food insecurity among Black, Indigenous, and People of Color (BIPOC), households with children, and those with job disruptions. The findings demonstrate lingering food insecurity, with high prevalence over time in sites with repeat cross-sectional surveys. There are no statistically significant differences between convenience and representative surveys, but a statistically higher prevalence of food insecurity among high-risk compared with convenience surveys.
Conclusions
This comprehensive study demonstrates a higher prevalence of food insecurity in the first year of the COVID-19 pandemic. These impacts were prevalent for certain demographic groups, and most pronounced for surveys targeting high-risk populations. Results especially document the continued high levels of food insecurity, as well as the variability in estimates due to the survey implementation method.
Keywords: food security, COVID-19, survey sampling, food insecurity, high-risk
Multi-site assessment demonstrates widespread food insecurity during COVID-19, especially for households with children, job loss, and Black, Indigenous, People of Color across multiple survey methods.
Introduction
The coronavirus disease 2019 (COVID-19) was declared a pandemic by the WHO in March 2020 (1), with widespread impact across the USA and globally. As of 12 April, 2021, the USA had over 20% of the confirmed cases and about 19% of the COVID-19-related deaths globally (2). Furthermore, COVID-19 was the third leading cause of death in the USA in 2020 (3).
The pandemic caused major disruptions to the USA economy, food system, and overall health and well-being of Americans. The unemployment rate in the USA reached an unprecedented high of 14.8% in April 2020 (4), with job disruptions concentrated in low-paying jobs, disproportionately affecting Black, Indigenous, and People of Color (BIPOC) (5). Although the unemployment rate declined to 6.7% in December 2020, the economic effects of the pandemic are likely to persist for years, consistent with the Great Recession of 2008 (6). The need to social distance and quarantine to contain disease spread led to stockpiling, placing a strain on the food supply chain, which was unable to adequately respond to the pandemic, resulting in food access concerns for many Americans (7). This, in combination with widespread disruption in employment, increased food-related hardship for many Americans, particularly those most vulnerable to economic disruption (8).
Disasters, like hurricanes, and public health emergencies, like the COVID-19 pandemic, disrupt built and social environments, and their impacts persist long after they occur (9–11). Disasters tend to impact housing stability, household composition, and financial obligations, which can limit resources for food and lead to food-related hardship (12). Groups most vulnerable to disasters were disproportionately affected during the pandemic, including low-income households, single-headed households with children, adults living alone, and black- and Hispanic-headed households (13–15). The COVID-19 pandemic magnified the health disparities that exist among low-income households, who were already more likely to struggle to meet basic needs (15).
Food insecurity, or the inability to consistently obtain enough, desirable, varied, and nutritious foods (16), is heightened during disasters and emergencies (17, 18). Emergency nutrition response aims to assist affected individuals; however, co-ordinating enough high-quality food remains a challenge in a postdisaster setting (19, 20). Quickly assessing food insecurity to inform pandemic relief efforts was a challenging task; for instance, the national food insecurity statistics for 2020 from the US Census Bureau, measured using the USDA's Household Food Security Survey Module (HFSS), was not released until September 2021 (21). As a result, agencies, organizations, and researchers deployed surveys and produced estimates to determine the impact of the pandemic on food insecurity. For example, the US Census Bureau released the Household Pulse Survey that captures food insufficiency, a higher severity of food insecurity, and Feeding America released projected food insecurity prevalence for 2020 and 2021 based on changes in unemployment and poverty (21–23). Food insufficiency prevalence increased from 8% prior to 13 March, 2020 to 10% in April and May 2020, and food insecurity was projected to increase from 11% in 2019 to 14% in 2020 (22, 24). A nationally representative cross-sectional study used the USDA's 10-item HFSS and found that food insecurity drastically increased at the onset of the COVID-19 pandemic, from 11% in 2018 to ≤38% in March 2020 (25). This is especially high considering the impact of the economic downturn during the Great Recession of 2008 when food insecurity peaked at a much lower 15% in 2011, as reported by the US Census Bureau using the USDA's 10-item HFSS (13). In addition, households that were food insecure prior to the pandemic were more likely to have their situations exacerbated due to less job flexibility, higher risk of job loss/furlough, and fewer resources/support to allow for complying with social distancing recommendations (15). In March 2020, the Coronavirus Aid, Relief, and Economic Security (CARES) Act was passed in the USA, which provided direct payments to Americans and expanded unemployment insurance (26). States were also able to issue additional Supplemental Nutrition Assistance Program (SNAP) benefits to households receiving less than the maximum benefits in March and April 2020 (27). Although the early months of the pandemic may have been the peak of food insecurity and insufficiency, higher than usual rates have persisted as the COVID-19 pandemic continues despite government relief efforts (28).
Despite several early surveys assessing food insecurity during the COVID-19 pandemic, and continued efforts to measure food insufficiency through the Census Household Pulse Survey, there have been few collaborative efforts to monitor and measure food insecurity across diverse geographic and social contexts, and to compare data. In May 2020, a national collaboration of researchers – The National Food Access and COVID Research Team (NFACT) – was formed to examine COVID-19 impacts on food access, food insecurity, and the overall food system. This study reports the findings of this collaborative effort, with data from 18 study sites including a nationally representative sample, to better understand food insecurity over diverse regions and timeframes. The study examined overall levels of food insecurity, as well as food insecurity among households with children, households that experienced job disruption, and participants identifying as BIPOC. We further assessed how different survey implementation methods associate with different levels of food insecurity, and report results from multiple time points within the same study site, based on data availability.
Methods
Survey development
A survey instrument, known as the NFACT Survey Version 1.0 (29) was developed in March 2020. This survey was developed in consultation with key stakeholders in the state of Vermont, where it was first implemented, and drew from the existing literature on food security and food access. Where possible, validated questions and instruments were used. The survey was piloted in Vermont, with 25 adult residents in late March, and validation methods (e.g. Cronbach α, factor analysis) were used to test the internal validity of questions with key constructs (α > 0.70) (30). A second version of the survey was released in May 2020 to reflect changes in the COVID-19 context (31) and include new questions. The surveys included questions on food access, food security, food purchasing, food assistance program participation, dietary intake, perceptions of COVID-19, and individual and household sociodemographic characteristics. The questions utilized in this study were included in both surveys and across study sites.
NFACT study sites and data collection
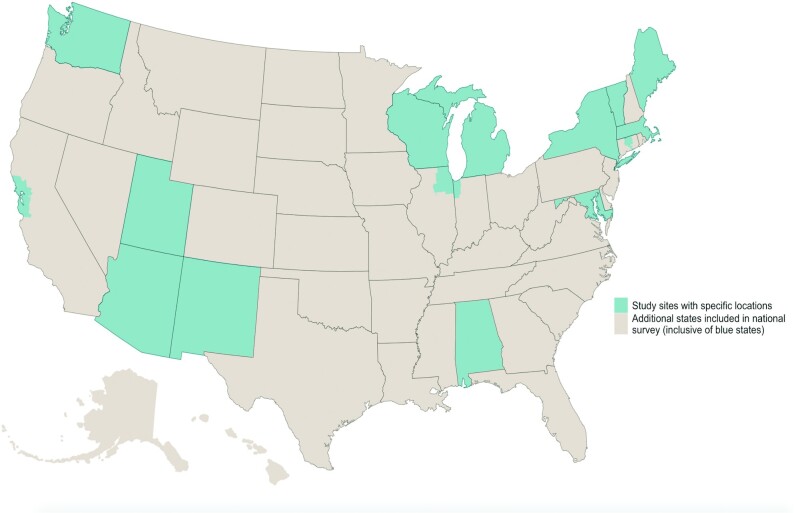
NFACT represents 18 study sites across 15 states, as well as a national sample (Figure 1). NFACT was formed as a result of interested teams generated through the presentation of results and communication primarily via The Nutrition and Obesity Policy Research and Evaluation Network (NOPREN) and through the open sourcing of version 1.0 of the survey. The NFACT Executive Team (University of Vermont, Johns Hopkins University, University of Arizona, and Arizona State University) further helped to solidify NFACT through coordinated national data collection efforts. NFACT study sites distributed the NFACT surveys (in whole or part) online pursuing one of three sampling strategies: 1) convenience sampling in partnership with community organizations, stakeholders, social media, and/or news media, which are not representative of a state population (10 sites); 2) quota sampling using survey panels administered by Qualtrics (Provo, UT), a survey research company, in which the quotas aimed to achieve state representation on some characteristics (e.g. race, ethnicity, income) (8 sites); or 3) quota or convenience sampling in which certain high-risk populations (e.g. low-income, BIPOC, or SNAP participants) were targeted (6 sites). In some cases where high-risk populations were targeted, these groups were oversampled to ensure adequate representation in the overall study sample. In one site, Vermont, the first two surveys are convenience but panel data, whereas the third survey is a representative sample using a Qualtrics sample. Table 1 provides specific details about the sampling strategies, target populations, representation of the data, and survey fielding dates. Potential participants under the age of 18 years old were excluded across all study sites. All study sites administered the survey in English; in Arizona, California-Bay Area, Maine, Massachusetts, Nationally, NY-Capital Region, New Mexico, and Utah, surveys were also administered in Spanish, which was done at the discretion of the site research team and the prevalence of Spanish speaking households in their site or desired sample. Sample size calculations for the adult population of each site indicate that a sample size of 384 or 385 was necessary to achieve a population with a 95% CI and a 5% margin of error. All sites exceeded these sample sizes with margins of error ranging from 1.8% (95% CI) to 4.7% ( Supplementary Table 1).
FIGURE 1.
NFACT study sites. Blue states and regions represent sites in addition to the national sample strategy, which includes additional data from all states. NFACT, National Food Access and COVID research Team. Visual credit: Samuel F. Rosenblatt
TABLE 1.
Study sites and relevant methods for each site
| Study site | Target population | Sample and recruitment | Weighting | Representative of state | Dates in field |
|---|---|---|---|---|---|
| Alabama | General population | Convenience sample. Recruitment via social media and community organizations | No weighting | No | June–July 2020 |
| Arizona | General population | Representative sample with survey panel (on race, ethnicity) with oversampling of low-income population with Qualtrics | Weighted on income | Yes | July–August 2020 |
| California-Bay Area | General population | Convenience sample. Recruitment via social media and community organizations | No weighting | No | August– November 2020 |
| Chicago/Illinois | High-risk population | High-risk sample. Survey panel sampling with Qualtrics to meet specific race, ethnicity, income, and education quotas. Oversampled low-income population (50%), black (50%), Hispanic (50%), and 50% high school education or less | No weighting | No | June–July 2020 |
| Connecticut | Oversampled low-income population | High-risk sample. Survey panel with oversampled low-income population, but representative on race and ethnicity with Qualtrics | No weighting | No | August 2020 |
| Maine | General population | Representative sample with survey panel (income) with Qualtrics | No weighting | Yes | August–September 2020 |
| Maryland | General population | Representative sample with survey panel (on race, ethnicity, and income) with Qualtrics | No weighting | Yes | July–September 2020 |
| Massachusetts | General population | Representative sample with survey panel (on race, ethnicity, education, age, gender, geographic region) with oversampling of low-income population with Qualtrics | Weighted on household income, age, gender, race/ethnicity, education, geographic region | Yes | October 2020 – January 2021 |
| Michigan | General population | Convenience sample. Recruitment via social media | No weighting | No | June 2020 |
| National | General population | Representative sample with survey panel (on race, ethnicity) and oversampling of low-income population with Qualtrics | Weighted on income | Yes | July–August 2020 |
| New Mexico | General population | Convenience sample. Recruitment via social media and community organizations | No weighting | No | May–June 2020 |
| New York City (May/June) | High-risk population | High-risk sample. Nested quota via social media campaign, community-based organizations, convenience sample, and survey consumer panel sampling via Qualtrics to meet specific race/ethnicity, income, and education quotas. This includes an oversampling of blacks (50%), Hispanics (50%), high school education or less (50%), and low income (50% below $25,000 annual income before taxes) | No weighting | No | May–June 2020 |
| New York City (July/August) | High-risk population | High-risk sample. Nonproportional quota sample, recruited by Qualtrics. Oversampled low-income population (50%), black (40%), Hispanic (40%), Native American (20%), and 50% high school education or less | No weighting | No | July–August 2020 |
| NY State except NYC | High-risk population | High-risk sample. Nonproportional quota sample recruited by Qualtrics. Quotas: low income or low education (50%), black (50%), and Hispanic (50%) | No weighting | No | July–September 2020 |
| NY-Capital Region (Oct–Jan) | General population | Representative sample with survey panel (on race, ethnicity, and income) with Qualtrics | No weighting | Yes | October 2020–January 2021 |
| NY-Capital Region (Jan/Feb) | General population | Convenience sample. Recruitment via social media and community organizations | No weighting | No | January–February 2021 |
| NY Central/Upstate | General population | Convenience sample. Recruitment via listservs, social media, community organizations | No weighting | No | October–December 2020 |
| Utah | High-risk population | Convenience sample. Recruited Supplemental Nutrition Assistance Program (SNAP) participants through state listserv of current SNAP recipients | No weighting | No | July–September 2020 |
| Vermont (March/April) | General population | Convenience sample. Recruitment via listservs, social media, community organizations | No weighting | No | March–April 2020 |
| Vermont1 (May/June) | General population | Convenience sample. Recruitment via listservs, social media, community organizations | No weighting | No | May–June 2020 |
| Vermont (August/Sept) | General population | Representative sample with survey panel (on race, ethnicity, and income) with Qualtrics | No weighting | Yes | July–September 2020 |
| Washington State (June/July) | General population | Convenience sample. Recruitment via listservs, social media, community organizations | No weighting | No | June–July 2020 |
| Washington State (Dec/Jan) | General population | Convenience sample. Recruitment via listservs, social media, community organizations, recontact of wave respondents | No weighting | No | December 2020–January 2021 |
| Wisconsin | General population | Representative sample with survey panel (on race, ethnicity, and income) with Qualtrics. Oversample Milwaukee area | No weighting | Yes | July–October 2020 |
Longitudinal sample of a subset of the same people who responded to the Vermont March/April survey
Institutional Review Board approval was obtained by each study site prior to commencing data collection. Institutional Review Board approval for the Alabama site was provided by the Auburn University at Montgomery Internal Review Board. The Arizona State University Office of Research Integrity and Assurance approved the study for the Arizona State University and University of Arizona teams under protocol number: 2004590240A00. The California-Bay Area study was approved by the San Jose State University Human Subjects Institutional Review Board under exempt registration (Institutional Review Board Protocol Tracking Number: 20162). The DePaul University Institutional Review Board reviewed and approved the Chicago site study as exempt research. The D'Youville College Institutional Review Board reviewed and approved the research for the Connecticut, Massachusetts, and New York City sites as exempt research. The University of Maine Institutional Review Board for the Protection of Human Subjects provided exempt ethical approval for the Maine site. Institutional Review Board exempt approval for the Maryland site was provided by Johns Hopkins Bloomberg School of Public Health Institutional Review Board under IRB#2359. The New Mexico site received Institutional Review Board approval from New Mexico State University's Office of Research Integrity and Ethics under protocol number 20024. The University at Albany Institutional Review Board provided the review for the Albany site. The 2 research projects were approved as exempt under protocol numbers 20 × 296 and 20 × 196. Institutional Review Board approval for the NY Central site was provided by the Cornell University Institutional Review Board for Human Participant Research. The Utah State University Institutional Review Board approved the Utah site research through exempt review under protocol number 11339. Institutional Review Board exempt status approval for the Washington site was provided by the University of Washington Institutional Review Board (UW IRB committee J). Institutional Review Board approval for the Wisconsin site was provided by the University of Wisconsin-Milwaukee Institutional Review Board under Category 2 exempt status. Institutional Review Board approval for the Vermont site was provided by The University of Vermont under protocol number 0000873.
Measures
Food security was assessed using the USDA’s 6-item Short Form Food Security Survey Module (32) which is designed to identify households with food insecurity. These 6 questions include those related to having enough food, enough money for food, affording balanced meals, and disrupting eating patterns (i.e. cutting, skipping meals, going hungry). In most sites, participants were asked to complete 6 items about the 12 months prior to COVID-19 and since the COVID-19 pandemic began in March 2020, though a few sites only asked these questions since the COVID-19 pandemic began. For example, the USDA 6-item module first question typically reads, “The food that (I/we) bought just didn't last, and (I/we) didn't have money to get more. Was that often, sometimes or never true for your household in the last 12 months?” This question would have been adapted to end “in the year before the COVID-19 pandemic” and “since the COVID-19 pandemic began (March 2020).” In some more recent surveys (i.e. Massachusetts, NY-Central/Upstate, and the second Washington survey) and in Michigan respondents answered questions about food security “in the past 30 days,” which is validated through the USDA module. Following standard USDA scoring, a score of 2–6 was categorized as food insecure (32). It is important to note that the prepandemic food security responses were retrospective and were answered at the same time as the questions about current food security. Households with children were determined with a question about household composition by age. Households with any members aged 0–17 years were classified as a household with children. Job disruption was assessed by asking participants if their household experienced a job disruption since the start of the pandemic, including job loss, furlough, or loss of hours/income reduction, categories which were not mutually exclusive. Participants indicating any negative job impact were categorized as experiencing a job disruption. BIPOC classification was determined based on survey questions about race and ethnicity. Participants indicating any race or ethnicity besides non-Hispanic white (NHW) were classified as BIPOC. Participants indicating NHW were classified as such and Hispanic of any race were classified as Hispanic. We report disaggregated race and ethnicity data in sites reporting >30 respondents identifying with a particular race or ethnicity. This number corresponds to the generally accepted number of respondents necessary to conduct normality tests in statistics.
Data aggregation and analysis
Food insecurity prevalence (overall and for specific populations of interest) by study site and survey were aggregated into a single dataset for analysis in Stata 16.0 (33). Although we primarily report descriptive statistics of the results across the multiple sites, we also used ANOVA with Scheffe multiple comparison tests (34) to assess whether there are statistically significant differences in prevalence of food insecurity (overall and for key subpopulations) between surveys based on the three different sampling techniques (i.e. convenience, representative, and high-risk). We report P values <0.05 as statistically significant in the results.
Results
Respondent characteristics
The sample included 27,168 adults from across the USA with data on food insecurity. The racial and ethnic make-up of the sample overall was 70.0% NHW and 28.6% BIPOC, with 1.4% of respondents not identifying race or ethnicity. Among BIPOC respondents, 8.0% identified as non-Hispanic black, 11.9% as Hispanic, and 8.1% other races or multiracial (Table 2). Given the diversity of NFACT study sites, including their sample size and diverse demographic make-up, the number of respondents with specific demographic characteristics or life experiences (e.g. job disruption or children in the household) varied across study sites. There was a large variation in the proportion of BIPOC respondents across study sites, because of differences in population composition, but also because some study sites oversampled BIPOC respondents. Slightly over 40% of respondents (40.6%) had children in the household, ranging from 19.2% of households in Maine to 85.6% of households in the California-Bay Area. Among all respondents, 35.3% had experienced some type of job disruption since the COVID-19 pandemic began, ranging from a low of 10.8% of respondents in a second Washington State survey in early 2021, to 76.5% of respondents in a NY-Capital Region survey in January and February 2021. Among representative samples, the range of respondents experiencing job disruptions varied from 37.6% in the national sample to 61.3% in the NY-Capital Region in October–January.
TABLE 2.
Total number of respondents and subpopulation characteristics by study site
| Study site | Total respondents1 | With children | Job disruption/(reduced income) | BIPOC2 | NHW3 | NHB4 | Hispanic | Other or multiple races |
|---|---|---|---|---|---|---|---|---|
| Alabama | 1247 | 541 | 546 | 226 | 1061 | 142 | 27 | 86 |
| Arizona | 576 | 189 | 221 | 268 | 352 | 32 | 194 | 42 |
| California-Bay Area | 724 | 203 | 321 | 232 | 223 | 6 | 122 | 49 |
| Chicago/Illinois | 680 | 379 | 314 | 498 | 169 | 215 | 258 | 103 |
| Connecticut | 512 | 199 | 286 | 158 | 354 | 56 | 73 | 54 |
| Maine | 504 | 97 | 193 | 42 | 477 | 9 | 8 | 8 |
| Maryland | 903 | 330 | 368 | 427 | 555 | 239 | 91 | 97 |
| Massachusetts | 2939 | 1098 | 1467 | 748 | 2191 | 202 | 292 | 254 |
| Michigan | 484 | 237 | 279 | 64 | 418 | 25 | 18 | 21 |
| National | 1510 | 515 | 568 | 585 | 925 | 212 | 255 | 118 |
| New Mexico | 1415 | 406 | 261 | 494 | 843 | 15 | 362 | 117 |
| New York City (May/June) | 1165 | 599 | 494 | 876 | 289 | 252 | 496 | 128 |
| New York City (July/August) | 525 | 317 | 285 | 484 | 41 | 154 | 123 | 102 |
| NY State | 494 | 207 | 189 | 494 | n/a | 260 | 234 | |
| NY-Capital Region (Oct–Jan) | 479 | 167 | 294 | 156 | 353 | 43 | 42 | 71 |
| NY-Capital Region (Jan–Feb) | 427 | 283 | 327 | 137 | 317 | 62 | 56 | 19 |
| NY-Central/Upstate | 434 | 120 | 144 | 30 | 380 | 2 | 10 | 22 |
| Utah | 644 | 219 | 277 | 102 | 392 | 12 | 61 | 56 |
| Vermont (March/April) | 3016 | 913 | 1103 | 150 | 2603 | 5 | 45 | 104 |
| Vermont (May/June) | 1212 | 383 | 294 | 57 | 1137 | 3 | 19 | 37 |
| Vermont (August/Sept) | 578 | 178 | 270 | 49 | 551 | 6 | 17 | 26 |
| Washington State (June/July) | 2514 | 1095 | 636 | 592 | 1910 | 93 | 210 | 289 |
| Washington State (Dec/Jan) | 3169 | 1541 | 343 | 737 | 2647 | 98 | 283 | 356 |
| Wisconsin | 1017 | 393 | 430 | 181 | 836 | 58 | 80 | 43 |
| TOTAL | 27,168 | 11,026 | 9589 | 7787 | 19,024 | 2195 | 3235 | 2202 |
| % of total | 40.6% | 35.3% | 28.7% | 70.0% | 8.1% | 11.9% | 8.1% |
Indicates number of total respondents with food security data
Black, Indigenous, People of Color (BIPOC) respondents. Number includes anyone identifying as other than non-Hispanic white.
Non-Hispanic white (NHW).
Non-Hispanic black (NHB).
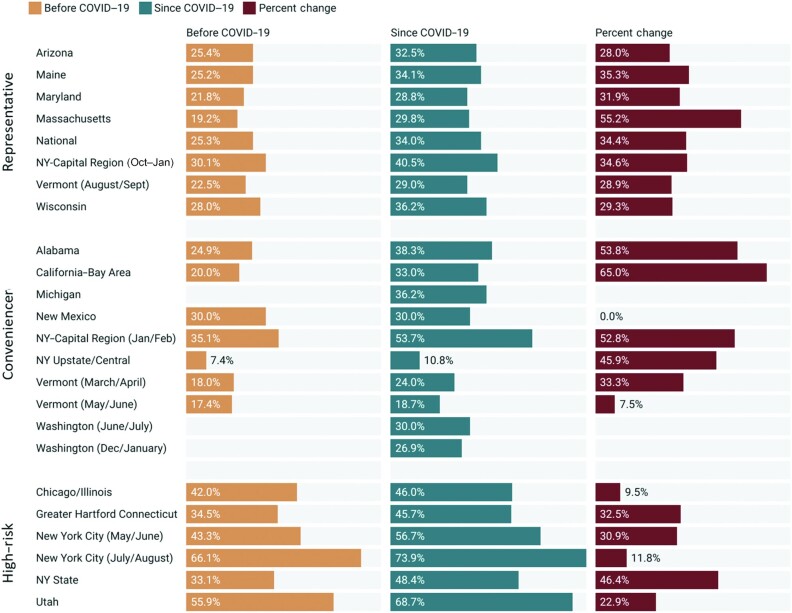
Overall prevalence of food insecurity
We found higher levels of food insecurity reported since the COVID-19 pandemic began, compared with ex-post levels reported for the pre-COVID-19 pandemic period. This finding was consistent in all 20 sites that asked about food insecurity both before and during the COVID-19 pandemic (Figure 2), with the exception of the New Mexico site (where no change was found). The prevalence of food insecurity across study sites during the COVID-19 pandemic ranged from 10.8% in a Central/Upstate New York convenience survey from October to December 2020 (which asked about the last 30 days), to 73.9% in a New York City high-risk survey in July/August 2020 which oversampled BIPOC, low-income respondents. Among states that represented state characteristics, food insecurity prevalence ranged from 28.8% in Maryland to 36.2% in Wisconsin since the start of the COVID-19 pandemic. In sites that gathered retrospective data on the time periods both before and during the COVID-19 pandemic, the rate of increase ranged from 0% in New Mexico to a 65% increase among respondents in the California-Bay Area. We found that both convenience and representative samples had significantly lower prevalence of food insecurity both before and since the COVID-19 pandemic, compared with surveys targeting high-risk populations, though the percent change did not significantly differ across survey sample type (Table 3).
FIGURE 2.
Overall prevalence of food insecurity across NFACT surveys and study sites. Before COVID-19 data was collected retrospectively at the same time as data regarding food insecurity since the COVID-19 pandemic. The timeframe of “since COVID-19” varied by site, depending on when the survey was fielded, but all used March 2020 as a reference point. NFACT, National Food Access and COVID research Team.
TABLE 3.
Overall prevalence of food insecurity across different measures and time periods by survey type. P values were obtained through ANOVAs with Scheffe multiple comparisons
| Survey type | P values | ||||||
|---|---|---|---|---|---|---|---|
| Prevalence of food insecurity | Timeframe | Convenience | State representative | High risk | Convenience – high risk | Convenience –representative | Representative – high risk |
| Overall food insecurity | Before COVID-19 | 21.8% | 23.9% | 43.6% | 0.002 | 0.918 | 0.004 |
| Since COVID-19 | 30.2% | 32.1% | 54.3% | 0.000 | 0.933 | 0.002 | |
| Percent change | 36.9% | 34.7% | 26.9% | 0.561 | 0.971 | 0.701 | |
| BIPOC food insecurity | Before COVID-19 | 29.5% | 32.1% | 37.3% | 0.211 | 0.818 | 0.497 |
| Since COVID-19 | 40.2% | 40.6% | 55.1% | 0.048 | 0.999 | 0.078 | |
| Percent change | 32.0% | 29.5% | 36.0% | 0.892 | 0.957 | 0.743 | |
| Households with children food insecurity | Before COVID-19 | 30.1% | 37.2% | 44.1% | 0.042 | 0.389 | 0.424 |
| Since COVID-19 | 39.0% | 49.2% | 57.6% | 0.003 | 0.117 | 0.272 | |
| Percent change | 31.8% | 33.4% | 32.7% | 0.995 | 0.983 | 0.997 | |
| Job disruption food insecurity | Any job disruption | 43.5% | 50.1% | 64.8% | 0.003 | 0.489 | 0.058 |
| Job loss | 51.3% | 60.8% | 72.1% | 0.003 | 0.216 | 0.168 | |
| Furlough | 44.2% | 51.2% | 63.1% | 0.081 | 0.679 | 0.383 | |
| Reduced hours | 43.0% | 51.5% | 63.5% | 0.036 | 0.524 | 0.320 | |
BIPOC, Black, Indigenous, and People of Color.
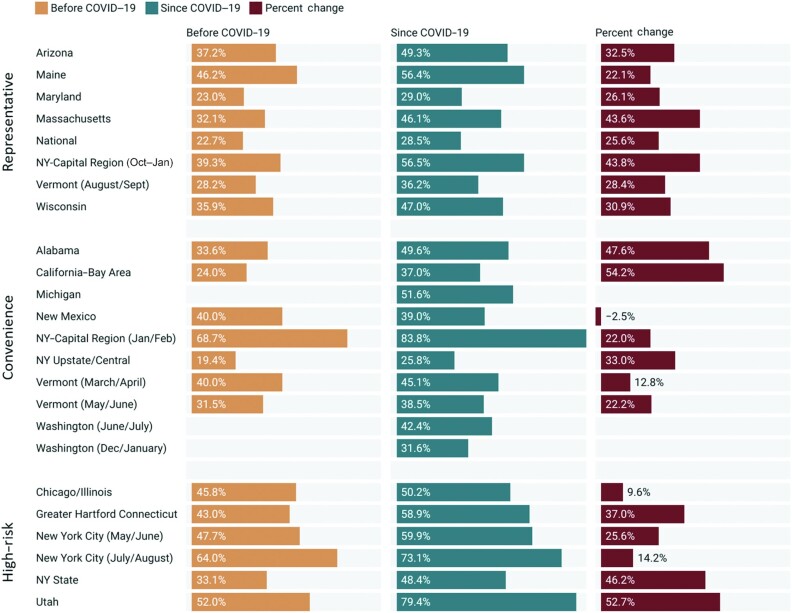
Prevalence of food insecurity among BIPOC respondents
In all survey sites that collected data on food insecurity before (ex-post) and during the COVID-19 pandemic, we found that food insecurity increased for BIPOC respondents since the onset of the COVID-19 pandemic, with the exception of New Mexico. Furthermore, we found that the prevalence of food insecurity among BIPOC respondents during the COVID-19 pandemic was higher than the overall prevalence of food insecurity in the majority of study sites (Figure 3); however, it is worth noting that this was also true for pre-COVID-19 food insecurity. The highest percent increase in food insecurity was identified in the California-Bay Area (54.2% increase in food insecurity among BIPOC respondents). However, the highest prevalence of food insecurity during the COVID-19 pandemic among BIPOC respondents was identified in the NY-Capital Region (83.8%). We found the prevalence of BIPOC food insecurity during the COVID-19 pandemic was significantly different (P = 0.048) for convenience (40.2%) versus high-risk (55.1%) survey types.
FIGURE 3.
Prevalence of food insecurity before and during the COVID-19 pandemic, and the percent change, among BIPOC respondents, by study site. Before COVID-19 data was collected retrospectively at the same time as data regarding food insecurity since the COVID-19 pandemic. The timeframe of “since COVID-19” varied by site, depending on when the survey was fielded, but all used March 2020 as a reference point. BIPOC, Black, Indigenous, and People of Color.
Furthermore, we disaggregated race and ethnicity data when a particular survey had ≥30 respondents identifying within a specific race or ethnic group (Figure 4). This additional breakdown further highlights disparities in food insecurity across many study sites among BIPOC respondents, as compared with NHW respondents. For example, although the majority of surveys found the prevalence of food insecurity was higher for BIPOC respondents both before and during the COVID-19 pandemic, the opposite is true of NHW respondents (i.e. the majority of surveys found the prevalence of food insecurity among NHW respondents before and during the COVID-19 pandemic was lower than the site's overall food insecurity).
FIGURE 4.

Prevalence of food insecurity before and during the COVID-19 pandemic among different racial and ethnic groups, by study site. Disaggregated race and ethnicity food insecurity prevalence is only reported for sites where ≥30 respondents identified as a specific race or ethnic group.
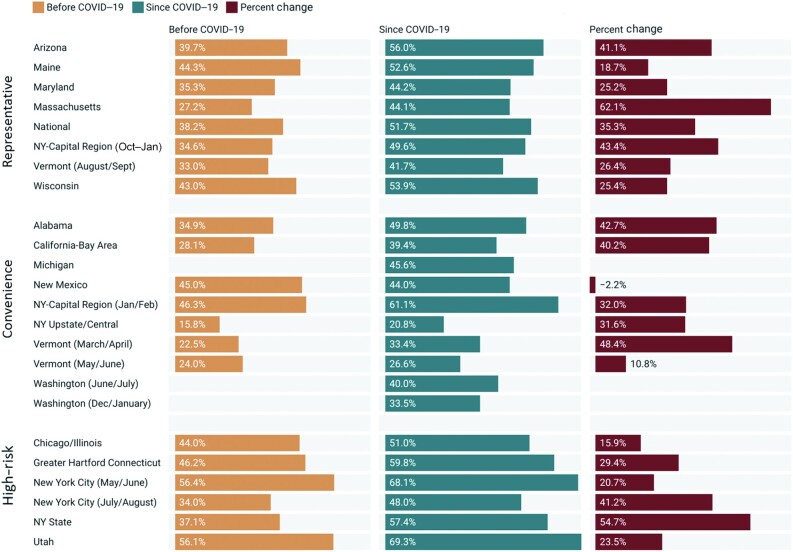
Prevalence of food insecurity among households with children
In all but one survey (New Mexico) with data on food insecurity before (ex-post) and during the COVID-19 pandemic, food insecurity increased among households with children (Figure 5). The highest reported percent change was in Massachusetts (a 62.1% increase), whereas the overall highest prevalence during the COVID-19 pandemic was 69.3% food insecurity among households with children in a Utah survey focused on SNAP participants. In surveys representative of the state population, the prevalence of food insecurity among households with children ranged from 41.7% in Vermont in August/September 2020 to 56% in Arizona. Convenience surveys had statistically lower food insecurity prevalence compared with high-risk survey populations both before the COVID-19 pandemic (P = 0.042) and during the COVID-19 pandemic (P = 0.003). We found no significant differences between the other survey types (Table 3).
FIGURE 5.
Prevalence of food insecurity before and during the COVID-19 pandemic among households with children in a study site, and the percent change. Before COVID-19 data was collected retrospectively at the same time as data regarding food insecurity since the COVID-19 pandemic. The timeframe of “since COVID-19” varied by site, depending on when the survey was fielded, but all used March 2020 as a reference point.
Prevalence of food insecurity among respondents experiencing job disruption
Food insecurity during the COVID-19 pandemic was higher in all surveys and study sites among respondents facing job disruption, compared with the overall prevalence of food insecurity in those sites (Figure 6). The range of food insecurity among respondents with job disruptions since the COVID-19 pandemic (March 2020) ranged from 21.5% in Central/Upstate New York to ≤77.2% in New York City among all surveys. Among surveys with state-wide representative samples on some characteristics, the prevalence of food insecurity for those with job disruptions ranged from 38.7% in Vermont in August/September 2020 to 59.8% in Wisconsin. Convenience surveys had statistically lower food insecurity prevalence compared with high-risk survey populations for any job disruption (P = 0.003), job loss (P = 0.003), and reduction in hours (P = 0.036) (Table 3).
FIGURE 6.
Prevalence of food insecurity since the COVID-19 pandemic among respondents with any job disruption, job loss, furlough, and/or reduction in hours, by study site.
Discussion
In this study, food insecurity was assessed in multiple sites across the USA using a common measurement instrument. Key trends in food insecurity were highly consistent among research sites, albeit with some significant differences in magnitude depending on survey type. This study utilized three different sampling methods (representative, convenience, and targeted high-risk populations), allowing us to compare results between both study sites and sampling strategies.
In our study, food insecurity increased across nearly all research sites between the pre- and during pandemic periods, with the exception of New Mexico. The New Mexico site may not have seen increases in food insecurity during COVID-19 because of the state's high rate of food insecurity prior to the pandemic; New Mexico ranked 4th in food insecurity in the USA in 2019 (35). Additionally, those experiencing food insecurity in the state may have limited access to the Internet in order to take the survey and may not have been reached through convenience sampling compared with other sites.
Although there have been several national surveys examining food insecurity during COVID-19 and its associated factors, only a few have examined the relation between food insecurity before and since the pandemic onset as the majority of our study sites did with posthoc data. Our results that show an increase in food insecurity from pre- to during pandemic is consistent with the few other national surveys examining the impact of COVID-19 on food insecurity. For example, data from the Census Household Pulse Survey and the COVID Impact Survey used probability sampling to obtain nationally representative samples, which Morales et al. (2020) used to find that household food insecurity prevalence increased from 30% prepandemic to 43% in late April 2020 (36). In the COVID Impact Survey, data collected in early April 2020 was extended using models to show that the overall prevalence of food insecurity was more than double the predicted rate (37). These same researchers found similar estimates of food insecurity increases using data from the Census Household Pulse Survey (38–40). Additionally, a study among parents in the USA recruited through Facebook showed that those reporting low or very low food security increased from 37% before COVID-19 to 54% in May 2020, and then decreased to 45% in September 2020 (39). Among one of the only cohort studies we are aware of to date, an investigation conducted in Pittsburgh, PA, also found that food insecurity increased among low-income, predominantly BIPOC residents in a study cohort from 20.7% before the pandemic to 36.9% in the months following COVID-19’s onset (36, 40).
In sites where NFACT predicted a rate of change in food insecurity, such results may be influenced by prepandemic trends, as summarized through the most recent USDA Economic Research Service (ERS) Household Food Security in the United States report (41), which shows regional differences in the prevalence of food insecurity rates averaged from 2018 to 2020. For example, some south-central and Appalachian states (e.g. New Mexico, Texas, Oklahoma, Louisiana, Mississippi) report food insecurity above the US average. West coast states (California, Oregon, Washington), upper Midwest and northern plains states (e.g. North Dakota, South Dakota, Minnesota), and some eastern states (Virginia, New Jersey, Vermont) report lower than average food insecurity. However, when we compared these prepandemic conditions to survey results, we found that regional differences in food insecurity (below, near, or above the national average) do not adequately explain differences between pre- and postpandemic food insecurity at NFACT study sites. For example, the average change in food security across NFACT representative surveys was 34.7%. Arizona, which the USDA-ERS report identifies as a state with near-average rates of food insecurity (∼10.7%), reported through NFACT survey results a lower than average rate of change pre- and postpandemic. Meanwhile, Vermont is a state that is reported by the USDA-ERS to have lower than average rates of food insecurity, yet the rate of change between pre- and postpandemic (28.9%) was close to the NFACT average rate of change. Similar findings emerge when considering the NFACT surveys that employed a convenience sampling approach, indicating that posthoc prepandemic conditions may not be an appropriate proxy for estimating the effect of the pandemic on food insecurity in the regional or state level.
Notably, select NFACT sites that utilized a representative high-risk sampling approach were more likely than surveys using a convenience or representative sample to document a higher prevalence of food insecurity since the onset of the COVID-19 pandemic. These results suggest that targeted oversampling of high-risk populations is likely to detect higher food insecurity outcomes, an important finding for future surveys and methodologies. These results may also be critical for policymakers who may seek to utilize these methods to understand the prevalence of food insecurity for specific vulnerable groups. Furthermore, when assessing overall food insecurity before or during the COVID-19 pandemic there were no statistically significant differences in food insecurity prevalence between convenience and representative sampling approaches. Among all survey approaches there were no significant differences in the percent change of prevalence of food insecurity, suggesting that the rate of change was consistent across all survey types. These results provide important findings for researchers who may consider various factors (e.g. cost, timeframe for data collection, ability to represent data at a state level) when determining a sampling approach in the future.
It should also be noted that our results show clear differences in food insecurity in different US regions. According to national food insecurity statistics from 2018 to 2020, regional differences were already present prepandemic and overall food insecurity rates were higher in southern states compared with the rest of the USA, ranging from 5.7% in New Hampshire to 15.3% in Mississippi (41). These differences may be partially attributed to unique economic vulnerabilities such as household characteristics (income, education, employment, and household composition) as well as state-level economic characteristics and policies (wages, cost of living, unemployment benefits, and assistance programs) (35, 42). Within the pandemic context, these differences may be further attributed to problems in the food supply chain and community purchasing behavior (i.e. stockpiling), especially at the beginning of the pandemic (37). Another likely cause for variation is the inconsistent national approach to pandemic-related restrictions such as stay-at-home orders, restrictions on businesses, and quarantine requirements. Variation in state response to the threat of rising food insecurity is best exemplified in state waivers authorized through SNAP and the Women, Infants and Children (WIC) program and administered through the USDA Food and Nutrition Services. Specifically, states had discretion about which benefits and waivers to request. Although some states made repeated requests for a wide range of allowances authorized by Congress, others requested only a few (43, 44). It is likely that variation in each state’s application of extra benefits and temporary waivers influenced differences in food insecurity across our study sites. We suggest that future research examine the relative effects of extra benefits and waivers granted to states, and their influence on both programmatic enrollment and food security outcomes.
Our study found that some populations have experienced higher rates of food insecurity since the COVID-19 pandemic (25, 45, 46). Consistent with recent studies (37, 47), BIPOC populations reported higher rates of food insecurity than NHW respondents in nearly all NFACT study sites both before and since the onset of the COVID-19 pandemic. Moreover, the three sampling approaches used by NFACT sites found strikingly similar results. There was no statistical difference between sampling strategies, with the exception of convenience and targeted high-risk approaches, specifically when addressing food insecurity among BIPOC respondents during the COVID-19 pandemic. Several other national surveys using professional survey platforms (Qualtrics and Turk Prime) have similarly found higher food insecurity rates among black and Hispanic respondents compared with NHW respondents (15, 25). The only study to provide food insecurity data for Native American respondents found that this population also has a higher rate of food insecurity than NHW populations since the beginning of the pandemic (25). Our research and the work of others (48, 49) clearly shows that the short-term effects of the pandemic expose underlying racial and economic inequalities, but also highlights that BIPOC respondents faced a higher prevalence of food insecurity before the COVID-19 pandemic. As a result, strategic policy interventions that include short-term relief and long-term programmatic efforts to support underserved individuals, households, and communities are needed (48). Additionally, it has been suggested that US policy shift towards a human rights framework for addressing food insecurity, an approach that necessitates attention to social and economic determinants (50).
As well, our research also found that the pandemic has disproportionately affected households with children. Although it is estimated that the overall prevalence of food insecurity doubled in the early days of the pandemic, it is estimated that food insecurity among households with children tripled during that time period (47). Again, our analysis showed few differences in results by sampling strategy, with these differences being limited to comparing convenience and high-risk approaches. Several other studies support our findings, showing consistently that households with children are experiencing high levels of food insecurity during the COVID-19 pandemic (15, 25). Though our study does not focus on household composition, past research has shown that single parent households where women are the head of the household are particularly vulnerable to food insecurity. Studies from across the world show that children who experience food insecurity are more likely to be undernourished and suffer from poor cognitive development as a result (51–53). Our results should be of concern to those who focus on child development and well-being.
One likely contributor to the disproportionate increase in food insecurity among households with children was the shift to online education, which increased challenges for families that depended on free or reduced-price school meals. Although federal support such as the Pandemic Electronic Benefits Transfer (P-EBT) program provided additional benefits to families who normally would qualify for these free and reduced-price meals (54), additional hurdles in accessing school meals were reported. For example, the national NFACT survey conducted in the summer of 2020 found that participation in the school meals program dropped during the beginning of the pandemic, likely before states had developed alternative school-meal delivery strategies or accessed federal funding for expanded programs. Further, between 45 and 55% of survey respondents who utilized school meal pick-ups during the pandemic reported difficulties with availability of delivery, meal pick-up sites being open, and the quantity of food provided (55). Compounding these challenges, low-income families with children were more likely to lose income during the COVID-19 pandemic compared with households without children (54). These findings strongly suggest a need for increased support for school food programs, enabling these important programs to ensure that meals reach families in need. Similarly, NFACT sites universally found a higher prevalence of food insecurity among households that experienced job or income loss during the pandemic compared to households with no change in employment status, a finding aligned with other recent research (15, 25, 56).
Several of our sites conducted repeated cross-sectional or panel surveys, providing insights into the prevalence of food insecurity over time, both within and across regions. Four NFACT study sites have conducted >1 round of surveys (New York City, New York Capital Region, Vermont, and Washington state), whereas more recent surveys (Massachusetts and the second Washington state survey) were designed to elucidate respondent experiences with food insecurity within the past 30 days, providing a more current understanding of food insecurity prevalence. All cross-sectional studies found an increasing prevalence of food insecurity as the pandemic continues, with each additional survey demonstrating a higher prevalence of food insecurity since the onset of the COVID-19 pandemic. All of these cross-sectional surveys measured food insecurity since the COVID-19 pandemic began, suggesting that additional numbers of individuals continue to become food insecure, even after the initial impacts of COVID-19 have been felt. Likewise, the recent NFACT Massachusetts survey, measuring food insecurity prevalence in the last 30 days, found that nearly 30% of respondents were classified as food insecure at the end of 2020. This prevalence is significantly higher than the prepandemic level of 8.4% for this state (13), though it should be noted that the prepandemic level for Massachusetts respondents was much higher than observed prepandemic levels. Although our study did not look at the severity of food insecurity, other studies have examined the change in food insecurity severity over time. A study consisting of repeated cross-sectional surveys in Mexico found that overall food insecurity increased monthly from April to June of 2020. Although mild food insecurity decreased from May to June of 2020, moderate and severe food insecurity increased over this time period (57).
Evidence from the NFACT surveys corroborates other studies suggesting that food insecurity levels are likely to persist above prepandemic levels for an extended period of time as occurred after the Great Recession and past disasters (13, 17, 20). As noted by Hernandez and Holtzclaw (58), the combined impact of a pandemic and a recession are unique in modern memory. However, the slow recovery from the 2008 Great Recession in the USA is instructive. It took 11 years for food insecurity levels to return to prerecession levels after the Great Recession; according to national data, food insecurity went from 11.1% in 2007 to 14.6% in 2008, reaching a peak of 14.9% in 2011, and back to 11.1% only in 2018 (13). Similarly, high levels of food insecurity were observed ≤5 y following other disasters, such as after Hurricanes Katrina and Harvey (20, 59). Besides factors such as age, race/ethnicity, and income, other factors such as support systems, community and generalized self-efficacy are also critical when addressing food insecurity in a postdisaster context. A 5-year follow-up study on Hurricane Katrina revealed that postdisaster food insecurity levels were associated with poor physical and mental health, as well as low social support, generalized self-efficacy, and sense of community (17, 59). Considering that the pandemic has disproportionately affected racial and ethnic minorities, these populations are likely to experience higher levels of food insecurity and be affected by its long-lasting health effects even after the economy recovers. Taken together, these results suggest that the impact of COVID-19 on food security in the USA is far from over, and additional support systems and policies will be necessary to continue to alleviate the long-term impacts of the global pandemic and recession.
This research is not without limitations. In presenting our results, we recognize 3 key limitations. First, research that requires participants to report eating or food-related behaviors is challenged by both recall and social desirability bias (60). Retrospectively asking participants about food insecurity has been shown to lead to overestimation of pre-COVID prevalence of food insecurity (38), suggesting our study may contain similar overestimations. However, we try to address this potential limitation by reporting percent change between pre- and during COVID-19 food security, in addition to absolute prevalence of food insecurity, though if the overall prepandemic levels of food insecurity are lower, our absolute food insecurity prevalence is likely underestimated. Although there has been some scepticism about the high prevalence of food insecurity reported since the COVID-19 pandemic began, our results confirm this high prevalence while providing a more robust measure to benchmark changes. Second, surveys across all research sites included in this study were administered online, limiting respondents to those with computer skills and Internet access. Although there are many studies that have utilized the USDA food security module in an online format (e.g. 61–63), this potentially introduced a barrier for some (though not all) elderly or low-income potential respondents (64, 65), as well as those living in rural areas without reliable Internet (66). Additionally, there have been some studies that show differences in respondent affirmations of food insecurity questions, depending on whether questionnaires are administered online or in person. Further research is needed before the effects of food insecurity survey modality is fully understood (67). Our study employed a number of methods to overcome this challenge across different sampling strategies. These strategies included partnering with nonprofit and community organizations as well as government assistance programs to advertise the survey, and seeking economic representation through sampling targets. Notably, our results show no statistically significant difference between sites using convenience and representative samples, indicating that even for study sites that employed a convenience sampling approach, this potential bias did not have a significant influence on our findings. Although differences did emerge when representative and targeted high-risk samples were compared, we argue that this shows the importance of purposeful sampling in target communities. Finally, all sites used the USDA 6-item Short Form Food Security Module, which we acknowledge is not as comprehensive as the 18-item measure, cannot measure the most severe levels of food insecurity, and does not ask about the conditions of children in the household. Furthermore, following the USDA standard scoring, we dichotomized our food insecurity prevalence given the number of sites and complexity of our data reporting. However, we recognize that there are degrees of food insecurity (very low, low, marginal) and that this can have important implications for food insecurity impacts (57) and policymaking (68).
A number of US studies have explored the impact of COVID-19 on food insecurity prevalence since the beginning of the COVID-19 pandemic, though most have been national samples, modeling efforts, or single site-specific studies. Here, we report the results from a nationwide collaborative effort across 18 study sites and a nationally representative sample, including 22 surveys since the beginning of the COVID-19 pandemic. The scale of our work provides data from >27,000 people, and more completely demonstrates the economic hardship the COVID-19 pandemic has had for many people. Our findings show that the economic impacts of the COVID-19 pandemic on food insecurity were felt particularly hard by households with children and BIPOC respondents, providing further evidence that the pandemic has exacerbated racial and ethnic disparities in food insecurity that existed prior to the pandemic. Surveys conducted in study sites more than once also demonstrate an increasing prevalence of food insecurity since the COVID-19 pandemic began, and more recent studies reaffirm that a high prevalence of food insecurity, compared with before the COVID-19 pandemic, continues. We further demonstrate how survey methodology can affect food insecurity estimates and changes in prevalence across pre- and post-COVID-19 data, demonstrating the importance of high-risk target studies for adequately assessing unique populations in need. These findings point to the clear continued need for additional programmatic and policy assistance to provide food insecurity and economic relief even as the pandemic may wane, but longer-term impacts from economic recessions set in. Our future work will continue to conduct additional surveys and comparative analysis to quantify changes in food access, food security, and food assistance use as the USA recovers from the COVID-19 pandemic.
State-specific acknowledgments
Arizona: We thank Aggie J Yellow Horse for their helpful feedback on the survey instrument. We also would like to thank Marina Acosta Ortiz for her assistance with the translation of the survey.
New Mexico: We want to thank Gaby Phillips and Aracely Tellez for help with translating the survey into Spanish.
The research design, data collection, and analysis of individual site data was conducted by site-level NFACT teams (see supplementary materials for all authors). The authors’ responsibilities were as follows—AWB, LAC, MMD, MTN, GAP, MSR, SR, RES, and RZ: wrote and edited the manuscript; MTN: conducted the analysis comparing the study site types and food security prevalence; MTN: had primary responsibility for final content; and all authors: read and approved the final manuscript.
Supplementary Material
ACKNOWLEDGEMENTS
We wish to thank the study participants for their time and dedication in completing the surveys and follow-up interviews. Additionally, we would like to thank Christi Sherlock and Mattie Alpaugh at The University of Vermont for their assistance with project management.
Notes
Alabama: No funding to report. Arizona: This project was supported by a COVID-19 seed grant from the College of Health Solutions, Arizona State University. California-Bay Area: This project was supported by the College of Health and Human Sciences, San Jose State University. Chicago/Illinois: This project was supported by the College of Liberal Arts and Social Sciences, DePaul University. Connecticut: Stop & Shop and the Hunger to Health Collaboratory (H2HC) provided funding for the NFACT study conducted by the Foodshare team. The funder did not play any role in the design, implementation, or analysis and interpretation of the data. Maine: The project was supported by the University of Maine School of Food and Agriculture and the George J. Mitchell Center for Sustainability Solutions. Maryland: This research was supported by a Directed Research grant from the Johns Hopkins Center for a Livable Future. Massachusetts: Stop & Shop and the Hunger to Health Collaboratory (H2HC) provided funding for the NFACT study conducted by The Greater Boston Food Bank team. The funder did not play any role in the design, implementation, or analysis and interpretation of the data. Michigan: Funding was provided from Wayne State University faculty startup funds. National: This research was supported by the College of Health Solutions, Arizona State University with support from the college's COVID-19 seed grant and the university's Investigator Research Funds; the University of Arizona College of Agriculture and Life Sciences Rapid COVID-19 seed grant; a Directed Research grant from the Johns Hopkins Center for a Livable Future; and the University of Vermont, the College of Agriculture and Life Sciences, the Gund Institute for Environment, Office of the Vice President of Research, and the University of Vermont, Agricultural Research Service Food Systems Research Center. New York City: St. John's University Vincentian Institute for Social Action. NY State: Funded by the University of Colorado Natural Hazards Center, Quick Response Grant. The Quick Response program is based on work supported by the National Science Foundation (Award #1635593). Any opinions, findings, conclusions, or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the views of NSF or the Natural Hazards Center. NY Capital Region: Funding for the Qualtrics Panel Survey was provided by the Foundation for Food and Agriculture Research. Funding for the non-Qualtrics Panel Survey was provided by UAlbany President's COVID-19 Minority Health Disparities Engaged Researchers Seed Funding Program. NY Central/Upstate: This work was supported by a Cornell Atkinson Center COVID-19 Rapid Response Fund award. Utah: Support for the project was provided by the Utah Create Better Health Program, Utah State University Extension, and the Utah Department of Workforce Services. Vermont: Funding was provided by The University of Vermont College of Agriculture and Life Sciences and Office of the Vice President of Research, The Gund Institute for Environment, and the University of Vermont Agricultural Research Service Food Systems Research Center. Washington: The project was supported by the University of Washington Population Health Initiative (UWPHI), the University of Washington School of Public Health (UWSPH), and the Department of Epidemiology.
Author disclosures: The authors report no conflicts of interest.
Supplemental Table 1 is available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/cdn/.
Abbreviations used: BIPOC, Black, Indigenous, and People of Color; COVID-19, coronavirus disease 2019; ERS, Economic Research Service; HFSS, Household Food Security Survey Module; NFACT, National Food Access and COVID research Team; NHW, non-Hispanic white; SNAP, Supplemental Nutrition Assistance Program.
Contributor Information
Meredith T Niles, Email: mtniles@uvm.edu, Department of Nutrition and Food Sciences, Gund Institute for Environment, University of Vermont, Burlington, VT.
Alyssa W Beavers, Department of Nutrition and Food Science, Wayne State University, Detroit, MI.
Lauren A Clay, Health Administration & Public Health Department, D'Youville College, Buffalo, NY.
Marcelle M Dougan, Department of Public Health and Recreation, San José State University, San José, CA.
Giselle A Pignotti, Department of Nutrition, Food Science, and Packaging, San José State University, San José, CA.
Stephanie Rogus, Department of Family and Consumer Sciences, New Mexico State University, Las Cruces, NM.
Mateja R Savoie-Roskos, Department of Nutrition, Dietetics and Food Sciences, Utah State University, Logan, UT.
Rachel E Schattman, School of Food and Agriculture, University of Maine, Orono, ME.
Rachel M Zack, Business and Data Analytics, The Greater Boston Food Bank, Boston, MA.
Francesco Acciai, College of Health Solutions, Arizona State University, Phoenix, AZ.
Deanne Allegro, Department of Kinesiology, Auburn University at Montgomery, Montgomery, AL.
Emily H Belarmino, Department of Nutrition and Food Sciences, Gund Institute for Environment, University of Vermont, Burlington, VT.
Farryl Bertmann, Department of Nutrition and Food Sciences, University of Vermont, Burlington, VT.
Erin Biehl, Johns Hopkins Center for a Livable Future, Johns Hopkins University, Baltimore, MD.
Nick Birk, Business and Data Analytics, The Greater Boston Food Bank, Boston, MA.
Jessica Bishop-Royse, Faculty Scholarship Collaborative, College of Liberal Arts and Social Sciences, DePaul University, Chicago, IL.
Christine Bozlak, Health Policy, Management, and Behavior, University at Albany- State University of New York, Rensselaer, NY.
Brianna Bradley, Johns Hopkins Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD.
Barrett P Brenton, Center for Civic Engagement, Binghamton University, Binghamton, NY.
James Buszkiewicz, Department of Epidemiology, University of Washington, Seattle, WA.
Brittney N Cavaliere, Institute for Hunger Research & Solutions, Connecticut Food Bank/Foodshare, Bloomfield, CT.
Young Cho, Joseph J Zilber School of Public Health, University of Wisconsin-Milwaukee, Milwaukee, WI.
Eric M Clark, Department of Plant and Soil Science, University of Vermont, Burlington, VT.
Kathryn Coakley, Department of Individual, Family, and Community Education, University of New Mexico, Albuquerque, NM.
Jeanne Coffin-Schmitt, Department of Natural Resources, Cornell University, Ithaca, NY.
Sarah M Collier, Department of Environmental and Occupational Health Sciences, University of Washington, Seattle, WA.
Casey Coombs, Department of Nutrition, Dietetics and Food Sciences, Utah State University, Logan, UT.
Anne Dressel, College of Nursing, University of Wisconsin-Milwaukee, Milwaukee, WI.
Adam Drewnowski, Department of Epidemiology, University of Washington, Seattle, WA.
Tom Evans, School of Geography, Development and Environment, University of Arizona, Tucson, AZ.
Beth J Feingold, Department of Environmental Health Sciences, University at Albany- State University of New York, Rensselaer, NY.
Lauren Fiechtner, Department of Gastroenterology and Nutrition, MassGeneral Hospital for Children, Boston, MA.
Kathryn J Fiorella, Department of Population Medicine and Diagnostic Sciences and Master of Public Health Program, Cornell University, Ithaca, NY.
Katie Funderburk, Alabama Cooperative Extension System, Auburn University, Auburn, AL.
Preety Gadhoke, Department of Pharmacy Administration and Public Health, College of Pharmacy and Health Sciences, St. John's University (at the time of study administration), Jamaica, NY.
Diana Gonzales-Pacheco, Department of Individual, Family, and Community Education, University of New Mexico, Albuquerque, NM.
Amelia Greiner Safi, Department of Population Medicine and Diagnostic Sciences and Master of Public Health Program, Cornell University, Ithaca, NY.
Sen Gu, Department of Pharmacy Administration and Public Health, College of Pharmacy and Health Sciences, St. John's University (at the time of study administration), Jamaica, NY.
Karla L Hanson, Department of Population Medicine and Diagnostic Sciences and Master of Public Health Program, Cornell University, Ithaca, NY.
Amy Harley, Joseph J Zilber School of Public Health, University of Wisconsin-Milwaukee, Milwaukee, WI.
Kaitlyn Harper, Department of International Health, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD.
Akiko S Hosler, Department of Epidemiology and Biostatistics, University at Albany- State University of New York, Rensselaer, NY.
Alan Ismach, Department of Environmental and Occupational Health Sciences, University of Washington, Seattle, WA.
Anna Josephson, Department of Agricultural and Resource Economics, University of Arizona, Tucson, AZ.
Linnea Laestadius, Joseph J Zilber School of Public Health, University of Wisconsin-Milwaukee, Milwaukee, WI.
Heidi LeBlanc, Department of Nutrition, Dietetics and Food Sciences, Utah State University, Logan, UT.
Laura R Lewis, Community and Economic Development, Washington State University, Port Hadlock, WA.
Michelle M Litton, Department of Nutrition and Food Science, Wayne State University, Detroit, MI.
Katie S Martin, Institute for Hunger Research & Solutions, Connecticut Food Bank/Foodshare, Bloomfield, CT.
Shadai Martin, Department of Family and Consumer Sciences, New Mexico State University, Las Cruces, NM.
Sarah Martinelli, College of Health Solutions, Arizona State University, Phoenix, AZ.
John Mazzeo, Master of Public Health Program, College of Liberal Arts and Social Sciences, DePaul University, Chicago, IL.
Scott C Merrill, Department of Plant and Soil Science, Gund Institute for Environment, University of Vermont, Burlington, VT.
Roni Neff, Department of Environmental Health & Engineering, Bloomberg School of Public Health; Johns Hopkins Center for a Livable Future, Johns Hopkins University, Baltimore, MD.
Esther Nguyen, Center for Public Health Nutrition, University of Washington, Seattle, WA.
Punam Ohri-Vachaspati, College of Health Solutions, Arizona State University, Phoenix, AZ.
Abigail Orbe, Institute for Hunger Research & Solutions, Connecticut Food Bank/Foodshare, Bloomfield, CT.
Jennifer J Otten, Department of Environmental and Occupational Health Sciences, University of Washington, Seattle, WA.
Sondra Parmer, Alabama Cooperative Extension System, Auburn University, Auburn, AL.
Salome Pemberton, Hunter College, City University of New York, New York, NY.
Zain Al Abdeen Qusair, Master of Public Health Program, College of Liberal Arts and Social Sciences, DePaul University, Chicago, IL.
Victoria Rivkina, Master of Public Health Program, College of Liberal Arts and Social Sciences, DePaul University, Chicago, IL.
Joelle Robinson, Department of Health, Behavior and Society, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD.
Chelsea M Rose, Department of Epidemiology, University of Washington, Seattle, WA.
Saloumeh Sadeghzadeh, School of Management, Binghamton University, Binghamton, NY.
Brinda Sivaramakrishnan, Health, Business, & Professional Services, Tacoma Community College, Tacoma, WA.
Mariana Torres Arroyo, Department of Environmental Health Sciences, University at Albany- State University of New York, Rensselaer, NY.
McKenna Voorhees, Department of Nutrition, Dietetics and Food Sciences, Utah State University, Logan, UT.
Kathryn Yerxa, Cooperative Extension, University of Maine, Orono, ME.
References
- 1. WHO coronavirus (COVID-19) dashboard. [Internet]. 2020–2021; [cited 7 October, 2021]. Available from: https://covid19.who.int. [Google Scholar]
- 2. World Health Organization (WHO) . [Internet]. Timeline: WHO's COVID-19 response. 2021[cited 7 October, 2021]; Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline?gclid=Cj0KCQjw38-DBhDpARIsADJ3kjn0CXSKxbndgAdwrXTCf1_VkG_S57hl4sbxqJ6SYw92H9JJlp3KrckaAs8FEALw_wcB#. [Google Scholar]
- 3. Ahmad FB, Cisewski JA, Miniño A, Anderson RN. Provisional mortality data – United States, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(14):519–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Falk G, Carter JA, Nicchitta IA, Nyhof EC, Romero PD. Unemployment rates during the COVID-19 pandemic: In Brief 2021. [Internet]. 2021[cited 8 October, 2021]; Available from: https://fas.org/sgp/crs/misc/R46554.pdf. [Google Scholar]
- 5. Center on Budget Policy and Priorities (CBPP) [Internet]. Tracking the COVID-19 Recession's Effects on Food, Housing, and Employment Hardships. 2021[cited 7 October, 2021]; Available from: https://www.cbpp.org/research/poverty-and-inequality/tracking-the-covid-19-recessions-effects-on-food-housing-and. [Google Scholar]
- 6. Center on Budget Policy and Priorities (CBPP). [Internet]. Chart book: the legacy of the Great Recession. 2019[cited 7 October, 2021]; Available from: https://www.cbpp.org/research/economy/the-legacy-of-the-great-recession#:∼:text=Technically%2C%20the%20recession%20ended%20in,the%20recession%2C%20until%20late%202015. [Google Scholar]
- 7. Chenarides L, Manfredo M, Richards TJ. COVID-19 and food supply chains. Appl Econ Perspect Policy. 2021;43(1):270–9. [Google Scholar]
- 8. Loopstra R, Tarasuk V. Severity of household food insecurity is sensitive to change in household income and employment status among low-income families. J Nutr. 2013;143(8):1316–23. [DOI] [PubMed] [Google Scholar]
- 9. Alesch DJ, Arendt LA, Holly JN. Managing for Long-Term Community Recovery in the Aftermath of Disaster. Fairfax, Virginia: Public Entity Risk Institute; 2009. [Google Scholar]
- 10. Haas JE, Kates R, Bowden MJ. Reconstruction Following Disaster. Cambridge, MA and London, UK: The MIT Press; 1977. [Google Scholar]
- 11. Johnson LA, Hayashi H. Synthesis efforts in disaster recovery research. Int J Mass Emerg Disasters. 2012;30(2):212–38. [Google Scholar]
- 12. Esnard AM, Sapat A. Population/Community Displacement. Handbook of Disaster Research. Cham: Springer; 2018. p. 431–46. [Google Scholar]
- 13. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2018, ERR-270, U.S. Department of Agriculture, Economic Research Service. 2019. [Google Scholar]
- 14. Thomas DSK, Phillips BD, Lovekamp WE, Fothergill A. Social Vulnerability to Disasters. 2nd ed. Boca Raton FL: CRC Press; 2013. [Google Scholar]
- 15. Wolfson JA, Leung CW. Food insecurity during COVID-19: an acute crisis with long-term health implications. Am J Public Health. 2020;110(12):1763–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. United Nations Food and Agriculture Organization (FAO) . [Internet]. An Introduction to the Basic Concepts of Food Security. 2008[cited 7 October, 2021]; Available from: http://www.fao.org/3/a-al936e.pdf. [Google Scholar]
- 17. Clay LA, Papas MA, Gill KB, Abramson DM. Factors associated with continued food insecurity among households recovering from Hurricane Katrina. Int J Environ Res Public Health. 2018;15(8):1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nord M, Coleman-Jensen A, Andrews M, Carlson S. Household food security in the United States, 2009, ERR-108, U.S. Department of Agriculture. Econ Res Serv. 2010. [Google Scholar]
- 19. Marchione TJ. Foods provided through U.S. government emergency food aid programs: policies and customs governing their formulation, selection and distribution. J Nutr. 2002;132(7):2104S–11S. [DOI] [PubMed] [Google Scholar]
- 20. Clay LA, Ross AD. Factors associated with food insecurity following Hurricane Harvey in Texas. Int J Environ Res Public Health. 2020;17(3):762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Food Research and Action Center (FRAC) . [Internet]. Defining food insecurity and measuring it during COVID-19. 2021; [cited 7 October 2021]; Available from: https://frac.org/wp-content/uploads/Defining-Food-Insecurity_2021.pdf. [Google Scholar]
- 22. Feeding America . [Internet]. The impact of the coronavirus on food security in 2020 & 2021. 2021; [cited 8 October 2021]; Available from: https://www.feedingamerica.org/research/coronavirus-hunger-research. [Google Scholar]
- 23. Gundersen C, Hake M, Dewey A, Engelhard E. Food insecurity during COVID-19. Appl Econ Perspect Policy. 2021;43(1):153–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. United States Census Bureau . [Internet]. Week 1 household pulse survey: April 23 – May 5. 2020–2021; [cited 7 October 2021]; Available from: https://www.census.gov/data/tables/2020/demo/hhp/hhp1.html. [Google Scholar]
- 25. Fitzpatrick KM, Harris C, Drawve G, Willis DE. Assessing food insecurity among US adults during the COVID-19 pandemic. J Hunger Environ Nutr. 2021;16(1):1–18. [Google Scholar]
- 26. American Journal of Managed Care . [Internet]. A timeline of COVID-10 developments in 2020. 2021; [cited 7 October 2021]; Available from: https://www.ajmc.com/view/a-timeline-of-covid19-developments-in-2020. [Google Scholar]
- 27. United States Department of Agriculture Food and Nutrition Service . [Internet]. SNAP COVID-19 emergency allotments guidance. 2021; [cited 21 October 2021]; Available from: https://www.fns.usda.gov/snap/covid-19-emergency-allotments-guidance. [Google Scholar]
- 28. United States Census Bureau . [Internet]. Measuring household experiences during the coronavirus pandemic. 2021; [cited 7 October 2021]; Available from: https://www.census.gov/data/experimental-data-products/household-pulse-survey.html. [Google Scholar]
- 29. Niles MT, Neff R, Biehl E, Bertmann F, Morgan EH, Wentworth T. Food access and security during coronavirus survey- version 1.0.V2 ed: harvard dataverse; 2020. [Google Scholar]
- 30. Niles MT, Bertmann F, Belarmino EH, Wentworth T, Biehl E, Neff R. The early food insecurity impacts of COVID-19. Nutrients. 2020;12(7):2096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Niles MT, Neff R, Biehl E, Bertmann F, Belarmino EH, Acciai F, Ohri-Vachaspati P. Food access and food security during COVID-19 survey- version 2.1. V3 ed: harvard dataverse; 2020. [Google Scholar]
- 32. United States Department of Agriculture Economic Research Service. U.S. Household Food Security Survey Module: Six-Item Short Form. [Internet]. 2012–2021; [cited 7 October 2021]; Available from: . [Google Scholar]
- 33. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC; 2019. [Google Scholar]
- 34. Jaccard J, Becker MA, Wood G. Pairwise multiple comparison procedures: a review. Psychol Bull. 1984;96(3):589–96. [Google Scholar]
- 35. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2019. United States Department of Agriculture (USDA) Economic Research Service, 2020. [Google Scholar]
- 36. Morales DX, Morales SA, Beltran TF. Racial/ethnic disparities in household food insecurity during the COVID-19 pandemic: a nationally representative study. J Racial Ethn Health Disparities. 2021;8(5):1300–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Schanzenbach D, Pitts A. Food Insecurity During COVID-19 in Households with Children: Results by Racial and Ethnic Groups. [Internet]. Institute for Policy Research, Northwestern University; 2020–2021; [cited 8 October, 2021]; Available from: https://www.ipr.northwestern.edu/documents/reports/ipr-rapid-research-reports-pulse-hh-data-9-july-2020-by-race-ethnicity.pdf. [Google Scholar]
- 38. Schanzenbach D, Pitts A. Food Insecurity in the Census Household Pulse Survey Data Tables. [Internet]. Institute for Policy Research, Northwestern University; 2020–2021; [cited 7 October 2021]; Available from: https://www.ipr.northwestern.edu/documents/reports/ipr-rapid-research-reports-pulse-hh-data-1-june-2020.pdf. [Google Scholar]
- 39. Adams EL, Caccavale LJ, Smith D, Bean MK. Longitudinal patterns of food insecurity, the home food environment, and parent feeding practices during COVID-19. Obes Sci Pract. 2021;7(4):415–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Dubowitz T, Dastidar MG, Troxel WM, Beckman R, Nugroho A, Siddiqi S, Cantor J, Baird M, Richardson AS, Hunter GPet al. . Food insecurity in a low-income, predominantly African American cohort following the COVID-19 pandemic. Am J Public Health. 2021;111(3):494–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2020. USDA-ERS Report No. ERR-298, U.S. Department of Agriculture, Economic Research Service. 2021. [Google Scholar]
- 42. Bartfeld J, Men F. Food insecurity among households with children: the role of the state economic and policy context. Soc Serv Rev. 2017;91(4):691–732. [Google Scholar]
- 43. Rocco P, Béland D, Waddan A. Stuck in neutral? Federalism, policy instruments, and counter-cyclical responses to COVID-19 in the United States. Policy Soc. 2020;39(3):458–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. United States Department of Agriculture Food and Nutrition Service . [Internet]. SNAP: COVID-19 Waivers by State. 2021; [cited 7 October 2021]; Available from: https://www.fns.usda.gov/disaster/pandemic/COVID-19/snap-waivers-flexibilities. [Google Scholar]
- 45. Lauren BN, Silver ER, Faye AS, Rogers AM, Woo-Baidal JA, Ozanne EM, Hur C. Predictors of households at risk for food insecurity in the United States during the COVID-19 pandemic. Public Health Nutr. 2021;24(12):3929–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kimani ME, Sarr M, Cuffee Y, Liu C, Webster NS. Associations of race/ethnicity and food insecurity with COVID-19 infection rates across US counties. JAMA Network Open. 2021;4(6):e2112852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Schanzenbach D, Pitts A. Estimates of Food Insecurity during the COVID-19 Crisis: Results from the COVID Impact Survey, Week 1 (April 20–26, 2020). [Internet]. Institute for Policy Research, Northwestern University, 2020–2021; [cited 8 October 2021]. Available from: https://www.ipr.northwestern.edu/documents/reports/food-insecurity-covid_week1_report-13-may-2020.pdf. [Google Scholar]
- 48. Perry BL, Aronson B, Pescosolido BA. Pandemic precarity: COVID-19 is exposing and exacerbating inequalities in the American heartland. PNAS. 2021;118(8):e2020685118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Swinburne M. Chapter 28: using SNAP to address food insecurity during the COVID-19 pandemic. In: Burris S, de Guia S, Gable L, Levin DE, Parmet WE, Terry NP, editors. COVID-19 Policy Playbook: Legal Recommendations for a Safer, More Equitable Future. Boston; Public Health Law Watch: 2021. p. 170–3. [Google Scholar]
- 50. Chilton M, Rose D. A rights-based approach to food insecurity in the United States. Am J Public Health. 2009;99(7):1203–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lima MC, Eickmann SH, Lima AC, Guerra MQ, Lira PI, Huttly SR, Ashworth A. Determinants of mental and motor development at 12 months in a low income population: a cohort study in northeast Brazil. Acta Paediatr. 2004;93(7):969–75. [DOI] [PubMed] [Google Scholar]
- 52. Chilton M, Chyatte M, Breaux J. The negative effects of poverty & food insecurity on child development. Indian J Med Res. 2007;126(4):262–72. [PubMed] [Google Scholar]
- 53. Rose-Jacobs R, Black MM, Casey PH, Cook JT, Cutts DB, Chilton M, Heeren T, Levenson SM, Meyers AF, Frank DA. Household food insecurity: associations with at-risk infant and toddler development. Pediatrics. 2008;121(1):65–72. [DOI] [PubMed] [Google Scholar]
- 54. Bauer L, Broady K, Edelberg W, O'Donnell J. Ten facts about COVID-19 and the U.S. economy. [Internet].Brookings;2021; [cited 7 October 2021]. Available from: https://www.brookings.edu/research/ten-facts-about-covid-19-and-the-u-s-economy/. [Google Scholar]
- 55. Ohri-Vachaspati P, Acciai F, Martinelli S, Harper K, Bertmann FM, Belarmino E, Neff R, Niles M. Food assistance program participation among US households during the COVID-19 pandemic. [Internet]. 2020–21[cited 7 October, 2021]. Available from: https://keep.lib.asu.edu/_flysystem/fedora/2021-04/food-assistance-program-participation-among-us-household-during-covid_final_dec-2020.pdf(Accessed 28 May, 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Berkowitz SA, Basu S. Unmet social needs and worse mental health after expiration of COVID-19 federal pandemic unemployment compensation. Health Aff. 2021;40(3):426–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Gaitan-Rossi P, Vilar-Compte M, Teruel G, Perez-Escamilla R. Food insecurity measurement and prevalence estimates during the COVID-19 pandemic in a repeated cross-sectional survey in Mexico. Public Health Nutr. 2021;24(3):412–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Hernandez DC, Holtzclaw LE. Commentary: the impact of the COVID-19 pandemic and the economic recession on food insecurity: short- and long-term recommendations to assist families and communities. Fam Community Health. 2021;44(2):84–6. [DOI] [PubMed] [Google Scholar]
- 59. Clay LA, Papas MA, Gill KB, Abramson DM. Application of a theoretical model toward understanding continued food insecurity post Hurricane Katrina. Disaster Med Public Health Prep. 2018;12(1):47–56. [DOI] [PubMed] [Google Scholar]
- 60. Njai R, Siegel P, Yin S, Liao Y. Prevalence of Perceived Food and Housing Security – 15 States, 2013. 13 January, 2017. Report No.: 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Parekh N, Ali SH, O'Connor J, Tozan Y, Jones AM, Capasso A, Foreman J, DiClemente RJ. Food insecurity among households with children during the COVID-19 pandemic: results from a study among social media users across the United States. Nutr J. 2021;20(1):73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Davidson AR, Morrell JS. Food insecurity prevalence among university students in New Hampshire. Journal of Hunger & Environmental Nutrition. 2020;15(1):118–27. [Google Scholar]
- 63. Flynn MM, Monteiro K, George P, Tunkel AR. Assessing food insecurity in medical students. Fam Med. 2020;52(7):512–3. [DOI] [PubMed] [Google Scholar]
- 64. Kelfve S, Kivi M, Johansson B, Lindwall M. Going web or staying paper? The use of web-surveys among older people. BMC Med Res Method. 2020;20(1):252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Pew Research Center. [Internet]. Internet Broadband Factsheet; 2021; [cited 8 October 2021]; Available from: https://www.pewresearch.org/internet/fact-sheet/internet-broadband/. [Google Scholar]
- 66. Voegels E (Pew Research Center). Some divides persist between rural, urban and surburban America. 2021; [Internet]. [cited 8 October 2021]:Available from: https://www.pewresearch.org/fact-tank/2021/08/19/some-digital-divides-persist-between-rural-urban-and-suburban-america/. [Google Scholar]
- 67. Nikolaus CJ, Ellison B, Nickols-Richardson SM. Food insecurity among college students differs by questionnaire modality: an exploratory study. Am J Health Behav. 2020;44(1):82–9. [DOI] [PubMed] [Google Scholar]
- 68. Pérez-Escamilla R, Vilar-Compte M, Gaitan-Rossi P. Why identifying households by degree of food insecurity matters for policymaking. Glob Food Sec. 2020;26:100459. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.