Abstract
The World Health Organization (WHO) Global Hearts Initiative offers technical packages to reduce the burden of cardiovascular diseases through population‐wide and targeted health services interventions. The Pan American Health Organization (PAHO) has led implementation of the HEARTS in the Americas Initiative since 2016. The authors mapped the developmental stages, barriers, and facilitators to implementation among the 371 primary health care centers in the participating 12 countries. The authors used the qualitative method of document review to examine cumulative country reports, technical meeting notes, and reports to regional stakeholders. Common implementation barriers include segmentation of health systems, overcoming health care professionals' scope of practice legal restrictions, and lack of health information systems limiting operational evaluation and quality improvement mechanisms. Main implementation facilitators include political support from ministries of health and leading scientific societies, PAHO's role as a regional catalyst to implementation, stakeholder endorsement demonstrated by incorporating HEARTS into official documents, and having a health system oriented to primary health care. Key lessons include the need for political commitment and cultivating on‐the‐ground leadership to initiate a shift in hypertension care delivery, accompanied by specific progress in the development of standardized treatment protocols and a set of high‐quality medicines. By systematizing an implementation strategy to ease integration of interventions into delivery processes, the program strengthened technical leadership and ensured sustainability. These study findings will aid the regional approach by providing a staged planning model that incorporates lessons learned. A systematic approach to implementation will enhance equity, efficiency, scale‐up, and sustainability, and ultimately improve population hypertension control.
Keywords: cardiovascular disease, hypertension, implementation science, Latin America and the Caribbean, non‐communicable diseases
1. INTRODUCTION
In 2016, in the World Health Organization (WHO) Region of the Americas, 5.5 million deaths were caused by non‐communicable diseases (NCD), of which 2.2 million deaths occurred in people under the age of 70 years. 1 Of the total NCD mortality, 28.1% were due to cardiovascular diseases (CVD), 2 and, now, after several years of notable reductions, CVD rates are leveling off or rising in several countries. 3 This situation has a significant negative economic and social impact. Therefore, any meaningful reduction in NCD mortality must tackle CVD more effectively.
To catalyze the reduction of the CVD burden, the WHO launched the Global Hearts Initiative in 2016. The initiative presents a set of technical packages to manage and control CVD and its risk factors at population and health services levels. The population‐level technical packages present steps to reduce the behavioral risk factors for CVD through legislative and preventive measures. 4 The health services technical package, HEARTS, provides a framework and the standards of clinical practice that are critical to guiding CVD interventions specifically for hypertension using the total CVD risk approach management including a recent module on diabetes. HEARTS stands for Healthy‐lifestyle counseling, Evidence‐based treatment protocols, Access to essential medicines and technology, Risk‐based CVD management, Team‐based care, and Systems for monitoring. 5
Given that hypertension is the main attributable factor for over 60% of all deaths due to CVD (mainly ischemic heart disease and stroke) in the Americas, its control is paramount to have a substantial effect on reducing both the CVD and the NCD burden. 6 , 7 , 8 The reality confronted by most of the countries in Latin America and the Caribbean, similar to the global situation, is very high prevalence of hypertension combined with very low levels of awareness, treatment, and control of hypertension within health systems poorly designed to respond to the rising demands of chronic conditions. 9 , 10 , 11 , 12 The application of the Global Hearts initiative through its regional adaptation, the HEARTS in the Americas, focuses on the full implementation of the HEARTS technical package using hypertension, as the entry point into the health system at primary care level to operationalize concrete interventions. The implementation of the HEARTS technical package is supported by a set of strategic technical pillars (Figure 1) designed to strength and catalyze the implementation.
FIGURE 1.
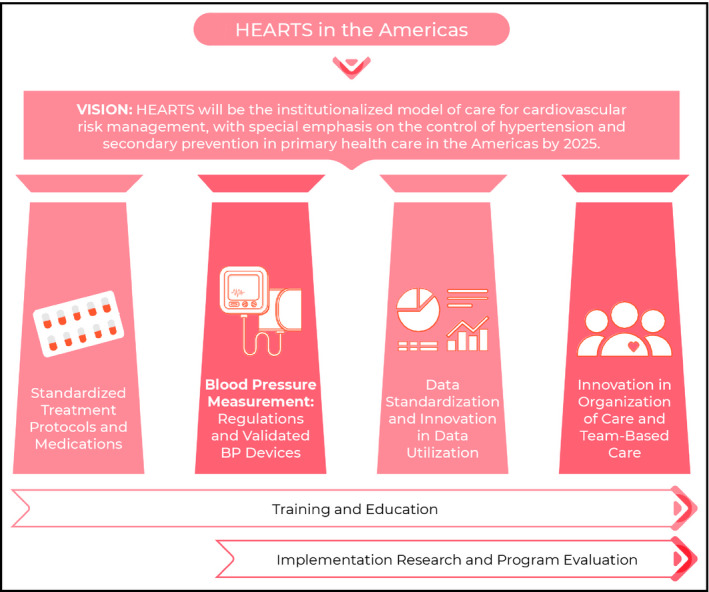
HEARTS in the Americas vision, technical pillars, and cross‐cutting implementation strategies
Due to the diverse social, political, and cultural landscape, health systems, and available resources of the countries and communities where HEARTS is applied, several challenges to implementation arise. Therefore, using implementation science to guide the HEARTS in the Americas Initiative advances the aim of reaching the population, as well as patients and health care providers, to affect health system organizational change and effectively impact the burden of CVD. Implementation science is the study of the methods and processes that take evidence‐based interventions into routine practice settings. This approach has emerged to identify potential solutions to amplify the execution of evidence‐based interventions. 13 , 14 , 15
In this paper, we aim to reconstruct an implementation model based on input provided by local implementers from countries, and by HEARTS in the Americas senior consultants from different countries and institutions. We map stages of country implementation onto an existing model and then describe the early barriers, facilitators, and lessons learned to implementation in countries.
2. METHODS
HEARTS in the Americas is a new initiative and the knowledge base of implementation and publications from country experiences is emerging but limited. 16 An exploratory qualitative approach is therefore an appropriate methodology to clarify conceptual and applied aspects of implementation. A document review, as described in the literature, 17 , 18 is a form of qualitative review in which relevant documents are interpreted on a specific topic and is a method to organize diverse materials over a short period into a cohesive narrative. Four years into implementation, various documents on the Global Hearts and HEARTS in the Americas offer a rich source of information on the uptake, implementation, and lessons learned. Thus, the document review for this study was a means to source background information and reconstruct implementation pathways by reviewing existing documents during the onset of the Initiative. In a document review, the documents may be internal to a program or organization or external such as published articles. 18 The first, an inventory of potential documents, in English and Spanish, included all publicly available materials produced and available on WHO web sites (https://www.who.int/cardiovascular_diseases/global‐hearts/en/) and PAHO HEARTS web site (https://www.paho.org/en/hearts‐americas). A second inventory was created with PAHO implementing countries' reports; and thirdly, a small set of published peer‐reviewed articles selected based on an explicit mention or reference to the Global Hearts Initiative, HEARTS in the Americas Initiative, or, its predecessor, the Standardized Hypertension Treatment Project. 9 The articles were then assessed for relevance if they mentioned rolling out of the initiative, conceptual aspects, components of the initiative, and/or operational guidance. HEARTS is in its early stages, articles used to introduce the Initiative by implementers were included and existed in the program's internal library. The resulting 23 primary documents were examined through inductive analysis. Appendix S1 (See Supplementary Materials) provides the inventory of program documents (6), country reports (10), and articles (7) used for this analysis.
The resulting themes from the document review were contextualized considering relevant literature on implementation science and scale‐up. 13 , 14 , 15 From the materials reviewed, the main themes that emerged were the contexts of implementation—specifically, where is the implementation occurring and at which level. The simultaneous application at coexisting multiple levels follows a staged model of implementation. Defining the stages and its corresponding implementation elements contextualizes common challenges and solutions.
We mapped the results on a model presented in the USAID Maternal and Child Program Survival Scale‐Up Coordinator's Manual 19 , 20 which describes the main stages of scale‐up. Therefore, the results were analyzed according to five stages of implementation: assess, develop, introduce, early expand, and mature expand. 20 We chose a scale‐up model to display our results because the implementation of a multi‐country program within those country's national health systems implies a scale‐up process. Past implementation and scale‐up of large, public health initiatives show that even if there is a strong will to scale‐up immediately, rolling out in waves that encompass incrementally larger geographic areas allows for opportunities for review and adaptation to keep the process on track. 19 , 21
3. RESULTS
The HEARTS Initiative in the Americas is in its fourth year of implementation. As part of the Standardized Hypertension and Treatment Program, in early 2014, a proof of concept was piloted in Barbados, followed by three country cohorts with an initial implementation rollout at the end of 2016 in Chile, Colombia, and Cuba. In 2018, the second cohort composed by Argentina, Ecuador, Panama and Trinidad and Tobago started and, 2019, Dominican Republic, Mexico, Peru, and Saint Lucia started implementation. Currently, Ministries of Health across 12 countries are implementing the program in 371 heterogeneous primary health care centers (PHCs) (of which 288 reported data at midpoint 2020). Table 1 shows an increasing number of PHCs implementing the HEARTS program, number of persons with hypertension in the registry, and percent of coverage. Coverage rate is defined as the percent of persons with hypertension in the registry and in pharmacological treatment based on the best estimate of prevalence for the catchment area. The source of data are the primary health care center registries which are a fundamental pillar of the HEARTS implementation.
TABLE 1.
Number of primary health care centers implementing the HEARTS technical package and program coverage a by countries, 2020
| Cohort | Country (Implementation starting year) | Numbers of HEARTS Implementing Primary Health Care Centers | Total population in catchment area | Adult population in the catchment area | Number of persons with hypertension in the registry | Coverage rate baseline | Coverage rate by March 2020 | |
|---|---|---|---|---|---|---|---|---|
| At baseline | At last evaluation | |||||||
| Cohort 1 | Barbados | 2 | 4 | 94 300 | ||||
| 2015 | ||||||||
| Colombia | 2 | 13 | 499 326 | 261 385 | 45 185 | 35% | 58% | |
| 2017 | ||||||||
| Chile | 2 | 79 | 1 850 970 | 1 446 624 | 185 759 | 48% | 46% | |
| 2017 | ||||||||
| Cuba | 1 | 20 | 565 499 | 401 056 | 65 832 | 52% | 69% | |
| 2017 | ||||||||
| Cohort 2 | Trinidad & Tobago | 5 | 14 | 381 041 | 238 051 | 12 527 | 31% | 33% |
| 2018 | ||||||||
| Ecuador | 10 | 30 | 662 448 | 412 265 | 7719 | 5% | 9% | |
| 2018 | ||||||||
| Argentina | 5 | 13 | 132 106 | 77 440 | 5602 | 22% | 21% | |
| 2018 | ||||||||
| Panamá | 7 | 37 | 570 994 | 630 195 | 52 872 | 21% | 38% | |
| 2018 | ||||||||
| Cohort 3 | Saint Lucia | 6 | 6 | 33 423 | 23 819 | 1406 | 19% | 21% |
| 2019 | ||||||||
| Peru | 34 | 34 | 720 597 | 486 058 | 7655 | 5% | 8% | |
| 2019 | ||||||||
| Dominican Republic | 26 | 18 | 70 296 | 41 169 | 5292 | 32% | 43% | |
| 2019 | ||||||||
| Mexico | 20 | 20 | 420 624 | 185 849 | 3606 | 10% | 8% | |
| 2019 | ||||||||
| Totals | 120 | 288 | 5 907 324 | 4 298 211 | 393 455 | |||
Source: Ministries of Health of corresponding countries.
Coverage: Percent of persons with hypertension in the registry and in pharmacological treatment based on the best estimate of prevalence for the catchment area.
The deductive analysis of implementing countries' reports describes on an institutional level how implementation unfolded and factors that facilitated through the implementation pathway. The following describes the nested multi‐levels of HEARTS implementation, then a reconstruction of the implementation pathway based on an adaptation of an existing model and, finally, a description of the facilitators, barriers, and solutions identified in the early implementation experience of HEARTS in the Americas.
3.1. Main actors and roles at the multi‐levels of the HEARTS Initiative in the Americas
HEARTS is a set of complex, multi‐level interventions containing several interacting components, delivered and received by individuals and communities as well by health providers and health facilities with different level of organization and resources. The technical package is a tool that guides and trains health care professionals, at PHCs, to screen, diagnose, treat, and monitor individuals with hypertension and encourage the adoption of management changes based on systems for monitoring at every level of implementation. The landscape of implementation unfolded within nested multi‐levels, where institutions are embedded within an encompassing overarching environment with existent formal linkages. These institutions at different levels operate with increasingly clear demarcation of stakeholders and roles. The variety of institutions organizations and individuals engaged in HEARTS in the Americas, at multiple and nested levels, is as depicted in Figure 2.
FIGURE 2.
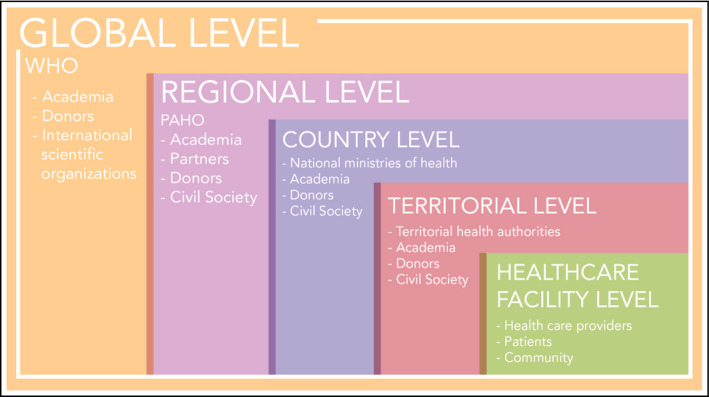
Nested multi‐level nature of HEARTS in the Americas
Responsibilities for HEARTS vary across levels and institutions. At the global level, WHO, along with international partners, including PAHO, compiled the best global practices and packaged them in modules that provide clinical guidance and direction. At the regional level, PAHO develops a comprehensive strategy for implementation which includes technical assistance to customize the HEARTS technical package to the country context and support to catalyze change based on a robust set of technical pillars, educational and training strategies, and the promotion of implementation science.
Pan American Health Organization works closely with each country Ministry of Health (MoH) and PAHO country‐based office to disseminate the intervention to reach a critical mass of countries in the region. MoH formally plan national scale‐up within their country and execute its implementation. At the provincial/state level, the health authorities directly conduct and supervise the implementation. And at the individual health center level, the smallest units of primary care provision in each health system, the primary health care leadership ensures teams are trained on the clinical and managerial strategies and delivery of the interventions within the health care centers working with the community, patients, and caregivers.
3.2. Staged model for implementation
Grounded in the chronic care model, PAHO's implementation strategy utilizes hypertension management as an entry point to care delivery at the primary health care level of countries. The introduction, rolling out, and adoption of the HEARTS model and its technical packages responds to two main factors: (a) PAHO's overarching implementation strategy and (b) the country's commitment and capacity to adapt and implement within the context of its health system. Therefore, implementation progress does not occur linearly, rather it is an iterative dynamic staged process. This iterative nature transpires in stages (Figure 3), which is the framework in which HEARTS is being implemented. The phasic‐cyclic process of implementation is occurring inside each country at different paces as displayed in Figure 4. After every cycle of implementation, the process has become more systematic allowing to gain experiences, partners, refine engagement with health leaders, and target technical support more directly to ministry officials.
FIGURE 3.
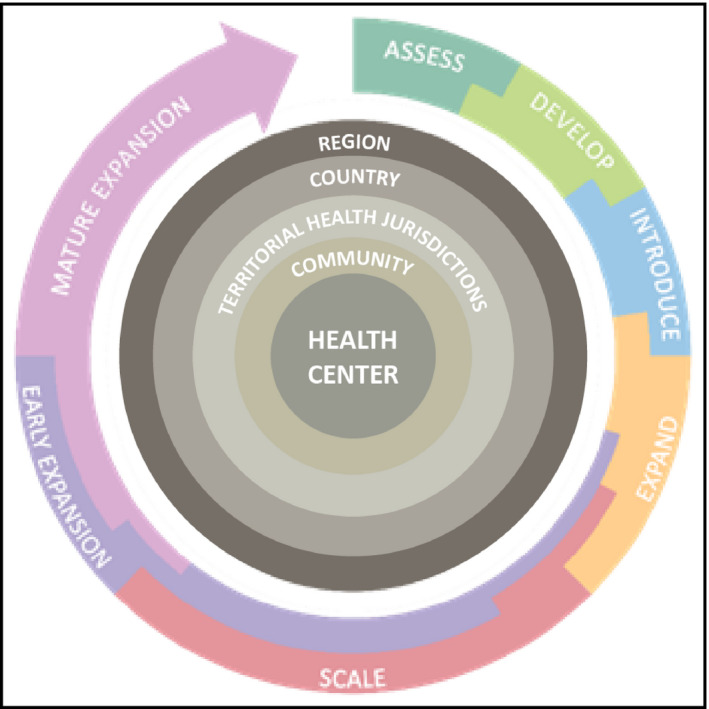
The modified stages model shown in cyclic format; adapted from innovation to full scale, leading to sustainable impact at scale from the USAID, Supporting Country‐Led Efforts to Systematically Scale‐Up and Sustain Reproductive, Maternal, Newborn, Child
FIGURE 4.
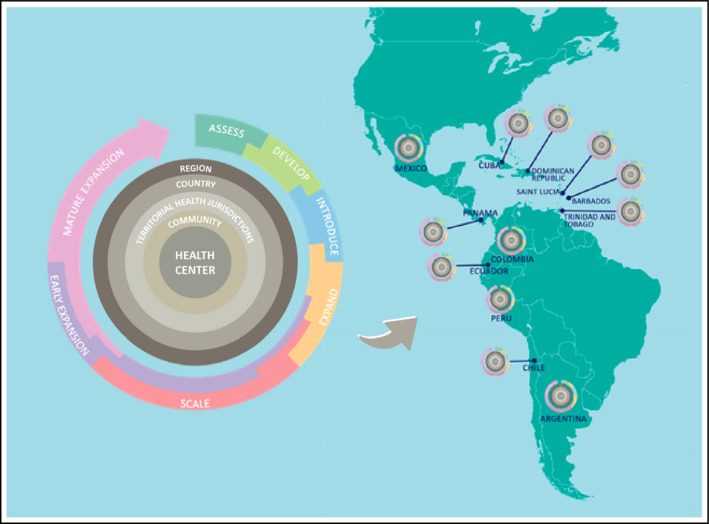
A cyclical, reiterative depiction of staged model of implementation occurring at every country implementing the HEARTS in the Americas Initiative
3.3. Description of stages of implementation of HEARTS in the Americas
3.3.1. Stage 1: Assess
The first stage is defining the health problem. The fundamental epidemiological problem of high mortality due to NCDs and CVD, and the key contributing role of hypertension, is solidly defined for the region and the problem is well documented in each country. Nonetheless, PAHO facilitates a review and analysis process using local data and reports for each country to generate attention at the political level. Higher awareness and a refined understanding of hypertension by measuring gaps in awareness, treatment, and control, and assessing the health infrastructure, and human and financial resources together evaluate the country and local capacity to respond. This assessment provides the platform for implementing HEARTS, by demonstrating that hypertension control is key to reducing CVD and creating political traction presenting the gaps as opportunities for improvement.
3.3.2. Stage 2: Develop
With PAHO's technical cooperation, in collaboration with international consultants and partners from the US Centers for Disease Control and Prevention (CDC), Taskforce for Global Health, the World Hypertension League (WHL), Inter‐American Society of Cardiology (IASC), Latin American Society of Hypertension (LASH) and Resolve to Save Lives (RTSL), among others, the HEARTS implementing countries have adapted the technical package to their unique context, while preserving the core standardized evidence‐based interventions.
3.3.3. Stage 3: Introduce
Pan American Health Organizations approach to country engagement is a critical step and planned in coordination with PAHO country offices. Countries are selected based upon their state of readiness, as indicated by strong political will and maturity of the health system, and their contribution to geographical diversity, drawn from the sub‐regions to have full representation and to facilitate the further expansion across neighboring countries. During four years of implementation, the introduction of HEARTS to MoH has become progressively more systematic. For example, the engagement of PAHO country offices has strengthened and HEARTS is increasingly incorporated into high‐level government strategic planning, including collaborative agreements with PAHO. Simultaneously, PAHO has gained consensus with scientific societies, allowing for a warmer reception of the initiative by health professionals at different levels of the health system. This dual engagement is also an attempt to create opportunities for national decrees or legislation, and to avoid programmatic vulnerabilities due to changing governments. Once the MoH agree to participate and designate a national coordination team, consisting of national and local representatives and main stakeholders including health services delivery personnel, then a geographical area or several geographical areas are selected based on a set of criteria for rollout of elements of the package.
3.3.4. Stage 4: Expand—early phase
Early in the expansion stage, the HEARTS technical package starts to harmonize with existing public health policies and programs and regulatory environment. A centerpiece of the early expansion is the role of in‐country coordinators both at MoH level and PAHO country offices, who lead the project by engaging key stakeholders and champions, building the implementation teams, coordinating training, holding regular data review meetings with participating health centers, and promoting the program. A pool of international technical experts is engaged in this phase to build capacity and constant coordination is present between PAHO and the HEARTS focal point. Given that the ultimate goal is full national implementation, the technical package is initiated where scale‐up is most attainable and feasible based on existing infrastructure.
In this stage, countries define a national plan and scalable units to ensure expansion at a manageable rate in the country. For example, the first set of scalable units could be a set of health centers that cover at least 100 000 population (based on country size, this recommendation is higher in larger countries or lower in the small countries) in the very initial wave of implementation which helps implementers to plan out how quickly the program can be scaled‐up. Additionally, PAHO encourages learning and information exchange within and among countries in the HEARTS network by bringing country coordinators or other consultants to share their perspective and commonality with the on‐the‐ground experience. Endorsement and adoption of the HEARTS model into the country's public health policy instruments are signs of early expansion. Notably, Chile, Colombia, Cuba, Panama and Trinidad and Tobago have incorporated the HEARTS technical package through the introduction of ministerial decrees, public health laws and regulations, and national clinical practice guidelines.
3.3.5. Stage 5: Expand—Mature phase
This is the ultimate stage of the scale‐up process when the interventions are fully adopted and are institutionalized within the delivery system. Because HEARTS has been in existence for less than 4 years, no country is currently at this stage. As countries advance in institutionalizing HEARTS and it becomes sustainable, PAHO continues to provide technical cooperation to assist countries to advance to the mature expansion stage.
Finally, an iterative staged model helps to situate main facilitators, barriers, and lessons learned. Table 2 presents a summary of key lessons learned from the implementation experience of HEARTS in the Americas followed by facilitators and barriers.
TABLE 2.
Summary of key lessons
| Theme | Lesson |
|---|---|
| Secure political support | The critical role of the MoH and the local authorities to implement and sustain a comprehensive program such as HEARTS in the Americas. MoH and the public health local authorities have the primary responsibility to manage and finance primary health care. |
| Shift health care provider roles | A paradigm shift is needed to change lead provider of CVD/ hypertension programs from the very specialized, secondary level of care to primary health care. Advocating for legislative changes to move away from physician‐centered to person‐centered health care, as well as training the new generation of leaders and health care staff to carry forward new roles and responsibilities. |
| Systematize implementation strategies | Systematizing the methodology of engagement, pre‐implementation, implementation, sustainment, and institutionalization facilitates the provision of technical assistance to each country following its stage of development within the continuum of adoption of HEARTS. |
| Provide strong technical leadership | Strong technical leadership is fundamental to engage, advise, and accompany the process of adoption. |
| Understand local organizational structures | Deep understanding of the culture, organizational structures of the health systems is prerequisites to interacting with the MoH. |
| Recruit and retain field champions | Recruiting strong recognized leaders—and upcoming new leaders—in the field of cardiovascular health, and forming strong alliances with scientific societies has proven an important ingredient to success. |
| Cultivate technical leadership | Cultivating in‐country technical leadership, particularly from underrepresented backgrounds (eg, class, race/ethnic, sex), is as important as obtaining and sustaining political will. |
3.4. Common facilitators across countries
At the national level, political support at the highest administrative level has been fundamental. Because HEARTS in the Americas Initiative is a concrete set of evidence‐based interventions, it provided an implementation pathway adaptable within a health system, which has contributed to quick uptake at the political level. For instance, the great majority of health ministers and senior authorities have participated personally in HEARTS events and have shown tangible support, the most significant being the designation of a national MoH focal point for HEARTS, officers with high‐level positions.
Secondly, a partnership with scientific and professional societies promotes wide acceptance of HEARTS by practicing clinicians who are involved at different implementation levels. Most countries report that their national scientific societies, such as the cardiology and hypertension‐related societies, are supportive and active in HEARTS. Leaders from the societies participate in activities such as developing the hypertension treatment protocol, master classes, and train‐the‐trainer sessions at regional and national level. The treatment protocol development process also acts as a convening strategy for stakeholders, generating inter‐programmatic and inter‐sectorial collaboration among clinicians, researchers, various MoH divisions, and medicine supply and procurement leaders. Engaging stakeholders of health systems allows them to manage built‐in incentives, creating an environment with greater receptivity for the interventions. The overarching facilitator for health systems stakeholder uptake has been the simplicity and pragmatic nature of a technical package that is solidly grounded in scientific evidence.
3.5. Common main barriers and solutions
A common barrier was the complexity introduced by the wide range of health information systems within countries, ranging from paper‐based record keeping to national electronic health records with unique identifiers, with a plethora of subsystems in between. Few countries have a single, interoperable, national information health system, although a number have independent, and incompatible data collecting systems operating within care delivery systems. As a result, most countries lack a functional data collection and reporting mechanism to demonstrate progress and identify areas for potential improvement. A second major barrier has been the updating of national essential medications lists (formularies) which are medications guaranteed by the MoH for the public health system—which lacked long‐acting antihypertensive and fixed‐dose medications. As a result, patients may not have access to medications and experience difficulties to adhere to treatment leading to uncontrolled hypertension. Another barrier was a weak and fragmented regulatory landscape to oversee validation of automated blood pressure monitors. Beyond the infrastructural limitations, most countries lack health system performance evaluation and quality improvement processes, and do not have built‐in incentives for improvement, particularly at the primary health care level.
Resistance to change coupled with competing priorities and limited or differing technical capacity at MoH is noted as a common obstacle for implementers. Resistance is present at different levels, for example, specialists in secondary and tertiary health centers are reluctant to adopt treatment protocols and standardizing treatment. This type of resistance initially caused delays in implementation in many countries. A solution is the provision of strong scientific evidence for initiating pharmacological therapy early, and strongly encouraging the adoption of combination therapy to progressively increase the use of fixed‐dose combination therapies.
Task‐sharing was another common hurdle where the health care team was not accustomed to changing roles and responsibilities in managing chronic care conditions. In most countries, most tasks related to hypertension control are considered to be mainly the responsibility of the physician. Compounded by countries having a physician‐centered health system, underpinned by local legislation, often limits the extent to which task shifting can occur. To counteract this barrier, technical assistance to implementers to define roles of the health care team, improve the availability of training and re‐training of personnel, and continuous support to staff. High staff turnover is a reality across all public health services; thus, HEARTS is counteracting this barrier by placing great importance on cultivating technical leadership and widespread training activities for primary care teams. Additionally, lower technical capacity in the area of health economics and economic analyses prevents decision‐making based on cost‐effectiveness of applied changes to managerial, staffing, and monitoring activities.
4. DISCUSSION
4.1. Overview of programmatic premises
The HEARTS in the Americas Initiative is a vehicle to catalyze technical cooperation from multilateral and international health organizations to the countries. It is an initiative of the countries, led by their MoH, with the active participation of local stakeholders with the technical cooperation of PAHO. The Initiative seeks to integrate seamlessly and progressively into existing health delivery systems to adopt global best practices in the prevention and control of CVD utilizing hypertension control as an entry way. It aims to improve the performance of the services through better control of high blood pressure and the promotion of secondary prevention with emphasis on primary health care. HEARTS in the America is not a vertical program. It is intended to be the model for cardiovascular disease risk management, including hypertension, diabetes, and dyslipidemia in primary health care in the region by 2025. While anchored in the evidence and the subject of ongoing data analysis and evaluation, HEARTS in the Americas was not designed as an academic implementation study nor as a research trial. It is an ongoing, evolving, continuous quality improvement public health program and model of care.
4.2. Facilitators for implementation
A number of factors created an auspicious environment for MoH to secure their commitment to implementation, among them the flexibility to adapt to unique local conditions. The adaptability signifies that guidance is provided; however, the implementation pathway is developed within each country rather than constricting a pre‐conceived one‐size‐fits‐all pathway. The implementation is solidly grounded on interventions that are concrete and based on scientific evidence. Coupled together, PAHO's approach in engaging MoH officials and professional societies and provision of technical assistance became more systematic over time. The staging model and early results show the first cohort of countries at a more advanced stage by incorporating the interventions in health care delivery and have higher number of registered patients with treatments based on standardized treatment protocols, but the second and third cohort are progressing more rapidly.
Understanding the sensitive nature of changing the practice in the primary health care level, PAHO collaborated with countries and consultants to create a step‐by‐step methodology to develop and implement a standardized hypertension treatment protocol. This facilitates a seamless transition from existing treatment practices (current protocols) to best practice (preferred protocols), built around a core set of ideal antihypertensive medications. 22 Likewise, based on a quantitative and qualitative analysis of laws and regulations on the accuracy of Blood Pressure Measurement Devices (BPMD) in 13 countries in Latin America and the Caribbean, 23 HEARTS in the Americas is working toward the adoption of a regulatory framework that guarantees the progressive exclusive use of validated automatic BPMDs along with the promotion of the best practices for accurate BP measurement.
4.3. Programmatic sustainability
Unlike some previous international projects and pilots terminated prior to institutionalization or sustainability, 24 HEARTS is meant to be institutionalized. In a context of very complex political scenarios, programs often stop when external funds expire. This flawed model of technical cooperation may create a contradictory set of expectations for MoH regarding implementation and sustainability pathways. HEARTS in the Americas accomplish six actions that foster scale‐up and sustainability by inherently designing the program for scale, generating evidence to inform scale‐up through the monitoring system, engaging influential individuals through MoH officials and professional societies, maintaining an agile implementation pathway responsive to change, and allowing country ownership by aligning with the country's priorities. 24
Country MoH are often inherently large and complex institutions, with limited resources and a huge agenda and competing priorities, that are resistant to change. As an implementation coordinating entity, PAHO acts as a catalyst in the regional implementation process, allowing for a relatively rapid spread of the Initiative in collaboration with MoH. A partnership between PAHO, MoH, and stakeholders engenders collective action and creates the space for gaining political will which is fundamental for institutionalized and sustainable change. This type of multi‐disciplinary, cross‐collaboration within, across, and beyond ministries promotes a shared sense of ownership, facilitates continued multisector support, and creates the environment needed to prevent, manage, and control NCDs.
4.4. Limitations
The limitations of this study are inherent to qualitative studies in general. The document review provided insight on the stages of implementation and the challenges, solutions, and facilitators the countries are experiencing; however, triangulation of information sources is needed. Alternative methods may have accounted for experiences that were not included in the reports and documents. Further implementation science studies are needed to examine differences in health systems (centralized compared to decentralized) and the ease of uptake of improvements in health systems. Finally, the study is not designed to link changes to outcome data such as rates of hypertension control and coverage to implementation.
5. CONCLUSION
Utilizing an implementation science lens to examine the unfolding of the HEARTS in the Americas allows us to identify factors, processes, and methods that support the successful integration of evidence‐based interventions within routine practices in PHCs to achieve the goals of reducing CVD and NCD burden. This paper sought to reconstruct an iterative staged model of implementation that applies a systematic approach to the scale‐up of HEARTS in the Americas. Given its complexity, a staged approach to implementation that is iterative and simultaneously occurring at several levels corresponds to the natural course of development of the Initiative. The identification of early barriers and facilitators through the qualitative approach offers a departure point for planning, monitoring, and evaluation for new implementing sites and countries. Key lessons learned from the first four years of implementation include the centrality of commitment and support from stakeholders within the MoH and on‐the‐ground technical leaders and champions. The capacity to engage early with key stakeholders with deep understanding of the local organizational context was another key lesson that allowed for an agile implementation pathway and initiated a paradigm shift for hypertension care delivery. And cultivating in‐country technical leadership at all levels of implementation has proven essential due to the high turnover of staff. From an implementation science perspective, some clarifying concepts such as situating the HEARTS implementation within nested multi‐levels and clarification of roles of corresponding actors may be useful to contribute building the knowledge base of a chronic disease management model scale‐up. It can assist in the ongoing construction of new paradigm of a public health model focused on CVD.
CONFLICT OF INTEREST
None.
AUTHOR CONTRIBUTIONS
GPG and PO were responsible for substantial contributions to the conception, design of the work, the data acquisition and analysis. GPG, KJ and PO prepared the first draft. All authors (GPG, KJ, PLJ, MHO, SYA, NRCC, KC, DJD, MCE, YVG, MGJ, TM, JM, PLJ, MHO, PO) were responsible for interpretation of data for the work and revising it critically for important intellectual content, providing final approval of the version to be published. And all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
DISCLAIMERS
GPG, MCE, TM and PO are staff members of the Pan American Health Organization. The authors alone are responsible for the views expressed in this publication, and they do not necessarily represent those of the Pan American Health Organization. KJ is a staff member of the US Centers for Disease Control and Prevention. The findings and conclusions in this report are those of this author and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Supporting information
Appendix S1
ACKNOWLEDGMENTS
This analysis was supported by Bloomberg Philanthropies and Resolve to Save Lives, an initiative of Vital Strategies, through a grant to the National Foundation for the Centers for Disease Control and Prevention Inc (CDC Foundation). Resolve to Save Lives is funded by grants from Bloomberg Philanthropies; the Bill and Melinda Gates Foundation; and Gates Philanthropy Partners, which is funded with support from the Chan Zuckerberg Foundation. We would also like to acknowledge the support of the mentorship collaboration consisting of the US Centers for Disease Control and Prevention, Resolve to Save Lives, World Hypertension League, and Lancet Commission on Hypertension Group.
REFERENCES
- 1. Pan‐American‐Health‐Organization . NCDs at a glance: NCD mortality and risk factor prevalence in the Americas: Pan‐American‐Health‐Organization; 2019. [Google Scholar]
- 2. Pan‐American‐Health‐Organization & World‐Health‐Organization . Evidence and intelligence for action in Health Department/Health analysis, metrics and evidence unit. PLISA Database. Core Indicators 2019: Health Trends in the Americas: World‐Health‐Organization ; 2019. [Google Scholar]
- 3. Martinez R, Soliz P, Mujica OJ, et al. The slowdown in the reduction rate of premature mortality from cardiovascular diseases puts the Americas at risk of achieving SDG 3.4: a population trend analysis of 37 countries from 1990 to 2017. J Clin Hypertens. 2020;22(8):1296‐1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World‐Health‐Organization . Global Hearts Initiative, working together to promote cardiovascular health. https://www.who.int/cardiovascular_diseases/global‐hearts/en/. Published 2020. Accessed.
- 5. World‐Health‐Organization . Hearts: technical package for cardiovascular disease management in primary health care: World‐Health‐Organization; 2016. [Google Scholar]
- 6. Campbell NRC, Schutte AE, Varghese CV, et al. Sao Paulo call to action for the prevention and control of high blood pressure: 2020. J Clin Hypertens (Greenwich). 2019;21(12):1744‐1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lloyd‐Sherlock P, Ebrahim S, Martinez R, McKee M, Ordunez P. Reducing the cardiovascular disease burden for people of all ages in the Americas region: analysis of mortality data, 2000–15. Lancet Glob Health. 2019;7(5):e604‐e612. [DOI] [PubMed] [Google Scholar]
- 8. Martinez R, Lloyd‐Sherlock P, Soliz P, et al. Trends in premature avertable mortality from non‐communicable diseases for 195 countries and territories, 1990–2017: a population‐based study. Lancet Glob Health. 2020;8(4):e511‐e523. [DOI] [PubMed] [Google Scholar]
- 9. Patel P, Ordunez P, DiPette D, et al. Improved blood pressure control to reduce cardiovascular disease morbidity and mortality: the standardized hypertension treatment and prevention project. J Clin Hypertens (Greenwich). 2016;18(12):1284‐1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ordunez P, Martinez R, Niebylski ML, Campbell NR. Hypertension prevention and control in Latin America and the Caribbean. J Clin Hypertens (Greenwich). 2015;17(7):499‐502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Olsen MH, Angell SY, Asma S, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. Lancet. 2016;388(10060):2665‐2712. [DOI] [PubMed] [Google Scholar]
- 12. Lamelas P, Diaz R, Orlandini A, et al. Prevalence, awareness, treatment and control of hypertension in rural and urban communities in Latin American countries. J Hypertens. 2019;37(9):1813‐1821. [DOI] [PubMed] [Google Scholar]
- 13. World‐Health‐Organization & ExpandNet . Nine steps for developing a scaling‐up strategy: World‐Health‐Organization; 2010. [Google Scholar]
- 14. Damschroder L. Clarity out of chaos: use of theory in implementation research. Psychiatry Res. 2020;283:e112461. [DOI] [PubMed] [Google Scholar]
- 15. Rapport F, Clay‐Williams R, Churruca K, Shih P, Hogden A, Braithwaite J. The struggle of translating science into action: foundational concepts of implementation science. J Eval Clin Pract. 2018;24(1):117‐126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Valdes Gonzalez Y, Campbell NRC, Pons Barrera E, et al. Implementation of a community‐based hypertension control program in Matanzas, Cuba. J Clin Hypertens (Greenwich). 2020;22(2):142‐149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bowen GA. Document analysis as a qualitative research method. Qual Res J. 2009;9(2):27‐40. [Google Scholar]
- 18. U.S.‐Department‐of‐Health‐and‐Human‐Services‐Centers‐for‐Disease‐Control‐and‐Prevention‐CDC . Data collection methods for evaluation: document review. Evaluation Briefs. 2018;18.
- 19. USAID . Supporting Country‐led efforts to systematically scale‐up and sustain reproductive, maternal, newborn, child and adolescent health interventions. Scale‐up Coordinator's Guide; 2020.
- 20. Smith JM, de Graft‐Johnson J, Zyaee P, Ricca J, Fullerton J. Scaling up high‐impact interventions: How is it done? Int J Gynaecol Obstet. 2015;130:S4‐S10. [DOI] [PubMed] [Google Scholar]
- 21. Massoud MR, Mensah‐Abrampah N. A promising approach to scale up health care improvements in low‐and middle‐income countries: the Wave‐Sequence Spread Approach and the concept of the Slice of a System. F1000Res. 2014;3:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. DiPette D, Goughnour K, Zuniga E, et al. Standardized treatment to improve hypertension control in primary health care: the HEARTS in the Americas initiative. J Clin Hypertens (Greenwich). 2020;22(12):2285–2295. 10.1111/jch.14072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lombardi C, Sharman JE, Padwal R, Ordunez P. Weak regulatory frameworks on automated blood pressure measuring devices pose a major impediment for the implementation of HEARTS in the Americas and hypertension control. J Clin Hypertens (Greenwich). 2020;22(12):2184–2191. 10.1111/jch.14058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Spicer N, Hamza YA, Berhanu D, et al. 'The development sector is a graveyard of pilot projects!' Six critical actions for externally funded implementers to foster scale‐up of maternal and newborn health innovations in low and middle‐income countries. Global Health. 2018;14(1):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1


