Supplemental Digital Content is available in the text.
Introduction:
The perioperative environment is one of the most complex areas within a hospital with significant safety risks. Despite a long history of safety-focused work, a recent cluster of patient safety events prompted a renewed comprehensive approach to improve safety processes and transform culture.
Methods:
Our team comprehensively approached perioperative safety through integration across traditional silos and a focus on institutional safety culture. This approach consisted of a careful review of all events, developing Perioperative Safety Coordinating and Education teams, testing and implementing new/revised safety processes, and an ongoing evaluation plan.
Results:
Updates to our Perioperative Safety Mission and Tenets and the development of an empowered Safety Culture Champion team composed of a diverse group of frontline team members addressed our safety culture. In addition, key safety processes (time-outs, intraoperative huddles, and prevention of retained foreign bodies) were revised and implemented. Observation of key safety processes demonstrates a 90% compliance, which includes all steps and team engagement. After implementation, a span of 377 days between events was accomplished, which is significantly higher than the 33 days between events during our cluster.
Conclusions:
This work builds upon prior incremental improvements through a comprehensive investment in not only improving key processes but transforming the safety culture. Acceptable deviance from the standard process is no longer the norm. Instead, an approach that emphasizes understanding, integration, engagement, and accountability for safety by each team member for every patient, every time, every day, has been implemented.
INTRODUCTION
The journey to eliminate all harm is a marathon and not a sprint. At our institution, safety has been a focus for more than 15 years.1,2 Over this time, much has been done to improve the safety of every patient in our perioperative environment.3–9 Although this foundational work has improved patient and employee safety, we recently had a concerning cluster of significant perioperative patient safety events (associated with the time-out process, intraoperative communication, and retained foreign bodies), moving from 133 days between events to only 33 days between events, demanding us to improve further.
Improving patient safety in a meaningful and sustained manner requires continuous work. As highlighted in the recent National Steering Committee for Patient Safety report,10 four key foundational areas must be addressed in an interdependent manner to improve safety: Culture/Leadership, Patient/Family Engagement, Workforce Safety, and a Learning System. In addition, addressing the healthcare culture of individual accountability, professional silos, and inconsistent collaboration to implement and sustain change is necessary.11
The perioperative area is an environment where multiple disciplines must work collaboratively to provide high-quality, safe care. Although each patient safety event is individually reviewed via a standardized root cause analysis process with specific action plans, coordination of efforts is required to maximize impact.11
Although our long-term goal will remain the elimination of all patient safety events in our perioperative environment, the specific aim of this work is to increase the days between events to greater than 200 days and sustain this improvement. This article describes our efforts to develop and implement an integrated, comprehensive, and collaborative plan to improve and sustain overall safety.
METHODS
Our institution is a large, urban, free-standing, >600 bed pediatric academic medical center. On average, there are over 35,000 surgical procedures each year. The institution serves a diverse local, national, and international population, with the level of care ranging from routine primary care to complex, interdisciplinary quaternary care.
The perioperative executive committee (Surgeon-in-Chief, Anesthesiologist-in-Chief, Vice President (VP) Perioperative Operations, Assistant VP Patient Services, Senior Director of Operations) identified the need to integrate the safety work across the individual action plans arising from the root cause analysis of each safety event to improve implementation, spread, and sustainability. In response, we formed a Perioperative Safety Coordinating Team that included members with expertise in safety, operations, surgery, anesthesia, quality improvement, and nursing. This team was responsible for integrating, testing, implementing, including developing an education plan and sustaining the safety improvements.
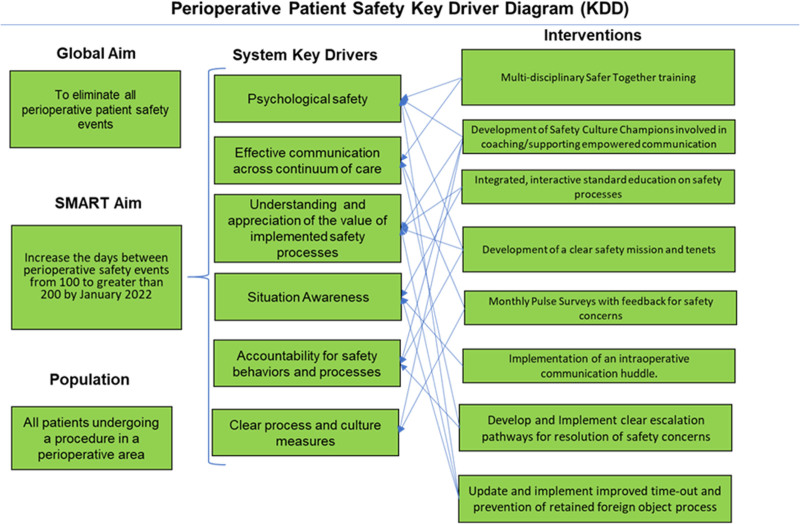
Key Driver Development: This team reviewed the action plans from each event, held meetings with key stakeholders to identify common themes and shared key drivers (Fig. 1). The key safety processes that immediately aligned with the shared themes and drivers included surgical time-outs, intraoperative communication, and prevention of retained foreign bodies. In addition, the key issues identified for building and sustaining a culture of safety included the psychological safety to speak up, effective communication, attention to detail, understanding and appreciating the value of expected safety processes, and accountability for safety behaviors and processes.
Fig. 1.
Key driver diagram.
Safety Stand-Down and Communication: Safety stand-downs, where all perioperative staff gather to review the prior year’s safety performance and opportunities to improve, have been held at our institution annually for the last 10 years. An off-cycle stand-down was held shortly after the cluster was identified and before process changes to review the events and to begin an open discussion of accountability and the impact of deviation from protocols. As a result, perioperative leadership openly accepted responsibility and committed to holding each other and all staff accountable for safety behaviors.
During weekly perioperative communications and all huddles and operations meetings, we reinforce safety principles, culture, and ongoing learnings. Weekly perioperative communications specifically start with safety and end with an emphasis on culture and expected behaviors. These updates include reminders of safety processes, feedback on revised protocols, and situation awareness of upcoming risks.
Safety Mission: Although we had a safety mission and tenets framework, it was now 10 years old and was no longer emphasized. Modifications to the new mission and tenets call on each team member to be responsible for safety, emphasizing being one team for safety. (See figure, Supplemental Digital Content 1, which shows Perioperative safety mission and tenets. http://links.lww.com/PQ9/A330.) We shared the new mission and tenets through a video module that included leaders representing all areas of the perioperative environment reading and committing to these principles. These documents were then displayed prominently throughout the perioperative areas, including family waiting areas.
Process Improvement: Multidisciplinary teams developed new and revised key safety processes. The teams tested proposed changes across various procedure types and areas to solicit feedback and engagement. The teams conducted testing over multiple plan-do-study-act (PDSA) cycles to refine the proposed changes further.12 Feedback was deliberately shared after each testing cycle in weekly perioperative communications to a diverse group of perioperative leaders, who then cascaded the information to their teams. Feedback from frontline employees in the perioperative environment was incorporated into protocol revisions.
Time-out Process: Within our environment, the first time-out occurs with the patient/family before the induction of anesthesia. The second takes place before the incision/start of the procedure. The third happens at the end of the procedure.
During testing of the first time-out, family representatives and staff feedback revealed that families often did not understand their role or the importance of this process. We, therefore, reframed this as a “safety check” to improve understanding by families. In addition, with input from our family advisory council, the team created a family education process beginning at the initial preprocedural ambulatory visit and reinforced during the preoperative preparation. During testing, the second time-out was restructured to move the introduction of all team members to the start of the time-out, rather than the end, to facilitate team communication, engagement, and empowerment. Within the third/final time-out, we included a discussion of potential ongoing patient-specific issues that may be of concern in the postoperative period and clarification as to who will place orders and perform a hand-off.
Intraoperative Huddles: We developed an intraoperative huddle process to improve intraoperative communication and situation awareness. The team identified the need for both “planned” and “unplanned” intraoperative huddles. The huddles were designed to capture a shared mental model with all team members engaged and empowered to seek clarification and additional information. Planned huddles were intended for cases deemed high-risk, either due to a complex medical history or a complicated, risky procedure. Unplanned huddles were designed to be triggered in response to physiologic changes or unexpected blood loss. Explicit criteria for each type of huddle were delineated. To ensure huddle consistency, we utilized a structured process termed VOICES (Vitals, Oxygenation/ventilation, Inotropes/pressors, Critical labs, Estimated blood loss, and Surgical time remaining). The process requires all team members to speak up to keep patients safe.
Prevention of Retained Foreign Bodies: The team performed a systematic review of episodes of retained foreign bodies at our institution over the last decade, as well as those documented in the existing literature.13 Based on this review, we emphasized avoiding interruptions during counts and the use of final sponge visual reconciliation between the surgeon, scrub nurse, and circulating nurse.
Education: The final implementation of these new safety protocols was carefully coordinated to avoid piecemeal sharing of information and allow adequate time for all staff to participate in prerequisite education before rollout. A team of medical and nursing education specialists and human resources representatives developed interactive education modules for each of the key safety improvements that incorporated our safety culture.
From a design standpoint, each education module had a similar flow that explained the “why” underlying these changes and reinforced the expectation of consistent performance by all team members. To complement these comprehensive modules, we created short just-in-time videos and made them available on our intranet site.
Safety Culture Champions: Awareness that education alone is a low-reliability intervention prompted a multidisciplinary group of Safety Culture Champions (”Champions”). Leaders nominated champions representing leadership roles and frontline staff from surgery, anesthesia, and patient services (nursing, surgical technologists, patient care assistants) based on their commitment to safety and recognition as informal leaders.
All champions completed two 60-minute training sessions. Our Human Resources team facilitated the first session and focused on coaching skills, including time for facilitated practice. The second session focused on the enhanced key safety processes. The education focused on changed practices, including an emphasis on “why” these changes were necessary. In addition, we emphasized the importance of measurement/evaluation and continuous learning. Champions were trained to use our web-based system to document the performance of key safety processes by staff members and specific coaching provided. The coaching celebrates positive behaviors and then corrects steps of protocols that have been either omitted or not performed with the expected team engagement and empowerment.
Pulse Surveys: In addition to the compliance and engagement measurement performed by the Champions, each month, an email with a link to a brief electronic survey was sent to 120 randomly selected staff to understand the perioperative safety culture. The survey consists of two questions taken from our employee engagement survey and scored on a Likert scale: (1) “There is a climate of trust in my work area;” (2) “When safety concerns have been raised in the last 3 months, how frequently have you observed others responding with grace and gratitude?” In addition, there is an option to add comments.
RESULTS
All perioperative team members were required to complete the same education modules. However, for consistency and to reinforce the mentality of one team working together in the perioperative environment, the training did not vary based on role across the traditional silos. Feedback on the education demonstrated that 70%–80% of participants found that the length of modules was appropriate, the content was well explained and demonstrated, and that the modules enhanced content learning.
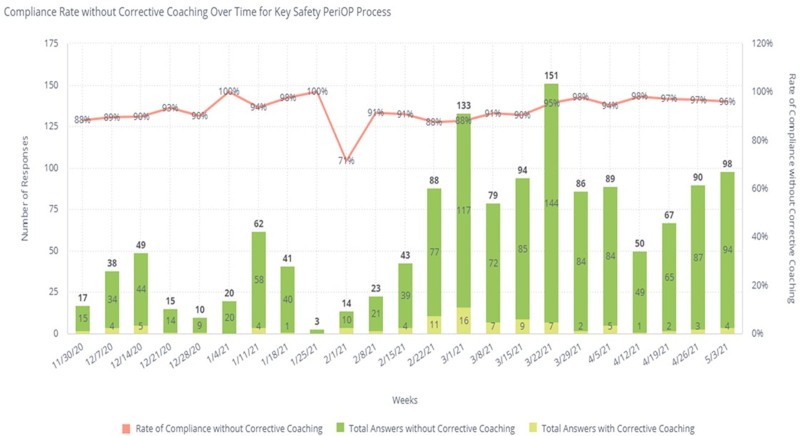
We trained a total of 103 Safety Culture Champions (12% of our perioperative team) over 4 months. During the initial 12 weeks of monitoring, the champions recorded 811 observations with an overall compliance of key process performance of just under 90% (Fig. 2). We have trained our champions to only rate a process as compliant if all steps are performed correctly and without the need for coaching and if all team members are appropriately engaged.
Fig. 2.
Key safety process monitoring number and compliance over time.
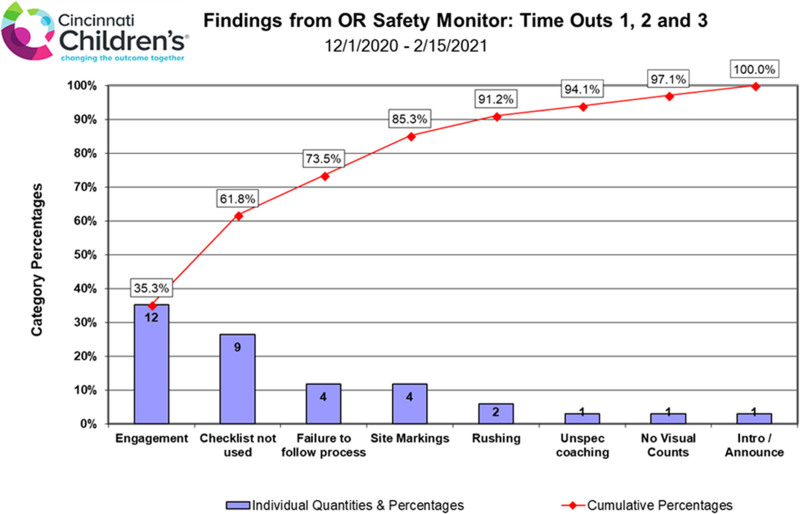
Early findings from coaching revealed specific opportunities for improvement: clarification of education materials, inconsistencies in the use of visual support tools, and diminished focus toward the end of busy days. Figure 3 demonstrates an initial Pareto chart of findings from our champions. We proactively shared key learnings and patterns with the entire culture champion team to enhance coaching and to the entire perioperative team to enhance group learning.
Fig. 3.
Pareto of initial coaching findings for our time-out process.
Over the initial 5 months of performing our pulse surveys, 230 people, 40% of those surveyed, have responded. These results serve as initial data, as this specific cohort of all those working within the perioperative area has not previously been surveyed together to allow an understanding of our culture before this most recent safety work. Currently, 75% of respondents strongly agree/agree that there is an environment of trust, and 73% of respondents feel that people always/most of the time respond with grace and gratitude. These findings compare to 83% and 68%, respectively, during our most recent institution-wide survey. Qualitative feedback to date has included both positive comments on the “improved communication and teamwork around safety” and comments that “things will never change,” supporting the need for ongoing work.
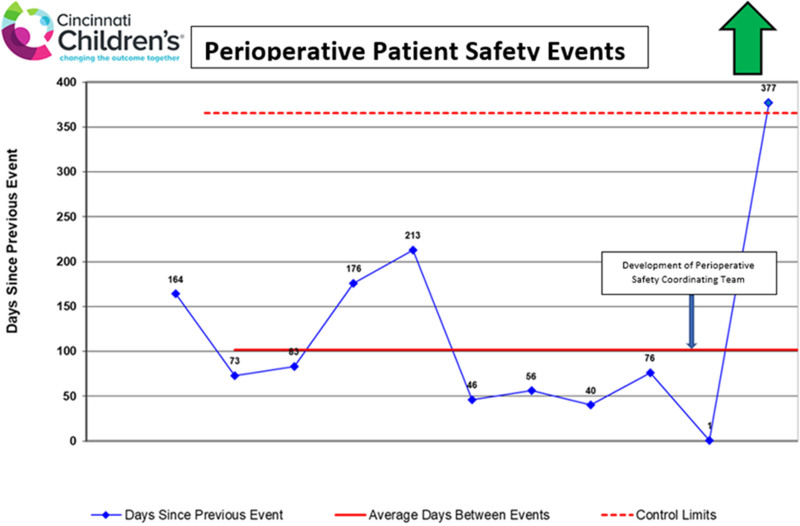
Although we need additional time to demonstrate true sustainability, we have recently gone 377 days between patient safety events, which extend outside our control limits. It is a marked improvement from 33 days between events during our cluster (Fig. 4).
Fig. 4.
Days between patient safety events run chart.
DISCUSSION
Despite a focus on safety, errors still occur in healthcare. Improvement requires constant focus, reevaluation, and learning. The majority of in-hospital adverse events are associated with the perioperative environment of care.14 Within this complex environment, three key disciplines—surgeons, anesthesiologists, and nursing—must all come together seamlessly to provide safe care. In response to a cluster of events, we addressed improving safety in an integrated fashion and designed for sustainability from the onset. Work focused on thoughtfully developed changes that incorporated institutional safety initiatives into the perioperative arena, intending to foster a more robust sustainable culture of safety. The preliminary results here demonstrate high compliance with updated key safety processes and an increased interval between patient safety events. In addition, baseline perioperative-specific safety culture metrics have been obtained and will allow us to follow trends in the culture.
Factors related to safety errors are tied to institutional context and organization.15 The Perioperative Safety Coordinating Team integrated safety processes that emphasized the institutional culture of safety and accountability and ensured these processes were organized for sustainment. This work intentionally focused on three of the four key areas recently highlighted by the Institute for Healthcare Improvement report: culture, patient/family engagement, and a learning system.10
Our team appreciated that change would require more than simple amendments to existing policies or checklists. Although teams appreciated the value in reviewing and improving current policies and checklists, they felt an emphasis on ensuring the underlying “why” was clearly understood would be necessary to elicit engaged commitment and drive sustainment. The leaders also appreciated that early engagement by stakeholders would be essential to ensure long-term support of changes. Team leaders achieved early engagement through the multiple PDSA ramps that began with small numbers of engaged staff and expanded to include an increasingly diverse and larger group of staff across multiple procedure types. The feedback received was expeditiously incorporated after each PDSA cycle, as each protocol was revised, and by communicating to participants how their input was being utilized. This type of transparency breeds trust and builds hope that sustainable changes and culture transformation are both possible.
It was essential to identify and share early successes to build momentum and garner enthusiasm and engagement. Therefore, team successes suggestive of a changing culture were actively discussed and celebrated at team meetings throughout all areas of the perioperative environment and via routine weekly email communications, within divisional staff meetings, and at institutional safety meetings. Examples include team members speaking up under several circumstances, such as during a time-out to identify an incorrect site marking, during an intraoperative huddle to share a safety concern, and numerous examples of people simply stopping to listen to each other’s concerns with grace and gratitude.
The Safety Culture Champions have helped embed the revised key safety processes by coaching on both the processes and safety culture specifics. In addition, through ongoing pulse surveys, communications, and, most importantly, actions by staff members, the changes are being institutionalized and embedded into the culture: patient safety is our number one priority.
Although we have completed implementing our integrated plan for improved safety, ongoing monitoring and measurement are critical to ensure a true and lasting impact on safety. It will also help us identify ongoing opportunities to improve continually. We have examined our events using a days between event approach for this work as we believed this would be the most consistent and reliable approach. Although we considered looking at events as a rate relative to performed procedures in our environment or by the number of operating room hours utilized, we felt this did not capture potential changing acuity and safety risks. Case volumes or hours could be increased simply by more low acuity procedures with less safety risk. We also realize that this work occurred during the COVID pandemic, which could have impacted our results. Although we had a brief period of significantly reduced case volume, many high-risk procedures continued through all phases, and our overall operating room volumes rapidly returned to near normal volumes by the summer of 2020. It is for all of these reasons that we must continue to monitor our safety performance carefully.
Not only are we monitoring for any potential near misses or safety events, but we are also continually monitoring our culture through pulse surveys and feedback from our Safety Culture Champions. Champions continue to share learnings via both monthly group email communications and quarterly group meetings. Key learnings/patterns identified from both the SCCs and the pulse surveys are communicated broadly to the entire perioperative team.
Although this work has been comprehensive, it does not directly address the challenge of predicting which patients or situations are most at-risk for safety errors. Perioperative situation awareness starting with presurgical huddles or briefs is crucial to ensure both optimal safety and outcomes. Although some specialized areas currently do this well in our system, there is no integrated system or method for sharing information among all those involved in care. In addition, ensuring situation awareness during transitions (eg, from an inpatient area, through surgical holding, the operating room, the recovery room, and then back to the inpatient unit) is necessary to maximize safety. Although the current work utilized intraoperative huddles to enhance team situation awareness during a procedure, and the final time-out added a clarification regarding the responsible individual to perform a hand-off to the next phase of care, ongoing work is in development and testing to further integrate perioperative situation awareness into our working systems.
This article is an early description of the comprehensive work. The ultimate desired outcome is a sustained reduction and elimination of safety events. Although our initial results are encouraging, the proof of lasting impact will not manifest for several years.
In conclusion, this work builds upon prior incremental improvements through a comprehensive investment in improving key processes and transforming the safety culture. Acceptable deviance from the standard process is no longer the norm. Instead, we have implemented an approach that emphasizes understanding, integration, engagement, and accountability for safety by each team member for every patient, every time, every day.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
ACKNOWLEDGMENTS
The entire Perioperative Executive Committee, each of the executive sponsors and team leaders, our education team, Safety Culture Champions, quality improvement experts, and every member of our perioperative team puts safety first every day. In addition, we would like to thank Fred Ryckman, MD and Barb Tofani, RN, NEA-BC, as key leaders who previously ignited our focus and passion around perioperative safety.
Supplementary Material
Footnotes
Published online December 15, 2021.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
To cite: Falcone RA, Simmons J, Carver AM, Mullett B, Kotagal M, Lin E, Muething S, von Allmen D. Perioperative Safety: Engage, Integrate, Empower, Sustain to Eliminate Patient Safety Events. Pediatr Qual Saf 2021;6:e495.
REFERENCES
- 1.Britto MT, Anderson JM, Kent WM, et al. Cincinnati Children’s Hospital Medical Center: transforming care for children and families. Jt Comm J Qual Patient Saf. 2006;32:541–548. [DOI] [PubMed] [Google Scholar]
- 2.Muething SE, Goudie A, Schoettker PJ, et al. Quality improvement initiative to reduce serious safety events and improve patient safety culture. Pediatrics. 2012;130:e423–e431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brady PW, Muething S, Kotagal U, et al. Improving situation awareness to reduce unrecognized clinical deterioration and serious safety events. Pediatrics. 2013;131:e298–e308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wheeler DS, Sheets AM, Ryckman FC. Improving transitions of care between the operating room and intensive care unit. Transl Pediatr. 2018;7:299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mercurio P, Shaffer Ellis A, Schoettker PJ, et al. Using improvement science methods to increase accuracy of surgical consents. AORN J. 2014;100:42–53. [DOI] [PubMed] [Google Scholar]
- 6.Schaffzin JK, Mangeot C, Sucharew H, et al. Factors affecting adherence to a preoperative surgical site infection prevention protocol. Infect Control Hosp Epidemiol. 2016;37:728–730. [DOI] [PubMed] [Google Scholar]
- 7.Ryckman FC, Schoettker PJ, Hays KR, et al. Reducing surgical site infections at a pediatric academic medical center. Jt Comm J Qual Patient Saf. 2009;35:192–198. [DOI] [PubMed] [Google Scholar]
- 8.Wagner ML, Doellman D, Forlenza KN, et al. Standardizing preoperative evaluation for pediatric central venous access: a care algorithm to improve safety. J Infus Nurs. 2020;43:262–274. [DOI] [PubMed] [Google Scholar]
- 9.Gurria JP, Nolan H, Polites S, et al. Don’t get stuck: a quality improvement project to reduce perioperative blood-borne pathogen exposure. Jt Comm J Qual Patient Saf. 2019;45:329–336. [DOI] [PubMed] [Google Scholar]
- 10.Safety NSCfP. Safer together: a national action plan to advance patient safety. Institute for Healthcare Improvement. 2020. [Google Scholar]
- 11.Advances in Patient Safety: From Research to Implementation (Volume 2: Concepts and Methodology). Agency for Healthcare Research and Quality; 2005. [PubMed] [Google Scholar]
- 12.Langley GJ, Moen RD, Nolan KM, et al. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. John Wiley & Sons; 2009. [Google Scholar]
- 13.Implementing a “visualize and verify” process for the surgical sponge count. AORN J. 2020;111:11–13. [DOI] [PubMed] [Google Scholar]
- 14.de Vries EN, Ramrattan MA, Smorenburg SM, et al. The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care. 2008;17:216–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. BMJ. 1998;316:1154–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.