Abstract
Objective
The 2020 coronavirus disease 2019 (COVID-19) pandemic resulted in state-specific quarantine protocols and introduced the concept of social distancing into modern parlance. We assess the impact of the COVID-19 pandemic on neurotrauma presentations in the first 3 months after shutdown throughout Pennsylvania.
Methods
The Pennsylvania Trauma Systems Foundation was queried for registry data from the Pennsylvania Trauma Outcomes Study between March 12 and June 5 in each year from 2017 to 2020.
Results
After the COVID-19 shutdown, there was a 27% reduction in neurotrauma volume, from 2680 cases in 2017 to 2018 cases in 2020, and a 28.8% reduction in traumatic brain injury volume. There was no significant difference in neurotrauma phenotype incurred relative to total cases. Injury mechanism was less likely to be motor vehicle collision and more likely caused by falls, gunshot wound, and recreational vehicle accidents (P < 0.05). Location of injury was less likely on roads and public locations and more likely at indoor private locations (P < 0.05). The proportion of patients with neurotrauma with blood alcohol concentration >0.08 g/dL was reduced in 2020 (11.4% vs. 9.0%; P < 0.05). Mortality was higher during 2020 compared with pre-COVID years (7.7% vs. 6.4%; P < 0.05).
Conclusions
During statewide shutdown, neurotrauma volume and alcohol-related trauma decreased and low-impact traumas and gunshot wounds increased, with a shift toward injuries occurring in private, indoor locations. These changes increased mortality. However, there was not a change in the types of injuries sustained.
Key words: COVID-19, Neurotrauma, Pennsylvania
Abbreviations and Acronyms: BAC, Blood alcohol concentration; COVID-19, Coronavirus disease 2019; GSW, Gunshot wound; IRR, Incidence rate ratio; TBI, Traumatic brain injury
Introduction
The coronavirus 2019 (COVID-19) pandemic incited a global public health response through government, commercial, and behavior protocols aimed at reducing spread. Within the United States and on a state-by-state basis, public health mandates were issued. Pennsylvania was an early adaptor of stay-at-home mandates and closing of nonessential businesses, issuing the mandate on March 12, 2020. During the week of March 10–16, nationwide perceptions of health risk dramatically increased.1 Several investigators have highlighted the impact of the pandemic on hospital bed availability, preparation, and resource use during the peak of the disease.2
The pandemic, statewide shutdowns, and the social distancing concept affected trauma volumes and mechanism of injury.3 , 4 The effect has been seen among many surgical subspecialties, including orthopedic and plastic surgery.5 In Europe, the pandemic affected the total number of patients presenting with neurosurgical emergencies, including aneurysmal subarachnoid hemorrhage, hydrocephalus, and spinal cord injury, whereas relative volumes were similar.6 More patients presented via the emergency room rather than outpatient clinics and patients with spinal emergencies presented an average of 48 hours later despite comparable symptoms to previous years studied.6 Mechanism of injury has been investigated among other surgical fields, in which increased assault-related injuries, including domestic abuse, as well as decreased motor vehicle collisions, were found.5 , 7 These findings have been seen both in adult and in pediatric realms.8 , 9
The COVID-19 pandemic and stay-at-home orders dramatically affected the public health landscape, with potential implications for our populations with trauma, mechanism/place of injury occurrence, and the ability to effectively respond to these emergencies. The goal of the current study was to evaluate neurotrauma presentations within Pennsylvania state as well as analyze our subset within Allegheny county.
Methods
The Pennsylvania Trauma Systems Foundation was queried for registry data from the Pennsylvania Trauma Outcome Study after obtaining institutional review board approval. Patient consent was not required or sought given that data were both de-identified and obtained from a registry. During the COVID-19 pandemic, social distancing measures were formally implemented on March 12, with urging of nonessential businesses to close. Approximately 3 months of social distancing ensued until June 5, when Allegheny county and the remaining large counties within Pennsylvania entered the green phase of planned reopening, thus allowing most businesses to reopen, following strict health guidelines. Thus, traumatic injuries incurred between March 12 and June 5, 2020 were analyzed and compared with the same period in 2017–2019. Trauma cases were grouped and reviewed among all trauma centers participating in Pennsylvania Trauma Outcomes Study within Pennsylvania state. A subgroup analysis among the only 3 level I trauma centers within Allegheny county was completed as well.
The International Classification of Diseases, Tenth Revision was used to select for cases of neurotrauma and to evaluate mechanism of injury, place of injury, diagnoses, procedures, and complications. S02/S06 codes were selected for skull fracture or intracranial injury, S15 codes for vascular injury of the carotid or vertebral artery, S14/S24/S34 codes for spinal cord injury, S12/S22/S32 codes for cervical, thoracic, or lumbar fracture, and S13/S23/S33codes selected for cervical, thoracic, or lumbar dislocation or subluxation. S06 diagnoses codes were used to define traumatic brain injuries (TBIs). Pathologies were excluded from the subsets as follows: facial fractures were excluded from S02, rib fractures were excluded from S22, and sacral/pelvic fractures were excluded from S33. Blood alcohol concentrations (BACs) >0.08 g/dL were used to define alcohol use as a factor in traumatic injuries.
Normality of continuous variable distributions was assessed graphically and statistically, with a Shapiro-Wilks test. Continuous variables with nonparametric and parametric distributions were represented as annual median and mean estimates, respectively, with their associated interquartile range or standard deviations. Bivariable comparisons of continuous variables were performed with a Student t test and Wilcoxon rank sums as appropriate, whereas multinomial comparisons were carried out with analysis of variance or the Kruskal-Wallis test. Categorical variables were represented as frequency and percent. Statistical analyses of categorical variables were carried out using χ2 and Fisher exact t tests, as appropriate. Comparison of annual trauma counts was performed with Poisson regression modeling. Poisson model significance was assessed with the likelihood ratio χ2 test and individual covariate incidence rate ratios (IRRs) were reported. A P value <0.05 was considered statistically significant. Statistical analysis was performed with SAS version 9.4 (SAS Institute Inc., Cary, North Carolina, USA) and RStudiov1.2.5001 (RStudio, Boston, Massachusetts, USA).
Results
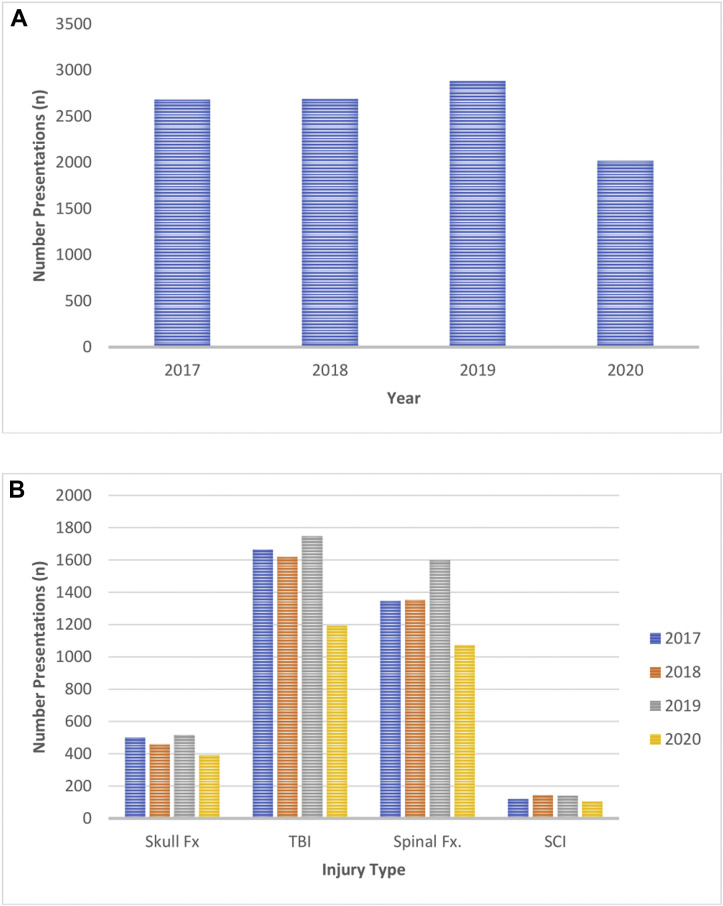
A total of 10,267 neurotrauma cases were identified between March 12 and June 5 in 2017–2020. By year, 2680 neurotrauma presentations occurred in 2017, 2687 i018, 2882 in 2019, and 2018 in 2020. Compared with the average number of presentations between 2017 and 2019, there was a 27% reduction in the number of neurotrauma presentations in 2020. There was a decreased neurotrauma incidence rate in 2020 compared with previous years (2017 IRR, 1.32, P < 0.0001; 2018 IRR, 1.33, P < 0.0001; 2019 IRR, 1.43, P < 0.0001). Allegheny county made up a large proportion of these data because there were 721 neurotrauma presentations in 2020, with a 26.5% reduction compared with 2017–2019 (P < 0.0001) (Figure 1 ).
Figure 1.
(A) Total neurotrauma presentations seen across Pennsylvania state between 2017 and 2020. (B) Subtype of neurotraumatic injuries incurred between 2017 and 2020, including skull fractures (Fx), traumatic brain injuries (TBIs), spinal fractures (Fx) (including cervical, thoracic, and lumbar), and spinal cord injury (SCI) (including cervical, thoracic, and lumbar).
Table 1 compares the demographics and characteristics of neurotrauma alerts between the pre-COVID and COVID periods. There was no difference in the race or sex of patients experiencing a neurotrauma among the 4 years. There was no difference in median age (P = 0.072); however, there was a change in neurotrauma incidence based on age-group subsets (P < 0.001) (Table 1). The trauma alert system is used to triage based on severity of injury and varies by institution. Generally, level 1 trauma alerts are anticipated as the most severe and level 3 as least severe. There was no change in level 1 trauma likelihood but there was a decrease in level 2 trauma (P = 0.008) and increase in level 3 likelihood during the 2020 index period (P = 0.005).
Table 1.
Pennsylvania Neurotrauma Demographics and Characteristics Before and During COVID-19 Pandemic
| Before COVID-19∗ | COVID-19 | P Value | |
|---|---|---|---|
| Race, n (%) | 0.372 | ||
| White | 2196 (83.3) | 1582 (82.0) | |
| Black | 335 (12.7) | 272 (14.1) | |
| Asian | 28 (1.1) | 17 (0.9) | |
| Other | 79 (3.0) | 59 (3.1) | |
| Male, n (%) | 1603 (58.3) | 1205 (59.7) | 0.248 |
| Age, median (IQR) | 62.0 (40) | 64 (41) | 0.072 |
| Age groups, n (%) | <0.001 | ||
| <15 years | 120 (4.4) | 103 (5.1) | |
| 16–30 years | 384 (14.0) | 254 (12.6) | |
| 30–45 years | 316 (11.5) | 249 (12.3) | |
| 45–60 years | 488 (17.7) | 289 (14.3) | |
| >60 years | 1442 (52.4) | 1123 (55.7) | |
| Trauma alert level, n (%) | |||
| 1 | 1924 (70.0) | 1387 (68.7) | 0.282 |
| 2 | 155 (5.6) | 84 (4.2) | 0.008 |
| 3 | 551 (20.0) | 462 (22.9) | 0.005 |
| Blood alcohol level >0.08 g/dL, n (%) | 313 (11.4) | 181 (9.0) | 0.002 |
| Drug associated, n (%) | 280 (10.2) | 232 (11.5) | 0.087 |
Reflects average number of presentations in a single year between 2017 and 2019.
Within all of Pennsylvania, alcohol intoxication was less of a factor during the 2020 index period compared with previous years as measured by the number of patients with neurotrauma presenting with admission BAC >0.08 g/dL (pre-COVID, 11.4% vs. COVID, 9.0%; P = 0.002) (Table 1). However, within Allegheny county, there was no change in rate of alcohol use during 2020 because 11.6% of patients with neurotrauma presented with BAC >0.08 g/dL. Within Allegheny county, the median BAC of those patients presenting with BAC >0.08 g/dL was higher in 2020 compared with 2017–2019 (0.19 g/dL vs. 0.15 g/dL; P = 0.005). There was no difference in statewide illicit drug use in neurotraumas during the 2020 COVID period compared with 2017–2019 (Table 1).
Table 2 compares injury type, mechanism, and location between pre-COVID and COVID periods across the state. There was no difference in likelihood of patients presenting with TBI, vascular injury, vertebral fracture or subluxation, or spinal cord injury over the index period between 2017 and 2020. During the COVID pandemic, there were fewer blunt and more penetrating subtypes of neurotrauma (P = 0.006). Compared with previous years, COVID neurotraumas were less likely to be caused by motor vehicle accidents (P < 0.001) and more likely to be caused from falls (P = 0.027) or recreational vehicle accidents, which includes bicycles and all-terrain vehicles (P < 0.001). There was an increase in the number of gunshot wound (GSW) assaults in 2020 (P = 0.006); however, the number of self-inflicted GSWs was unchanged. Neurotrauma injuries during the index period were more likely to occur in private indoor establishments and less likely to occur on roads and public areas (Table 3 ). There was no significant change in the frequency of injuries occurring outdoors or in other locations, which included nursing homes, medical centers, educational establishments, and prisons.
Table 2.
Neurotrauma Type, Mechanism, and Location Before and During COVID
| Before COVID-19∗ | COVID-19 | P Value | |
|---|---|---|---|
| Type of neurotrauma, n (%) | |||
| Skull | 491 (17.9) | 392 (19.4) | 0.104 |
| Traumatic brain injury | 1675 (60.9) | 1192 (59.1) | 0.128 |
| Vascular injury | 47 (1.8) | 43 (2.3) | 0.200 |
| Cervical fracture | 474 (17.2) | 373 (18.5) | 0.187 |
| Cervical SCI | 99 (3.6) | 77 (3.8) | 0.624 |
| Thoracic fracture | 468 (17.0) | 356 (17.6) | 0.515 |
| Thoracic SCI | 17 (0.6) | 14 (0.7) | 0.750 |
| Lumbar fracture | 481 (17.5) | 358 (17.7) | 0.793 |
| Lumbar SCI | 19 (0.7) | 15 (0.7) | 0.800 |
| Injury type, n (%) | 0.006 | ||
| Blunt | 2656 (96.7) | 1921 (95.4) | |
| Penetrating | 92 (3.4) | 93 (4.9) | |
| Mechanism, n (%) | |||
| Motor vehicle accident | 440 (16.0) | 254 (12.6) | <0.001 |
| Fall | 1607 (62.5) | 1314 (65.1) | 0.027 |
| Assault | 198 (7.2) | 149 (7.4) | 0.791 |
| Gunshot wound | 63 (2.3) | 68 (3.4) | 0.006 |
| Motor vehicle versus pedestrian | 82 (3.0) | 50 (2.5) | 0.225 |
| Recreational vehicles | 97 (3.5) | 108 (5.4) | <0.001 |
| Self-harm | 25 (0.9) | 14 (0.7) | 0.330 |
| Self-inflicted gunshot wound | 18 (0.7) | 8 (0.4) | 0.180 |
| Other | 190 (6.9) | 129 (6.4) | 0.419 |
| Location of injury, n (%) | |||
| Private residence | 1100 (45.4) | 911 (50.9) | <0.001 |
| Roads | 799 (33.0) | 538 (30.4) | 0.017 |
| Public area | 380 (15.7) | 245 (13.7) | 0.035 |
| Industrial/agricultural | 46 (1.9) | 25 (1.4) | 0.151 |
| Other | 96 (4.0) | 72 (4.2) | 0.911 |
Cervical, thoracic, and lumbar fractures include fractures, dislocations, and subluxations.
SCI, spinal cord injury.
Reflects average number of presentations in a single year between 2017 and 2019.
Table 3.
Complications within Patients with Neurotrauma Before and During COVID-19 Pandemic
| Before COVID-19∗ | COVID-19 | P Value | |
|---|---|---|---|
| Deaths, n (%) | 177 (6.4) | 155 (7.7) | 0.044 |
| Complication, n (%) | 188 (6.9) | 109 (5.4) | 0.019 |
| Wound infection | 13 (0.5) | 6 (0.3) | 0.285 |
| Unexpected intensive care unit return | 88 (3.2) | 58 (2.9) | 0.467 |
| Unexpected operating room return | 15 (0.6) | 0 (0.0) | <0.001 |
| Unexpected intubation | 55 (2.0) | 41 (2.0) | 0.900 |
| Central nervous system infection | 2 (0.1) | 0 (0.0) | 0.358 |
| Sepsis | 17 (0.6) | 11 (0.6) | 0.701 |
| Deep vein thrombosis | 28 (1.0) | 10 (0.5) | 0.027 |
| Pulmonary embolism | 14 (0.5) | 5 (0.3) | 0.106 |
| Respiratory failure | 13 (0.48) | 0 (0.0) | <0.001 |
| Acute respiratory distress syndrome | 5 (0.2) | 8 (0.4) | 0.068 |
Reflects average number of presentations in a single year between 2017 and 2019.
There were 1663 TBIs in 2017, 1616 in 2018, 1746 in 2019, and 1191 in 2020. The COVID period showed a TBI incidence reduction of 28.8% compared with previous years (P < 0.0001). Within Allegheny county, there were 358 TBI presentations during the 2020 index period, representing 30% of the state total, with a similar reduction of 29% compared with 2017–2019 (P < 0.0001). The distribution of mild, moderate, and severe TBI was unchanged between the index year and previous years (P = 0.27). The likelihood of TBI necessitating craniotomy was unchanged compared with previous years (pre-COVID, 5.4% vs. COVID, 6.1%; P = 0.134). Average hospital stay for patients with TBI was shorter during the 2020 index period (pre-COVID, 5.7 days vs. COVID, 5.1 days; P = 0.014).
There was a significant increase in mortality during the 2020 index period across the entire state compared with previous years (pre-COVID, 6.4% vs. COVID, 7.7%; P = 0.044). Within Allegheny county, there was no observed mortality difference (pre-COVID, 6.2% vs. COVID, 6.2%; P = 0.95). Rates of significant respiratory and neurologic complications were assessed over the index period between 2017 and 2020. Overall, there was a decrease in complication rate during 2020 compared with previous years (pre-COVID 6.9% vs. COVID 5.4%; P = 0.019). There were noted reductions in incidence of deep vein thrombosis, unplanned return to the operating room, and episodes of respiratory failure during the 2020 index period. There was no difference in rates of pneumonia (ventilator-associated or community-acquired), acute respiratory distress syndrome, acute respiratory failure, pulmonary arrest, pulmonary edema, pulmonary embolism, unplanned intubation, or unplanned intensive care unit admission (P > 0.05). Regarding neurologic complications, there were no changes in rates of meningitis, ventriculitis, anoxic encephalopathy, seizure, diabetes insipidus, or syndrome of inappropriate antidiuretic hormone secretion (P > 0.05).
Discussion
The statewide restrictions caused by COVID-19 implemented in March 2020 resulted in a 27% absolute and significant reduction in neurotrauma volume in Pennsylvania. There was a shift from motor vehicle accidents to recreational vehicle accidents, GSWs, and falls. In addition, during the COVID-19 shutdown phase, more injuries occurred at private indoor residences and fewer on the roads. In addition, we found that there was a reduced likelihood of patients presenting intoxicated across the state; however, this latter finding did not hold within Allegheny county, where rates were similar and median BAC was higher.
Other studies evaluating traumatic injuries identified similar trends but unique differences exist. One study10 evaluated traumas at a level 1 center in New Orleans, Louisiana and found a 70% reduction in traumatic injuries at their center, whereas the present study found a 27% reduction within both Pennsylvania and Allegheny county. Similarly, that cohort identified a reduction in road-related trauma during the index period as well as increased gunshot-related trauma.10 , 11 A level 1 trauma center in Virginia identified a reduction of trauma volume by 43%, with a likewise increase in traumas caused by chronic alcohol use.12 At level 2 trauma centers, orthopedic-related trauma volume decreased by approximately 45%.13 Internationally, a study from New Zealand identified a similar reduction of 43% during their nation's lockdown.14 From South Carolina, 1 study15 identified an increase in the prevalence of domestic violence–related trauma at a rural trauma center. The 27% reduction in neurotrauma presentations in Pennsylvania was less than in other locations studied, highlighting the regional variability. The larger number of quaternary, referral-receiving centers is a possible explanation for this effect.16 However, the time frame of shutdown, strictness of mandates, and the socioeconomic climate of the region are all variables that have a bearing on these estimates. The present study does contain data on a subset of pediatric patients and several of these findings apply to both pediatric and adult patients.8 , 9
The alcohol abuse use was anticipated to be affected in 1 disparate ways by the pandemic. One theory hypothesizes increased use of alcohol because of distress caused by the pandemic. Another postulates decreased intake because of financial and availability restrictions for many citizens.17 In the present study, there were fewer alcohol-related neurotraumas across the state; however, this finding was not evident within Allegheny county, where alcohol was a factor in 11.6% of neurotraumas. Among those patients who presented intoxicated, the median BAC was higher during the index period of 2020 in Allegheny county. Multiple factors play a role in determining alcohol use during the pandemic, including age and psychological history. Lechner et al.18 found alcohol use on a college campus to increase after campus closure because of the pandemic; increased use was associated with those students with fewer social supports.
Conversely, illicit drug use was unchanged across the state in our study. Others19 found drug testing frequency reduced during the pandemic, but positivity rates increased for heroin and nonprescription fentanyl. Those with a history of substance use disorders are particularly susceptible to increasing use in the stressful setting of pandemic.20 Surveyed participants during the pandemic noted symptoms of anxiety or depression in 31%, described pandemic-associated stress/trauma in 26%, increased substance use related to stress in 13%, and recent contemplation of suicide in 11%.21
Among the population with TBI, we identified a 28.8% reduction in volume compared with previous years. The clinical severity of TBI and number of patients requiring craniotomy was similar across years. Surprisingly, there was an approximately 50% increase in GSWs leading to neurotrama compared with pre-COVID years (P = 0.006). This was an unexpected finding given the expectation that state shutdown and social distancing would reduce social interactions and gatherings that may result in GSWs.
There are several limitations to the current study. Mistranslation and misinterpretation of medical record data to a registry is one concern. In addition, registries require assumptions to be made when interpreting data. For instance, assessing patient Glasgow Coma Scale score highlights these limitations because the Glasgow Coma Scale score reported in the field before presentation and initially on hospital arrival is often incorrect and varies based on the familiarity of personnel with the scale.22 Likewise, the scale is often erroneously scored in patients who remain paralyzed or sedated from the field, and thus, the registry data probably overestimate severe TBIs. Another limitation is diagnostic data and International Classification of Diseases, Tenth Revision coding. TBI is indicated by the S06.0 code and has multiple subsets based on intracranial bleed pattern. However, this code also includes concussion. In this vein, mild TBI and mild neurotrauma may be overestimated as well. Despite limitations, there are several strengths, particularly analysis of large quaternary metropolitan care centers as opposed to referral centers. Other studies evaluating similar trends often compare with single previous years as opposed to the present study, which evaluates similar time periods from 2017 to 2019.
The reduction in neurotrauma volume and shifts in mechanism and location of injury during the pandemic have several implications. Quantifying the reduction in trauma volume helps identify adequate resource availability, including hospital and intensive care unit beds, ventilators, and staff, which have been a limited resource during the pandemic. Multiple neurosurgeons have commented on the reduction in these resources and methods to manage these scarcities.23, 24, 25 In addition, although the neurotrauma phenotype was unchanged, mortality increased. One possibility may be that the pandemic led to delayed presentations and thus increased morbidity on presentation. Another possibility is that limited resources, hospital staff, and longer times to interventions in the setting of mandated coronavirus precautions may have contributed to an increase in mortality. The societal response to shutdown is reflected in the shifts in mechanism and location of neurotrauma and is useful in understanding the response to future similar events. Inversely, the same information can be used to predict the expected trend when shutdown orders are lifted and we move into later phases of the pandemic. For instance, and anecdotally, several surgeons have commented on the larger than anticipated increase in gun violence and neurotrauma when shutdown orders were lifted. Gun violence increased across the state even during the pandemic and may even be expected to further increase after. Also, based on the recent literature, neurotrauma volumes within Pennsylvania were not affected as largely as was seen in other locations. If similar shutdown measures are reimplemented, the current findings may provide guidance for preparedness, the injury types requiring further vigilance, and management of hospital resources and availability. Characterizing the initial response to the statewide shutdown is only the first step in understanding the entirety of the effect of the pandemic on trauma as well as the complex interplay between societal mandates and individual response.
CRediT authorship contribution statement
Hanna N. Algattas: Conceptualization, Methodology, Formal analysis, Investigation, Resources, Writing - original draft. David McCarthy: Methodology, Software, Writing - review & editing. Brandon Kujawski: Conceptualization, Writing - review & editing. Nitin Agarwal: Writing - review & editing. Joshua Brown: Methodology, Validation, Data curation. Raquel M. Forsythe: Data curation, Writing - review & editing, Supervision. Jody Leonardo: Writing - review & editing, Supervision. Kevin Walsh: Validation, Writing - review & editing. Bradley A. Gross: Writing - review & editing, Supervision. Robert M. Friedlander: Writing - review & editing, Supervision. David O. Okonkwo: Validation, Writing - review & editing, Supervision. Donald Whiting: Writing - review & editing, Supervision. Vincent J. Miele: Conceptualization, Data curation, Writing - review & editing, Supervision.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Ciancio A., Kämpfen F., Kohler I.V., et al. Know your epidemic, know your response: early perceptions of COVID-19 and self-reported social distancing in the United States. PLoS One. 2020;15:e0238341. doi: 10.1371/journal.pone.0238341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Noronha K., Guedes G.R., Turra C.M., et al. The COVID-19 pandemic in Brazil: analysis of supply and demand of hospital and ICU beds and mechanical ventilators under different scenarios. Cad Saude Publica. 2020;36:e00115320. doi: 10.1590/0102-311X00115320. [DOI] [PubMed] [Google Scholar]
- 3.Bram J.T., Johnson M.A., Magee L.C., et al. Where have all the fractures gone? The epidemiology of pediatric fractures during the COVID-19 pandemic. J Pediatr Orthop. 2020;40:373–379. doi: 10.1097/BPO.0000000000001600. [DOI] [PubMed] [Google Scholar]
- 4.Probert A.C., Sivakumar B.S., An V., et al. Impact of COVID-19-related social restrictions on orthopaedic trauma in a level 1 trauma centre in Sydney: the first wave. ANZ J Surg. 2021;91:68–72. doi: 10.1111/ans.16375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hassan K., Prescher H., Wang F., Chang D.W., Reid R.R. Evaluating the effects of COVID-19 on plastic surgery emergencies: protocols and analysis from a level I trauma center. Ann Plast Surg. 2020;85(2S suppl 2):S161–S165. doi: 10.1097/SAP.0000000000002459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hecht N., Wessels L., Werft F.O., Schneider U.C., Czabanka M., Vajkoczy P. Need for ensuring care for neuro-emergencies–lessons learned from the COVID-19 pandemic. Acta Neurochir (Wien) 2020;162:1795–1801. doi: 10.1007/s00701-020-04437-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gerber L.M., Ni Q., Härtl R., Ghajar J. Impact of falls on early mortality from severe traumatic brain injury. J Trauma Manag Outcomes. 2009;3:9. doi: 10.1186/1752-2897-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wellons J.C., Grant G., Krieger M.D., et al. Editorial. Early lessons in the management of COVID-19 for the pediatric neurosurgical community from the leadership of the American Society of Pediatric Neurosurgeons [e-pub ahead of print]. J Neurosurg Pediatr. https://doi.org/10.3171/2020.3.peds20215 [DOI] [PMC free article] [PubMed]
- 9.Ceraudo M., Balestrino A., Cama A., Macrina G., Piatelli G., Consales A. Pediatric neurosurgery after the COVID-19 pandemic: management strategies from a single pediatric hospital in Italy. World Neurosurg. 2021;146:e1079–e1082. doi: 10.1016/j.wneu.2020.11.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sherman W.F., Khadra H.S., Kale N.N., Wu V.J., Gladden P.B., Lee O.C. How did the number and type of injuries in patients presenting to a regional level I trauma center change during the COVID-19 pandemic with a stay-at-home order? Clin Orthop Relat Res. 2021;479:266–275. doi: 10.1097/CORR.0000000000001484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lubbe R.J., Miller J., Roehr C.A., et al. Effect of statewide social distancing and stay-at-home directives on orthopaedic trauma at a southwestern level 1 trauma center during the COVID-19 pandemic. J Orthop Trauma. 2020;34:e343–e348. doi: 10.1097/BOT.0000000000001890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leichtle S.W., Rodas E.B., Procter L., Bennett J., Schrader R., Aboutanos M.B. The influence of a statewide “Stay-at-Home” order on trauma volume and patterns at a level 1 trauma center in the United States. Injury. 2020;51:2437–2441. doi: 10.1016/j.injury.2020.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stoker S., McDaniel D., Crean T., et al. The effect of shelter-in-place orders and the COVID-19 pandemic on orthopaedic trauma at a community level II trauma center. J Orthop Trauma. 2020;34:e336–e342. doi: 10.1097/BOT.0000000000001860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Christey G., Amey J., Campbell A., Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. NZ Med J. 2020;133:81–88. [PubMed] [Google Scholar]
- 15.Rhodes H.X., Petersen K., Lunsford L., Biswas S. COVID-19 resilience for survival: occurrence of domestic violence during lockdown at a rural American College of Surgeons verified level one trauma center. Cureus. 2020;12:e10059. doi: 10.7759/cureus.10059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Placella G., Salvato D., Delmastro E., Bettinelli G., Salini V. CoViD-19 and ortho and trauma surgery: the Italian experience. Injury. 2020;51:1403–1405. doi: 10.1016/j.injury.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rehm J., Kilian C., Ferreira-Borges C., et al. Alcohol use in times of the COVID 19: implications for monitoring and policy. Drug Alcohol Rev. 2020;39:301–304. doi: 10.1111/dar.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lechner W.V., Laurene K.R., Patel S., Anderson M., Grega C., Kenne D.R. Changes in alcohol use as a function of psychological distress and social support following COVID-19 related University closings. Addict Behav. 2020;110:106527. doi: 10.1016/j.addbeh.2020.106527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Niles J.K., Gudin J., Radcliff J., Kaufman H.W. The opioid epidemic within the COVID-19 pandemic: drug testing in 2020. Popul Health Manag. 2021;24(S1):S43–S51. doi: 10.1089/pop.2020.0230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hochstatter K.R., Akhtar W.Z., Dietz S., et al. Potential influences of the COVID-19 pandemic on drug use and HIV care among people living with HIV and substance use disorders: experience from a pilot mHealth intervention. AIDS Behav. 2021;25:354–359. doi: 10.1007/s10461-020-02976-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Czeisler M., Lane R.I., Petrosky E., et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heim C., Schoettker P., Gilliard N., Spahn D.R. Knowledge of Glasgow Coma Scale by air-rescue physicians. Scand J Trauma Resusc Emerg Med. 2009;17:39. doi: 10.1186/1757-7241-17-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zoia C., Bongetta D., Veiceschi P., et al. Neurosurgery during the COVID-19 pandemic: update from Lombardy, northern Italy. Acta Neurochir (Wien) 2020;162:1221–1222. doi: 10.1007/s00701-020-04305-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Balestrino A., Robba C., Ceraudo M., et al. Turning tables: a war-like approach to neurosurgical emergencies in the Covid-19 [e-pub ahead of print]. J Neurosurg Sci. https://doi.org/10.23736/s0390-5616.21.05226-7 [DOI] [PubMed]
- 25.Fontanella M.M., Saraceno G., Lei T., et al. Neurosurgical activity during COVID-19 pandemic: an experts' opinion from China, South Korea, Italy, the USA, Colombia, and the UK. J Neurosurg Sci. 2020;64:383–388. doi: 10.23736/S0390-5616.20.04994-2. [DOI] [PubMed] [Google Scholar]