Abstract
BACKGROUND:
Elevated troponin I (TnI) is common among trauma patients. TnI is an indicator of myocardial injury, but clinical diagnosis of blunt cardiac injury cannot be based solely on an increase in TnI. Therefore, this study aims to explore the changes and clinical significance of serum TnI in trauma patients.
METHODS:
The clinical data of consecutive trauma patients admitted to our trauma center between July 1, 2017 and July 31, 2020 were retrospectively analyzed. According to TnI levels within 24 hours of admission, patients were divided into the elevated and normal TnI groups. According to the TnI levels after 7 days of admission, a graph depicting a change in trend was drawn and then analyzed whether TnI was related to in-hospital mortality.
RESULTS:
A total of 166 patients (69 and 97 cases with elevated and normal TnI, respectively) were included in this study. The average hospital stay, intensive care time, mechanical ventilation time, and in-hospital mortality were higher in the elevated TnI group than in the normal TnI group (P<0.05). The TnI level of trauma patients gradually increased after admission and peaked at 48 hours (7.804±1.537 ng/mL). Subsequently, it decreased, and then recovered to normal within 7 days. However, 13 patients did not recover. Logistic regression analysis revealed that abnormal TnI at 7 days was independently related to in-hospital mortality.
CONCLUSIONS:
Trauma patients with elevated TnI levels may have a worse prognosis. Monitoring the changes in serum TnI is important, which can reflect the prognosis better than the TnI measured immediately after admission.
Keywords: Trauma, Blunt cardiac injury, Troponin I, Electrocardiography
INTRODUCTION
Trauma is a major medical and public health problem in many countries, and at least 5.8 million people die due to severe trauma every year.[1] Troponin I (TnI) is a specific indicator of myocardial injury, and up to 70% of patients with blunt chest trauma have increased levels of TnI, which plays an important role in blunt cardiac injury (BCI) diagnosis; however, there are various reasons for its increase, including hypotensive shock, traumatic brain injury, hypoxemia, and others.[2] Therefore, BCI diagnosis cannot be solely based on an increase in the TnI level. Nevertheless, the TnI has a high value in the screening and excluding BCI, and the Eastern Association for the Surgery of Trauma guidelines recommends patients suspected of BCI to undergo electrocardiogram (ECG) and TnI assessment.[3] However, the trend of TnI changes in trauma patients is rarely reported, and there is no regulation regarding the monitoring time of TnI. There is a controversy regarding the prognostic value of TnI.[4-5] Briefly, there is no conclusion on the changes and clinical values of TnI; therefore, we aim to explore the changes and clinical significance of serum TnI in trauma patients.
METHODS
Study participants
This study was a retrospective analysis. The inclusion criterion was as follows: consecutive trauma patients admitted to our trauma center between July 1, 2017 and July 31, 2020.
Exclusion criteria were as follows: (1) incomplete records; (2) time from onset to admission >24 hours; (3) previous cardiac diseases, such as coronary heart disease, arrhythmia, valvular disease, pulmonary heart disease; and (4) hypertension, diabetes, malignant tumors, kidney disease, and intracranial disease (Figure 1).
Figure 1.
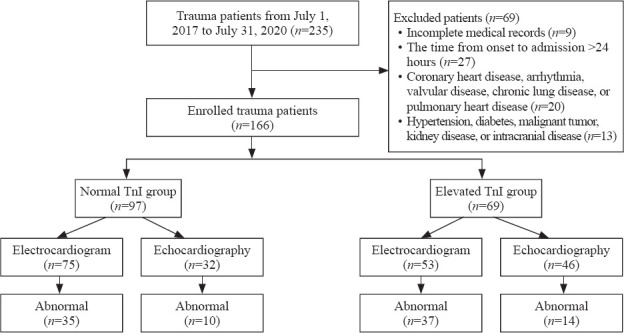
Flowchart showing the enrollment and exclusion processes.
Study design
Data on the general demographic characteristics, Injury Severity Score (ISS), TnI levels within 7 days after trauma, other laboratory examinations, ECG, echocardiography, computed tomography or magnetic resonance imaging, length of intensive care admission and hospitalization, mechanical ventilation time, and outcome of patients, along with other aspects, were collected.
ECG abnormalities included the following factors: arrhythmia (sinus bradycardia/bradycardia, premature beats, supraventricular tachycardia, atrial fibrillation, bundle branch block, and QT interval prolongation), ST-segment depression or elevation >1 mm, and T wave flat and/or inversion.[4] Echocardiographic abnormalities included the following factors: pericardial effusion, local ventricular wall motion abnormalities, acute valve dysfunction, ventricular enlargement, ventricular septal rupture, and heart thrombosis.[6] In our study, patients with elevated TnI and abnormal ECG and/or echocardiography findings were diagnosed with BCI.
Patients were divided into elevated and normal TnI groups according to whether they had increased TnI levels (≥0.04 ng/mL) within 24 hours of admission. Clinical characteristics were subsequently compared and analyzed. A graph depicting a change in trend was drawn according to TnI levels on admission, on reaching a peak point, and 7 days after admission. Patients were divided into survival and death groups. The age, sex, ISS, lactic acid level, creatinine level, diagnosis of BCI, TnI level on admission, and abnormal TnI on day 7 were included in the comparative study, and significant differences were found. Finally, we analyzed the independent correlation factors related to in-hospital mortality.
Statistical analyses
SPSS statistical software (version 22.0; IBM Corp, USA) was used for data processing. Data are presented as mean±standard deviation. Two independent sample t-tests were used to compare parameters between the groups. Furthermore, the Chi-square test was used to compare both groups, and a logistic regression analysis was performed to analyze factors related to binary variables. The P-value <0.05 was considered statistically significant.
RESULTS
During our study, there were 235 trauma patients; 36 patients were excluded because they had incomplete data or the time from onset to admission was over 24 hours; 33 patients with a history of cardiac and other chronic diseases were also excluded. Finally, 166 trauma patients were included. Sixty-nine (41.57%) patients had elevated TnI levels, whereas 97 patients had normal TnI values. Compared with the normal TnI group, the ISS and lactic acid level were higher, the heart rate was faster, and systolic blood pressure was lower in the elevated TnI group (Table 1).
Table 1.
Baseline characteristics of patients with trauma

Abnormal ECGs were found in 56.25% (72/128) of the trauma patients and were more frequent in the elevated TnI group than in the normal TnI group (69.81% vs. 46.67%, P<0.05). Arrhythmia (48.43%, 62/128) was the most common cardiac disease among the patients in this study, followed by ST-T abnormalities (13.28%, 17/128). Nevertheless, there were no significant differences in the rate of echocardiographic abnormalities between the groups (30.43% [14/46] in TnI elevated group vs. 31.25% [10/32] in normal TnI group, P>0.05). Valve regurgitation was the leading abnormal finding on bedside echocardiography, but there was no hemodynamic instability caused by acute valve dysfunction, which required emergency surgery.
In this study, 40 patients met the diagnosis of BCI, with an incidence rate of 24.10% (40/166), and 8 patients had abnormalities on ECG and echocardiography. The all-cause mortality in these patients was 25%. Compared with the normal TnI group, the average hospital stays, intensive care time, and mechanical ventilation time were longer, and the in-hospital mortality was higher in the elevated TnI group (Table 1).
The TnI level of trauma patients gradually increased after admission (1.346±0.569 ng/mL), peaked at 48 hours (7.804±1.537 ng/mL), and gradually decreased within 7 days after trauma (0.579±0.159 ng/mL), but the TnI levels of some patients (n=13) did not return to baseline values. TnI levels of patients in the normal TnI group did not elevate within 24 hours and continued to be normal for 1 week (supplementary Figure 1).
All trauma patients were divided into survival and death groups, and there were differences in ISS, abnormal TnI on day 7, lactic acid level, creatinine level, and whether BCI was diagnosed between the two groups (P<0.05) (Table 2). Further, logistic regression analysis revealed that TnI abnormality on day 7 and the lactic acid level were independently correlated with in-hospital mortality, but the TnI level on admission did not play a role in predicting the prognosis (Table 3).
Table 2.
Comparative analysis of possible death-related factors in trauma patients

Table 3.
Factors related to in-hospital mortality

DISCUSSION
In our study, patients with elevated TnI had higher ISS and lactic acid levels, faster heart rate, and lower systolic blood pressure on admission, reflecting that the patients in this group were more serious. Hajsadeghi et al[7] found that critically ill patients were more likely to be exposed to shock, anemia, tachycardia, and other factors that may cause myocardial hypoxia, which led to the release of TnI. They considered that critically ill patients had an increased risk of cardiomyocyte damage; our research also reflected indirectly that the risk and degree of cardiomyocyte damage in severely traumatized patients were high.
BCI can damage the cardiac conduction system and cause structural damage.[8] The clinical manifestations of BCI vary, ranging from asymptomatic ECG changes to life-threatening cardiac complications, and there is no gold standard for diagnosis, making early identification difficult. According to a previous study,[9] the incidence of BCI ranged from 8% to 76%, largely owing to the different diagnostic criteria. In this study, the incidence rate of BCI was 24.10%, and the all-cause in-hospital mortality rate was 25%. The diagnosis rate of BCI in the death group was significantly higher than that in surviving patients, but further regression analysis did not show that it was independently related to the in-hospital death. In BCI patients with high ISS and abnormal cardiac structure, once clinical hemodynamic and malignant arrhythmia occurred, even if they could be successfully transported to the hospital, their mortality rate was as high as 80%.[10] However, for patients whose BCI was diagnosed by abnormal TnI and/or ECG, the prognosis was usually good.[11] The majority of patients in this study did not have acute and severe cardiac structural abnormalities; therefore, the overall prognosis was good, and BCI was not an independent risk factor affecting in-hospital death.
Cardiac TnI is an important component of myocardial cell contraction and a specific indicator of heart injury; therefore, it has become a specific biomarker for the clinical diagnosis of myocardial infarction.[12] However, elevated TnI levels are related to many factors, including sex, age, renal insufficiency, heart failure, and trauma.[13] Although the diagnostic criteria for BCI are currently not uniform, TnI greatly contributes to BCI diagnosis, and previous clinical studies depicted that if ECG findings and TnI levels were normal, the predicted value was 100% for clinical exclusion of severe BCI.[14] The current guidelines recommended TnI monitoring for trauma patients with suspected cardiac injury,[3] but the specific monitoring time and clinical significance were still unclear, and there are few reports on the trend of TnI changes in trauma patients. Our study showed that the peak of TnI appeared about 48 hours after admission, and then gradually decreased. Most patients returned to normalcy within 7 days after admission. In contrast, trauma patients whose TnI did not increase within 24 hours continued to be normal in the next week. Therefore, we recommend that for patients with normal TnI immediately after admission, TnI should be monitored for 24 hours. If TnI continues to be normal, the possibility of an increase of TnI is minor. If TnI rises within 24 hours, continued monitoring of TnI levels for 7 days is recommended.
The prognostic value of TnI is still controversial, and a previous clinical study[4] has reported that the release of TnI is not related to the prognosis of trauma patients. However, the retrospective clinical study of Martin et al[15] found that increases in serum TnI were related to the patient’s overall degree of injury and that elevated TnI levels were an independent predictor of mortality in trauma patients admitted to the intensive care unit. Keskpaik et al[16] conducted a clinical study on high-sensitivity cardiac troponin T (hs-cTnT) and found that patients with elevated hs-cTnT levels had a higher ISS, higher lactic acid levels, and lower systolic blood pressure than those with normal TnT on admission. Moreover, vasopressor support was needed during treatment, and hs-cTnT >14 ng/L was associated with increased in-hospital mortality, ventilator use, and longer intensive care time. However, neither our study nor the study by Keskpaik et al[16] could prove that elevated TnI was independently related to poor prognosis, because there were differences in severity between groups. Therefore, we further found the difference between death and survival patients. Through regression analysis, we found that abnormal TnI on day 7 was independently associated with in-hospital mortality. In retrospect, the patients whose TnI levels were still abnormal after 7 days of admission usually had severe trauma; their condition worsened or more severe systemic inflammatory reaction appeared 7 days later, leading to aggravation of ischemia and hypoxia. Therefore, their risk of death was comparatively higher. We believe that changes in TnI but not the baseline TnI level play an important role in predicting the prognosis. The clinical study about TnT in intensive care conducted by Hajsadeghi et al,[7] which monitored the changes of TnT, found that the level of TnT on day 7 could predict the poor prognosis of critically ill patients. These results are in line with the results of our study.
BCI can cause various arrhythmias.[17] We found that 56.25% of patients had abnormal ECG findings. The possible mechanisms of arrhythmia included abnormal perfusion, ischemia, hypoxia, abnormal vagus/sympathetic reflex, and impaired myocardial conduction.[18] ST-T changes were also common in trauma patients,[19] which was caused by local myocardial damage as well as non-traumatic heart disease, hypoxia, electrolyte imbalance, and disease deterioration.[20]
Echocardiography is the first choice for trauma patients who are suspected to have cardiac injury, especially in patients with hemodynamic instability.[3] In our study, valvular regurgitation was a major finding. Because most patients did not have basic echocardiographic data, we could not determine it as trauma-induced valvular regurgitation, especially in patients with no relevant clinical manifestations. Speckle tracking echocardiography is a new technology that can comprehensively evaluate myocardial movement and detect subclinical myocardial injury at the early stages of development, which may improve the positive findings.[21]
This study has some limitations. First, this was a single-center retrospective clinical study with a small amount of data. Second, it was an observational study, and we recommend that further clinical studies be conducted to confirm the findings of this study.
CONCLUSIONS
Elevated TnI is common among trauma patients; TnI has great value in the diagnosis and exclusion of BCI. Trauma patients with elevated TnI levels have longer hospital stays and higher in-hospital mortality. If the TnI does not increase within 24 hours on admission, the chance of increase within 7 days is less, unless the condition worsens. In patients with elevated TnI within 24 hours, the peak occurs at 48 hours after admission, and most patients return to normalcy within 7 days. Failure to recover may be related to an increased risk of death in the hospital. Therefore, we recommend monitoring TnI levels in all trauma patients for 24 hours after admission. If TnI levels increase within 24 hours, monitoring must be continued for 7 days. If TnI does not recover after 7 days, there is a high risk of in-hospital death. Monitoring the changes in serum TnI is very important among trauma patients.
Footnotes
Funding: The study was supported by a grant from the National Key R&D Program of China (2018YFF0301103).
Ethical approval: This study was approved by the Ethics Committee of Peking University People’s Hospital.
Conflicts of interests: The authors declare that they have no competing interests.
Contributors: LWD and TBW conceived, designed the study, analyzed the data, and wrote the paper. JHZ and ZD contributed to data acquisition and analysis.
REFERENCES
- 1.GBD Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017:a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736–88. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Decavèle M, Gault N, Gauss T, Pease S, Moyer JD, Paugam-Burtz C, et al. Cardiac troponin I as an early prognosis biomarker after trauma:a retrospective cohort study. Br J Anaesth. 2018;120(6):1158–64. doi: 10.1016/j.bja.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 3.Clancy K, Velopulos C, Bilaniuk JW, Collier B, Crowley W, Kurek S, et al. Screening for blunt cardiac injury:an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73(5 Suppl 4):S301–6. doi: 10.1097/TA.0b013e318270193a. [DOI] [PubMed] [Google Scholar]
- 4.Edouard AR, Felten ML, Hebert JL, Cosson C, Martin L, Benhamou D. Incidence and significance of cardiac troponin I release in severe trauma patients. Anesthesiology. 2004;101(6):1262–8. doi: 10.1097/00000542-200412000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Joseph B, Jokar TO, Khalil M, Haider AA, Kulvatunyou N, Zangbar B, et al. Identifying the broken heart:predictors of mortality and morbidity in suspected blunt cardiac injury. Am J Surg. 2016;211(6):982–8. doi: 10.1016/j.amjsurg.2015.10.027. [DOI] [PubMed] [Google Scholar]
- 6.Sybrandy KC, Cramer MJ, Burgersdijk C. Diagnosing cardiac contusion:old wisdom and new insights. Heart. 2003;89(5):485–9. doi: 10.1136/heart.89.5.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hajsadeghi S, Gholami S, Gohardehi G, Moghadam NS, Sabet AS, Kerman SR, et al. Association between troponin T and ICU mortality, a changing trend. Cardiovasc J Afr. 2012;23(4):186–90. doi: 10.5830/CVJA-2011-034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huis In't Veld MA, Craft CA, Hood RE. Blunt cardiac trauma review. Cardiol Clin. 2018;36(1):183–91. doi: 10.1016/j.ccl.2017.08.010. [DOI] [PubMed] [Google Scholar]
- 9.Leite L, Gonçalves L, Nuno Vieira D. Cardiac injuries caused by trauma:review and case reports. J Forensic Leg Med. 2017;52:30–4. doi: 10.1016/j.jflm.2017.08.013. [DOI] [PubMed] [Google Scholar]
- 10.Leavitt BJ, Meyer JA, Morton JR, Clark DE, Herbert WE, Hiebert CA. Survival following nonpenetrating traumatic rupture of cardiac chambers. Ann Thorac Surg. 1987;44(5):532–5. doi: 10.1016/s0003-4975(10)62116-9. [DOI] [PubMed] [Google Scholar]
- 11.Yousef R, Carr JA. Blunt cardiac trauma:a review of the current knowledge and management. Ann Thorac Surg. 2014;98(3):1134–40. doi: 10.1016/j.athoracsur.2014.04.043. [DOI] [PubMed] [Google Scholar]
- 12.Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018) Circulation. 2018;138(20):e618–51. doi: 10.1161/CIR.0000000000000617. [DOI] [PubMed] [Google Scholar]
- 13.Harvell B, Henrie N, Ernst AA, Weiss SJ, Oglesbee S, Sarangarm D, et al. The meaning of elevated troponin I levels:not always acute coronary syndromes. Am J Emerg Med. 2016;34(2):145–8. doi: 10.1016/j.ajem.2015.09.037. [DOI] [PubMed] [Google Scholar]
- 14.Cho JW, Bae CH. Stress-induced cardiomyopathy with electrocardiographic ST-segment elevation in a patient with pneumothorax. World J Emerg Med. 2020;11(4):260–2. doi: 10.5847/wjem.j.1920-8642.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martin M, Mullenix P, Rhee P, Belzberg H, Demetriades D, Salim A. Troponin increases in the critically injured patient:mechanical trauma or physiologic stress? J Trauma. 2005;59(5):1086–91. doi: 10.1097/01.ta.0000190249.19668.37. [DOI] [PubMed] [Google Scholar]
- 16.Keskpaik T, Starkopf J, Kirsimägi Ü, Mihnovitš V, Lomp A, Raamat EM, et al. The role of elevated high-sensitivity cardiac troponin on outcomes following severe blunt chest trauma. Injury. 2020;51(5):1177–82. doi: 10.1016/j.injury.2019.12.037. [DOI] [PubMed] [Google Scholar]
- 17.Potkin RT, Werner JA, Trobaugh GB, Chestnut CH, 3rd, Carrico CJ, Hallstrom A, et al. Evaluation of noninvasive tests of cardiac damage in suspected cardiac contusion. Circulation. 1982;66(3):627–31. doi: 10.1161/01.cir.66.3.627. [DOI] [PubMed] [Google Scholar]
- 18.Hahn RT, Wan EY, Leon MB. Inter-ethnic differences in cardiovascular disease:impact on therapies and outcomes. JACC:Asia. 2021;1(1):117–20. doi: 10.1016/j.jacasi.2021.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guy RJ, Watkins PE, Edmondstone WM. Electrocardiographic changes following primary blast injury to the thorax. J R Nav Med Serv. 2000;86(3):125–33. [PubMed] [Google Scholar]
- 20.Berk WA. ECG findings in nonpenetrating chest trauma:a review. J Emerg Med. 1987;5(3):209–15. doi: 10.1016/0736-4679(87)90180-6. [DOI] [PubMed] [Google Scholar]
- 21.Krishnamoorthy V, Chaikittisilpa N, Lee J, Mackensen GB, Gibbons EF, Laskowitz D, et al. Speckle tracking analysis of left ventricular systolic function following traumatic brain injury:a pilot prospective observational cohort study. J Neurosurg Anesthesiol. 2020;32(2):156–61. doi: 10.1097/ANA.0000000000000578. [DOI] [PMC free article] [PubMed] [Google Scholar]


