Abstract
The median nerve is a mixed sensory and motor nerve that innervates part of the flexor muscles in the anterior compartment of the forearm and muscles in the lateral part of the hand; palmar cutaneous and digital cutaneous nerves branch from the median nerve, which provides sensory innervation to the skin on the radial side of the palm. Also, the median nerve is an object of interest because neuropathy of the median nerve at the level of the carpal tunnel is the most common entrapment neuropathy which increases dramatically in patients with diabetes. Neuromuscular ultrasound provides extensive diagnostic information and has proved itself as a useful complementary test to electrodiagnostic examinations in cases involving median nerve neuropathy. It often happens that the cause of nerve entrapment and neuropathy are variants of several anatomical structures along the course of the median nerve. It is important to be aware and report such anatomical variations of the median nerve in order to avoid damaging the nerve during surgical treatment. Despite the frequently documented abnormalities in the pathway of the brachial plexus and the median nerve, the anatomical variations are unusual to see and are rarely reported. Moreover, there are variations that do not fit under any of the classifications described in the literature.
Keywords: median nerve, musculoskeletal ultrasound, normal and variant anatomy
Aim of the study
The aim of this study is to perform a systemic review of the available literature and current knowledge on the normal, variant and pathological anatomical course patterns and visual presentations of the median nerve in ultrasound examination. The goal of this article is to introduce readers to the basics of ultrasonography (US) of the peripheral nerves of the upper extremity with a focus on the median nerve. The common and important anatomic variations will be reviewed.
Material and methods
A systemic search of major electronic databases (PubMed, ScienceDirect, SAGE, ProQuest) was performed to identify eligible studies. The search terms included the median nerve, median nerve, anatomic, variations, carpal canal.
Normal anatomy and pathway of the median nerve
The median nerve is a mixed sensory and motor nerve(1). In the arm, it gives articular branches to the elbow joint and supplies the pronator teres muscle, pronator quadratus muscle, and flexors of the anterior compartment of the forearm (except the flexor carpi ulnaris muscle and medial half of the flexor digitorum profundus muscle). At wrist, the median nerve supplies the flexor pollicis longus muscle, pronator quadratus muscle, and lateral half of the flexor digitorum profundus muscle. At hand, the median nerve gives motor branches to the thenar and first and second lumbrical muscles as well as sensory branches to radial half of the palm and radial three and half digits(1,2).
The median nerve receives its name from the middle position at the end of the brachial plexus and the forearm(1). Along the pathway from the brachial plexus to its terminal branches, it interacts with various potentially compressive structures, such as the pronator teres muscle (high inserted PT, humeral PT belly, muscular and fibrous PT, PT arcade), flexor digitorum superficialis muscle arcade, lacertus fibrosus, Gantzer’s muscle, vascular pedicle, fibrous arcade of fascia of biceps brachii muscle and medial intermuscular septum, and Struthers’ ligament(3).
Proximally, in the axillary fossa, the median nerve runs posteriorly to the pectoralis major and pectoralis minor muscles, and anteriorly to the subscapularis muscle(1). It leaves the axillary fossa under the inferior edge of the pectoralis major muscle, and in the upper arm it lies medial to the brachial artery and vein(1,3).
In this canal, it is located in front of the intermuscular septum, between the biceps brachii muscle and the brachialis muscle.
In distal part of canal, the median nerve crosses in front of the brachial artery and finds itself on the medial side of it, entering the cubital fossa in front of the brachialis muscle(1).
The median nerve passes the ulnar artery and finds itself laterally to the artery in the lower cubital fossa(1). In the cubital fossa, the median nerve runs deep to the bicipital aponeurosis a.k.a. lacertus fibrosus, which arises from the biceps musculotendinous junction and inserts into the antebrachial fascia(3). Afterwards, the median nerve courses deep to the tendinous (sublimis) bridge connecting the humero-ulnar and radial heads of the flexor digitorum superficialis muscle(4).
The nerve then crosses to the forearm through the body of the pronator teres muscle, crossing between its humeral (superficial) and ulnar (deep) heads(1).
As it exits the pronator teres muscle, it passes under the arch of the flexor digitorum superficialis muscle and courses between the flexor digitorum superficialis muscle and the flexor digitorum profundus muscle(1) (Fig. 1). At underarm and towards the wrist, the median nerve lies along the axis of the ring finger(1,3). At wrist, the median nerve emerges from the lateral side of the flexor digitorum superficialis muscle, and runs more superficially and deep to the tendon of the palmaris longus muscle towards the carpal canal(3). Before entering the carpal canal, the median nerve is deep to the palmaris longus muscle, medial and superficial to the flexor carpi radialis and flexor pollicis longus muscles, and lateral and superficial to the digitorum superficialis muscle(3).
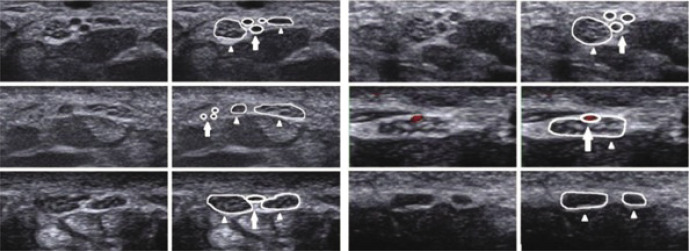
Fig. 1.
Transverse grayscale US of normal median nerve at proximal border of pronator quadratus muscle (A, B), proximal to carpal tunnel inlet (C, D), at tunnel inlet (E, F) and at tunnel outlet (G). Orange dotted circle and M – median nerve; FPL – flexor pollicis longus muscle; FDS – flexor digitorum superficialis muscle; PQ – pronator quadratus muscle; FCR – flexor carpi radialis muscle; FDP – flexor digitorum profundus muscle; R – radius; white dotted line – os lunatum; pink dotted line – flexor retinaculum. Reference: Medical Imaging. Riga East Clinical University Hospital
Ten anatomical structures pass through the carpal tunnel: superficially located median nerve (deep only to the retinaculum) is accompanied by 4 flexor digitorum superficialis muscles, 4 flexor digitorum profundus muscles, and one flexor pollicis longus muscle tendon(1,3).
The nerve ends distal to the carpal tunnel, where it divides into its medial and lateral branches(5).
Variant anatomy of the median nerve
At the origin/upper arm
The median nerve arises from both medial and lateral cords of the brachial plexus, but the location of this merge can vary. It has been found that both cords can merge at the axillary fossa (60%), below the axillary fossa at the level of the pectoralis major muscle (39%), or at the level of medial part of the humeral shaft (1%)(1). The relation of the median nerve with the brachial artery in the arm has also been described. The median nerve enters the upper arm laterally to the brachial artery. In most cases (92%), at the level of insertion of the coracobrachialis muscle (anteriomedial surface of humerus distal to lesser tubercle) the median nerve crosses the brachial artery in front from the lateral to medial sides. In some cases, the median nerve can cross the brachial artery posteriorly(6).
At the elbow/forearm
Variations at the elbow mainly impact the relationship between the median nerve and the pronator teres muscle. In a vast majority of cases (95%), the nerve passes between both heads of the pronator teres muscle. Rarely, the median nerve passes between the pronator teres muscle and the flexor digitorum profundus muscle, or goes through the humeral head of the muscle, or the brachialis muscle (Fig. 2). When Struthers’ ligament (an anatomical variation found in 1–3% of the population) is present, the median nerve passes behind it, and this may be a potential compression site(1). Regardless of the site where the median nerve is compressed, this condition is called pronator teres syndrome, since the compression itself often occurs between the heads of the pronator teres muscle. In the majority of people, both (humeral and ulnar) heads are present (86%), and the median nerve can course between the two heads of the pronator teres muscle (72%), posteriorly to the two heads (3%) or through the ulnar head of the pronator teres muscle (11%). In some cases (14%), the ulnar head is absent, in which case the median nerve courses through the humeral head (3%) or posteriorly to the humeral head of the pronator teres muscle (11%)(7).
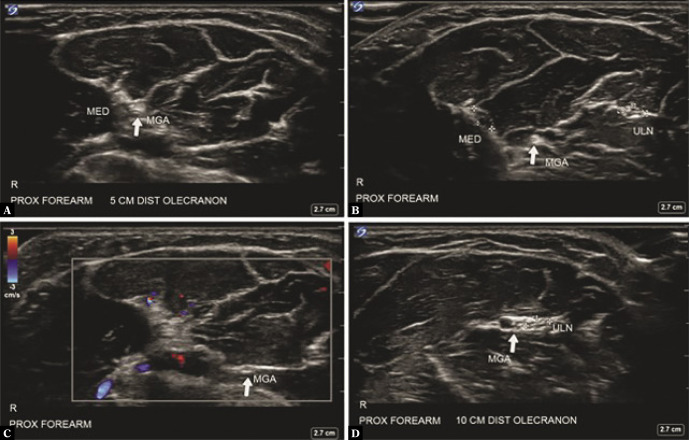
Fig. 2.
Transverse sonography over the proximal humeral head of pronator teres muscle depicting median nerve (white arrow) running deep between humeral head of pronator muscle (PTHH) and brachial anterior muscle (BA), with nerve located distally to brachial artery (black arrow)(17)
At the carpal tunnel
Median nerve variations at the level of the carpal tunnel might be the most widely described site mainly due to the high prevalence of carpal tunnel syndrome and surgical decompression therapy in this region. The Poisel classification regards the branching types of the recurrent branch of the median nerve (a.k.a. thenar motor branch):
Type I or extraligamentous (approximately 45% of all cases) where the recurrent branch divides distal to the flexor retinaculum in a retrograde manner.
Type II or subligamentous (about 30%) where the recurrent branch divides at the level of the carpal tunnel, runs under the flexor retinaculum, and reaches the thenar muscle.
Type III or transligamentous (about 25%) where the recurrent branch divides in the carpal tunnel and crosses the flexor retinaculum.
Some authors have also described a preligamentous form in which the recurrent branch divides proximal to the carpal tunnel and runs in front of the flexor retinaculum(8). Furthermore, in a vast majority of cases the recurrent branch of the median nerve divides from the radial side of the nerve, but in about 2% of all cases it arises from the ulnar side(5).
Three years later, in 1977, Lanz expanded the Poisel classification (Fig. 3):
Fig. 3.
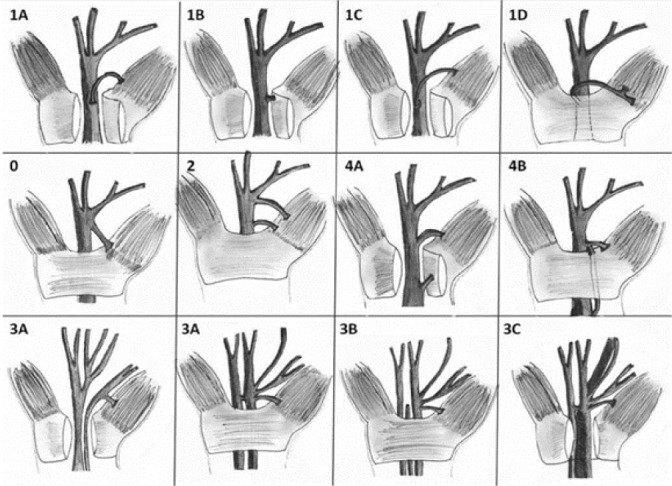
Lanz classification of median nerve anatomical variations at the wrist. Group I, thenar branch variations; 1A: Subligamentous; 1B: Transligamentous; 1C: Ulnarwards; 1D: Supraligamentous. Group 0, extraligamentous thenar branch. Group II, distal accessory thenar branch. Group IV, proximal accessory thenar branch; 4A: Running directly in the thenar muscles; 4B: Joining another branch. Group III, high division of the median nerve; 3A: Without artery of muscle; 3B: With artery; 3C: With lumbrical muscle(18)
Group 0 corresponds to standard anatomy or the extraligamentous course of the recurrent branch of the median nerve.
Group 1 includes the subligamentous, transligamentous, preligamentous and supraligamentous courses.
Group 2 is characterised by the presence of a distal accessory recurrent branch.
Group 3 includes high division of the median nerve with bifid configuration at the carpal tunnel which is associated with the presence of a persistent median artery, as Lanz reported(5) (Fig. 4). Although in most subjects the median nerve courses through the carpal tunnel as a single nerve, the bifurcation of the median nerve proximal to transverse carpal ligament presents in 1% to 3.3% of individuals undergoing carpal tunnel release surgery(9).
Group 4 is characterised by an accessory branch of the median nerve which divides proximal to the carpal tunnel and connects to the recurrent branch of the median nerve(5).
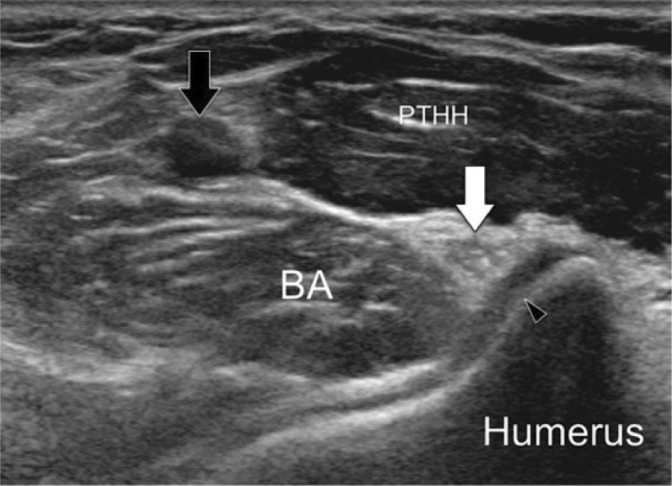
Fig. 4.
Transverse ultrasonographic image and marked image of bifid median nerve (white arrowhead) and persistent median artery (white arrow)(19)
Some authors propose to modify the Lanz classification by including trifurcation of the median nerve (Fig. 5) in the 3rd group because even though bifurcation of the median nerve has shown not to be associated with carpal tunnel syndrome, theoretically an increase in cross-sectional volume of the nerve within the carpal tunnel might contribute to compression. Furthermore, there is a risk of injury to the median nerve if trifurcation goes undiagnosed(10).
Fig. 5.
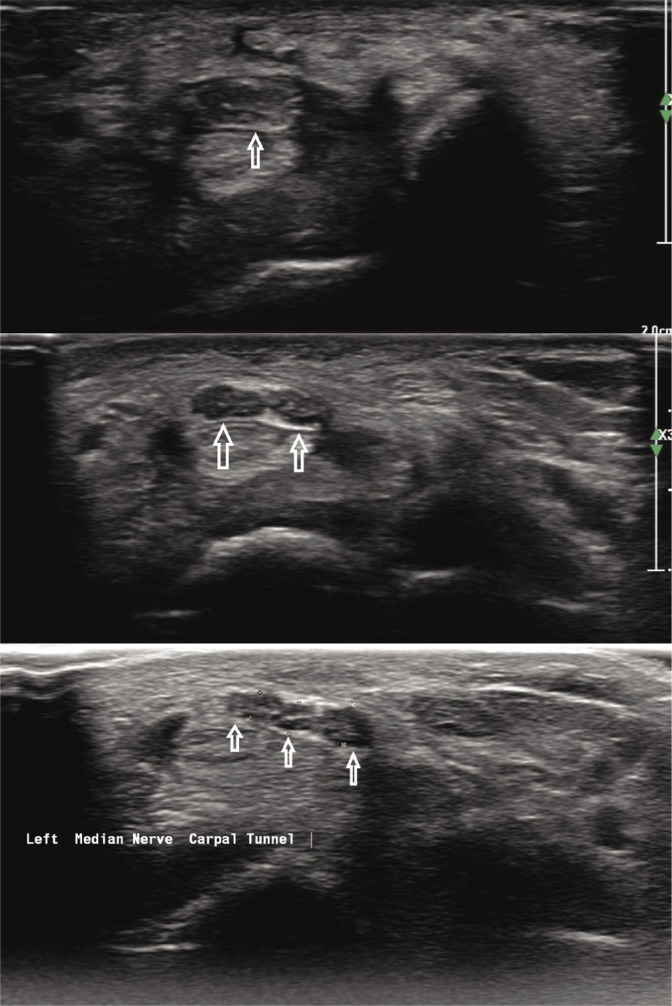
Transverse ultrasonographic image and marked image of trifurcation of median nerve at the level of carpal canal (white arrows). Reference: Medical Imaging. Riga East Clinical University Hospital
If clinically necessary, both arms should be assessed preoperatively because no one can surely assume the anatomical pathway of the median nerves between the arms, as only 72% of patients had an identical nerve course on both sides(1,5).
In addition to various branching sites of the median nerve, many authors in anatomical research papers have observed communicating branches between the median nerve and the musculocutaneous nerve, emerging directly from the lateral cord of the brachial plexus in the axilla(11). The overall prevalence of the median nerve and musculocutaneous nerve branches is estimated to be about 30%, and anastomoses are bilateral in up to 14.1% of cases(1,8). Choi et al. described three patterns of anastomosis between the median and musculocutaneous nerves(8) (Fig. 6):
Fig. 6.
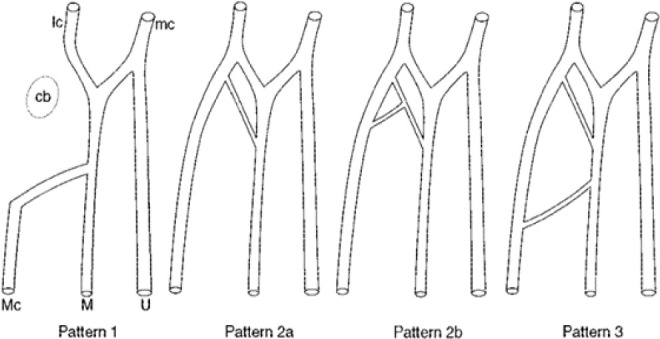
Patterns of connection between musculocutaneous and median nerves. cb, coracobrachialis muscle; lc, lateral cord; mc, medial cord; Mc, musculocutaneous nerve; M, median nerve; U, ulnar nerve(8)
In I type pattern both musculocutaneous and median nerves are fused (19.2% of all cases).
Type II (about 72.6%) can be divided further based on whether there is one (2a subcategory) or two or more (2b subcategory) connective branches emerging from the musculocutaneous and connecting to the median nerve.
In type III pattern, there are two connecting branches present between the musculocutaneous and median nerves (it occurs in about 6.8% of cases)(8).
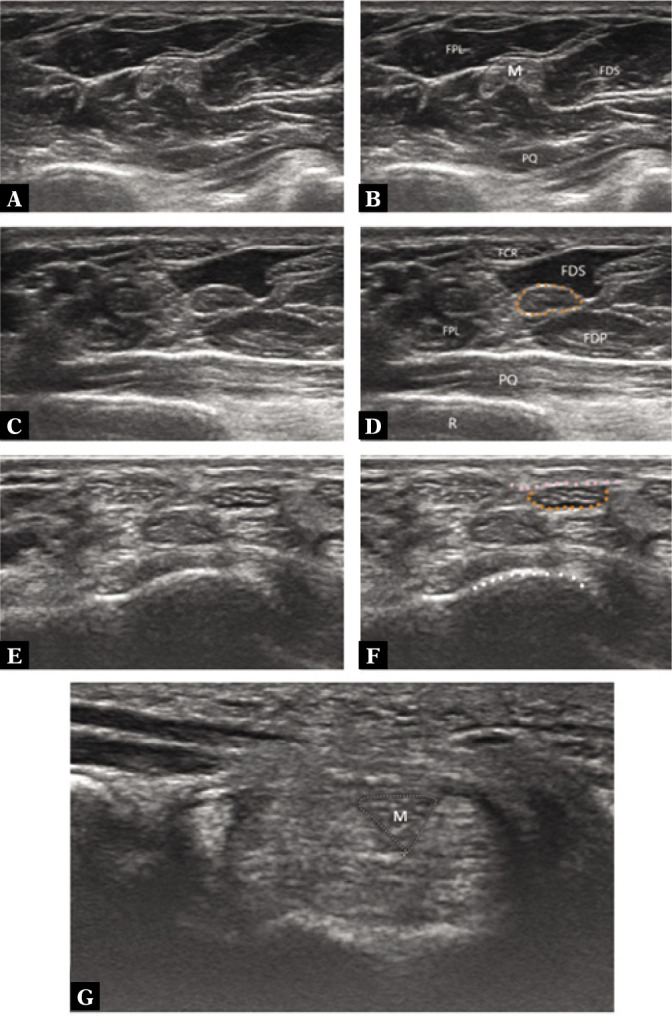
Another extensively studied anastomosis is between the median nerve and ulnar nerve a.k.a. the Martin–Gruber communicating branch (Fig. 7). Its incidence varies greatly depending on the study, from 7% to 40% (with a mean prevalence of 19.5%)(1,12).
Fig. 7.
Transverse sonography showing Martin-Gruber anastomosis (MGA) branching off of median nerve (MED) 5 cm distal to olecranon (A) and running mediocaudally (B, C) and joining ulnar nerve (ULN) (D)(20)
In most of these cases, the axons course in direction from the median nerve (or interosseous anterior nerve) proximally to the ulnar nerve distally. Usually, the Martin-Gruber anastomosis emerges 1 to 9 cm below the transepicondylar line(1) (Fig. 7).
Other (rarer) variations are possible, including:
Double branch between the interosseous anterior nerve and ulnar nerve (7.4%);
Direct anastomosis between the median and ulnar nerves (15%);
Anastomosis from a branch of the median nerve to the flexor digitorum profundus muscle (18%);
Intramuscular anastomosis (18%);
Anastomosis from a branch of the median nerve destined to the flexor digitorum superficialis muscle (8%).
Another communicating branch between the median nerve and ulnar nerve at the forearm is the Marinacci anastomosis (with estimated frequency of at least 0,7%), which in contrast to the Martin-Gruber anastomosis, goes in the opposite direction(1).
Riche´–Cannieu communicating branch is an anastomosis between the recurrent motor thenar branch of the median nerve and the deep branch of the ulnar nerve at the thenar eminence(13). Some authors state the prevalence of the Riche´–Cannieu anastomosis at 55%-70%, though this anastomosis is not widely known and reported(1,13).
The Berrettini communicating branch is an anastomosis between common digital nerves that arise from the ulnar nerve and median nerve in the palmar surface of the hand(13).
A summary of the main anatomical interneural anastomoses of the median nerve is illustrated in Fig. 8.
Fig. 8.
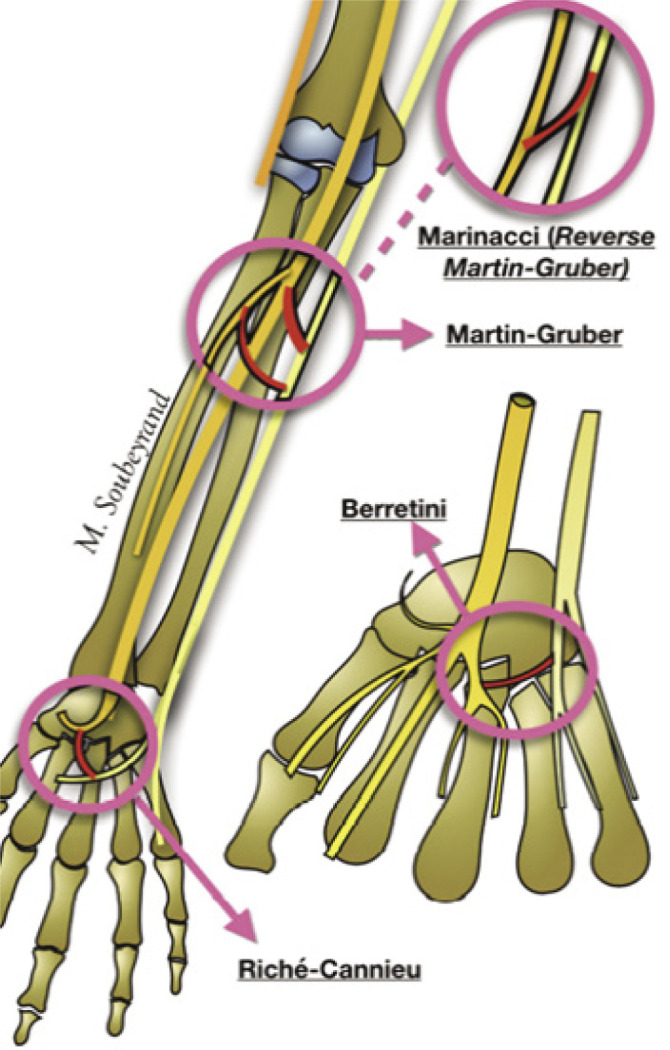
Summary of main anatomical interneural anastomosis of median nerve: MartinGruber anastomosis ‒ anastomosis from the main trunk of median nerve or interosseous anterior nerve to ulnar nerve; Marinacci anastomosis ‒ the reverse of Martin-Gruber anastomosis ulnar-to-median communication; Berretini anastomosis – communications between common digital nerves that arise from ulnar and median nerves in the palmar surface of hand; Riche-Cannieu anastomosis ‒ connection between the deep branch of ulnar nerve and recurrent branch of median nerve at thenar eminence(1)
Normal appearance of the median nerve on ultrasound
Technical considerations
The diagnostic information which can be obtained during sonography of peripheral nerves is to large extent influenced by the operator and the availability and technical considerations of state-of-the-art equipment(14). For peripheral nerve sonography, the type of transducer depends on the anatomical region, but superficially lying median nerves should be scanned with a high-frequency, linear array transducer(15). At sites where the surface does not allow adequate contact between the probe and skin, the best choice is a hockey-stick probe, however they are characterised by a relatively small field of view(4). The visualisation of superficial structures with modern transducers is possible at frequencies of up to 17 MHz(14). When imaging anatomical structures, the depth should be kept to a minimum, the focus values should be directed to the area of interest, and gains adjusted in order to differentiate the nerve fascicles(16).
Anatomy and appearance on ultrasonography
The nerves are depicted as well-circumscribed, roundish hypoechoic fascicles with a honeycomb-like pattern within the hyperechoic epineurium on transverse imaging(15). The nerves are easier to detect when they are coursing among hypoechoic muscles than those among hyperechoic fat tissue, which is why a nerve of a physically active patient is better visualised than the same nerve examined in a patient with atrophic muscles(4). Also, the nerves are compressible and alter their shape depending on the volume of the anatomical spaces within which they course, so when assessing nerve compression, it is advised to measure the cross-section area (CSA), and for the median nerve this is done at four sites: proximal border of the pronator quadratus muscle, proximal to the carpal tunnel inlet, at tunnel inlet, and at tunnel outlet (Fig. 1). Maximal CSA of 12 mm2 or more at any site is diagnostic of carpal tunnel syndrome(2). It is also good to remember that when the nerves cross tight passages, for example, neural foramina and osteofibrous tunnels, changes in echotexture can be detected, with a more homogeneous hypoechoic appearance due to the tighter packing of the fascicles and local reduction in the volume of the epineurium(4).
It is preferable to examine the median nerve in transverse plane to be able to easily follow the nerve pathway throughout the limb. Proximally, the median nerve is located between the biceps brachii and brachialis muscles in the bicipital fossa, and it lies lateral to the brachial vein and artery(4,15) (Fig. 9).
Fig. 9.
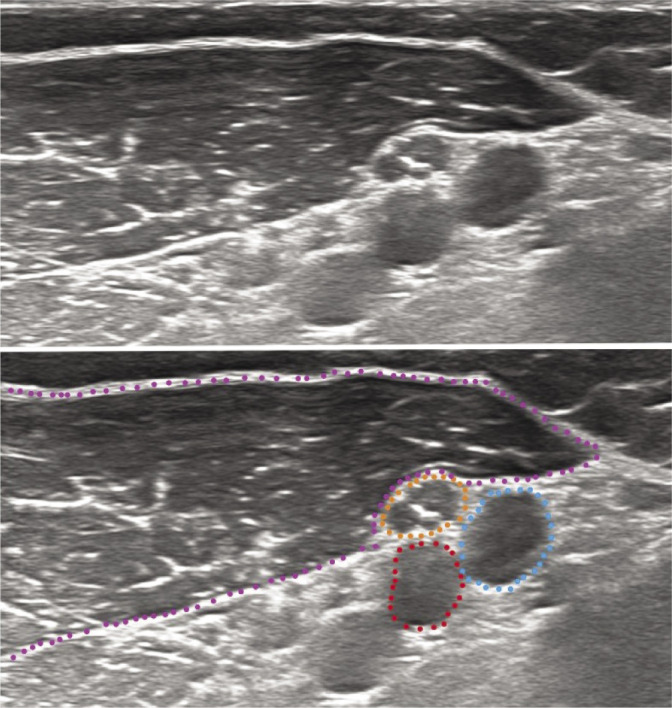
Transverse grayscale US of median nerve in upper arm; orange dotted circle – median nerve; red dotted circle – brachial artery; blue dotted circle – brachial vein; purple dotted line – biceps brachii muscle. Reference: Medical Imaging. Riga East Clinical University Hospital
Important landmarks that a specialist should look out for at the elbow include the brachial artery, pronator teres muscle, and ulnar artery. At the elbow, the median nerve courses through the Lacertus tunnel, where the median nerve lies medial to the brachial artery (which branches into the radial and ulnar arteries), and between the humeral and ulnar heads of the pronator teres muscle, more lateral the distal part of biceps brachii can be visualised (“BAM” view)(1,4,15).
The landmark ulnar artery is seen deep to the ulnar head of the pronator teres. The median nerve runs along the medial aspect of the ulnar artery in the forearm. In the middle part of the forearm, the median nerve moves distally to the ulnar artery and travels between the flexor digitorum profundus muscle and the flexor digitorum superficialis(2,4) (Fig. 10).
Fig. 10.
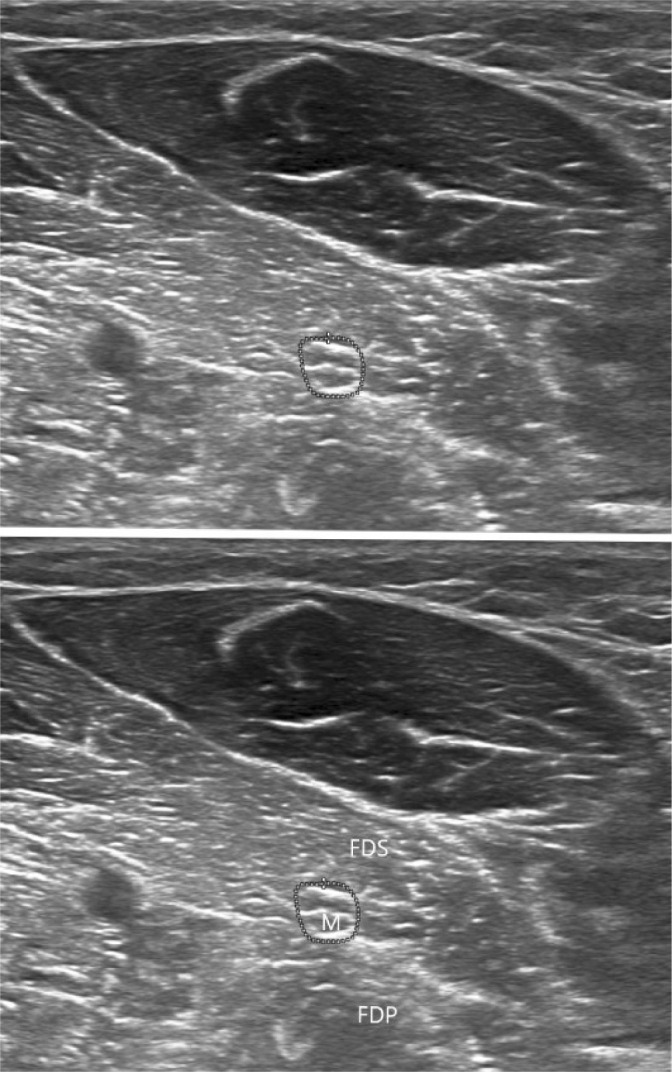
Transverse grayscale US of median nerve in forearm. M – median nerve; FDS – flexor digitorum superficialis muscle; FDP – flexor digitorum profundus muscle. Reference: Medical Imaging. Riga East Clinical University Hospital
At the wrist, the median nerve is superficially located, just deep to the palmaris longus tendon and flexor retinaculum, lateral to the FDS tendons, and medial to the FCR (Fig. 11).
Fig. 11.
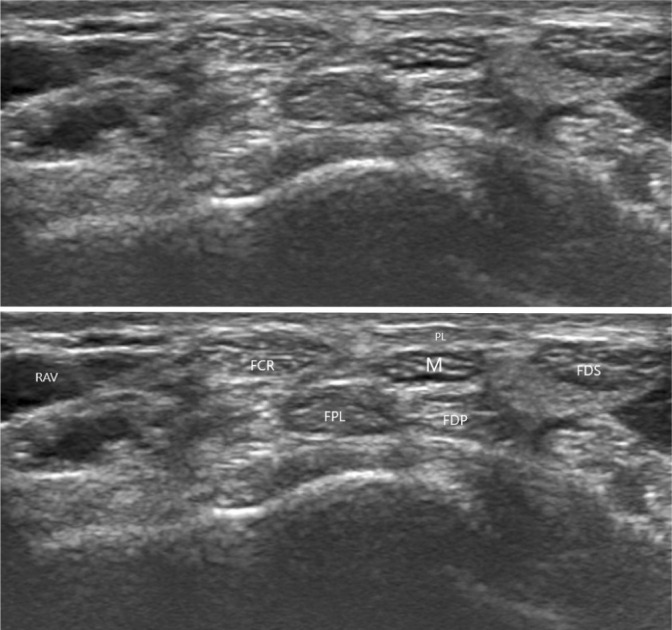
Transverse grayscale US of median nerve in carpal tunnel. M – median nerve; FCR – flexor carpi radialis muscle; FDS – flexor digitorum superficialis muscle; FPL -flexor pollicis longus muscle; FDP – flexor digitorum profundus muscle. Reference: Medical Imaging. Riga East Clinical University Hospital
At the wrist level, the anisotropy of the tendons surrounding the median nerve can be noted. In contrast to the nerve, the tendons will be hypoechoic and hyperechoic, and the median nerve will remain hypoechoic and fascicular(4) (Fig. 11). In the carpal tunnel, the median nerve is superficial and radial to the deep and superficial flexor digitorum, and superficial and ulnar to the tendon of the flexor pollicis longus muscle(2) (Fig. 11).
Conclusion
US provides superior resolution to MR imaging of the peripheral nerves, offers an advantage of dynamic evaluation, and allows for direct correlation with signs and symptoms. Good knowledge of anatomical landmarks is, therefore, crucial and facilitates an evaluation of the entire nerve. US offers an effective means to confirm findings of electrodiagnostic studies, and in addition it can reliably diagnose entrapment neuropathies as a stand-alone examination.
Footnotes
Conflict of interest
There are no conflicts of interest to declare.
References
- 1.Soubeyrand M, Melhem R, Protais M, Artuso M, Crézé M: Anatomy of the median nerve and its clinical applications – a literature review. Hand Surg Rehabil 2020; 39: 2–18. [DOI] [PubMed] [Google Scholar]
- 2.Griffith James F.: Diagnostic Ultrasound. Musculoskeletal. Elsevier, Philadelphia: 2015. [Google Scholar]
- 3.de Mont-Marin GD, Laulan J, Le Nen Dominique, Bacle G: Topographic anatomy of structures liable to compress the median nerve at the elbow and proximal forearm. Orthop Traumatol Surg Res 2021; 107: 102813. [DOI] [PubMed] [Google Scholar]
- 4.Bianchi S, Martinoli C: Ultrasound of the Musculoskeletal System. Springer-Verlag Berlin Heidelberg; 2007. [Google Scholar]
- 5.Henry MB, Zwinczewska H, Joyeeta R, Vikse J, Ramakrishnan PK, Walocha JA. et al. : The prevalence of anatomical variations of the median nerve in the carpal tunnel: a systemic review and meta-analysis. PLoS One 2015; 10: e0136477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sthapak E, Pasricha N, Bhatnagar R: Relation of median nerve with brachial artery: a cadaveric study. J Anat Science 2019; 27: 10–14. [Google Scholar]
- 7.Caetano EB, Vieira LA, Sprovieri FAA, Petta GC, Nakasone MT, Serafim BLC: Anatomical variations of pronator teres muscle: predispositional role for nerve entrapment. Rev Bras Ortop 2017; 52: 169–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi D, Rodríguez-Niedenführ M, Vázquez T, Parkin I, Sañudo J. et al. : Patterns of connections between the musculocutaneous and median nerves in the axilla and arm. Clin Anat 2002; 15: 11–17. [DOI] [PubMed] [Google Scholar]
- 9.Mitchell R, Chesney A, Seal S, McKnight L, Thoma A: Anatomical variation of the carpal tunnel structures. Can J Plast Surg 2009; 17: e3–e7. [PMC free article] [PubMed] [Google Scholar]
- 10.Lonie S, Niumsawatt V, Rozen WM: Median nerve trifurcation. Plast Reconstr Surg Glob Open 2016; 4: e1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gelmi CAE, Pedrini FA, Fermi M, Mariani GA, Cocco LI, Billi AM: Communication between median and musculocutaneous nerve at the level of cubital fossa – a case report. Translat Res Anat 2018; 11: 1–4. [Google Scholar]
- 12.Narayana K, Narendiran K, Shetty KP, Prachanthi N: A case of coexistence of three anatomical variations in the forearm: Gantzer’s muscles, Martin-Gruber anastomosis, and nerve of Henle. Eur J Anat 2004; 8: 81–84. [Google Scholar]
- 13.Unver Dogan N, Uysal IU, Seker M: The communication between the ulnar and median nerves in upper limb. Neuroanatomy 2009; 8: 15–19. [Google Scholar]
- 14.Peer S, Bodner G: High-Resolution Sonography of the Peripheral Nervous System. 2nd Edition. Springer-Verlag Berlin Heidelberg; 2008. [Google Scholar]
- 15.Brown JM, Yablon MC, Morag Y, Brandon JC, Jacobson AJ: US of the peripheral nerves of the upper extremity: a landmark approach. Radiographics 2016; 36: 452–463. [DOI] [PubMed] [Google Scholar]
- 16.Mota SJ, Pereira da Silva FMGS, Gil-Pereira M, Donato H, Donato P, Caseiro Alves F: Peripheral nerve ultrasound–anatomy and technique for diagnosis and procedures. ECR 2014: C-2342. [Google Scholar]
- 17.Créteur V, Madani A, Sattari A, Bianchi S: Sonography of the pronaor teres: normal and pathologic appearances. J Ultrasound Med 2017; 36: 2585–2597. [DOI] [PubMed] [Google Scholar]
- 18.Al-Quattan Mohammad M.: Variations in the course of the thenar motor branch of the median nerve and their relationship to the hypertrophic muscle overlying the transverse carpal ligament. J Hand Surg Am 2010; 35: 1820–1824. [DOI] [PubMed] [Google Scholar]
- 19.Chen L, Chen J, Hu B, Jiang L: Sonographic findings of the bifid median nerve and persistent median artery in carpal tunnel: a preliminary study in chinese individuals. Clinics (Sao Paulo) 2017; 72: 358–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gans P, Van Alfen N: Nerve ultrasound showing Martin-Gruber anastomosis. Muscle Nerve 2017; 56: 46–47. [DOI] [PubMed] [Google Scholar]