Abstract
Objective:
Probing targeted, mechanism-based interventions is the next generation of treatment innovation. Biased threat labeling of ambiguous face emotions (interpretation bias) is a potential behavioral treatment target for anger, aggression, and irritability. Changing biases in face-emotion labeling may improve irritability-related outcomes. Here, we report the first randomized, double-blind, placebo-controlled targeted trial (RCT) of interpretation bias training (IBT) in youth with chronic, severe irritability.
Method:
Patients with current Disruptive Mood Dysregulation Disorder (DMDD; N=44) were randomly assigned to complete four sessions of active (n=22) or sham (n=22) computerized IBT training within a one-week period. The first and last trainings were completed onsite, and two trainings were completed at home. We examined the effects of active IBT on labeling bias, primary outcome measures of irritability, and secondary outcome measures of anxiety, depression, and functional impairment. Follow-up assessments were completed immediately after the intervention and two weeks following the intervention.
Results:
We found that active IBT engaged the behavioral target in the active relative to the sham condition, shown by a significant shift toward labeling ambiguous faces as happy. However, there was no consistent clinical improvement in active IBT relative to the sham condition, immediately after, or two weeks following training in either primary or secondary outcome measures.
Conclusion:
While this RCT of IBT in youth with DMDD engaged the proposed behavioral target, there was no statistically significant improvement on clinical outcome. Identifying and changing behavioral targets is a first step in novel treatment development; these results have broader implications for targeted-based intervention development.
Clinical trial registration information:
Psychological Treatments for Youth With Severe Irritability; https://clinicaltrials.gov/; NCT02531893.
Keywords: RCT, face-emotion labeling, cognitive bias, children and adolescents, irritability
Introduction
Identifying and changing targeted, mechanism-based deficits has been proposed as the next generation of treatment innovation 1,2. Irritability is a common pediatric psychiatric problem 3,4 with very few non-pharmacological, mechanism-based, empirically supported treatments 5. Recent work reveals a key behavioral target that provides a promising avenue for treatment. Specifically, irritability and its related constructs are associated with a form of biased face-emotion labeling 6-10, which can be altered through cognitive training 11,12. In the present study, we report the first randomized controlled trial (RCT) of a face-emotion cognitive training as a potential targeted treatment for pediatric irritability.
A number of psychosocial, evidence-based interventions exist to treat externalizing behaviors such as aggression, oppositionality and impulsivity across various pediatric diagnoses. Parent Management Training 13, Cognitive Behavioral Therapy 14,15, Dialectical Behavior Therapy 16 and Interpersonal Therapy 17, either address forms of anger and temper outbursts characteristic of DMDD, or have been adapted to include these symptoms and behaviors as targets. While these interventions have shown some efficacy in treating anger and behavioral outbursts 18, they can be costly and time-intensive; here we test a computer-delivered training program to complement existing efforts to develop comprehensive psychosocial and pharmacological options.
Hostile interpretation bias (HIB), the proneness to interpreting ambiguous social cues as threatening, is thought to enhance threat salience, increase anger, and motivate reactive aggression 6,8,19-23. Given this potentially causal role for threat biases in anger and externalizing behaviors, research on face-emotion labeling may provide an avenue for novel therapies 24. Training protocols have been devised to investigate whether these biases can be modified and whether doing so decreases anger and aggression. Specifically, interpretation bias training, “IBT”, is a computer-based training protocol aiming to change participants’ labeling of ambiguous face-emotions towards more benign (“happy”) interpretations.
Several studies have examined the effects of computerized cognitive training programs targeting hostile attributions and interpretations in youth with internalizing and externalizing difficulties 21,25-28. An open label trial established feasibility and acceptability of IBT for youth with impairing irritability i.e., a lifetime diagnosis of DMDD 6. An early study found that IBT in youth at risk of conduct problems resulted in decreases in self- and blinded staff-rated anger and aggression 21. Change in HIB in the experimental condition was related to change in state anger, lending support to the hypothesized mechanism. Similarly, an open label trial in youth with irritability showed decreased symptoms alongside change in HIB and a relationship between cognitive and symptom change. A small number of more recent studies have failed to find clinical improvement for social anxiety, anger, or aggression despite target engagement, i.e., a shift towards labeling ambiguous face-emotions as happy 27,29-31. Hence, across studies, active IBT successfully shifts labeling of face-emotions through personalized corrective feedback. Training effects appear to be sustained beyond training sessions across samples. Findings regarding the effects of this shift on symptoms and behavior are less consistent, but studies especially in developmental populations are limited, with divergent samples and outcome measures.
Many new treatments are ineffective or suboptimal, which has led researchers to propose the “fast-fail approach” 1 to accelerate the pace of therapeutic discovery. In a fast-fail approach, a small trial is performed with an identified treatment target to establish proof of mechanism thought to mediate the clinical effect. Both target engagement and predefined efficacy, i.e., evidence for the specific therapeutic target effect rather than non-specific improvements, are required before a larger, definitive trial is conducted. If either efficacy or target are not supported, the fast-fail trial should provide information for treatment development. The fast-fail approach was developed for small-scale studies of medications 32,33; this approach has yet to be applied systematically to cognitive training. Given research linking malleable forms of biased face-emotion labeling to irritability, here we apply this fast-fail approach to a computer-based training. Such an application is particularly needed in youth, given concerns about pediatric psychopharmacology, especially potential endocrine and metabolic effects in certain classes of psychotropic medications 34, and poorly understood effects on the developing brain.
In summary, prior data lay the groundwork for an RCT targeting biased face-emotion labeling to change irritability. Here, we employ a fast-fail approach via an RCT in youth with chronic, severe irritability; we test the hypothesis that active relative to sham cognitive training produces greater changes in biased labeling of ambiguous face-emotions and decreases symptoms of irritability.
Method
Sample
The study was conducted at the National Institutes of Health with active enrollment from November 2015 to December 2018. Study procedures were approved by the National Institute of Mental Health (NIMH) Institutional Review Board (IRB). This trial was registered under NCT02531893 on clinicaltrials.gov on August 25, 2015 (https://clinicaltrials.gov/ct2/show/record/NCT02531893), and the proposed study protocol for this trial is published 35. Participants were recruited nationwide via IRB-approved mailings and websites.
Patients were eligible if they met full, current Disruptive Mood Dysregulation Disorder (DMDD) criteria as assessed by a structured clinical interview Kiddie-Schedule for Affective Disorders and Schizophrenia Present and Lifetime Version; K-SADS-PL; 36 including a supplementary module to assess the presence of DMDD 37. Additionally, to be eligible to enroll, patients’ response to their current community treatment was assessed by the research team to be no more than minimal. This was formally operationalized by a CGI-S score (1-month version) of ≥3 focusing on DMDD symptoms 38. Parents and youth provided informed consent and assent, respectively. Forty-four patients were enrolled in the study (see Table 1 and 2 for demographics and clinical characteristics of the sample and Table S1, available online, for additional measures of anxiety, depression, and functional impairment by training group). Participants were randomized to receive four IBT training sessions (active vs. sham training) in a double-blind design over four days. Participants completed clinician- and child-report ratings pre- and post-training and two weeks following training. The endpoint for the primary outcome measures was the first follow-up visit. See Figure S1, available online, for a CONSORT diagram detailing the flow of participants through the study as well as Supplement 1, available online, for additional information on recruitment, eligibility criteria and randomization procedures.
Table 1.
Participant Characteristics N=44
| DMDD | |
|---|---|
| N=44 | |
| Age (years) M (SD) | 11.96 (2.11) |
| Sex % male | 57% |
| Race N (%) | |
| Black or African American | 1 (2) |
| White | 39 (89) |
| Multiple races | 3 (7) |
| Unknown | 1 (2) |
| Ethnicity N (%) | |
| Latino or Hispanic | 6 (14) |
| Unknown | 1 (2) |
| IQ M (SD) | 111.4 (12.5) |
| K-SADS diagnoses, current N (%) | |
| Any anxietya | 27 (61) |
| ADHD | 32 (73) |
| DMDD | 44 (100) |
| MDD | 0 (0) |
| Medicationsb N (%) | |
| Antidepressants | 20 (46) |
| Antipsychotics | 10 (23) |
| Antiepileptic | 6 (14) |
| Stimulants | 24 (55) |
| Psychotherapyc N (%) | |
| Individual therapy | 17 (39) |
| Group therapy | 1 (2) |
Note: ADHD = attention-deficit/hyperactivity disorder; DMDD = disruptive mood dysregulation disorder; K-SADS = Kiddie Schedule for Affective Disorders and Schizophrenia for School-Aged Children; MDD = major depressive disorder
Any anxiety disorder includes generalized anxiety disorder, social phobia, specific phobia, and/or separation anxiety disorder
Data was not available from 2 participants.
Regularity varied from weekly to monthly.
Table 2.
Pretraining Demographic and Clinical Characteristics by Training Group
| Active (n=22) | Sham (n=22) | |
|---|---|---|
| Age (years) | 11.48 (2.05) | 12.44 (2.11) |
| Sex (% male) | 16 (72.73) | 9 (40.91) |
| IQ | 113.91 (11.64) | 108.95 (13.19) |
| CL-ARI | 58.33 (11.15) | 61.62 (13.95) |
| ARI-C | 3.05 (2.32) | 4.64 (2.77) |
| ARI-P | 8.73 (1.88) | 8.05 (3.05) |
Note: n = 1 missing Clinician Affective Reactivity Index (CL-ARI). ARI-CL = Affective Reactivity Index-Clinician; ARI-C = Affective Reactivity Index-Child; ARI-P = Affective Reactivity Index-Parent.
Measures
Primary and secondary outcome measures were completed at baseline, post-training, and follow-up. Ratings were administered by trained masters- or doctoral-level clinicians. Primary outcome measures assessed changes in irritability using the Clinician Affective Reactivity Index (CL-ARI) 39, Clinical Global Impressions Scale-Improvement for DMDD (CGI-I) 38, and parent- and child-report Affective Reactivity Index (ARI-C/P) 40. Secondary outcome measures were ratings of anxiety, rated by clinicians (Pediatric Anxiety Rating Scale, PARS 41) and the parent/child (Screen for Childhood Anxiety Related Emotional Disorders-parent/child, SCARED 42), as well as measures of depression assessed via clinician- (Children’s Depression Rating Scale, CDRS 43) and child-report (Children’s Depression Inventory, CDI 44).
Additionally, clinician-rated measures of severity (Clinical Global Impressions Scale-Severity for DMDD, CGI-S 45) and impairment (Children’s Global Assessment Scale, CGAS 46) were collected. For additional measures assessed at baseline see Table S2 and Supplement 2, available online.
Interpretation bias assessment and training
The Interpretation Bias Task (IBT Task; see Figure 2 for task schematic) estimates and trains happy-angry interpretations of face-emotions 47. The stimulus set for assessment and training consisted of 15 face-emotion pictures linearly morphed at equal intervals from unambiguously happy to unambiguously angry facial expressions, created from a happy and angry composite face from the Karolinska Directed Emotional Faces database 48. Stimuli were first generated by Penton-Voak and colleagues 21 using established procedures designed to maintain relevant features and textures of facial expressions 49.
Figure 2. Balance Point by Training Group and Session.
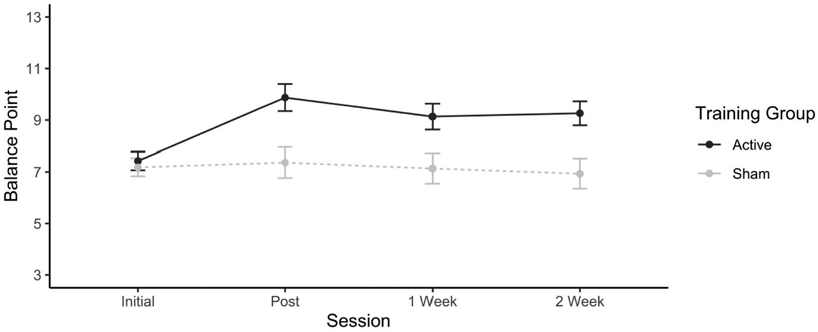
Note: Error bars show standard error.
Assessment Task. Each trial consisted of a fixation cross (1500-2500 ms), face presentation (150 ms), visual noise mask (250 ms), and response prompt (no time limit). Participants entered a forced-choice response of “happy” or “angry” via keyboard button press. Face-morphs were presented in random order. The Assessment Task measured participants’ “balance point” (i.e., the morph along the continuum at which the participant shifts his or her judgment from predominantly happy to predominately angry). The balance point is estimated as the proportion of happy responses to total responses multiplied by 15 during the 45 trials of the assessment task. A low balance point indexes a hostile interpretation bias, a balance point of 8 indicates no bias (middle of morphs 1 to 15). Assessment tasks were completed before and after each training and at the two follow-up assessments.
Training Task. The training task was identical to the assessment task, but feedback was provided to the participant on every trial after the participant’s response. Feedback consists of a message saying “Right!/Wrong!”. In sham IBT training, feedback was based on the participant’s balance point, as measured using the assessment task before training (i.e., the feedback is consistent with the participant’s pre-training interpretation bias). In the active training, feedback was designed to shift the participant’s balance point two face-morphs along the face-morph continuum, so that two ambiguous morphs that were rated angry at pre-training would be rated as happy post-training. The maximum training threshold was face-morph 12, as positive feedback associated with the three most extreme angry morphs was always congruent with an angry interpretation. There were 6 training blocks of 30 trials each.
Sample size and statistical analysis
Power calculations were based on Stoddard and colleagues (2016) who completed an open, uncontrolled arm pilot trial in youth with DMDD which found a large effect of IBT on outcomes (d=1.2 for CGI-I for symptoms of DMDD). However, randomized, controlled designs of similar computer-based approaches have reported more moderate effect sizes 50, which likely relates to the presence of a control condition in these studies. Thus, we adjusted our expected effect size to d=0.9 for the primary outcome. At an accrual target of 20 per group and an alpha of 5%, this study has 85% power to detect an effect of this size. Dropouts were replaced for a minimum N=40 of participants who completed the trial. Data were analyzed according to the intention-to-treat (ITT) principle and included all patients who underwent randomization. One participant randomized to active IBT withdrew assent after the first training session. For this participant, where baseline scores were available, these were carried forward and imputed at all time points for any corresponding outcome measures. Interpretation bias and outcome measures were analyzed as a function of training (active vs. sham) and session (pre-training, post-training, one week and two weeks follow-up) using a linear-mixed effects model with participant as a random factor and group and session as a fixed factor. Missing datapoints were rare and not imputed (<2.5%, <1.5%, and <5% of primary outcome, secondary outcome, and interpretation bias measures, respectively).
In secondary analyses, we used Spearman correlations to examine i) associations between pre-training balance point and baseline measures of irritability and ii) associations between shifts in balance point pre- to post-training and irritability-related clinical improvement (CGI-I) or reductions in irritability at the primary outcome time point (i.e., 1-week post-training). Additionally, we used a mediation analysis to test whether change in balance point from baseline to post-training (i.e., first pre-training assessment at day 1 to post-training assessment at day 4) mediated clinical improvement (CGI-I) at the primary outcome time point by training group. All statistical analyses were performed using R statistical software (Version 3.5). The package lme4 was used for linear mixed-effects modeling 51 and lavaan for mediation analyses 52.
Results
Balance point (interpretation bias)
The Session-by-Training interaction was significant (F(3,121.92)=6.33, p<.001, see Figure 2). As expected, there was no difference in mean balance point between IBT conditions pre-training (Active: b[SE]=7.42[0.50], Sham: b[SE]=7.18[0.50], t(41.98)=0.49, p=0.63, d=0.15). However, at post-training assessment, patients in the active IBT condition had a significantly higher balance point (i.e., more happy judgements on ambiguous morphs) compared to the sham condition by b[95%CI] =2.51[0.90, 4.12] face-morphs (t(40.57)=3.16, p=0.003, d=0.96). The active IBT group also had a significantly higher mean balance point at both the 1-week (by b[95%CI] =1.99[0.44, 3.56] face-morphs, t(40.31)=2.59, p=0.01, d=0.79) and the 2-week follow-up (by b[95%CI] =2.33[0.82, 3.83] face-morphs, t(38.17)=3.12, p=0.003, d=0.96), indicating maintenance of balance point change post training completion. Sham training balance points remained stable across all four training sessions (ICC[2,1]=.72).
Primary outcome measures
The main effect of Training and the Session-by-Training interaction term were not significant for clinician-rated improvement scores (CGI-I scores all F<0.90, ps>.34; see Figure 3). For both training groups, CGI-I scores post-training were in the “slightly improved” range (Active: M[SE]=3.95[0.32], Sham: M[SE]=3.67[0.32], t(38.04)=0.60, p=.55, d=.19). CGI-I scores at 1- and 2-weeks post-training were similarly in the “slightly improved/improved” range for both training groups (1-week follow-up: Active: M[SE]=3.71[0.32], Sham: M[SE]=3.52[0.32], t(36.92)=0.44, p=.66, d=.14; 2-week follow-up: Active: M[SE]=3.95[0.32], Sham: M[SE]=3.48[0.32], t(39.99)=1.10, p=.28 d=.34).
Figure 3. Irritability Outcome Measures.

Note: (A) Clinician- and (B) parent-rated irritability by group and session. (C) Improvement scores relative to baseline by group (active vs sham interpretation bias training [IBT]) and session (post-training and 1- and 2-weeks following training; 5 = No Improvement). Right panel: Error bars show standard error.
The Session-by-Training interaction was not significant for either clinician- or parent-rated irritability (ARI-CL: F(3,123)=0.67, p=.55; ARI-P: F(3,122.92)=1.11, p=.35). Training was associated with a reduction in clinician- and parent-reported irritability symptoms across both training groups (ARI-CL: F(3,123)=15.94, p<.001; ARI-P: F(3,122.92)=7.06, p<.001). Pre-training ratings of clinician- and parent-reported irritability symptoms were ARI-CL M[SE]=60.01[1.92], and ARI-P M[SE]=8.39[.29]. Ratings reduced significantly, on average ARI-CL: M[95%CI] =16.83[11.61, 22.04] and ARI-P: M[95%CI] = 2.11[1.21, 3.02] points respectively by 1-week post training (ARI-CL: t(42)=6.52, p<0.001, d=.93; ARI-P: t(43)=4.70, p<0.001, d=.74). Child-rated irritability showed a significant Training-by-Time interaction (F(3,123.03)=3.18, p=.03). Post-hoc analyses indicated marginally significant decreases in child-rated irritability over time in the sham condition (F(3,61)=2.72, p=.05), but not in the active IBT condition (F(3,62)=1.40, p=.25). However, further analyses showed that training group differences in child-rated irritability were only significant at baseline, with marginally higher irritability reported by the sham group (baseline: t(40.7)=2.07, p=.05, d=.62).
Secondary outcome measures
None of the secondary outcome measures showed improvements specific to the active IBT training group, see Supplement 3, available online, for detailed analyses of secondary measures.
Associations between balance point and outcome
We examined associations between pre-training balance point and clinician-, parent- and child-report irritability. We did not find significant correlations between baseline irritability measures and pre-training balance point (all rs<−.22, ps>.15) or shifts in balance point and irritability reductions (all rs<−.08, ps>.60) or irritability-related clinical improvement (r=.05, p=.73). An additional mediation further investigated the relations between target engagement and outcome. The indirect effect of balance point change as a mediator in the relation between training group status and irritability-related clinical improvement was not significant (z=−.57, p=.57).
Discussion
This RCT of computer-based IBT engaged the behavioral target in the active relative to the sham condition, shown by a significant shift toward labeling ambiguous faces as happy; however, active IBT produced no detectable clinical improvement over and above improvement in the sham condition. Thus, while the target was engaged, and the effect size of this change was large (d=.96 after 4 days of training, d=.79 1-week post training), there was no consistent clinical improvement associated with target engagement.
Fast-fail approaches aim to accelerate the pace of discovery via small scale, iterative, rigorous testing of target-based treatments 32,33. The negative result is consistent with the mixed findings in prior work on IBT. While the sample size in this trial was small, the change in the behavioral target was large; considering this change in the behavioral target, we would expect differential clinical improvement or associations between target engagement (change in labeling) and improvement even with this modest sample size. More consistent efficacy might accrue following refinements in specific recruitment features by first identifying individuals who might most likely benefit from face-emotion labelling training.
IBT is a basic category learning task, where both sham and active IBT train towards reliable judgments of facial affect at a specific target balance point, or category boundary. At this boundary, participants are trained to shift from one response abruptly and reliably to another. Without an active comparator, for example, training individuals on nonsocial features of objects, it is not clear whether the general improvement across arms is attributable to category learning on facial affect or common reasons for improvement participation in clinical trials, such as regression to the mean or demand effects.
The study suggests that behaviorally training a shift in balance point does not lead to clinical improvement in youth with irritability post-training or within the two weeks follow-up period. It is possible that shifts in face-emotion labeling need longer to consolidate before impacting symptom reports 53. Findings support the need to integrate multiple features (i.e., behavioral deficits, neural correlates, phenotypic specificity) when developing novel targets. Behavioral deficits alone may not be sufficient as a treatment target as there may be multiple neural pathways to a common behavioral deficit. Lessons may be learned from RCTs of attention bias modification training (ABMT) as a treatment for anxiety. Similar to attentional processes 54, biases in interpretation related to anger appear only moderate in size 22, based on the very limited data available. Thus, a significant proportion of patients may present without this bias toward ambiguous social cues. Future work could select participants based on their initial bias and ability to incorporate trial-by-trial feedback to update their categorical labeling. Selecting participants based on these features may create a more homogenous treatment group more likely to benefit from this targeted cognitive training.
Several limitations need to be noted. First, the RCT is underpowered to detect small effects or examine efficacy in subgroups of youth with more specific characteristics (e.g., current anxiety disorder, specific age range). Second, we used the same face-emotion stimulus set across all training units; a composite face averaged across different male actors with different apparent races and features. Hence, youths were trained on specific face-stimuli, rather than on face-emotions more generally. However, recent work has provided first evidence that training effects on specific faces generalize to identities and facial configurations beyond those included in the training 55. Future work should use several different sets of face-emotion stimuli, which may reduce fatigue, and increase transfer to new social material. Third, while community treatment was kept stable throughout the duration of the RCT, participants had a variety of concurrent treatments including psychotropic medication.
Results from this and other fast-fail RCTs might discourage further investments in targeting of behavioral biased face processing. However, IBT involves complex processes such as attention orienting, updating, and decision-making, and each of these parameters could be further explored; post-hoc analyses on data from this report may be informative. Work on other computer-based interventions suggests that it is important to fully couple behavioral dysfunction with specific neural targets 54.
Aberrant threat interpretation has been suggested as a cognitive pathway to emotional problems across internalizing and externalizing phenotypes. An RCT of IBT in youth with DMDD found no significant differential improvement on clinical outcome.
Supplementary Material
Figure 1. Interpretation Bias Training (IBT).
Note: (A) Illustration of a training trial. (B) Active IBT was designed to shift the balance point two morphs along the continuum of face-morphs. Hence, by the end of the training session, participants were expected to rate two ambiguous morphs as happy that were rated angry pre-treatment. Sham IBT provided feedback consistent with the pre-training balance point.
Acknowledgments
This research was supported by the Intramural Research Program of the National Institute of Mental Health (NIMH), National Institutes of Health (NIH; ZIAMH002778-17 and ZIAMH002786-15) and was conducted under NIH Clinical Study Protocols 15-M-0182 and 02-M-0021 (ClinicalTrials.gov ID: NCT02531893 and NCT00025935). J.S. was supported by a grant from NIH, NIMH, (K23MH113731) and the Pediatric Mental Health Institute at Children’s Hospital Colorado and the Division of Child and Adolescent Psychiatry, Department of Psychiatry, University of Colorado School of Medicine. The funding source was not involved in study design; the collection, analysis, and interpretation of data; writing of the report; and the decision to submit the article for publication. M.M. and I.P.-V. are supported by the National Institute for Health Research (NIHR) Biomedical Research Centre at University Hospitals Bristol National Health Service (NHS) Foundation Trust and the University of Bristol. The views expressed in this publication are those of the author(s) and not necessarily those of NHS, NIHR, or the Department of Health and Social Care.
The authors thank the clinicians, patients, and their families that contributed to this research.
Footnotes
Disclosure: Dr. Haller has received grant support through a Brain and Behavior Research Foundation (BBRF) Young Investigator Award. Dr. Stoddard has received grant or research support from NIMH. He has served as a DSMB committee member: Threat Interpretation Bias as Cognitive Marker and Treatment Target in Pediatric Anxiety (R61 Phase). Drs. Penton-Voak and Munafò are co-directors of Jericoe Ltd., a company that licenses software for the assessment and modification of emotion recognition. Dr. Bar-Haim has received grant or research support from the Israel Science Foundation and the US Department of Defense. Dr. Brotman has served as a principal investigator (PI) on a Bench-to-Bedside grant from NIH. Drs. Kircanski and Towbin, Mr. Botz-Zapp, and Mss. Clayton, MacGillivray, Perhamus, and Stiles have reported no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Simone P. Haller, National Institute of Mental Health, and National Institutes of Health, Bethesda, Maryland..
Joel Stoddard, University of Colorado, Anschutz Medical Campus, Aurora..
Christian Botz-Zapp, National Institute of Mental Health, and National Institutes of Health, Bethesda, Maryland..
Michal Clayton, National Institute of Mental Health, and National Institutes of Health, Bethesda, Maryland..
Caroline MacGillivray, National Institute of Mental Health, and National Institutes of Health, Bethesda, Maryland..
Gretchen Perhamus, National Institute of Mental Health, and National Institutes of Health, Bethesda, Maryland..
Kelsey Stiles, National Institute of Mental Health, and National Institutes of Health, Bethesda, Maryland..
Katharina Kircanski, National Institute of Mental Health, and National Institutes of Health, Bethesda, Maryland..
Ian S. Penton-Voak, University of Bristol, United Kingdom.
Yair Bar-Haim, Tel Aviv University, Israel..
Marcus Munafò, University of Bristol, United Kingdom.
Kenneth E. Towbin, National Institute of Mental Health, and National Institutes of Health, Bethesda, Maryland..
Melissa A. Brotman, National Institute of Mental Health, and National Institutes of Health, Bethesda, Maryland..
References
- 1.Insel. The NIMH experimental medicine initiative. World Psychiatry. 2015;14(2):151–153. 10.1002/wps.20227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hyman SE. Revolution stalled. Sci Transl Med. 2012;4(155):155cm111. 10.1126/scitranslmed.3003142 [DOI] [PubMed] [Google Scholar]
- 3.Peterson BS, Zhang H, Santa Lucia R, King RA, Lewis MJJotAAoC, Psychiatry A. Risk factors for presenting problems in child psychiatric emergencies. 1996;35(9):1162–1173 [DOI] [PubMed] [Google Scholar]
- 4.Collishaw S, Maughan B, Natarajan L, Pickles A. Trends in adolescent emotional problems in England: a comparison of two national cohorts twenty years apart. J Child Psychol Psychiatry. 2010;51(8):885–894. 10.1111/j.1469-7610.2010.02252.x [DOI] [PubMed] [Google Scholar]
- 5.Brotman MA, Kircanski K, Stringaris A, Pine DS, Leibenluft EJAJoP. Irritability in youths: a translational model. 2017;174(6):520–532 [DOI] [PubMed] [Google Scholar]
- 6.Stoddard J, Sharif-Askary B, Harkins EA, et al. An Open Pilot Study of Training Hostile Interpretation Bias to Treat Disruptive Mood Dysregulation Disorder. J Child Adolesc Psychopharmacol. 2016;26(1):49–57. 10.1089/cap.2015.0100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crick NR, Dodge KA. A review and reformulation of social information-processing mechanisms in children's social adjustment. Psychological bulletin. 1994;115(1):74 [Google Scholar]
- 8.Crick NR, Dodge KA. Social information-processing mechanisms in reactive and proactive aggression. Child Dev. 1996;67(3):993–1002. https://www.ncbi.nlm.nih.gov/pubmed/8706540. Published 1996/June/01 [PubMed] [Google Scholar]
- 9.Hall CW. Self-reported aggression and the perception of anger in facial expression photos. J Psychol. 2006;140(3):255–267. 10.3200/JRLP.140.3.255-267 [DOI] [PubMed] [Google Scholar]
- 10.Wilkowski BM, Robinson MD. When Aggressive Individuals See the World More Accurately: The Case of Perceptual Sensitivity to Subtle Facial Expressions of Anger. Personality and Social Psychology Bulletin. 2012;38(4):540–553. 10.1177/0146167211430233 [DOI] [PubMed] [Google Scholar]
- 11.MacLeod C, Mathews A. Cognitive bias modification approaches to anxiety. Annu Rev Clin Psychol. 2012;8:189–217. 10.1146/annurev-clinpsy-032511-143052 [DOI] [PubMed] [Google Scholar]
- 12.Hallion LS, Ruscio AM. A meta-analysis of the effect of cognitive bias modification on anxiety and depression. Psychol Bull. 2011;137(6):940–958. 10.1037/a0024355 [DOI] [PubMed] [Google Scholar]
- 13.Comer JS, Chow C, Chan PT, Cooper-Vince C, Wilson LAS. Psychosocial Treatment Efficacy for Disruptive Behavior Problems in Very Young Children: A Meta-Analytic Examination. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52(1):26–36. 10.1016/j.jaac.2012.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sukhodolsky DG, Kassinove H, Gorman BS. Cognitive-behavioral therapy for anger in children and adolescents: A meta-analysis. Aggression and Violent Behavior. 2004;9(3):247–269.DOI 10.1016/j.avb.2003.08.005 [DOI] [Google Scholar]
- 15.Evans SC, Weisz JR, Carvalho AC, et al. Effects of standard and modular psychotherapies in the treatment of youth with severe irritability. J Consult Clin Psychol. 2020;88(3):255–268. 10.1037/ccp0000456 [DOI] [PubMed] [Google Scholar]
- 16.Perepletchikova F, Nathanson D, Axelrod SR, et al. Randomized Clinical Trial of Dialectical Behavior Therapy for Preadolescent Children With Disruptive Mood Dysregulation Disorder: Feasibility and Outcomes. J Am Acad Child Adolesc Psychiatry. 2017;56(10):832–840. 10.1016/j.jaac.2017.07.789 [DOI] [PubMed] [Google Scholar]
- 17.Miller L, Hlastala SA, Mufson L, Leibenluft E, Yenokyan G, Riddle M. Interpersonal psychotherapy for mood and behavior dysregulation: Pilot randomized trial. Depress Anxiety. 2018;35(6):574–582. 10.1002/da.22761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaminski JW, Claussen AH. Evidence Base Update for Psychosocial Treatments for Disruptive Behaviors in Children. J Clin Child Adolesc Psychol. 2017;46(4):477–499. 10.1080/15374416.2017.1310044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilkowski BM, Robinson MD. The anatomy of anger: an integrative cognitive model of trait anger and reactive aggression. J Pers. 2010;78(1):9–38. 10.1111/j.1467-6494.2009.00607.x [DOI] [PubMed] [Google Scholar]
- 20.Perhamus GR, Ostrov JM. Emotions and Cognitions in Early Childhood Aggression: the Role of Irritability and Hostile Attribution Biases. Res Child Adolesc Psychopathol. 2021;49(1):63–75. 10.1007/s10802-020-00707-7 [DOI] [PubMed] [Google Scholar]
- 21.Penton-Voak IS, Thomas J, Gage SH, McMurran M, McDonald S, Munafo MR. Increasing recognition of happiness in ambiguous facial expressions reduces anger and aggressive behavior. Psychol Sci. 2013;24(5):688–697. 10.1177/0956797612459657 [DOI] [PubMed] [Google Scholar]
- 22.Mellentin AI, Dervisevic A, Stenager E, Pilegaard M, Kirk U. Seeing enemies? A systematic review of anger bias in the perception of facial expressions among anger-prone and aggressive populations. Aggression and violent behavior. 2015;25:373–383 [Google Scholar]
- 23.Deveney CM, Stoddard J, Evans R, Chavez G, Harney M, Wulff R. On Defining Irritability and its Relationship to Affective Traits and Social Interpretations. Pers Individ Dif. 2019;144:61–67. 10.1016/j.paid.2019.02.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Penton-Voak IS, Munafò MR, Looi CYJCdips. Biased facial-emotion perception in mental health disorders: a possible target for psychological intervention? 2017;26(3):294–301 [Google Scholar]
- 25.Vassilopoulos SP, Brouzos A, Andreou E. A Multi-Session Attribution Modification Program for Children with Aggressive Behaviour: Changes in Attributions, Emotional Reaction Estimates, and Self-Reported Aggression. Behav Cogn Psychother. 2015;43(5):538–548. 10.1017/S1352465814000149 [DOI] [PubMed] [Google Scholar]
- 26.Krebs G, Pile V, Grant S, Degli Esposti M, Montgomery P, Lau JYF. Research Review: Cognitive bias modification of interpretations in youth and its effect on anxiety: a meta-analysis. J Child Psychol Psychiatry. 2018;59(8):831–844. 10.1111/jcpp.12809 [DOI] [PubMed] [Google Scholar]
- 27.Hiemstra W, De Castro BO, Thomaes S. Reducing Aggressive Children's Hostile Attributions: A Cognitive Bias Modification Procedure. Cognitive Therapy and Research. 2019;43(2):387–398. 10.1007/s10608-018-9958-x [DOI] [Google Scholar]
- 28.Menne-Lothmann C, Viechtbauer W, Höhn P, et al. How to boost positive interpretations? A meta-analysis of the effectiveness of cognitive bias modification for interpretation. PloS one. 2014;9(6):e100925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Penton-Voak IS, Adams S, Button KS, et al. Emotional recognition training modifies neural response to emotional faces but does not improve mood in healthy volunteers with high levels of depressive symptoms. bioRxiv. 2018:335042. [DOI] [PubMed] [Google Scholar]
- 30.Kuin NC, Masthoff ED, Nunnink VN, Munafò MR, Penton-Voak IS. Changing perception: A randomized controlled trial of emotion recognition training to reduce anger and aggression in violent offenders. Psychology of Violence. 2019 [Google Scholar]
- 31.Rawdon C, Murphy D, Motyer G, Munafo MR, Penton-Voak I, Fitzgerald A. An investigation of emotion recognition training to reduce symptoms of social anxiety in adolescence. Psychiatry Res. 2018;263:257–267. 10.1016/j.psychres.2018.02.023 [DOI] [PubMed] [Google Scholar]
- 32.Insel Scolnick EM. Cure therapeutics and strategic prevention: raising the bar for mental health research. Mol Psychiatry. 2006;11(1):11–17. 10.1038/sj.mp.4001777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hyman SE, Fenton WSJS. What are the right targets for psychopharmacology? 2003;299(5605):350–351 [DOI] [PubMed] [Google Scholar]
- 34.Correll CU, Carlson HE. Endocrine and metabolic adverse effects of psychotropic medications in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2006;45(7):771–791. 10.1097/01.chi.0000220851.94392.30 [DOI] [PubMed] [Google Scholar]
- 35.Haller SP, Stoddard J, MacGillivray C, et al. A double-blind, randomized, placebo-controlled trial of a computer-based Interpretation Bias Training for youth with severe irritability: a study protocol. 2018;19(1):626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kaufman J, Birmaher B, Brent D, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. 1997;36(7):980–988 [DOI] [PubMed] [Google Scholar]
- 37.Wiggins JL, Brotman MA, Adleman NE, et al. Neural correlates of irritability in disruptive mood dysregulation and bipolar disorders. 2016;173(7):722–730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Towbin K, Vidal-Ribas P, Brotman MA, et al. A Double-Blind Randomized Placebo-Controlled Trial of Citalopram Adjunctive to Stimulant Medication in Youth With Chronic Severe Irritability. J Am Acad Child Adolesc Psychiatry. 2020;59(3):350–361. 10.1016/j.jaac.2019.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haller SP, Kircanski K, Stringaris A, et al. The Clinician Affective Reactivity Index: Validity and Reliability of a Clinician-Rated Assessment of Irritability. Behav Ther. 2020;51(2):283–293. 10.1016/j.beth.2019.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stringaris A, Goodman R, Ferdinando S, et al. The Affective Reactivity Index: a concise irritability scale for clinical and research settings. J Child Psychol Psychiatry. 2012;53(11):1109–1117. 10.1111/j.1469-7610.2012.02561.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Group RUoPPAS. The pediatric anxiety rating scale (PARS): Development and psychometric properties. 2002;41(9):1061–1069 [DOI] [PubMed] [Google Scholar]
- 42.Birmaher B, Brent DA, Chiappetta L, et al. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. 1999;38(10):1230–1236 [DOI] [PubMed] [Google Scholar]
- 43.Poznanski EO, Mokros HB. Children's depression rating scale, revised (CDRS-R). Western Psychological Services Los Angeles; 1996. [Google Scholar]
- 44.Kovacs M Rating scales to assess depression in school-aged children. Acta Paedopsychiatr. 1981;46(5-6):305–315. https://www.ncbi.nlm.nih.gov/pubmed/7025571. Published 1981/02/01 [PubMed] [Google Scholar]
- 45.Towbin K, Vidal-Ribas P, Brotman MA, et al. A Double-Blind Randomized Placebo-Controlled Trial of Citalopram Adjunctive to Stimulant Medication in Youth With Chronic Severe Irritability. 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shaffer D, Gould MS, Brasic J, et al. A children's global assessment scale (CGAS). 1983;40(11):1228–1231 [DOI] [PubMed] [Google Scholar]
- 47.Penton-Voak IS, Thomas J, Gage SH, McMurran M, McDonald S, Munafò MRJPs. Increasing recognition of happiness in ambiguous facial expressions reduces anger and aggressive behavior. 2013;24(5):688–697 [DOI] [PubMed] [Google Scholar]
- 48.Lundqvist D, Flykt A, Öhman A. The Karolinska directed emotional faces (KDEF). CD ROM from Department of Clinical Neuroscience, Psychology section, Karolinska Institutet. 1998;91(630):2–2 [Google Scholar]
- 49.Tiddeman B, Burt M, Perrett D. Prototyping and transforming facial textures for perception research. Ieee Computer Graphics and Applications. 2001;21(5):42–50.Doi 10.1109/38.946630 [DOI] [Google Scholar]
- 50.Price RB, Wallace M, Kuckertz JM, et al. Pooled patient-level meta-analysis of children and adults completing a computer-based anxiety intervention targeting attentional bias. 2016;50:37–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. arXivpreprint arXiv: 14065823. 2014 [Google Scholar]
- 52.Rosseel Y Lavaan: An R package for structural equation modeling and more. Version 0.5–12 (BETA). Journal of statistical software. 2012;48(2):1–36 [Google Scholar]
- 53.Hollon SD, Stewart MO, Strunk D. Enduring effects for cognitive behavior therapy in the treatment of depression and anxiety. Annu Rev Psychol. 2006;57:285–315. 10.1146/annurev.psych.57.102904.190044 [DOI] [PubMed] [Google Scholar]
- 54.Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, van MIH. Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychol Bull. 2007;133(1):1–24. 10.1037/0033-2909.133.1.1 [DOI] [PubMed] [Google Scholar]
- 55.Leitzke BT, Plate RC, Pollak SD. Training reduces error in rating the intensity of emotions. Emotion. 2020. 10.1037/emo0000763 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



