Abstract
Background:
There are substantial racial and socioeconomic disparities underlying endovascular abdominal aortic aneurysm repair (EVAR) in the United States. To date, race-based variations in reinterventions following elective EVAR have not been studied. Here, we aim to examine racial disparities associated with reinterventions following elective EVAR in a real-world cohort.
Materials and Methods:
We used the Vascular Quality Initiative (VQI) EVAR dataset to identify all patients undergoing elective EVAR between January 2009 and December 2018 in the United States. We compared the association of race with reinterventions after EVAR and all-cause mortality using Welch two-sample t-tests, multivariate logistic regression, and Cox proportional hazards analyses adjusting for baseline differences between groups.
Results:
At median follow-up of 1.1±1.1 years (1.3±1.4 years Black, 1.1±1.1 years White; P=0.02), a total of 1,164 of 42,481 patients (2.7%) underwent reintervention after elective EVAR, including 2.7% (n = 1,096) White vs. 3.2% (n = 68) Black (P = 0.21). Black patients requiring reintervention were more frequently female, more frequently current or former smokers, and less frequently insured by Medicare/Medicaid (P<0.05). After adjusting for baseline differences, the risk of reintervention after elective EVAR was significantly lower for Black vs. White patients (HR 0.74, 95% CI 0.55–0.99; P=0.04). All-cause mortality was comparable between groups (HR 0.81, 95% CI 0.33–2.00, P=0.65).
Conclusions:
There are significant differences between Black and White patients in the risk of reintervention after elective EVAR in the United States. The etiology of this difference deserves investigation.
Keywords: EVAR, Vascular Surgery, Health Services Research
1. Introduction
Endovascular aortic aneurysm repair (EVAR) has become the preferred method to repair anatomically-appropriate abdominal aortic aneurysms (AAAs) and currently make up approximately 80% of all AAA repairs.(1) Compared to open repair, EVAR is associated with significantly reduced short-term morbidity and mortality and earlier hospital discharge.(2) As a result, a growing proportion of elective and ruptured AAAs are treated with EVAR.(2)
In the United States, significant health care disparities exist in AAA repairs. Individuals that are not covered by insurance more commonly undergo open repair compared to those covered by Medicare.(3) Similarly, claims data from the Medicare Provider Analysis and Review have shown that Black and Hispanic patients are less likely to undergo elective EVAR and more often receive emergency AAA surgery than White patients.(4,5) Non-White populations have a lower incidence of AAA, yet face higher perioperative morbidity and mortality after AAA repair.(6) Understanding why non-White populations have reduced or delayed access to vascular services compared to White patients may address these disparities and, accordingly, reduce incidence rates of ruptured aneurysms and complex aneurysms unsuitable for EVAR among minority populations.
Over 50,000 people undergo EVAR in the United States each year, and up to 30% are expected to require reinterventions within ten years after EVAR.(7,8) Based on prior literature, minority patients frequently have reduced access to care compared to White patients.(3,4) This may partially explain the racial disparities in outcomes following open and endovascular AAA repair that have been reported previously.(3,6) However, there is a paucity of data examining race-based differences in reintervention rates following AAA repair. The aim of our study was to investigate the risk of reintervention after elective EVAR among Black versus White patients. We hypothesized that reintervention rates would be higher in Black versus White patients.
2. Materials and Methods
2.1. Data Source
The Vascular Quality Initiative (VQI) EVAR dataset was used to perform a retrospective analysis of reinterventions following elective EVAR. The VQI is a multicenter, deidentified registry pooling data from 635 vascular surgery centers across the United States and Canada. It comprises twelve registries with over 650,000 procedures, and collects information on patient characteristics, procedural techniques, and short- and long-term outcomes. We followed published recommendations for best-practice use of VQI for research.(9) The study protocol was approved by the Johns Hopkins Medicine Institutional Review Board and the VQI Research Advisory Committee. Informed consent was waived because this was a retrospective review of a deidentified database.
2.2. Study Population
All patients who underwent elective EVAR in the VQI dataset between January 1, 2009 and December 31, 2018 from the United States were included. We excluded patients who were a race other than Black or White in order to reduce cohort heterogeneity (n = 2,446). Patients were also excluded if they had undergone prior EVAR or open AAA repair or information was unknown (n = 1,769), repair for a ruptured AAA (n = 2,574), or an urgent or emergent repair (n = 4,005), or urgency was unknown (n = 80).
2.3. Outcomes
The primary outcome of the study was reintervention following elective EVAR. Reintervention was defined as any reoperation performed after the index EVAR. Secondary outcomes included postoperative outcomes following reintervention, including all-cause mortality, conversion to open repair, intensive care unit (ICU) and hospital length of stay, and 30-day perioperative complications (i.e. myocardial infarction, congestive heart failure, respiratory failure, acute renal failure or new dialysis, leg ischemia, intestinal ischemia, surgical site infection, and stroke as defined by the VQI registry).(10) Reintervention indications after elective EVAR were classified as sac growth, endoleak, migration, occlusion, stenosis, rupture, graft infection, or other indications in accordance with the VQI definitions. For all groups, time zero represents the index EVAR procedure for which patients were registered in the VQI dataset.
2.4. Statistical Analysis
We used univariable analyses including χ2, Student’s t-test, and Wilcoxon rank-sum tests to compare baseline characteristics of patients who required a reintervention after EVAR, stratified by race (Black versus White). We used Cox proportional hazards analyses to examine the association of race with reinterventions and all-cause mortality over time. The covariates (predictor variables) were chosen for inclusion in the multivariable models based on significant (P-values < 0.05) differences in the baseline characteristics between Black and White patients. This subset selection approach was chosen to achieve the most parsimonious model for our final study sample. We also compared crude outcomes following reintervention for Black vs. White patients using Chi-square tests. Missing covariate data were assumed to be missing completely at random, and missing values were excluded for each individual analysis. All analyses were performed using R statistical software (R Foundation for Statistical Computing, Vienna, Austria). Statistical significance was accepted at P-values < 0.05.
3. Results
3.1. Patient Characteristics
Overall, 3,372 Black and 55,975 White patients were identified in the EVAR dataset from 2009 to 2018 with follow-up data available for 72.4% of Black and 75.7% of White patients. One- and two-year follow-up rates were 44.4% vs. 45.9% and 3.8% vs. 3.6% for Black vs. White patients, respectively. 42,481 Black (n = 2,140) and White patients (n = 40,341) underwent elective EVAR during the 10-year study period, of which 1,164 (2.7%) required reintervention. Here, follow-up data was available for 83.2% of Black patients and 84.9% of White patients. The median follow-up time overall was 1.1±0.7 years (1.1±0.8 years Black, 1.1±0.7 years White; P<0.01). At one and two years, follow-up rates were 51.4% vs. 52.4% and 4.2% vs. 4.0% for Black vs. White patients, respectively. The median follow-up time in the reintervention sample was 1.1±1.1 years (1.3±1.4 years Black, 1.1±1.1 years White; P=0.02). The crude reintervention rate was similar among Black patients (68 of 2,140 EVAR, 3.2%) compared to White patients (1,096 of 40,341 EVAR, 2.7%) (P=0.21). The median time to reintervention was 0.8±1.3 years (1.1±1.6 years Black, 0.7±1.2 years White; P=0.01).
3.2. Association of Race with Reintervention after Elective EVAR
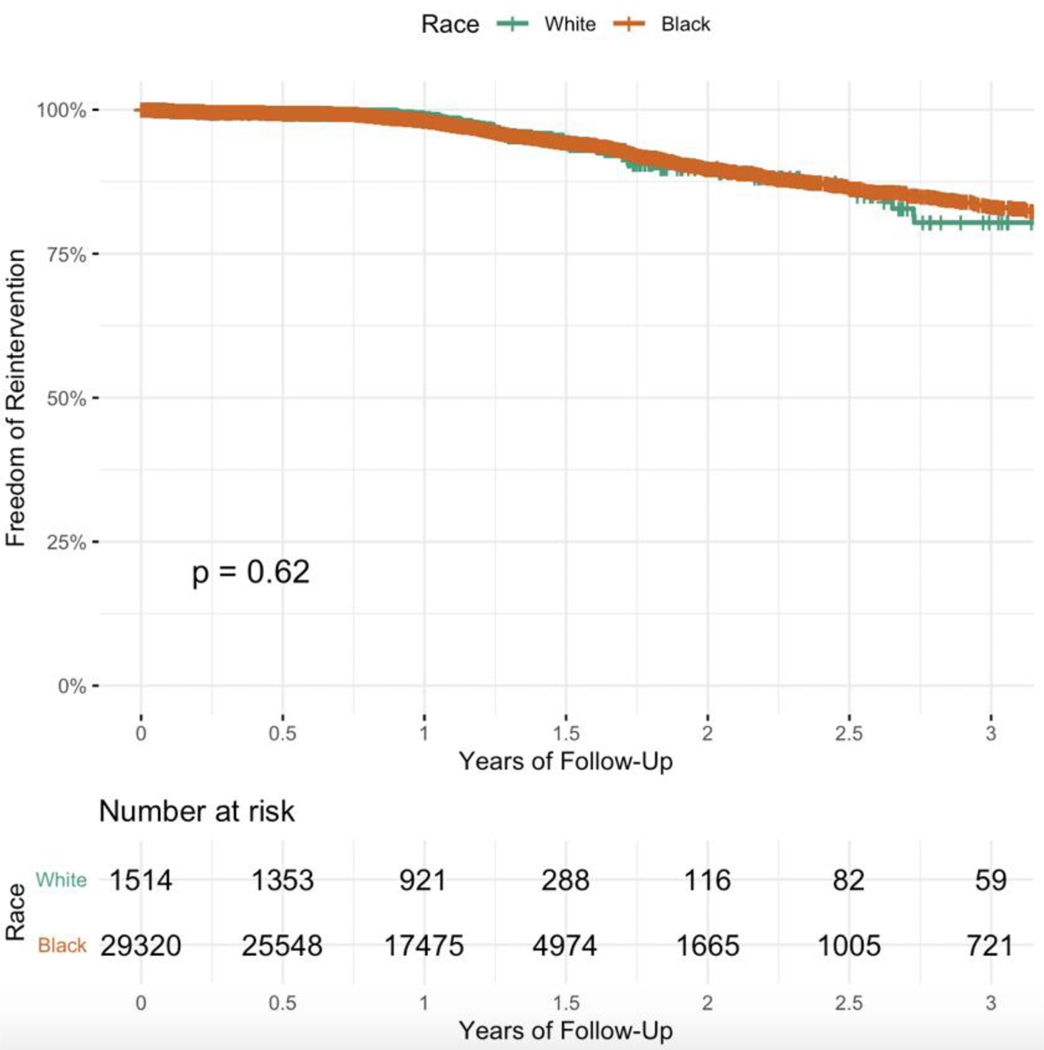
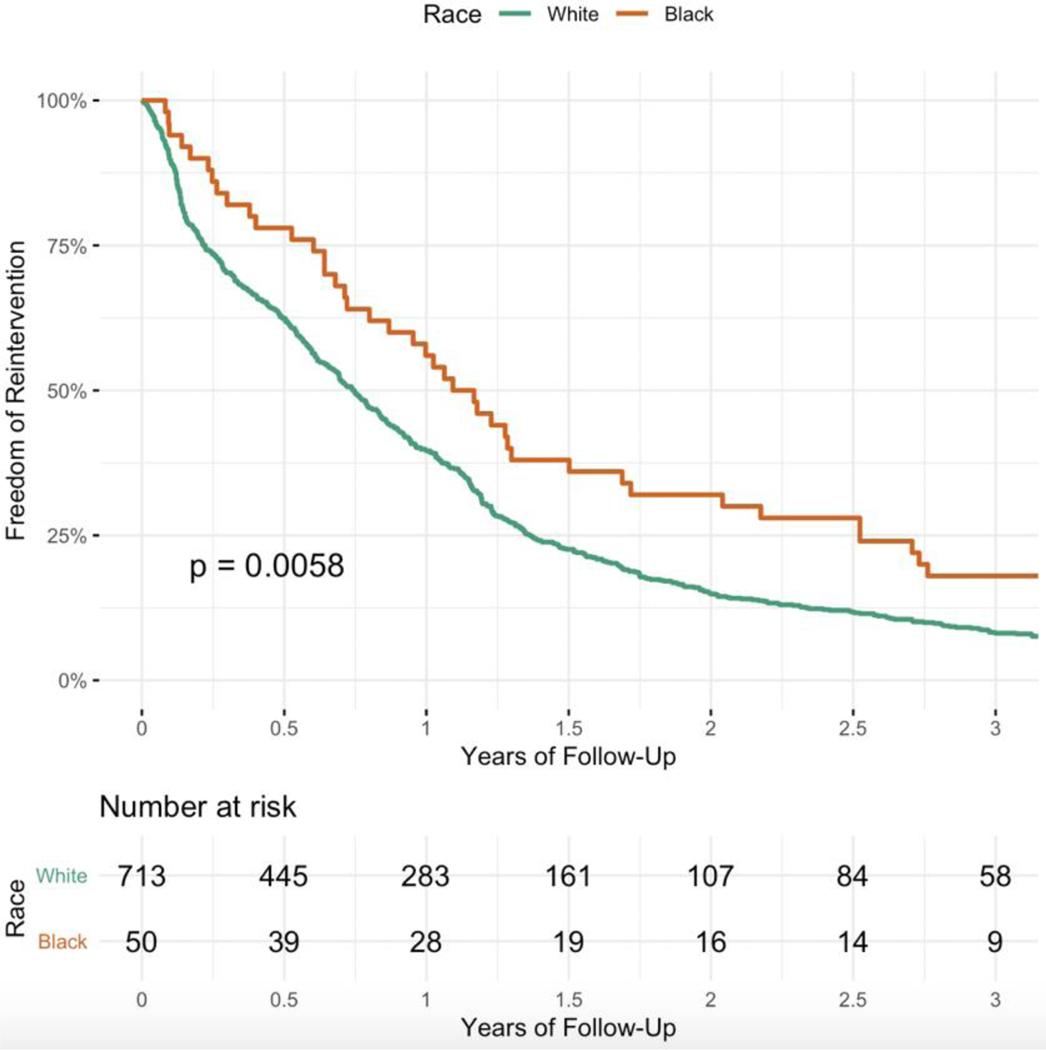
The estimated one- and three-year reintervention rates after elective EVAR were 1.3% (95% CI 0.7–2.0%) vs. 2.0% (95% CI 1.8–2.1%) and 19.6% (95% CI 12.6–26.1%) vs. 16.9% (95% CI 15.2–18.5%) for Black vs. White patients, respectively. Based on Kaplan-Meier curve analysis, there was no significant difference in the rate of reintervention for Black vs. White patients (Figure 1; log-rank P=0.62). Among those patients that required reintervention after EVAR, reintervention procedures occurred earlier among White patients compared to Black patients (log-rank P=0.01; Figure 2).
Figure 1.
Kaplan-Meier curves showing reinterventions following elective EVAR for Black vs. White patients in the Vascular Quality Initiative (2009–2018).
Figure 2.
Kaplan-Meier curves showing timing of reinterventions following elective EVAR for Black vs. White patients requiring reinterventions in the Vascular Quality Initiative (2009–2018).
Black patients requiring reintervention were more frequently female (33.8% vs. 19.3%), more likely to be current or former smokers (89.7% vs. 83.1%), less likely to have Medicare/Medicaid insurance (39.7% vs. 58.2%), and had a lower prevalence of congestive heart failure (6.0% vs. 13.0%) than White patients (all, P<0.05; Table I). There was no correlation (r = 0.08, P<0.01) in the rate of reinterventions between race and sex. There was also no significant difference in mean AAA diameter at baseline for Black (55.7±14.6 mm) vs. White (56.9±11.8 mm) patients (P=0.52) The most common reason for reinterventions among both Black (49.1%) and White (54.1%) patients was endoleak. Black patients were more likely to require reintervention due to occlusion (32.1% vs. 17.9%; P=0.04) but less likely due to graft infection compared to White patients (0.0% vs. 2.8%; P<0.01) (Table II).
Table 1.
Baseline characteristics of patients undergoing reintervention after elective EVAR (n=1164), stratihed by race.
| Black (n = 68) | White (n = 1096) | P-value | |
|---|---|---|---|
| Age in years, mean ± SD | 71.9 ± 10.1 | 73.7 ± 8.5 | 0.16 |
| Female sex | 33.8 (23) | 19.3 (212) | 0.02 |
| Initial preoperative AAA diameter in mm, mean ± SD | 55.7 ± 14.6 | 56.9 ± 11.8 | 0.52 |
| Aortic neck length in mm, mean ± SD | 28.2 ± 15.8 | 25.4 ± 12.1 | 0.49 |
| Aortic neck diameter in mm, mean ± SD | 21.5 ± 2.98 | 23.8 ± 5.25 | 0.01 |
| Aorta-neck angle, median | <45 degrees | <45 degrees | 0.73 |
| Neck-AAA angle, median | <45 degrees | <45 degrees | 0.13 |
| Graft components | |||
| Proximal aortic extensions, mean | 0.3 | 0.2 | 0.64 |
| Iliac devices, left, mean | 0.8 | 1.0 | 0.21 |
| Iliac devices, right, mean | 0.8 | 0.8 | 0.66 |
| Primary Insurer | 0.01 | ||
| Medicaid/Medicare | 39.7 (27) | 58.2 (638) | |
| Private | 35.3 (24) | 26.5 (290) | |
| Other | 25.0 (17) | 15.3 (168) | |
| Co-Morbidities | |||
| CAD | 27.9 (19) | 27.6 (303) | 0.30 |
| Hypertension | 89.7 (61) | 83.3 (913) | 0.10 |
| Diabetes | 23.5 (16) | 16.3 (179) | 0.13 |
| CHF | 6.0 (4) | 13.0 (143) | 0.01 |
| COPD | 33.8 (23) | 26.9 (295) | 0.36 |
| Dialysis | 4.4 (3) | 1.1 (12) | 0.19 |
| Smoking history | 89.7 (61) | 83.1 (911) | <0.01 |
| Family history of AAA | 10.3 (7) | 10.7 (117) | 0.91 |
Categorical variables are presented as % (number).
AAA = abdominal aortic aneurysm; CAD = coronary artery disease; CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease; SD = standard deviation.
Table 2.
Reintervention indications after elective EVAR (n=1164), stratihed by race.
| Black n = 68) | White (n = 1,096) | P-value | |
|---|---|---|---|
| Indication | |||
| Sac growth | 20.8 (14) | 22.0 (241) | 0.83 |
| Endoleak | 49.1 (33) | 54.1 (593) | 0.49 |
| Migration | 7.6(5) | 2.4 (26) | 0.17 |
| Occlusion | 32.1 (22) | 17.9 (196) | 0.04 |
| Stenosis | 3.8 (2) | 8.2 (90) | 0.13 |
| Rupture | 1.9(1) | 2.6 (28) | 0.71 |
| Graft infection | 0.0 (0) | 2.8 (31) | <0.01 |
| Other | 11.3 (8) | 10.4 (114) | 0.84 |
Multiple indications may be present for a given reintervention. Categorical variables are presented as % (number).
Based on univariable Cox proportional hazards model analyses, baseline patient characteristics associated with reintervention included White race (P=0.01) and prevalent congestive heart failure (P=0.04) (Table III). After adjusting for baseline differences between groups, the risk of reintervention after EVAR was significantly lower for Black vs. White patients (HR 0.74, 95% CI 0.55–0.99; P=0.04; Table IV and Supplemental Table I).
Table 3.
Univariate Cox proportional hazards model analyses (HR,95% CI) for the associations of baseline patient characteristics With reintervention after elective EVAR.
| Hazard Ratio | 95% Cl | P-value | |
|---|---|---|---|
| Age, per year | 1.00 | 0.99–1.01 | 0.77 |
| Black race (versus White) | 0.70 | 0.55–0.91 | 0.01 |
| Female sex (versus Male) | 1.02 | 0.88–1.18 | 0.82 |
| AAA diameter <60 mm (versus ≥60 mm) | 1.00 | 0.99–1.00 | 0.19 |
| Primary insurer | |||
| Medicaid/Medicare (versus Private) | 1.08 | 0.94–1.24 | 0.29 |
| Other (versus Private) | 1.11 | 0.72–1.72 | 0.62 |
| Co-morbidities (versus none) | |||
| CAD | 0.99 | 0.91–1.07 | 0.78 |
| Hypertension | 1.02 | 0.87–1.20 | 0.81 |
| Diabetes | 0.99 | 0.92–1.07 | 0.78 |
| CHF | 1.12 | 1.00–1.26 | 0.04 |
| COPD | 1.07 | 0.99–1.14 | 0.07 |
| Dialysis | 1.24 | 0.95–1.61 | 0.11 |
| Smoking history (versus none) | 1.04 | 0.95–1.14 | 0.36 |
| Family history of AAA (versus none) | 1.06 | 0.88–1.29 | 0.53 |
AAA - abdominal aortic aneurysm; CAD = coronary artery disease; CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease.
Table 4.
Multivariable* Cox regression analyses (HR,95% CI) for the associations of race with reintervention and mortality after elective EVAR.
| Hazard Ratio | 95% Cl | P-value | |
|---|---|---|---|
| Reintervention | |||
| White | Ref | ||
| Black | 0.74 | 0.55–0.99 | 0.04 |
| Mortality | |||
| White | Ref | ||
| Black | 0.81 | 0.33–2.00 | 0.65 |
Adjusted for sex, smoking, insurance status, and congestive heart failure.
3.3. Association of Race with Postoperative Outcomes following Reintervention after EVAR
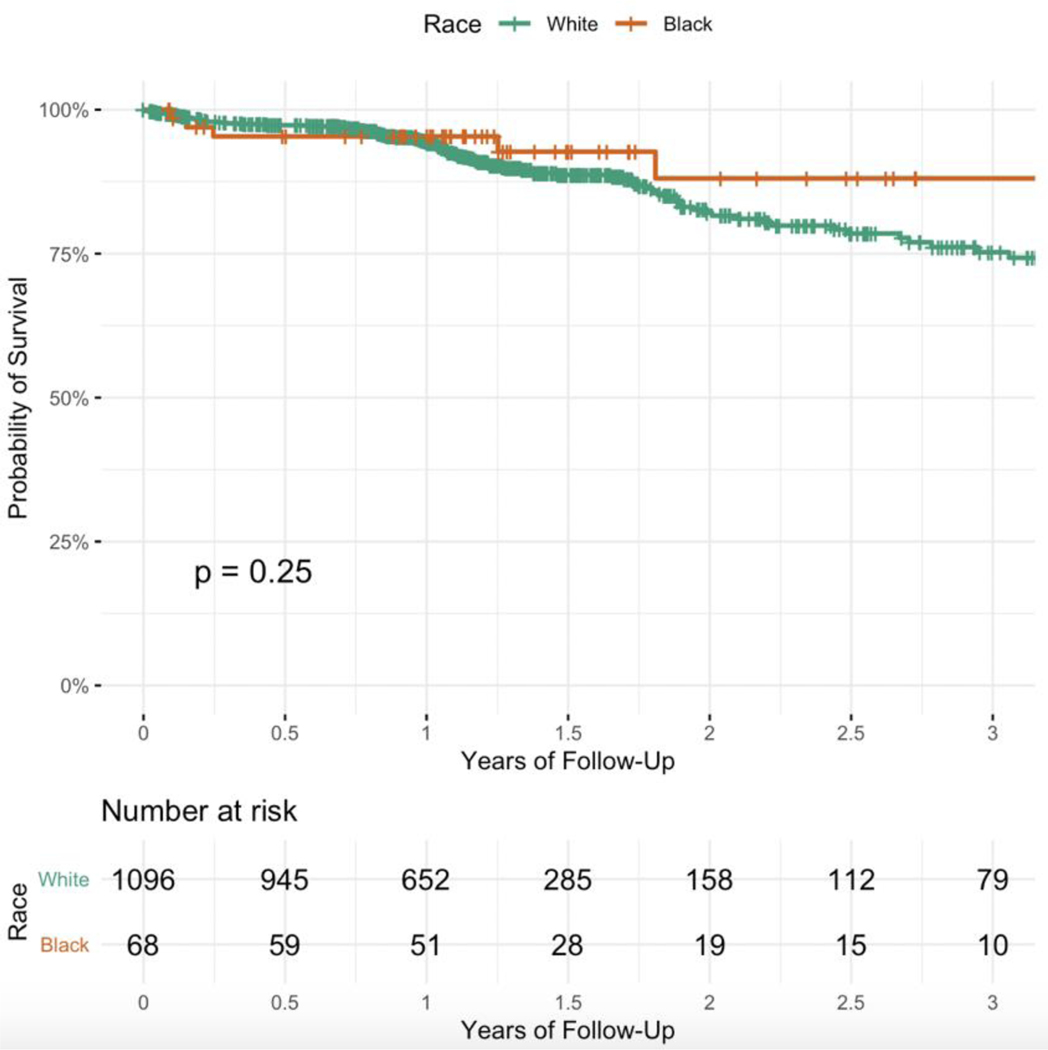
8.8% of Black and 10.5% of White patients died after reintervention following elective EVAR during the follow-up period (P = 0.64). Based on Kaplan-Meier analyses, all-cause mortality was similar between groups (log-rank P=0.25; Figure 3). After adjusting for baseline differences, all-cause mortality did not significantly differ for Black vs. White patients (HR 0.81, 95% CI 0.33–2.00; Table IV).
Figure 3.
Kaplan-Meier curves showing mortality for Black vs. White patients requiring reintervention after the index elective EVAR in the Vascular Quality Initiative (2009–2018).
For other secondary outcomes, there was no difference in ICU length of stay (0.57±0.99 days vs. 0.51±1.44 days, P=0.64) or total hospital length of stay (3.28±3.32 days vs. 2.61±9.09 days, P=0.17) for Black vs. White patients following reintervention after EVAR. (Table V). Conversion to open repair occurred infrequently and was also similar between groups (P=0.16, Table V).
Table 5.
Crude postoperative outcomes of patients undergoing reintervention after EVAR, stratified by race (n = 1164). Categorical variables are presented as % (number).
| Black (n = 68) | White (n = 1096) | P-value | |
|---|---|---|---|
| Follow-up time, median years ± SD | 1.3 ± 1.4 | 1.1 ± 1.1 | 0.02 |
| Overall mortality | 8.8 (6) | 10.5 (115) | 0.64 |
| ICU length of stay, mean days ± SD | 0.6 ± 1.0 | 0.5 ± 1.4 | 0.64 |
| Total hospital length of stay, mean days ± SD | 3.3 ± 3.3 | 2.6 ± 9.1 | 0.17 |
| Conversion to open repair | 0.0 (0) | 0.2 (2) | 0.16 |
ICU = intensive care unit; SD = standard deviation
4. Discussion
Race-based differences in the treatment of AAA are well described.(6) However, there is a paucity of data evaluating racial differences in the rate of reinterventions following EVAR. We analyzed ten years of data from the VQI database to assess the association of Black versus White race with reinterventions following elective EVAR. We found that Black patients were less likely to undergo reintervention after elective EVAR compared to White patients in the first postoperative year, but all-cause mortality did not significantly differ between groups.
The racial disparities in reinterventions after elective EVAR that we report adds to prior literature demonstrating persistent inequalities in treating patients with AAA.(3,6) Black patients are less likely to undergo elective EVAR versus open repair compared to White patients, and are more likely to require emergency surgery.(11) In our study, we found that Black patients are less likely to undergo reinterventions following elective EVAR compared to White patients. Overall, the frequency of reinterventions in the VQI was low (1.3–2.0%) compared to prior literature (6.0%) at the one-year period, but higher at the three-year period (16.9–19.6% vs. 15%).(7,8)
The etiology of these findings are unclear. It is possible that Black patients have fewer endoleaks following elective EVAR, and are thus less likely to require an intervention. If EVAR is reserved only for Black patients with better aortic anatomy, it is possible they have better postoperative outcomes than White patients. This would align with previous observations of reduced access to EVAR for non-White populations.(4,5) It is also possible that Black patients have worse follow-up than White patients, and thus are less frequently diagnosed with endoleaks requiring reintervention. A prior VQI study demonstrated that approximately 15% of Black patients are lost to any follow-up after elective EVAR, compared to 10% of White patients.(12) In our study, 16.8% of Black and 15.1% of White patients undergoing elective EVAR were lost to any follow-up; however, one- and two-year follow-up rates were comparable between groups. Black patients have also been shown to have worse compliance with surveillance imaging after EVAR, possibly as a result of cultural differences, lower social economic status, and more limited access to outpatient healthcare.(13) The concept of poor follow-up among minority patients is supported by our finding that Black patients presented more frequently with the potentially preventable complication of stent-graft occlusion than White patients. This stresses the importance of establishing robust follow-up mechanisms to monitor postoperative outcomes and timely identify potential development of endoleaks in patients, especially in populations previously associated with worse outcomes after primary interventions.
Our study deserves some discussion in light of the recent findings by Columbo et al., which suggested higher reintervention rates among Black patients undergoing all EVAR.(14) Our study was limited to elective EVAR only, and we excluded reinterventions after urgent/emergent AAA repairs. In contrast, the prior study included all EVAR procedures, ranging from elective to urgent to emergent. Taken together, the two studies suggest that the higher reintervention rates among Black patients reported by Columbo et al. may primarily be a result of urgent/emergent repairs. This is consistent with previous findings reporting higher rates of urgent/emergent, ruptured, and symptomatic presentations among Black patients, which are less amenable to EVAR and thus may result in a less favorable postoperative disease course.(4,5)
All-cause mortality following reintervention was comparable to previous literature.(15) We found no significant differences in mid-term mortality between Black and White patients following reintervention after EVAR. This finding stands in contrast with previous race-related mortality differences following primary EVAR and open AAA repairs.(5) Notably, our survival analysis was limited to patients requiring reintervention, so the lack of mortality difference does not reflect post-EVAR outcomes as a whole. The median follow-up time in our study was also limited to just over a year, which may be too abbreviated to detect all-cause race-based mortality differences. The number of Black patients requiring reinterventions in our study sample was small, which may also explain the lack of differences we observed, and the aforementioned possible differences in surveillance between Black and White patients after EVAR may further contribute to these findings.
The limitations of our study deserve discussion. First, the VQI database is subject to selection bias and data validity issues due to self-reporting by physician and hospitals. However, it is the most contemporary non-administrative database to report perioperative and long-term vascular outcomes, and is thought to generally reflect current vascular surgery practices in the US.(16) Future analyses can, however, link VQI data with Medicare claims data to better assess reintervention rates beyond VQI follow-up.(17) Second, the number of Black patients who underwent reinterventions after primary elective EVAR was small, limiting any meaningful analysis of secondary outcomes. For example, data on postoperative complications was missing for 43% (n = 29) of Black patients, leading to a high risk of type II error in our secondary outcomes analyses. Similarly, we excluded patients with a race other than Black or White due to small sample sizes, limiting the power in analyses including patients from other races. Future studies will be needed to validate these findings in larger cohorts and/or cohorts with improved longitudinal follow-up beyond that of the VQI database. Third, in our analysis, we were unable to assess or adjust for differences in patients’ socioeconomic status due to the lack of such data in the available dataset. Socioeconomic status has previously been associated with differential access to and outcomes after EVAR, and may thus have confounded our findings.(18,19) As non-White patients are more likely to have lower socioeconomic status compared to White patients, our findings may be conservative, thus requiring further investigation. Fourth, the median follow-up for the study cohort was just over one year, so our findings do not represent long-term racial differences in reinterventions or subsequent mortality after EVAR. Despite these limitations, this study has highlighted disparities in the need for reintervention after elective EVAR that deserve further investigation.
5. Conclusions
We found significant variation between Black and White patients associated with reinterventions after elective EVAR in the United States. Black patients were less likely to undergo reintervention after elective EVAR compared to White patients, but all-cause mortality did not significantly differ between groups. Further investigation is warranted to assess the etiology of these findings.
Supplementary Material
Acknowledgements
We would like to acknowledge the Johns Hopkins Surgery Center for Outcomes Research for the surgical research mentorship program and the assistance with this project.
Funding Source:
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of Interest:
Dr. Hicks is supported by NIH/NIDDK grant 1K23DK124515-01. Dr. Haut is/was primary investigator of contracts from The Patient-Centered Outcomes Research Institute (PCORI) (CE-12-11-4489 and DI-1603-34596). Dr. Haut is primary investigator of a grant from the Agency for Healthcare Research and Quality (AHRQ) (1R01HS024547) and is a co-investigator on a grant from the NIH/NHLBI (R21HL129028). Dr. Haut is supported by a contract from PCORI, (PCS-1511-32745). Dr. Haut receives research grant support from the DOD/Army Medical Research Acquisition Activity and has received grant support from the Henry M. Jackson Foundation for the Advancement of Military Medicine (HJF). Dr. Haut receives royalties from Lippincott, Williams, Wilkins for a book - “Avoiding Common ICU Errors.” Dr. Haut was a paid consultant to Vizient for their HIIN Venous Thromboembolism (VTE) Preventigon Action Network.
Disclosures: Dr. Hicks is supported by NIH/NIDDK grant 1K23DK124515. Dr. Haut is/was primary investigator of contracts from The Patient-Centered Outcomes Research Institute (PCORI) (CE-12-11-4489 and DI-1603-34596) and the Agency for Healthcare Research and Quality (1R01HS024547) and is a co-investigator on a grant from the NIH/NHLBI (R21HL129028). Dr. Haut is supported by a contract from PCORI (PCS-1511-32745). Dr. Haut receives research grant support from the DOD/Army Medical Research Acquisition Activity and has received grant support from the Henry M. Jackson Foundation for the Advancement of Military Medicine. Dr. Haut receives royalties from Lippincott, Williams, Wilkins for a book - “Avoiding Common ICU Errors.” Dr. Haut was a paid consultant to Vizient for their HIIN Venous Thromboembolism (VTE) Prevention Action Network.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Suckow BD, Goodney PP, Columbo JA, Kang R, Stone DH, Sedrakyan A, et al. National trends in open surgical, endovascular, and branched-fenestrated endovascular aortic aneurysm repair in Medicare patients. J Vasc Surg [Internet]. 2018;67(6):1690–1697.e1. Available from: http://www.sciencedirect.com/science/article/pii/S0741521417325107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giles KA, Pomposelli F, Hamdan A, Wyers M, Jhaveri A, Schermerhorn ML. Decrease in total aneurysm-related deaths in the era of endovascular aneurysm repair. J Vasc Surg [Internet]. 2009/01/09. 2009. March;49(3):543–51. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19135843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lemaire A, Cook C, Tackett S, Mendes DM, Shortell CK. The impact of race and insurance type on the outcome of endovascular abdominal aortic aneurysm (AAA) repair. J Vasc Surg [Internet]. 2008. June 1;47(6):1172–80. Available from: 10.1016/j.jvs.2008.01.033 [DOI] [PubMed] [Google Scholar]
- 4.Osborne NH, Mathur AK, Upchurch GRJ, Dimick JB. Understanding the racial disparity in the receipt of endovascular abdominal aortic aneurysm repair. Arch Surg. 2010. November;145(11):1105–8. [DOI] [PubMed] [Google Scholar]
- 5.Vogel TR, Cantor JC, Dombrovskiy VY, Haser PB, Graham AM. AAA repair: sociodemographic disparities in management and outcomes. Vasc Endovascular Surg. 2008;42(6):555–60. [DOI] [PubMed] [Google Scholar]
- 6.Deery SE, O’Donnell TFX, Shean KE, Darling JD, Soden PA, Hughes K, et al. Racial disparities in outcomes after intact abdominal aortic aneurysm repair. J Vasc Surg. 2018. April;67(4):1059–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wanken ZJ, Barnes JA, Trooboff SW, Columbo JA, Jella TK, Kim DJ, et al. A systematic review and meta-analysis of long-term reintervention after endovascular abdominal aortic aneurysm repair. J Vasc Surg [Internet]. 2020; Available from: http://www.sciencedirect.com/science/article/pii/S0741521420303232 [DOI] [PubMed] [Google Scholar]
- 8.Columbo JA, Martinez-Camblor P, O’Malley AJ, Suckow BD, Hoel AW, Stone DH, et al. Long-term Reintervention After Endovascular Abdominal Aortic Aneurysm Repair. Ann Surg. 2019. July; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Desai SS, Kaji AH, Upchurch G Jr. Practical Guide to Surgical Data Sets: Society for Vascular Surgery Vascular Quality Initiative (SVS VQI). JAMA Surg [Internet]. 2018. October 1;153(10):957–8. Available from: 10.1001/jamasurg.2018.0498 [DOI] [PubMed] [Google Scholar]
- 10.Society for Vascular Surgery. Vascular Quality Initiative [Internet]. 2019. [cited 2019 Oct 18]. Available from: https://www.vqi.org/
- 11.Yang Y, Lehman EB, Aziz F. African Americans are less likely to have elective endovascular repair of abdominal aortic aneurysms. J Vasc Surg. 2019. August;70(2):462–70. [DOI] [PubMed] [Google Scholar]
- 12.Hicks CW, Zarkowsky DS, Bostock IC, Stone DH, Black JH, Eldrup-Jorgensen J, et al. Endovascular aneurysm repair patients who are lost to follow-up have worse outcomes. J Vasc Surg [Internet]. 2017;65(6):1625–35. Available from: http://www.sciencedirect.com/science/article/pii/S0741521416316688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jasinski PT, Labropoulos N, Christoforatos OG, Tassiopoulos AK. Factors Affecting Follow-Up Compliance in Patients After Endovascular Aneurysm Repair. Aorta (Stamford, Conn). 2017. October;5(5):148–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Columbo JA, Ramkumar N, Martinez-Camblor P, Kang R, Suckow BD, O’Malley AJ, et al. Five-year reintervention after endovascular abdominal aortic aneurysm repair in the Vascular Quality Initiative. J Vasc Surg. 2020. March;71(3):799–805.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Giles KA, Landon BE, Cotterill P, O’Malley AJ, Pomposelli FB, Schermerhorn ML. Thirty-day mortality and late survival with reinterventions and readmissions after open and endovascular aortic aneurysm repair in Medicare beneficiaries. J Vasc Surg [Internet]. 2010/10/27. 2011. January;53(1):6–13.e1. Available from: https://pubmed.ncbi.nlm.nih.gov/21030195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sutzko DC, Mani K, Behrendt C-A, Wanhainen A, Beck AW. Big Data in Vascular Surgery: Registries, International Collaboration and Future Directions. J Intern Med. 2020. April; [DOI] [PubMed] [Google Scholar]
- 17.Columbo JA, Kang R, Hoel AW, Kang J, Leinweber KA, Tauber KS, et al. A comparison of reintervention rates after endovascular aneurysm repair between the Vascular Quality Initiative registry, Medicare claims, and chart review. J Vasc Surg [Internet]. 2018/06/15. 2019. January;69(1):74–79.e6. Available from: https://pubmed.ncbi.nlm.nih.gov/29914838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Faulds J, Bell NJ, Harrington DM, Novick T V, Harris JR, DeRose G, et al. Socioeconomic and geographic disparities in access to endovascular abdominal aortic aneurysm repair. Ann Vasc Surg. 2013. November;27(8):1061–7. [DOI] [PubMed] [Google Scholar]
- 19.Al Adas Z, Nypaver TJ, Shepard AD, Weaver MR, Ryan JT, Huang J, et al. Survival after abdominal aortic aneurysm repair is affected by socioeconomic status. J Vasc Surg. 2019. May;69(5):1437–43. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.