HIGHLIGHTS
-
•
All groups experienced notable disruption in health care utilization.
-
•
Disruption in care for traumatic brain injury or mental health was associated with decreased health-related quality of life.
-
•
Telehealth was a viable alternative to in-person visits.
-
•
Telehealth is not a panacea and should be adopted using a nuanced approach.
KEYWORDS: Brain injuries, traumatic; COVID-19; Healthcare disparities; Patient acceptance of health care; Quality of life; Rehabilitation; Stroke; Telemedicine
List of abbreviations: ABI, acquired brain injury; ANOVA, analysis of variance; HRQoL, health-related quality of life; TBI, traumatic brain injury
Abstract
Objective
To delineate health care disruption for individuals with acquired brain injury (ABI) during the peak of the pandemic and to understand the impact of health care disruption on health-related quality of life (HRQoL).
Design
Cross-sectional survey.
Setting
General community.
Participants
Volunteer sample of adults with traumatic brain injury (TBI; n=33), adults with stroke (n=66), and adults without TBI or stroke (n=108) with access to the internet and personal technology (N=207).
Interventions
Not applicable.
Main Outcome Measures
Not applicable.
Results
Participants with TBI and stroke reported high rates of disruption in care specific to their diagnosis (53%-54.5%), while participants across all groups reported disruption for major medical care (range, 68.2%-80%), general health care (range, 60.3%-72.4%), and mental health care (range, 31.8%-83.3%). During the pandemic, participants with TBI and stroke used telehealth for care specific to their diagnosis (40.9%-42.4%), whereas all participants used telehealth for major medical care (range, 50%-86.7%), general health care (range, 31.2%-53.3%), and mental health care (range, 53.8%-72.7%). Disruption in TBI or stroke care and type of ABI explained 27.1% of the variance in HRQoL scores (F2,95=16.82, P<.001, R2=0.262), and disruption in mental health care explained 14.8% of the variance (F1,51=8.86, P=.004, R2=0.148).
Conclusions
Individuals with and without ABI experienced pronounced disruption in health care utilization overall. However, individuals who experienced a disruption in care specific to TBI or mental health care were most vulnerable to decreased HRQoL. Telehealth was a viable alternative to in-person visits for individuals with and without ABI, but limitations included difficulty with technology, difficulty with comprehensive examination, and decreased rapport with providers.
The global SARS-CoV-2 (COVID-19) pandemic has resulted in government-issued lockdowns, social distancing, and stay-at-home orders.1 These public health measures to decrease the spread of COVID-19 upended patterns of work, school attendance, and participation in everyday activities, resulting in profound secondary consequences for both general and vulnerable populations.2
Over the past year, health care systems were overburdened because of the high rates of patients with COVID-19, which disrupted access and use of both urgent and nonurgent health care utilization across clinical services.3, 4, 5, 6, 7, 8, 9, 10 Individuals with acquired brain injury (ABI), such as traumatic brain injury (TBI) and stroke, may be particularly vulnerable to disruption or changes to health care utilization because of ongoing health care needs. TBI is the leading cause of long-term disability in individuals younger than 40 years, characterized by impairment in cognition (especially memory and executive function), depressed mood, and behavioral issues.11 Stroke is the leading cause of serious long-term disability for older adults.12 Common symptoms include upper and lower hemiparesis, decreased sensation, hemi-inattention, difficulty with speech and swallowing, changes in vision, and depression.12, 13, 14 While individuals with TBI and stroke may have distinct clinical symptoms, both groups experience decreased participation in activities of daily living, leisure activities, and work, which can adversely affect quality of life.15, 16, 17
Studies focused on the impact of the COVID-19 pandemic on populations with ABI are emerging. There was a persistent decline in acute hospitals admissions and emergency care visits for the management of stroke symptoms.18,19 Individuals with TBI identified health care professionals as trusted sources for information on COVID-19, and they reported mental health changes and social isolation as barriers to coping with the pandemic.20 Community-dwelling individuals with brain injury in the United Kingdom reported increased anxiety (64%), a negative effect on their mental health (60%), and a disruption in rehabilitation care (42%) because of the pandemic.21
Much of the current literature for stroke focus on changes to health care and rehabilitation delivery models for patients in the inpatient hospital setting and discharge planning.22, 23, 24, 25 There is much less research published on TBI. Additional research is needed on community-dwelling individuals with stroke and TBI to better understand the disruption in health care utilization patterns (eg, disruption in different types health care, adoption of alternate telehealth strategies) and how these changes in health care utilization may affect quality of life. Therefore, the aims of this study were to delineate the health care utilization patterns during the peak of the pandemic and the effect of the changes in health care utilization on health-related quality of life (HRQoL).
Methods
Design
This was a cross-sectional survey study investigating the effect of the COVID-19 pandemic on individuals with and without neurologic injury.
Recruitment
Institutional review board approval was acquired at the primary research site. Individuals provided consent before the completion of a self-administered online survey in Research Electronic Data Capture. All groups were recruited from social media posts (Facebook) and study flyers. Additional recruitment methods for participants with TBI and stroke included email outreach to local neurologic clinical departments and existing stroke research registries from 2 research sites. All potential participants were directed to an online link containing information about the study. Potential participants independently completed screening questions and provided written consent to proceed to the study questions. Participants with ABI were included if they were older than 18 years, had a diagnosis of stroke or TBI, and were living in the community. They were excluded if they had neurologic conditions other than TBI or stroke (eg, Parkinson disease) or a diagnosis of mental illness (eg, bipolar disorder, schizophrenia). Participants without ABI were included if they were older than 18 years and living in the community. They were excluded if had a history of neurologic conditions or mental illness. All participants who completed the survey were entered into a raffle for an Amazon gift card.
Data collection
Data collection was conducted between August and November 2020. No surveys existed at the time of study inception related to the effects of the pandemic on individuals with brain injury. Therefore, the study survey was composed of customized demographic questions and items from preexisting COVID-19–specific surveys recommended by the National Institutes of Health Office of Behavioral and Social Sciences Research (https://www.nlm.nih.gov/dr2/COVID-19_BSSR_Research_Tools.pdf). Language was adjusted for some of the preexisting survey items in to address neurologic groups. The survey took approximately 30-40 minutes to complete.
The current study focused on questions related to demographics, medical history, COVID-19 exposure, health care utilization, and HRQoL. Binary (yes/no) questions were asked to describe the presence of neurologic symptoms or prior psychosocial history. The COVID-19 Experiences subsection of the COVID-19: Impact of the Pandemic and Health Related Quality of Life in Cancer Patients and Survivors Scale (F. J. Penedo et al, unpublished data, 2020) consists of 12 items related to COVID-19 exposure. Example questions included items such as “have you been tested for COVID-19” and “If you tested positive, did you have symptoms.”
Twenty-two items related to health care utilization were modified from the COVID-19 Experiences subscale of the COVID-19: Impact of the Pandemic and Health-Related Quality of Life in Cancer Patients and Survivors Scale and Coronavirus Impact Scale (https://doi.org/10.31234/osf.io/kz4pg). Binary questions (yes/no) regarding health utilization for TBI- or stroke-specific care, major medical care, general health care, and mental health care were asked. Questions included items such as “Have you missed care related to your diagnosis,” “Have you experienced a delay in care related to major medical issues,” and “Did you attend telehealth for care related to mental health?” Frequencies were calculated for individual items. Scores from “delayed appointments” and “missed appointments” items were combined to create a composite item called “health care disruption” representing missed or delayed appointments. Degree of satisfaction for telehealth appointments were rated on a 5-point ordinal scale ranging from 1 (very dissatisfied) to 5 (very satisfied).
The HRQoL subscale of the COVID-19: Impact of the Pandemic and Health-Related Quality of Life in Cancer Patients and Survivors Scale consists of 7 items related to health-related symptoms experienced during the pandemic.26 Items were rated on a 5-point ordinal scale ranging from 1 (not at all) to 5 (very much). Participants indicated the presence of any listed symptoms (eg, lack of energy, pain, sleeping difficulty). Four of the 7 items were reverse coded and adjusted before analysis. Group mean scores were calculated for each item, and a composite score was calculated by taking the sum of the 7 items, with higher scores indicating greater HRQoL.
Analysis
Descriptive statistics were used to summarize participant characteristics, and frequencies were used for health utilization items. Analysis of variance (ANOVA), chi-square, and Fisher exact tests were used to compare differences between groups. Nonparametric alternatives (Kruskal-Wallis, Welch ANOVA) were used when data were not normally distributed or the variances were not equal between groups. Alpha level was set at 0.05. We used linear regression models to examine the relationship between health care disruption (independent variable) and HRQoL composite scores (dependent variable). A separate model was run for each type of health care disruption (TBI or stroke care, major medical issue, general health care and mental health care). Regression diagnostics were examined to verify the assumptions of heteroscedasticity and normality of residuals. To control for the type I error rate among the regressions, we used the Benjamini-Hochberg method27 to control the false discovery rate. Similarly, after significant omnibus tests, post hoc tests were conducted using Bonferroni correction for parametric ANOVA and Dunnett T3 for Welch ANOVA. All analyses were conducted using SPSS v 27.a
Results
Participants
See table 1 for detailed description of all baseline participant characteristics. A total of 207 participants completed the questionnaire, with a subset of 33 in the TBI group, 66 in the stroke group, and 108 in the group without ABI. Because we used social media posts for recruitment, we had a small percentage of participants complete the survey from outside of the United States. The countries of residence for the ABI group were the United States (91.9%), Canada (4%), United Kingdom (2%), Greece (1%), and Ghana (1%). For the group without ABI, the countries of residence were the United States (90.7%), Israel (8.3%), and Ghana (0.9%). Mean age for the entire sample was 47.8 years. Stroke group (55 years) was significantly older than the TBI group (45.7 years) and the group without ABI (42.7 years). Participants in the stroke group had higher ratio of men (54.5%) compared with the TBI group (30.3%) and group without ABI (17.6%). Participants in all groups were predominantly White, and more than 85% were educated at the college level (some college, undergraduate or graduate degree). The group without ABI reported higher employment rate than the stroke and TBI groups (P<.001). More participants in the TBI group were in the lowest financial bracket compared with the stroke group and group without ABI (P<.001).
Table 1.
Participant demographics before the pandemic (N=207)
| Variable | Traumatic Brain Injury(n=33) | Stroke(n=66) | Without ABI(n=108) | P Value |
|---|---|---|---|---|
| Age, mean ± SD (y) | 45.7±12.8 | 55.0±16.8 | 42.7±14.8 | <.001* |
| Sex, n (%) | <.001† | |||
| Female | 23 (69.7) | 28 (42.4) | 88 (81.5) | |
| Male | 10 (30.3) | 36 (54.5) | 19 (17.6) | |
| Other | 0 (0.0) | 2 (3.0) | 1 (0.9) | |
| Race, n (%) | NS | |||
| Asian | 3 (9.1) | 4 (6.1) | 8 (7.4) | |
| Black | 1 (3.0) | 8 (12.1) | 9 (8.3) | |
| Hispanic/Latino | 0 (0.0) | 0 (0.0) | 2 (1.8) | |
| White | 26 (78.8) | 52 (78.8) | 84 (77.8) | |
| Other | 3 (9.1) | 2 (3.0) | 5 (4.6) | |
| Education, n (%) | NS | |||
| Grade school | 1 (3.0) | 2 (3.0) | 0 (0.0) | |
| High school | 1 (3.0) | 5 (7.5) | 8 (7.4) | |
| Some college/undergraduate | 20 (60.7) | 31 (46.9) | 52 (48.1) | |
| Graduate degree | 11 (33.3) | 27 (40.9) | 48 (44.4) | |
| Other | 0 (0.0) | 1 (1.5) | 0 (0.0) | |
| Marital status, n (%) | NS | |||
| Married/unmarried couple | 17 (51.5) | 32 (48.5) | 63 (58.3) | |
| Divorced/separated/widowed | 3 (9.1) | 5 (7.6) | 10 (9.2) | |
| Never married | 11 (33.3) | 27 (40.9) | 31 (28.7) | |
| Other | 2 (6.1) | 2 (3.0) | 4 (3.7) | |
| Household number, mean ± SD‡ | 2.3±1.3 | 2.3±1.4 | 3.1±1.5 | .002* |
| Household income, n (%) | <.001§ | |||
| <$25,000 | 9 (27.3) | 2 (3.0) | 9 (8.3) | |
| $25,000-$49,000 | 6 (18.2) | 10 (15.2) | 15 (13.9) | |
| $50,000-$74,000 | 2 (6.1) | 15 (22.7) | 4 (3.7) | |
| ≥$75,000 | 10 (30.3) | 30 (45.5) | 70 (64.8) | |
| Other | 6 (18.2) | 9 (13.6) | 10 (9.3) | |
| Employment, n (%) | 11 (33.3) | 18 (27.3) | 69 (63.9) | <.001§ |
| Psychosocial history, n (%) | ||||
| Depression | 17 (51.5) | 11 (16.7) | 14 (13.0) | <.001§ |
| Anxiety | 15 (45.5) | 11 (16.7) | 14 (13.0) | <.001§ |
| Time post injury, mean ± SD (y)‖ | 13.2±11.7 | 8.8±5.4 | - | .014¶ |
| TBI/stroke functional status, n (%) | ||||
| UE limitations | 14 (42.4) | 55 (83.3) | - | <.001§ |
| LE limitations | 14 (42.4) | 57 (86.4) | - | <.001§ |
| Visual disturbance | 16 (48.5) | 12 (18.2) | - | .002§ |
| Speech problems | 14 (42.4) | 10 (15.2) | - | .003§ |
| Seizures | 3 (9.1) | 9 (13.6) | - | NS |
| Annual care, n (%) | ||||
| TBI/stroke care | 27 (84.4) | 45 (72.6) | - | NS |
| Major medical issues | 15 (55.6) | 31 (49.2) | 22 (23.7) | .001§ |
| General medical issues | 30 (90.9) | 58 (89.2) | 93 (86.9) | NS |
| Mental health | 18 (62.1) | 13 (22.4) | 22 (22.7) | <.001§ |
Abbreviations: LE, lower extremity; NS, nonsignificant; UE, upper extremity.
ANOVA.
Fisher exact test.
Missing data (n=4).
χ2 test.
Missing data (n=5).
Independent groups t test.
Prior functional history for stroke and TBI
Time post injury was chronic for both the stroke (8.8 years) and TBI (13.2 years) groups. The TBI group reported higher rates of visual and speech difficulties than the stroke group (P=.002, P=.003, respectively). The stroke group reported more upper and lower extremity limitations than the TBI group (P<.001).
Prior psychosocial history
Prior to the pandemic, the TBI and stroke groups reported greater use of major medical care than the group without ABI (P=.001). The TBI group reported greater prepandemic depression, anxiety, and use of mental health care than the stroke group and group without ABI (P<.001).
COVID-19 testing and positivity rates
Rates for getting tested for COVID-19 were similar across groups: 33.3% (TBI), 36.4% (stroke), and 39.8% (without ABI). The most common reason across all groups for not being tested was “experiencing no symptoms”: 48.5% (TBI), 43.9% (stroke), and 45.4% (without ABI). Of those tested for COVID-19, the positivity rates were 18.2% (TBI), 12.5% (stroke), and 4.7% (without ABI). Hospitalization rates for those who tested positive ranged from 50% (TBI), 33.3% (stroke), and 0% (without ABI).
Health care utilization during the peak of the pandemic
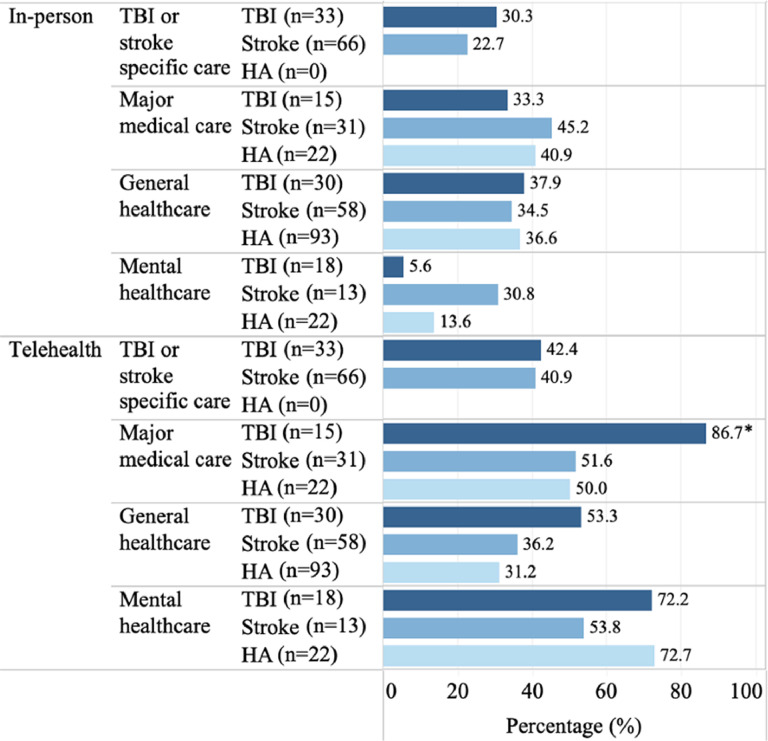
See Fig 1, Fig 2 for visual summary of health care disruption and utilization patterns for care specific to TBI or stroke diagnosis, major medical care, general health care, and mental health care. More than half of participants who experienced a TBI or stroke reported disruption in care specific to their diagnosis (53%-54.5%). Participants across all groups reported health care disruption for major medical care (range, 68.2%-80%), general health care (range, 60.3.%-70%), and mental health care (range, 31.8%-83.3%). Members of the TBI group reported greater frequency of disruption in mental health care than the stroke group and group without ABI (P=.003). Participants in the stroke and TBI groups reported attending telehealth for care specific to their diagnosis (range, 40.9%-42.4%), while all participants reported using telehealth for major medical care (range, 50%-86.7%), general health care (range, 31.2%-53.3%), and mental health care (range, 53.8%-72.7%). Members of the TBI group reported greater frequency of telehealth use for major medical care than the stroke group and group without ABI (P=.046).
Fig 1.
Health care disruption during the pandemic for TBI group, stroke group, and group without ABI. Health care disruption: missed or delayed appointments, variable group sample sizes reflect the number of participants that indicated participation in each type of health care. *Significantly higher for TBI group than stroke group and group without ABI (P<.05).
Fig 2.
Health care utilization during the pandemic for in-person and telehealth visits for TBI group, stroke group, and group without ABI. Variable group sample sizes reflect participants who indicated participation in each type of health care. *Significantly higher for TBI group than stroke group and group without ABI (P<.05). †Missing data (n=1).
Mean telehealth satisfaction ratings across all groups ranged from 3.63-4.07 (TBI or stroke care), 3.69-3.92 (major medical care), 3.81-3.94 (general health care), and 3.69-4.29 (mental health care). There were no differences between groups in satisfaction with telehealth visits. A subset of participants (n=43) provided open-ended responses for being satisfied or dissatisfied with telehealth appointments. The most frequent reasons for satisfaction with telehealth across all groups included convenience, able to address patient needs, good for routine visits. Most frequent reasons for dissatisfaction with telehealth across all groups included technical difficulties, less comprehensive examination (limitations with physical examination or thorough diagnosis), and less sense of connection with provider. All satisfied and dissatisfied responses were summarized in fig 3.
Fig 3.
Self-reported reasons for telehealth satisfaction/dissatisfaction in TBI group, stroke group, and group without ABI (n=43). For Convenient category, participant responses included: easy, fast, appointment starts on time, and more appointment availability. For Routine visits category, participant responses included: requesting COVID-19 test, diagnosis, medication prescription, follow-ups. For Safe category, participant responses included decrease the risk of infection. For Difficulties with technology category, participant responses included: inaccessible technology, poor internet connection, no technical assistance, and technical issues. For Noncomprehensive examination, category, participant responses included: not able to cover all needs, limited physical examination, difficulties with diagnosis, and limitations on what health care providers can see via a video call.
(1) All groups experienced notable disruption in health care utilization. (2) Disruption in care for traumatic brain injury or mental health was associated with decreased health-related quality of life. (3) Telehealth was a viable alternative to in-person visits. (4) Telehealth is not a panacea and should be adopted using a nuanced approach.
Health-related quality of life
See table 2 for detailed description of individual and composite items. Based on composite scores, the TBI group reported lower overall HRQoL than the stroke group and group without ABI (P<.001).
Table 2.
HRQoL during COVID-19 pandemic (N=207)
| Variable, mean ± SD | Traumatic Brain Injury*(n=33) | Stroke† (n=66) | Without ABI‡(n=108) | P Value | |
|---|---|---|---|---|---|
| Lack of energy§ | 2.91†±1.31 | 3.58*±1.04 | 3.21±1.10 | .015‖ | |
| Pain§ | 3.24†,‡±1.28 | 3.92*±1.33 | 4.35*±1.00 | <.001¶ | |
| Nausea§ | 4.24±0.97 | 4.64±0.84 | 4.58±0.83 | NS | |
| Worry condition will get worse§ | 3.52†,‡±1.37 | 4.24*±1.05 | 4.35*±1.04 | .008¶ | |
| Sleeping well | 2.36†,‡±1.22 | 3.42*±1.35 | 3.12*±1.10 | .001¶ | |
| Able to enjoy life | 2.73†±1.07 | 3.46*±0.99 | 3.19±0.92 | .002‖ | |
| Content with QoL right now | 2.33†,‡±1.14 | 3.11*±1.13 | 3.19*±1.02 | <.001‖ | |
| Composite score# | 21.33†,‡±5.73 | 26.38*±5.20 | 25.99*±4.65 | <.001* | |
Abbreviations: NS, nonsignificant; QoL, quality of life.
Indicates other groups that differed significantly from that group mean.
Reverse-coded item.
ANOVA.
Welch ANOVA.
Possible range of scores: 7-35 (higher scores indicate better HRQoL).
Health care disruption and HRQoL
Results of the linear regression models are presented in table 3. Results from model 1 identified a significant relationship between disruption in TBI or stroke care and the type of ABI with care disruption (F2,95=16.82, P<.001, R2=0.262), explaining 26.2% of the variance in HRQoL scores. Controlling for TBI and stroke care disruption, we found participants with TBI had on average HRQoL scores 5.03 points lower than participants with stroke (B=5.03, t=4.62, P<.001). In other words, participants with TBI had on average HRQoL scores 5.03 points lower than participants with stroke when they had the same experience of TBI or stroke care disruption. Controlling for type of ABI, we found those who experienced a disruption in TBI and stroke care had on average HRQoL scores 3.59 points lower than those who did not (B=−3.59, t=−3.48, P<.001).
Table 3.
Results of linear regression models predicting HRQoL
| Model | Dependent Variable: HRQoL |
||||||
|---|---|---|---|---|---|---|---|
| Health Care Disruption | Unstandardized Coefficient |
Standardized Coefficient |
t | P Value | R2 | ||
| B | SE | β | |||||
| 1 | ABI (0=TBI, 1=stroke) | 5.03 | 1.09 | 0.41 | 4.62 | <.001* | 0.262 |
| Care specific to TBI or stroke† | −3.59 | 1.03 | −0.31 | −3.48 | <.001* | ||
| 2 | Major medical care† | −2.60 | 1.60 | −0.20 | −1.63 | NS | 0.039 |
| 3 | General health care† | −0.81 | 0.85 | −0.07 | −0.96 | NS | 0.005 |
| 4 | Mental health care† | −4.30 | 1.45 | −0.39 | −2.98 | .004* | 0.148 |
Abbreviation: NS, nonsignificant.
Significant after B-H adjustment.
When independent variable is 0=no experience of disruption; when independent variable is 1=experience of disruption.
There was also a significant relationship between disruption in mental health care and HRQoL (F1,51=8.86, P=.004, R2=0.148), explaining 14.8 % of the variance in HRQoL scores. Those who experienced a disruption in mental health care had HRQoL scores that were on average 4.30 points lower than those who did not have a disruption (B=−4.30, t=−2.98, P=.004). Disruptions in major medical care and general health care were not associated with HRQoL.
Discussion
Participants across all groups experienced notable disruption in major medical and general care, mental health care, and diagnosis-specific care for TBI or stroke. However, there was a differential negative effect on HRQoL for individuals with ABI and for participants who received mental health care. For those who received TBI- or stroke-specific care, participants with TBI were more vulnerable to decreased HRQoL than the stroke group. While it is unclear why the participants in the stroke group had better outcomes, selection bias may have contributed to our results. The stroke group had greater financial resources and lower prepandemic anxiety and/or depression than the TBI group. Our TBI group also consisted of 70% women, while epidemiologic studies report that women in young adulthood represent about one-third of TBI hospital admissions.28 TBI outcomes research stratified by sex and gender are generally scarce; however, the existing studies indicate that women with TBI report increased mental health, posttraumatic stress disorder symptoms, and financial barriers compared with women without TBI.29,30 Further work may need to be done to explore the role of sex and financial resources on health outcomes for people with TBI during the pandemic.
Our results partially supported the existing literature that populations with neurologic conditions were particularly at risk of decreased HRQoL during the pandemic.31 We found this to be true particularly for the TBI group. Therefore, the delivery and utilization of health care to manage diagnosis specific care, particularly for TBI-related symptoms, must remain a priority to mitigate the negative effects on HRQoL and overall well-being. Participants with and without disability who experienced a disruption in mental health services were also vulnerable to experiencing a decrease in HRQoL. Our results reinforce the larger societal needs that mental health services must be prioritized and available for all individuals as the COVID-19 pandemic continues on globally.32, 33, 34
Participants across all groups used telehealth as an alternative to in-person visits for major and general medical care, mental health care, and diagnosis-specific care. This supports the literature on the rapid proliferation of telehealth service delivery across all types of health care service.4,35,36 Moreover, individuals with chronic disease within resource-rich environments received telehealth as a viable alternative and were satisfied with telehealth services.4,31 In support of the literature,37 our study participants reported that telehealth was convenient and safe, and they identified technical difficulties as the most common barrier for access to telehealth visits. Unique to our study, participants reported that telehealth was most beneficial for addressing general medical questions or for follow-up visits and was limited for visits requiring thorough evaluations, physical assessments, and establishing clinician-patient rapport.
Study limitations
Because of the time-sensitive nature of collecting data during the pandemic, there were several limitations for this study that may have contributed to selection and measurement bias. We used diverse recruitment methods to recruit self-selecting participants including social media posts, recruitment flyers, outreach to outpatient clinical departments, and stroke research registries. Only participants with access to personal technology and the internet were able to participate. Because this was a self-selecting sample, the overall sample size was small and not equal across groups, and participants were mostly White and well educated. Because this was not a representative sample, the results cannot be generalized to all individuals with ABI. Additionally, there were no published surveys at the time of study inception (summer 2020) related to the effects of the pandemic on individuals with brain injury. Therefore, we modified available surveys based on the population with cancer.
Future directions
Further research on the effects of the pandemic with larger and more heterogeneous sample of the community with ABI are warranted to expand the current study. Additional studies investigating the influence of sex on the effects of the pandemic for populations with TBI is also warranted. Telehealth and the use of mobile technology has emerged as a comparable and viable option for the delivery of neurorehabilitation.38,39 Telehealth utilization during the pandemic has been lower among individuals in marginalized communities (Black, Hispanic, Asian, immigrants/non-English speakers, low income), those in older age groups (older than 60 years), and those living in rural areas with less access to built-in structural hospital resources, the internet, and personal technology.40,41 Even for participants in our study who lived in resource-rich environments, limited structural access and technical difficulties were common reported barriers to use. To mitigate the existing health inequities for marginalized communities with ABI,42,43 future studies understanding the specific issues and barriers for telehealth use in vulnerable communities with ABI will be critical prior to general adoption.44
Conclusions
Individuals with and without disability living in the community experienced pronounced disruption in TBI- and stroke-specific care, health care related general and major medical care, and mental health care. However, those who experienced a disruption in care specific to TBI or mental health care were most vulnerable to decreased HRQoL. While people with ABI used telehealth as a viable alternative to in-person visits during the pandemic, it is not a panacea and should be adopted using a nuanced approach.
Supplier
-
a.
SPSS v 27; IBM.
Acknowledgments
We thank Michelle Chen and Amanda Botticello for RedCAP survey set up and administration.
Footnotes
This material has been accepted for an oral presentation at the American Occupational Therapy Association Conference, April 3, 2022, San Antonio, TX.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.arrct.2021.100176.
Appendix. Supplementary materials
References
- 1.Di Corrado D, Magnano P, Muzii B, et al. Effects of social distancing on psychological state and physical activity routines during the COVID-19 pandemic. Sport Sci Health. 2020 doi: 10.1007/s11332-020-00697-5. Sep 25 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holmes EA, O'Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walter J, Sellmer L, Kahnert K, et al. Daily routine and access to care: initial patient reported experiences at a german lung cancer center during the COVID-19 pandemic. Respiration. 2021;100:90–92. doi: 10.1159/000513849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kendzerska T, Zhu DT, Gershon AS, et al. The effects of the health system response to the COVID-19 pandemic on chronic disease management: a narrative review. Risk Manag Healthc Policy. 2021;14:575–584. doi: 10.2147/RMHP.S293471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chaiyachati BH, Agawu A, Zorc JJ, Balamuth F. Trends in pediatric emergency department utilization after institution of coronavirus disease-19 mandatory social distancing. J Pediatr. 2020;226:274–277. doi: 10.1016/j.jpeds.2020.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dopfer C, Wetzke M, Zychlinsky Scharff A, et al. COVID-19 related reduction in pediatric emergency healthcare utilization - a concerning trend. BMC Pediatr. 2020;20:427. doi: 10.1186/s12887-020-02303-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seidu S, Kunutsor SK, Cos X, Khunti K. Indirect impact of the COVID-19 pandemic on hospitalisations for cardiometabolic conditions and their management: a systematic review. Prim Care Diabetes. 2021;15:653–681. doi: 10.1016/j.pcd.2021.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shinan-Altman S, Levkovich I, Tavori G. Healthcare utilization among breast cancer patients during the COVID-19 outbreak. Palliat Support Care. 2020;18:385–391. doi: 10.1017/S1478951520000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liang Y, Chang C, Chen Y, Dong F, Zhang L, Sun Y. Symptoms, management and healthcare utilization of COPD patients during the COVID-19 epidemic in Beijing. Int J Chron Obstruct Pulmon Dis. 2020;15:2487–2494. doi: 10.2147/COPD.S270448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosencrans M, Arango P, Sabat C, et al. The impact of the COVID-19 pandemic on the health, wellbeing, and access to services of people with intellectual and developmental disabilities. Res Dev Disabil. 2021;114 doi: 10.1016/j.ridd.2021.103985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dang B, Chen W, He W, Chen G. Rehabilitation treatment and progress of traumatic brain injury dysfunction. Neural Plast. 2017;2017 doi: 10.1155/2017/1582182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. 2021;143:e254–e743. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 13.Lee KB, Lim SH, Kim KH, et al. Six-month functional recovery of stroke patients: a multi-time-point study. Int J Rehabil Res. 2015;38:173–180. doi: 10.1097/MRR.0000000000000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bartels M, Duffy C, Beland Edgar, Pathophysiology H. In: Stroke rehabilitation. 4th ed. Gillen G, editor. Mosby; St Louis: 2015. medical management and acute rehabilitation of stroke survivors; pp. 1–48. editor. [Google Scholar]
- 15.Godwin KM, Ostwald SK, Cron SG, Wasserman J. Long-term health-related quality of life of stroke survivors and their spousal caregivers. J Neurosci Nurs. 2013;45:147–154. doi: 10.1097/JNN.0b013e31828a410b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lyu W, Wolinsky FD. The onset of ADL difficulties and changes in health-related quality of life. Health Qual Life Outcomes. 2017;15:217. doi: 10.1186/s12955-017-0792-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Medhi GK, Sarma J, Pala S, Bhattacharya H, Bora PJ, Visi V. Association between health related quality of life (HRQOL) and activity of daily living (ADL) among elderly in an urban setting of Assam. India. J Family Med Prim Care. 2019;8:1760–1764. doi: 10.4103/jfmpc.jfmpc_270_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sheng S, Wang X, Gil Tommee C, et al. Continued underutilization of stroke care during the COVID-19 pandemic. Brain Behav Immun Health. 2021;15 doi: 10.1016/j.bbih.2021.100274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020;51:1996–2001. doi: 10.1161/STROKEAHA.120.030225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morrow EL, Patel NN, Duff MC. Disability and the COVID-19 pandemic: a survey of individuals with traumatic brain injury. Arch Phys Med Rehabil. 2021;102:1075–1083. doi: 10.1016/j.apmr.2021.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Headway: The Brain Injury Association. The impact of lockdown on brain injury survivors and their families. Available at: https://www.headway.org.uk/media/8564/the-impact-of-lockdown-on-brain-injury-survivors-and-their-families.pdf. Accessed January 13, 2022.
- 22.Zedde M, Pezzella FR, Paciaroni M, et al. Stroke care in Italy: an overview of strategies to manage acute stroke in COVID-19 time. Eur Stroke J. 2020;5:222–229. doi: 10.1177/2396987320942622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dafer RM, Osteraas ND, Biller J. Acute stroke care in the coronavirus disease 2019 pandemic. J Stroke Cerebrovasc Dis. 2020;29 doi: 10.1016/j.jstrokecerebrovasdis.2020.104881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kamdar HA, Senay B, Mainali S, et al. Clinician's perception of practice changes for stroke during the COVID-19 pandemic. J Stroke Cerebrovasc Dis. 2020;29 doi: 10.1016/j.jstrokecerebrovasdis.2020.105179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith EE, Mountain A, Hill MD, et al. Canadian stroke best practice guidance during the COVID-19 pandemic. Can J Neurol Sci. 2020;47:474–478. doi: 10.1017/cjn.2020.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mah K, Swami N, Le LW, et al. Validation of the 7-item Functional Assessment of Cancer Therapy-General (FACT-G7) as a short measure of quality of life in patients with advanced cancer. Cancer. 2020;126:3750–3757. doi: 10.1002/cncr.32981. [DOI] [PubMed] [Google Scholar]
- 27.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;57:289–300. [Google Scholar]
- 28.Colantonio A. Sex, gender, and traumatic brain injury: a commentary. Arch Phys Med Rehabil. 2016;97(2 Suppl):S1–S4. doi: 10.1016/j.apmr.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 29.Valera EM, Joseph AC, Snedaker K, et al. Understanding traumatic brain injury in females: a state-of-the-art summary and future directions. J Head Trauma Rehabil. 2021;36:E1–17. doi: 10.1097/HTR.0000000000000652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Toor GK, Harris JE, Escobar M, et al. Long-term health service outcomes among women with traumatic brain injury. Arch Phys Med Rehabil. 2016;97(2 Suppl):S54–S63. doi: 10.1016/j.apmr.2015.02.010. [DOI] [PubMed] [Google Scholar]
- 31.Guo D, Han B, Lu Y, et al. Influence of the COVID-19 pandemic on quality of life of patients with Parkinson's disease. Parkinsons Dis. 2020;2020 doi: 10.1155/2020/1216568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bao L, Li WT, Zhong BL. Feelings of loneliness and mental health needs and services utilization among Chinese residents during the COVID-19 epidemic. Global Health. 2021;17:51. doi: 10.1186/s12992-021-00704-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Niedzwiedz CL, Green MJ, Benzeval M, et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK Household Longitudinal Study. J Epidemiol Community Health. 2021;75:224–231. doi: 10.1136/jech-2020-215060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fiorillo A, Sampogna G, Giallonardo VA-O, et al. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: results from the COMET collaborative network. Eur Psychiatry. 2020;63:e87. doi: 10.1192/j.eurpsy.2020.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pierce BS, Perrin PB, Tyler CM, McKee GB, Watson JD. The COVID-19 telepsychology revolution: a national study of pandemic-based changes in U.S. mental health care delivery. Am Psychol. 2021;76:14–25. doi: 10.1037/amp0000722. [DOI] [PubMed] [Google Scholar]
- 36.Bokolo Anthony J. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020;44:132. doi: 10.1007/s10916-020-01596-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guzik AK, Martin-Schild S, Tadi P, et al. Telestroke across the continuum of care: lessons from the COVID-19 pandemic. J Stroke Cerebrovasc Dis. 2021;30 doi: 10.1016/j.jstrokecerebrovasdis.2021.105802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cramer SC, Dodakian L, Le V, et al. Efficacy of home-based telerehabilitation vs in-clinic therapy for adults after stroke: a randomized clinical trial. JAMA Neurol. 2019;76:1079–1087. doi: 10.1001/jamaneurol.2019.1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Laver KE, Adey-Wakeling Z, Crotty M, Lannin NA, George S, Sherrington C. Telerehabilitation services for stroke. Cochrane Database Syst Rev. 2020;1 doi: 10.1002/14651858.CD010255.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nouri SS, Avila-Garcia P, Cemballi AG, Sarkar U, Aguilera A, Lyles CR. Assessing mobile phone digital literacy and engagement in user-centered design in a diverse, safety-net population: mixed methods study. JMIR mHealth and uHealth. 2019;7:e14250. doi: 10.2196/14250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Eberly LA, Khatana SAM, Nathan AS, et al. telemedicine outpatient cardiovascular care during the COVID-19 pandemic: bridging or opening the digital divide? Circulation. 2020;142:510–512. doi: 10.1161/CIRCULATIONAHA.120.048185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ellis C, Boan AD, Turan TN, Ozark S, Bachman D, Lackland DT. Racial differences in poststroke rehabilitation utilization and functional outcomes. Arch Phys Med Rehabil. 2015;96:84–90. doi: 10.1016/j.apmr.2014.08.018. [DOI] [PubMed] [Google Scholar]
- 43.Simmonds KP, Luo Z, Reeves M. Race/ethnic and stroke subtype differences in poststroke functional recovery after acute rehabilitation. Arch Phys Med Rehabil. 2021;102:1473–1481. doi: 10.1016/j.apmr.2021.01.090. [DOI] [PubMed] [Google Scholar]
- 44.Hewitt MA, Smith DG, Heckman JT, Pasquina PF. COVID-19: a catalyst for change in virtual health care utilization for persons with limb loss. PM R. 2021;13:637–646. doi: 10.1002/pmrj.12605. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.