Abstract
Until recently, few studies have reported the secular trend and associated factors of hypertension severities and phenotypes in China. In this study, the authors aimed to assess the trend in the prevalence of hypertension according to severity and phenotype in Chinese adults from 1991 to 2015 and to explore potential cardiometabolic factors. From the China Health and Nutrition Survey (CHNS), the authors included 164 682 records of adults (≥18 years). The prevalence of hypertension by severity (stage 1 and stage 2 hypertension) and by phenotype (isolated systolic hypertension [ISH], isolated diastolic hypertension [IDH], and systolic‐diastolic hypertension [SDH]), during 1991‐2015 was explored. The potential effects of demographic, socioeconomic, geographic, and cardiometabolic factors on hypertension severities and phenotypes were assessed by multivariable logistic regression. During 1991‐2015, the overall prevalence of hypertension increased dramatically from 15.7% to 23.3%. For stage 1 and stage 2 hypertension, the age‐standardized prevalence increased from 10.1% to 15.6% and from 5.5% to 7.4%, respectively. For ISH and SDH, the age‐standardized prevalence rates rose from 3.6% to 6.4% and from 6.9% to 10.4%, respectively. Advanced age and medium/high urbanization were positively associated factors, whereas females, higher educational attainments, and residing in Southern China were negatively associated factors. Additionally, general obesity, central obesity, diabetes, and elevated triglyceride levels were linked to ISH, IDH, and SDH. The present study documents an increasing trend in the prevalence of hypertension, including different severities and phenotypes, among Chinese adults over more than two decades. Efforts for the prevention and management of hypertension are in urgent need in China.
Keywords: cardiometabolic risk, Chinese adults, hypertension, phenotypes, severity
1. INTRODUCTION
Hypertension, or elevated blood pressure (BP), is a major modifiable risk factor for cardiovascular disease (CVD) and chronic kidney disease. 1 Understanding the epidemiology of hypertension is essential for quantifying the public health burden of disease, as well as guiding adequate health care planning and provision. 2 As a prevalent condition, hypertension affected more than one billion people and was responsible for 11 million deaths and 212 million disability‐adjusted life years globally in 2015, bringing a significant public health challenge to the global society. 1 , 3 It is estimated that, from 2000 to 2010, the age‐standardized prevalence of hypertension has decreased by 2.6% in high‐income countries (HIC), but increased by 7.7% in low‐ and middle‐income countries (LMIC). 4 Overall, the absolute burden of hypertension worldwide is still consistently on the rise during 2000‐2010, with the number of people affected by hypertension having increased by 27 million in HIC and 440 million in LMIC. 4
In the largest developing country‐China, the emergence of hypertension has also become a major public health challenge. 5 Thus far, several large‐scale investigations have revealed the prevalence of hypertension in the Chinese population. The China Health and Nutrition Survey (CHNS, from 1989 to 2015) adopted a standard procedure for BP measurement over time and across geographic regions, providing an opportunity to track the trends of BP distribution and hypertension prevalence. 6 Different hypertension phenotypes represent potentially distinct underlying pathophysiological mechanisms and clinical impacts. 7 , 8 For example, isolated systolic hypertension (ISH, abnormal systolic blood pressure [SBP] and normal diastolic blood pressure [DBP]) represents a particularly salient subtype of hypertension and a reliable predictor for adverse cardiovascular outcomes. 9 Using CHNS 1991‐2009, a previous study has revealed an increasing trend in mean systolic BP and hypertension prevalence among Chinese adults; however, secular trends in the prevalence of different severities and phenotypes of hypertension remain unknown. 6
To fill this knowledge gap, we herein report a comprehensive analysis from CHNS to assess the dynamic prevalence of hypertension severities and phenotypes in Chinese adults over more than two decades (1991‐2015). The specific objectives of the present study were twofold. The first was to assess secular trends in the prevalence of hypertension, different severities and phenotypes of hypertension, including prehypertension, stage 1 and stage 2 hypertension, ISH, isolated diastolic hypertension (IDH, abnormal DBP and normal SBP), combined systolic and diastolic hypertension (SDH, abnormal SBP and abnormal DBP), and controlled hypertension, among the general Chinese adults. 2 The second objective was to explore the associations of hypertension, different severities and phenotypes, with selected demographic, geographic, socioeconomic, health behavioral, and cardiometabolic factors.
2. MATERIALS AND METHODS
2.1. Survey methods
Details of the study design were described previously. 10 Briefly, CHNS is an ongoing prospective household‐based health and nutrition survey that covered a set of large provinces across China (the list and locations of investigated provinces are shown in Table S1 and Figure S1). CHNS was approved by the Institutional Review Committees of the University of North Carolina at Chapel Hill and the National Institute of Nutrition and Food Safety, Chinese Center for Disease Control and Prevention. Informed consents were obtained from all participants.
Beginning in 1989, CHNS has been continuously conducted, and data have been released for ten rounds between 1989 and 2015 (1989, 1991, 1993, 1997, 2000, 2004, 2006, 2009, 2011, and 2015). 10 CHNS maintains a high standard in sampling, data collection, and processing. In each wave, a multistage, random‐clustered sampling approach was adopted. First, all counties and cities in each province were stratified into low‐, middle‐, and high‐income groups based on income, among which four counties (one low‐, two middle‐, and one high‐income) and two cities (usually the provincial capital and a lower‐income city) were selected. Second, two urban and two suburban communities within selected cities, one community within the provincial capital city, and three rural villages within selected counties were randomly chosen. Third, 20 households were randomly selected for participation from each selected community/village, and all members of the selected households were interviewed. 10
2.2. Data collection
Throughout the ten rounds of CHNS surveys, trained interviewers (investigators) collected information on demographics (eg, age and sex), geographic location (eg, urban or rural, north region or south region), socioeconomic status (eg, marriage, educational attainment, economic level), and health‐related behaviors (eg, smoking and alcohol drinking) by a structured questionnaire. Blood pressure, weight, height, and waist circumference (WC) were examined following a standard protocol from the World Health Organization. 11 After a 10‐minute seated rest, blood pressure was measured on the participant's right arm using a mercury sphygmomanometer by trained examiners. Three BP measurements, separated by a 3‐ to 5‐minute interval, were successively taken on one visit for each participant. SBP and DBP were, respectively, recorded as the average of the three readings. On a calibrated beam scale, weight was measured to the nearest 0.1 kg with lightweight clothing. Height was measured to the nearest 0.1 cm without shoes by a portable stadiometer. With a non‐elastic tape, WC was measured to the nearest 0.1 cm at the mid‐level between the iliac crest and the lowest rib in a horizontal plane. 12 Body mass index (BMI) was calculated as weight divided by height squared (kg/m2). Participants’ blood samples were collected in CHNS 2009, and the levels of various biochemical indexes, including fasting plasma glucose (FPG), glycosylated hemoglobin A1c (HbA1c), total cholesterol (TC), low‐density lipoprotein cholesterol (LDL‐C), high‐density lipoprotein cholesterol (HDL‐C), and triglyceride (TG), were measured at a national laboratory.
2.3. Definitions
2.3.1. Hypertension severities and phenotypes
The definitions of hypertension, hypertension severities, and hypertension phenotypes were in accordance with the “Guidelines for prevention and treatment of hypertension in Chinese adults (Revised Edition 2018)” (Chinese Guidelines 2018) and listed in Table 1. 13 Hypertension was considered as “controlled” if SBP < 120 mmHg and DBP < 80 mmHg while taking antihypertensive medication.
TABLE 1.
Classification of blood pressure in adults according to Chinese Guidelines 2018
| Category | Definition |
|---|---|
| Normal | SBP < 120 mmHg and DBP < 80 mmHg |
| Prehypertension | SBP = 120‐139 mmHg or DBP = 80‐89 mmHg |
| Hypertension | SBP ≥ 140 mmHg or DBP ≥ 90 mmHg or currently on antihypertensive medication |
| Severities | |
| Stage 1 | SBP = 140‐159 mmHg or DBP = 90‐99 mmHg |
| Stage 2 | SBP ≥ 160 mmHg or DBP ≥ 100 mmHg |
| Phenotypes | |
| Isolated systolic hypertension | SBP ≥ 140 mmHg and DBP < 90 mmHg |
| Isolated diastolic hypertension | SBP < 140 mmHg and DBP ≥ 90 mmHg |
| Systolic‐diastolic hypertension | SBP ≥ 140 mmHg and DBP ≥ 90 mmHg |
Abbreviations: DBP, diastolic blood pressure; SBP, systolic blood pressure.
2.3.2. Demographic, socioeconomic, and behavioral factors
All participants were divided into three age‐groups: 18‐39 years, 40‐59 years, and 60 years and above. Marital status was classified into single (unmarried, divorced, widowed, or separated) and married. Education attainment was categorized as no formal education, primary education, middle education (including middle or high school degree), and higher education (including a technical school degree, college school degree, or above). Tertiles of per capita household income (PCHI) were used to define the economic status as poor, middle, and rich. 14 We divided all participants’ residence into Southern China and Northern China. The former regions included Shanghai, Jiangsu, Hubei, Hunan, Guangxi, Guizhou, and Chongqing and the latter included Beijing, Liaoning, Heilongjiang, Shandong, and Henan in CHNS. Other well‐established behavioral factors (eg, smoking and alcohol drinking) were also included. 15 , 16 Based on a face‐to‐face interview, people who smoke at least one cigarette per day were identified as smokers (including former smokers and current smokers). Similarly, alcohol consumers (including former drinkers and current drinkers) were defined by the question “did you drink beer or any alcoholic beverage last year?”.
2.3.3. Cardiometabolic factors
Following the Working Group on Obesity in China criteria, general obesity was defined as a BMI of 28.0 kg/m2 or higher. 17 Central obesity was defined as a WC of >85 cm in males or >80 cm in females, or a waist to height ratio (WHtR) of ≥0.5, or a waist to hip ratio (WHR) of ≥0.9 in males or ≥0.85 in females. 17 According to the World Health Organization (WHO) recommendation in 2011, diabetes was diagnosed as an FPG ≥7.0 mmol/L or an HbA1c ≥ 6.5%, or currently on anti‐diabetic medication. 18 Consistent with the guidelines for prevention and treatment of dyslipidemia in Chinese adults (Revised Edition 2016), elevated TC, elevated LDL‐C, low HDL‐C, and elevated TG were, respectively, defined as a level of ≥5.18 mmol/L (200 mg/dL), ≥3.37 mmol/L (130 mg/dL), ≤1.04 mmol/L (40 mg/dL), and ≥1.70 mmol/L (150 mg/dL). 19
2.4. Statistical analysis
In descriptive analyses, continuous variables were presented as means with standard deviations (SDs), and categorical variables were expressed as percentages with 95% confidence intervals (CIs). Using the direct standardization method, we estimated the age‐standardized prevalence of hypertension in each CHNS wave with the 2010 China Census population as the reference population. 20 Considering dependencies within the same participants across survey years, generalized linear models (GLMs) using generalized estimating equation method were adopted. 21 The individual calendar year was included as a single continuous variable and adjusted for age in GLMs to examine the significance of trends in the prevalence of hypertension, hypertension severities, and phenotypes. Subgroup trend analysis between 1991 and 2015 was conducted by strata of demographic (age, sex), socioeconomic (marital status, education, economic status), geographic (setting, region), and behavioral (smoking, drinking) groups, separately. Furthermore, univariable and multivariable logistic regression models were used to explore the associated demographic, socioeconomic, geographic, and behavioral factors of hypertension, severities, and phenotypes.
Biochemical indexes were only available in CHNS 2009, based on which we additionally assessed the effects of cardiometabolic factors using multivariable logistic regression. The outcome variables were hypertension, hypertension severities, and phenotypes. The independent variables included general obesity, central obesity, diabetes, elevated TC, elevated LDL‐C, low HDL‐C, and elevated TG levels. Odds ratios (ORs) and corresponding 95% CIs were reported to quantify the extent of associations. All statistical analyses were conducted using Stata statistical software (version 14.0; Stata Corporation, College Station, TX, USA). Differences were considered statistically significant if a P value was less than .05.
3. RESULTS
3.1. Characteristics of participants
In total, 164,682 records were obtained from CHNS 1991‐2015, of which 86 623 were used for the descriptive analysis of hypertension prevalence. For the analysis of demographic, socioeconomic, geographic, and behavioral factors, a total of 80 594 observations were eligible. Since the cardiometabolic factors were only assessed in one survey year, we captured 8010 records from CHNS 2009 adult database. The selection procedure of records is summarized in Figure S2. The demographic characteristics of the included and excluded records are shown in Table S2. For all survey rounds, the included participants were relatively older than the excluded (all P values <.001). The proportions of female participants in the included groups were slightly higher than those in the excluded groups across all survey rounds, except for CHNS 2006, 2009, and 2011. The socioeconomic, geographic, health behavioral, and cardiometabolic characteristics are presented in Tables S3 and S4.
3.2. Trends in SBP, DBP, and prevalence of hypertension, hypertension severities, and phenotypes
Table 2 shows the age‐standardized mean SBP and DBP levels in Chinese adults over the 25 years of survey. From 1991 to 2015, both SBP and DBP levels increased by 0.3%, from 115.9 mmHg (95% CI: 115.5‐116.2) to 123.6 mmHg (95% CI: 123.2‐123.9) and from 74.9 mmHg (95% CI: 74.6‐75.1) to 79.6 mmHg (95% CI: 79.4‐79.9), respectively (both P values for age‐adjusted trend < .001). Over the same period, the mean SBP and DBP levels all increased significantly across age‐ and sex groups.
TABLE 2.
Age‐standardized mean SBP and DBP in Chinese adults, CHNS 1991‐2015
| Variable | 1991 (n = 8604) | 1993 (n = 8203) | 1997 (n = 8592) | 2000 (n = 9473) | 2004 (n = 9209) | 2006 (n = 9165) | 2009 (n = 9499) | 2011 (n = 12 542) | 2015 (n = 11 296) | AAI (mmHg) | Average relative increase (%) | P for age‐adjusted trend |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SBP (mmHg), mean (95% CI) | ||||||||||||
| Overall | 115.9 (115.5‐116.2) | 116.1 (115.7‐116.4) | 118.8 (118.4‐119.1) | 119.0 (118.7‐119.3) | 120.2 (119.9‐120.5) | 119.1 (118.7‐119.4) | 121.0 (120.7‐121.4) | 120.9 (120.6‐121.2) | 123.6 (123.2‐123.9) | 0.3 | 0.3 | <.001 |
| Age‐group | ||||||||||||
| 18‐39 years | 108.7 (108.4‐109.1) | 109.6 (109.2‐110.0) | 112.2 (111.8‐112.6) | 112.2 (111.8‐112.6) | 113.7 (113.3‐114.2) | 113.0 (112.5‐113.5) | 113.7 (113.2‐114.2) | 114.1 (113.7‐114.6) | 116.0 (115.4‐116.6) | 0.3 | 0.3 | <.001 |
| 40‐59 years | 117.2 (116.5‐117.8) | 117.0 (116.4‐117.7) | 120.1 (119.5‐120.8) | 120.8 (120.3‐121.3) | 121.8 (121.3‐122.3) | 120.8 (120.3‐121.3) | 123.5 (123.0‐124.0) | 123.5 (123.1‐123.9) | 126.8 (126.3‐127.3) | 0.4 | 0.3 | <.001 |
| ≥60 years | 132.5 (131.1‐133.9) | 131.5 (130.2‐132.8) | 133.8 (132.7‐134.9) | 133.9 (132.9‐134.9) | 134.4 (133.4‐135.3) | 131.9 (131.0‐132.7) | 135.7 (134.9‐136.5) | 133.7 (133.1‐134.4) | 137.4 (136.8‐137.9) | 0.2 | 0.2 | <.001 |
| Sex | ||||||||||||
| Male | 117.8 (117.3‐118.3) | 117.9 (117.4‐118.4) | 120.6 (120.1‐121.1) | 120.9 (120.5‐121.4) | 122.5 (122.0‐122.9) | 121.3 (120.9‐121.8) | 123.2 (122.7‐123.6) | 123.4 (123.0‐123.8) | 126.7 (126.2‐127.2) | 0.4 | 0.3 | <.001 |
| Female | 114.1 (113.6‐114.6) | 114.4 (113.9‐114.9) | 117.0 (116.5‐117.5) | 117.2 (116.8‐117.7) | 118.0 (117.6‐118.5) | 116.9 (116.5‐117.4) | 119.0 (118.5‐119.4) | 118.7 (118.4‐119.1) | 121.1 (120.7‐121.5) | 0.3 | 0.3 | <.001 |
| DBP (mmHg), mean (95% CI) | ||||||||||||
| Overall | 74.9 (74.6‐75.1) | 75.8 (75.5‐76.0) | 77.1 (76.9‐77.3) | 77.3 (77.1‐77.5) | 77.8 (77.6‐78) | 77.7 (77.4‐77.9) | 79.0 (78.8‐79.2) | 77.8 (77.7‐78.0) | 79.6 (79.4‐79.9) | 0.2 | 0.3 | <.001 |
| Age‐group | ||||||||||||
| 18‐39 years | 71.5 (71.2‐71.8) | 72.7 (72.4‐73.0) | 74.1 (73.8‐74.3) | 74.1 (73.8‐74.4) | 75.1 (74.8‐75.5) | 74.8 (74.5‐75.2) | 75.6 (75.2‐76) | 74.8 (74.5‐75.1) | 76.5 (76.0‐76.9) | 0.2 | 0.3 | <.001 |
| 40‐59 years | 76.5 (76.0‐76.9) | 77.2 (76.8‐77.6) | 78.5 (78.1‐78.9) | 79.1 (78.8‐79.5) | 79.6 (79.2‐79.9) | 79.5 (79.2‐79.8) | 81.5 (81.2‐81.9) | 80.5 (80.2‐80.8) | 82.3 (81.9‐82.6) | 0.2 | 0.3 | <.001 |
| ≥60 years | 80.6 (79.8‐81.3) | 80.9 (80.1‐81.7) | 82.3 (81.7‐82.9) | 82.0 (81.4‐82.5) | 81.2 (80.7‐81.8) | 81.3 (80.8‐81.8) | 82.7 (82.3‐83.2) | 80.5 (80.1‐80.8) | 82.5 (82.2‐82.9) | 0.1 | 0.1 | .001 |
| Sex | ||||||||||||
| Male | 76.3 (75.9‐76.6) | 77.2 (76.8‐77.5) | 78.5 (78.2‐78.8) | 78.8 (78.5‐79.1) | 79.5 (79.2‐79.8) | 79.5 (79.1‐79.8) | 81.0 (80.7‐81.3) | 79.8 (79.5‐80) | 82.2 (81.8‐82.6) | 0.3 | 0.3 | <.001 |
| Female | 73.6 (73.3‐74.0) | 74.5 (74.1‐74.8) | 75.7 (75.4‐76.0) | 75.9 (75.6‐76.2) | 76.2 (75.9‐76.5) | 76.0 (75.7‐76.3) | 77.1 (76.8‐77.4) | 76.2 (75.9‐76.4) | 77.5 (77.3‐77.8) | 0.2 | 0.2 | <.001 |
AAI, average annual increase, AAI was computed by dividing the difference of blood pressure between 1991 and 2015 by the number of years covered; ARI, average relative increase, ARI was calculated by dividing the average annual change by the baseline mean blood pressure in 1991; the mean systolic and diastolic blood pressure values were age‐standardized to the China 2010 Census population; and age‐adjusted trends in mean blood pressure from 1991 to 2015 were assessed by the generalized estimating equation method.
The trends of age‐standardized prevalence of hypertension, severities, and phenotypes from 1991 to 2015 are listed in Table 3. For prehypertension, the age‐standardized prevalence increased from 30.1% (95% CI: 29.1‐31.1) to 43.1% (95% CI: 41.9‐44.2). Prehypertension was consistently more prevalent in males (than among females) and people aged 40‐59 years (than in those aged 18‐39 years and ≥60 years). Across the study period, the overall age‐standardized prevalence of hypertension significantly increased from 15.7% (95% CI: 15.0‐16.5) to 23.3% (95% CI: 22.5‐24.1), yielding a relative increasing rate of 2.0%. The prevalence of hypertension was generally higher in males (than in females) and the elderly aged 60 years and above (than in the younger groups). However, the relative increasing rate of prevalence was the highest in young adults aged 18‐39 years (5.4%), being twice that in those aged 40‐59 years (2.7%) and more than ten times of that in over 60 years of age (0.4%).
TABLE 3.
Age‐standardized prevalence of hypertension, hypertension severities, and phenotypes in Chinese adults, CHNS 1991‐2015
| Variable | 1991 (n = 8604) | 1993 (n = 8203) | 1997 (n = 8592) | 2000 (n = 9473) | 2004 (n = 9209) | 2006 (n = 9165) | 2009 (n = 9499) | 2011 (n = 12 542) | 2015 (n = 11 296) | AAI (mmHg) | Average relative increase (%) | P for age‐adjusted trend |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prehypertension (%, 95% CI) | ||||||||||||
| Overall | 30.1 (29.1‐31.1) | 33.4 (32.4‐34.4) | 36.9 (35.9‐37.9) | 38.4 (37.5‐39.4) | 41.3 (40.2‐42.4) | 41.6 (40.5‐42.8) | 41.0 (39.9‐42.1) | 42.4 (41.4‐43.4) | 43.1 (41.9‐44.2) | 0.5 | 1.8 | <.001 |
| Age‐group | ||||||||||||
| 18‐39 years | 26.8 (25.5‐28.1) | 30.6 (29.2‐32.1) | 35.4 (33.9‐37.0) | 35.9 (34.3‐37.4) | 40.7 (38.8‐42.6) | 39.6 (37.6‐41.7) | 37.3 (35.3‐39.3) | 38.3 (36.5‐40.1) | 41.0 (38.8‐43.2) | 0.6 | 2.2 | <.001 |
| 40‐59 years | 33.7 (32.0‐35.5) | 36.7 (35.0‐38.5) | 39.9 (38.2‐41.6) | 42.2 (40.7‐43.8) | 44.2 (42.7‐45.8) | 45.4 (43.9‐46.9) | 46.2 (44.7‐47.7) | 47.4 (46.1‐48.7) | 45.8 (44.4‐47.2) | 0.5 | 1.5 | <.001 |
| ≥60 years | 31.1 (28.6‐33.8) | 33.7 (31.2‐36.3) | 34.2 (31.9‐36.6) | 37.2 (35.0‐39.4) | 36.4 (34.3‐38.4) | 38.8 (36.8‐40.8) | 39.6 (37.8‐41.5) | 42.9 (41.3‐44.5) | 42.6 (41.1‐44.1) | 0.5 | 1.5 | <.001 |
| Sex | ||||||||||||
| Male | 34.5 (33.0‐36.0) | 38.3 (36.7‐39.8) | 41.0 (39.5‐42.5) | 44.2 (42.8‐45.7) | 47.2 (45.6‐48.8) | 47.8 (46.1‐49.4) | 46.2 (44.5‐47.8) | 49.4 (47.9‐50.9) | 48.9 (47.1‐50.7) | 0.6 | 1.7 | <.001 |
| Female | 26.0 (24.8‐27.3) | 29.0 (27.7‐30.4) | 32.7 (31.3‐34.1) | 33.0 (31.7‐34.4) | 35.4 (34.0‐36.9) | 35.8 (34.3‐37.4) | 36.0 (34.5‐37.5) | 36.4 (35.1‐37.7) | 38.2 (36.7‐39.7) | 0.5 | 1.9 | <0.001 |
| Hypertension (%, 95% CI) | ||||||||||||
| Overall | 15.7 (15.0‐16.5) | 16.4 (15.7‐17.2) | 19.2 (18.5‐20.0) | 18.7 (18.0‐19.4) | 18.5 (17.8‐19.3) | 16.9 (16.2‐17.6) | 20.9 (20.1‐21.6) | 17.3 (16.7‐17.9) | 23.3 (22.5‐24.1) | 0.3 | 2.0 | <0.001 |
| Age‐group | ||||||||||||
| 18‐39 years | 4.5 (3.9‐5.1) | 5.5 (4.9‐6.3) | 7.2 (6.4‐8.0) | 6.6 (5.8‐7.4) | 7.0 (6.1‐8.0) | 6.0 (5.1‐7.0) | 8.0 (7.0‐9.2) | 5.7 (4.9‐6.6) | 10.3 (9.0‐11.7) | 0.2 | 5.4 | <.001 |
| 40‐59 years | 17.4 (16.1‐18.8) | 17.8 (16.5‐19.3) | 21.2 (19.9‐22.7) | 21.6 (20.3‐22.9) | 21.2 (20.0‐22.5) | 19.6 (18.4‐20.8) | 25.2 (23.9‐26.5) | 21.3 (20.3‐22.4) | 28.7 (27.4‐30.0) | 0.5 | 2.7 | <.001 |
| ≥60 years | 42.8 (40.1‐45.6) | 43.1 (40.4‐45.8) | 47.8 (45.3‐50.3) | 45.5 (43.2‐47.9) | 44.3 (42.2‐46.4) | 40.7 (38.7‐42.7) | 46.3 (44.4‐48.2) | 40.3 (38.8‐41.9) | 47.1 (45.5‐48.6) | 0.2 | 0.4 | .005 |
| Sex | ||||||||||||
| Male | 17.3 (16.2‐18.4) | 18.0 (16.8‐19.2) | 21.6 (20.5‐22.8) | 20.8 (19.7‐21.9) | 21.3 (20.1‐22.4) | 19.5 (18.4‐20.7) | 24.3 (23.0‐25.5) | 20.1 (19.1‐21.1) | 28.4 (27.0‐29.8) | 0.5 | 2.7 | <.001 |
| Female | 14.4 (13.4‐15.4) | 15.0 (14.0‐16.0) | 16.9 (15.9‐17.9) | 16.7 (15.8‐17.6) | 15.9 (15.1‐16.8) | 14.5 (13.7‐15.4) | 17.6 (16.8‐18.5) | 14.9 (14.2‐15.6) | 19.3 (18.4‐20.2) | 0.2 | 1.4 | <.001 |
| Stage 1 hypertension (%, 95% CI) | ||||||||||||
| Overall | 10.1 (9.5‐10.8) | 11.4 (10.7‐12.1) | 13.2 (12.6‐14.0) | 12.8 (12.2‐13.5) | 12.8 (12.1‐13.4) | 11.7 (11.1‐12.3) | 13.5 (12.9‐14.2) | 12.0 (11.5‐12.6) | 15.6 (14.8‐16.3) | 0.2 | 2.2 | <.001 |
| Age‐group | ||||||||||||
| 18‐39 years | 3.9 (3.4‐4.5) | 4.8 (4.2‐5.5) | 6.2 (5.4‐7.0) | 5.4 (4.8‐6.2) | 5.9 (5.1‐6.8) | 4.8 (4.0‐5.7) | 6.0 (5.1‐7.0) | 4.8 (4.1‐5.6) | 8.1 (7.0‐9.4) | 0.2 | 4.5 | <.001 |
| 40‐59 years | 11.6 (10.4‐12.8) | 12.9 (11.7‐14.2) | 14.6 (13.5‐15.9) | 14.9 (13.8‐16.0) | 14.5 (13.4‐15.6) | 13.6 (12.6‐14.7) | 16.1 (15.1‐17.2) | 14.5 (13.6‐15.4) | 18.3 (17.2‐19.4) | 0.3 | 2.4 | <.001 |
| ≥60 years | 24.0 (21.7‐26.5) | 25.8 (23.5‐28.3) | 29.6 (27.3‐31.9) | 28.6 (26.6‐30.8) | 27.7 (25.8‐29.7) | 26.4 (24.6‐28.2) | 28.3 (26.6‐30.0) | 26.5 (25.1‐28) | 29.8 (28.4‐31.2) | 0.2 | 1.0 | .004 |
| Sex | ||||||||||||
| Male | 11.7 (10.7‐12.7) | 12.9 (11.9‐14.0) | 15.4 (14.4‐16.5) | 15.1 (14.1‐16.1) | 15.5 (14.5‐16.5) | 13.9 (12.9‐14.9) | 16.0 (15.0‐17.1) | 14.6 (13.7‐15.5) | 18.9 (17.7‐20.2) | 0.3 | 2.6 | <.001 |
| Female | 8.8 (8.0‐9.7) | 10.0 (9.1‐10.9) | 11.2 (10.3‐12.1) | 10.8 (10.0‐11.6) | 10.2 (9.4‐10.9) | 9.7 (9.0‐10.5) | 11.1 (10.4‐11.9) | 9.8 (9.2‐10.5) | 12.9 (12.1‐13.7) | 0.2 | 1.9 | <.001 |
| Stage 2 hypertension (%, 95% CI) | ||||||||||||
| Overall | 5.5 (5.0‐6.0) | 4.9 (4.5‐5.4) | 5.9 (5.4‐6.4) | 5.6 (5.2‐6.1) | 5.5 (5.1‐5.9) | 4.9 (4.6‐5.3) | 7.1 (6.6‐7.6) | 4.9 (4.5‐5.2) | 7.4 (6.9‐7.8) | 0.1 | 1.5 | <.001 |
| Age‐group | ||||||||||||
| 18‐39 years | 0.5 (0.3‐0.7) | 0.7 (0.4‐1.0) | 1.0 (0.7‐1.4) | 1.1 (0.8‐1.4) | 1.0 (0.7‐1.4) | 1.2 (0.8‐1.7) | 2.0 (1.5‐2.7) | 0.9 (0.6‐1.3) | 2.1 (1.6‐2.8) | 0.1 | 14.1 | <.001 |
| 40‐59 years | 5.7 (4.9‐6.6) | 4.8 (4.0‐5.6) | 6.5 (5.7‐7.4) | 6.5 (5.8‐7.3) | 6.4 (5.7‐7.2) | 5.7 (5.0‐6.4) | 8.7 (7.9‐9.6) | 6.3 (5.7‐6.9) | 9.9 (9.1‐10.8) | 0.2 | 3.1 | <.001 |
| ≥60 years | 18.6 (16.5‐20.9) | 17.0 (15.0‐19.2) | 17.9 (16.1‐20.0) | 16.1 (14.5‐17.9) | 15.9 (14.4‐17.5) | 13.5 (12.2‐15.0) | 17.2 (15.8‐18.7) | 12.5 (11.5‐13.6) | 16.3 (15.2‐17.5) | −0.1 | −0.5 | .071 |
| Sex | ||||||||||||
| Male | 5.5 (4.8‐6.2) | 4.9 (4.2‐5.6) | 6.2 (5.5‐6.9) | 5.6 (5.0‐6.2) | 5.6 (5.0‐6.2) | 5.4 (4.8‐6.1) | 8.0 (7.3‐8.8) | 5.2 (4.7‐5.7) | 9.1 (8.3‐9.9) | 0.2 | 2.8 | <.001 |
| Female | 5.5 (4.8‐6.2) | 4.9 (4.3‐5.6) | 5.6 (5.0‐6.3) | 5.6 (5.1‐6.2) | 5.4 (4.9‐6.0) | 4.5 (4.0‐5.0) | 6.2 (5.6‐6.7) | 4.6 (4.2‐5.0) | 6.0 (5.5‐6.5) | 0.0 | 0.4 | <.001 |
| ISH (%, 95% CI) | ||||||||||||
| Overall | 3.6 (3.2‐4.1) | 3.1 (2.7‐3.5) | 4.8 (4.4‐5.3) | 4.0 (3.7‐4.4) | 4.9 (4.5‐5.3) | 4.3 (3.9‐4.6) | 4.9 (4.5‐5.2) | 5.2 (4.9‐5.5) | 6.4 (6.0‐6.8) | 0.1 | 3.1 | <.001 |
| Age‐group | ||||||||||||
| 18‐39 years | 0.3 (0.1‐0.5) | 0.5 (0.3‐0.7) | 1.0 (0.7‐1.4) | 0.5 (0.3‐0.8) | 1.0 (0.7‐1.4) | 0.6 (0.4‐1.0) | 1.1 (0.7‐1.7) | 0.9 (0.6‐1.3) | 1.3 (0.9‐1.9) | 0.0 | 16.1 | <.001 |
| 40‐59 years | 2.7 (2.1‐3.3) | 2.0 (1.5‐2.6) | 4.0 (3.4‐4.8) | 3.1 (2.6‐3.7) | 3.0 (2.6‐3.6) | 3.6 (3.1‐4.1) | 3.5 (3.0‐4.1) | 4.0 (3.5‐4.5) | 5.4 (4.8‐6.0) | 0.1 | 4.3 | <.001 |
| ≥60 years | 14.9 (13.0‐17.1) | 12.7 (10.9‐14.7) | 17.1 (15.2‐19.1) | 15.6 (14.0‐17.4) | 19.5 (17.9‐21.2) | 15.8 (14.3‐17.3) | 18.1 (16.6‐19.6) | 19.6 (18.4‐21.0) | 22.4 (21.1‐23.7) | 0.3 | 2.1 | <.001 |
| Sex | ||||||||||||
| Male | 3.4 (2.8‐4.0) | 2.7 (2.3‐3.3) | 4.9 (4.3‐5.6) | 4.0 (3.5‐4.6) | 5.0 (4.4‐5.6) | 4.3 (3.8‐4.9) | 4.7 (4.2‐5.4) | 5.1 (4.6‐5.6) | 6.1 (5.5‐6.7) | 0.1 | 3.3 | <.001 |
| Female | 3.8 (3.3‐4.4) | 3.4 (2.9‐4.0) | 4.7 (4.1‐5.3) | 4.0 (3.5‐4.5) | 4.7 (4.3‐5.3) | 4.2 (3.8‐4.7) | 4.9 (4.5‐5.4) | 5.3 (4.9‐5.7) | 6.6 (6.2‐7.2) | 0.1 | 3.1 | <.001 |
| IDH (%, 95% CI) | ||||||||||||
| Overall | 5.1 (4.6‐5.6) | 6.5 (5.9‐7.0) | 6.7 (6.2‐7.2) | 6.6 (6.1‐7.1) | 6.2 (5.7‐6.7) | 6.0 (5.5‐6.5) | 6.9 (6.3‐7.4) | 5.1 (4.7‐5.5) | 6.2 (5.7‐6.8) | 0.0 | 0.9 | .132 |
| Age‐group | ||||||||||||
| 18‐39 years | 3.2 (2.7‐3.8) | 4.1 (3.6‐4.8) | 4.7 (4.1‐5.4) | 4.4 (3.8‐5.1) | 4.4 (3.7‐5.2) | 3.9 (3.2‐4.8) | 5.1 (4.3‐6.1) | 3.6 (3.0‐4.3) | 5.8 (4.8‐6.9) | 0.1 | 3.4 | <.001 |
| 40‐59 years | 7.2 (6.3‐8.2) | 8.2 (7.3‐9.3) | 8.4 (7.5‐9.4) | 8.5 (7.7‐9.5) | 8.5 (7.6‐9.4) | 7.9 (7.2‐8.8) | 9.2 (8.4‐10.1) | 7.1 (6.5‐7.8) | 7.6 (6.9‐8.4) | 0.0 | 0.2 | .316 |
| ≥60 years | 5.7 (4.5‐7.1) | 9.1 (7.6‐10.8) | 8.4 (7.1‐9.9) | 8.1 (6.9‐9.5) | 6.1 (5.1‐7.2) | 7.4 (6.4‐8.5) | 6.4 (5.6‐7.5) | 4.6 (4.0‐5.4) | 4.3 (3.7‐4.9) | −0.1 | −1.0 | <.001 |
| Sex | ||||||||||||
| Male | 6.3 (5.6‐7.1) | 8.1 (7.3‐9.0) | 8.3 (7.5‐9.2) | 8.4 (7.6‐9.2) | 8.3 (7.5‐9.2) | 7.8 (7.0‐8.6) | 9.3 (8.4‐10.3) | 7.0 (6.3‐7.7) | 8.9 (7.9‐10.0) | 0.1 | 1.7 | .029 |
| Female | 4.0 (3.4‐4.6) | 5.0 (4.4‐5.7) | 5.1 (4.5‐5.8) | 4.9 (4.3‐5.5) | 4.2 (3.6‐4.8) | 4.4 (3.9‐5.0) | 4.6 (4.1‐5.2) | 3.4 (3.0‐3.9) | 4.0 (3.5‐4.6) | 0.0 | 0.0 | .912 |
| SDH (%, 95% CI) | ||||||||||||
| Overall | 6.9 (6.4‐7.4) | 6.7 (6.2‐7.3) | 7.6 (7.1‐8.2) | 7.9 (7.4‐8.4) | 7.2 (6.8‐7.7) | 6.4 (5.9‐6.8) | 8.9 (8.4‐9.4) | 6.6 (6.3‐7.0) | 10.4 (9.9‐10.9) | 0.1 | 2.1 | <.001 |
| Age‐group | ||||||||||||
| 18‐39 years | 0.9 (0.7‐1.3) | 0.9 (0.6‐1.2) | 1.5 (1.2‐1.9) | 1.6 (1.3‐2.0) | 1.6 (1.2‐2.1) | 1.4 (1.0‐1.9) | 1.8 (1.3‐2.4) | 1.3 (0.9‐1.7) | 3.2 (2.5‐4.0) | 0.1 | 9.9 | <.001 |
| 40‐59 years | 7.4 (6.5‐8.4) | 7.5 (6.6‐8.5) | 8.6 (7.7‐9.7) | 9.7 (8.8‐10.7) | 9.4 (8.5‐10.3) | 7.8 (7.1‐8.6) | 12.2 (11.2‐13.2) | 9.7 (8.9‐10.4) | 15.2 (14.3‐16.3) | 0.3 | 4.4 | <.001 |
| ≥60 years | 22.0 (19.8‐24.4) | 21.1 (18.9‐23.5) | 22.0 (20.0‐24.2) | 21.0 (19.2‐23.0) | 18.0 (16.4‐19.7) | 16.8 (15.3‐18.4) | 21.0 (19.5‐22.6) | 14.8 (13.7‐16.0) | 19.5 (18.3‐20.7) | ‐0.1 | ‐0.5 | .005 |
| Sex | ||||||||||||
| Male | 7.4 (6.6‐8.3) | 7.0 (6.2‐7.8) | 8.3 (7.5‐9.2) | 8.2 (7.5‐9.0) | 7.8 (7.1‐8.5) | 7.2 (6.5‐7.9) | 10.0 (9.3‐10.9) | 7.7 (7.1‐8.3) | 13.0 (12.1‐14.0) | 0.2 | 3.2 | <.001 |
| Female | 6.4 (5.7‐7.2) | 6.5 (5.8‐7.3) | 7.0 (6.3‐7.7) | 7.5 (6.9‐8.2) | 6.7 (6.1‐7.3) | 5.6 (5.1‐6.1) | 7.8 (7.2‐8.4) | 5.7 (5.3‐6.2) | 8.2 (7.6‐8.8) | 0.1 | 1.2 | <.001 |
| Controlled hypertension (%, 95% CI) | ||||||||||||
| Overall | 0.1 (0.1‐0.2) | 0.1 (0.1‐0.2) | 0.1 (0‐0.2) | 0.2 (0.2‐0.4) | 0.3 (0.2‐0.4) | 0.2 (0.2‐0.4) | 0.3 (0.2‐0.4) | 0.4 (0.3‐0.5) | 0.4 (0.3‐0.5) | 0.0 | 6.9 | <.001 |
| Age‐group | ||||||||||||
| 18‐39 years | 0.1 (0.0‐0.2) | 0.1 (0‐0.2) | 0.0 (0.0‐0.0) | 0.1 (0.0‐0.2) | 0.0 (0.0‐0.2) | 0.1 (0.0‐0.2) | 0.0 (0.0‐0.0) | 0.0 (0.0‐0.0) | 0.1 (0.0‐0.3) | 0.0 | ‐0.8 | .634 |
| 40‐59 years | 0.2 (0.1‐0.4) | 0.1 (0.1‐0.4) | 0.1 (0‐0.3) | 0.2 (0.1‐0.4) | 0.4 (0.2‐0.6) | 0.3 (0.1‐0.5) | 0.3 (0.2‐0.5) | 0.5 (0.4‐0.8) | 0.5 (0.3‐0.7) | 0.0 | 6.9 | <.001 |
| ≥60 years | 0.2 (0.1‐0.6) | 0.2 (0.1‐0.7) | 0.3 (0.1‐0.7) | 0.8 (0.5‐1.3) | 0.8 (0.5‐1.2) | 0.8 (0.5‐1.2) | 0.8 (0.6‐1.3) | 1.3 (1‐1.7) | 1.0 (0.7‐1.3) | 0.0 | 15.8 | <.001 |
| Sex | ||||||||||||
| Male | 0.1 (0.1‐0.3) | 0.2 (0.1‐0.4) | 0.1 (0.0‐0.2) | 0.2 (0.1‐0.3) | 0.2 (0.1‐0.4) | 0.2 (0.1‐0.4) | 0.2 (0.1‐0.3) | 0.4 (0.3‐0.5) | 0.4 (0.2‐0.5) | 0.0 | 6.3 | <.001 |
| Female | 0.1 (0.1‐0.3) | 0.1 (0.0‐0.2) | 0.1 (0.0‐0.3) | 0.3 (0.2‐0.5) | 0.3 (0.2‐0.5) | 0.3 (0.2‐0.4) | 0.3 (0.2‐0.5) | 0.5 (0.4‐0.6) | 0.4 (0.3‐0.5) | 0.0 | 7.5 | <.001 |
AAI, average annual increase, AAI was computed by dividing the difference of prevalence between 1991 and 2015 by the number of years covered; ARI=average relative increase, ARI was calculated by dividing the average annual change by the baseline prevalence in 1991; the prevalence estimates were age‐standardized to the China 2010 Census population; and age‐adjusted trends in prevalence from 1991 to 2015 were assessed by the generalized estimating equation method.
For stage 1 and stage 2 hypertension, the age‐standardized prevalence increased from 10.1% (95% CI: 9.5‐10.8) to 15.6% (95% CI: 14.8‐16.3) and from 5.5% (95% CI: 5.0‐6.0) to 7.4% (95% CI: 6.9‐7.8), respectively, from 1991 to 2015. The prevalence of stage 1 hypertension was generally higher than stage 2 hypertension. Within this time frame, the relative increasing rates of both stage 1 and stage 2 hypertension were greater in males than in females, and the highest was in people aged 18‐39 years. However, no statistically significant secular trend of increasing stage 2 hypertension prevalence was observed among people aged 60 years or older (P = .071).
SDH accounted for the largest share of hypertension subtypes (Figure S3). For ISH, the age‐standardized prevalence increased from 3.6% to 6.4% (men from 3.4% to 6.1%, women from 3.8% to 6.6%) over the 25 years (1991‐2015). The prevalence of ISH in three age‐groups (18‐39, 40‐59, and ≥60 years) increased by 16.1%, 4.3%, and 2.1% (all age‐adjusted P values < .001). Similar to ISH, the age‐standardized prevalence of SDH increased from 6.9% (95% CI: 6.4‐7.4) in 1991 to 10.4% (95% CI: 9.9‐10.9) in 2015. Upward trends were seen in all subgroups (males, females, 18‐39 years, 40‐59 years), except in people over 60 years (decreased from 22.0% to 19.5%). For IDH, however, no significant trend of age‐standardized prevalence was observed from 1991 to 2015 (P = .132). An overall increasing trend of IDH prevalence was found in the age‐groups of 18‐39 years (from 3.2% to 5.8%) and in males (from 6.3% to 8.9%), but was insignificant in the middle‐aged and in females (P = .316 and 0.912) across the survey period. During 1991‐2015, the prevalence of controlled hypertension rose from 0.1% (95% CI: 0.1‐0.2) to 0.4% (95% CI: 0.3‐0.5). The corresponding relative increasing rates in males, females, 18‐39, 40‐59, and ≥60 years were 6.3%, 7.5%, −0.8%, 6.9%, and 15.8%, respectively (Table 3).
3.3. Demographic, socioeconomic, geographic, behavioral, and cardiometabolic factors of hypertension, hypertension severities, and phenotypes
Table 4 shows the associated demographic, socioeconomic, geographic, and behavioral factors of hypertension, severities, and phenotypes. After adjusting for demographic characteristics, socioeconomic status, geographic location, and health behaviors, the prevalence of prehypertension, hypertension, stage 1 hypertension, and IDH increased gradually with survey years. For stage 2 hypertension, ISH, and SDH, it was progressive more common in 1997‐2015 than in 1991. In addition, advanced age, being rich, highly urbanized, and alcohol drinking were all positively associated with prehypertension, hypertension, and stage 1 and stage 2 hypertension, whereas females, higher educational attainments, and living in Southern China were negatively associated factors. For ISH, people aged over 60 were positively associated with higher odds (OR = 40.2, 95% CI: 34.6‐46.6). Moreover, participants residing in highly or moderately urbanized areas were more likely to have ISH, with an odds ratio of 1.7 (95% CI: 1.5‐2.0) and 1.5 (95% CI: 1.4‐1.7), compared with those living in less urbanized regions. However, being females (vs. males), married status (vs. single status), a higher education level (vs. no formal education), and south residence (vs. north residence) were associated with a decreased risk of ISH. For IDH, where people aged 40‐59 years (OR = 2.6, 95%CI: 2.4‐2.8) and those aged over 60 years (OR = 3.7, 95%CI: 3.3‐4.2) had a higher risk of IDH than those aged 18‐39 years, advanced age was also a positively associated factor. Moreover, being married, higher economic level, medium/high urbanization, and drinkers were positively related to IDH with ORs of 1.3(95% CI: 1.2‐1.)4, 1.2(95% CI: 1.1‐1.3), 1.2(95% CI: 1.1‐1.3)/1.4(95% CI: 1.3‐1.6), and 1.2(95% CI: 1.1‐1.3), respectively. A consistent inverse association existed between females, higher education attainments, or south regions and the prevalence of IDH. For SDH, elevated risks were evaluated between the middle‐aged (OR = 5.4, 95% CI: 4.9‐5.9) or the elderly (OR = 13.1, 95% CI: 11.8‐14.6), being rich (OR = 1.1, 95% CI: 1.0‐1.2), higher urbanization level (OR = 1.4, 95% CI: 1.3‐1.5 and 1.5, 95% CI: 1.3‐1.6), drinking alcohol (OR = 1.1, 95%CI: 1.0‐1.2), and the prevalence of SDH. However, being males was related to a negative association. Compared with people with no formal education and in Northern China, those receiving higher education and from Southern China were less likely to have SDH. Neither urban residence nor smoking was independently associated with a higher risk of hypertension, the two different hypertension severities, and all the three phenotypes.
TABLE 4.
Multivariable odds ratios of demographic, socioeconomic, and behavioral factors for hypertension, hypertension severities, and phenotypes
| Characteristic | Prehypertension | Hypertension | Stage 1 hypertension | Stage 2 hypertension | ISH | IDH | SDH | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Odds ratio (95% CI) | P value | Odds ratio (95% CI) | P value | Odds ratio (95% CI) | P value | Odds ratio (95% CI) | P value | Odds ratio (95% CI) | P value | Odds ratio (95% CI) | P value | Odds ratio (95% CI) | P value | |
| Survey year | ||||||||||||||
| 1991 | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | |||||||
| 1993 | 1.2 (1.1‐1.3) | <.001 | 1.2 (1.1‐1.3) | <.001 | 1.3 (1.1‐1.4) | <.001 | 1.0 (0.9‐1.1) | .952 | 1.0 (0.9‐1.2) | .854 | 1.4 (1.2‐1.5) | <.001 | 1.0 (1.0‐1.1) | .364 |
| 1997 | 1.5 (1.4‐1.6) | <.001 | 1.6 (1.5‐1.7) | <.001 | 1.7 (1.5‐1.8) | <.001 | 1.4 (1.2‐1.5) | <.001 | 1.9 (1.6‐2.2) | <.001 | 1.6 (1.4‐1.8) | <.001 | 1.3 (1.2‐1.5) | <.001 |
| 2000 | 1.5 (1.4‐1.7) | <.001 | 1.5 (1.4‐1.7) | <.001 | 1.6 (1.5‐1.8) | <.001 | 1.4 (1.2‐1.6) | <.001 | 1.6 (1.3‐1.9) | <.001 | 1.6 (1.4‐1.8) | <.001 | 1.5 (1.3‐1.6) | <.001 |
| 2004 | 1.7 (1.6‐1.9) | <.001 | 1.8 (1.6‐1.9) | <.001 | 1.8 (1.7‐2.0) | <.001 | 1.6 (1.5‐1.8) | <.001 | 2.0 (1.7‐2.3) | <.001 | 1.6 (1.4‐1.8) | <.001 | 1.6 (1.5‐1.8) | <.001 |
| 2006 | 1.7 (1.6‐1.8) | <.001 | 1.6 (1.5‐1.7) | <.001 | 1.7 (1.5‐1.9) | <.001 | 1.4 (1.2‐1.6) | <.001 | 1.8 (1.5‐2.1) | <.001 | 1.6 (1.4‐1.8) | <.001 | 1.4 (1.2‐1.5) | <.001 |
| 2009 | 2.1 (1.9‐2.2) | <.001 | 2.2 (2‐2.4) | <.001 | 2.4 (2.1‐2.6) | <.001 | 1.9 (1.7‐2.2) | <.001 | 2.5 (2.1‐2.9) | <.001 | 2.0 (1.8‐2.3) | <.001 | 2.0 (1.8‐2.3) | <.001 |
| 2011 | 1.9 (1.8‐2.1) | <.001 | 1.9 (1.7‐2.1) | <.001 | 2.0 (1.8‐2.2) | <.001 | 1.7 (1.5‐1.9) | <.001 | 2.3 (2.0‐2.7) | <.001 | 1.4 (1.2‐1.6) | <.001 | 1.8 (1.6‐2.0) | <.001 |
| 2015 | 2.5 (2.3‐2.8) | <.001 | 3.0 (2.7‐3.3) | <.001 | 3.1 (2.7‐3.4) | <.001 | 2.4 (2.1‐2.7) | <.001 | 3.9 (3.2‐4.6) | <.001 | 2.0 (1.7‐2.3) | <.001 | 2.6 (2.3‐3.0) | <.001 |
| Age‐group | ||||||||||||||
| 18‐39 years | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | |||||||
| 40‐59 years | 1.8 (1.7‐1.9) | <.001 | 3.5 (3.3‐3.7) | <.001 | 3.4 (3.2‐3.6) | <.001 | 5.0 (4.5‐5.6) | <.001 | 6.5 (5.7‐7.4) | <.001 | 2.6 (2.4‐2.8) | <.001 | 5.4 (4.9‐5.9) | <.001 |
| ≥60 years | 3.2 (3.0‐3.4) | <.001 | 9.5 (8.8‐10.2) | <.001 | 9.8 (9.1‐10.7) | <.001 | 14.3 (12.7‐16.1) | <.001 | 40.2 (34.6‐46.6) | <.001 | 3.7 (3.3‐4.2) | <.001 | 13.1 (11.8‐14.6) | <.001 |
| Sex | ||||||||||||||
| Male | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | |||||||
| Female | 0.5 (0.5‐0.6) | <.001 | 0.5 (0.5‐0.5) | <.001 | 0.5 (0.5‐0.5) | <.001 | 0.6 (0.5‐0.6) | <.001 | 0.7 (0.6‐0.8) | <.001 | 0.4 (0.4‐0.4) | <.001 | 0.5 (0.5‐0.6) | <.001 |
| Marital status | ||||||||||||||
| Single | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | |||||||
| Married | 1.1 (1.1‐1.2) | <.001 | 1.0 (1.0‐1.1) | .16 | 1.0 (1.0‐1.1) | .355 | 0.9 (0.9‐1.0) | .148 | 0.8 (0.7‐0.9) | <.001 | 1.3 (1.2‐1.4) | <.001 | 1.0 (0.9‐1.1) | .604 |
| Education | ||||||||||||||
| No formal education | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | |||||||
| Primary education | 0.9 (0.9‐1.0) | .075 | 0.8 (0.7‐0.8) | <.001 | 0.8 (0.8‐0.9) | <.001 | 0.8 (0.7‐0.8) | <.001 | 0.8 (0.7‐0.9) | <.001 | 0.9 (0.8‐1.0) | .086 | 0.8 (0.7‐0.9) | <.001 |
| Middle education | 0.9 (0.8‐0.9) | <.001 | 0.6 (0.6‐0.7) | <.001 | 0.7 (0.6‐0.8) | <.001 | 0.6 (0.6‐0.7) | <.001 | 0.6 (0.6‐0.7) | <.001 | 0.8 (0.7‐0.9) | <.001 | 0.7 (0.6‐0.7) | <.001 |
| Higher education | 0.8 (0.7‐0.8) | <.001 | 0.5 (0.4‐0.5) | <.001 | 0.5 (0.4‐0.5) | <.001 | 0.5 (0.4‐0.5) | <.001 | 0.5 (0.4‐0.5) | <.001 | 0.6 (0.5‐0.7) | <.001 | 0.5 (0.4‐0.5) | <.001 |
| Economic status | ||||||||||||||
| Poor | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | |||||||
| Middle | 1.0 (1.0‐1.1) | .177 | 1.1 (1.0‐1.1) | .023 | 1.0 (1.0‐1.1) | .122 | 1.1 (1‐1.1) | .088 | 1.0 (0.9‐1.1) | .622 | 1.1 (1.0‐1.1) | .106 | 1.1 (1.0‐1.1) | .051 |
| Rich | 1.1 (1.0‐1.1) | .005 | 1.1 (1.1‐1.2) | <.001 | 1.1 (1.0‐1.2) | .003 | 1.1 (1.0‐1.2) | .005 | 1.1 (1.0‐1.2) | .060 | 1.2 (1.1‐1.3) | .001 | 1.1 (1.0‐1.2) | .005 |
| Setting | ||||||||||||||
| Rural | 1 (reference) | 1.0 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||||
| Urban | 1.0 (0.9‐1.0) | .631 | 1.0 (0.9‐1.0) | .144 | 1.0 (0.9‐1.0) | .365 | 1.0 (0.9‐1.1) | .864 | 1.0 (0.9‐1.1) | .506 | 1.0 (0.9‐1.1) | .763 | 1.0 (0.9‐1.1) | .682 |
| Urbanization | ||||||||||||||
| Low | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | |||||||
| Medium | 1.1 (1.0‐1.1) | <.001 | 1.3 (1.3‐1.4) | <.001 | 1.3 (1.2‐1.4) | <.001 | 1.4 (1.3‐1.5) | <.001 | 1.5 (1.4‐1.7) | <.001 | 1.2 (1.1‐1.3) | <.001 | 1.4 (1.3‐1.5) | <.001 |
| High | 1.3 (1.2‐1.4) | <.001 | 1.5 (1.4‐1.6) | <.001 | 1.5 (1.4‐1.6) | <.001 | 1.4 (1.3‐1.6) | <.001 | 1.7 (1.5‐2.0) | <.001 | 1.4 (1.3‐1.6) | <.001 | 1.5 (1.3‐1.6) | <.001 |
| Region | ||||||||||||||
| North | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||||
| South | 0.5 (0.5‐0.5) | <.001 | 0.4 (0.4‐0.5) | <.001 | 0.4 (0.4‐0.5) | <.001 | 0.4 (0.4‐0.5) | <.001 | 0.6 (0.5‐0.6) | <.001 | 0.3 (0.3‐0.4) | <.001 | 0.5 (0.4‐0.5) | <.001 |
| Smoking | ||||||||||||||
| Non‐smoker | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1 (reference) | 1 (reference) | |||||||
| Smoker | 1.0 (0.9‐1.0) | .800 | 1.0 (0.9‐1.1) | .806 | 1.0 (0.9‐1.1) | .586 | 0.9 (0.8‐1.0) | .032 | 0.9 (0.8‐1.0) | .197 | 0.9 (0.9‐1.0) | .217 | 1.0 (0.9‐1.0) | .223 |
| Alcohol drinking | ||||||||||||||
| Non‐drinker | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) | 1 (reference) | 1.0 (reference) | |||||||
| Drinker | 1.1 (1.0‐1.1) | .004 | 1.1 (1.1‐1.2) | <.001 | 1.1 (1.1‐1.2) | <.001 | 1.1 (1.0‐1.2) | .003 | 1.1 (1.0‐1.2) | .22 | 1.2 (1.1‐1.3) | <.001 | 1.1 (1.0‐1.2) | .001 |
Values were odds ratio (95% confidence interval); odds ratio for each variable was adjusted for all other variables in the table. The comparisons were between hypertension groups and normotensives; the multivariable generalized estimating equation (GEE) logistic regression adjusted all variables listed.
Using CHNS 2009 data, the cardiometabolic factors related to hypertension, severities and phenotypes were assessed after adjusting for the demographic, socioeconomic, geographic, and behavioral factors (Figure 1). General obesity, central obesity, diabetes, and elevated TG levels were estimated to be positively associated with all types of hypertension (prehypertension, hypertension, stage 1 and stage 2 hypertension). Besides, compared with people who had normal TC levels, those with elevated TC levels were more likely to have hypertension. General obesity, central obesity, diabetes, and elevated TG were associated with an increased risk of ISH. General and central obesity and elevated TG were linked to the presence of IDH, as well. Moreover, two types of obesity, diabetes, and elevated TC and TG levels were related to a positive association of SDH. However, no significant associations between elevated LDL or low HDL and severity of hypertension or hypertension phenotypes were observed.
FIGURE 1.
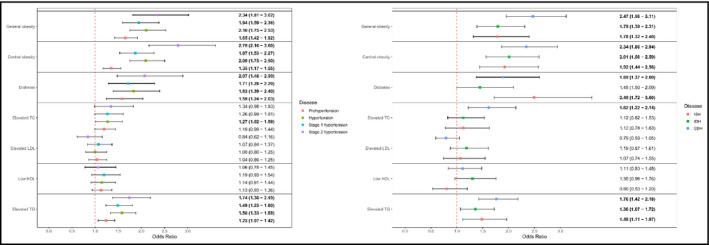
Cardiometabolic factors associated with severities and phenotypes of hypertension in CHNS 2009. *Note: Demographic, socioeconomic, geographic, and behavioral factors were adjusted; values were odds ratio (95% confidence interval), and statistically significant odds ratios are shown in bold
4. DISCUSSION
In this nationwide household‐based study, the prevalence and cardiometabolic factors of hypertension, severities, and phenotypes were estimated in the general adult population for the first time. From 1991 to 2015, the age‐standardized prevalence of hypertension, hypertension severities and hypertension phenotypes in Chinese adults increased dramatically. The prevalence of hypertension severities and phenotypes varied in different demographic, socioeconomic, geographic, and health behavioral groups. Advanced age and medium or high urbanization were positively associated factors of hypertension, hypertension severities, and phenotypes, whereas females, higher educational attainments, and living in Southern China were all negatively related factors. Regarding cardiometabolic factors, general obesity, central obesity, and elevated TG levels were linked to ISH, IDH, and SDH. Furthermore, ISH was associated with diabetes, and SDH was additionally associated with diabetes and elevated TC levels.
To the best of our knowledge, previous studies have mainly focused on the trends of hypertension, but findings on the trends in hypertension severities and phenotypes were limited in China. 6 Compared with previous studies, we extended the study period to 1991‐2015. We additionally assessed the prevalence of hypertension severity (stage 1 hypertension and stage 2 hypertension) and phenotypes (ISH, IDH and SDH) by age and sex. Our findings were largely reliable based on a substantial number of participants, the stringent sampling approach and standard procedure for BP measurements across diverse economic and geographic regions. 6 , 10 The diagnosis of hypertension has been evolving over time. According to the US National Health and Nutrition Examination Survey (NHANES), where hypertension was defined as a BP ≥ 140/90 mmHg, the prevalence remained stable with a rate of 29.6% (95% CI: 26.7‐32.4) in 1999 and 29.5% (95% CI: 27.7‐31.4) in 2010. 22 In comparison with their results, lower age‐standardized prevalence estimates of hypertension (18.7% and 17.3%) among the general Chinese adults in 2000 and 2011 were revealed in our study. In Korea, the absolute number of people with treated hypertension increased remarkably from 1.4 million to 5.7 million during 1998‐2012, whereas the prevalence of ISH and SDH decreased. 23 On the contrary, the current study revealed a rising tendency in ISH as well as SDH in Chinese adults. Moreover, 8.1% of Japanese adults aged 30‐49 were diagnosed as ISH patients during a 29‐year follow‐up. 24
Our results showed a notable and consistent increment in sex‐ and age‐specific hypertension rates between 1991 and 2015. Compared with females and younger generations, males and older people were more vulnerable to hypertension. Although the mechanisms for the sex disparities in hypertension are still not clear, it has been realized that sex hormones may play an important role in BP regulation. 25 Hormone replacement therapy in postmenopausal women does not significantly decrease BP levels, as determined by numerous clinical studies, suggesting that estrogens may not be the only factor contributing to BP control. 25 Instead, animal experiments found that androgens, such as testosterone, may increase BP via the renin angiotensin‐aldosterone system (RAAS). 25 , 26 In addition, the rates of unhealthy lifestyles, such as alcohol intake, overweight and obesity, and high salt intake, were higher in Chinese men than in Chinese women. 27 , 28 , 29 These factors may have resulted in a greater risk of hypertension in Chinese males. Aging is the irresistible degeneration of biological functions after tissues and organs have attained their maximal reproductive competence. 30 Vascular‐aging is associated with an impairment of blood vessel function, including increased arterial stiffness, dilation of central elastic arteries, and endothelial dysfunction. 31 On this account, nearly half of the elderly (ranging from 40.3% to 47.8%) suffered from hypertension, and about one‐sixth were stage 2 hypertension patients (ranging from 12.5% to 18.6%). As population aging progresses, the number of people with high BP, especially stage 2 hypertension, is likely to rise to a much higher level in the coming decades. 22 , 32
In line with the discovery of a large cross‐sectional study, ISH took up around a quarter of hypertension (from 22.3% in 1991 to 33.9% in 2015) and was more common in older population (ranging from 12.7% to 22.4%, OR = 40.2) in our study. 33 The predominant cause of ISH is a reduced compliance of the large elastic arteries during the aging process. 34 , 35 Previous studies have demonstrated a marked increase in arterial stiffness and aortic characteristic impedance, and elevated central pulse pressure and central SBP in ISH patients. 36 This hemodynamic features for ISH lead to a myriad of downstream effects (eg, endothelial dysfunction, increased inflammatory cytokines levels, end‐organ hypoperfusion, and activation of the RAAS and sympathetic tone), which could in turn enhance arterial stiffness and result in a worse stage of ISH if uncontrolled. 37 However, in contrast with the pattern of ISH, IDH was mainly observed in middle‐aged people (ranging from 7.1% to 9.2%, OR = 2.6). IDH was manifested as an increased DBP (DBP ≥ 90 mmHg), normal or slightly elevated SBP (SBP < 140 mmHg), and decreased pulse pressure difference. 2 There is evidence that the RAAS and vasoactive substances (eg, catecholamine) contribute to the increase of vascular resistance and, thus, the DBP levels. 38 Given that arteries in the young generation are generally in good condition, unhealthy lifestyles, such as obesity, sedentariness, alcohol consumption, and excessive intake of salt, might serve as possible contributors of IDH. 16
We discovered that higher educational attainments (OR = 0.5, 0.6, and 0.5, respectively), higher urbanization (OR = 1.7, 1.4, and 1.5, respectively), and dwelling in Southern China (OR = 0.6, 0.3, and 0.5, respectively) were related to the occurrence of ISH, IDH, and SDH. Indeed, the negative association between education degree and hypertension has been previously discussed, the possible contributors of which might be the higher knowledge or awareness of hypertension and healthier lifestyles in educated people. 5 , 6 Since the Reform and Opening in the late 1970s, rapidly expanding urbanization has sprawled out in China. Particularly, urbanization rate has marvelously increased from 26.94% in 1991 to 56.10% in 2015, with a great acceleration compared to ever before. 39 Sedentary lifestyle instead of manual labor and changes in dietary pattern, as a consequence of urbanization, may partly explain the low‐high urbanization gradient in hypertension. For the geographic variation of ISH, IDH, and SDH between Southern and Northern China, different climates, temperature degrees, air pollution, dietary compositions, and obesity rates were taken into consideration. 40 Moreover, genetics was also suggested as an essential factor for assessing this disparity by a previous study on hypertension and CVD. 41 Given the rising prevalence of hypertension, severities, and phenotypes in populations with low education, high urbanization, and residing in Southern China, critical measures, including strengthening the primary care system, scaling up education programs, and promoting diet and physical activity interventions, are needed to mitigate the CVD burden in China.
Our study extends the existing knowledge by demonstrating the associations of cardiometabolic factors with hypertension, hypertension severities, and phenotypes. We found that both general obesity and central obesity were connected with ISH (OR = 1.78 and 1.92), IDH (OR = 1.79 and 2.01), and SDH (OR = 2.47 and 2.34), as depicted in previous researches. 16 Furthermore, we revealed an association between diabetes and ISH (OR = 2.49) or SDH (OR = 1.89). Although this finding was supported by evidence from a population‐based prospective cohort study using Mendelian randomization analysis and a meta‐analysis of 49 trials, 42 , 43 the precise mechanisms for the relationship of diabetes with ISH and SDH (with elevated SBP) but not IDH (with elevated DBP) are largely unknown. Broad cardiometabolic disorders in diabetic patients, including RAAS activation, endothelial dysfunction, insulin resistance, and the elevated level of advanced glycation end products, may be responsible for the initiation and maintenance of hypertension. 44 , 45 Our study also showed that elevated TG was positively linked to ISH, IDH, and SDH, with ORs of 1.48, 1.36, and 1.76. Consistent with our outcomes, a study in Korea presented a significant role of elevated TG in predicting hypertension and CVD. 46 Tohidi et al also reported that a 1‐standard deviation increment in TG levels was correlated with a 16% increased risk of developing hypertension. 47 However, the mechanisms underlying the interaction between hypertriglyceridemia and hypertension are uncertain to date. Some studies suggest that insulin resistance and increased renal Na reabsorption play a potentially key role in obesity‐induced hypertension. 48 , 49 In this study, the elevated TC was also observed as a useful predictor for identifying SDH (OR = 1.62, 1.22‐2.14), indicating the necessity of screening for dyslipidemia in public.
However, some limitations should be noted. First, the national representativeness of CHNS could not be fully ensured, despite the large sample size and a range of economic and demographic variations. Second, several confounding factors (eg, family history, physical activity, sodium intake, and comorbidities) were not accounted for in our multivariable analyses for lack of relative information. Third, biochemical indexes, such as FPG, HbA1c, TC, LDL‐C, HDL‐C, and TG, were only detected in CHNS 2009, based on which we explored the associations between cardiometabolic factors and hypertension subtypes. This may result in a weaker statistical power when compared to the assessment of other factors (eg, sex, age, education) in this study. Fourth, the current study did not report the percentage of resistant and secondary hypertension since information on target organ damage, drug‐resistant (≥3 drugs), and comorbidities was not collected in CHNS.
In conclusion, the present study demonstrates an increasing trend in the prevalence of hypertension, hypertension severities, and phenotypes among Chinese adults over two decades. Various demographic, socioeconomic, geographic, and behavioral predictors (sex, age, urbanization, educational attainments, Southern China), as well as cardiometabolic factors (general obesity, central obesity, elevated TG levels), were associated with ISH, IDH, and SDH. Efforts for the prevention and management of hypertension are in urgent need in China.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Conceptualization, PS; methodology, PS, MZ, QY and YZ; validation, MZ, QY and YZ; formal analysis, PS, MZ, QY and YZ; writing—original draft preparation, QY; writing—review and editing, PS, XY, LH, QY; All authors have read and agreed to the published version of the manuscript.
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
This research uses data from China Health and Nutrition Survey (CHNS). We thank the National Institute for Nutrition and Health, China Center for Disease Control and Prevention, Carolina Population Center (P2C HD050924, T32 HD007168), the University of North Carolina at Chapel Hill, the NIH (R01‐HD30880, DK056350, R24 HD050924, and R01‐HD38700), and the NIH Fogarty International Center (D43 TW009077, D43 TW007709) for financial support for the CHNS data collection and analysis files from 1989 to 2015 and future surveys, and the China‐Japan Friendship Hospital, Ministry of Health for support for CHNS 2009, Chinese National Human Genome Center at Shanghai since 2009, and Beijing Municipal Center for Disease Prevention and Control since 2011.
Yi Q, Zha M, Yang Q, et al. Trends in the prevalence of hypertension according to severity and phenotype in Chinese adults over two decades (1991‐2015). J Clin Hypertens. 2021;23:1302–1315. 10.1111/jch.14306
Funding information
This research did not receive any specific grant from funding agencies in the public, commercial, or not‐for‐profit sectors
REFERENCES
- 1. Forouzanfar MH, Afshin A, Alexander LT, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016;388(10053):1659‐1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560‐2571. [DOI] [PubMed] [Google Scholar]
- 3. Collaboration NRF. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population‐based measurement studies with 19· 1 million participants. Lancet (London, England). 2017;389(10064):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population‐based studies from 90 countries. Circulation. 2016;134(6):441‐450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lu J, Lu Y, Wang X, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population‐based screening study (China PEACE Million Persons Project). The Lancet. 2017;390(10112):2549‐2558. [DOI] [PubMed] [Google Scholar]
- 6. Xi B, Liang Y, Reilly KH, Wang Q, Hu Y, Tang W. Trends in prevalence, awareness, treatment, and control of hypertension among Chinese adults 1991–2009. Int J Cardiol. 2012;158(2):326‐329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Huang J, Wildman RP, Gu D, Muntner P, Su S, He J. Prevalence of isolated systolic and isolated diastolic hypertension subtypes in China. Am J Hypertens. 2004;17(10):955‐962. [DOI] [PubMed] [Google Scholar]
- 8. Verdecchia P, Angeli F. Natural history of hypertension subtypes. Circulation. 2005;111(9):1094‐1096. [DOI] [PubMed] [Google Scholar]
- 9. Lee H, Yano Y, Cho SMJ, et al. Cardiovascular risk of isolated systolic or diastolic hypertension in young adults. Circulation. 2020;141(22):1778‐1786. [DOI] [PubMed] [Google Scholar]
- 10. Popkin BM, Du S, Zhai F, Zhang B. Cohort Profile: The China Health and Nutrition Survey—monitoring and understanding socio‐economic and health change in China, 1989–2011. Int J Epidemiol. 2010;39(6):1435‐1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. World Health Organization . Physical status: The use of and interpretation of anthropometry, Report of a WHO Expert Committee. Geneva: World Health Organization; 1995. [PubMed] [Google Scholar]
- 12. Xi B, Liang Y, He T, et al. Secular trends in the prevalence of general and abdominal obesity among Chinese adults, 1993‐2009. Obes Rev. 2012;13(3):287‐296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Control RCoCGfhpa . The Guidelines for prevention and treatment of hypertension in Chinese adults (Revised Edition 2018). Prevent Treat Cardio‐Cerebral‐Vascular Dis. 2019;19(1):1‐44. [Google Scholar]
- 14. Zhang L, Wang F, Wang L, et al. Prevalence of chronic kidney disease in China: a cross‐sectional survey. The Lancet. 2012;379(9818):815‐822. [DOI] [PubMed] [Google Scholar]
- 15. Aldiab A, Shubair MM, Al‐Zahrani JM, et al. Prevalence of hypertension and prehypertension and its associated cardioembolic risk factors; a population based cross‐sectional study in Alkharj, Saudi Arabia. BMC Public Health. 2018;18(1):1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Price AJ, Crampin AC, Amberbir A, et al. Prevalence of obesity, hypertension, and diabetes, and cascade of care in sub‐Saharan Africa: a cross‐sectional, population‐based study in rural and urban Malawi. The Lancet Diabetes & Endocrinology. 2018;6(3):208‐222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bei‐Fan Z. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults: study on optimal cut‐off points of body mass index and waist circumference in Chinese adults. Asia Pacific J Clin Nutr. 2002;11(Suppl):S685‐S693. [PubMed] [Google Scholar]
- 18. Organization WH. Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus. Diabetes Res Clin Pract. 2011;93(3):299‐309. [DOI] [PubMed] [Google Scholar]
- 19. Adults CJCoTRoGftPaToDi . The guidelines for prevention and treatment of dyslipidemia in Chinese adults (Revised Edition 2016). Chinese Circulation Journal. 2016;31(10):937‐953. [Google Scholar]
- 20. Statistics NBo . Tabulation on the 2010 population census of the People’s Republic of China. Beijing, China: China Statistics Press; 2012. [Google Scholar]
- 21. Liang K‐Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13‐22. [Google Scholar]
- 22. Guo F, He D, Zhang W, Walton RG. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol. 2012;60(7):599‐606. [DOI] [PubMed] [Google Scholar]
- 23. Kim NR, Kim HC. Prevalence and Trends of Isolated Systolic Hypertension among Korean Adults: the Korea National Health and Nutrition Examination Survey, 1998–2012. Korean Circulation Journal. 2015;45(6):492‐499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hisamatsu T, Miura K, Ohkubo T, et al. Isolated systolic hypertension and 29‐year cardiovascular mortality risk in Japanese adults aged 30‐‐49 years. J Hypertens. 2020;38(11):2230‐2236; Publish Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 25. Reckelhoff JF. Gender differences in the regulation of blood pressure. Hypertension (Dallas, Tex: 1979). 2001;37(5):1199‐1208. [DOI] [PubMed] [Google Scholar]
- 26. Reckelhoff JF, Zhang H, Granger JP. Testosterone exacerbates hypertension and reduces pressure‐natriuresis in male spontaneously hypertensive rats. Hypertension (Dallas, Tex: 1979). 1998;31(1 Pt 2):435‐439. [DOI] [PubMed] [Google Scholar]
- 27. Millwood IY, Li L, Smith M, et al. Alcohol consumption in 0.5 million people from 10 diverse regions of China: prevalence, patterns and socio‐demographic and health‐related correlates. Int J Epidemiol. 2013;42(3):816‐827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. J. Y. Study on Prevalence . Secular Trends and Health Risk of Overweight and Obesity among Chinese Adults. Beijing, China: Epidemiology and Health Statistics, Chinese Center for Disease Control and Prevention; 2013. [Google Scholar]
- 29. Yu D, He Y, Fang H, et al. Salt intake among Chinese adults in 2010–2012. Zhonghua yu fang yi xue za zhi [Chinese journal of preventive medicine]. 2016;50(3):217‐220. [DOI] [PubMed] [Google Scholar]
- 30. Veronica G, Esther RR. Aging, metabolic syndrome and the heart. Aging and Disease. 2012;3(3):269‐279. [PMC free article] [PubMed] [Google Scholar]
- 31. El Assar M, Angulo J, Vallejo S, Peiró C, Sánchez‐Ferrer CF, Rodríguez‐Mañas L. Mechanisms involved in the aging‐induced vascular dysfunction. Front Physiol. 2012;3:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Falaschetti E, Mindell J, Knott C, Poulter N. Hypertension management in England: a serial cross‐sectional study from 1994 to 2011. The Lancet. 2014;383(9932):1912‐1919. [DOI] [PubMed] [Google Scholar]
- 33. Yano Y, Stamler J, Garside DB, et al. Isolated systolic hypertension in young and middle‐aged adults and 31‐year risk for cardiovascular mortality: the Chicago Heart Association Detection Project in Industry study. J Am Coll Cardiol. 2015;65(4):327‐335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Umemura S, Arima H, Arima S, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42(9):1235‐1481. [DOI] [PubMed] [Google Scholar]
- 35. Tsai TY, Cheng HM, Chuang SY, et al. Isolated systolic hypertension in Asia. Journal of Clinical Hypertension (Greenwich, Conn). 2021;23(3):467‐474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Avolio AP, Deng FQ, Li WQ, et al. Effects of aging on arterial distensibility in populations with high and low prevalence of hypertension: comparison between urban and rural communities in China. Circulation. 1985;71(2):202‐210. [DOI] [PubMed] [Google Scholar]
- 37. Bavishi C, Goel S, Messerli FH. Isolated systolic hypertension: an update after SPRINT. The American Journal of Medicine. 2016;129(12):1251‐1258. [DOI] [PubMed] [Google Scholar]
- 38. Drummond GR, Vinh A, Guzik TJ, Sobey CG. Immune mechanisms of hypertension. Nat Rev Immunol. 2019;19(8):517‐532. [DOI] [PubMed] [Google Scholar]
- 39. National Bureau of Statistics P . China Statistical Yearbook. Beijing, China: National Bureau of Statistics P; 2019. [Google Scholar]
- 40. Huang C, Moran AE, Coxson PG, Yang X, Liu F. Potential cardiovascular and total mortality benefits of air pollution control in Urban China. Circulation. 2017;136(17):1575‐1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Koch L. Disease genetics: Under pressure ‐ genetics of hypertension. Nat Rev Genet. 2016;17(11):658‐659. [DOI] [PubMed] [Google Scholar]
- 42. Sun D, Zhou T, Heianza Y, et al. Type 2 diabetes and hypertension. Circ Res. 2019;124(6):930‐937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Brunström M, Carlberg B. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: systematic review and meta‐analyses. BMJ (Clinical research ed). 2016;352:i717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cheung BM, Li C. Diabetes and hypertension: is there a common metabolic pathway? Current Atherosclerosis Reports. 2012;14(2):160‐166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ferrannini E, Cushman WC. Diabetes and hypertension: the bad companions. Lancet. 2012;380(9841):601‐610. [DOI] [PubMed] [Google Scholar]
- 46. Kim JA, Kim SM, Choi YS, et al. The prevalence and risk factors associated with isolated untreated systolic hypertension in Korea: the Korean National Health and Nutrition Survey 2001. J Hum Hypertens. 2007;21(2):107‐113. [DOI] [PubMed] [Google Scholar]
- 47. Tohidi M, Hatami M, Hadaegh F, Azizi F. Triglycerides and triglycerides to high‐density lipoprotein cholesterol ratio are strong predictors of incident hypertension in Middle Eastern women. J Hum Hypertens. 2012;26(9):525‐532. [DOI] [PubMed] [Google Scholar]
- 48. Kotchen TA. Obesity‐related hypertension: epidemiology, pathophysiology, and clinical management. Am J Hypertens. 2010;23(11):1170‐1178. [DOI] [PubMed] [Google Scholar]
- 49. De Boer MP, Meijer RI, Wijnstok NJ, et al. Microvascular dysfunction: a potential mechanism in the pathogenesis of obesity‐associated insulin resistance and hypertension. Microcirculation (New York, NY: 1994). 2012;19(1):5‐18. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


