Abstract
Introduction/Objectives:
Many health systems screen patients for social determinants of health and refer patients with social needs to community service organizations for assistance. We developed a framework based on sequential steps to evaluate this process.
Methods:
We reviewed efforts by The MetroHealth System in Cleveland, Ohio and identified 6 sequential steps: patient screened, has social needs, consents to referral to a service organization, referral placed, referral accepted, and referral outcome. Referral outcomes were categorized as resolved (organization provided requested service or patient self-resolved problem), or unresolved (patient unable to be contacted or declined assistance). We then determined the numbers of patients with food insecurity who completed each step, how completion differed by patient characteristics and service organization, and reasons for failure to complete specific steps.
Results:
We used the framework to evaluate screening and assistance steps among 5741 patients who attended a COVID-19 vaccine clinic from February 15-March 31, 2021 and were followed through April 30, 2021. The percentage of patients who completed each step ranged from 17-98%. Step completion differed by patient age, patient race, and clinic. Of 360 referrals accepted by community organizations, 98 (27%) were resolved. The most common reasons for unresolved referrals were inability of service organization to contact patients (151), no reason stated (71), and patients declined service (30).
Conclusions:
A framework based on sequential steps may be used to evaluate social determinants of health screening and assistance programs. Further work is needed to address reasons for failure to complete steps, to include patient perspectives, and to determine long-term outcomes.
Keywords: social determinants, social services, food insecurity
Introduction
Because social determinants influence healthcare cost, quality, and outcomes, many health systems are screening patients for social needs and referring them to community service organizations for assistance. 1 Examples of topics addressed in screening include food, housing, transportation, utilities, and exposure to interpersonal violence. A recent large national study of primary care clinics and emergency departments found that 65% of patients had one or more social needs. The most common needs were related to housing (52%) and food (41%). 2
The overall impact of specific interventions has been evaluated. For example, participant observation, questionnaires, interviews, and focus groups have been used to determine the impact of food assistance programs. 3 However, there has been limited work to evaluate each step of the screening and assistance process. In particular, it would be important to know how well this process works overall and for specific patient subgroups, whether service organizations have resources to help referred patients, and what the most common barriers to referral and assistance are.
We sought to develop and use a framework based on sequential steps for evaluating social determinants of health screening and assistance. We illustrate this approach by focusing on patients who attended our health system’s COVID-19 vaccine clinics and reported having food insecurity. We focused on food insecurity because it is common need among our patients and leads to numerous referrals to community organizations.
Methods
The MetroHealth System Institute for Health, Opportunity, Partnership, and Empowerment initiated a program to systematically screen patients for social determinants of health and refer patients with social needs to a network of over 80 community service organizations for help such as food assistance, financial counseling, transportation, housing and utility assistance, educational programs, and mental health treatment. Screening occurred (1) in-person or by telephone through contact with a care coordinator or other staff person or (2) online through a MyChart patient portal questionnaire triggered by an appointment for a primary care, OB-GYN, or geriatrics visit.
Beginning on January 15, 2021, the MetroHealth System offered COVID-19 vaccines to patients at multiple clinical locations in and near Cleveland, Ohio. From February 15-March 30, Institute staff approached and administered a social determinants of health questionnaire (Appendix) to patients after they were vaccinated at 7 clinic locations. The questionnaire asked about 9 topics, including food insecurity, financial strain, transportation limitations, inability to pay for housing or utilities, intimate partner violence, social isolation, infrequent physical activity, daily stress, and lack of internet access. The questions were obtained from previously validated surveys.4-11 Patients also wrote their names and dates of birth on these paper questionnaires. Patients who answered often or sometimes to either of the 2 food security questions were categorized as being food insecure. Staff then reviewed responses and asked patients with social needs for permission to refer them to community service organizations. Patients were not told about specific assistance programs while they were in the vaccine clinics.
Within 1 week after screening, staff used Unite Us, an electronic referral platform, to refer patients to specific community organizations. Patients were then contacted by community organizations to arrange for assistance. The types of food assistance included help to assess benefits eligibility, identify local food resources, access emergency food pantries and distributions, and apply for the Supplemental Nutrition Assistance Program (SNAP). This process is generally completed within 30 days of initial screening for food insecurity. It is worth noting that referral resolution may take longer for other social needs that are more complex and may have waiting lists, for example, housing. Based on reports received from service organizations by April 30, we determined if referrals were accepted or declined (because organization does not provide requested service or patient ineligible for service) and their outcomes. Referral outcomes were categorized as resolved (organization provided requested service or patient self-resolved problem), or unresolved (patient unable to be contacted or declined assistance).
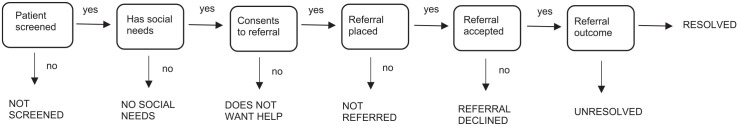
We identified 6 sequential steps based on our experience with this process. The steps include patient screened, has social needs, consents to referral to service organization, referral placed, referral accepted, and referral resolved (Figure 1). We used these steps as a framework to evaluate the screening and assistance process and illustrate this approach for food insecurity. For each step, we determined the number of patients who were available to complete the step and the percentage of those patients who actually completed the step. We used a similar method to evaluate referrals accepted and resolved. The number of referrals is slightly larger than the number of patients because some patients had food insecurity referrals to more than 1 service organization or for multiple needs. For example, a patient might be referred to a food bank for emergency food and assistance in signing up for SNAP and to another organization for prepared meals. Next, we examined completion of steps for age, gender, race, and vaccine clinic subgroups. We also used logistic regression to examine completion of each step after adjustment for patient demographic characteristics (listed in Table 1) and vaccine clinic. Finally, we examined referral results for a specific service organization (ie, a food bank) and quantified the reasons for failure to complete specific steps based on staff notes and service organization reports.
Figure 1.
Sequential steps in social determinants of health screening and assistance.
Table 1.
Characteristics of Screened Patients, Patients With and Without Food Insecurity, and Patients With and Without Referrals.*
| Patients screened | Have food insecurity | Referrals placed | |||||
|---|---|---|---|---|---|---|---|
| Yes | No | P-value | Yes | No | P-value | ||
| Number of patients | 5741 | 988 | 4753 | 356 | 492 | ||
| Age, years | 63.7 (11.4) | 62.9 (10.6) | 63.7 (11.7) | <.001 | 65.1 (9.6) | 60.5 (10.7) | <.001 |
| Female (%) | 3470 (60) | 624 (63) | 2708 (60) | .06 | 227 (64) | 308 (63) | .73 |
| Race (%) | |||||||
| White | 3321 (58) | 415 (42) | 2793 (62) | <.001 | 126 (35) | 213 (43) | .05 |
| Black | 1935 (34) | 462 (47) | 1371 (30) | 187 (53) | 222 (45) | ||
| Other | 205 (4) | 45 (5) | 153 (3) | 13 (4) | 26 (5) | ||
| Unknown | 280 (5) | 66 (7) | 198 (4) | 30 (8) | 31 (6) | ||
| Ethnicity (%) | |||||||
| Hispanic | 260 (5) | 72 (7) | 171 (4) | <.001 | 28 (8) | 38 (8) | .68 |
| Non-Hispanic | 5220 (91) | 880 (89) | 4132 (91) | 314 (88) | 440 (89) | ||
| Unknown | 261 (5) | 36 (4) | 212 (5) | 14 (4) | 14 (3) | ||
| Marital status (%) | |||||||
| Married | 2701 (47) | 328 (33) | 2256 (50) | <.001 | 124 (35) | 152 (31) | .32 |
| Widowed | 456 (8) | 80 (8) | 358 (8) | 29 (8) | 39 (8) | ||
| Divorced | 737 (13) | 172 (17) | 537 (12) | 63 (18) | 79 (16) | ||
| Single | 1651 (29) | 382 (39) | 1204 (27) | 126 (35) | 214 (43) | ||
| Other | 8 (0.1) | 4 (0.4) | 4 (0.1) | 1 (0.2) | 2 (0.4) | ||
| Unknown | 188 (3) | 22 (2) | 156 (3) | 13 (4) | 6 (1) | ||
| Primary health insurance (%) | |||||||
| Medicare | 2688 (47) | 489 (49) | 2075 (46) | <.001 | 208 (58) | 198 (40) | <.001 |
| Medicaid | 712 (12) | 247 (25) | 440 (10) | 74 (21) | 148 (30) | ||
| Private | 1,801 (31) | 173 (18) | 1564 (35) | 51 (14) | 102 (21) | ||
| Uninsured | 224 (4) | 42 (4) | 169 (4) | 13 (4) | 23 (5) | ||
| Other | 195 (3) | 10 (1) | 183 (4) | 3 (1) | 5 (1) | ||
| Unknown | 121 (2) | 27 (3) | 84 (2) | 7 (2) | 16 (3) | ||
| Median annual zip code income (%) | |||||||
| Less than $20,000 | 1,106 (19) | 300 (30) | 752 (17) | <.001 | 122 (34) | 141 (29) | 0.16 |
| $20,000-$29,999 | 2,181 (38) | 401 (41) | 1681 (37) | 150 (42) | 198 (40) | ||
| $30,000-$39,999 | 1,457 (25) | 190 (19) | 1230 (27) | 56 (16) | 102 (21) | ||
| $40,000 or higher | 907 (16) | 81 (8) | 785 (17) | 23 (7) | 44 (9) | ||
| Unknown | 90 (2) | 16 (2) | 67 (2) | 5 (1) | 7 (1) | ||
| Social determinants of health (%) | |||||||
| Food insecurity | 988 (17) | — | — | — | — | ||
| Financial strain | 347 (6) | 199 (20) | 137 (3) | <.001 | 77 (22) | 94 (19) | .13 |
| Transportation limitations | 299 (5) | 168 (17) | 116 (3) | <.001 | 71 (20) | 79 (16) | .16 |
| Unable to pay for housing or utilities | 1,264 (22) | 414 (42) | 787 (17) | <.001 | 149 (42) | 218 (44) | .73 |
| Intimate partner violence | 71 (1) | 25 (2) | 46 (1) | <.001 | 4 (1) | 14 (3) | .09 |
| Social isolation | 2,587 (45) | 549 (56) | 1914 (42) | <.001 | 196 (55) | 270 (55) | .55 |
| Infrequent physical activity | 1,195 (21) | 226 (23) | 925 (20) | <.001 | 96 (27) | 101 (21) | .07 |
| Daily stress | 829 (14) | 273 (28) | 537 (12) | <.001 | 94 (26) | 140 (28) | .81 |
| Lack of internet access | 245 (4) | 84 (8) | 147 (3) | <.001 | 35 (10) | 37 (8) | .36 |
Results are number (percentage) for categorical variables and mean (standard deviation) for continuous variables.
This program evaluation does not qualify as human subjects research and did not require Institutional Review Board review or approval. All analyses were conducted using R version 4.0.3, Vienna, Austria.
Results
A total of 9537 patients received COVID-19 vaccines from February 15-March 30 at 7 clinics. Of these, 5741 (60%) completed a social determinants of health screening questionnaire. Screened patients had a mean age of 63.7 years (Table 1). A majority were female and about half had Medicare as their primary health insurance. Food insecurity was reported by 988 (17%) patients. Compared to patients without food insecurity, patients with food insecurity were more likely to be Black, have Medicaid, and have a lower income.
Completion of specific screening and assistance steps related to food insecurity are listed in Table 2. For example, 848 of the 988 patients (86%) reporting food insecurity consented to a referral for assistance and 356 of these 848 (42%) had a referral placed. Of 360 referrals accepted by community organizations, 98 (27%) were resolved. Compared to younger patients, older patients were more likely to have referrals placed (58% vs 31%, P < .001) and referrals resolved (34% vs 18%, P < .001). Compared to Whites, Blacks were more likely to have food insecurity (24% vs 12%, P < .001). The Greater Cleveland Food Bank was the primary recipient of referrals for food assistance programs (356 of 366 referrals).
Table 2.
Completion of Specific Food Insecurity Screening and Assistance Steps by All Patients and Illustrative Subgroups.
| Group | Number of patients | Patients screened (%) | Have food insecurity (%) | Consents to referral (%) | Referrals placed (%) | Total referrals | Referrals accepted (%) | Referrals resolved (%) |
|---|---|---|---|---|---|---|---|---|
| All patients | 9537 | 5741/9537 (60) | 988/5741 (17) | 848/988 (86) | 356/848 (42) | 366 | 360/366 (98) | 98/360 (27) |
| Age* | ||||||||
| <65 years | 4368 | 2985/4368 (68) | 560/2985 (19) | 497/560 (89) | 152/497 (31) | 154 | 152/154 (99) | 27/152 (18) |
| >65 years | 5163 | 2756/5163 (53) | 428/2756 (16) | 351/428 (82) | 204/351 (58) | 212 | 208/212 (98) | 71/208 (34) |
| Gender | ||||||||
| Female | 5783 | 3470/5783 (60) | 624/3470 (18) | 535/624 (86) | 227/535 (42) | 236 1 | 231/236 (98) | 66/231 (29) |
| Male | 3754 | 2271/3754 (60) | 364/2271 (16) | 313/364 (86) | 129/313 (41) | 30 | 129/130 (99) | 32/129 (25) |
| Race | ||||||||
| White | 5290 | 3321/5290 (63) | 415/3321 (12) | 339/415 (82) | 126/339 (37) | 126 | 126/126 (100) | 34/126 (27) |
| Black | 3348 | 1935/3348 (58) | 462/1935 (24) | 409/462 (89) | 187/409 (46) | 196 | 189/196 (96) | 53/189 (28) |
| Vaccination clinic | ||||||||
| Bedford | 2420 | 1307/2420 (54) | 221/1307 (17) | 191/221 (86) | 135/191 (71) | 140 | 139/140 (99) | 48/139 (35) |
| Parma | 3610 | 2423/3610 (67) | 376/2423 (16) | 314/376 (84) | 110/314 (35) | 111 | 110/111 (99) | 29/110 (26) |
| Cleveland Heights | 2267 | 1309/2267 (58) | 248/1309 (19) | 216/248 (87) | 94/216 (44) | 98 | 94/98 (96) | 12/94 (13) |
| Northfield | 940 | 583/940 (62) | 110/583 (19) | 101/110 (92) | 2/101 (2) | 2 | 2/2 (100) | 2/2 (100) |
| Other | 300 | 119/300 (40) | 33/119 (28) | 26/33 (79) | 15/26 (58) | 15 | 15/15 (100) | 7/15 (47) |
| Referred to** Greater Cleveland Food Bank | — | — | — | — | — | 356 | 356/356 (100) | 96/356 (27) |
| Benjamin Rose Institute on aging | — | — | — | — | — | 5 | 1/5 (20) | 0/1 (0) |
| AmeriCorps program | — | — | — | — | — | 2 | 1/2 (50) | 0/1 (0) |
| Fairhill partners | — | — | — | — | — | 1 | 1/1 (100) | 1/1 (100) |
| Providence house | — | — | — | — | — | 1 | 0/1 (0) | 0/0 (—) |
| Western Reserve Area Agency on aging | — | — | — | — | — | 1 | 1/1 (100) | 1/1 (100) |
Age missing for 6 unscreened patients.
Analyses only applicable to referrals.
Multivariate analyses for each step are listed in Table 3. There were differences by vaccination clinic in completion of several steps. For example, patients at the Parma clinic were more likely to be screened and to have food insecurity but less likely to have referrals placed.
Table 3.
Multivariate Analysis of Completion of Specific Food Insecurity Screening and Assistance Steps.*
| Patients screened | Have food insecurity | Consents to referral | Referrals placed | Referrals resolved | |
|---|---|---|---|---|---|
| Age | |||||
| <65 years | Reference | Reference | Reference | Reference | Reference |
| >65 years | 0.53 (<.001) | 0.59 (<.001) | 0.70 (.37) | 2.63 (<.001) | 1.59 (.20) |
| Gender | |||||
| Female | Reference | Reference | Reference | Reference | Reference |
| Male | 1.02 (.63) | 0.53 (.62) | 1.02 (.95) | 0.93 (.66) | 1.12 (.70) |
| Race | |||||
| White | Reference | Reference | Reference | Reference | Reference |
| Black | 0.81 (<.001) | 0.93 (.87) | 0.67 (.71) | 1.21 (.65) | 0.65 (.54) |
| Vaccination clinic | |||||
| Bedford | Reference | Reference | Reference | Reference | Reference |
| Parma | 1.74 (<.001) | 1.30 (.02) | 1.15 (.35) | 0.58 (.001) | 0.69 (.34) |
| Cleveland heights | 1.16 (.01) | 0.86 (.17) | 0.65 (.004) | 0.51 (.002) | 0.26 (.001) |
| Northfield | 1.39 (<.001) | 0.83 (.22) | 1.61 (.09 | 0.04 (<.001) | Reference |
| Other | 0.56 (<.001) | 4.94 (<.001) | 2.66 (.34) | 4.08 (<.001) | 1.84 (.32) |
Numbers in each cell represent odds ratios (P values).
Unable to perform analyses for referrals accepted because acceptance rate was close to 100% for all subgroups.
The reasons for failure to complete specific steps are listed in Table 4. The reasons were sometimes not elicited or recorded. For example, the reasons for unresolved referrals were unclear in 71 cases.
Table 4.
Reasons for Failure to Complete Specific Food Insecurity Screening and Assistance Steps.
| Step not completed | Reasons for failure to complete (number of patients or referrals) |
|---|---|
| Patient not screened | Patient not approached for screening (number not recorded) |
| Patient declined screening (number not recorded) | |
| Patient does not have food insecurity | Patient not at risk for food insecurity based on screening questionnaire (4753) |
| Patient does not want help | Patient did not consent to referral to community service organizations (140) |
| Patient not referred | Reasons not recorded (492) |
| Referral declined | Patient ineligible for services (3) |
| Community organization does not provide service requested (2) | |
| Missing reason (1) | |
| Referral unresolved | Patient unable to be contacted (151) |
| Patient declined services (30) | |
| Patient denied having food insecurity (8) | |
| Duplicate referral (2) | |
| Missing reason (71) |
Discussion
As value-based care arrangements between health care payers and providers increasingly shift responsibility for health care quality and costs to providers, assessing and addressing the non-clinical factors that impact these outcomes is assuming greater importance among providers. Electronic social care referral platforms are being deployed as a method to achieve these goals, but little is yet known about their impact. We focused on food insecurity because it is one of the most prevalent health-related social needs reported by patients, and resources to address this need are present in many communities. Since the link between an unhealthy diet and poor control of chronic illnesses such as diabetes, hypertension, and heart disease is well established, addressing food insecurity may lead to better control of these conditions as well as lower health care costs.
Examining sequential steps related to social determinants of health screening and assistance provides insight into how well this process works. We found that there may be opportunities for health systems, community organizations, and research teams to work together to increase screening, placement of referrals, and resolution of referrals. There are also sizeable demographic disparities that need to be examined and reduced. More detailed information on reasons for failure to complete specific steps should help improve the process (see Table 4). Because differences in step completion rates by clinic persisted after adjustment for patient characteristics (Table 3), we hypothesize that there were differences in the number and expertise of staff across sites.
By contrast, the rate of acceptance of referrals was very high, particularly by the Greater Cleveland Food Bank (Table 2). This community organization is our primary referral partner for food insecurity and has capacity to accept and act on referrals in a timely manner. They employ a team dedicated to food and benefits navigation who work via telephone to assist individuals in need. They also serve all who may be in need, without strict eligibility criteria.
Several recent studies provide additional context for our results. A study of 2 urban neighborhoods in Cleveland and Columbus, Ohio, found a much higher rate of food insecurity (57%), perhaps because the neighborhoods were purposely selected as low-income and with low access to healthy food. 12 A Boston study examined 3 parts of the screening and referral process, including proportion of eligible patients screened, providers signing orders for positive patient screenings, and provider orders for resource referral guides among patients requesting resource connections. The investigators found that about 70% of eligible patients were screened, 82% of patients with a social need had ICD-10 codes added to their visit diagnoses, and 86% of patients requesting resources received a resource referral guide. 13 A qualitative evaluation of a pediatric social determinants of health screening and referral program focused on the perspective of 7 caregivers. Caregivers reported overall satisfaction with the program but identified a number of areas for improvement such as streamlining the referral process. 14
Based on our experience, we suggest several measures to increase completion of specific steps. Ensure that there are sufficient and trained staff to administer the screening questionnaire and to address any problems or concerns patients have about answering questions. Ask patients if they want assistance immediately after they screen positive instead of contacting them at a later date to find out if they want help. This will reduce staff workload as well as problems reaching patients. Obtain alternate contact information, for example, a second phone number, an electronic mail address, or the name and phone number of a family member, to use if the primary contact information doesn’t work. Keep track of detailed reasons for patients not referred and referrals unresolved and use this information to refine the process.
Strengths of this study include a large and diverse patient sample, standardized assessment of social determinants and needs, and information on completion of each step. Limitations include a modest number of referrals, a focus on one health system, and lack of details about why certain steps were not completed. In addition, elderly and high-risk populations preferentially received COVID-vaccinations during the time period of our study. As a result, the findings may not apply to healthy, younger adults. The need to quickly establish new vaccine clinics also limited our ability to train and deploy staff for screening and referrals.
Our approach may be used by other health systems to evaluate similar efforts for food insecurity or for other social determinants. Based on our experience with the framework, we recommend 4 refinements. First, health systems and community service organizations should develop methods to better identify and address reasons for failure to complete specific steps. Second, patient perspectives should be added to the framework and corresponding evaluations. For example, why do patients think specific steps are not completed? How do patients rate the timeliness and usefulness of services provided by community organizations? Third, health systems should repeat social determinants questions after receipt of services to determine if social needs are still present. Fourth, health systems should determine the long-term impact of these programs on patient health, cost, and quality of life outcomes.
Appendix. Social Determinants of Health Questionnaire
MetroHealth is committed to providing quality health care and resources to help you live a healthy life.
The questions below will help us understand how you are doing and if you might need additional assistance.
Physical Activity
On average, how many days per week do you engage in moderate to strenuous exercise (like walking fast, jogging, dancing, swimming, biking, or other activities that cause a light or heavy sweat)?
☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 Days
On average, how many minutes do you engage in exercise at this level?
☐ 0 ☐ 10 ☐ 20 ☐ 30 ☐ 40 ☐ 50 ☐ 60 ☐ 70 ☐ 80 ☐ 90 Min
Financial Stability
How hard is it for you to pay for basics like food, housing, medical care, and heating?
☐ Not at all ☐ Not very hard ☐ Somewhat hard ☐ Hard ☐ Very hard
Housing and Utilities
In the last 12 months:
Were you unable to pay the rent or mortgage on time? ☐ Yes ☐ No
Did you not have a steady place to sleep, or sleep in a shelter? ☐ Yes ☐ No
How many places have you lived?
Do you have any problems at home with: ☐ Lack of heat ☐ Water leaks ☐ Mold ☐ Pests
☐ Lead paint or pipes ☐ Oven/stove not working ☐ Smoke detectors not working ☐ None
In the last 12 months, has the electric, gas, oil, or water company threatened to shut off your services?
☐ Yes ☐ No ☐ Currently shut off
Transportation
In the last 12 months, has lack of transportation:
Kept you from medical appointments or from getting medications? ☐ Yes ☐ No
Kept you from meetings, work, or getting things needed for daily living? ☐ Yes ☐ No
Food Security
In the last 12 months:
- Have you worried your food would run out before you had money to buy more?
- ☐ Never ☐ Sometimes ☐ Often
- Did the food you bought just not last and you didn’t have money to buy more?
- ☐ Never ☐ Sometimes ☐ Often
Stress
How often do you feel stress these days (tense, restless, nervous, anxious, or trouble sleeping)?
☐ Not at all ☐ Only a little ☐ To some extent ☐ Rather much ☐ Very Much
Social Connections
In a typical week, how often do you talk on the phone with family, friends, or neighbors?
☐ Never ☐ Once a week ☐ Twice a week ☐ 3 times a week ☐ More than 3 × week
How often do you get together with friends or relatives?
☐ Never ☐ Once a week ☐ Twice a week ☐ 3 times a week ☐ More than 3 × week
How often do you attend church or religious services?
☐ Never ☐ 1 to 4 times per year ☐ more than 4 times per year
Do you belong to any clubs or organizations (such as church groups, unions, fraternal, athletic, or school)? ☐ Yes ☐ No
How often do you attend meetings of the clubs or organizations you belong to?
☐ Never ☐ 1 to 4 times per year ☐ more than 4 times per year
Are you currently:
☐ Married ☐ Widowed ☐ Divorced ☐ Separated ☐ Never married ☐ Living with partner
Personal Safety
Within the last 12 months, have you been:
Afraid of your partner or ex-partner? ☐ Yes ☐ No
Humiliated or emotionally abused by your partner or ex-partner? ☐ Yes ☐ No
Kicked, hit, slapped, or otherwise physically hurt by your partner or ex-partner? ☐ Yes ☐ No
Forced to have any kind of sexual activity by your partner or ex-partner? ☐ Yes ☐ No
Digital Connectivity
Do you currently have internet access at home? ☐ Yes ☐ No
Do you have internet access on a device or in another location? ☐ Yes ☐ No
If Yes, where? ☐ On a cell phone ☐ At work ☐ Other (Library) ☐ Multiple access options
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Kevin Chagin  https://orcid.org/0000-0002-8618-9419
https://orcid.org/0000-0002-8618-9419
Ashwini R. Sehgal  https://orcid.org/0000-0002-7458-2731
https://orcid.org/0000-0002-7458-2731
References
- 1. National Academies of Sciences, Engineering, and Medicine. Integrating Social Care Into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. The National Academies Press; 2019. [PubMed] [Google Scholar]
- 2. De Marchis EH, Hessler D, Fichtenberg C, et al. Assessment of social risk factors and interest in receiving health care-based social assistance among adult patients and adult caregivers of pediatric patients. JAMA Network Open. 2020;3(10):e2021201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Loopstra R. Interventions to address household food insecurity in high-income countries. Proc Nutr Soc. 2018;77:270-281. [DOI] [PubMed] [Google Scholar]
- 4. Puterman E, Haritatos J, Adler NE, Sidney S, Schwartz JE, Epel ES. Indirect effect of financial strain on daily cortisol output through daily negative to positive affect index in the coronary artery risk development in young adults study. Psychoneuroendocrinology. 2013;38:2883-2889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126:e26-e32. [DOI] [PubMed] [Google Scholar]
- 6. Sohal H, Eldridge S, Feder G. The sensitivity and specificity of four questions (HARK) to identify intimate partner violence: a diagnostic accuracy study in general practice. BMC Fam Pract. 2007;8:49-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Coleman KJ, Ngor E, Reynolds K, et al. Initial validation of an exercise “vital sign” in electronic medical records. Med Sci Sports Exerc. 2012;44:2071-2076. [DOI] [PubMed] [Google Scholar]
- 8. Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N. Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am J Public Health. 2013;103:2056-2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Elo AL, Leppänen A, Jahkola A. Validity of a single-item measure of stress symptoms. Scand J Work Environ Health. 2003;29:444-451. [DOI] [PubMed] [Google Scholar]
- 10. National Association of Community Health Centers; 2016. Protocol for responding to and assessing patients’ assets, risks, and experiences (PRAPARE). Accessed June 25, 2021. https://www.nachc.org/wp-content/uploads/2020/04/PRAPARE-One-Pager-9-2-16-with-logo-and-trademark.pdf
- 11. De Marchis EH, Ettinger de Cuba SA, Chang L, et al. Screening discordance and characteristics of patients with housing-related social risks. Am J Prev Med. 2021;61:e1-e12. [DOI] [PubMed] [Google Scholar]
- 12. Banks AR, Bell BA, Ngendahimana D, Embaye M, Freedman DA, Chisolm DJ. Identification of factors related to food insecurity and the implications for social determinants of health screenings. BMC Public Health. 2021;21:1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. De La Vega PB, Losi S, Sprague Martinez L, et al. Implementing an EHR-based screening and referral system to address social determinants of health in primary care. Med Care. 2019;57(Suppl 2):S133-S139. [DOI] [PubMed] [Google Scholar]
- 14. Emengo VN, Williams MS, Odusanya R, et al. Qualitative program evaluation of social determinants of health screening and referral program. PLoS One. 2020;15(12):e0242964. [DOI] [PMC free article] [PubMed] [Google Scholar]