Abstract
Introduction:
The impact of injury extends beyond the hospital stay, but trauma center performance metrics typically focus on in-hospital mortality. We compared risk adjusted rates of in-hospital and long-term mortality among Pennsylvania trauma centers. We hypothesized that centers with low rates of in-hospital mortality would also have low rates of long-term mortality.
Methods:
We identified injured patients (age ≥ 65) admitted to Pennsylvania trauma centers in 2013 and 2014 using the Pennsylvania Trauma Outcomes Study, a robust, state-wide trauma registry. We matched trauma registry records to Medicare claims from the years 2013–2015. Matching variables included admission date and patient demographics including date of birth, zip, sex, and race/ethnicity. Outcomes examined were inpatient, 30-day, and 1-year mortality. Multivariable logistic regression models including presenting physiology, comorbidities, injury characteristics, and demographics were developed to calculate expected mortality rates for each trauma center at each time point. Trauma center performance was assessed using observed-to-expected ratios and ranking for in-hospital, 30-day, and 1-year mortality.
Results:
Of the 15,451 patients treated at 28 centers, 8.1% died before discharge or were discharged to hospice. Another 3.4% died within 30 days, and another 14.7% died within one year of injury. Of patients who survived hospitalization but died within 30 days, 92.5% were injured due to fall, and 75.0% sustained head injuries. Survival at one year was higher in patients discharged home (88.4%), compared to those discharged to a skilled nursing facility or long-term acute care hospital (72.7% and 52.6%, respectively). Three centers were identified as outliers (two low and one high) for in-hospital mortality, none of which were outliers when the horizon was stretched to 30 days from injury. At 30 days, two different low and two different high outliers were found.
Conclusion:
Nearly one-in-three injured older adults who die within 30 days of injury dies after hospital discharge. Hospital rankings for in-hospital mortality correlate poorly with long-term outcomes. These findings underscore the importance of looking beyond survival to discharge for quality improvement and benchmarking.
Keywords: trauma systems, long-term outcomes
Introduction
Mortality after trauma has traditionally been described with a trimodal distribution: an immediate peak at the scene of injury, a second peak of deaths occurring within 24 hours among patients who survive to hospital care but succumb to their injuries, and a third peak occurring days to weeks later as a result of injury complications or organ failure.1 Major trauma patients have higher rates of death up to 3 years after discharge.2 Organized trauma systems have been shown to flatten this third peak by reducing late deaths, likely through a combination of direct care of injuries and prevention and management of complications after injury.3,4 Despite the importance of late mortality, research and performance improvement efforts in trauma have typically focused on inpatient morbidity and mortality, and much less is known about outcomes after discharge, including residual late deaths.5
As the population of the United States ages, older adults make up a growing proportion of trauma patients, with individuals age ≥ 65 now accounting for one-in-three admissions to U.S. trauma centers.6 Designated trauma centers operating within organized trauma systems have been shown to reduce death rates up to 1 year after major trauma, including among older adults,7,8 and geriatric trauma care is a major focus of performance improvement efforts at U.S. trauma centers.6,9,10
Rates of death after discharge vary according to population and study design, but are higher among older adults.11 Including all degrees of injury severity and all hospital types, Clark et al. found a 3.7% rate of inpatient mortality among Medicare patients age ≥ 65, which more than doubled to 7.5% by 30 days.12 This stands in contrast to findings of the National Study on Costs and Outcomes of Trauma, in which an initial mortality rate of 21.3% in severely injured patients, more than half of whom are < 55 years old, increased by less than 5% at one year.13
Incorporating longer-term outcomes could open new avenues for performance improvement, particularly with regard to post-discharge care. While 30-day mortality has been recommended as a key outcome after trauma,14 fragmentation of care and data inaccessibility make post-discharge data collection rare.3 To our knowledge, death after hospital discharge has not been incorporated into trauma center benchmarking efforts. To assess long-term mortality after injury we linked data from a state-wide trauma registry to Medicare claims for injured older adults. We compared risk adjusted rates of in-hospital, 30-day and 1-year mortality among Pennsylvania trauma centers with the hypothesis that centers with low rates of in-hospital mortality would also have low rates of long-term mortality.
Methods
Data sources and population
We identified injured patients with age ≥ 65 admitted to Pennsylvania trauma centers from January 1, 2013 through December 31, 2014 using the Pennsylvania Trauma Outcomes Study (PTOS). PTOS is a robust state-wide trauma registry collected prospectively by trained registrars at every Pennsylvania trauma center and monitored by the Pennsylvania Trauma System Foundation, Mechanicsburg, PA. The foundation specifically disclaims responsibility for any analyses, interpretations, or conclusions. These years were selected due to availability of corresponding Medicare claims data. We linked trauma registry records to Medicare claims using the following matched variables: sex, residential zip code, day of birth, month of birth, year of birth, day of admission, month of admission, year of admission, and race/ethnicity. Because each data source provided only a generic hospital identification number, we first matched facilities by comparing all patient records from one facility to another. After facility matching was complete, patients were matched 1:1 within each facility using the same matching attributes listed above. Matches were discarded if more than one attribute did not match or if there was another patient pair that matched the same or better. This study was approved by the Institutional Review Board of Thomas Jefferson University and a waiver of informed consent was granted.
Inclusion and exclusion criteria
Patients were excluded if they had transfer out listed as their disposition from the trauma center in the PTOS database, as their inpatient outcomes could not be determined. There were 159 transfers out that were excluded. Centers were excluded if they treated fewer than 50 otherwise-eligible patients, resulting in the exclusion of 24 patients. One patient who was listed as dead in PTOS but not Medicare was excluded. Patients listed as discharged to hospice were included as inpatient mortality.
Analysis
Outcomes were inpatient, 30-day, and 1-year mortality. Patient demographics, comorbidities, injury mechanism, type, and severity, and presenting physiology were tabulated. Dates of death were collected from Medicare claims, which are successfully validated against social security administration records in > 98% of cases.15 We used a validated, multivariable logistic regression model to calculate expected mortality rates for each trauma center at each time point. Models included presenting physiology, comorbidities, injury characteristics, and demographics.16 The model for 30-day mortality included in-hospital deaths, to mirror what would occur if 30-day mortality were to be used as a trauma center benchmarking outcome. Center performance was assessed using observed-to-expected (O:E) ratios displayed as caterpillar plots. O:E ratios sum the actual number of deaths for patients treated at hospital and divide them by the summed total of the expected number of deaths for those patients (based on the predicted probabilities estimated for each patient from the multi-variable model described above). Centers were considered low outliers if the upper bound of the 95% confidence interval for the O:E ratio was < 1 and high outliers if the lower bound was > 1.
Results
Matches were found for 16,446 of 29,063 PTOS patients (56.7%), Of these, 15,451 (93.9%) were treated at 28 centers and met inclusion criteria. Mortality rates were equivalent in matched and unmatched patients, but more matched than unmatched patients were female (61.1% vs. 53.6%, p < 0.001), white (93.8 vs. 89.4%, p < 0.001), and injured in a fall (83.6 vs. 74.9%, p < 0.001). Matched patients were slightly older (median age 74 vs. 71, p < 0.001). For centers treating ≥ 100 eligible patients, match rates ranged from 35.0 to 68.6%.
Timing of Mortality
Of 15,451 included patients, 1,256 (8.1%) died before discharge or were discharged to hospice. Another 520 (3.4%) were discharged alive, but died within 30 days, and 2,264 (14.7%) died after discharge, between 30 days and one year after injury, for a cumulative incidence of mortality of 26.1% within one year. In other words, 29.3% of patients who died within 30 days died after hospital discharge, and 68.9% of those who died within one year of injury died after hospital discharge. There were 8 patients who died in the hospital with stays longer than 30 days. Patients recorded as discharged to hospice were considered as inpatient deaths for the purposes of this analysis. Of these 333 discharged patients (2.2%), median time to death was 9 days (IQR 6–14), with 35 (10.5%) surviving more than 30 days and 6 (1.8%) surviving more than a year. Timing of mortality is shown in Table 1.
Table 1:
Timing of Mortality by Trauma Center Discharge Destination
| Died < 30 days | Died < 1 year | Alive at 1 year | |
|---|---|---|---|
| Home/routine discharge (N=4,636) | 86 (1.9) | 454 (9.8) | 4,096 (88.4) |
| Long-term acute care hospital (N=209) | 13 (6.2) | 86 (41.2) | 110 (52.6) |
| Rehabilitation facility (N=3,126) | 58 (1.8) | 385 (12.3) | 2,684 (85.9) |
| Skilled nursing facility (N=6,222) | 362 (5.8) | 1,339 (21.5) | 4,521 (72.7) |
Overall, 83.4% of injuries were due to falls. This proportion was 92.5% of those who survived their initial hospitalization but died within 30 days, and 92.2% of those who died within one year. Seventy-five percent of patients who survived to discharge but died within 30 days had head injuries, compared to 46.3% overall. Of the 4,636 (30.0%) patients who were discharged home, 88.4% were alive at 1 year, as were 85.0% discharged to rehabilitation. By contrast, just 52.6% of patients discharged to a long-term acute care hospital, and 72.7% of those discharged to a skilled nursing facility were alive at 1 year. Patient characteristics are shown in Table 2.
Table 2:
Patient Characteristics by Timing of Mortality
| Death in hospital | Death after discharge, within 30 days of injury | Death after 30 days, within 1 year of injury | Alive at 1 year | Total | |
|---|---|---|---|---|---|
|
| |||||
| Male | 677 (11.3) | 236 (3.9) | 951 (15.8) | 4,128 (68.8) | 6,002 (38.9) |
|
| |||||
| Female | 579 (6.1) | 284 (3.0) | 1,313 (13.9) | 7,273 (77.0) | 9,449 (61.2) |
|
| |||||
| Age | 84 (78–89) | 86 (81–91) | 85 (79–90) | 80 (73–86) | 82 (74–87) |
|
| |||||
| Systolic blood pressure | 144 (122–170) | 145 (126–165) | 146 (126–167) | 150 (133–170) | 150 (131–170) |
|
| |||||
| Heart rate | 84 (73–99) | 83 (71–95) | 80 (70–93) | 80 (70–91) | 80 (70–92) |
|
| |||||
| GCS | 14 (6–15) | 15 (14–15) | 15 (14–15) | 15 (15–15) | 15 (15–15) |
|
| |||||
| Injury Severity Score | 16 (9–26) | 10 (5–14) | 9 (5–11) | 9 (5–11) | 9 (5–13) |
|
| |||||
| Body regions injured (AIS ≥2) | |||||
|
| |||||
| Head | 4,873 (68.2) | 703 (9.8) | 503 (7.0) | 1,067 (14.9) | 7,146 (46.3) |
|
| |||||
| Face | 661 (71.8) | 78 (8.5) | 58 (6.3) | 123 (13.4) | 920 (6.0) |
|
| |||||
| Chest | 2,945 (73.2) | 279 (6.9) | 189 (4.7) | 609 (15.1) | 4,022 (26.0) |
|
| |||||
| Abdomen | 1,160 (72.5) | 135 (8.4) | 78 (4.9) | 226 (14.1) | 1,599 (10.4) |
|
| |||||
| Extremities | 5,100 (78.8) | 256 (4.0) | 241 (3.7) | 875 (13.5) | 6,472 (41.9) |
|
| |||||
| Mechanism of injury | |||||
|
| |||||
| Fall | 1,019 (7.9) | 481 (3.7) | 2,078 (16.1) | 9,334 (72.3) | 12,912 (83.4) |
|
| |||||
| Pedestrian/Pedal cyclist | 6 (6.5) | 0 (0.0) | 2 (2.2) | 84 (91.3) | 92 (0.6) |
|
| |||||
| Motor vehicle crash | 160 (8.9) | 22 (1.2) | 122 (6.8) | 1,500 (83.1) | 1,804 (11.7) |
|
| |||||
| Firearm injury | 34 (54.8) | 0 (0.0) | 4 (6.5) | 24 (38.7) | 62 (−0.4) |
|
| |||||
| Struck | 5 (2.1) | 9 (3.8) | 23 (9.7) | 200 (84.4) | 237 (1.5) |
|
| |||||
| Cut or stabbed | 7 (10.3) | 1 (1.5) | 4 (5.9) | 56 (82.4) | 68 (0.4) |
|
| |||||
| Other | 22 (10.2) | 7 (3.2) | 22 (10.2) | 165 (76.4) | 216 (1.4) |
|
| |||||
| Comorbidities | |||||
|
| |||||
| Heart disease | 585 (10.2) | 250 (4.4) | 1,084 (18.9) | 3,815 (66.5) | 5,734 (37.1) |
|
| |||||
| Liver disease | 20 (14.3) | 5 (3.6) | 43 (30.7) | 72 (51.4) | 140 (0.9) |
|
| |||||
| Cancer | 83 (17.1) | 45 (9.3) | 134 (27.6) | 223 (46.0) | 485 (3.1) |
|
| |||||
| Hypertension | 849 (7.3) | 407 (3.5) | 1,771 (15.3) | 8,542 (73.8) | 11,569 (74.9) |
|
| |||||
| Diabetes | 342 (8.1) | 158 (3.7) | 673 (15.9) | 3,060 (72.3) | 4,233 (27.4) |
|
| |||||
| Coagulopathy/anticoagulants/antiplatelet | 539 (10.3) | 213 (4.1) | 891 (17.0) | 3,606 (68.7) | 5,249 (34.0) |
| Functional dependence | 141 (7.4) | 116 (6.1) | 437 (23.0) | 1,206 (63.5) | 1,900 (12.3) |
Multivariable regression results
Results of multivariable logistic regression models for mortality at each time point are shown in Table 3. For inpatient mortality, the area under the receiver-operator curve was 0.85 and the Hosmer-Lemeshow test showed no significant lack of fit (p=0.15). Factors associated with in-hospital mortality included male sex, older age, higher maximum AIS overall and for the head/neck region, motor vehicle crash or firearm injury, transfer status, and abnormal vital signs or GCS motor score. Comorbidities associated with in-hospital mortality included heart disease, liver disease, cancer, diabetes, and coagulopathy. Hypertension was associated with lower odds of death.
Table 3:
Multivariable logistic regression results
| Inpatient mortality | 30-day mortality | 1-year mortality* | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age | 1.05 (1.04, 1.06) | 1.08 (1.07, 1.09) | 1.08 (1.07, 1.09) |
| Female | 0.68 (0.58, 0.8) | 0.63 (0.56, 0.71) | 0.68 (0.61, 0.75) |
| Mechanism (reference = fall) | |||
| Cut/pierce | 0.75 (0.2, 2.8) | 0.75 (0.26, 2.17) | 0.33 (0.12, 0.94) |
| Motorvehicle crash | 1.45 (1.14, 1.84) | 0.94 (0.76, 1.14) | 0.44 (0.35, 0.53) |
| Pedestrian/cyclist | 1.04 (0.35, 3.05) | 0.54 (0.19, 1.52) | 0.19 (0.05, 0.79) |
| Firearm | 3.76 (1.73, 8.16) | 2.44 (1.2, 4.97) | 0.59 (0.19, 1.86) |
| Struck | 0.53 (0.21, 1.38) | 0.75 (0.42, 1.34) | 0.56 (0.35, 0.9) |
| Other | 0.61 (0.31, 1.18) | 0.99 (0.62, 1.58) | 0.69 (0.45, 1.06) |
| Transfer patient | 1.25 (1.04, 1.5) | 1.22 (1.06, 1.4) | 1.09 (0.97, 1.23) |
| Systolic blood pressure | 0.99 (0.99, 1) | 0.99 (0.99, 1) | 0.99 (0.99, 0.99) |
| Systolic Blood pressure ≤ 40 | 5.99 (1.79, 20.09) | 4.23 (1.43, 12.53) | 0.32 (0.03, 3.15) |
| Heart rate | 1.01 (1.01, 1.01) | 1.01 (1.01, 1.01) | 1.01 (1.01, 1.01) |
| GCS motor response (reference = 6) | |||
| 1 | 30.03 (23.26, 38.78) | 20.69 (15.98, 26.78) | 3.1 (1.99, 4.82) |
| 2 | 20.97 (8.09, 54.36) | 25.49 (8.64, 75.2) | 8.71 (1.29, 58.68) |
| 3 | 28.77 (14.24, 58.15) | 20.75 (9.89, 43.53) | 8.03 (2.35, 27.49) |
| 4 | 15.1 (10.26, 22.24) | 16.08 (10.88, 23.78) | 4.03 (2.19, 7.41) |
| 5 | 4.47 (3.35, 5.95) | 4.36 (3.44, 5.52) | 2.63 (1.99, 3.47) |
| Maximum AIS head/neck | 1.17 (1.09, 1.25) | 1.19 (1.13, 1.25) | 1.02 (0.98, 1.06) |
| Maximum AIS extremities | 0.86 (0.73, 1.02) | 0.89 (0.79, 1) | 1.03 (0.93, 1.14) |
| Maximum AIS | 1.4 (1.24, 1.59) | 1.31 (1.2, 1.44) | 1.03 (0.96, 1.11) |
| Comorbidities | |||
| Heart disease | 1.46 (1.24, 1.73) | 1.44 (1.27, 1.63) | 1.52 (1.37, 1.68) |
| Liver disease | 1.71 (1.19, 2.46) | 3.12 (2.42, 4.01) | 3.91 (3.07, 4.98) |
| Cancer | 2.73 (1.51, 4.94) | 2.01 (1.2, 3.37) | 3.72 (2.42, 5.72) |
| Hypertension | 0.72 (0.61, 0.87) | 0.83 (0.72, 0.95) | 0.99 (0.88, 1.12) |
| Diabetes | 1.21 (1.02, 1.45) | 1.21 (1.06, 1.39) | 1.29 (1.15, 1.44) |
| Coagulopathy | 1.46 (1.24, 1.73) | 1.33 (1.18, 1.51) | 1.15 (1.03, 1.27) |
includes only those who survived to discharge and ≥ 30 days
For 30-day mortality using the same variables, the AUC was 0.81 and the Hosmer-Lemeshow test showed no significant lack of fit (p=0.25). Independent predictors of 30-day mortality were very similar to in-hospital mortality. Motor vehicle crash was not associated with mortality at 30 days. The impact of liver disease was more pronounced, and the impact of physiologic indicators was attenuated.
For 1-year mortality, the AUC was 0.73, again with no significant lack of fit (Hosmer-Lemeshow p-value 0.34). Indicators of physiology were not significant, with the exception of depressed GCS, and injury severity was not significant, while the role of comorbidities was larger. Compared to patients injured in a fall, those with a cut or stab wound had lower odds of 1-year mortality (OR 0.33, 95% CI 0.12, 0.94) as did those injured in a motor vehicle crash (OR 0.44, 95% CI 0.35, 0.53), a pedestrian or pedal cyclist crash (OR 0.19, 95% CI 0.05, 0.79), or struck (OR 0.56, 95% CI 0.35, 0.90).
Center-level comparison
Timing of mortality by center is shown in Figure 1. Focusing on in-hospital mortality, we identified 2 low outliers for mortality, and one high outlier (poor performer), as shown in Figure 2. For 30-day mortality (including in-hospital deaths), none of these three were outliers, but 2 different centers were identified as low outliers and 2 as high outliers, as shown in Figure 3. While the remainder of centers had adjusted mortality rates whose confidence intervals crossed one, all but one changed its ranking.
Figure 1:

Timing of Mortality for Pennsylvania Trauma Patients Age ≥ 65, 2013–2014, by Trauma Center
Figure 2:
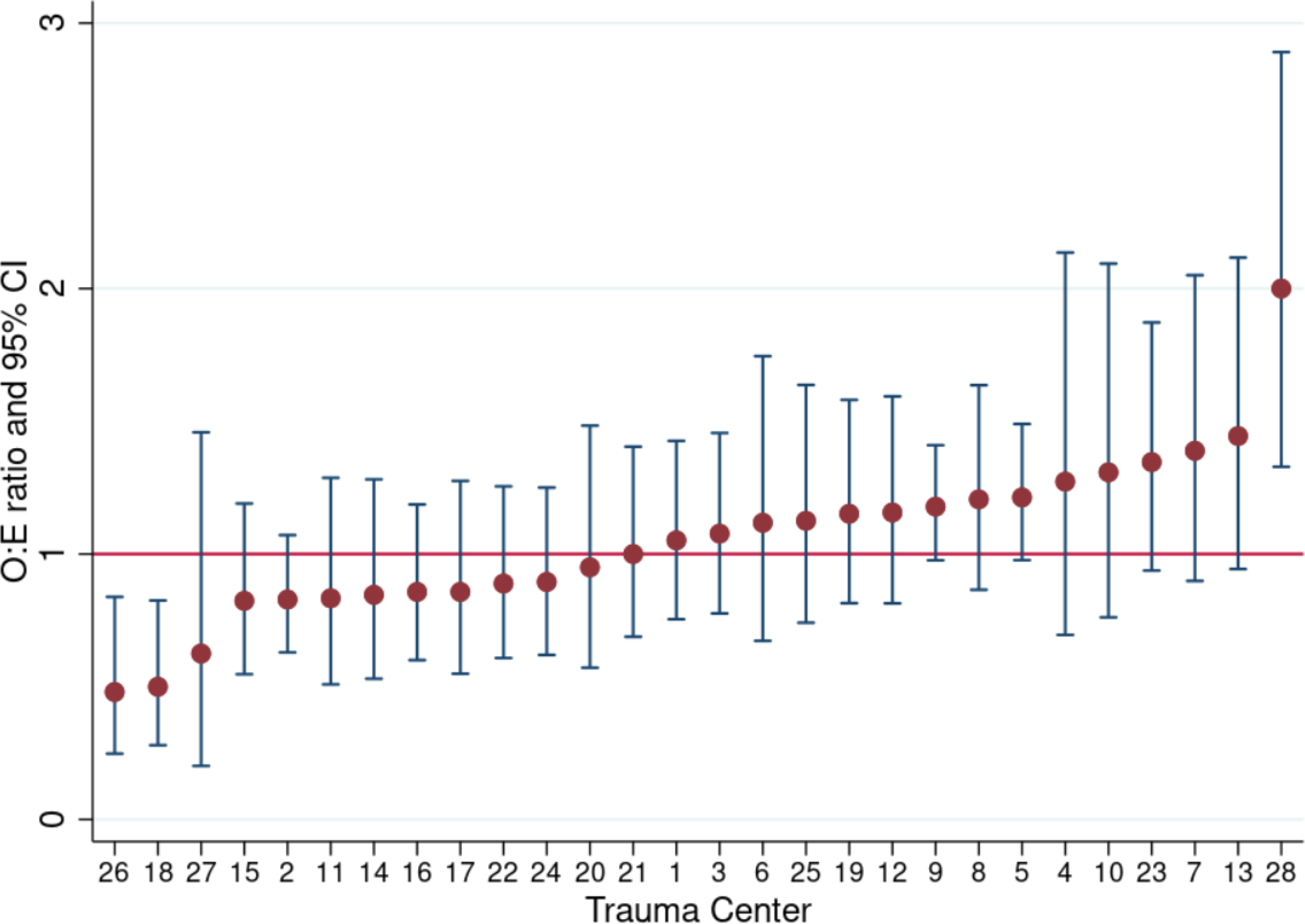
Trauma Center Performance for In-Hospital Mortality
Figure 3:
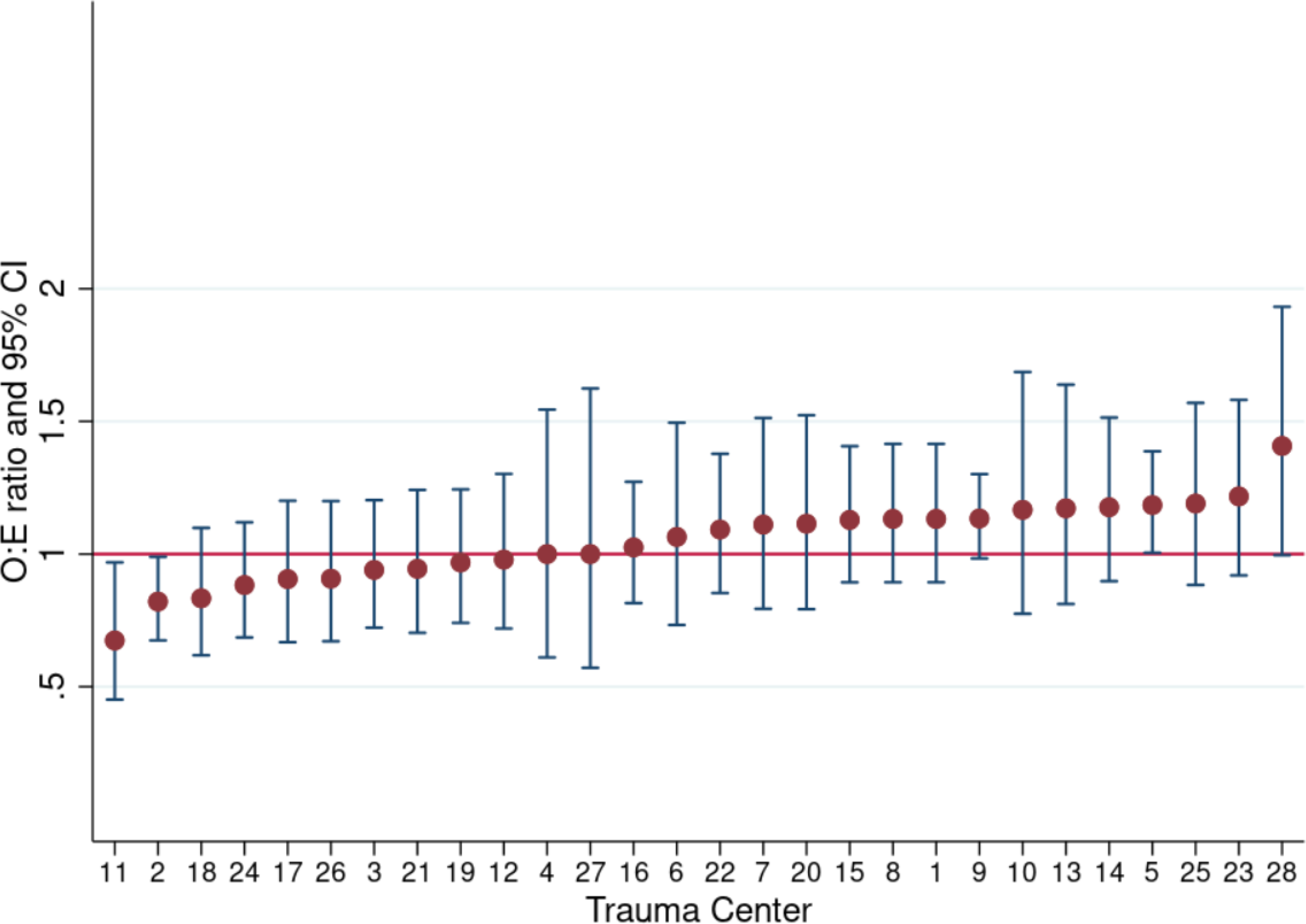
Trauma Center Performance for 30-day Mortality
Discussion
Among Medicare beneficiaries age ≥ 65 admitted to Pennsylvania trauma centers in 2013 and 2014, 8.1% died in the hospital and another 3.4% died after discharge but within 30 days. While risk factors associated with death in the hospital or in the first 30 days were very similar, center rankings and outlier status changed substantially when the threshold for mortality was extended to thirty days, which has implications for trauma center performance benchmarking.
Our results confirm prior studies that found elevated risk of death in injured patients well beyond the immediate post-injury period.2,12 To our knowledge, these results have not previously been applied in the context of trauma center benchmarking. While 30-day outcomes have been recommended for trauma quality improvement, post-discharge outcomes are not routinely captured by trauma registrars, and there are substantial logistical barriers to expanding the time horizon of the trauma registry. However, we found that the measurement horizon impacted benchmarking significantly, identifying new high and low performing centers and potentially leading to new areas of focus for performance improvement.
It is not surprising that age and comorbidities accounted for higher odds of death further out from injury, while immediate physiology and injury severity were less significant in the long term. Our results may reflect underlying patient frailty not clearly captured in the database. For example, injury mechanisms that initially conferred higher risk, such as motor vehicle crashes, appeared protective among survivors. We suspect that these mechanisms of injury are more likely to occur in those patients who were more able and active at baseline, whereas the group injured by falls are more frail overall.16,17 Future work should leverage the power of big data to determine whether claims data preceding the fall could be used to predict long term outcomes.
One in four patients died within one year of injury, indicating a long third peak, or third plateau of injury deaths that accrue form a combination of pre-existing health and frailty, injury factors, and treatment. Risk was highest in patients with head injuries, who fell, and who were discharged to skilled nursing facilities. These populations may represent important areas of focus for performance improvement. Injury hospitalization may also uncover pre-existing, but unacknowledged debility. This information can also be incorporated into conversations with patients and their families who have unanswered questions about life after the hospital. Hemorrhage and brain injury account for more than 80% of early deaths after injury. Head injury remains an important cause of deaths in those who survive the immediate post-injury period, with sepsis, lung injury, and multisystem organ failure contributing to later in-hospital deaths.3 Ghorbani et al found that 10% of deaths within 30 days of injury were not related to the injury itself.19 These deaths often occurred after low energy blunt injury. In a study of deaths occurring within 30 days of discharge after an injury admission, less than one-in-five were directly related to injury.20 Grossman et al studied geriatric trauma patients who survived severe injuries (ISS ≥ 30). Although 1/3 died in the hospital, median survival for those discharged alive was more than 3 years, and more than 2/3 ultimately returned to living at home.21 Routine trauma follow up can miss both injuries and medical complications. In one study, 17% of patients contacted one month after injury reported issues that were not identified in routine trauma follow up, although nearly all patients sought outpatient or emergency department medical care. These included severe pain, missed injuries, infections, venous thromboembolism, and mental illness.22 These outcomes may represent missed opportunities to intervene in medically fragile patients.
Limitations of this study include those inherent in the data sources. These data are from 2013–2014, and with the rise in geriatric trauma over the last several years has come an increased focus on quality of care for these patients. It remains to be seen how these efforts will impact short- and long-term outcomes for injured older adults. Although the quality control processes of the PTOS database are excellent, coding may vary from center to center, introducing bias. In particular, patients who died early after presentation may have had less thorough documentation of their injuries or comorbidities. Despite the rigorous matching process, mismatches remain possible; if an injured patient was matched to a different Medicare beneficiary, the outcome of death may have been mislabeled. For this analysis, we emphasized the accuracy of the match over the completenss of the population to ensure that our outcomes assessment was as accurate as possible. Therefore, patients who were unmatched likely had Medicare claims but may have had demographic data used for matching mis-recorded in one dataset or the other. Unmatched patients were different from matched patients, limiting generalizability to the unmatched population. Because long-term outcomes are unknown for unmatched patients, center-level results may be misestimated. Of 28 centers, 24 had match rates over 50%. The median center-level match rate was 57%, with a range from 35–69%. Lastly, PTOS provides detailed clinical data, but is geared toward evaluating immediate outcomes of trauma. Longer term mortality is likely less closely related to an index injury, and other factors not included here may be more predictive. Unfortunately, we do not have data on cause of death after hospital discharge that might allow us to assess the role of injury.
Conclusion
Injured older adults who survive their initial hospitalization are at high risk of death in the immediate post-discharge period, and in the first year after injury. Patients and families should be counseled about these risks, particularly for older patients, those with head injuries, and those discharged to a skilled nursing facility. Additional attention to post-discharge care and home transitions might serve both to identify patients at risk and to reduce post-discharge mortality in the injured elderly. Moreover, trauma center benchmarking initiatives should incorporate 30 day outcomes into center-level comparisons and performance improvement initiatives.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Elinore J. Kaufman, Division of Traumatology, Surgical Critical Care, and Emergency Surgery, University of Pennsylvania Perelman School of Medicine, Penn Presbyterian Medical Center, Medical Office Building Suite 120, 51 N. 39th Street, Philadelphia, PA 19104.
Alexis Zebrowski, Department of Emergency Medicine, Icahn School of Medicine at Mount Sinai.
Daniel N. Holena, Division of Traumatology, Surgical Critical Care, and Emergency Surgery, University of Pennsylvania Perelman School of Medicine.
Phillipe Loher, Computational Medicine Center, Thomas Jefferson University.
Douglas J. Wiebe, Department of Biostatistics, Epidemiology, and Informatics, and Department of Surgery, University of Pennsylvania Perelman School of Medicine.
Brendan G. Carr, Department of Emergency Medicine, Icahn School of Medicine at Mount Sinai.
References
- 1.Demetriades D, Kimbrell B, Salim A, et al. Trauma Deaths in a Mature Urban Trauma System: Is “Trimodal” Distribution a Valid Concept? Journal of the American College of Surgeons. 2005;201(3):343–348. doi: 10.1016/j.jamcollsurg.2005.05.003 [DOI] [PubMed] [Google Scholar]
- 2.Shafi S, Renfro LA, Barnes S, et al. Chronic consequences of acute injuries: worse survival after discharge. J Trauma Acute Care Surg. 2012;73(3):699–703. doi: 10.1097/TA.0b013e318253b5db [DOI] [PubMed] [Google Scholar]
- 3.Sobrino J, Shafi S. Timing and causes of death after injuries. Proc (Bayl Univ Med Cent). 2013;26(2):120–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gunst M, Ghaemmaghami V, Gruszecki A, Urban J, Frankel H, Shafi S. Changing epidemiology of trauma deaths leads to a bimodal distribution. Proc (Bayl Univ Med Cent). 2010;23(4):349–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shafi S, Nathens AB, Cryer HG, et al. The Trauma Quality Improvement Program of the American College of Surgeons Committee on Trauma. J Am Coll Surg. 2009;209(4):521–530.e1. doi: 10.1016/j.jamcollsurg.2009.07.001 [DOI] [PubMed] [Google Scholar]
- 6.Kozar RA, Arbabi S, Stein DM, et al. Injury in the aged: Geriatric trauma care at the crossroads. J Trauma Acute Care Surg. 2015;78(6):1197–1209. doi: 10.1097/TA.0000000000000656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MacKenzie Ellen J., Rivara Frederick P., Jurkovich Gergory J., et al. A national evaluation of the effect of trauma-center care on mortality. New Engl J Med. 2006;354:366–378. [DOI] [PubMed] [Google Scholar]
- 8.Kaufman EJ, Ertefaie A, Small DS, Holena DN, Delgado MK. Comparative Effectiveness of Initial Treatment at Trauma Center vs Neurosurgery-Capable Non-Trauma Center for Severe, Isolated Head Injury. J Am Coll Surg. Published online March 1, 2018. doi: 10.1016/j.jamcollsurg.2018.01.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Newgard CD, Caughey A, McConnell KJ, et al. Comparison of Injured Older Adults Included in vs Excluded From Trauma Registries With 1-Year Follow-up. JAMA Surg. 2019;154(9):e192279–e192279. doi: 10.1001/jamasurg.2019.2279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trauma Quality Improvement Program (TQIP). American College of Surgeons. Accessed November 18, 2020. https://www.facs.org/quality-piograms/trauma/tqp/center-programs/tqip [Google Scholar]
- 11.Skaga NO, Eken T, Jones JM, Steen PA. Different definitions of patient outcome: consequences for performance analysis in trauma. Injury. 2008;39(5):612–622. doi: 10.1016/j.injury.2007.11.426 [DOI] [PubMed] [Google Scholar]
- 12.Clark DE, DeLorenzo MA, Lucas FL, Wennberg DE. Epidemiology and Short-Term Outcomes of Injured Medicare Patients. Journal of the American Geriatrics Society. 2004;52(12):2023–2030. doi: 10.1111/j.1532-5415.2004.52560.x [DOI] [PubMed] [Google Scholar]
- 13.MacKenzie EJ, Rivara FPM, Jurkovich GJ, et al. The National Study on Costs and Outcomes of Trauma. Journal of Trauma-Injury Infection. 2007;63(6). doi: 10.1097/TA.0b013e31815acb09 [DOI] [PubMed] [Google Scholar]
- 14.Ringdal KG, Coats TJ, Lefering R, et al. The Utstein template for uniform reporting of data following major trauma: A joint revision by SCANTEM, TARN, DGU-TR and RITG. Scand J Trauma Resusc Emerg Med. 2008;16:7. doi: 10.1186/1757-7241-16-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Death Information in the Research Identifiable Medicare Data | ResDAC Data Dictionary. Accessed April 9, 2021. https://resdac.org/articles/death-information-research-identifiable-medicare-data [Google Scholar]
- 16.Wiebe DJ, Holena DN, Delgado MK, McWilliams N, Altenburg J, Carr BG. The Pennsylvania Trauma Outcomes Study Risk-Adjusted Mortality Model: Results of a Statewide Benchmarking Program. Am Surg. 2017;83(5):445–452. [PMC free article] [PubMed] [Google Scholar]
- 17.Alamgir H, Muazzam S, Nasrullah M. Unintentional falls mortality among elderly in the United States: Time for action. Injury. 2012;43(12):2065–2071. doi: 10.1016/j.injury.2011.12.001 [DOI] [PubMed] [Google Scholar]
- 18.Ayoung-Chee P, McIntyre L, Ebel BE, Mack CD, McCormick W, Maier RV. Long-term outcomes of ground-level falls in the elderly: Journal of Trauma and Acute Care Surgery. 2014;76(2):498–503. doi: 10.1097/TA.0000000000000102 [DOI] [PubMed] [Google Scholar]
- 19.Ghorbani P, Falkén M, Riddez l, Sundelöf M, Oldner A, Strömmer L. Clinical review is essential to evaluate 30-day mortality after trauma. Scand J Trauma Resusc Emerg Med. 2014;22:18. doi: 10.1186/1757-7241-22-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mullins RJ. adequacy of Hospital Discharge Status as a Measure of Outcome Among Injured Patients. JAMA. 1998;279(21):1727. doi: 10.1001/jama.279.21.1727 [DOI] [PubMed] [Google Scholar]
- 21.Grossman MD, Ofurum U, Stehly CD, Stoltzfus J. Long-term survival after major trauma in geriatric trauma patients: The glass is half full. The Journal of Trauma Injury Infection and Critical Care. 2012;72(5):1181–1185. doi: 10.1097/TA.0b013e31824d0e6d [DOI] [PubMed] [Google Scholar]
- 22.Malhotra AK, Martin N, Jacoby M, et al. What are we missing: results of a 13-month active follow-up program at a level I trauma center. J Trauma. 2009;66(6):1696–1702; discussion 1702–1703. doi: 10.1097/TA.0b013e31819ea529 [DOI] [PubMed] [Google Scholar]


