Abstract
Objective:
To determine age- and sex-specific predictors of discharge destination among patients with traumatic brain injury (TBI) receiving inpatient rehabilitation facility (IRF) care.
Design:
Secondary analysis of Uniform Data System for Medical Rehabilitation data.
Methods:
Logistic regression of patients (N=221,961) age ≥18, TBI diagnosis, admitted to IRF between 2002-2018.
Outcome:
Discharge destination (subacute vs. home/community settings)
Results:
Approximately 16% were discharged to subacute vs. 84% home. Younger versus older adults had lower odds of subacute discharge [OR=0.72; 95% CI: 0.69, 0.76]. Age and sex stratification of discharge destination was significant. Younger females had lower odds of subacute discharge (vs. home) than older females [OR=0.68; 95% CI: 0.63, 0.74]; younger males had lower odds of subacute discharge (vs. home) than older males [OR=0.74; 95% CI: 0.70, 0.78]. Younger females versus younger males had lower odds of subacute discharge (vs. home) [OR=0.83; 95% CI: 0.79, 0.87]. Older females versus older males had lower odds of subacute discharge (vs. home) [OR=0.93; 95% CI: 0.90, 0.97]. Predictors of discharge destination for age- and sex-stratified groups varied.
Conclusions:
Younger (vs. older) and female (vs. male) patients had lower odds of subacute discharge vs. home. Findings can inform IRF and transitional care planning and resource allocation.
Keywords: Brain Injuries, Traumatic, Rehabilitation, Outcome Assessment, Health Care
Introduction
According to the Centers for Disease Control and Prevention, the rates of traumatic brain injury (TBI)-related emergency department visits in the United States (U.S.) are highest among adults ≥ 75 years of age and age 15-24 years.1 TBI can result in significant impairments in emotion, cognition, communication, behavior, and physical functioning, which may affect the patient’s independence.2,3 The impairments caused by TBI are often addressed with inpatient rehabilitation facility (IRF) care,4 which has been shown to be beneficial in assessing and treating cognitive and physical impairments and improving the patient’s functional status for patients with TBI.5
Age is often stratified in TBI cohort studies (younger age [18-64] vs. older age [65+]), with numerous studies showing that younger adults typically have better outcomes compared to older adults.6-9 While sex differences in TBI outcomes are debated in the literature, multiple studies have shown that sex is a significant predictor of outcomes.10-15 Although research shows that both age and sex are independently important predictors of a variety of outcomes for adult patients with TBI,8,10,11,16,17 the interaction between the two remain unclear. In addition, although several studies have investigated sex-specific predictors of TBI acute care discharge destination,18-23 no studies have identified sex-specific predictors of IRF discharge destination for patients with TBI. Finally, the few studies that have focused on predictors of TBI IRF discharge to subacute settings24 have not used discharge to home/community settings as a comparator, even though returning to home/community settings after IRF care is the expected discharge destination.25
To address these gaps in knowledge, the purpose of this study was to identify the age- and sex-specific predictors of discharge destination (subacute vs. home) among patients with TBI who received IRF care. Our findings can be used to inform development of interventions aimed to address needs, allocation of resources, and transitional care planning.
Methods
Study Design
This was a secondary analysis of a national cohort of adult patients with TBI who received U.S. IRF care. Findings are reported in accordance with STROBE guidelines.26 This study was approved by the participating institutional review board before commencement.
Data Source
We used data from the Uniform Data System for Medical Rehabilitation® (UDSMR). UDSMR is a not-for-profit organization affiliated with UB Foundation Activities, Inc. at State University of New York at Buffalo. Annually, UDSMR collects data from over 70% of all IRFs in the U.S., containing patient-level rehabilitation and administrative data for over 800,000 adult patient records per year.27 We used data for adult patients with TBI who were admitted to an IRF and received care during 2002-2018.
Sample
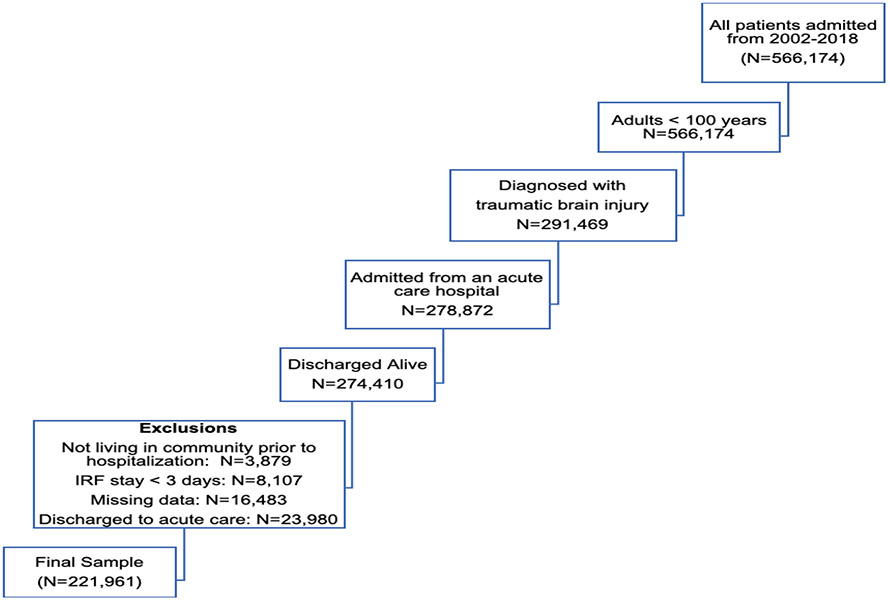
Our sample included: 1) adults (age ≥18); 2) diagnosed with TBI (impairment group codes 02.21,02.22, and 02.9); 3) admitted to an IRF from the acute hospital; and 4) discharged alive from an IRF between 2002 and 2018. We excluded patients with TBI who: 1) were not living in the community prior to acute hospital and IRF care; 2) had an IRF stay <3 days; 3) were missing data on key variables; and 4) died during the IRF stay (see Figure 1 for flow diagram).
Figure 1.
Flow Diagram
Study Variables
The primary outcome was discharge destination. We compared discharge to subacute settings (intermediate care, skilled nursing facility, chronic hospital, alternate level of care unit, rehabilitation facility, subacute setting, other) to discharge home/community settings (discharge to home with/without home health, assisted living, board and care, or transitional living). Discharge to subacute settings was the reference group. We include discharge to home/community settings as the reference group because this is considered to be a successful discharge living setting based on Centers for Medicare & Medicaid Services (CMS) quality measures benchmarks.25
The independent variables were covariates of interest that were available in the dataset and previously used in TBI outcomes research.10,11,16,17 We organized our variables into sociodemographic, clinical, and facility characteristics.
The sociodemographic variables included in our analysis were:
Age: patient’s age at IRF admission (categorized by younger [18-64] and older [65+]);
Sex: patient’s sex (male or female);
Race/ethnicity: patient’s race or ethnicity (White, Black, Hispanic/Latino, other);
Marital status: patient’s marital status (married, never married, widowed, divorced, separated);
Pre-admission living arrangement: the individuals who were living with the patient prior to hospitalization (alone, family/relative, friends, attendant, other);
Discharge living arrangement: the individuals who planned to live with patient at time of discharge (alone, family/relative, friends, attendant, other);
Insurance status: primary and secondary source of payment for inpatient rehabilitation services (Medicare, Medicaid, private, other, and none).
The clinical variables included in our analysis were:
Comorbidities: patient’s individual comorbidities, defined as co-existing medical; conditions present on IRF admission,28 indicated by ICD-9 or ICD-10 codes (only included comorbidities that affected ≥ 0.5% of the sample);
Complications: patient’s individual complications, defined as medical conditions that began during IRF stay,28 indicated by ICD-9 or ICD-10 codes (only included complications that affected ≥ 0.5% of the sample);
Case mix group (CMG) comorbidity tier: CMS payment tier for comorbid conditions. “Medicare groups cases into one of four tiers within each CMG according to patient comorbidities (conditions secondary to the principal admitting diagnosis). Each tier adds a higher case-payment amount.”29(p3) Tier 1 (high cost), Tier 2 (medium cost), Tier 3 (low cost), and no Tier (Tier 0).28,29
Admission functional status: as indicated by the total Functional Independence Measure (FIM) score on admission (score ranging from 18 to 126).30 Functional status on admission was used as a proxy for injury severity.
Days onset to admission: total number of days between onset of symptoms to IRF admission;
Length of stay: total number of days patient spent at IRF;
Year of admission: year in which patient as admitted to IRF.
The facility variables included in our analysis were:
- IRF location: the facility’s CMS region, which includes multiple states in a geographic region, categorized as:
- Region P01 = CT, MA, ME, NH, RI, VT
- Region P02 = NJ, NY, PR
- Region P03 = DE, MD, PA, VA, WV
- Region P04 = AL, FL, GA, KT, MS, NC, TN, SC
- Region P05 = IL, IN, MI, MN, OH, WI
- Region P06 = AR, LA, NM, OK, TX
- Region P07 = IA, KS, MO, NE
- Region P08 = CO, MT, ND, SD, UT, WY
- Region P09 = AZ, CA, HI, NV
- Region P10 = AK, ID, OR, WA
IRF type: type of IRF facility (free-standing or rehabilitation unit in hospital);
IRF accreditation: accreditation of IRF (accreditation from Joint Commission and/or Commission on Accreditation of Rehabilitation Facilities (CARF) accreditation vs. no accreditation).
Data Analysis
Sociodemographic, clinical, and facility characteristics were summarized using counts and percentage for categorical variables and mean and standard deviation for continuous variables for different age groups (younger vs older). The differences by age group were assessed by using independent t-tests for continuous variables and chi-square tests for categorical data. Sociodemographic, clinical, and facility characteristics were also summarized for different sex groups (male vs. female) within each age group.
Simple logistic regression models were used to estimate unadjusted odds ratio for each of the significant factors in predicting discharge to subacute settings compared to home. Multiple logistic regression models were built to estimate adjusted odds ratio of each of the sociodemographic, clinical, and facility factors for predicting discharge to subacute settings compared to home after adjusting for all other significant predictors. The multiple regression model was built by including all significant predictors in the bivariate analysis and performing a stepwise variable selection procedure. The entry of p-value was 0.2 and 0.05 was used as the threshold for retaining the predictor.
To further assess the effect of age and sex on predicting discharge to subacute settings compared to home, simple and multiple logistic regression was used, including presenting unadjusted and adjusted odds ratios for younger vs. older patients stratified by different sex group and for female vs. male patients stratified by different age groups.
To assess and identify age- and sex-specific predictors, we also built four separate logistic models for each subgroup: (1) younger males, (2) younger females, (3) older males, and (4) older females. For each of the multiple logistic regression model, we used a separate stepwise model selection process. The stay criterion for all stepwise selection models was 0.05 and the entry criterion was set at 0.15.
The percentage of missing data per variable was low (<5%). We decided not to use any form of imputation and subjects with missing data were excluded from analysis. The level of significance was set at 0.05 for all statistical tests. All analyses were conducted using SAS version 9.4 (SAS Ins., Cary, NC).31
Results
Overall Sample
This sample of 221,961 adults had a mean age of 62 years, 39% were female, and 78% were White (Table 1). The total percentage of patients living alone pre-admission (26%) decreased post-discharge (8%), as most patients lived with family or relatives upon discharge home (86%). Most patients had Medicare (58%) or private insurance (29%). Mean functional status on admission was 56.68, while mean days of onset to admission and length of stay were 14.74 and 16.11, respectively. Region P04 had the highest number of patients with TBI, representing 17.83% of the sample. Most patients received care in a rehabilitation unit located in a hospital (64%) that was accredited by the Joint Commission and/or CARF (64%). The majority of patients were discharged to home/community (84%) compared to subacute (16%).
Table 1.
Patient and Facility Characteristics of Younger (18-64) vs Older (65+) TBI Patients Receiving Inpatient Rehabilitation (N=221961)
| Variables | Values | Overall (N=221961) |
Younger (18-64) (N=99614, 44.88%) |
Older (65+) (N=122347, 55.12%) |
p |
|---|---|---|---|---|---|
| Sociodemographic characteristics | |||||
| Age | Years, Mean (SD) | 62.25 (21.35) | 42.14 (14.68) | 78.62 (7.37) | NA |
| Sex | Female | 86215 (38.84%) | 28548 (28.66%) | 57667 (47.13%) | <0.0001 |
| Race/Ethnicity | White | 173617 (78.22%) | 70610 (70.88%) | 103007(84.19%) | <0.0001 |
| Black | 18175 (8.19%) | 11877 (11.92%) | 6298 (5.15%) | ||
| Hispanic/Latino | 15394 (6.94%) | 9754 (9.79%) | 5640 (4.61%) | ||
| Other | 14775 (6.66%) | 7373 (7.4%) | 7402 (6.05%) | ||
| Marital status | Never Married | 57827 (26.05%) | 46935 (47.12%) | 10892 (8.90%) | <0.0001 |
| Married | 101438 (45.70%) | 37611 (37.76%) | 63827 (52.17%) | ||
| Widowed | 40792 (18.38%) | 2173 (2.18%) | 38619 (31.57%) | ||
| Separated | 3029 (1.36%) | 2186 (2.19%) | 843 (0.69%) | ||
| Divorced | 18875 (8.50%) | 10709 (10.75%) | 8166 (6.67%) | ||
| Pre-admission living arrangement | Alone | 57127 (25.74%) | 19489 (19.56%) | 37638 (30.76%) | <0.0001 |
| Family/Relatives | 152531 (68.72%) | 71020 (71.3%) | 81511 (66.62%) | ||
| Friends | 8850 (3.99%) | 7485 (7.51 %) | 1365 (1.12%) | ||
| Other | 3453 (1.56%) | 1620 (1.63%) | 1833 (1.5%) | ||
| Discharge living arrangement ** | Alone | 12128 (7.76%) | 4144 (5.06%) | 7984 (10.71%) | NA |
| Family/Relatives | 134965 (86.31%) | 72356 (88.40%) | 62609 (84.01%) | ||
| Friends | 4427 (2.83%) | 3445 (4.21%) | 982 (1.32%) | ||
| Other | 4859 (3.11%) | 1910 (2.33%) | 2949 (3.96%) | ||
| Insurance status | None | 8365 (3.77%) | 8190 (8.22%) | 175 (0.14%) | <0.0001 |
| Medicare | 124810 (56.23%) | 12538 (12.59%) | 112272 (91.77%) | ||
| Medicaid | 18670 (8.41%) | 17925 (17.99%) | 745 (0.61%) | ||
| Private | 66150 (29.80%) | 57515 (57.74%) | 8635 (7.06%) | ||
| Other | 3966 (1.79%) | 3446 (3.46%) | 520 (0.43%) | ||
| Clinical characteristics | |||||
| CMG Comorbidity Tier | Tier 0/None | 120271 (54.19%) | 52136 (52.34%) | 68135 (55.69%) | <0.0001 |
| Tier 1 | 14002 (6.31%) | 10767 (10.81%) | 3235 (2.64%) | ||
| Tier 2 | 42418 (19.11%) | 19891 (19.97%) | 22527 (18.41%) | ||
| Tier 3 | 45270 (20.40%) | 16820 (16.89%) | 28450 (23.25%) | ||
| Comorbidities | Infectious and Parasitic Diseases | 339 (0.15%) | 79 (0.08%) | 260 (0.21%) | <0.0001 |
| Neoplasms | 259 (0.12%) | 179 (0.18%) | 80 (0.07%) | <0.0001 | |
| Endocrine, Nutritional and Metabolic Diseases, and Immunity Disorders | 15983 (7.20%) | 4190 (4.21%) | 11793 (9.64%) | <0.0001 | |
| Diseases of the Blood and Blood-Forming Organs | 6966 (3.14%) | 2470 (2.48%) | 4496 (3.67%) | <0.0001 | |
| Mental Disorders | 10659 (4.80%) | 5592 (5.61%) | 5067 (4.14%) | <0.0001 | |
| Diseases of the Nervous System and Sense Organs | 8930 (4.02%) | 3350 (3.36%) | 5580 (4.56%) | <0.0001 | |
| Diseases of the Circulatory System | 21164 (9.54%) | 1451 (1.46%) | 2239 (1.83%) | ||
| Diseases of the Respiratory System | 962 (0.43%) | 522 (0.52%) | 440 (0.36%) | <0.0001 | |
| Diseases of the Digestive System | 4646 (2.09%) | 1359 (1.36%) | 3287 (2.69%) | <0.0001 | |
| Diseases of the Genitourinary System | 4508 (2.03%) | 1048 (1.05%) | 3460 (2.83%) | <0.0001 | |
| Diseases of the Skin and Subcutaneous Tissue | 984 (0.44%) | 381 (0.38%) | 603 (0.49%) | <0.0001 | |
| Diseases of the Musculoskeletal System and Connective Tissue | 6749 (3.04%) | 2583 (2.59%) | 4166 (3.41%) | <0.0001 | |
| Symptoms, Signs, And Ill-Defined Conditions | 20956 (9.44%) | 8408 (8.44%) | 12548 (10.26%) | <0.0001 | |
| Injury and Poisoning | 1826 (0.82%) | 1165 (1.17%) | 661 (0.54%) | <0.0001 | |
| Supplementary Classification of External Causes of Injury and Poisoning | 2267 (1.02%) | 687 (0.69%) | 1580 (1.29%) | <0.0001 | |
| Supplementary Classification of Factors Influencing Health Status and Contact with Health Service | 15316 (6.90%) | 6555 (6.58%) | 8761 (7.16%) | <0.0001 | |
| Complications | Infectious and Parasitic Diseases | 504 (0.23%) | 152 (0.15%) | 352 (0.29%) | <0.0001 |
| Neoplasms | 155 (0.07%) | 113 (0.11%) | 42 (0.03%) | <0.0001 | |
| Endocrine, Nutritional and Metabolic Diseases, and Immunity Disorders | 6884 (3.10%) | 2215 (2.22%) | 4669 (3.82%) | <0.0001 | |
| Diseases of The Blood and Blood-Forming Organs | 2552 (1.15%) | 1034 (1.04%) | 1518 (1.24%) | <0.0001 | |
| Mental Disorders | 3357 (1.51%) | 1650 (1.66%) | 1707 (1.4%) | <0.0001 | |
| Diseases of The Nervous System and Sense Organs | 1262 (0.57%) | 679 (0.68%) | 583 (0.48%) | <0.0001 | |
| Diseases of The Circulatory System | 3690 (1.66%) | 1451 (1.46%) | 2239 (1.83%) | <0.0001 | |
| Diseases of The Respiratory System | 508 (0.23%) | 176 (0.18%) | 332 (0.27%) | <0.0001 | |
| Diseases of the Digestive System | 943 (0.42%) | 478 (0.48%) | 465 (0.38%) | <0.0001 | |
| Diseases of The Genitourinary System | 1900 (0.86%) | 445 (0.45%) | 1455 (1.19%) | <0.0001 | |
| Diseases of the Skin and Subcutaneous Tissue | 1015 (0.46%) | 469 (0.47%) | 546 (0.45%) | 0.3939 | |
| Diseases of the Musculoskeletal System and Connective Tissue | 3065 (1.38%) | 1563 (1.57%) | 1502 (1.23%) | <0.0001 | |
| Symptoms, Signs, And Ill-Defined Conditions | 12178 (5.49%) | 5242 (5.26%) | 6936 (5.67%) | <0.0001 | |
| Injury and Poisoning | 322 (0.15%) | 181 (0.18%) | 141 (0.12%) | <0.0001 | |
| Supplementary Classification of External Causes of Injury and Poisoning | 577 (0.26%) | 245 (0.25%) | 332 (0.27%) | 0.2423 | |
| Supplementary Classification of Factors Influencing Health Status and Contact with Health Service | 1352 (0.61%) | 698 (0.7%) | 654 (0.53%) | <0.0001 | |
| Admission Motor Function | Admission FIM Motor Score, Mean (SD) | 36.41 (14.06) | 38.03 (15.74) | 35.09 (12.37) | <0.0001 |
| Admission Cognitive Function | Admission FIM Cognitive Score, Mean (SD) | 17.97 (7.62) | 16.79 (7.88) | 18.93 (7.27) | <0.0001 |
| Discharge Motor Function | Discharge FIM Motor Score, Mean (SD) | 60.94 (14.93) | 64.78 (14.80) | 57.83 (14.29) | <0.0001 |
| Discharge Cognitive Function | Discharge FIM Cognitive Score, Mean (SD) | 24.51 (6.61) | 24.39 (6.67) | 24.60 (6.56) | <0.0001 |
| Days Onset to Admission | Number of days, Mean (SD) | 14.74 (21.25) | 19.83 (25.69) | 10.59 (15.61) | <0.0001 |
| Length of Stay | Number of days, Mean (SD) | 16.11 (12.45) | 17.89 (16.41) | 14.67 (7.58) | <0.0001 |
| Year of Admission | 2002 | 10459 (4.71%) | 6107 (6.13%) | 4352 (3.56%) | <0.0001 |
| 2003 | 10663 (4.80%) | 5971 (5.99%) | 4692 (3.83%) | ||
| 2004 | 11046 (4.98%) | 5885 (5.91%) | 5161 (4.22%) | ||
| 2005 | 12415 (5.59%) | 6586 (6.61%) | 5829 (4.76%) | ||
| 2006 | 12719 (5.73%) | 6628 (6.65%) | 6091 (4.98%) | ||
| 2007 | 12840 (5.78%) | 6462 (6.49%) | 6378 (5.21%) | ||
| 2008 | 13848 (6.24%) | 6863 (6.89%) | 6985 (5.71%) | ||
| 2009 | 14025 (6.32%) | 6345 (6.37%) | 7680 (6.28%) | ||
| 2010 | 13512 (6.09%) | 6175 (6.2%) | 7337 (6%) | ||
| 2011 | 13674 (6.16%) | 6071 (6.09%) | 7603 (6.21%) | ||
| 2012 | 14276 (6.43%) | 6157 (6.18%) | 8119 (6.64%) | ||
| 2013 | 14292 (6.44%) | 6096 (6.12%) | 8196 (6.7%) | ||
| 2014 | 10060 (4.53%) | 4091 (4.11%) | 5969 (4.88%) | ||
| 2015 | 13876 (6.25%) | 4975 (4.99%) | 8901 (7.28%) | ||
| 2016 | 13748 (6.19%) | 4970 (4.99%) | 8778 (7.17%) | ||
| 2017 | 15109 (6.81%) | 5215 (5.24%) | 9894 (8.09%) | ||
| 2018 | 15399 (6.94%) | 5017 (5.04%) | 10382 (8.49%) | ||
| Facility Characteristics | |||||
| IRF location | Region P01 : CT, MA, ME, NH, RI, VT | 10501 (4.73%) | 4234 (4.25%) | 6267 (5.12%) | <0.0001 |
| Region P02 : NJ, NY, PR | 19707 (8.88%) | 8359 (8.39%) | 11348 (9.28%) | ||
| Region P03 : DE, MD, PA, VA, WV | 30555 (13.77%) | 12530 (12.58%) | 18025 (14.73%) | ||
| Region P04: AL, FL, GA, KT, MS, NC, TN, SC | 39579 (17.83%) | 17185 (17.25%) | 22394 (18.3%) | ||
| Region P05: IL, IN, MI, MN, OH, WI | 33136 (14.93%) | 15026 (15.08%) | 18110 (14.8%) | ||
| Region P06: AR, LA, NM, OK, TX | 28047 (12.64%) | 11246 (11.29%) | 16801 (13.73%) | ||
| Region P07: IA, KS, MO, NE | 13683 (6.16%) | 6658 (6.68%) | 7025 (5.74%) | ||
| Region P08: CO, MT, ND, SD, UT, WY | 12301 (5.54%) | 7473 (7.5%) | 4828 (3.95%) | ||
| Region P09: AZ, CA, HI, NV | 27503 (12.39%) | 12825 (12.87%) | 14678 (12%) | ||
| Region P10: AK, ID, OR, WA | 6949 (3.13%) | 4078 (4.09%) | 2871 (2.35%) | ||
| IRF type | Freestanding | 80421 (36.23%) | 35023 (35.16%) | 45398 (37.11%) | <0.0001 |
| Rehab Unit in Hospital | 141540 (63.77%) | 64591 (64.84%) | 76949 (62.89%) | ||
| IRF accreditation | Accreditation (Joint Commission and/or CARF) | 140971 (63.51%) | 70609 (70.88%) | 70362 (57.51%) | <0.0001 |
| No accreditation | 80990 (36.49%) | 29005 (29.12%) | 51985 (42.49%) | ||
| Discharge Destination | Home/community settings | 186460 (84%) | 88894 (89.24%) | 97566 (79.75%) | <0.0001 |
| Subacute settings | 35501 (16%) | 10720 (10.76%) | 24781 (20.25%) | ||
Note:
Discharge living arrangement only reported for those who went home, N=65582 missing; FIM = Functional Independence Measure; CARF = Commission on Accreditation of Rehabilitation Facilities; CMG = case mix group
Findings for Younger and Older Adults
Within the study sample, 45% of patients with TBI were between the ages of 18 and 64 years, and 55% were at least 65 years of age (Table 1). Although the sample was predominantly White, there was a larger proportion of Black, Hispanic and other races/ethnicities among younger adults. More older adults lived alone than younger adults, but the percentage of individuals living alone changed for both age groups from pre-admission (31% of older vs. 20% of younger) to post-IRF care (11% of older vs. 5% of younger). Nearly all of the patients without health insurance were younger adults. The primary payer was Medicare for older adults (92%) but was private insurance for younger adults (58%). Comorbidities, complications, admission FIM, days of onset to admission, and length of stay were significantly different between groups, but the differences were not clinical meaningful. Analysis by year showed more IRF admissions for younger and older adults after the enactment of the Affordable Care Act in 2010 than before. It was more common for younger adults to be discharged home (89%) than older adults (80%).
After adjusting for covariates, younger adults were less likely to be discharged to subacute than older adults [OR=0.72, 95%CI: 0.69, 0.76] (Table 2). Significant covariates (at p<.01) included sex, race/ethnicity, marital status, insurance status, CMG comorbidity tier, admission FIM cognitive score, discharge FIM motor and cognitive score, length of stay, days onset to admission, year of admission, IRF location, IRF type, and IRF accreditation.
Table 2.
Multivariate Logistic Regression (unadjusted and adjusted) for Association of Younger Age with Discharge to Subacute (vs. home [ref]) for Patients with TBI (N=221961)
| Variables | Values | Unadjusted | Adjusted | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | ||||
| Sociodemographic characteristics | |||||||||
| Age (reference = 65+ years) | 18-64 years | 0.48 | 0.46 | 0.49 | <.0001 | 0.72 | 0.69 | 0.76 | <.0001 |
| Sex (Ref = Male) | Female | 1.10 | 1.08 | 1.13 | <.0001 | 0.89 | 0.87 | 0.92 | <.0001 |
| Race/Ethnicity (Ref = White) | Black | 0.90 | 0.86 | 0.94 | <.0001 | 0.78 | 0.74 | 0.82 | <.0001 |
| Hispanic/Latino | 0.64 | 0.61 | 0.68 | <.0001 | 0.59 | 0.56 | 0.63 | <.0001 | |
| Other | 0.76 | 0.73 | 0.80 | <.0001 | 0.83 | 0.78 | 0.88 | <.0001 | |
| Marital status (Ref = Married) | Never Married | 1.02 | 0.99 | 1.05 | 0.2418 | 1.85 | 1.78 | 1.93 | <.0001 |
| Widowed | 1.87 | 1.82 | 1.92 | <.0001 | 1.80 | 1.74 | 1.87 | <.0001 | |
| Separated | 1.38 | 1.26 | 1.52 | <.0001 | 2.60 | 2.32 | 2.90 | <.0001 | |
| Divorced | 1.52 | 1.46 | 1.59 | <.0001 | 2.52 | 2.40 | 2.64 | <.0001 | |
| Insurance status (Ref = Private) | None | 0.90 | 0.83 | 0.98 | 0.0101 | 0.91 | 0.83 | 1.00 | 0.0389 |
| Medicare | 2.34 | 2.28 | 2.41 | <.0001 | 1.57 | 1.50 | 1.65 | <.0001 | |
| Medicaid | 1.45 | 1.38 | 1.53 | <.0001 | 1.24 | 1.17 | 1.32 | <.0001 | |
| Other | 1.03 | 0.93 | 1.15 | 0.5951 | 1.06 | 0.94 | 1.20 | 0.3446 | |
| Clinical characteristics | |||||||||
| CMG Comorbidity Tier (Ref = Tier 0/None) | Tier 1 | 1.61 | 1.54 | 1.68 | <.0001 | 0.84 | 0.79 | 0.89 | <.0001 |
| Tier 2 | 1.86 | 1.80 | 1.91 | <.0001 | 1.06 | 1.02 | 1.10 | 0.0018 | |
| Tier 3 | 1.23 | 1.20 | 1.27 | <.0001 | 1.04 | 1.01 | 1.08 | 0.0264 | |
| Admission Motor Function | Admission FIM Motor Score | 0.95 | 0.94 | 0.95 | <.0001 | ||||
| Admission Cognitive Function | Admission FIM Cognitive Score | 0.93 | 0.93 | 0.93 | <.0001 | 0.99 | 0.99 | 0.99 | <.0001 |
| Discharge Motor Function | Discharge FIM Motor Score | 0.93 | 0.93 | 0.93 | <.0001 | 0.94 | 0.94 | 0.934 | <.0001 |
| Discharge Cognitive Function | Discharge FIM Cognitive Score | 0.89 | 0.89 | 0.89 | <.0001 | 0.96 | 0.96 | 0.96 | <.0001 |
| Days Onset to Admission | Number of days | 1.01 | 1.01 | 1.01 | <.0001 | 1.00 | 1.00 | 1.00 | <.0001 |
| Length of Stay | Number of days | 1.03 | 1.03 | 1.03 | <.0001 | 1.01 | 1.01 | 1.02 | <.0001 |
| Year of admission (Ref = 2018) | 2002 | 1.05 | 0.98 | 1.12 | 0.2123 | 1.11 | 1.02 | 1.21 | 0.0135 |
| 2003 | 1.03 | 0.96 | 1.10 | 0.4908 | 1.00 | 0.92 | 1.09 | 0.9970 | |
| 2004 | 1.02 | 0.95 | 1.10 | 0.5325 | 1.01 | 0.93 | 1.10 | 0.7599 | |
| 2005 | 1.04 | 0.98 | 1.11 | 0.2158 | 0.99 | 0.92 | 1.07 | 0.8463 | |
| 2006 | 1.18 | 1.11 | 1.26 | <.0001 | 1.10 | 1.02 | 1.19 | 0.0114 | |
| 2007 | 1.18 | 1.11 | 1.26 | <.0001 | 1.09 | 1.01 | 1.18 | 0.0215 | |
| 2008 | 1.20 | 1.12 | 1.28 | <.0001 | 1.08 | 1.00 | 1.16 | 0.0413 | |
| 2009 | 1.24 | 1.16 | 1.32 | <.0001 | 1.10 | 1.03 | 1.19 | 0.0079 | |
| 2010 | 1.23 | 1.16 | 1.31 | <.0001 | 1.11 | 1.03 | 1.20 | 0.0047 | |
| 2011 | 1.13 | 1.06 | 1.21 | 0.0001 | 1.03 | 0.96 | 1.11 | 0.3838 | |
| 2012 | 1.14 | 1.07 | 1.22 | <.0001 | 1.06 | 0.99 | 1.15 | 0.0959 | |
| 2013 | 1.10 | 1.03 | 1.17 | 0.0049 | 1.04 | 0.97 | 1.12 | 0.2748 | |
| 2014 | 1.07 | 1.00 | 1.15 | 0.0547 | 1.07 | 0.98 | 1.15 | 0.1265 | |
| 2015 | 1.07 | 1.00 | 1.14 | 0.0424 | 1.02 | 0.95 | 1.10 | 0.6301 | |
| 2016 | 1.06 | 1.00 | 1.13 | 0.0616 | 1.05 | 0.98 | 1.13 | 0.1878 | |
| 2017 | 1.00 | 0.94 | 1.07 | 0.9134 | 0.99 | 0.92 | 1.07 | 0.8466 | |
| Facility Characteristics | |||||||||
| IRF location (Ref = Region P02: NJ, NY, PR) | Region P01: CT, MA, ME, NH, RI, VT | 1.01 | 0.95 | 1.06 | 0.8647 | 1.08 | 1.01 | 1.16 | 0.0321 |
| Region P03: DE, MD, PA, VA, WV | 0.67 | 0.64 | 0.70 | <.0001 | 0.62 | 0.59 | 0.66 | <.0001 | |
| Region P04: AL, FL, GA, KT, MS, NC, TN, SC | 0.52 | 0.50 | 0.55 | <.0001 | 0.37 | 0.35 | 0.39 | <.0001 | |
| Region P05: IL, IN, MI, MN, OH, WI | 0.72 | 0.69 | 0.75 | <.0001 | 0.76 | 0.72 | 0.80 | <.0001 | |
| Region P06: AR, LA, NM, OK, TX | 0.69 | 0.66 | 0.73 | <.0001 | 0.64 | 0.61 | 0.68 | <.0001 | |
| Region P07: IA, KS, MO, NE | 0.74 | 0.70 | 0.79 | <.0001 | 0.85 | 0.79 | 0.90 | <.0001 | |
| Region P08: CO, MT, ND, SD, UT, WY | 0.52 | 0.49 | 0.55 | <.0001 | 0.70 | 0.65 | 0.75 | <.0001 | |
| Region P09: AZ, CA, HI, NV | 0.41 | 0.39 | 0.43 | <.0001 | 0.33 | 0.31 | 0.35 | <.0001 | |
| Region P10: AK, ID, OR, WA | 0.32 | 0.29 | 0.35 | <.0001 | 0.40 | 0.36 | 0.44 | <.0001 | |
| IRF type (Ref = Rehab Unit in Hospital) | Freestanding | 0.97 | 0.94 | 0.99 | 0.0034 | 0.81 | 0.79 | 0.84 | <.0001 |
| IRF accreditation (Ref = No accreditation) | Accreditation (Joint Commission and/or CARF) | 1.05 | 1.02 | 1.07 | <.0001 | 1.13 | 1.10 | 1.17 | <.0001 |
Note: Ref = Reference; FIM = Functional Independence Measure; CMG = case mix group
Findings by Sex for Younger and Older Adults
Specific to younger adults, the mean age of younger males was 41 compared to 44 for younger females. Most younger males (70%) and younger females (75%) were White, and there were high proportions of Black, Hispanic/Latino, and other races/ethnicities. Specific to living arrangement, 20% of younger males and 18% of younger females lived alone pre-admission, but most younger males and younger females lived with family or relatives upon discharge (88% vs. 89%). Most younger males and younger females had private insurance (57% vs. 59%). Most younger males and females had Tier 1 case mix group comorbidities. Younger males had higher admission and discharge FIM motor scores than younger females but lower admission and discharge FIM cognitive scores. Analysis by year shows more IRF admissions were present before the enactment of the Affordable Care Act in 2010 for younger males and females.
Specific to older adults, the mean age of older males was 78 compared to 80 for older females. Most older males and older females were White (83% vs. 85%), and there were low percentages of Black, Hispanic/Latino and other races/ethnicities. Although many older males and older females lived alone pre-admission (21% of males vs. 41% of females), the percentage of patients living alone post-discharge decreased after IRF care (7% of males vs. 15% of females); most older males and older females lived with family or relatives upon IRF discharge (88% of males vs. 79% of females). Most older males (90%) and older females (93%) had Medicare. Most older males and females had Tier 1 case mix group comorbidities. Older males had lower admission and discharge FIM motor and cognitive scores than older females. Analysis by year shows fewer IRF admissions for younger males and females after enactment of the Affordable Care Act in 2010 than before; in contrast, there were more IRF admissions for older males and females after enactment of the Affordable Care Act in 2010 than before.
Findings on Discharge Destination Stratified by Age and Sex
Among females (Table 4), 9.99% of younger females were discharged to subacute (vs. home) compared to 20.20% of older females. Similarly, among males, 11.08% of younger males were discharged to subacute settings compared to 20.56% of older males. Among females, younger females were significantly less likely to be discharged to subacute settings (vs. home) compared to older females [OR=0.68, 95% CI: 0.63, 0.74] after adjusting for all other significant predictors. Similar trends were seen in male patients, as younger males were significantly less likely to be discharged to subacute settings (vs. home) [OR=0.74, 95% CI: 0.70, 0.78] compared to older males, but the odds ratio for males was larger than in the female group.
Table 4.
Logistic Regression (unadjusted and adjusted) for Discharge to Subacute for Younger vs. Older Age by Sex Group (N=221961)
| Discharge Destination |
Younger (18-64) |
Older (65+) |
Unadjusted | Adjusted | ||
|---|---|---|---|---|---|---|
| OR (95% CI) |
p | OR (95% CI) |
p | |||
| Females | N=28,548 | N=57,667 | ||||
| Subacute | 2850 (9.99% of younger females) | 11645 (20.20% of older females) | 2.28 (2.18, 2.38) | <.0001 | 0.68 (0.63, 0.74)* | <.0001 |
| Home [ref] | 25698 (90.01% of younger females) | 46022 (79.80% of older females) | ||||
| Males | N=71,066 | N=64,880 | ||||
| Subacute | 7870 (11.08% of younger males) | 13136 (20.56% of older males) | 2.05 (1.99, 2.11) | <.0001 | 0.74 (0.70, 0.78)+ | <.0001 |
| Home [ref] | 63196 (88.92% of younger males) | 51544 (79.44% of older males) | ||||
Note:
Adjusted for admission motor FIM, discharge motor FIM, discharge cognition FIM, CMG comorbidity tier, length of stay, days onset to admission, race/ethnicity, region, facility type, IRF certification, insurance, marital status
Adjusted for admission cognition FIM, discharge motor FIM, discharge cognition FIM, CMG comorbidity tier, length of stay, days onset to admission, race/ethnicity, region, facility type, IRF certification, insurance, marital status
Among younger patients (Table 5), younger females were significantly less likely to be discharged to subacute settings (vs. home) compared to younger males [OR=0.83, 95%CI: 10.79, 0.87] after adjusting for all other significant predictors. Similarly for older patients, older females were more likely to be discharged to subacute settings (vs. home) compared to older males, [OR=0.93, 95% CI: 0.90, 0.97], but the odds ratio among older patients was a little larger than in the younger group.
Table 5.
Logistic Regression (unadjusted and adjusted) for Discharge to Subacute for Female vs. Male Sex by Age Group (N=221961)
| Discharge Destination |
Females | Males | Unadjusted | Adjusted | ||
|---|---|---|---|---|---|---|
| OR (95% CI) |
p | OR (95% CI) |
p | |||
| Younger (18-64) | N=28,548 | N=71,066 | ||||
| Subacute | 2850 (9.99% of younger females) | 7870 (11.08% of younger males) | 0.89 (0.85, 0.93) | <.0001 | 0.83 (0.79, 0.87)* | <.0001 |
| Home [ref] | 25698 (90.01% of younger females) | 63196 (88.92% of younger males) | ||||
| Older (65+) | N=57,667 | N=64,880 | ||||
| Subacute | 11645 (20.20% of older females) | 13136 (20.56% of older males) | 0.99 (0.97, 1.02) | 0.6153 | 0.93 (0.90, 0.97)+ | <.0001 |
| Home [ref] | 46022 (79.80% of older females) | 51544 (79.44% of older males) | ||||
Note:
Adjusted for admission cognitive FIM, discharge motor FIM, discharge cognition FIM, CMG comorbidity tier, length of stay, days onset to admission, race/ethnicity, discharge year, region, facility type, insurance, marital status
Adjusted for admission motor FIM, discharge motor FIM, discharge cognition FIM, length of stay, days onset to admission, race/ethnicity, discharge year, region, facility type, IRF certification, insurance, marital status
Findings on Predictors of Discharge Home by Sex for Younger and Older Adults
Regression models to identify independent predictors of discharge home among the four population subgroups illustrated the importance of sociodemographic variables and facility characteristics but variables in the model explained very little of the variance (R2=0.14-0.24) and did not identify a consistent set of variables for predicting discharge to subacute settings (see Table 6). Significant covariates in adjusted models (at p<.01) included: race/ethnicity; marital status; insurance status; CMG comorbidity tier; admission and discharge cognitive and motor FIM scores; days of onset to admission; length of stay; year of admission; and IRF location, type, and accreditation.
Table 6.
Four models displaying predictors of discharge to subacute (vs. home [ref]) for younger males, younger females, older males, and older females, adjusted for covariates
| Variables | Values | Younger Males N=71066 |
Younger Females N=28548 |
Older Males N=64680 |
Older Females N=57667 |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | ||||||
| Race/Ethnicity (Ref = White) | Black | 1.00 | 0.93 | 1.09 | 0.9115 | 0.81 | 0.70 | 0.94 | 0.0053 | 0.75 | 0.68 | 0.83 | <.0001 | 0.48 | 0.42 | 0.54 | <.0001 |
| Hispanic/Latino | 0.70 | 0.64 | 0.77 | <.0001 | 0.64 | 0.52 | 0.78 | <.0001 | 0.61 | 0.54 | 0.68 | <.0001 | 0.38 | 0.33 | 0.44 | <.0001 | |
| Other | 0.87 | 0.78 | 0.97 | 0.0113 | 0.86 | 0.72 | 1.04 | 0.1294 | 0.79 | 0.71 | 0.88 | <.0001 | 0.83 | 0.74 | 0.93 | 0.0010 | |
| Marital status (Ref = Married) | Never Married | 1.34 | 1.26 | 1.43 | <.0001 | 1.32 | 1.18 | 1.48 | <.0001 | 2.93 | 2.72 | 3.17 | <.0001 | 2.55 | 2.33 | 2.79 | <.0001 |
| Widowed | 2.23 | 1.83 | 2.73 | <.0001 | 1.89 | 1.55 | 2.30 | <.0001 | 1.95 | 1.84 | 2.08 | <.0001 | 1.84 | 1.74 | 1.95 | <.0001 | |
| Separated | 2.35 | 2.00 | 2.76 | <.0001 | 2.04 | 1.57 | 2.65 | <.0001 | 2.68 | 2.10 | 3.42 | <.0001 | 2.59 | 1.94 | 3.45 | <.0001 | |
| Divorced | 2.19 | 2.01 | 2.39 | <.0001 | 2.55 | 2.24 | 2.90 | <.0001 | 2.82 | 2.57 | 3.09 | <.0001 | 2.23 | 2.02 | 2.45 | <.0001 | |
| Insurance status (Ref = Private) | None | 0.98 | 0.89 | 1.09 | 0.7484 | 0.84 | 0.67 | 1.056 | 0.1386 | 0.30 | 0.13 | 0.71 | 0.0065 | 0.46 | 0.20 | 1.04 | 0.0633 |
| Medicare | 1.97 | 1.82 | 2.13 | <.0001 | 2.03 | 1.80 | 2.28 | <.0001 | 1.20 | 1.10 | 1.31 | <.0001 | 1.24 | 1.11 | 1.39 | 0.0002 | |
| Medicaid | 1.34 | 1.24 | 1.43 | <.0001 | 1.40 | 1.24 | 1.58 | <.0001 | 0.62 | 0.44 | 0.89 | 0.0082 | 0.59 | 0.40 | 0.88 | 0.0088 | |
| Other | 1.05 | 0.90 | 1.22 | 0.5608 | 1.08 | 0.81 | 1.43 | 0.6216 | 0.96 | 0.68 | 1.37 | 0.8320 | 1.17 | 0.75 | 1.82 | 0.4989 | |
| CMG Comorbidity Tier (Ref = 0/None) | Tier 1 | 0.88 | 0.81 | 0.96 | 0.0041 | 1.00 | 0.85 | 1.17 | 0.9799 | ||||||||
| Tier 2 | 1.06 | 0.99 | 1.14 | 0.1035 | 1.28 | 1.14 | 1.44 | <.0001 | |||||||||
| Tier 3 | 1.10 | 1.02 | 1.19 | 0.0170 | 1.24 | 1.10 | 1.41 | 0.0004 | |||||||||
| Admission Motor Function | Admission FIM Motor Score | 1.00 | 0.99 | 1.00 | 0.0497 | 1.01 | 1.00 | 1.01 | <.0001 | ||||||||
| Admission Cognitive Function | Admission FIM Cognitive Score | 0.99 | 0.98 | 1.00 | 0.0006 | 0.98 | 0.97 | 0.99 | <.0001 | ||||||||
| Discharge Motor Function | Discharge FIM Motor Score | 0.96 | 0.96 | 0.96 | <.0001 | 0.95 | 0.94 | 0.95 | <.0001 | 0.92 | 0.92 | 0.93 | <.0001 | 0.92 | 0.92 | 0.93 | <.0001 |
| Discharge Cognitive Function | Discharge FIM Cognitive Score | 0.95 | 0.94 | 0.95 | <.0001 | 0.95 | 0.94 | 0.96 | <.0001 | 0.96 | 0.96 | 0.96 | <.0001 | 0.97 | 0.96 | 0.97 | <.0001 |
| Days Onset to Admission | Number of days | 1.00 | 1.00 | 1.00 | <.0001 | 1.00 | 1.00 | 1.00 | <.0001 | 1.00 | 1.00 | 1.00 | <.0001 | ||||
| Length of Stay | Number of days | 1.01 | 1.01 | 1.01 | <.0001 | 1.01 | 1.01 | 1.01 | <.0001 | 1.03 | 1.03 | 1.03 | <.0001 | 1.04 | 1.03 | 1.04 | <.0001 |
| Year of admission (Ref = 2018) | 2002 | 1.20 | 1.02 | 1.41 | 0.0309 | 0.91 | 0.78 | 1.06 | 0.2146 | 1.01 | 0.87 | 1.18 | 0.8726 | ||||
| 2003 | 1.09 | 0.92 | 1.28 | 0.3233 | 0.87 | 0.75 | 1.01 | 0.0671 | 0.87 | 0.74 | 1.01 | 0.0747 | |||||
| 2004 | 1.06 | 0.89 | 1.25 | 0.5260 | 0.88 | 0.76 | 1.02 | 0.0788 | 0.85 | 0.73 | 0.99 | 0.0378 | |||||
| 2005 | 0.94 | 0.80 | 1.10 | 0.4359 | 0.91 | 0.79 | 1.04 | 0.1640 | 0.93 | 0.81 | 1.08 | 0.3439 | |||||
| 2006 | 1.07 | 0.91 | 1.25 | 0.4088 | 1.00 | 0.88 | 1.14 | 0.9611 | 1.14 | 1.00 | 1.31 | 0.0580 | |||||
| 2007 | 1.01 | 0.86 | 1.18 | 0.9394 | 1.11 | 0.98 | 1.26 | 0.0955 | 1.02 | 0.89 | 1.17 | 0.7608 | |||||
| 2008 | 0.98 | 0.84 | 1.15 | 0.8394 | 1.07 | 0.94 | 1.21 | 0.3127 | 1.11 | 0.97 | 1.26 | 0.1310 | |||||
| 2009 | 1.08 | 0.92 | 1.26 | 0.3629 | 1.05 | 0.93 | 1.18 | 0.4632 | 1.10 | 0.97 | 1.25 | 0.1437 | |||||
| 2010 | 1.15 | 0.98 | 1.35 | 0.0842 | 0.99 | 0.88 | 1.12 | 0.9148 | 1.13 | 0.99 | 1.29 | 0.0608 | |||||
| 2011 | 1.04 | 0.89 | 1.23 | 0.6141 | 0.94 | 0.83 | 1.07 | 0.3495 | 1.14 | 1.00 | 1.30 | 0.0518 | |||||
| 2012 | 1.07 | 0.91 | 1.25 | 0.4411 | 1.04 | 0.92 | 1.18 | 0.4943 | 1.09 | 0.96 | 1.24 | 0.1913 | |||||
| 2013 | 0.95 | 0.81 | 1.12 | 0.5659 | 1.08 | 0.96 | 1.22 | 0.2050 | 1.11 | 0.98 | 1.26 | 0.1121 | |||||
| 2014 | 1.02 | 0.85 | 1.22 | 0.8638 | 1.01 | 0.89 | 1.16 | 0.8627 | 1.17 | 1.02 | 1.35 | 0.0258 | |||||
| 2015 | 0.92 | 0.77 | 1.09 | 0.3123 | 0.98 | 0.87 | 1.10 | 0.6913 | 1.08 | 0.95 | 1.23 | 0.2385 | |||||
| 2016 | 1.06 | 0.90 | 1.26 | 0.5012 | 1.01 | 0.90 | 1.14 | 0.8145 | 1.12 | 0.99 | 1.27 | 0.0803 | |||||
| 2017 | 0.95 | 0.80 | 1.13 | 0.5444 | 1.03 | 0.92 | 1.16 | 0.6074 | 1.01 | 0.89 | 1.14 | 0.9223 | |||||
| IRF location (Ref = Region P02: NJ, NY, PR) | P01: CT, MA, ME, NH, RI, VT | 0.79 | 0.69 | 0.91 | 0.0013 | 1.15 | 0.91 | 1.44 | 0.2401 | 1.19 | 1.06 | 1.34 | 0.0040 | 1.34 | 1.18 | 1.52 | <.0001 |
| P03: DE, MD, PA, VA, WV | 0.48 | 0.44 | 0.54 | <.0001 | 0.53 | 0.44 | 0.63 | <.0001 | 0.74 | 0.67 | 0.81 | <.0001 | 0.76 | 0.69 | 0.83 | <.0001 | |
| P04: AL, FL, GA, KT, MS, NC, TN, SC | 0.20 | 0.18 | 0.23 | <.0001 | 0.21 | 0.18 | 0.25 | <.0001 | 0.51 | 0.47 | 0.56 | <.0001 | 0.55 | 0.50 | 0.61 | <.0001 | |
| P05: IL, IN, MI, MN, OH, WI | 0.63 | 0.57 | 0.70 | <.0001 | 0.69 | 0.59 | 0.82 | <.0001 | 0.85 | 0.77 | 0.93 | 0.0005 | 0.95 | 0.86 | 1.04 | 0.2583 | |
| P06: AR, LA, NM, OK, TX | 0.47 | 0.42 | 0.52 | <.0001 | 0.49 | 0.41 | 0.59 | <.0001 | 0.77 | 0.70 | 0.85 | <.0001 | 0.88 | 0.79 | 0.97 | 0.0079 | |
| P07: IA, KS, MO, NE | 0.66 | 0.59 | 0.75 | <.0001 | 0.56 | 0.45 | 0.69 | <.0001 | 0.97 | 0.87 | 1.09 | 0.6042 | 1.19 | 1.05 | 1.34 | 0.0054 | |
| P08: CO, MT, ND, SD, UT, WY | 0.42 | 0.37 | 0.48 | <.0001 | 0.49 | 0.39 | 0.61 | <.0001 | 0.99 | 0.87 | 1.13 | 0.9312 | 1.12 | 0.97 | 1.30 | 0.1228 | |
| P09: AZ, CA, HI, NV | 0.27 | 0.25 | 0.31 | <.0001 | 0.28 | 0.23 | 0.34 | <.0001 | 0.37 | 0.34 | 0.41 | <.0001 | 0.41 | 0.37 | 0.46 | <.0001 | |
| P10: AK, ID, OR, WA | 0.31 | 0.26 | 0.37 | <.0001 | 0.32 | 0.24 | 0.44 | <.0001 | 0.45 | 0.37 | 0.54 | <.0001 | 0.51 | 0.41 | 0.63 | <.0001 | |
| IRF type (Ref = Rehabilitation Unit in Hospital) | Freestanding | 0.77 | 0.72 | 0.81 | <.0001 | 0.76 | 0.69 | 0.85 | <.0001 | 0.83 | 0.79 | 0.87 | <.0001 | 0.85 | 0.80 | 0.89 | <.0001 |
| IRF accreditation (Ref = No accreditation) | Accreditation (JACHO and/or CARF) | 1.123 | 1.02 | 1.25 | 0.0198 | 1.16 | 1.10 | 1.212 | <.0001 | 1.20 | 1.14 | 1.26 | <.0001 | ||||
| R2 | R2=0.14 | R2=0.15 | R2=0.24 | R2=0.22 | |||||||||||||
Discussion
The purpose of this study was to determine the association of age and sex on discharge destination among adult patients with TBI who received IRF care. Findings from multivariate models showed age and sex were significant predictors of discharge to subacute settings, as patients who were younger (vs. older) and female (vs. male) were less likely to be discharged to subacute settings than home. The stratification of age and sex on discharge destination was also significant, as females regardless of age, and younger patients, regardless of sex, were significantly less likely to be discharged to subacute than home. Predictors of discharge destination for groups stratified by age and sex varied by subgroup.
Similar to prior research,11,18 findings show age and sex as covariates in multivariate models predict IRF discharge destination. Findings from the present study make a significant contribution to TBI outcomes literature due to investigation of both younger and older adults in the same sample; examination of differences in predictors by age and sex group; and incorporation of comorbidities, complications, and facility-level variables into multivariate models.
Findings showed more patients were discharged to subacute compared to home/community settings. In addition, the age and sex stratification of discharge destination showed women are more likely to go home (vs. subacute) after IRF care than men, regardless of age. Although discharge to home is a positive outcome, upon returning home, many patients deal with residual impairments and may be unable to return to pre-injury levels of functioning, as TBI is considered a chronic condition.2 The struggle to return to pre-injury roles is associated with depression, and rates of depression after TBI are often higher among women.14,32 In addition, as women are often the primary caregivers at home, and may struggle to return to their pre-injury caregiving role, concerns exist regarding the adequate level of social support for women after discharge home from IRF care.18
Specific to predictors of discharge destination by subgroup (younger females, younger males, older females, and older males), findings showed two of the strongest predictors of discharge to subacute settings among these subgroups were marital status and insurance status. In particular, being never married, widowed, separated, or divorced (vs. married) increased likelihood of discharge to home. Having Medicare, Medicaid, or no insurance (vs. private insurance) either increased or decreased the likelihood of discharge to subacute settings (vs. home), depending on subgroup. Marital status, often used as a proxy for social support, is an important factor to be considered in selection of discharge destination and community reintegration, as patients with less social support may struggle to live independently post-discharge.33,34 Insurance status has been shown in prior research to be a strong predictor of patient outcomes, demonstrated in TBI research conducted using emergency department, acute care, and IRF data.35-39 Our findings showing insurance is a strong predictor of discharge destination echo the multitude of research that shows having health insurance can improve patient health and increase healthcare utilization.40
Our findings can be used to inform IRF planning, allocation of resources, and transitional care planning. Although age and sex are not modifiable variables, they are factors that clinicians can account for when making clinical decisions. Findings from the present study demonstrate the need for individualized planning based on the unique characteristics of the patient as older (vs. younger) and male (vs. male) patients are more likely to be discharged to subacute settings, as approximately 10% of younger and 20% of older adults are discharged to subacute settings. Based on these findings, providers may wish to provide additional rehabilitation or increase the intensity of rehabilitation for older patients and male patients may be at higher risk for discharge to subacute settings to increase the likelihood that these patients return home at rates comparable to younger and female patients. Alternatively, researchers and providers may wish to develop transitional care interventions to improve provide support given to who are at risk for poorer outcomes.
Strengths and Limitations
This study includes multiple strengths including a large, multi-year, multi-site dataset. However, this study is not without limitations. This dataset contains no information on the patient’s injury severity or hospital care prior to admission to the IRF. As a result, we controlled for admission functional status as a proxy for injury severity. In addition, selection bias is a limitation as there are multiple factors (such as patient’s insurance status and ability to tolerate rehabilitation) that determine which post-acute care services a patient with TBI receives rehabilitation that are complex and beyond the scope of our study. This study also has other limitations that are common in secondary analyses. For instance, the dataset we used does not allow us to assess causality or to test for potential confounders, even though variables that were unmeasured in the data set or are unmeasurable in clinical settings may have influenced our findings. The dataset also does not include data on the hospital subscribers or data on the specific IRF in which patients received care, so we are unable to assess IRF-level clustering effects. In addition, we did not adjust for multiple comparisons.
Conclusions
The findings show that age and sex are significant predictors of discharge destination among patients with TBI who received IRF care, as younger patients (vs. older) and female patients (vs. male) had higher odds of discharge to home. In addition, the interaction of age and sex significantly predicted the likelihood of discharge to home. However, predictors of discharge home varied by age and sex group. Findings can be used to inform providers of factors increasing odds of poor discharge outcomes and can also be used to inform development of interventions aimed to address IRF patient needs, allocation of resources, and transitional care planning. Future studies may also examine interconnections between factors that predict discharge rehabilitation outcomes.
Table 3.
Patient and Facility Characteristics of TBI Patients Receiving Inpatient Rehabilitation by Age and Sex (N = 221961)
| Variables | Values | Younger Males N = 71066, 32.01% |
Younger Females N = 28548, 12.86% |
Older Males N =64680, 29.14% |
Older Females N =57667, 25.99% |
|---|---|---|---|---|---|
| Sociodemographic characteristics | |||||
| Age | Years, Mean (SD) | 41.20 (14.63) | 44.46 (14.55) | 77.84 (7.31) | 79.50 (7.34) |
| Race/Ethnicity | White | 49324 (69.41%) | 21286 (74.56%) | 53872 (83.29%) | 49135 (85.20%) |
| Black | 8698 (12.24%) | 3179 (11.14%) | 3515 (5.43%) | 2783 (4.83%) | |
| Hispanic/Latino | 7719 (10.86%) | 2035 (7.13%) | 3152 (4.87%) | 2488 (4.31%) | |
| Other | 5325 (7.49%) | 2048 (7.17%) | 4141 (6.40%) | 3261 (5.65%) | |
| Marital status | Never Married | 35904 (50.52%) | 11031 (38.64%) | 5888 (9.10%) | 5004 (8.68%) |
| Married | 26038 (36.64%) | 11573 (40.54%) | 43774 (67.68%) | 20053 (34.77%) | |
| Widowed | 851 (1.20%) | 1322 (4.63%) | 10670 (16.50%) | 27949 (48.47%) | |
| Separated | 1472 (2.07%) | 714 (2.50%) | 480 (0.74%) | 363 (0.63%) | |
| Divorced | 6801 (9.57%) | 3908 (13.69%) | 3868 (5.98%) | 4298 (7.45%) | |
| Pre-admission living arrangement | Alone | 14211 (20.00%) | 5278 (18.49%) | 13987 (21.62%) | 23651 (41.01%) |
| Family/Relatives | 49943 (70.28%) | 21077 (73.83%) | 49040 (75.82%) | 32471 (56.31%) | |
| Friends | 5721 (8.05%) | 1764 (6.18%) | 868 (1.34%) | 497 (0.86%) | |
| Other | 1191 (1.68 %) | 429 (1.50 %) | 785 (1.21%) | 1048 (1.82%) | |
| Discharge living arrangement** | Alone | 2878 (4.93%) | 1266 (5.39%) | 2887 (7.20%) | 5097 (14.82%) |
| Family/Relatives | 51540 (88.30%) | 20816 (88.64%) | 35342 (88.09%) | 27267 (79.26%) | |
| Friends | 2539 (4.35%) | 906 (3.86%) | 583 (1.45%) | 399 (1.16%) | |
| Other | 1413 (2.42%) | 497 (2.12%) | 1308 (3.26%) | 1641 (4.77%) | |
| Insurance status | None | 6637 (9.34%) | 1553 (5.44%) | 99 (0.15%) | 76 (0.13%) |
| Medicare | 8028 (11.30%) | 4510 (15.80%) | 58382 (90.26%) | 53890 (93.45%) | |
| Medicaid | 13016 (18.32%) | 4909 (17.20%) | 403 (0.62%) | 342 (0.59%) | |
| Private | 40764 (57.36%) | 16751 (58.68%) | 5472 (8.46%) | 3163 (5.48%) | |
| Other | 2621 (3.69%) | 825 (2.89%) | 324 (0.50%) | 196 (0.34%) | |
| Clinical characteristics | |||||
| CMG Comorbidity Tier | Tier 0/None | 36643 (51.56%) | 15493 (54.27%) | 33274 (51.44%) | 34861 (60.45%) |
| Tier 1 | 8192 (11.53%) | 2575 (9.02%) | 2061 (3.19%) | 1174 (2.04%) | |
| Tier 2 | 14719 (20.71%) | 5172 (18.12%) | 13711 (21.20%) | 8816 (15.29%) | |
| Tier 3 | 11512 (16.20%) | 5308 (18.59%) | 15634 (24.17%) | 12816 (22.22%) | |
| Comorbidities | Infectious and Parasitic Diseases | 43 (0.06%) | 36 (0.13%) | 151 (0.23%) | 109 (0.19%) |
| Neoplasms | 136 (0.19%) | 43 (0.15%) | 37 (0.06%) | 43 (0.07%) | |
| Endocrine, Nutritional and Metabolic Diseases, and Immunity Disorders | 2777 (3.91%) | 1413 (4.95%) | 6021 (9.31%) | 5772 (10.01%) | |
| Diseases of the Blood and Blood-Forming Organs | 1627 (2.29%) | 843 (2.95%) | 2331 (3.60%) | 2165 (3.75%) | |
| Mental Disorders | 4138 (5.82%) | 1454 (5.09%) | 2834 (4.38%) | 2233 (3.87%) | |
| Diseases of the Nervous System and Sense Organs | 2312 (3.25%) | 1038 (3.64%) | 3178 (4.91%) | 2402 (4.17%) | |
| Diseases of the Circulatory System | 3705 (5.21%) | 1582 (5.54%) | 8455 (13.07%) | 7422 (12.87%) | |
| Diseases of the Respiratory System | 373 (0.52%) | 149 (0.52%) | 274 (0.42%) | 166 (0.29%) | |
| Diseases of the Digestive System | 885 (1.25%) | 474 (1.66%) | 1541 (2.38%) | 1746 (3.03%) | |
| Diseases of the Genitourinary System | 740 (1.04%) | 308 (1.08%) | 2197 (3.40%) | 1263 (2.19%) | |
| Diseases of the Skin and Subcutaneous Tissue | 274 (0.39%) | 107 (0.37%) | 365 (0.56%) | 238 (0.41%) | |
| Diseases of the Musculoskeletal System and Connective Tissue | 1736 (2.44%) | 847 (2.97%) | 2116 (3.27%) | 2050 (3.55%) | |
| Symptoms, Signs, And Ill-Defined Conditions | 5889 (8.29%) | 2519 (8.82%) | 6794 (10.50%) | 5754 (9.98%) | |
| Injury and Poisoning | 852 (1.20%) | 313 (1.10%) | 365 (0.56%) | 296 (0.51%) | |
| Supplementary Classification of External Causes of Injury and Poisoning | 484 (0.68%) | 203 (0.71%) | 784 (1.21%) | 796 (1.38%) | |
| Supplementary Classification of Factors Influencing Health Status and Contact with Health Service | 4764 (6.70%) | 1791 (6.27%) | 4814 (7.44%) | 3947 (6.84%) | |
| Complications | Infectious and Parasitic Diseases | 90 (0.13%) | 62 (0.22%) | 196 (0.30%) | 156 (0.27%) |
| Neoplasms | 94 (0.13%) | 19 (0.07%) | 16 (0.02%) | 26 (0.05%) | |
| Endocrine, Nutritional and Metabolic Diseases, and Immunity Disorders | 1584 (2.23%) | 631 (2.21%) | 2392 (3.70%) | 2277 (3.95%) | |
| Diseases of The Blood and Blood-Forming Organs | 715 (1.01%) | 319 (1.12%) | 818 (1.26%) | 700 (1.21%) | |
| Mental Disorders | 1215 (1.71%) | 435 (1.52%) | 930 (1.44%) | 777 (1.35%) | |
| Diseases of The Nervous System and Sense Organs | 497 (0.70%) | 182 (0.64%) | 331 (0.51%) | 252 (0.44%) | |
| Diseases of The Circulatory System | 1026 (1.44%) | 425 (1.49%) | 1254 (1.94%) | 985 (1.71%) | |
| Diseases of The Respiratory System | 124 (0.17%) | 52 (0.18%) | 182 (0.28%) | 150 (0.26%) | |
| Diseases of the Digestive System | 349 (0.49%) | 129 (0.45%) | 239 (0.37%) | 226 (0.39%) | |
| Diseases of The Genitourinary System | 348 (0.49%) | 97 (0.34%) | 967 (1.50%) | 488 (0.85%) | |
| Diseases of the Skin and Subcutaneous Tissue | 342 (0.48%) | 127 (0.44%) | 308 (0.48%) | 238 (0.41%) | |
| Diseases of the Musculoskeletal System and Connective Tissue | 1093 (1.54%) | 470 (1.65%) | 734 (1.13%) | 768 (1.33%) | |
| Symptoms, Signs, And Ill-Defined Conditions | 3681 (5.18%) | 1561 (5.47%) | 3608 (5.58%) | 3328 (5.77%) | |
| Injury and Poisoning | 134 (0.19%) | 47 (0.16%) | 65 (0.10%) | 76 (0.13%) | |
| Supplementary Classification of External Causes of Injury and Poisoning | 161 (0.23%) | 84 (0.29%) | 188 (0.29%) | 144 (0.25%) | |
| Supplementary Classification of Factors Influencing Health Status and Contact with Health Service | 532 (0.75%) | 166 (0.58%) | 362 (0.56%) | 292 (0.51%) | |
| Admission Motor Function | Admission FIM Motor Score | 38.13 (16.08) | 37.77 (14.84) | 34.66 (12.63) | 35.58 (12.06) |
| Admission Cognitive Function | Admission FIM Cognitive Score | 16.19 (7.72) | 18.28 (8.07) | 18.22 (7.28) | 19.72 (7.17) |
| Discharge Motor Function | Discharge FIM Motor Score | 65.21 (14.90) | 63.70 (14.49) | 57.47 (14.59) | 58.23 (13.94) |
| Discharge Cognitive Function | Discharge FIM Cognitive Score | 24.03 (6.66) | 25.29 (6.62) | 24.13 (6.60) | 25.13 (6.48) |
| Days Onset to Admission | Number of days, Mean (SD) | 20.71 (26.26) | 17.64 (24.07) | 11.87 (16.89) | 9.16 (13.91) |
| Length of Stay | Number of days, Mean (SD) | 18.21 (16.87) | 17.09 (15.16) | 15.07 (8.17) | 14.22 (6.82) |
| Year of Admission | 2002 | 4333 (6.10%) | 1774 (6.21%) | 2229 (3.45%) | 2123 (3.68%) |
| 2003 | 4245 (5.97%) | 1726 (6.05%) | 2473 (3.82%) | 2219 (3.85%) | |
| 2004 | 4158 (5.85%) | 1727 (6.05%) | 2660 (4.11%) | 2501 (4.34%) | |
| 2005 | 4721 (6.64%) | 1865 (6.53%) | 3010 (4.65%) | 2819 (4.89%) | |
| 2006 | 4808 (6.77%) | 1820 (6.38%) | 3171 (4.90%) | 2920 (5.06%) | |
| 2007 | 4655 (6.55%) | 1807 (6.33%) | 3364 (5.20%) | 3014 (5.23%) | |
| 2008 | 4888 (6.88%) | 1975 (6.92%) | 3616 (5.59%) | 3369 (5.84%) | |
| 2009 | 4550 (6.40%) | 1795 (6.29%) | 4084 (6.31%) | 3596 (6.24%) | |
| 2010 | 4395 (6.18%) | 1780 (6.24%) | 3891 (6.02%) | 3446 (5.98%) | |
| 2011 | 4282 (6.03%) | 1789 (6.27%) | 4023 (6.22%) | 3580 (6.21%) | |
| 2012 | 4419 (6.22%) | 1738 (6.09%) | 4203 (6.50%) | 3916 (6.79%) | |
| 2013 | 4291 (6.04%) | 1805 (6.32%) | 4342 (6.71%) | 3854 (6.68%) | |
| 2014 | 2839 (3.99%) | 1252 (4.39%) | 3179 (4.91%) | 2790 (4.84%) | |
| 2015 | 3543 (4.99%) | 1432 (5.02%) | 4760 (7.36%) | 4141 (7.18%) | |
| 2016 | 3596 (5.06%) | 1374 (4.81%) | 4687 (7.25%) | 4091 (7.09%) | |
| 2017 | 3790 (5.33%) | 1425 (4.99%) | 5327 (8.24%) | 4567 (7.92%) | |
| 2018 | 3553 (5.00%) | 1464 (5.13%) | 5661 (8.75%) | 4721 (8.19%) | |
| Facility Characteristics | |||||
| IRF location | Region P01 : CT, MA, ME, NH, RI, VT | 2958 (4.16%) | 1276 (4.47%) | 3383 (5.23%) | 2884 (5.00%) |
| Region P02 : NJ, NY, PR | 5881 (8.28%) | 2478 (8.68%) | 6050 (9.35%) | 5298 (9.19%) | |
| Region P03 : DE, MD, PA, VA, WV | 8926 (12.56%) | 3604 (12.62%) | 9129 (14.11%) | 8896 (15.43%) | |
| Region P04: AL, FL, GA, KT, MS, NC, TN, SC | 12207 (17.18%) | 4978 (17.44%) | 11416 (17.65%) | 10978 (19.04%) | |
| Region P05: IL, IN, MI, MN, OH, WI | 10570 (14.87%) | 4456 (15.61%) | 9778 (15.12%) | 8332 (14.45%) | |
| Region P06: AR, LA, NM, OK, TX | 7997 (11.25%) | 3249 (11.38%) | 8292 (12.82%) | 8509 (14.76%) | |
| Region P07: IA, KS, MO, NE | 4758 (6.70%) | 1900 (1900%) | 3857 (5.96%) | 3168 (5.49%) | |
| Region P08: CO, MT, ND, SD, UT, WY | 5362 (7.55%) | 2111 (7.39%) | 2868 (4.43%) | 1960 (3.40%) | |
| Region P09: AZ, CA, HI, NV | 9452 (13.30%) | 3373 (11.82%) | 8165 (12.62%) | 6513 (11.29%) | |
| Region P10: AK, ID, OR, WA | 2955 (4.16%) | 1123 (3.93%) | 1742 (2.69%) | 1129 (1.96%) | |
| IRF type | Freestanding | 25286 (35.58%) | 9737 (34.11%) | 23058 (35.65%) | 22340 (38.74%) |
| Rehab Unit in Hospital | 45780 (64.42%) | 18811 (65.89%) | 41622 (64.35%) | 35327 (61.26%) | |
| IRF accreditation | Accreditation (Joint Commission and/or CARF) | 51035 (71.81%) | 19574 (68.57%) | 37918 (58.62%) | 32444 (56.26%) |
| No accreditation | 20031 (28.19%) | 8974 (31.43%) | 26762 (41.38%) | 25223 (43.74%) | |
Acknowledgements:
Special thanks to Ziqi Zhang for assisting manuscript formatting. The data for this study were obtained and used with permission from the Uniform Data System for Medical Rehabilitation, a division of UB Foundation Activities, Inc.
Funding:
This research was funded by the National Institutes of Health, Grant #P2CHD065702, PI Ottenbacher and Grant #5U54MD012530-03; PI, Johnson.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to declare.
References
- 1.Centers for Disease Control and Prevention. TBI data and statistics. Published 2017. https://www.cdc.gov/traumaticbraininjury/data/index.html
- 2.Corrigan JD, Hammond FM. Traumatic brain injury as a chronic health condition. Archives of Physical Medicine and Rehabilitation. 2013;94(6):1199–1201. doi: 10.1016/j.apmr.2013.01.023 [DOI] [PubMed] [Google Scholar]
- 3.Walker WC, Pickett TC. Motor impairment after severe traumatic brain injury: A longitudinal multicenter study. Journal of Rehabilitation Research and Development. 2007;44(7):975. [DOI] [PubMed] [Google Scholar]
- 4.de Koning ME, Spikman JM, Coers A, Schönherr MC, van der Naalt J. Pathways of care the first year after moderate and severe traumatic brain injury—Discharge destinations and outpatient follow-up. Brain Injury. 2015;29(4):423–429. [DOI] [PubMed] [Google Scholar]
- 5.Chua KSG, Ng Y-S, Yap SGM, Bok C-W. A brief review of traumatic brain injury rehabilitation. Annals of the Academy of Medicine, Singapore. 2007;36(1):31–42. [PubMed] [Google Scholar]
- 6.Garza N, Toussi A, Wilson M, Shahlaie K, Martin R. The Increasing Age of TBI Patients at a Single Level 1 Trauma Center and the Discordance Between GCS and CT Rotterdam Scores in the Elderly. Frontiers in Neurology. 2020;11:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elkbuli A, Smith Z, Shaikh S, Hai S, McKenney M, Boneva D. Mild and moderate traumatic brain injury and gender-based critical care outcomes. World journal of surgery. Published online 2020:1–6. [DOI] [PubMed] [Google Scholar]
- 8.Gardner RC, Dams-O’Connor K, Morrissey MR, Manley GT. Geriatric traumatic brain injury: epidemiology, outcomes, knowledge gaps, and future directions. Journal of neurotrauma. 2018;35(7):889–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li W, Risacher SL, McAllister TW, Saykin AJ, Initiative ADN. Age at injury is associated with the long-term cognitive outcome of traumatic brain injuries. Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring. 2017;6:196–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan V, Mollayeva T, Ottenbacher KJ, Colantonio A. Sex-specific predictors of inpatient rehabilitation outcomes after traumatic brain injury. Archives of physical medicine and rehabilitation. 2016;97(5):772–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Graham JE, Radice-Neumann DM, Reistetter TA, Hammond FM, Dijkers M, Granger CV. Influence of sex and age on inpatient rehabilitation outcomes among older adults with traumatic brain injury. Archives of Physical Medicine and Rehabilitationa. 2010;91(1):43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Slewa-Younan S, Baguley IJ, Heriseanu R, Cameron ID, Pitsiavas V, Mudaliar Y, Nayyar V. Do men and women differ in their course following traumatic brain injury? A preliminary prospective investigation of early outcome. Brain Injury. 2008;22(2):183–191. [DOI] [PubMed] [Google Scholar]
- 13.Albrecht JS, McCunn M, Stein DM, Simoni-Wastila L, Smith GS. Sex differences in mortality following isolated traumatic brain injury among older adults. The journal of trauma and acute care surgery. 2016;81(3):486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bay E, Sikorskii A, Saint-Arnault D. Sex differences in depressive symptoms and their correlates after mild-to-moderate traumatic brain injury. Journal of Neuroscience Nursing. 2009;41(6):298–309. [DOI] [PubMed] [Google Scholar]
- 15.Despins EH, Turkstra LS, Struchen MA, Clark AN. Sex-based differences in perceived pragmatic communication ability of adults with traumatic brain injury. Archives of physical medicine and rehabilitation. 2016;97(2):S26–S32. doi: 10.1016/j.apmr.2014.06.023 [DOI] [PubMed] [Google Scholar]
- 16.Ottochian M, Salim A, Berry C, Chan LS, Wilson MT, Margulies DR. Severe traumatic brain injury: Is there a gender difference in mortality? American Journal of Surgery. 2009;197(2):155–158. doi: 10.1016/j.amjsurg.2008.09.008 [DOI] [PubMed] [Google Scholar]
- 17.Ratcliff JJ, Greenspan AI, Goldstein FC, Stringer AY, Bushnik T, Hammond FM, Novack TA, Whyte J, Wright DW. Gender and traumatic brain injury: do the sexes fare differently? Brain Injury. 2007;21(10):1023–1030. [DOI] [PubMed] [Google Scholar]
- 18.Brown SB, Colantonio A, Kim H. Gender differences in discharge destination among older adults following traumatic brain injury. Health care for women international. 2012;33(10):896–904. [DOI] [PubMed] [Google Scholar]
- 19.Schumacher R, Walder B, Delhumeau C, Müri RM. Predictors of inpatient (neuro) rehabilitation after acute care of severe traumatic brain injury: An epidemiological study. Brain Injury. 2016;30(10):1186–1193. [DOI] [PubMed] [Google Scholar]
- 20.Zarshenas S, Tam L, Colantonio A, Alavinia SM, Cullen N. Predictors of discharge destination from acute care in patients with traumatic brain injury. BMJ open. 2017;7(8):e016694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zarshenas S, Colantonio A, Alavinia SM, Jaglal S, Tam L, Cullen N. Predictors of discharge destination from acute care in patients with traumatic brain injury: a systematic review. The Journal of Head Trauma Rehabilitation. 2019;34(1):52–64. [DOI] [PubMed] [Google Scholar]
- 22.Chen AY, Zagorski B, Parsons D, Vander Laan R, Chan V, Colantonio A. Factors associated with discharge destination from acute care after acquired brain injury in Ontario, Canada. BMC Neurology. 2012;12:16. doi: 10.1186/1471-2377-12-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cuthbert JP, Corrigan JD, Harrison-Felix C, Coronado V, Dijkers MP, Heinemann AW, Whiteneck GG. Factors that predict acute hospitalization discharge disposition for adults with moderate to severe traumatic brain injury. Archives of Physical Medicine and Rehabilitation. 2011;92(5):721–730.e3. doi: 10.1016/j.apmr.2010.12.023 [DOI] [PubMed] [Google Scholar]
- 24.Eum RS, Seel RT, Goldstein R, Brown AW, Watanabe TK, Zasler ND, Roth EJ, Zafonte RD, Glenn MB. Predicting institutionalization after traumatic brain injury inpatient rehabilitation. Journal of neurotrauma. 2015;32(4):280–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Medicare & Medicaid Services (CMS), Medicare Shared Saving Program. Quality Measure Benchmarks for the 2018 and 2019 Reporting Years. Published online 2018. https://www.cms.gov/Medicare/…/2018-and-2019-quality-benchmarks-guidance.pdf [Google Scholar]
- 26.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS medicine. 2007;4(10):e296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Uniform Data System for Medical Rehabilitation. About the UDSPRO system. Published 2017. http://www.udsmr.org/ [Google Scholar]
- 28.Centers for Medicare & MedicaidServices. The Inpatient Rehabilitation Facility-Patient Assessment Instrument (IRF-PAI) Training Manual. Baltimore, MD: Centers for Medicare & Medicaid Services (CMS). Published online 2012. [Google Scholar]
- 29.Centers for Medicare & Medicaid Services (CMS) HHS. Medicare program: Inpatient rehabilitation facility prospective payment system for federal fiscal year 2010. Final rule. Federal register. 2009;74(151):39761. [PubMed] [Google Scholar]
- 30.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Archives of physical medicine and rehabilitation. 1996;77(12):1226–1232. [DOI] [PubMed] [Google Scholar]
- 31.SAS Institute. SAS 9.4 Output Delivery System: User’s Guide. SAS Institute; 2014. [Google Scholar]
- 32.Oyesanya TO, Ward EC. Mental health in women with traumatic brain injury: A systematic review on depression and hope. Health Care for Women International. 2015;37(1):45–74. doi: 10.1080/07399332.2015.1005307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kersey J, Terhorst L, Wu C-Y, Skidmore E. A scoping review of predictors of community integration following traumatic brain injury: a search for meaningful associations. The Journal of head trauma rehabilitation. 2019;34(4):E32–E41. [DOI] [PubMed] [Google Scholar]
- 34.Oyesanya TO. Selection of discharge destination for patients with moderate-to-severe traumatic brain injury. Brain Injury. 2020;34(9):1222–1228. doi: 10.1080/02699052.2020.1797172 [DOI] [PubMed] [Google Scholar]
- 35.Gardizi E, Hanks RA, Millis SR, Figueroa MJ. Comorbidity and insurance as predictors of disability after traumatic brain injury. Archives of physical medicine and rehabilitation. 2014;95(12):2396–2401. [DOI] [PubMed] [Google Scholar]
- 36.Schiraldi M, Patil CG, Mukherjee D, Ugiliweneza B, Nuño M, Lad SP, Boakye M. Effect of insurance and racial disparities on outcomes in traumatic brain injury. Journal of Neurological Surgery Part A: Central European Neurosurgery. 2015;76(03):224–232. [DOI] [PubMed] [Google Scholar]
- 37.Colantonio A, Escobar MD, Chipman M, McLellan B, Austin PC, Mirabella G, Ratcliff G. Predictors of postacute mortality following traumatic brain injury in a seriously injured population. Journal of Trauma and Acute Care Surgery. 2008;64(4):876–882. [DOI] [PubMed] [Google Scholar]
- 38.Asemota AO, George BP, Cumpsty-Fowler CJ, Haider AH, Schneider EB. Race and insurance disparities in discharge to rehabilitation for patients with traumatic brain injury. Journal of Neurotrauma. 2013;30(24):2057–2065. doi: 10.1089/neu.2013.3091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McQuistion K, Zens T, Jung HS, Beems M, Leverson G, Liepert A, Scarborough J, Agarwal S. Insurance status and race affect treatment and outcome of traumatic brain injury. Journal of surgical research. 2016;205(2):261–271. [DOI] [PubMed] [Google Scholar]
- 40.Kumara AS, Samaratunge R. Health insurance ownership and its impact on healthcare utilization. International Journal of Social Economics. Published online 2019. [Google Scholar]