Abstract
IgA nephropathy (IgAN), membranous nephropathy (MN), and lupus nephritis (LN) represent important causes of chronic kidney disease. They belong to the immune-mediated glomerulonephritis (GNs), and have distinct pathogenesis, distinct clinical courses, and variable responses to treatment. Therefore, specific diagnostic procedures are necessary for more effective patient management. Recently, a role for oxidative stress has been proposed in various renal disorders. Thus, molecules related to oxidative stress, such as 2-Cys-peroxiredoxins (PRDXs), may represent plausible candidates for biomarkers in renal pathologies. The aim of this study was to assess whether there are differences between individual GNs and healthy controls in the context of PRDXs serum concentration. We enrolled 108 patients with biopsy-proven IgAN (47), MN (26), LN (35) and 30 healthy age- and sex-matched controls. The serum concentrations of PRDX 1–5 were measured with ELISA assays and correlated with demographic and clinical data. The PRDXs’ concentration varied depending on the GN type. We also observed an association of PRDXs with lower estimated glomerular filtration rates, complement, hemoglobin, and body mass index. Our study indicates that individual PRDX can play roles in pathophysiology of selected GNs and that their serum concentrations may become useful as a new supplementary diagnostic markers in IgAN, MN as well as LN. The results of this study open a new avenue for prospective research on PRDXs in renal diseases.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00005-021-00638-1.
Keywords: Chronic kidney disease, IgA nephropathy, Lupus nephritis, Membranous nephropathy, Oxidative stress, Peroxiredoxins
Introduction
Chronic kidney disease (CKD) is a growing public health problem, affecting approximately 8–13% of the population (Brück et al. 2016; Hill et al. 2016). Furthermore, it is projected that in 2040, CKD will be the fifth leading cause of death in the world (Foreman et al. 2018). Glomerulonephropathies (GNs) such as IgA nephropathy (IgAN), membranous nephropathy (MN), and lupus nephritis (LN) are immune-mediated, although they have different etiologies, and are among the most frequent causes of CKD (Pippias et al. 2017). GNs account for about 20% of CKD cases in most countries, usually affecting young people and carry a lifelong CKD burden (Floege and Amann 2016). IgAN and MN belong to the primary GNs, and their annual incidence is estimated at 2–5 and 1–2 cases per 100,000 adults, respectively (McGrogan et al. 2011). LN develops secondary to systemic disease, and its incidence is estimated at 0.4–0.7 cases per 100,000 population per year (Patel et al. 2006). Unfortunately, GNs frequently progress asymptomatically or present with proteinuria, erythrocyturia or hematuria, edema, and hypertension (Vassalotti et al. 2010). These symptoms are neither specific nor sensitive enough for any GN. The diagnosis is difficult and frequently too late, and still requires histopathological evaluation by kidney biopsy, an invasive procedure with known risks (Mucha et al. 2016). Therefore, alternative, specific, reproducible, and safer methods are needed to facilitate noninvasive diagnosis.
There are specific markers that may help to diagnose glomerular diseases, including galactose-deficient IgA1 and IgG autoantibodies that correlate with IgAN (Placzek et al. 2018), anti-phospholipid 2 receptor antibodies that correlate with the histological picture of MN, and anti-double-stranded DNA antibodies associated with LN activity (Na et al. 2017). Multiple urine and serum proteins (Gao et al. 2018; Krata et al. 2018; Moszczuk et al. 2021; Mucha et al. 2014) or gene polymorphisms (Xie et al. 2020; Pac et al 2021) have been proposed as markers of different kidney diseases in the last decade. However, their diagnostic and/or prognostic utility remains to be validated (Krata et al. 2018; Selvaskandan et al. 2020; Sethi et al. 2019, 2020; Yanagawa et al. 2014). In this study, we focused on oxidative stress-related markers, 2-cysteine peroxiredoxins (2-Cys PRDXs), as potentially discriminatory in renal diseases.
Oxidative stress (OS) is one of the mechanisms involved in the progression of every type of CKD, including GN (Krata et al. 2018). Indeed, specific CKD-related conditions may lead to the overproduction of reactive oxygen species (ROS). It was reported that CKD patients have increased levels of plasma thiol oxidation and carbonylation, but the role of PRDXs in the pathophysiology of kidney diseases remains unknown (Cachofeiro et al. 2008; Krata et al. 2018). PRDXs, which are similar in function to well-known antioxidant enzymes such as catalase and glutathione peroxidase, possess the ability to reduce excessive levels of hydrogen peroxide, one of the major OS mediators (Jeong et al. 2012; Yang and Lee 2015). Importantly, kinetics measurements imply that PRDXs reduce more than 90% of cellular peroxides (Adimora et al. 2010; Perkins et al. 2015; Winterbourn 2008), which predisposes them to being a crucial factor in cellular OS regulation. Oxidative stress has been reported in kidney disease, due to both antioxidant depletions as well as increased production of ROS (Daenen et al. 2019; Irazabal and Torres 2020). The kidney is a highly metabolic organ, rich in oxidation reactions in mitochondria, which makes it vulnerable to damage caused by ROS (Aranda-Rivera et al. 2021). Therefore, OS can accelerate kidney disease progression. Different PRDX isoforms were reported to be involved in diabetic nephropathy (Lee and Lee 2018), ischemia/reperfusion damage (Sharapov et al. 2020), obstructive kidney disease (Hwang et al. 2019), ciliopathies (Zacchia et al. 2020) and acute tubular necrosis (Wu et al. 2017). However, the role of PRDXs in the pathophysiology of glomerular diseases is not well known.
In the current study, we hypothesized that 2-Cys PRDXs could be differentially involved in IgAN, MN, and LN. If so, the PRDX family could serve as additional markers of specific GNs. Therefore, the aim of this study was to evaluate PRDX 1–5 serum concentrations in IgAN, MN, and LN patients and healthy controls.
Materials and Methods
Patients
We enrolled 108 patients (GN group) diagnosed by renal biopsy with IgAN (47), MN (26), and LN (35). The exclusion criteria were active infection, current pregnancy, history of malignancy, or previous organ transplantation. The healthy control group was defined by the absence of any kidney disease or other chronic diseases requiring treatment and consisted of 30 age- and sex-matched volunteers. Demographic characteristics of study participants are presented in Table 1. The study was performed in accordance with the Declaration of Helsinki guidelines for research on human subjects and was approved by the Ethics Committee of the Medical University of Warsaw (KB/9/2010 and KB/199/2016), and written informed consent was obtained from all the participants.
Table 1.
Characteristics of study participants
| Healthy controls | IgAN | MN | LN | GN group | P value | |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age (years) | 44.4 ± (12.9) | 43.1 ± (13.3) | 54.1 ± (13.4) | 45.2 ± (12.4) | 46.4 ± (13.6) | 0.022 |
| Male (%)** | 43.3% | 51.1% | 57.7% | 31.4% | 46.3% | 0.773 |
| BMI (kg/m2) | 23.8 ± (3.4) | 27.3 ± (3.8) | 25.7 ± (4.1) | 24.7 ± (7.9) | 26.1 ± (5.5) | < 0.001 |
| Laboratory data | ||||||
| WBC (G/L) | 5.6 ± (1.02) | 8.2 ± (2.4) | 8.6 ± (3.1) | 7.0 ± (3.5) | 7.9 ± (3.02) | < 0.001 |
| HGB (g/dL) | 13.9 ± (1.2) | 14.1 ± (1.5) | 13.6 ± (1.8) | 13.2 ± (1.8) | 13.5 ± (2.4) | 0.128 |
| HCT (L/L) | 0.422 ± (0.036) | 0.434 ± (0.042) | 0.423 ± (0.052) | 0.411 ± (0.056) | 0.424 ± (0.049) | 0.289 |
| PLT (G/L) | 236.2 ± (53.8) | 251.3 ± (54.6) | 248.5 ± (78.9) | 243.6 ± (87.2) | 248.1 ± (71.5) | 0.842 |
| C3 (mg/dL)* | n.a | 114.1 ± (27.7) | 106.5 ± (48.9) | 94 ± (26.6) | 106.1 ± (30.2) | 0.006 |
| C4 (mg/dL)* | n.a | 26.2 ± (6.9) | 29.0 ± (11.3) | 16.3 ± (8.0) | 22.8 ± (9.0) | < 0.001 |
| Serum creatinine (mg/dL) | 0.86 ± (0.14) | 1.47 ± (1.11) | 1.13 ± (0.46) | 1.07 ± (0.68) | 1.26 ± (0.87) | 0.013 |
| eGFR (ml/min/1.73 m2) | 92.2 ± (13.7) | 71.7 ± (34.4) | 74.2 ± (26.2) | 82.1 ± (27.9) | 75.6 ± (30.5) | 0.059 |
|
Proteinuria* (g/24 h) |
n.a | 0.96 ± (1.14) | 1.00 ± (1.23) | 0.46 ± (0.63) | 0.82 ± (1.05) | < 0.001 |
| Total serum protein (g/dL) | 7.4 ± (0.3) | 7.0 ± (0.6) | 6.5 ± (1.2) | 7.0 ± (0.5) | 6.9 ± (0.7) | 0.139 |
| Serum albumin (g/dL) | 4.3 ± (0.1) | 3.9 ± (0.4) | 3.9 ± (0.6) | 3.9 ± (0.3) | 3.9 ± (0.4) | 0.029 |
| Serum α-1 (g/dL) | 0.3 ± (0.03) | 0.3 ± (0.05) | 0.3 ± (0.06) | 0.3 ± (0.06) | 0.3 ± (0.05) | 0.345 |
| Serum α-2 (g/dL) | 0.6 ± (0.07) | 0.725 ± (0.1) | 0.8 ± (0.12) | 0.789 ± (0.13) | 0.750 ± (0.11) | 0.011 |
| Serum β-1 (g/dL) | 0.5 ± (0.05) | 0.487 ± (0.07) | 0.477 ± (0.07) | 0.478 ± (0.11) | 0.484 ± (0.07) | 0.909 |
| Serum β-2 (g/dL) | 5.6 ± (1.4) | 4.7 ± (2.8) | 6.0 ± (1.2) | 4.9 ± (2.6) | 5.00 ± (2.6) | 0.413 |
| Serum γ (g/dL) | 1.3 ± (0.2) | 1.1 ± (0.2) | 0.8 ± (0.3) | 1.1 ± (0.3) | 1.1 ± (0.3) | 0.018 |
Values are given as mean ± SD. Level of significance was calculated with Chi-squared test and non-parametric Kruskal–Wallis test. P < 0.05 indicates that at least one studied group is significantly different from one other group. *Healthy controls group excluded from comparison; **comparison between GN and healthy control; n.a. not available; BMI body mass index, WBC white blood count, HGB hemoglobin, HCT hematocrit, PLT platelets, eGFR estimated glomerular filtration rate
Methods
Material Collection
Blood samples were collected once from each of the individuals (fasting) into serum separating tubes (Becton Dickinson, Franklin Lakes, NJ, USA). To obtain serum, blood samples were left to clot at 23–25 °C (room temperature, RT) for 30 min and centrifuged at 2000 RPM at RT. Serum samples were stored in aliquots at − 80 °C until further measurements.
PRDX Measurements
The serum concentration of each of PRDX (1–5) was measured using commercially available enzyme-linked immunosorbent assays (EIAab, Wuhan, China). Briefly, the samples and standards were added to the microtiter plate and pre-coated with a biotin-conjugated antibody specific to the target antigen. The standards and samples were added in a determined order the amount of 100 µL per well. Then, avidin-conjugated horseradish peroxidase was added to each microplate well. The enzyme–substrate reaction was terminated by the addition of sulfuric acid solution. Color changes in each well were measured spectrophotometrically at a wavelength of 450 nm on a BioTekPowerWave XS microplate reader (BioTek, Winooski, VT, USA). The targeted antigen concentration was determined by comparing the optical density absorbance of samples to the standard curve. Samples below the detection range for each test were set as the lowest concentration obtained from the standard curve to avoid losing the meaningful part of the results and compute reliable statistical analysis.
Biochemical and Clinical Characteristics
Laboratory tests of serum creatinine, proteins, complement, blood morphology, urine analysis, and urinary protein were assayed by routine laboratory techniques. The estimated glomerular filtration rate (eGFR) was calculated according to the Chronic Kidney Disease—Epidemiology Collaboration equation. Body weight in kilograms was divided by the square of height in meters (kg/m2) to evaluate body mass index (BMI).
Statistical Analysis
Statistical analysis was performed in R version 3.6.1. and Statistica 13.1 (StatSoft). Results were expressed as mean ± standard deviation, median ± interquartile range, or a percentage value. All variables were tested for normal distribution by the Shapiro–Wilk test. Non-normally distributed variables were analyzed by non-parametric tests. Comparisons between demographic data were tested by the Kruskal–Wallis test (quantitative variables) and Chi-squared test (qualitative variables), whereas comparisons in biomarker levels between control and GN groups were tested by the Mann–Whitney U test. Given that the biomarkers are non-normally distributed, the association between pairs of parameters were analyzed using Spearman’s correlation. To correct for testing multiple hypotheses, in PRDX assessment in three GN groups, we used the Bonferroni method—given a total number of 15 comparative tests: 5 biomarkers and 3 disease groups compared to controls, we considered P value < 0.05/15 or 0.0033 statistically significant. Receiver-operating characteristic curves (ROC) were calculated with cutoff points established by binary logistic regression with a significance level of P < 0.05 and 95% confidence interval. The ROC analysis results were interpreted as follows: AUC < 0.50, low diagnostic accuracy; AUC in the range of 0.50–0.70, moderate diagnostic accuracy; and AUC > 0.70, high diagnostic accuracy.
Results
Discrimination Between GN Patients and Healthy Subjects
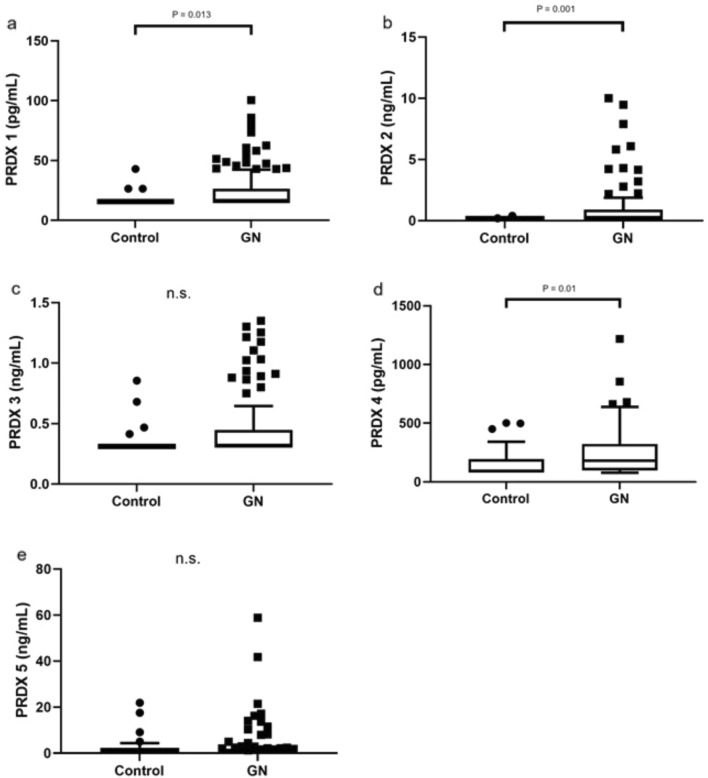
We were able to discriminate GN patients in total from healthy subjects based on significantly elevated PRDX 1, 2, and 4 (Fig. 1a, b, d). No differences in PRDX 3 and 5 levels were observed between GN and controls (Fig. 1c, e); however, a clear tendency for higher concentrations of these PRDXs in GN patients has been observed in case of PRDX 3.
Fig. 1.
PRDX 1–5 concentrations in patients with GN and healthy controls. Data are presented as box-and-whisker plots; box represents interquartile range (IRQ) with line set as median value for each PRDX concentration, ends of whiskers represent ± 1.5 IQR of value (maximum/minimum), and individual data points indicate outliers. P < 0.05 was considered significant (Mann–Whitney U test). GN—IgAN, MN, LN combined; (a) PRDX 1; (b) PRDX 2; (c) PRDX 3; (d) PRDX 4; (e) PRDX 5; n.s.—not significant
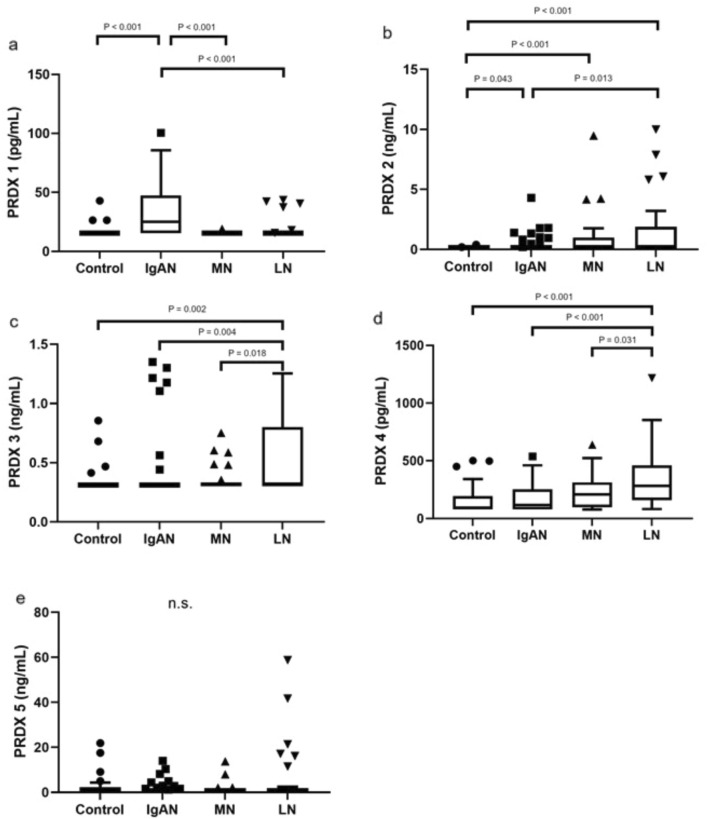
Subclass Variability
Depending on the PRDX subclass, the serum concentration varied between IgAN, MN, and LN patients and healthy controls (Fig. 2). IgAN patients had significantly higher concentrations of PRDX 1 and 2 (P < 0.001 and < 0.043, respectively; however, only PRDX 1 remained significant after Bonferroni correction; Fig. 2a, b); the MN group had almost the same PRDX levels, except for PRDX 2 (P = 0.001; Fig. 2b), whereas the levels of PRDX 2, 3, and 4 in LN patients were significantly elevated (P < 0.001, < 0.002, and < 0.001, respectively; Fig. 2b–d) compared to those in the control group. Importantly, we noticed significant differences between the disease groups. Comparing IgAN and MN, higher PRDX 1 level was revealed level in IgAN patients (Fig. 2a). The significant differences between IgAN and LN varied depending on the PRDX subclass (1–4) (Fig. 2a–d), whereas comparing LN assessment and MN revealed higher levels of PRDX 3 and 4 in LN individuals (Fig. 2c, d).
Fig. 2.
Peroxiredoxin (PRDX) 1–5 concentrations in IgA nephropathy (IgAN), membranous nephropathy (MN), lupus nephritis (LN) and healthy controls. Data are presented as box-and-whisker plots; box represents interquartile range (IRQ) with line set as median value for each PRDX concentration, ends of whiskers represent ± 1.5 IQR of value (maximum/minimum), and individual data points indicate outliers (Mann–Whitney U test). P value was considered significant if < 0.05 and < 0.033 after Bonferroni correction; (a) PRDX 1; (b) PRDX 2; (c) PRDX 3; (d) PRDX 4; (e) PRDX 5; n.s. not significant
To confirm the diagnostic accuracy of PRDX levels, we performed ROC analysis to strengthen the significance of the obtained results. The most prominent AUC values were detected for PRDX 2 (0.652) and 4 (0.653) to discriminate GN from controls and for PRDX 1 to discriminate IgAN from LN (0.733) and MN (0.788) (Table 2).
Table 2.
Receiver-operating characteristic (ROC) analysis for serum PRDX 1–5 concentration in GN’s and healthy controls
| Area AUC | 95% CI (lower) | 95% CI (upper) | P value | Cutoff point | True positive | False positive | False negative | True negative | Sensitivity | Specificity | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| PRDX 1 | |||||||||||
| IgAN_LN | 0.733 | 0.625 | 0.840 | < 0.001 | 19.107 | 27 | 4 | 20 | 31 | 0.574 | 0.886 |
| IgAN_MN | 0.788 | 0.687 | 0.890 | < 0.001 | 16.954 | 28 | 1 | 19 | 25 | 0.596 | 0.962 |
| IgAN_Control | 0.761 | 0.656 | 0.866 | < 0.001 | 16.954 | 28 | 3 | 19 | 27 | 0.596 | 0.900 |
| LN_Control | 0.536 | 0.395 | 0.677 | 0.619 | 15.828 | 6 | 3 | 29 | 27 | 0.171 | 0.900 |
| MN_Control | 0.467 | 0.315 | 0.619 | 0.673 | 19.115 | 1 | 3 | 25 | 27 | 0.038 | 0.900 |
| LN_MN | 0.568 | 0.424 | 0.711 | 0.357 | 15.828 | 6 | 1 | 29 | 25 | 0.171 | 0.962 |
| GN_Control | 0.617 | 0.515 | 0.720 | 0.025 | 15.828 | 35 | 3 | 73 | 27 | 0.324 | 0.900 |
| PRDX 2 | |||||||||||
| IgAN_LN | 0.365 | 0.240 | 0.491 | 0.035 | 0.165 | 11 | 16 | 36 | 19 | 0.234 | 0.543 |
| IgAN_MN | 0.402 | 0.262 | 0.541 | 0.168 | 0.165 | 11 | 11 | 36 | 15 | 0.234 | 0.577 |
| IgAN_Control | 0.590 | 0.464 | 0.717 | 0.163 | 0.165 | 11 | 2 | 36 | 28 | 0.234 | 0.933 |
| LN_Control | 0.710 | 0.584 | 0.835 | 0.001 | 0.426 | 15 | 0 | 20 | 30 | 0.429 | 1.000 |
| MN_Control | 0.688 | 0.544 | 0.833 | 0.010 | 0.476 | 9 | 0 | 17 | 30 | 0.346 | 1.000 |
| LN_MN | 0.543 | 0.398 | 0.689 | 0.560 | 0.165 | 16 | 11 | 19 | 15 | 0.457 | 0.577 |
| GN_Control | 0.652 | 0.557 | 0.748 | 0.002 | 0.165 | 38 | 2 | 70 | 28 | 0.352 | 0.933 |
| PRDX 3 | |||||||||||
| IgAN_LN | 0.350 | 0.226 | 0.473 | 0.017 | 0.325 | 7 | 17 | 40 | 18 | 0.149 | 0.514 |
| IgAN_MN | 0.470 | 0.330 | 0.609 | 0.670 | 0.325 | 7 | 6 | 40 | 20 | 0.149 | 0.769 |
| IgAN_Control | 0.514 | 0.382 | 0.646 | 0.833 | 0.325 | 7 | 4 | 40 | 26 | 0.149 | 0.867 |
| LN_Control | 0.690 | 0.561 | 0.818 | 0.004 | 0.513 | 15 | 2 | 20 | 28 | 0.429 | 0.933 |
| MN_Control | 0.547 | 0.394 | 0.700 | 0.543 | 0.480 | 5 | 2 | 21 | 28 | 0.192 | 0.933 |
| LN_MN | 0.656 | 0.521 | 0.792 | 0.024 | 0.513 | 15 | 3 | 20 | 23 | 0.429 | 0.885 |
| GN_Control | 0.579 | 0.472 | 0.687 | 0.150 | 0.325 | 30 | 4 | 78 | 26 | 0.278 | 0.867 |
| PRDX 4 | |||||||||||
| IgAN_LN | 0.230 | 0.131 | 0.329 | < 0.001 | 85.899 | 30 | 34 | 17 | 1 | 0.638 | 0.029 |
| IgAN_MN | 0.394 | 0.257 | 0.531 | 0.131 | 79.722 | 31 | 20 | 16 | 6 | 0.660 | 0.231 |
| IgAN_Control | 0.545 | 0.412 | 0.678 | 0.507 | 79.722 | 31 | 18 | 16 | 12 | 0.660 | 0.400 |
| LN_Control | 0.800 | 0.691 | 0.909 | < 0.001 | 102.148 | 33 | 13 | 2 | 17 | 0.943 | 0.567 |
| MN_Control | 0.650 | 0.504 | 0.796 | 0.045 | 221.942 | 12 | 5 | 14 | 25 | 0.462 | 0.833 |
| LN_MN | 0.663 | 0.522 | 0.803 | 0.023 | 140.977 | 31 | 15 | 4 | 11 | 0.886 | 0.423 |
| GN_Control | 0.653 | 0.543 | 0.763 | 0.007 | 79.722 | 86 | 18 | 22 | 12 | 0.796 | 0.400 |
| PRDX 5 | |||||||||||
| IgAN_LN | 0.472 | 0.344 | 0.601 | 0.674 | 1.247 | 11 | 9 | 36 | 26 | 0.234 | 0.743 |
| IgAN_MN | 0.538 | 0.400 | 0.675 | 0.591 | 1.247 | 11 | 4 | 36 | 22 | 0.234 | 0.846 |
| IgAN_Control | 0.459 | 0.324 | 0.593 | 0.549 | 1.247 | 11 | 9 | 36 | 21 | 0.234 | 0.700 |
| LN_Control | 0.490 | 0.348 | 0.631 | 0.885 | 1.247 | 9 | 9 | 26 | 21 | 0.257 | 0.700 |
| MN_Control | 0.424 | 0.274 | 0.575 | 0.324 | 1.247 | 4 | 9 | 22 | 21 | 0.154 | 0.700 |
| LN_MN | 0.562 | 0.417 | 0.706 | 0.403 | 1.247 | 9 | 4 | 26 | 22 | 0.257 | 0.846 |
| GN_Control | 0.460 | 0.341 | 0.580 | 0.517 | 1.247 | 24 | 9 | 84 | 21 | 0.222 | 0.700 |
P < 0.05 was considered significant. AUC under the curve, 95% CI 95% confidence interval
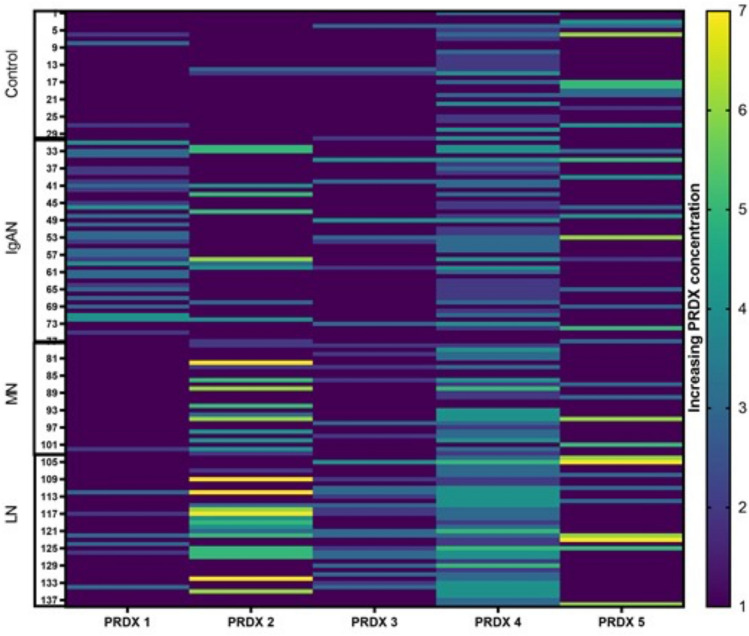
Single-Patient PRDX Concentration Panel (Heatmap)
Based on our results, we prepared a heatmap (Fig. 3) of PRDX concentrations for all the studied groups. The detection range was set as consecutive concentrations obtained from the standard curve (Table 3). The heatmap suggests the PRDX 1 potential to differentiate IgAN from other GN or controls. Moreover, PRDX 2 concentrations seem significantly higher in LN patients, than in IgAN and controls (as shown in Fig. 2b). This illustrates possible differential GN diagnostic pattern for PRDX 1 and 2; however, to confirm it is applicability, further studies addressing the subclass variability, relationship to such parameters as age, eGFR, proteinuria and anemia are required.
Fig. 3.
PRDX concentration panel (heatmap) of study participants
Table 3.
Consecutive standard PRDX dilutions obtained from standard curve
| PRDX | PRDX 1 (pg/mL) | PRDX 2 (ng/mL) | PRDX 3 (ng/mL) | PRDX 4 (pg/mL) | PRDX 5 (ng/mL) |
|---|---|---|---|---|---|
| Concentration range | |||||
| 1 | < 15.6 | < 0.156 | < 0.312 | < 78.0 | < 0.78 |
| 2 | 15.6–31.2 | 0.156–0.312 | 0.312–0.625 | 78.0–156 | 0.78–1.56 |
| 3 | 31.3–62.5 | 0.313–0.625 | 0.626–1.25 | 157–312 | 1.57–3.12 |
| 4 | 62.6–125 | 0.626–1.25 | 1.251–2.5 | 313–625 | 3.13–6.25 |
| 5 | 125.1–250 | 1.251–2.5 | 2.501–5.0 | 626–1250 | 6.26–12.5 |
| 6 | 250.1–500 | 2.501–5.0 | 5.001–10 | 1251–2500 | 12.51–25 |
| 7 | 500.1–1000 | 5.001–10 | 10.001–20 | 2501–5000 | 25.01–50 |
Correlations
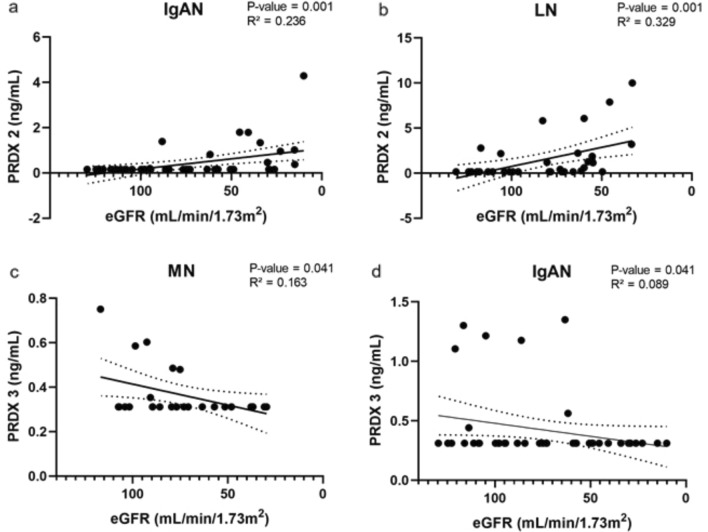
Glomerular Filtration Rate
We observed significant correlation between PRDX 2 serum concentration and renal function as expressed by the eGFR in IgAN (P = 0.001) and LN (P = 0.001) patients (Fig. 4a, b), and similarly for PRDX 3 in MN (P = 0.041) and IgAN (P = 0.041) patients (Fig. 4c, d).
Fig. 4.
Spearman’s correlation analysis of eGFR and PRDX 2 (IgAN, LN) and PRDX 3 in (IgAN, MN) patients. Correlation was fitted with linear model with 95% confidence interval bands; P < 0.05 was considered significant
Complement components C3 and C4
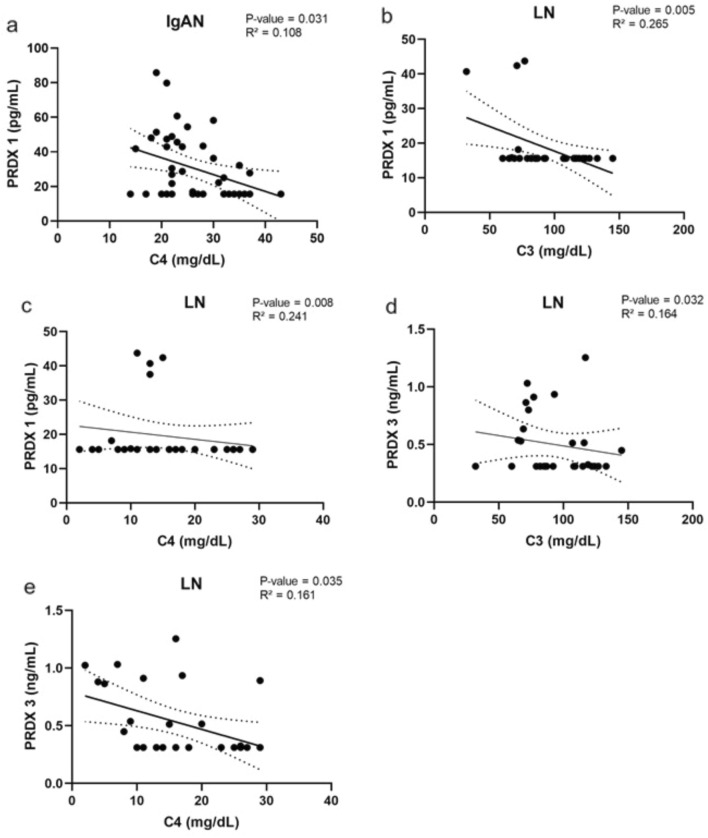
The complement component concentration showed an inverse association with PRDX 1 in IgAN (P = 0.031) and LN (P = 0.005 and P = 0.008) patients (Fig. 5a, b, c) and PRDX 3 (P = 0.032 and P = 0.035) in LN patients (Fig. 5d,e). An association was also found with PRDX 3 in the whole GN group (Supplementary Table 1) (Fig. 5).
Fig. 5.
Spearman’s correlation analysis of complements C3 and C4 in IgAN and LN patients. Correlation was fitted with linear model with 95% confidence interval, P < 0.05 was considered significant
Other Parameters
In addition, a significant inverse correlation between PRDX 2 and hematocrit (HCT) was observed in the GN group (P = 0.001). Further analysis revealed that HCT was correlated with PRDX 2 in LN only (P = 0.011). The association between hemoglobin (HGB) level and serum PRDX 2 concentration was found in the whole GN group (P = 0.001) and in IgAN (P = 0.025) and LN (P = 0.005) separately (Supplementary Table 1).
We noticed a significant correlation between PRDX 3 and 24 h proteinuria in the whole GN group (P = 0.013), but not in IgAN, MN or LN separately. Moreover, 24 h proteinuria was correlated to PRDX 2 only in MN patients (P = 0.014) (Supplementary Table 1). At the same time, we did observe an association of PRDX with serum proteinogram changes. For example, in IgAN patients, serum α-1 and β-1 globulins, were correlated significantly with PRDX 1 (P = 0.032; P = 0.001, respectively), while β-2 globulins were correlated with PRDX 1 (P = 0.021), 3 (P = 0.018) and 4 (P = 0.004). Furthermore, in the MN group, β-2 globulins correlated with PRDX 2 (P = 0.033), and in the LN group, β-1 globulins correlated with PRDX 1 (P = 0.048) (Supplementary Table 1).
A significant correlation was also found between BMI and PRDX 5 in IgAN patients (P = 0.012). Other significant associations are summarized in Supplementary Table 1.
Discussion
In this study, we show that serum levels of PRDX 1–4 were significantly elevated in IgAN, MN, and LN patients compared to healthy individuals. In addition to the differences between disease and control groups, we also found that each GN type revealed a distinct PRDX pattern. There is no straight explanation why there would be differences in oxidative stress markers between different types of GN. The data on biological reasons for these differences are largely missing.
Oxidative stress is defined as a disturbance in the natural ability of cells to maintain a balance between pro- and antioxidant systems (Krata et al. 2018; Selvaskandan et al. 2020; Sethi et al. 2019, 2020; Yanagawa et al. 2014). Although moderate levels of hydrogen peroxide are necessary for numerous cellular processes, in excessive concentrations it can cause cell and tissue damage (mediated by oxidation of lipids, proteins, or DNA). Several mechanisms are responsible for the removal of reactive oxygen species, including superoxide dismutase, catalase, peroxidase, the peroxide–redox–thioredoxin–thioredoxin reductase enzymatic chain, and a number of non-enzymatic antioxidants (Descamps-Latscha et al. 2001). PRDXs are known as biomarkers for cancer (Basu et al. 2011; O'Leary et al. 2014), bacterial infections (Yang et al. 2018), and neurodegenerative (Goemaere and Knoops 2012) and inflammatory-related diseases (Park et al. 2016). Their role in the pathophysiology and/or diagnostics of IgAN, MN, and LN has not been characterized yet.
The fundamental method of following up CKD, including GN patients, is eGFR estimation. We observed an inverse correlation between eGFR and PRDX 2 in IgAN and LN but not MN patients and PRDX3 in IgAN and MN individuals. For the obvious reasons, a simple link between eGFR and serum PRDX probably does not exist. However, declining eGFR is the evident effect of kidney disease progression involving, e.g., oxidative stress. Coexisting secondary anemia or other comorbidities could additionally influence PRDX levels in serum (discussed below). Another gold standard for GN follow-up is 24-h urine protein loss analysis. Higher proteinuria usually indicates more advanced or active GN. However, we observed only one correlation between PRDX 2 and 24 h proteinuria in MN patients. The implication of this is unclear. The highly variable degree of proteinuria in MN patients, related to the MN biology could explain this finding. On the other hand, a potential relation to protein loss may be suspected also in other GNs based on the observed PRDX association with serum proteinogram changes. Therefore, the causes of proteinogram changes are probably multifactorial and OS is differentially involved. Moreover, to date, there has not been much published data about PRDX and GN, particularly in the context of proteinuria. Of note, proteinuria may additionally serve as an indirect indicator of the GN activity. One could speculate that due to the relative unspecificity of OS, PRDX serum levels might be expected to reflect disease activity rather than disease itself. This speculation could not be elucidated with our study design, since each studied GN has distinct activity scale. Thus, the comparison of disease activity between these groups is impossible. Moreover, diagnostic renal biopsies were performed in history, not at the time of sampling.
OS is implicated in various or almost all disease states, including atherosclerosis, cardiovascular disease, obesity, diabetes, cancer, neurodegeneration, aging, drugs (e.g., allopurinol) and many others. Such conditions could confound the results and anemia belongs to the most potent OS confounders. Along with CKD progression, the uremic toxins increase red blood cell (RBC) damage and erythropoietin deficiency reduces HGB production, resulting in tissue hypoxia. The latter may stimulate OS responses, including, e.g., increased PRDXs (Gwozdzinski et al. 2021). Indeed, we found a correlation between HGB and serum PRDX 2 concentrations in IgAN and LN patients. It was reported that PRDX 2 plays an important role in the protection of RBCs from OS through HGB autoxidation (Johnson et al. 2005), e.g., in iron-deficiency anemia (Nagababu et al. 2008). The protective function of PRDX 2 in HGB stability has been investigated in PRDX 2 knockout mice and RBCs from patients with hereditary hemolytic anemia. The authors of this study suggested that PRDX 2 could bind to HGB and protect it from oxidative denaturation and aggregation in RBCs (Han et al. 2012). What is very important in our study is the fact that our patients had stage 2 CKD and an average eGFR of 71, 74, and 84 mL/min (for IgAN, MN, and LN, respectively), thus had normal RBC and HGB levels. One of the limitations of our study was relatively low patient numbers in each GN group, which precluded analysis of the effect other comorbidities on PRDX concentrations. Therefore, the question is, what does the increased serum PRDX really mean? Do PRDX levels behave as a damage marker or damage type marker? Is it possible that it is just a very early marker of preexisting hypoxia and/or OS in CKD patients long before the development of even early stages of anemia? The fact that different GNs enhance different PRDX classes also suggests different disease-specific mechanisms of hypoxia, which needs additional research. Another question is whether the serum concentrations of PRDXs should be only used as markers for a specific disease type or can also reflects the activity of this particular disease at the time of sample collection? In addition, oxidative stress activity in serum may not always reflect that of changes cellular microdomains in the kidney, which should be taken under consideration while interpreting the results of the current study. Finally, it is also worth adding that evaluation of all GN groups vs. healthy individuals showed significant differences in PRDX 1 and 2 (as illustrated on a heatmap). Therefore, it is an open question whether serum PRDX 1 and 2 might help in the future to distinguish patients suspected of having IgAN, MN-, or LN-related oxidative stress?
Complement activation and its regulation are complex phenomena. It is not definitive whether these phenomena are the direct primary cause or the effector mechanism of kidney injury, but they are involved in GN development and progression; thus, inhibiting them has become an emerging treatment option (Kaartinen et al. 2019). In patients with IgAN, the immunoglobulin A deposited in the mesangial area of the kidney can activate the complement system through either the lectin pathway or an alternative pathway. This may amplify the local inflammatory response and contribute to renal injury (Daha and van Kooten 2016). The immunopathology of human MN shows evidence of complement activation within immune deposits (Beck and Salant 2010). Therefore, it is thought likely that the complement system also plays a substantial role in MN pathogenesis. Although serum levels of complement proteins are usually normal in MN patients, it was recently reported that measuring the circulating complement activation products may be a way to detect ongoing complement activation (Zhang et al. 2019). Complement also has an important role in the pathogenesis of LN. On the one hand, a deficiency of complement components predisposes to lupus, while on the other hand, excess complement activation increases renal damage, and measuring it is done to assess disease activity (Sharma et al. 2020). Although OS involvement in renal injury being driven by complement activation seems obvious, to the best of our knowledge, to date there are no available data linking complement activation in GNs to PRDXs. We assume that the disease-specific PRDX associations with circulating C3 and C4 complement components observed in our study suggest differential OS responses depending on the GN etiology and the mode of complement activation. If so, PRDX subclass assessment might be useful as an adjunct in the diagnosis of GNs.
Another finding of our study is the positive correlation between PRDX 5 and BMI in the IgAN group. It was previously demonstrated in obese mouse models that PRDX 5 inhibits adipogenesis by modulating ROS generation and adipogenic gene expression, implying that it may serve as a potential target to prevent and treat obesity (Kim et al. 2018). Moreover, in vitro and in vivo experiments suggested that PRDX 5 functions as a protective regulator in fatty liver disease and may be a valuable therapeutic target for the management of obesity-related metabolic diseases (Kim et al. 2020). Taking these findings and our results together, it is possible that PRDX 5 is upregulated in response to chronic nephritis depending on BMI value, but this hypothesis needs further elucidation.
It is important to mention that in the current study the serum levels of PRDXs were evaluated, which might not reflect the intracellular changes in PRDXs expression within the tissue. As PRDXs can be released as damage-associated molecular pattern markers from injured tissues (He et al. 2019), this subject warrants further investigations.
Generally, our study indicates potential applicability of antioxidant supplementation in renal disease. The potential compounds to be used are, for instance: coenzyme Q10, Vitamins B, C, D, and E, L-carnitine, statins, or N-acetylcysteine (Liakopoulos et al. 2019). Indeed, application of coenzyme Q10 has been reported beneficial in the treatment of chronic diseases, including CKD (Gutierrez-Mariscal et al. 2020).
In conclusion, our results highlight the link between PRDXs and GNs (IgAN, MN, and LN). Our study indicates that individual PRDXs can play roles in pathophysiology of selected GNs and that their concentrations in serum may become useful as new supplementary diagnostic markers in IgAN, MN, and LN. Validation studies including other kidney diseases are required to better understand GNs and enable their less invasive diagnosis.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This project is the continuation of our study on the role of 2-Cys-PRDXs in GNs, the results of which have been included in the patent application from February 2017 to the European Patent Office (No. WO/2018/141975). The latest letter received from the patent office, dated 17 April 2020, stated: “The claimed subject matter is considered novel over the cited prior Art. 54 EPC”. We thank prof. Krzysztof Kiryluk from the Division of Nephrology in the Department of Medicine at Columbia University (New York, USA) for consulting the results and the final version of the manuscript. The routine laboratory tests were performed at the diagnostic laboratory of Infant Jesus Hospital, University Medical Center of the Medical University of Warsaw, during routine patient visits to the Nephrology and Transplantation Outpatient Clinic. The healthy control subjects donated their blood voluntarily. The ELISA measurements were performed with kind support from Kamila Gala, PhD. Figures were prepared with GraphPad Prism 9 software.
Author Contributions
KM and NK designed the study; NK carried out the experiments; NK and KM analyzed the data and generated the figures; BF, BM, and KM collected samples; NK, BF, RZ, BM, MZ, LP, and KM analyzed the data; NK, BF, RZ, BM, LP, and KM drafted and revised the article; all the authors approved the final version of the manuscript.
Funding
This research was supported by the Medical University of Warsaw, internal funding No. N1/16/16.
Data Availability
Data available upon request.
Code Availability
Not applicable.
Declarations
Conflict of Interest
None declared.
Ethics Approval
The study was conducted according to the guidelines of the Declaration of Helsinki for research on human subjects of 1975, revised in 2013, and approved by the Ethics Committee of the Medical University of Warsaw (KB/9/2010 and KB/199/2016).
Consent to Participate
Informed consent was obtained from all the subjects involved in the study.
Consent for Publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Adimora NJ, Jones DP, Kemp ML. A model of redox kinetics implicates the thiol proteome in cellular hydrogen peroxide responses. Antioxid Redox Signal. 2010;13:731–743. doi: 10.1089/ars.2009.2968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aranda-Rivera AK, Cruz-Gregorio A, Aparicio-Trejo OE, et al. Mitochondrial redox signaling and oxidative stress in kidney diseases. Biomolecules. 2021;11:1144. doi: 10.3390/biom11081144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu A, Banerjee H, Rojas H, et al. Differential expression of peroxiredoxins in prostate cancer: consistent upregulation of PRDX3 and PRDX4. Prostate. 2011;71:755–765. doi: 10.1002/pros.21292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck LH, Jr, Salant DJ. Membranous nephropathy: recent travels and new roads ahead. Kidney Int. 2010;77:765–770. doi: 10.1038/ki.2010.34. [DOI] [PubMed] [Google Scholar]
- Brück K, Stel VS, Gambaro G, et al. CKD prevalence varies across the European general population. J Am Soc Nephrol. 2016;27:2135–2147. doi: 10.1681/asn.2015050542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cachofeiro V, Goicochea M, de Vinuesa SC, et al. Oxidative stress and inflammation, a link between chronic kidney disease and cardiovascular disease. Kidney Int Suppl. 2008;111:S4–9. doi: 10.1038/ki.2008.516. [DOI] [PubMed] [Google Scholar]
- Daenen K, Andries A, Mekahli D, et al. Oxidative stress in chronic kidney disease. Pediatr Nephrol. 2019;34:975–991. doi: 10.1007/s00467-018-4005-4. [DOI] [PubMed] [Google Scholar]
- Daha MR, van Kooten C. Role of complement in IgA nephropathy. J Nephrol. 2016;29:1–4. doi: 10.1007/s40620-015-0245-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Descamps-Latscha B, Drüeke T, Witko-Sarsat V. Dialysis-induced oxidative stress: biological aspects, clinical consequences, and therapy. Semin Dial. 2001;14:193–199. doi: 10.1046/j.1525-139x.2001.00052.x. [DOI] [PubMed] [Google Scholar]
- Floege J, Amann K. Primary glomerulonephritides. Lancet. 2016;387:2036–2048. doi: 10.1016/s0140-6736(16)00272-5. [DOI] [PubMed] [Google Scholar]
- Foreman KJ, Marquez N, Dolgert A, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016–40 for 195 countries and territories. Lancet. 2018;392:2052–2090. doi: 10.1016/s0140-6736(18)31694-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J, Meyer K, Borucki K, et al. Multiplex immuno-MALDI-TOF MS for targeted quantification of protein biomarkers and their proteoforms related to inflammation and renal dysfunction. Anal Chem. 2018;90:3366–3373. doi: 10.1021/acs.analchem.7b04975. [DOI] [PubMed] [Google Scholar]
- Goemaere J, Knoops B. Peroxiredoxin distribution in the mouse brain with emphasis on neuronal populations affected in neurodegenerative disorders. J Comp Neurol. 2012;520:258–280. doi: 10.1002/cne.22689. [DOI] [PubMed] [Google Scholar]
- Gutierrez-Mariscal FM, Arenas-de Larriva AP, Limia-Perez L, et al. Coenzyme Q(10) supplementation for the reduction of oxidative stress: clinical implications in the treatment of chronic diseases. Int J Mol Sci. 2020;21:7870. doi: 10.3390/ijms21217870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwozdzinski K, Pieniazek A, Gwozdzinski L. Reactive oxygen species and their involvement in red blood cell damage in chronic kidney disease. Oxid Med Cell Longev. 2021;2021:6639199. doi: 10.1155/2021/6639199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han YH, Kim SU, Kwon TH, et al. Peroxiredoxin II is essential for preventing hemolytic anemia from oxidative stress through maintaining hemoglobin stability. Biochem Biophys Res Commun. 2012;426:427–432. doi: 10.1016/j.bbrc.2012.08.113. [DOI] [PubMed] [Google Scholar]
- He Y, Li S, Tang D, et al. Circulating peroxiredoxin-1 is a novel damage-associated molecular pattern and aggravates acute liver injury via promoting inflammation. Free Radic Biol Med. 2019;137:24–36. doi: 10.1016/j.freeradbiomed.2019.04.012. [DOI] [PubMed] [Google Scholar]
- Hill NR, Fatoba ST, Oke JL, et al. Global prevalence of chronic kidney disease—a systematic review and meta-analysis. PLoS ONE. 2016;11:e0158765. doi: 10.1371/journal.pone.0158765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang I, Uddin MJ, Lee G, et al. Peroxiredoxin 3 deficiency accelerates chronic kidney injury in mice through interactions between macrophages and tubular epithelial cells. Free Radic Biol Med. 2019;131:162–172. doi: 10.1016/j.freeradbiomed.2018.12.002. [DOI] [PubMed] [Google Scholar]
- Irazabal MV, Torres VE. Reactive oxygen species and redox signaling in chronic kidney disease. Cells. 2020;9:1342. doi: 10.3390/cells9061342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong J, Kim Y, Kyung Seong J, et al. Comprehensive identification of novel post-translational modifications in cellular peroxiredoxin 6. Proteomics. 2012;12:1452–1462. doi: 10.1002/pmic.201100558. [DOI] [PubMed] [Google Scholar]
- Johnson RM, Goyette G, Jr, Ravindranath Y, et al. Hemoglobin autoxidation and regulation of endogenous H2O2 levels in erythrocytes. Free Radic Biol Med. 2005;39:1407–1417. doi: 10.1016/j.freeradbiomed.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Kaartinen K, Safa A, Kotha S, et al. Complement dysregulation in glomerulonephritis. Semin Immunol. 2019;45:101331. doi: 10.1016/j.smim.2019.101331. [DOI] [PubMed] [Google Scholar]
- Kim MH, Park SJ, Kim JH, et al. Peroxiredoxin 5 regulates adipogenesis-attenuating oxidative stress in obese mouse models induced by a high-fat diet. Free Radic Biol Med. 2018;123:27–38. doi: 10.1016/j.freeradbiomed.2018.05.061. [DOI] [PubMed] [Google Scholar]
- Kim MH, Seong JB, Huh JW, et al. Peroxiredoxin 5 ameliorates obesity-induced non-alcoholic fatty liver disease through the regulation of oxidative stress and AMP-activated protein kinase signaling. Redox Biol. 2020;28:101315. doi: 10.1016/j.redox.2019.101315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krata N, Zagożdżon R, Foroncewicz B, et al. Oxidative stress in kidney diseases: the cause or the consequence? Arch Immunol Ther Exp. 2018;66:211–220. doi: 10.1007/s00005-017-0496-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee E, Lee HS. Peroxidase expression is decreased by palmitate in cultured podocytes but increased in podocytes of advanced diabetic nephropathy. J Cell Physiol. 2018;233:9060–9069. doi: 10.1002/jcp.26875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liakopoulos V, Roumeliotis S, Bozikasb A, et al. Antioxidant supplementation in renal replacement therapy patients: is there evidence? Oxid Med Cell Longev. 2019;2019:9109473. doi: 10.1155/2019/9109473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrogan A, Franssen CF, de Vries CS. The incidence of primary glomerulonephritis worldwide: a systematic review of the literature. Nephrol Dial Transplant. 2011;26:414–430. doi: 10.1093/ndt/gfq665. [DOI] [PubMed] [Google Scholar]
- Moszczuk B, Kiryluk K, Pączek L, et al. Membranous nephropathy: from research bench to personalized care. J Clin Med. 2021;10:1205. doi: 10.3390/jcm10061205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mucha K, Bakun M, Jaźwiec R, et al. Complement components, proteolysis-related, and cell communication-related proteins detected in urine proteomics are associated with IgA nephropathy. Pol Arch Med Wewn. 2014;124:380–386. doi: 10.20452/pamw.2345. [DOI] [PubMed] [Google Scholar]
- Mucha K, Foroncewicz B, Pączek L. How to diagnose and follow patients with glomerulonephritis without kidney biopsy? Pol Arch Med Wewn. 2016;126:471–473. doi: 10.20452/pamw.3510. [DOI] [PubMed] [Google Scholar]
- Na W, Yi K, Song YS, et al. Dissecting the relationships of IgG subclasses and complements in membranous lupus nephritis and idiopathic membranous nephropathy. PLoS ONE. 2017;12:e0174501. doi: 10.1371/journal.pone.0174501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagababu E, Gulyani S, Earley CJ, et al. Iron-deficiency anaemia enhances red blood cell oxidative stress. Free Radic Res. 2008;42:824–829. doi: 10.1080/10715760802459879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Leary PC, Terrile M, Bajor M, et al. Peroxiredoxin-1 protects estrogen receptor α from oxidative stress-induced suppression and is a protein biomarker of favorable prognosis in breast cancer. Breast Cancer Res. 2014;16:R79. doi: 10.1186/bcr3691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pac M, Krata N, Moszczuk B, Wyczałkowska-Tomasik A, Kaleta B, Foroncewicz B, Rudnicki W, Pączek L, Mucha K. NR3C1 Glucocorticoid Receptor Gene Polymorphisms Are Associated with Membranous and IgA Nephropathies. Cells. 2021;10(11):3186. doi: 10.3390/cells10113186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park MH, Jo M, Kim YR, et al. Roles of peroxiredoxins in cancer, neurodegenerative diseases and inflammatory diseases. Pharmacol Ther. 2016;163:1–23. doi: 10.1016/j.pharmthera.2016.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel M, Clarke AM, Bruce IN, et al. The prevalence and incidence of biopsy-proven lupus nephritis in the UK: Evidence of an ethnic gradient. Arthritis Rheum. 2006;54:2963–2969. doi: 10.1002/art.22079. [DOI] [PubMed] [Google Scholar]
- Perkins A, Nelson KJ, Parsonage D, et al. Peroxiredoxins: guardians against oxidative stress and modulators of peroxide signaling. Trends Biochem Sci. 2015;40:435–445. doi: 10.1016/j.tibs.2015.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pippias M, Kramer A, Noordzij M, et al. The European renal association—European dialysis and transplant association registry annual report 2014: a summary. Clin Kidney J. 2017;10:154–169. doi: 10.1093/ckj/sfw135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Placzek WJ, Yanagawa H, Makita Y, et al. Serum galactose-deficient-IgA1 and IgG autoantibodies correlate in patients with IgA nephropathy. PLoS ONE. 2018;13:e0190967. doi: 10.1371/journal.pone.0190967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selvaskandan H, Shi S, Twaij S, et al. Monitoring immune responses in IgA nephropathy: biomarkers to guide management. Front Immunol. 2020;11:572754. doi: 10.3389/fimmu.2020.572754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sethi S, Madden BJ, Debiec H, et al. Exostosin 1/exostosin 2-associated membranous nephropathy. J Am Soc Nephrol. 2019;30:1123–1136. doi: 10.1681/asn.2018080852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sethi S, Debiec H, Madden B, et al. Neural epidermal growth factor-like 1 protein (NELL-1) associated membranous nephropathy. Kidney Int. 2020;97:163–174. doi: 10.1016/j.kint.2019.09.014. [DOI] [PubMed] [Google Scholar]
- Sharapov MG, Goncharov RG, Filkov GI, et al. Comparative study of protective action of exogenous 2-Cys peroxiredoxins (Prx1 and Prx2) under renal ischemia-reperfusion injury. Antioxidants. 2020;9:680. doi: 10.3390/antiox9080680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma M, Vignesh P, Tiewsoh K, et al. Revisiting the complement system in systemic lupus erythematosus. Expert Rev Clin Immunol. 2020;16:397–408. doi: 10.1080/1744666x.2020.1745063. [DOI] [PubMed] [Google Scholar]
- Vassalotti JA, Fox CH, Becker BN. Risk factors and screening for chronic kidney disease. Adv Chronic Kidney Dis. 2010;17:237–245. doi: 10.1053/j.ackd.2010.03.003. [DOI] [PubMed] [Google Scholar]
- Winterbourn CC. Reconciling the chemistry and biology of reactive oxygen species. Nat Chem Biol. 2008;4:278–286. doi: 10.1038/nchembio.85. [DOI] [PubMed] [Google Scholar]
- Wu CL, Su TC, Chang CC, et al. Tubular peroxiredoxin 3 as a predictor of renal recovery from acute tubular necrosis in patients with chronic kidney disease. Sci Rep. 2017;7:43589. doi: 10.1038/srep43589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J, Liu L, Mladkova N, Li Y, Ren H, Wang W, Cui Z, Lin L, Hu X, Yu X, Xu J, Liu G, Caliskan Y, Sidore C, Balderes O, Rosen RJ, Bodria M, Zanoni F, Zhang JY, Krithivasan P, Mehl K, Marasa M, Khan A, Ozay F, Canetta PA, Bomback AS, Appel GB, Sanna-Cherchi S, Sampson MG, Mariani LH, Perkowska-Ptasinska A, Durlik M, Mucha K, Moszczuk B, Foroncewicz B, Pączek L, Habura I, Ars E, Ballarin J, Mani LY, Vogt B, Ozturk S, Yildiz A, Seyahi N, Arikan H, Koc M, Basturk T, Karahan G, Akgul SU, Sever MS, Zhang D, Santoro D, Bonomini M, Londrino F, Gesualdo L, Reiterova J, Tesar V, Izzi C, Savoldi S, Spotti D, Marcantoni C, Messa P, Galliani M, Roccatello D, Granata S, Zaza G, Lugani F, Ghiggeri G, Pisani I, Allegri L, Sprangers B, Park JH, Cho B, Kim YS, Kim DK, Suzuki H, Amoroso A, Cattran DC, Fervenza FC, Pani A, Hamilton P, Harris S, Gupta S, Cheshire C, Dufek S, Issler N, Pepper RJ, Connolly J, Powis S, Bockenhauer D, Stanescu HC, Ashman N, Loos RJF, Kenny EE, Wuttke M, Eckardt KU, Köttgen A, Hofstra JM, Coenen MJH, Kiemeney LA, Akilesh S, Kretzler M, Beck LH, Stengel B, Debiec H, Ronco P, Wetzels JFM, Zoledziewska M, Cucca F, Ionita-Laza I, Lee H, Hoxha E, Stahl RAK, Brenchley P, Scolari F, Zhao MH, Gharavi AG, Kleta R, Chen N, Kiryluk K. The genetic architecture of membranous nephropathy and its potential to improve non-invasive diagnosis. Nat Commun. 2020 doi: 10.1038/s41467-020-15383-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanagawa H, Suzuki H, Suzuki Y, et al. A panel of serum biomarkers differentiates IgA nephropathy from other renal diseases. PLoS ONE. 2014;9:e98081. doi: 10.1371/journal.pone.0098081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang HY, Lee TH. Antioxidant enzymes as redox-based biomarkers: a brief review. BMB Rep. 2015;48:200–208. doi: 10.5483/bmbrep.2015.48.4.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang YZ, Zhao Y, Yang L, et al. Characterization of 2-Cys peroxiredoxin 3 and 4 in common carp and the immune response against bacterial infection. Comp Biochem Physiol B Biochem Mol Biol. 2018;217:60–69. doi: 10.1016/j.cbpb.2017.12.012. [DOI] [PubMed] [Google Scholar]
- Zacchia M, Marchese E, Trani EM, et al. Proteomics and metabolomics studies exploring the pathophysiology of renal dysfunction in autosomal dominant polycystic kidney disease and other ciliopathies. Nephrol Dial Transplant. 2020;35:1853–1861. doi: 10.1093/ndt/gfz121. [DOI] [PubMed] [Google Scholar]
- Zhang MF, Huang J, Zhang YM, et al. Complement activation products in the circulation and urine of primary membranous nephropathy. BMC Nephrol. 2019;20:313. doi: 10.1186/s12882-019-1509-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data available upon request.
Not applicable.