Summary
Data are conflicting regarding the impact of weight loss on mood and anxiety in adolescent and young adult females with moderate to severe obesity (OB), who are at increased risk for mood dysfunction compared with normal-weight females (NW). We examined depressive and anxiety symptoms in 94 females 13–21 years old: 39 in the NW group (body mass index [BMI]: 5th–85th percentiles) and 55 in the OB group (BMI >40 kg/m2 or >35 kg/m2 with comorbidities). Fifteen participants in the OB group who underwent bariatric surgery (gastric bypass or sleeve gastrectomy) and 15 getting routine care were re-assessed after 6 months. The Beck Depression Inventory-II (BDI-II) and State-Trait Anxiety Inventory (STAI) assessed depressive and anxiety symptoms, respectively. The OB group had higher BDI-II and STAI T-scores (P < .0001), a higher prevalence of clinical depression and anxiety (P < .001), and reported greater suicidal ideation (P = .02) vs the NW group. The bariatric surgery and non-surgical groups did not differ for changes in BDI-II and STAI T-Scores and suicidality over 6-month follow-up, despite greater weight loss in the former. Depressive and anxiety symptoms and suicidality were more frequently observed in the OB vs NW group. These symptoms did not improve following bariatric surgery despite significant weight loss, underscoring the need to investigate determinants of emergence and resolution of these symptoms in the OB group.
Keywords: adolescents, anxiety, bariatric surgery, depression, moderate to severe obesity, young adults
1 |. INTRODUCTION
Rates of severe obesity in children and adolescents have increased markedly in the last decade.1–3 Recent data indicate that 4.5% of adolescents aged 16–19 years meet criteria for severe obesity (class III), with an increasing linear trend for all obesity classes between 1999 and 2016.2 In females, the pubertal years are also characterized by an increase in the prevalence of mood and anxiety symptoms.4–6 Data regarding the prevalence of mood and anxiety disorders in adolescents and youth with obesity are conflicting. Most studies, however, suggest an increased risk of developing these disorders in those with obesity.
Vila et al. showed that children 5–17 years old of both sexes with severe obesity (defined in this cohort as a body mass index [BMI] z-score ≥8) had lower anxiety and depression scores compared to children with obesity with BMI z-scores 2–8.7 Contrary to this, some studies have reported no relationship between BMI (expressed as a continuous variable) and depression,8 unless weight status was dichotomized into mild to moderate obesity vs. severe obesity, with only severe obesity being associated with increased depression and anxiety scores.9 The majority of studies indicate a strong positive association between obesity and depression/anxiety,9–11 with one study reporting a diagnosis of mood or anxiety disorder in over 40% of male and female adolescents with severe obesity compared with only 15% of normal-weight controls.12 Further, some studies that have reported a positive link between weight status and psychiatric measures have specifically demonstrated a female preponderance of these disorders.11,13
In contrast to adults, the association with suicidality is less clear in adolescents with moderate to severe obesity, and the limited available data are equivocal.14 One Dutch study that classified weight status based on self-reported height and weight demonstrated that boys and girls with obesity were more likely to have suicidal thoughts (odds ratio [OR] of 4 for both boys and girls) and suicide attempts (OR of 7 and 4 for boys and girls, respectively) compared with normal-weight participants.15 Similarly, Zeller et al.reported that the odds of having suicidal ideation in high school children with obesity or severe obesity was twice as high as that in adolescents with normal weight.16 Goldstein et al., on the other hand, found no difference in suicidality between children with overweight/obesity vs. normal-weight children with bipolar disorders.17 Of note, some adult studies have reported associations of higher BMI with lower suicide rates—this finding has not been replicated in adolescents.18,19 Further data on suicidality in adolescents and young adults with obesity are necessary, and our study adds to this limited literature.
With the drastic rise in adolescent and young adult obesity, bariatric surgery has become an accepted and growing therapeutic modality for moderate to severe obesity not only in adults but also in adolescents. Studies evaluating changes in depression and anxiety symptoms following weight loss surgery are mostly limited to adults with mixed results. Most studies show a short-term decrease in depressive and anxiety symptoms, while some demonstrate that this short-term decrease is followed by a subsequent worsening of symptoms.20,21 Similarly, in adolescents and young adults, a few studies, mainly comprised of single cohorts, indicate an improvement in mood symptoms over a short duration, but data are equivocal.22–24 Our study is a novel addition to the field of bariatric surgery research in that it compares adolescent and young adult participants with moderate to severe obesity who underwent bariatric surgery with a non-surgical cohort over 6 months.
Our objective was to evaluate depressive and anxiety symptoms and suicidality in adolescent and young adult females with moderate to severe obesity (OB) vs normal-weight females (NW). We also conducted an exploratory analysis to assess changes in these symptoms in OB group following weight loss surgery compared to a non-surgical group. We hypothesized that the prevalence of depressive and anxiety symptoms and suicidal ideation would be more pronounced in the OB group compared to the NW group, and would improve following weight loss surgery.
2 |. METHODS
2.1 |. Subjects
We included 94 females ages 13 to 21 years enrolled in studies conducted by our group between 2004 and 2018 for this analysis (55 in the OB group and 39 in the NW group). All studies were approved by the Partners HealthCare Institutional Review Board. Subjects were recruited from Massachusetts General Hospital and community providers, through mailings to primary care paediatric practices in and around Boston, and via advertisements. Subjects >18 years of age and parents of subjects <18 years of age provided informed consent, and informed assent was obtained from subjects <18 years of age.
Data for depressive and anxiety symptoms were obtained through self-report questionnaires. Participants in OB and NW groups were recruited from studies in which bone health was the primary outcome; therefore, participants on medications affecting bone metabolism and those with thyroid dysfunction, primary ovarian insufficiency and hyperprolactinemia were excluded.25 Participants in the NW group who were on antipsychotic medication were also excluded. Participants in the OB group met criteria for weight loss surgery; they either had a BMI of >40 kg/m2 regardless of comorbidities, or > 35 kg/m2 with comorbidities, such as type 2 diabetes, elevated liver enzymes, high blood pressure or polycystic ovarian syndrome. Definition of severe obesity in adults per Centers for Disease Control and Prevention guidelines is based on BMI. In adults Class 2 obesity refers to a BMI between 35 and 40 kg/m2 and Class 3 obesity (or severe or extreme obesity) refers to a BMI above 40 kg/m2. In children; however, the definition for severe obesity is dependent on both BMI percentiles and BMI. A BMI ≥120% of the 95th percentile or an absolute BMI ≥35 kg/m2, whichever is lower based on age and sex is considered severe obesity in a paediatric population up to 18 years old.26 All adolescents in our study under 18 years of age had a BMI that was more than 120% of the 95th percentile of BMI for age and sex and a BMI ≥35 kg/m2. Given that our study included both adolescents and young adults to the age of 21, and some adults with a BMI >35 kg/m2 have associated comorbidity, we defined our population as having “moderate to severe obesity” thereby including Class 2 and Class 3 obesity. Subjects in the NW group had a BMI percentile between the 5th and 85th percentiles for age and sex.27
2.2 |. Questionnaires
Depression was assessed using the Beck Depression Inventory-II (BDI-II).28 Anxiety was assessed using the Trait Scale of the State-Trait Anxiety Inventory (STAI) versions X2 and Y2.29,30 All raw scores were converted to T-scores to enable comparisons across different STAI versions used for the adolescent and young adult participants. Subjects with BDI-II raw scores ≥14 were considered to have symptoms suggestive of clinical depression.28 Similarly, BDI-II raw scores ≥29 were representative of severe depression.28 Suicidality was assessed using the BDI-II single item Question 9 asking about suicidal ideation. The questionnaire was scored at the time of the visit and the answers to this item were reviewed at the same time. The question explicitly asks about thoughts of killing oneself and includes the following options: “0: I don’t have any thoughts of killing myself. 1: I have thoughts of killing myself, but I would not carry them out. 2: I would like to kill myself. 3: I would kill myself if I had the chance.” Participants who scored 1,2,3 on this question were considered to have suicidal thoughts and were followed up by our study psychologist soon after to assess safety of the patient. STAI raw scores more than 1 SD from the population mean were considered suggestive of clinical anxiety.31 This was based on a female population between 19 and 39 years old, in whom the STAI-Trait score mean was 36.2 ± 9.5.30 In addition, follow-up BDI-II and STAI T-scores were available at 6 months in 30 adolescents and 27 adolescents, respectively, in the OB group. These subjects were followed by their primary care physician or at the Weight Center at the Massachusetts General Hospital. Of these 30 subjects, 15 underwent weight loss surgery (Roux-en-Y gastric bypass [RYGB] [n = 6] or vertical sleeve gastrectomy [VSG] [n = 9]) and 15 were followed without surgical intervention. Participants who were followed without surgical management received “routine care” consisting of behavioural and lifestyle modifications. Of note, four non-surgical subjects (two on selective serotonin reuptake inhibitors [SSRIs] and two on SSRIs as well as bupropion) and two surgical subjects (both on SSRIs) were on mood-altering medications prior to surgery.
2.3 |. Statistical analysis
Statistical analysis was conducted using JMP version Pro 13. The Shapiro-Wilk test showed that data were not distributed normally and therefore nonparametric tests were used for the analysis. The Wilcoxon test was used for two-group comparisons. Correlation analysis (Spearman) was utilized to test associations of BMI and BMI z-scores with BDI-II and STAI T-scores. In testing differences among NW and OB groups, we performed multivariate analysis to control for confounding variables such as age, ethnicity/race, and BMI or BMI z-scores. BDI-II and STAI T-scores over 6 months of follow-up in surgical and non-surgical groups were compared using paired t-tests. Data are reported as median and interquartile range. A P-value <.05 was considered statistically significant. Effect sizes were calculated using formula r = Z/sqrt N for differences between surgical and non-surgical group for depression and anxiety scores.
3 |. RESULTS
3.1 |. Cross-sectional analysis across the weight groups
Table 1 shows the clinical characteristics of the study groups. The NW group was significantly older than the OB group. As per study design, the OB group had a significantly higher BMI compared with the NW group (P < .0001). The OB group had a higher proportion of non-Whites and Hispanics than the NW group (OB vs NW group P < .0001). BDI-II and STAI T-scores are shown in Table 1. Depression and anxiety scores were higher in the OB compared with the NW group, and these differences persisted even after controlling for age and ethnicity/race (P < .0001 for both anxiety and depression).
TABLE 1.
Subject characteristics across the weight groups
| NW group (n = 39) | OB group (n = 55) | P-value (Wilcoxon) | |
|---|---|---|---|
| Age (years) | 19.2 (18.7–20.6) | 17.8 (15.7–19.6) | <.0001 |
| Ethnicity (% non-Hispanic) | 100% | 56% | <.0001 |
| Race (% Caucasian) | 82% | 51% | <.0001 |
| BMI (kg/m2) | 21.8 (21.4–23.4) | 44.5 (39.4–48.0) | <.0001 |
| BMI z-score | 0.08 (−0.05–0.47) | 2.41 (2.34–2.50) | <.0001 |
| Percent median BMI (%) | 101.1 (98.6–108.9) | 209.7 (193.8–228.0) | <.0001 |
| BDI-II T-score | 42.3 (34.9–44.4) | 51.0 (44.4–59.9) | <.0001 |
| BDI-II raw score | 2.0 (0–3.0) | 8.0 (3.0–21.0) | <.0001 |
| STAI T-score | 42.0 (37.0–49.0) | 55.0 (46.0–62.0) | <.01 |
| Suicidal ideations (%) | 3% | 16% | .02 |
Abbreviations: BDI-II, Beck Depression Inventory-II; BMI, body mass index; NW, normal-weight females; OB, obesity; STAI, State-Trait Anxiety Inventory.
Thirty-six percent of subjects in the OB group had clinical depression based on their raw scores, compared to 5% in NW group, P = .0001. Eleven percent of subjects in the OB group had severe depression compared to 3% in the NW group (P = .1). Of note, the proportion of participants who endorsed suicidal ideation was significantly higher in the OB group (16%) compared to the NW group (3%) P = .02. Forty percent in the OB group vs 5% in the NW group (P < .0001) had clinical anxiety based on STAI scores.
3.2 |. Longitudinal analysis in the group with moderate to severe obesity
Within the subset of 30 subjects in the OB group in whom follow-up data were available, 37% were Hispanic. Females who underwent surgery were older than those followed with routine care (19.8 years [17.5–21.0] vs. 16.8 years [14.9–18.8], P = .02). Surgical and non-surgical groups did not differ in race or ethnicity. The surgical group had a higher BMI than the non-surgical group (47.5 kg/m2 [42.5–54.5] vs. 38.3 kg/m2 [36.2–42.2], P = .001). There were no differences in baseline depression and anxiety scores between the groups (Table 2). The BDI-II scores decreased over 6 months for the whole group (surgical and non-surgical groups together); 50.7 at baseline to 46.9 at 6 months, P = .008), while the decrease in STAI scores was not significant (P = .16). Over 6-month follow-up, the surgical group had a significant decrease in BMI compared to the non-surgical group (Table 2, Figure 1). Despite the decrease in BMI in the surgical group over 6-month follow-up, the surgical and non-surgical groups did not differ for changes in anxiety and depression scores at follow-up, even after controlling for baseline age and BMI. The proportion of participants with suicidal ideation did not change from baseline to follow-up in surgical or non-surgical groups.
TABLE 2.
Depression and anxiety scores at baseline and 6-month follow-up in surgical and non-surgical groups
| Non-surgical group (n = 15) | Surgical group (n = 15) | Effect size | P-value (Wilcoxon) | |
|---|---|---|---|---|
| BDI-II T-score BL | 51 (42.3–62.7) | 48.9 (39.4–59.9) | −0.13 | .48 |
| STAI T-score BL | 54 (44.3–60.3) | 55 (38–58) | 0.08 | .66 |
| Suicidal ideation (%) BL | 21% | 21% | - | 1.00 |
| BDI-II T-score 6 M | 46.2 (39.4–58.2) | 46.2 (34.9–50) | −0.07 | .68 |
| STAI T-score 6 M | 44.0 (37.5–58) | 46.5 (39.5–55) | −0.03 | .86 |
| Suicidal ideation (%) 6 M | 20% | 13% | - | .62 |
| Change in BDI T-score (6 M-BL) | −2.1 (−7.7–0) | −1.6 (−9.5–0) | −0.01 | .93 |
| Change in STAI T-score (6 M-BL) | −3 (−8–0.5) | −6.5 (−12–9.75) | 0.05 | .77 |
| Change in BMI (6 M-BL) | −0.20 (−1.0–1.6) | −11.2 (−15.1 to −7.8) | −0.76 | <.0001 |
Abbreviations: BDI-II, Beck Depression Inventory-II; BMI: body mass index; M, month; M-BL, month baseline; STAI, State-Trait Anxiety Inventory.
FIGURE 1.
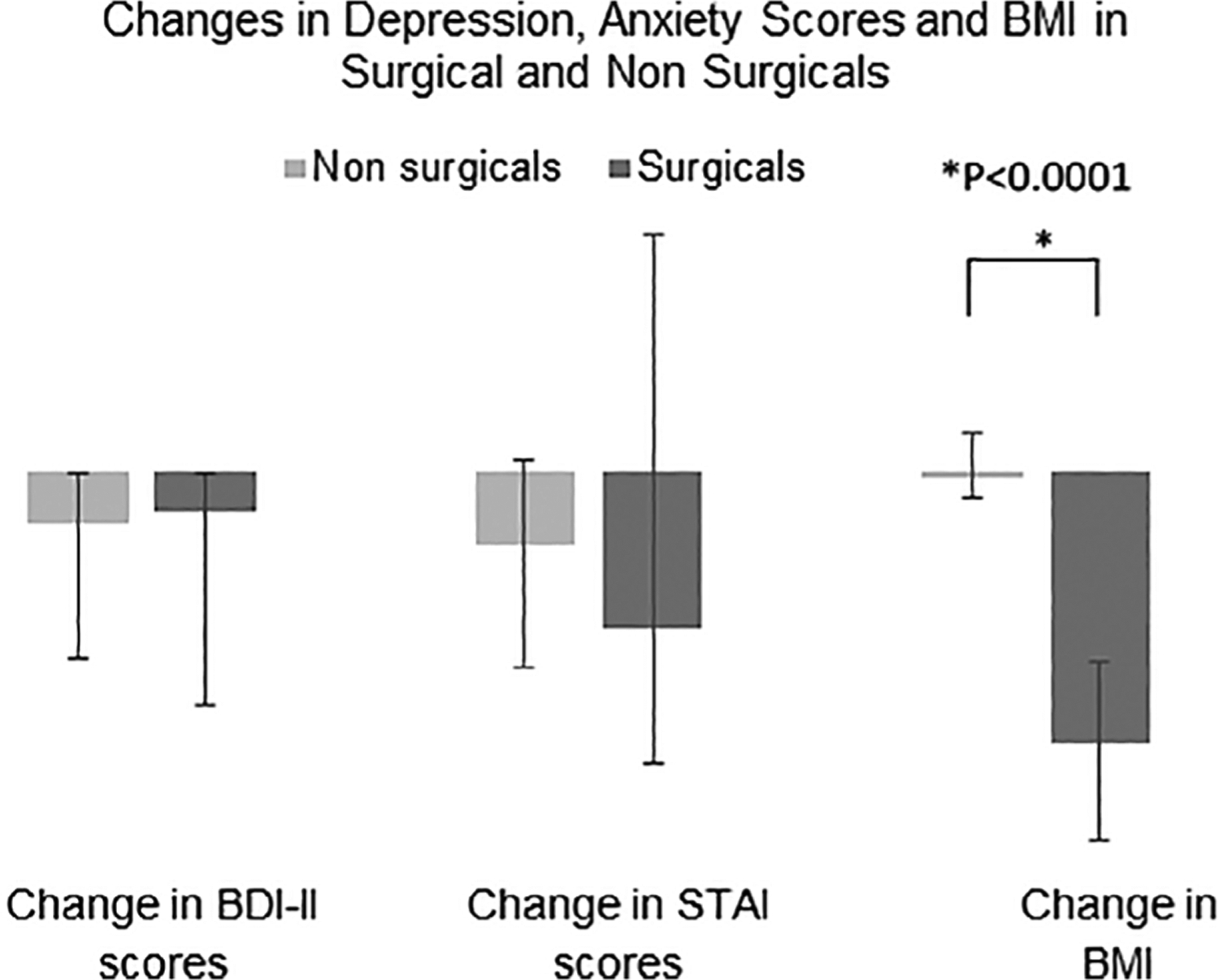
Changes in Depression, Anxiety T-scores and BMI in the Surgical and Non-Surgical Groups over 6 months. BDI-II, Beck Depression Inventory-II; BMI, body mass index; STAI, State-Trait Anxiety Inventory
4 |. DISCUSSION
Our study compares depression and anxiety symptomatology and suicidal ideation between OB and NW groups. We demonstrate that depression and anxiety scores are higher in the OB group. Of concern, the suicidal ideations and suicidality is significantly higher in this group compared with NW group. In our cohort, over 6 months of follow-up, all participants with obesity experienced a reduction in depressive symptoms. However, participants who underwent weight loss surgery did not differ from non-surgical controls for change in depression and anxiety symptomatology and suicidal ideations over time despite a significant decrease in BMI at follow-up in the former.
A higher prevalence of depression and anxiety has been reported in both adolescent and adult women with obesity compared with normal-weight controls.11,13 A large database evaluating 177,047 participants more than 18 years old reported that women with overweight or obesity were more likely to have depression or anxiety compared with women of normal BMI.13 Similarly, in a cohort of 776 subjects 9–18 years old followed over a period of 20 years, females with obesity had a fourfold higher risk for subsequent major depressive disorder and anxiety compared with NW.11 Another study of 108 adolescents with obesity reported that the odds of having severe vs mild to moderate obesity was 3.5 times higher in patients with depression and five times higher for patients with anxiety.9 In our study, we show that BDI-II and STAI T-scores are higher in the OB compared to the NW group, consistent with existing literature supporting higher depressive and anxiety symptomatology in this population.
Although many studies have examined mood in adolescents and young adults with obesity, data examining suicidality in this population are limited and mixed.15–17 In our study, the OB group attested to increased suicidal ideations compared to the NW group, which is a statistically significant finding. Given that suicide is the second leading cause of death in adolescents,32 it is even more important to screen adolescents and young adults with obesity for suicidal ideations.
The psychopathology associated with increased weight states is likely multifactorial. While some have postulated that shared genetic risks33 and the underlying chronic inflammatory state in obesity are a common link in noted psychiatric alterations,34 others report that structural changes in the brain in severe obesity may be a potential contributor to mood and emotional changes.35 Diffusion indices which measure structural connectivity in areas of the brain that control feeding behaviours have been shown to correlate negatively with BMI, depression and anxiety symptoms.35 Whether changes in the hormonal milieu observed in states of severe obesity cause these structural changes is yet to be determined.
Our exploratory analyses show that there was no difference in the change in depressive and anxiety symptoms in subjects who underwent bariatric surgery compared with the non-surgical group at follow-up, despite significant weight loss in the surgical group. Data regarding psychiatric outcomes after weight loss surgery are mixed. In one multicentre study of 357 adult patients (average age 43.7 ± 10 years) followed over 24 months after weight loss surgery, rates of depression assessed using the BDI-II decreased from a baseline level of 45% to 12 and 13% at 6 and 12 months, respectively, but thereafter increased to 18% at 24 months.20 In contrast, our cohort in this exploratory analysis consisted of adolescents and young adults less than 22 years old. Zeller et al. examined 31 adolescents; mean age 16.4 years with 65% females, and showed that depressive symptoms decreased 1 year following RYGB.23 Another study in 37 adolescents who underwent RYGB showed fewer symptoms of anxiety and depression 4 months after surgery.22 A few other authors have also reported a decrease in depressive symptoms ranging from 25% to 100% at follow-up (up to 2 years).24,36–38 In contrast, Ivezaj et al. reported no change in depression scores in 74%, and an increase in scores in 13% of subjects 6–12 months post weight loss surgery.39
In our study, there were no significant improvements in depression and anxiety scores at 6 months in the surgical and non-surgical groups leading to comparable scores across groups at 6-month follow-up. The variance for the BDI-II and STAI T-scores at follow-up in our surgical subjects was high. This may have contributed to the lack of difference in the change in scores between the surgical and non-surgical groups and indicate within-group individual differences in trajectories of depressive and anxiety symptoms. Of note, most earlier studies did not compare symptoms in the surgical group to a group of non-surgical adolescents with obesity. Ratcliff et al. compared adolescents who were candidates for bariatric surgery with controls and found no differences between the two groups for depression scores; however, in this study the evaluation was done at baseline and just prior to weight loss surgery.40 Interestingly, bariatric surgery candidates had mild improvement in depression scores even before undergoing surgery likely due to a positive attitude resulting from expectation of weight loss.40 We did not find significant differences for depressive symptoms between the surgical and non-surgical groups over 6 months suggesting that weight loss may not be a prerequisite for improvement in psycho-emotional functioning in this population. However, we are limited in drawing these conclusions by the small number of subjects in the bariatric surgery group, many of whom had low follow-up rates, as is commonly seen in other studies involving these high-risk participants.41 Further, one should acknowledge the fact that a single item self-report question was used to assess suicidality in this study. The number of adolescent and young adults undergoing bariatric surgery, although increasing, is still much lower than in the adult population. As more youth undergo such procedures, more data will become available for changes in depressive and anxiety symptoms following surgery.
The fact that some of our adolescents who underwent surgery were on mood-altering medications is another limitation of the study. Monte et al. identified adult patients with obesity on treatment with medications for mood disorders who underwent sleeve gastrectomy, and demonstrated that anxiety and depression symptoms improved by >50% 3–6 months after the procedure while on medications.42 In our study, a few non-surgical and surgical subjects were on mood-altering medications prior to surgery. Thus, it is possible that there were some mood-enhancing effects from these medications in the participants. However, both surgical and non-surgical subjects were on these medications, and there were no differences between groups for depressive and anxiety scores at baseline.
Our study includes adolescents and young adults 13–21 years of age with moderate to severe obesity, and our data in this age group are a significant contribution to the existing literature. Adolescents with severe obesity have been shown to have poor quality of life comparable to children with chronic health conditions such as cancer,43 and it is possible that coexistent psychiatric comorbidities contribute to this. The high prevalence of depression and anxiety symptoms and suicidality in the OB group in our study highlights the need to evaluate underlying predisposing mechanisms in order to develop appropriate therapeutic strategies.
5 |. CONCLUSION
Depressive and anxiety symptoms are more pronounced in adolescent and young adult women with moderate to severe obesity. Of concern, suicidal ideations were more frequently observed in these women with moderate to severe obesity compared with normal-weight women. Weight loss surgeries, although beneficial for weight loss, did not result in an improvement in depressive and anxiety symptoms and suicidality in our cohort. Future research exploring psychiatric comorbidities in moderate to severe obesity and their determinants is warranted.
What is already known about this subject
Adolescents and young adult females with obesity have increased rates of depression and anxiety compared with their normal-weight peers.
Data regarding suicidal tendencies in adolescents and young adult females with obesity are limited.
Studies examining the effects of weight loss surgery on depression and anxiety symptoms in young women with obesity show mixed results.
What this study adds
Our study confirms the finding that adolescent and young adult women with moderate to severe obesity have higher suicidal ideation compared with normal-weight females.
We show that weight loss surgery in female adolescents and young adults with moderate to severe obesity does not result in improvement in depressive and anxiety symptoms over 6 months of follow-up compared with those followed without surgery.
Suicidal ideation in female adolescents and young adults with moderate to severe obesity following weight loss surgery are comparable to females with moderate to severe obesity followed without surgery.
Footnotes
CONFLICTS OF INTEREST
No conflict of interest was declared.
REFERENCES
- 1.Skinner AC, Perrin EM, Skelton JA. Prevalence of obesity and severe obesity in US children, 1999–2014. Obesity (Silver Spring). 2016;24: 1116–1123. [DOI] [PubMed] [Google Scholar]
- 2.Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics. 2018;141:e20173459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Skelton JA, Cook SR, Auinger P, Klein JD, Barlow SE. Prevalence and trends of severe obesity among US children and adolescents. Acad Pediatr. 2009;9:322–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saluja G, Iachan R, Scheidt PC, Overpeck MD, Sun W, Giedd JN. Prevalence of and risk factors for depressive symptoms among young adolescents. Arch Pediatr Adolesc Med. 2004;158:760–765. [DOI] [PubMed] [Google Scholar]
- 5.Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics. 2010;125:75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. 2011;45:1027–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vila G, Zipper E, Dabbas M, et al. Mental disorders in obese children and adolescents. Psychosom Med. 2004;66:387–394. [DOI] [PubMed] [Google Scholar]
- 8.Benson LP, Williams RJ, Novick MB. Pediatric obesity and depression: a cross-sectional analysis of absolute BMI as it relates to children’s depression index scores in obese 7- to 17-year-old children. Clin Pediatr (Phila). 2013;52:24–29. [DOI] [PubMed] [Google Scholar]
- 9.Fox CK, Gross AC, Rudser KD, Foy AMH, Kelly AS. Depression, anxiety, and severity of obesity in adolescents: is emotional eating the link? Clin Pediatr (Phila). 2016;55:1120–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sysko R, Zakarin EB, Devlin MJ, Bush J, Walsh BT. A latent class analysis of psychiatric symptoms among 125 adolescents in a bariatric surgery program. Int J Pediatr Obes. 2011;6:289–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson SE, Cohen P, Naumova EN, Jacques PF, Must A. Adolescent obesity and risk for subsequent major depressive disorder and anxiety disorder: prospective evidence. Psychosom Med. 2007;69: 740–747. [DOI] [PubMed] [Google Scholar]
- 12.Britz B, Siegfried W, Ziegler A, et al. Rates of psychiatric disorders in a clinical study group of adolescents with extreme obesity and in obese adolescents ascertained via a population based study. Int J Obes Relat Metab Disord. 2000;24:1707–1714. [DOI] [PubMed] [Google Scholar]
- 13.Zhao G, Ford ES, Dhingra S, Li C, Strine TW, Mokdad AH. Depression and anxiety among US adults: associations with body mass index. Int J Obes (Lond). 2009;33:257–266. [DOI] [PubMed] [Google Scholar]
- 14.Heneghan HM, Heinberg L, Windover A, Rogula T, Schauer PR. Weighing the evidence for an association between obesity and suicide risk. Surg Obes Relat Dis. 2012;8:98–107. [DOI] [PubMed] [Google Scholar]
- 15.van Wijnen LG, Boluijt PR, Hoeven-Mulder HB, et al. Weight status, psychological health, suicidal thoughts, and suicide attempts in Dutch adolescents: results from the 2003 E-MOVO project. Obesity. 2010; 18:1059–1061. [DOI] [PubMed] [Google Scholar]
- 16.Zeller MH, Reiter-Purtill J, Jenkins TM, Ratcliff MB. Adolescent suicidal behavior across the excess weight status spectrum. Obesity. 2013;21:1039–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldstein BI, Birmaher B, Axelson DA, et al. Preliminary findings regarding overweight and obesity in pediatric bipolar disorder. J Clin Psychiatry. 2008;69:1953–1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaplan MS, McFarland BH, Huguet N. The relationship of body weight to suicide risk among men and women: results from the US National Health Interview Survey Linked Mortality File. J Nerv Ment Dis. 2007;195:948–951. [DOI] [PubMed] [Google Scholar]
- 19.Mukamal KJ, Kawachi I, Miller M, Rimm EB. Body mass index and risk of suicide among men. Arch Intern Med. 2007;167:468–475. [DOI] [PubMed] [Google Scholar]
- 20.White MA, Kalarchian MA, Levine MD, Masheb RM, Marcus MD, Grilo CM. Prognostic significance of depressive symptoms on weight loss and psychosocial outcomes following gastric bypass surgery: a prospective 24-month follow-up study. Obes Surg. 2015;25:1909–1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ribeiro G, Giapietro HB, Belarmino LB, Salgado-Junior W. Depression, anxiety, and binge eating before and after bariatric surgery: problems that remain. Arq Bras Cir Dig. 2018;31:e1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jarvholm K, Olbers T, Marcus C, et al. Short-term psychological outcomes in severely obese adolescents after bariatric surgery. Obesity (Silver Spring). 2012;20:318–323. [DOI] [PubMed] [Google Scholar]
- 23.Zeller MH, Modi AC, Noll JG, Long JD, Inge TH. Psychosocial functioning improves following adolescent bariatric surgery. Obesity (Silver Spring). 2009;17:985–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zeller MH, Reiter-Purtill J, Ratcliff MB, Inge TH, Noll JG. Two-year trends in psychosocial functioning after adolescent Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2011;7:727–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ackerman KE, Singhal V, Baskaran C, et al. Oestrogen replacement improves bone mineral density in oligo-amenorrhoeic athletes: a randomised clinical trial. Br J Sports Med. 2019;53:229–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kelly AS, Barlow SE, Rao G, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128:1689–1712. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention. Defining Childhood Obesity. Atlanta, GA: Centers for Disease Control and Prevention. 2018: [Google Scholar]
- 28.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 29.Charles D, Spielberger RLG, Lushene R. State-Trait Anxiety Inventory for Adults—Form X. Menlo Park, CA: Mind Garden, Inc; 1970. [Google Scholar]
- 30.Spielberger CD et al. Manual for the State-Trait Anxiety Inventory (Form Y). Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 31.Vautier S A longitudinal SEM approach to STAI data:two comprehensive multitrait-multistate models. J Pers Assess. 2004;83: 167–179. [DOI] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. WISQARS Leading Causes of Death Report. Atlanta, GA: Centers for Disease Control and Prevention, 2017. https://www.nimh.nih.gov/health/statistics/suicide.shtml#part_154968NIMH. 2017. [Google Scholar]
- 33.Afari N, Noonan C, Goldberg J, et al. Depression and obesity: do shared genes explain the relationship? Depress Anxiety. 2010;27: 799–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schachter J, Martel J, Lin CS, et al. Effects of obesity on depression: a role for inflammation and the gut microbiota. Brain Behav Immun. 2018;69:1–8. [DOI] [PubMed] [Google Scholar]
- 35.Chen VC-H, Liu Y-C, Chao S-H, et al. Brain structural networks and connectomes: the brain–obesity interface and its impact on mental health. Neuropsychiatr Dis Treat. 2018;14:3199–3208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sysko R, Devlin MJ, Hildebrandt TB, Brewer SK, Zitsman JL, Walsh BT. Psychological outcomes and predictors of initial weight loss outcomes among severely obese adolescents receiving laparoscopic adjustable gastric banding. J Clin Psychiatry. 2012;73:1351–1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Herget S, Rudolph A, Hilbert A, Bluher S. Psychosocial status and mental health in adolescents before and after bariatric surgery: a systematic literature review. Obes Facts. 2014;7:233–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jarvholm K, Karlsson J, Olbers T, et al. Two-year trends in psychological outcomes after gastric bypass in adolescents with severe obesity. Obesity. 2015;23:1966–1972. [DOI] [PubMed] [Google Scholar]
- 39.Ivezaj V, Grilo CM. When mood worsens after gastric bypass surgery: characterization of bariatric patients with increases in depressive symptoms following surgery. Obes Surg. 2015;25: 423–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ratcliff MB, Reiter-Purtill J, Inge TH, Zeller MH. Changes in depressive symptoms among adolescent bariatric candidates from preoperative psychological evaluation to immediately before surgery. Surg Obes Relat Dis. 2011;7:50–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Halvorson EE, Skelton JA. Appointment attendance in a pediatric weight management clinic. Clin Pediatr. 2012;51: 888–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Monte SV, Russo KM, Mustafa E, Caruana JA. Impact of sleeve gastrectomy on psychiatric medication use and symptoms. J Obes. 2018; 2018:8532602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA. 2003;289:1813–1819. [DOI] [PubMed] [Google Scholar]


