PURPOSE:
Cervical cancer (CC) disproportionately affects minorities who have higher incidence and mortality rates. Standard of care for locally advanced CC involves a multimodality approach including brachytherapy (BT), which independently improves oncologic outcomes. Here, we examine the impact of insurance status and race on BT utilization with the SEER database.
MATERIALS AND METHODS:
In total, 7,266 patients with stage I-IV CC diagnosed from 2007 to 2015 were included. BT utilization, overall survival (OS), and disease-specific survival (DSS) were compared.
RESULTS:
Overall, 3,832 (52.7%) received combined external beam radiation therapy (EBRT) + BT, whereas 3,434 (47.3%) received EBRT alone. On multivariate logistic regression analysis, increasing age (OR, 0.98; 95% CI, 0.98 to 0.99; P < .001); Medicaid (OR, 0.80; 95% CI, 0.72 to 0.88; P < .001), uninsured (OR, 0.67; 95% CI, 0.56 to 0.80; P < .001), and unknown versus private insurance (OR, 0.61; 95% CI, 0.43 to 0.86; P < .001); Black (OR, 0.68; 95% CI, 0.60 to 0.77; P < .001) and unknown versus White race (OR, 0.30; 95% CI, 0.13 to 0.77; P = .047); and American Joint Committee on Cancer stage II (OR, 1.07; 95% CI, 0.93 to 1.24; P = .36), stage III (OR, 0.82; 95% CI, 0.71 to 0.94; P = .006), stage IV (OR, 0.30; 95% CI, 0.23 to 0.40; P < .001), and unknown stage versus stage I (OR, 0.36; 95% CI, 0.28 to 0.45; P < .001) were associated with decreased BT utilization. When comparing racial survival differences, the 5-year OS was 44.2% versus 50.9% (P < .0001) and the 5-year DSS was 55.6% versus 60.5% (P < .0001) for Black and White patients, respectively. Importantly, the racial survival disparities resolved when examining patients who received combined EBRT + BT, with the 5-year OS of 57.3% versus58.5% (P = .24) and the 5-year DSS of 66.3% versus 66.6% (P = .53) for Black and White patients, respectively.
CONCLUSION:
This work demonstrates notable inequities in BT utilization for CC that particularly affects patients of lower insurance status and Black race, which translates into inferior oncologic outcomes. Importantly, the use of BT was able to overcome racial survival differences, thus highlighting its essential value.
INTRODUCTION
Cervical cancer (CC) is the fourth most common cancer and the second leading cause of cancer mortality among middle-age women in the United States.1,2 Most patients present with locally advanced disease for which the standard of care includes multimodality therapy with platinum-based chemotherapy and a combination of external beam radiation therapy (EBRT) and a brachytherapy (BT) boost.3 BT is a specialized procedure entailing the direct placement of radiation into the tumor, resulting in high intratumoral dose to affect local tumor control while sparing normal surrounding organs to minimize toxicity. The addition of BT improves oncologic outcomes, including overall survival (OS).4-7 Professional societies, including the American Brachytherapy Society, American Society of Therapeutic Radiation Oncology, the Society of Gynecologic Oncology, and the National Comprehensive Cancer Network, recommend BT as an essential component of care for locally advanced CC.8-10
Because of its unique epidemiology, CC represents an ideal disease to evaluate inequalities in cancer care. CC is a highly preventable disease given the efficacy of vaccine administration and screening protocols for prevention and detection.11-14 Despite such benefits, evidence suggests that these preventative measures might have exacerbated existing socioeconomic and racial disparities. In particular, rates of vaccination and screening are significantly lower among Black women who accordingly have an increased incidence of advanced-stage disease and CC mortality rates.15-18 Furthermore, women residing in the southern United States and those of lower socioeconomic status have lower vaccination rates, higher incidence, and marked inferior outcomes.19-24
Despite its profound benefits, BT utilization has declined in the United States with approximately 50% of patients receiving standard-of-care therapy with chemotherapy, EBRT, and BT.6,25-27 Although a highly effective form of treatment, BT requires increased training, expertise, and effort, but reimbursement for BT has been suggested to be inadequate, thus fueling the decreased utilization.28 With the looming changes in reimbursement for radiation services with the initiation of the Radiation Oncology Alternative Payment Model (RO-APM) in January 2022, there are increasing concerns regarding this issue and how these changes will affect BT practice patterns and patient care accordingly. Furthermore, these reimbursement issues may further widen the disparity in BT utilization and partially explain the inferior outcomes noted in specific patient populations.29-32 As a result, we sought to evaluate the impact of socioeconomic and demographic factors on BT utilization and CC outcomes in the SEER.
MATERIALS AND METHODS
Patient Population and Data Selection
The National Cancer Institute SEER program is one of the largest national cancer databases (NCDBs) that collects and publishes clinical and survival data of approximately 30% of the patients with cancer treated in the United States.33 Patients included in this analysis were those with a diagnosis of American Joint Committee on Cancer (AJCC) stage I-IV CC between 2007 and 2015 who received radiation therapy without any surgery to their primary site (N = 7,266). All histology types were available with squamous cell carcinoma (79.2%), adenocarcinoma (9.0%), and adenosquamous subtypes (2.7%) representing the majority of patients. Patients who received only BT were excluded from this cohort. Treatment groups were divided into patients who received EBRT alone (n = 3,832) versus those who received EBRT + BT (n = 3,434).
Statistical Analysis
Data procurement was conducted using SEER*stat software (version 8.3.8).34 Descriptive statistics were used to summarize patient characteristics. Chi-square and Student t-tests were used to test for differences between categorical variable and continuous variables between treatment groups.35 OS and disease-specific survival (DSS) distributions were estimated by the Kaplan-Meier method, with DSS being measured from the date of diagnosis to the date of death or last known follow-up. Differences in survival were assessed using the log-rank test.36 A Cox proportional hazards analysis of the DSS was performed using the Cox proportional hazards model to compare outcomes between treatment groups.37 Multivariate logistic regression analysis was performed to assess for independent determinants of BT utilization. Both these models were constructed in the forward step. Variables present in the multivariate model included age at diagnosis, radiation treatment type (EBRT alone v EBRT + BT), race or ethnicity, stage at diagnosis, and insurance status. Statistical analysis was performed using JMP 15.0.0 statistical software (SAS Institute Inc, Cary, NC).38
Ethics
This study was exempt from review of the institutional review boards, as the data used are publicly available anonymized data that are compliant with the Health Insurance Portability and Accountability Act.
RESULTS
Patient Characteristics
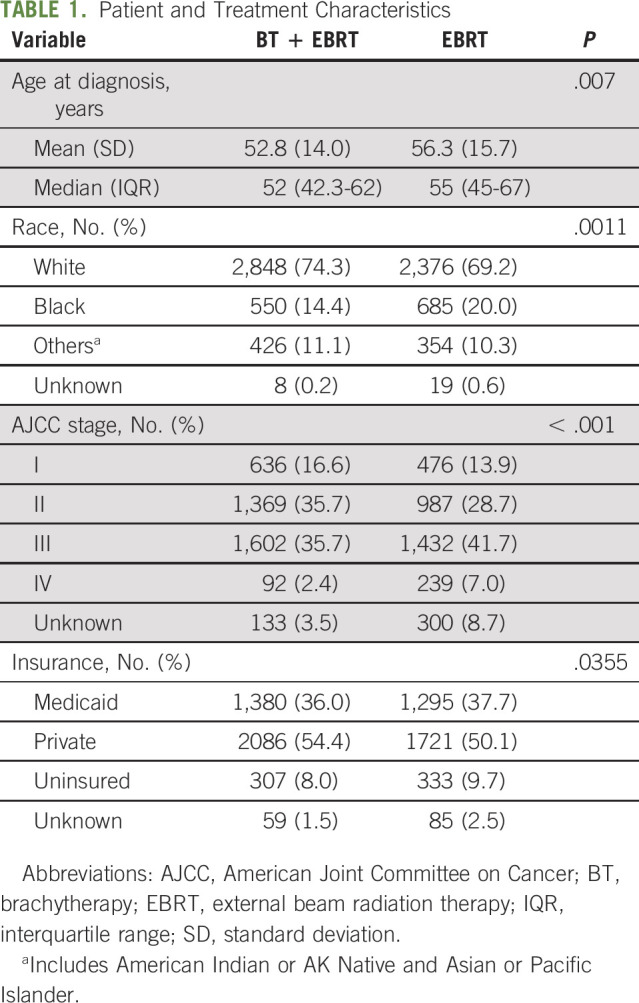
Three thousand eight hundred thirty-two (52.7%) patients received combined EBRT + BT, whereas 3,434 (47.3%) patients received EBRT alone. Table 1 depicts the differences in patient characteristics. Notably, patients treated with EBRT alone were more likely to be of older age (median 56.3 v 52.8 years; P ≤ .0001), have stage IV (7% v 2.4%; P ≤ .0001), or be unknown stage disease (8.7% v 3.5%; P ≤ .0001) and be of Black race (20% v 14.4%; P ≤ .0001).
TABLE 1.
Patient and Treatment Characteristics
BT Utilization
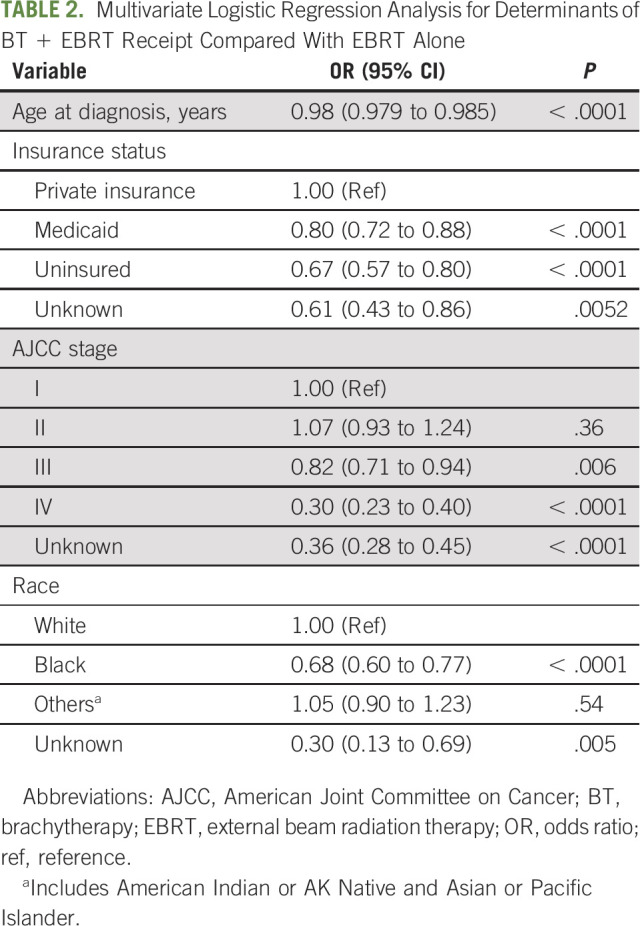
On univariate logistic regression analysis, private insurance status, lower AJCC stage, younger age, and White race were associated with increased likelihood of BT utilization. On multivariate logistic regression analysis (Table 2), increasing age at diagnosis (OR, 0.98; 95% CI, 0.98 to 0.99; P < .001); Medicaid (OR, 0.80; 95% CI, 0.72 to 0.88; P < .001), uninsured (OR, 0.67; 95% CI, 0.56 to 0.80; P < .001), and unknown insurance status versus private insurance (OR, 0.61; 95% CI, 0.43 to 0.86; P < .001); Black (OR, 0.68; 95% CI, 0.60 to 0.77; P < .001) and unknown versus White race (OR, 0.30; 95% CI, 0.13 to 0.77; P = .047); and AJCC stage II versus 1 (OR, 1.07; 95% CI, 0.93 to 1.24; P = .36), stage III versus 1 (OR, 0.82; 95% CI, 0.71 to 0.94; P = .006), stage IV versus 1 (OR, 0.30; 95% CI, 0.23 to 0.40; P < .001), and unknown stage versus stage 1 (OR, 0.36; 95% CI, 0.28 to 0.45; P < .001) were associated with decreased BT utilization.
TABLE 2.
Multivariate Logistic Regression Analysis for Determinants of BT + EBRT Receipt Compared With EBRT Alone
Survival Outcomes
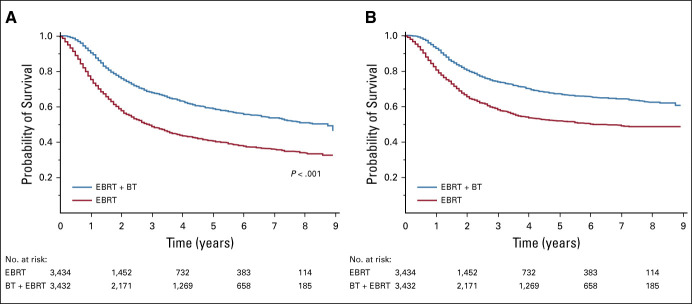
OS and DSS outcomes are displayed in Figure 1. BT + EBRT demonstrated superior OS compared with EBRT alone, with the 5-year OS of 58.8% versus 40.5%, respectively (P < .0001). Additionally, BT + EBRT was associated with improved DSS compared with EBRT alone, with the 5-year DSS of 67.0% versus 51.8%, respectively (P < .0001).
FIG 1.
Kaplan-Meier survival curves comparing outcomes by radiation treatment modality in terms of (A) overall survival and (B) disease-specific survival.
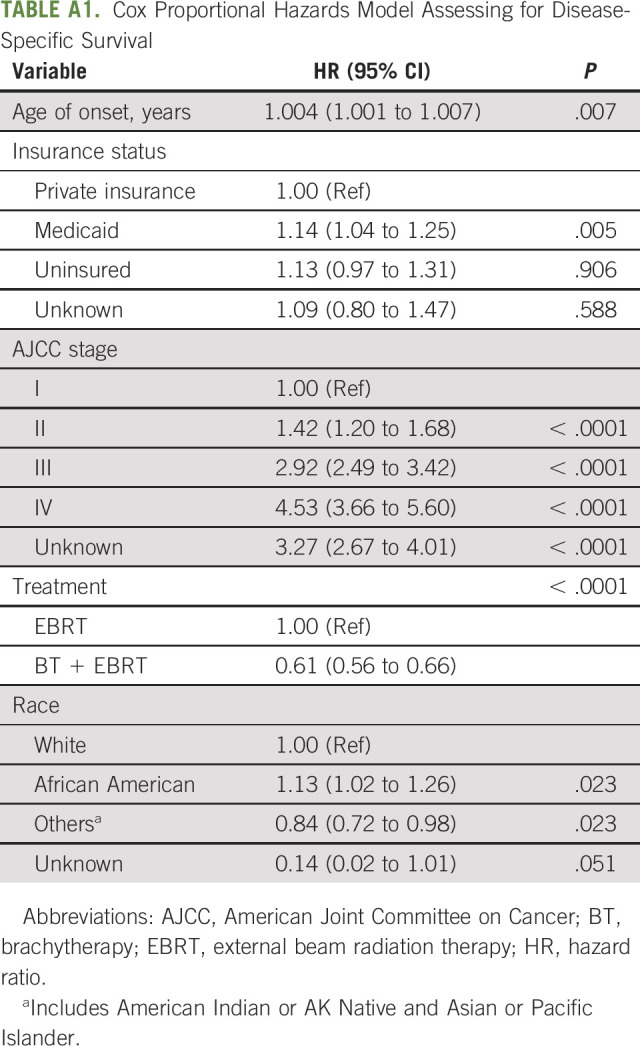
Univariate Cox proportional hazards analysis demonstrated that Medicaid insurance status, higher disease stage, and Black race are associated with poorer DSS. On multivariate Cox proportional hazards analysis (Appendix Table A1, online only), Medicaid vs private insurance (hazard ratio [HR], 1.14; 95% CI, 1.04 to 1.25; P = .007), Black versus White race (HR, 1.13; 95% CI, 1.02 to 1.26; P < .001), and increasing AJCC stage (P < .001) were associated with inferior DSS-specific survival, whereas the use of EBRT + BT versus EBRT alone (HR, 0.61; 95% CI, 0.56 to 0.66; P < .001) and Other versus White race (HR, 0.84; 95% CI, 0.72 to 0.98; P < .001) was associated with improved DSS.
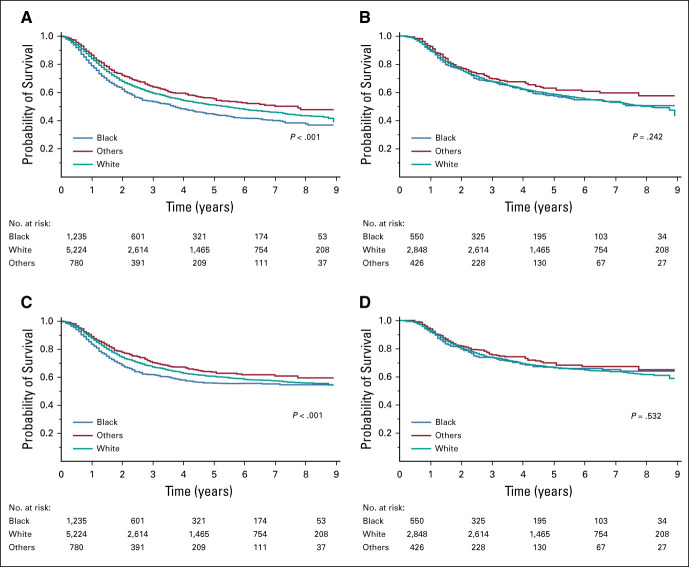
Despite Black race being a strong correlative factor for inferior OS and DSS in our cohort, a secondary survival analysis conducted in patients who received only standard-of-care therapy with combined EBRT + BT negated this racially driven survival difference (Fig 2). When comparing Black and White patients in our entire cohort, the 5-year OS was 44.2% versus 50.9% (P < .0001) and the 5-year DSS was 55.6% versus 60.5% (P < .0001) for Black and White patients, respectively. When examining only patients who received combined EBRT + BT, these racial disparities were attenuated with the 5-year OS of 57.3% versus 58.5% (P = .24) and the 5-year DSS of 66.3% versus 66.6% (P = .53) for Black and White patients, respectively.
FIG 2.
Kaplan-Meier survival curves comparing outcomes by race in terms of (A) OS in all patients, (B) OS in EBRT + BT patients, (C) DSS in all patients, and (D) DSS in EBRT + BT patients. BT, brachytherapy; DSS, disease-specific survival; EBRT, external beam radiation therapy; OS, overall survival.
DISCUSSION
Overall, this work adds to the existing body of literature demonstrating that Black women and those who are uninsured or have public insurance are significantly less likely to receive BT for the management of their CC despite this therapeutic modality being known as an independent predictor of improved DSS. From the current study, Black patients and individuals on Medicaid are demonstrated to have significantly worse OS and DSS. Significantly, we identified resolution of the racial survival disparities when comparing only patients who received BT as part of their treatment. Altogether, this work highlights the primary socioeconomic and racial disparities that exist in CC care, which may be directly reflective of the limited use of and/or access to vital BT services.
Similar findings have been reported by multiple studies.29,30,39-41 The first report evaluating such disparities was completed by the University of Chicago.39 This study noted a strong trend toward inferior 8-year cause-specific survival (CSS) in Black versus White patients (47.9 v 60.6%; P = .10) with low income (P = .001) and that the absence of BT (P = .09) is associated with worse survival in Black patients.39 A population-based study conducted from the California Cancer Registry included 4,783 patients with CC, of which 45% were treated with BT boost. This study reported BT to be an independent predictor of OS and CSS and noted Black race (P = .0002) and lower socioeconomic status (P = .0263) to be significantly associated with inferior CSS.29 An NCDB analysis performed on 15,194 patients again confirmed the positive influence of BT on survival outcomes.41 More importantly, this study emphasized notable racial disparities in quality of care as only 16.7% of Black women received standard-of-care treatment with chemotherapy, EBRT, and BT in comparison with 64.4% of White women.41 A second NCDB study that included 16,116 women found that Black women had significantly worse all-cause mortality compared with White women (median 3.9 v 5.2 years; P < .001) and were also much less likely to receive treatment with BT (OR, 0.87; 95% CI, 0.79 to 0.96; P = .007).30 Arguably, the most meaningful finding from this study was the fact that the survival detriment Black patients incurred was eliminated when limiting comparison to patients who received BT.30 This concept supported by our manuscript suggests that BT utilization may be one of the primary drivers of the inferior survival outcomes found in Black and socioeconomically disadvantaged patients and therefore makes access to BT services a potential simple solution to a complex problem. With that being said, this finding was refuted in a larger NCDB analysis consisting of more than 25,000 patients with CC where the use of BT was not found to be a driver of race-based or insurance-based survival disparities.42
The decreased utilization of BT services for Black and socioeconomically marginalized patients is likely a multifactorial problem involving socioeconomic, environmental, cultural, and health system-based issues. First, a majority of evidence suggests that BT utilization for CC, in general, has been declining across the nation.6,25-27 This itself is a result of several factors, including decreased training, a nonevidence-based movement toward noninvasive external beam boost options, and financial incentives favoring alternative radiation treatments.43 Declining utilization of BT may stem from limited access in patients who are socioeconomically disadvantaged. Access has undoubtedly been shown to be significant barrier for Black and non-White minority patients to receive specialized cancer therapy. This includes decreased enrollment in clinical trials, less access to life-prolonging therapies, and decreased screening, resulting in advanced-stage disease and limited treatment options.16,44 This finding was reported from a population-based study from the Maryland Cancer Registry that noted that Black patients frequently presented with more advanced-stage disease and were limited in their ability to receive surgical procedures for their care including BT (P < .01).40 Furthermore, lack of equitable representation of Black physicians within oncology may alienate patients and accentuate a growing level of mistrust in the medical system among such communities.44-46 Data suggest that despite the fact that Black individuals represent more than 13% of the US population, only 2% of oncologists are identified as being Black.44 Consistent with our findings, several studies have shown that patients with public (Medicaid or Medicare) insurance or those who are uninsured have decreased access to BT.30,42 Considering that Black and Hispanic patients have a disproportionately higher likelihood of having Medicaid or being uninsured, they may be restricted from obtaining resource-intensive or costly oncologic therapy such as BT.47 Finally, broader cultural, historical, and political issues, encompassing education, personal finances, and lack of domestic or family support, may disproportionately limit the access of specialized cancer therapy such as BT among patients in minority groups.44,48,49
Although there have been an increasing emphasis and awareness of racial and socioeconomic disparities within oncology, significant work is still needed to level the playing ground and provide high-quality value-based equitable and accessible cancer care nationally. Several studies have shown that patient navigation programs are promising avenues to reduce such disparities, resulting in increased adherence to cancer screening and early follow-up to minimize advanced disease presentation.50,51 Increased research, as exemplified by the recent efforts of government programs, including the NCI Community Oncology Research Program and The National Cancer Institute Community Cancer Centers Program, can make great strides in identifying important disparities in oncology and aim to find effective solutions.52,53 Expansion of Medicaid and insurance benefits such as the Affordable Care Act (ACA) has been shown to reduce disparities in cancer care, including improving access to cancer surgeries and screening programs.54-56 Importantly, a recent NCDB analysis reported that BT rates have stabilized in recent years because of the implementation of the ACA and, in particular, positively affected patients with Medicaid or those who are uninsured.57 Finally, aiming to build culturally competent cancer center, engaging minority community leaders, and encouraging minority physician recruitment in oncology can help breach significant cultural barriers, increase trust in medical providers, and expand access to necessary cancer services.58-60
One important looming event that may further affect BT practice patterns is the upcoming implementation of the RO-APM. The RO-APM represents an initiative from The Center for Medicare and Medicaid Services Innovation Center to transform Medicare reimbursement from a fee-for-service model to an episode-based payment schema.61 Although there have been several concerns with this payment model, one of the primary agreed-upon issues by professional societies has been the potential negative impact that this may have on BT services.28,62
This is especially pertinent for CC, considering that BT represents the most resource-intensive component of radiation therapy, accounting for 67% of total costs and requiring significantly more physician time.63 The RO-APM largely disincentives BT use for CC from a financial perspective because of the additional provider time, the availability of less resource-intensive (albeit inferior) alternative options, and high-cost variability on the basis of radiation sources. This amplifies existing fears regarding declining BT utilization that, on the basis of the aforementioned data, will likely disproportionately disenfranchise Black and socioeconomically disadvantaged women. Considering this, we urge Center for Medicare and Medicaid Services to strongly consider implementing changes suggested by the American Brachytherapy Society to ensure equitable access to BT for all patients with CC.28
This analysis was subject to several inherent limitations of population database studies. Accuracy of data is a common concern of national registries; however, SEER has been found to have high-quality data and excellent accuracy in the assessment of radiation utilization.64,65 Aside from survival outcomes, SEER lacks other relevant clinical end points including locoregional recurrence, patient-reported outcomes, and toxicity. Additionally, more granular socioeconomic and demographic data, as well as the presence of comorbidities, are lacking. With regard to radiation modality, information regarding dosing and palliative intent was unavailable. Although our data suggest that EBRT + BT offers improved DSS, it is important to note that staging differences between groups may be in part driving this difference. Despite these limitations, SEER is considered among the gold standard of population cancer databases because of its representation of 30% of cancer cases and high data accuracy and can thus provide a reasonable representation of general practice patterns and outcomes within the United States. Additionally, our study provides an important update of previous work but is now in the context of the ACA. This manuscript displays that despite efforts to increase insurance coverage with the ACA, racial disparities for CC continue to exist.
In conclusion, our work provides further support to a growing body of important literature that highlights disparities in access to essential BT services for Black and uninsured or Medicare patients. Such disparities unfortunately result in inferior oncologic outcomes for some patients. Importantly, we highlight several reasons for such disparities and suggest important changes that must be considered to increase access to BT and ensure equitable cancer care. Finally, we show that the use of BT can independently reverse racially driven survival differences, highlighting its fundamental importance for the management of locally advanced CC.
Appendix
TABLE A1.
Cox Proportional Hazards Model Assessing for Disease-Specific Survival
Nikhil G. Thaker
Employment: Arizona Oncology
Consulting or Advisory Role: US Oncology
Patents, Royalties, Other Intellectual Property: Software copyright for Python Programming Code for RO-APM Analysis
Firas Mourtada
Honoraria: Elekta
Consulting or Advisory Role: Siemens Healthineers
Patents, Royalties, Other Intellectual Property: GYN applicator for brachytherapy, royalty received from license by Elekta
Albert J. Chang
Stock and Other Ownership Interests: Myovant Sciences
Consulting or Advisory Role: Boston Scientific
No other potential conflicts of interest were reported.
Footnotes
D.B.-F. and K.A.N. contributed equally to this work.
AUTHOR CONTRIBUTIONS
Conception and design: David Boyce-Fappiano, Kevin A. Nguyen, Mitchell Kamrava, Peter F. Orio III, Nikhil G. Thaker, Firas Mourtada, Albert J. Chang
Provision of study materials or patients: Kevin A. Nguyen
Collection and assembly of data: David Boyce-Fappiano, Kevin A. Nguyen, Nikhil G. Thaker
Data analysis and interpretation: David Boyce-Fappiano, Kevin A. Nguyen, Olsi Gjyshi, Gohar Manzar, Chike O. Abana, Ann H. Klopp, Mitchell Kamrava, Nikhil G. Thaker, Albert J. Chang
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Socioeconomic and Racial Determinants of Brachytherapy Utilization for Cervical Cancer: Concerns for Widening Disparities
The following represents disclosure information provided by the authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Nikhil G. Thaker
Employment: Arizona Oncology
Consulting or Advisory Role: US Oncology
Patents, Royalties, Other Intellectual Property: Software copyright for Python Programming Code for RO-APM Analysis
Firas Mourtada
Honoraria: Elekta
Consulting or Advisory Role: Siemens Healthineers
Patents, Royalties, Other Intellectual Property: GYN applicator for brachytherapy, royalty received from license by Elekta
Albert J. Chang
Stock and Other Ownership Interests: Myovant Sciences
Consulting or Advisory Role: Boston Scientific
No other potential conflicts of interest were reported.
REFERENCES
- 1.Siegel RL, Miller KD, Jemal A: Cancer statistics, 2020. CA Cancer J Clin 70:7-30, 2020 [DOI] [PubMed] [Google Scholar]
- 2.Islami F, Fedewa SA, Jemal A: Trends in cervical cancer incidence rates by age, race/ethnicity, histological subtype, and stage at diagnosis in the United States. Prev Med 123:316-323, 2019 [DOI] [PubMed] [Google Scholar]
- 3.Rose PG, Bundy BN, Watkins EB, et al. : Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med 340:1144-1153, 1999 [DOI] [PubMed] [Google Scholar]
- 4.Tanderup K, Eifel PJ, Yashar CM, et al. : Curative radiation therapy for locally advanced cervical cancer: Brachytherapy is NOT optional. Int J Radiat Oncol Biol Phys 88:537-539, 2014 [DOI] [PubMed] [Google Scholar]
- 5.Karlsson J, Dreifaldt A-C, Mordhorst LB, et al. : Differences in outcome for cervical cancer patients treated with or without brachytherapy. Brachytherapy 16:133-140, 2017 [DOI] [PubMed] [Google Scholar]
- 6.Han K, Milosevic M, Fyles A, et al. : Trends in the utilization of brachytherapy in cervical cancer in the United States. Int J Radiat Oncol Biol Phys 87:111-119, 2013 [DOI] [PubMed] [Google Scholar]
- 7.Logsdon MD, Eifel PJ: FIGO IIIB squamous cell carcinoma of the cervix: An analysis of prognostic factors emphasizing the balance between external beam and intracavitary radiation therapy. Int J Radiat Oncol 43:763-775, 1999 [DOI] [PubMed] [Google Scholar]
- 8.Holschneider CH, Petereit DG, Chu C, et al. : Brachytherapy: A critical component of primary radiation therapy for cervical cancer: From the Society of Gynecologic Oncology (SGO) and the American Brachytherapy Society (ABS). Gynecol Oncol 152:540-547, 2019 [DOI] [PubMed] [Google Scholar]
- 9.National Comprehensive Cancer Network : NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines). Cervical Cancer. Version 1, 2021. https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf [Google Scholar]
- 10.Chino J, Annunziata CM, Beriwal S, et al. : Radiation therapy for cervical cancer: Executive summary of an ASTRO clinical practice guideline. Pract Radiat Oncol 10:220-234, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garland SM, Hernandez-Avila M, Wheeler CM, et al. : Quadrivalent vaccine against human papillomavirus to prevent anogenital diseases. N Engl J Med 356:1928-1943, 2007 [DOI] [PubMed] [Google Scholar]
- 12.FUTURE II Study Group : Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med 356:1915-1927, 2007 [DOI] [PubMed] [Google Scholar]
- 13.Mayrand M-H, Duarte-Franco E, Rodrigues I, et al. : Human papillomavirus DNA versus papanicolaou screening tests for cervical cancer. N Engl J Med 357:1579-1588, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Paavonen J, Jenkins D, Bosch FX, et al. : Efficacy of a prophylactic adjuvanted bivalent L1 virus-like-particle vaccine against infection with human papillomavirus types 16 and 18 in young women: An interim analysis of a phase III double-blind, randomised controlled trial. Lancet Lond Engl 369:2161-2170, 2007 [DOI] [PubMed] [Google Scholar]
- 15.Simard EP, Naishadham D, Saslow D, et al. : Age-specific trends in black–white disparities in cervical cancer incidence in the United States: 1975–2009. Gynecol Oncol 127:611-615, 2012 [DOI] [PubMed] [Google Scholar]
- 16.Wharam JF, Zhang F, Xu X, et al. : National trends and disparities in cervical cancer screening among commercially insured women, 2001–2010. Cancer Epidemiol Prev Biomark 23:2366-2373, 2014 [DOI] [PubMed] [Google Scholar]
- 17.Patel DA, Barnholtz-Sloan JS, Patel MK, et al. : A population-based study of racial and ethnic differences in survival among women with invasive cervical cancer: Analysis of Surveillance, Epidemiology, and End Results data. Gynecol Oncol 97:550-558, 2005 [DOI] [PubMed] [Google Scholar]
- 18.Weragoda J, Azuero A, Badiga S, et al. : An examination of racial differences in 5-year survival of cervical cancer among African American and white American women in the southeastern US from 1985 to 2010. Cancer Med 5:2126-2135, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu L, Deapen D, Bernstein L: Socioeconomic status and cancers of the female breast and reproductive organs: A comparison across racial/ethnic populations in Los Angeles County, California (United States). Cancer Causes Control 9:369-380, 1998 [DOI] [PubMed] [Google Scholar]
- 20.Krieger N, Quesenberry C, Peng T, et al. : Social class, race/ethnicity, and incidence of breast, cervix, colon, lung, and prostate cancer among Asian, Black, Hispanic, and White residents of the San Francisco Bay Area, 1988-92 (United States). Cancer Causes Control 10:525-537, 1999 [DOI] [PubMed] [Google Scholar]
- 21.Hirth J: Disparities in HPV vaccination rates and HPV prevalence in the United States: A review of the literature. Hum Vaccin Immunother 15:146-155, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hirth JM, Rahman M, Smith JS, et al. : Regional variations in HPV vaccination among 9-17 year old adolescent females from the BRFSS, 2008-2010. Hum Vaccin Immunother 10:3475-3483, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yoo W, Kim S, Huh WK, et al. : Recent trends in racial and regional disparities in cervical cancer incidence and mortality in United States. PLoS One 12:e0172548, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention (CDC) : National, state, and local area vaccination coverage among adolescents aged 13-17 years—United States, 2009. MMWR Morb Mortal Wkly Rep 59:1018-1023, 2010 [PubMed] [Google Scholar]
- 25.Ma TM, Harkenrider MM, Yashar CM, et al. : Understanding the underutilization of cervical brachytherapy for locally advanced cervical cancer. Brachytherapy 18:361-369, 2019 [DOI] [PubMed] [Google Scholar]
- 26.Gill JM, Mainous AG, Nsereko M: The effect of continuity of care on emergency department use. Arch Fam Med 9:333-338, 2000 [DOI] [PubMed] [Google Scholar]
- 27.Bagshaw HP, Pappas LM, Kepka DL, et al. : Patterns of care with brachytherapy for cervical cancer. Int J Gynecol Cancer 24:1659-1664, 2014 [DOI] [PubMed] [Google Scholar]
- 28.Orio PF, Thaker NG: ABS Comment Letter on the RO Model Proposal. 2019. https://www.americanbrachytherapy.org/ABS/document-server/?cfp=ABS/assets/File/public/resources/ABS-RO-Model-Comment-Letter-09162019.pdf [Google Scholar]
- 29.Mayadev J, Klapheke A, Yashar C, et al. : Underutilization of brachytherapy and disparities in survival for patients with cervical cancer in California. Gynecol Oncol 150:73-78, 2018 [DOI] [PubMed] [Google Scholar]
- 30.Alimena S, Yang DD, Melamed A, et al. : Racial disparities in brachytherapy administration and survival in women with locally advanced cervical cancer. Gynecol Oncol 154:595-601, 2019 [DOI] [PubMed] [Google Scholar]
- 31.Chaiyachati KH, Bhatt J, Zhu JM: Time for value-based payment models to adopt a disparities-sensitive frame shift. Ann Intern Med 168:509-510, 2018 [DOI] [PubMed] [Google Scholar]
- 32.Jeong I, Rosenquist R: Unintended Consequences of Bundled Payment on Racial Disparities. LDI. https://ldi.upenn.edu/healthpolicysense/unintended-consequences-bundled-payment-racial-disparities [Google Scholar]
- 33.National Cancer Institute : About the SEER Program. https://seer.cancer.gov/about/ [Google Scholar]
- 34.Surveillance Research Program, National Cancer Institute SEER*Stat Software. 2020. seer.cancer.gov/seerstat [Google Scholar]
- 35.Woolson RF, Clarke WR: Statistical Methods for the Analysis of Biomedical Data. New York, NY, John Wiley & Sons, 2011 [Google Scholar]
- 36.Kaplan EL, Meier P: Nonparametric estimation from incomplete observations. J Am Stat Assoc 53:457-481, 1958 [Google Scholar]
- 37.Cox DR: Regression models and life-tables. J R Stat Soc Ser B Methodol 34:187-220, 1972 [Google Scholar]
- 38.JMP® Statistical Discovery. SAS Institute; 2019 [Google Scholar]
- 39.Mundt AJ, Connell PP, Campbell T, et al. : Race and clinical outcome in patients with carcinoma of the uterine cervix treated with radiation therapy. Gynecol Oncol 71:151-158, 1998 [DOI] [PubMed] [Google Scholar]
- 40.Fleming S, Schluterman NH, Tracy JK, et al. : Black and white women in Maryland receive different treatment for cervical cancer. PLoS One 9:e104344, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Robin TP, Amini A, Schefter TE, et al. : Disparities in standard of care treatment and associated survival decrement in patients with locally advanced cervical cancer. Gynecol Oncol 143:319-325, 2016 [DOI] [PubMed] [Google Scholar]
- 42.Bruce SF, Joshi TV, Chervoneva I, et al. : Disparities among cervical cancer patients receiving brachytherapy. Obstet Gynecol 134:559-569, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Petereit DG, Frank SJ, Viswanathan AN, et al. : Brachytherapy: Where has it gone? J Clin Oncol 33:980-982, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Speaking up against inequity and racism. Nat Cancer. 2020;1:563-564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jacobs EA, Rolle I, Ferrans CE, et al. : Understanding African Americans' views of the trustworthiness of physicians. J Gen Intern Med 21:642-647, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Penner LA, Dovidio JF, Hagiwara N, et al. : An analysis of race-related attitudes and beliefs in Black cancer patients: Implications for health care disparities. J Health Care Poor Underserved 27:1503-1520, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.National Research Council (US) Panel on Race, Ethnicity, and Health in Later Life : Understanding Racial and Ethnic Differences in Health in Late Life: A Research Agenda, in Bulatao RA, Anderson NB. (eds): Washington, DC, National Academies Press (US), 2004. http://www.ncbi.nlm.nih.gov/books/NBK24692/ [PubMed] [Google Scholar]
- 48.Albano JD, Ward E, Jemal A, et al. : Cancer mortality in the United States by education level and race. J Natl Cancer Inst 99:1384-1394, 2007 [DOI] [PubMed] [Google Scholar]
- 49.Nonzee NJ, Ragas DM, Ha Luu T, et al. : Delays in cancer care among low-income minorities despite access. J Womens Health 24:506-514, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Raich PC, Whitley EM, Thorland W, et al. : Patient navigation improves cancer diagnostic resolution: An individually randomized clinical trial in an underserved population. Cancer Epidemiol Biomark Prev 21:1629-1638, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Phillips CE, Rothstein JD, Beaver K, et al. : Patient navigation to increase mammography screening among inner city women. J Gen Intern Med 26:123-129, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.The NCI Community Oncology Research Program (NCORP) : The NCI Community Oncology Research Program (NCORP). https://ncorp.cancer.gov/ [Google Scholar]
- 53.O’Brien DM, Hood DD, Katurakes NC, et al. : Strategies and benefits to effectively engage minority patients in their cancer care. J Clin Oncol 28, 2010. (suppl; e19501) [Google Scholar]
- 54.Sun M, Cole AP, Lipsitz SL, et al. : Trends in breast, colorectal, and cervical cancer incidence following the Affordable Care Act: Implications for cancer screening. JAMA Oncol 4:128-129, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Al-Refaie WB, Zheng C, Jindal M, et al. : Did pre-Affordable Care Act Medicaid expansion increase access to surgical cancer care? J Am Coll Surg 224:662-669, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Eguia E, Cobb AN, Kothari AN, et al. : Impact of the Affordable Care Act (ACA) Medicaid expansion on cancer admissions and surgeries. Ann Surg 268:584-590, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Schad MD, Patel AK, Glaser SM, et al. : Declining brachytherapy utilization for cervical cancer patients—Have we reversed the trend? Gynecol Oncol 156:583-590, 2020 [DOI] [PubMed] [Google Scholar]
- 58.Epner DE, Baile WF: Patient-centered care: The key to cultural competence. Ann Oncol 23:iii33-iii42, 2012 [DOI] [PubMed] [Google Scholar]
- 59.Nead KT, Linos E, Vapiwala N: Increasing diversity in radiation oncology: A call to action. Adv Radiat Oncol 4:226-228, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McNeill LH, Wu IHC, Cho D, et al. : Community outreach and engagement strategies to address breast cancer disparities. Curr Breast Cancer Rep 12:209-215, 2020 [Google Scholar]
- 61.Papanicolas I, Woskie LR, Jha AK: Health care spending in the United States and other high-income countries. JAMA 319:1024-1039, 2018 [DOI] [PubMed] [Google Scholar]
- 62.ASTRO comments to the Centers for Medicare and Medicaid Services regarding their proposed radiation oncology alternative payment model Recommendations include starting the program in a voluntary manner and scaling back excessive payment cuts. ASTRO, 2019. https://www.astro.org/News-and-Publications/News-and-Media-Center/News-Releases/2019/ASTRO-comments-to-the-Centers-for-Medicare-and-Med [Google Scholar]
- 63.Bauer-Nilsen K, Hill C, Trifiletti DM, et al. : Evaluation of delivery costs for external beam radiation therapy and brachytherapy for locally advanced cervical cancer using time-driven activity-based costing. Int J Radiat Oncol Biol Phys 100:88-94, 2018 [DOI] [PubMed] [Google Scholar]
- 64.Kraus RD, Hamilton AS, Carlos M, et al. : Using hospital medical record data to assess the accuracy of the SEER Los Angeles Cancer Surveillance Program for initial treatment of prostate cancer: A small pilot study. Cancer Causes Control 29:815-821, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Virnig BA, Warren JL, Cooper GS, et al. : Studying radiation therapy using SEER-Medicare-linked data. Med Care 40:IV-49-54, 2002 [DOI] [PubMed] [Google Scholar]