Abstract
Introduction
Chronic kidney disease (CKD) is a major threat to public health, especially in low-income and lower middle-income countries, where resources for treating patients with advanced CKD are scarce. Although early CKD identification and intervention hold promise for reducing the burden of CKD and risk factors, it remains unclear if an uniform strategy can be applicable across all income groups. The aim of this scoping review is to synthesise available evidence on early CKD identification programmes in all world regions and income groups. The study will also identify efforts that have been made to use interventions and implementation of early identification programmes for CKD across countries and income groups.
Methods and analysis
This review will be guided by the methodological framework for conducting scoping studies developed by Arksey and O’Malley. Empirical (Medline, Embase, Cochrane Library, CINAHL, ISI Web of Science and PsycINFO) and grey literature references will be searched to identify studies on CKD screening, early identification and interventions across all populations. Two reviewers will independently screen references in consecutive stages of title/abstract screening and then full-text screening. We will use a general descriptive overview, tabular summaries and content analysis on extracted data.
Ethics and dissemination
The findings from our planned scoping review will enable us to identify items in early identification programmes that can be used in developing screening toolkits for CKD. We will disseminate our findings using traditional approaches that include open-access peer-reviewed publication, scientific presentations and a white paper (call to action) report. Ethical approval will not be required for this scoping review as the data will be extracted from already published studies.
Keywords: chronic renal failure, end stage renal failure, adult nephrology, epidemiology
Strengths and limitations of this study.
This study will provide a comprehensive overview (where, when, why, how, and who) of studies on early detection of chronic kidney disease (CKD).
This study will identify proportion of studies that used interventions following CKD early identification as well as the types of interventions commonly used.
This study will also provide information on where early identification programmes have become integrated or implemented in health policies and practices.
This study will also identify international variations and components of early identification programmes to be used for developing CKD screening toolkits for countries in different income groups.
We foresee that a potential limitation of this study could include our inability to access policy documents related to implementation of screening and early detection programmes, particularly in low-income and lower-middle income countries.
Introduction
Worldwide, the burden of chronic kidney disease (CKD) continues to rise. This is evidenced by its climb in ranking of global causes of death from 17th in 1990 to 12th in 2017 when the global prevalence of CKD was 697.5 million with an estimated 1.2 million deaths.1 More recently, the WHO ranked CKD as the 10th most common cause of death.2 It is currently the third fastest-growing cause of death and, according to projections, will become the fifth most common cause of years of life lost, rising from 16th in 2016.3 Even more alarmingly, although increase in CKD is occurring globally, most of this growth is projected to be in low-income and lower middle-income countries (LLMICs) and among disadvantaged and indigenous communities in high-income countries (HICs) where access to care is significantly limited.1 4
Although cost,4–6 workforce,7 leadership8 9 and organisation of care10 represent major barriers to accessing kidney care in LLMICs, the impact of cost of care and excessive out-of-pocket payment systems affect the people directly and are more devastating. While governments pay for dialysis in HICs, patients in LLMICs often have to partly or fully cover the cost of treatment out-of-pocket. One study has estimated that the annual cost of providing haemodialysis (HD) in Kenya, Nigeria and Senegal to be (International dollar) Int$1·7 billion, Int$3·5 billion and Int$450 million, respectively, equivalent to 15.2%, 55.8% and 35.8% of the total domestic government health expenditure of those countries.6 The annual cost of HD in Nepal is about US$2500, far higher than the minimum wage.11 Moreover, CKD, even in early stages, massively increases the risk of development of cardiovascular disease (CVD).12 13 In addition, other modalities of kidney replacement therapies (KRT—that is, peritoneal dialysis (PD) and kidney transplantation (KT)) are unavailable in many LLMICs. Compared with HICs, PD and KT availability was very low in low-income countries: 0.9 per million population (pmp) versus 53.0 pmp14 and 23% countries versus 89% countries, respectively.4
The massive cost of KRT suggests the need to prioritise preventive strategies to delay kidney failure, rather than expand dialysis services.6 This requires implementation of efficient and cost-effective screening and early detection and treatment programmes to delay progression of kidney disease.15–17 A few studies have shown that this is indeed possible. Out of 20 811 individuals screened for CKD in Nepal,18 4471 were found to have hypertension, diabetes, proteinuria or impaired kidney function. After 3 years of treatment with low-cost antihypertensive medications, antidiabetic medications or angiotensin converting enzyme-inhibitors (ACE-i), 63% of dipstick positive proteinuria had decreased to normal and 48% of those with mildly to moderately impaired kidney function at baseline had stabilised or improved, highlighting the impact of early disease detection for reducing or halting CKD progression and cardiovascular morbidity and mortality in such settings.18
Screening and early identification programmes are also used in HICs to assess disease burden and institute measures to improve kidney health, prevent dialysis and improve cardiovascular outcomes.19–22 However, these measures have sometimes been criticised as ineffective as they show no overall benefits23 or are not cost-effective.24 25
The concept of prevention being better than cure is not new—but preventive measures are more effective if directed at those identified to be in danger of harm. Intuitively, screening and early CKD detection should lead to better outcomes as patients and their care givers are able to apply measures to retard progression and improve outcomes; however, this has not always been the case and has prompted the age-old nephrology debate ‘To Screen or not to Screen?’.25–27 In many instances, attempts to determine CKD prevalence, increase awareness and determine cardiovascular risk through screening or early detection programmes have not been coupled with follow-up actions.28 The futility and possible harms of screening for CKD without availability of treatment have been pointed out.29 Other programmes have included interventions, for example, referral to nephrology30–32 or commencing specific therapies33 34 when CKD or risk factors were detected. Despite these, various questions persist regarding the usefulness and methodology of CKD screening programmes (table 1).15 26 29 35 36 As these questions linger, there remains limited evidence to guide choices and decisions about screening, which continues to be based on available local and regional resources as well as the cultural acceptability of modality of screening. An initial approach with risk scores and questionnaires to identify high-risk individuals appears to be potentially useful for large-scale screening. However, available models for risk prediction and CKD progression are largely based on European or North American populations and often require measuring biomarkers. This is a major inconvenience in many LLMICs, where laboratory testing is not readily available.15
Table 1.
Persisting questions on usefulness and methodology of CKD screening programmes
| Questions related to the usefulness of CKD screening | Questions related to the methodology of CKD screening |
|
|
CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate.
These persistent questions led to a controversies conference on ‘early identification and interventions in CKD’ organised by Kidney Disease Improving Global Outcomes (KDIGO) after which a consensus emerged that CKD screening coupled with risk stratification and treatment should be implemented in primary or community care settings for high-risk persons.37 Major nephrology groups and regional bodies of nephrology have also developed guidelines for CKD screening tailored to their population with differences arising around who to test (general public vs those at risk), recommended tests to use (urine protein vs serum creatinine vs cystatin C assays) and frequency of testing (once annually vs more than once annually).38–40 As most of the recommendations are largely based on evidence from observational studies (there are no randomised controlled studies assessing the benefits or harms of screening), selective approaches have been used in making recommendations for screening in different income groups and populations, including CKD hotspots.29
Due to the weak and observational nature of the evidence base, guidelines that have made recommendations have tended not to be readily accepted, based on the degree of uncertainty and the magnitude of impact of kidney disease on public health. In 2012, the report of a systematic review on CKD screening and monitoring conducted for the US Preventive Services Task Force and the American College of Physicians did not recommend CKD screening in asymptomatic adults without risk factors as no direct evidence was found that such screening improved outcomes.23 The American Society of Nephrology countered this with a strong recommendation to continue regular screening for kidney disease, regardless of an individual’s risk factors.41
Lack of awareness of CKD is still perceived as a significant challenge to tackling the public health problems of CKD, particularly in LLMIC, where most individuals with CKD remain undetected until they have progressed to kidney failure.42 Population wide studies in high-risk individuals have reported high prevalence and low awareness of CKD.43–45 In Mexico, of 1519 participants of a CKD screening programme, only 1% of those with CKD were aware, despite 71% having visited a physician in the preceding year.44 However, recent data from participants with CKD in the REasons for Geographic And Racial Differences in Stroke study, a national, longitudinal, population-based cohort did not show an association between awareness of CKD with odds of subsequent changes in health behaviours, CKD management indicators or changes in estimated glomerular filtration rate (eGFR) and urine albumin–creatinine ratio.46 The study concluded that clinician education needs to be coupled with interventions to increase popular awareness of CKD for optimal impact on health behaviours and chronic disease management indicators.
As these controversies continue and given the large body of literature on screening, early identification programmes and interventions in CKD, we have designed a scoping review to identify, describe and assess CKD early identification/screening/awareness programmes worldwide. Our aim is to synthesise available evidence on early CKD identification programmes in all world regions and income groups and to use the strengths and weaknesses of such programmes into developing a toolkit that can be used by nephrologists across all income groups for early identification and intervention programmes in CKD.
Methods and analysis
Approach
We will be guided by the methodological framework for conducting scoping studies developed by Arksey and O’Malley in 2005.47 This framework has been further enhanced by work done by others including the JBI International Committee.48–51 The framework includes five steps (with an optional sixth step): (1) identifying the research question; (2) identifying the relevant studies; (3) study selection; (4) charting the data and (5) reporting the results and (6) consultation (optional). We will also use best practices for conducting and reporting systematic reviews (ie, Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Protocols and Scoping Reviews for reporting our findings.52 53
Stage 1. Identifying the research question
We used a comprehensive approach that included screening methods, target population and interventions used in framing our research question: ‘What attempts have been made to establish CKD early detection/screening/awareness programmes?’. Using key themes in the conclusions from KDIGO37 and to be able to fully answer the main study question, other questions will need to be addressed, including:
What populations have been screened for CKD and what risk stratification has been included in screening?
What measurement methods have been used to screen for CKD?
What secondary preventive interventions have been used in those identified with CKD?
What efforts have been made to implement or integrate CKD screening programmes into health system?
We believe that answering these questions will enable us to identify all potential components required to launch and sustain a CKD screening or early detection programme.
Stage 2. Identifying the relevant studies
Development of the search strategy will aim at getting a comprehensive review of the existing evidence base. We will identify studies through a detailed search (from inception) of the following bibliographic databases: Medline (Ovid), Embase (Ovid), Cochrane Library, CINAHL, ISI Web of Science and PsycINFO. We will also search grey literature (including ProQuest Dissertations & Theses Global and Conference Proceedings Citation Index (Clarivate Analytics)) using recommended resources in consultation with our medical librarian (LH). However, we will specifically hand search for information (eg, policy documents or position papers) on guidelines for CKD early identification/screening for countries and regions that will be represented in our study. We have developed the search strategy to be used in Medline (box 1) and will adapt this strategy for other databases. The search strategy includes subject headings, related terms and key words necessary for the research question. We will use Boolean logic and operators (ie, ‘AND’, ‘OR’, ‘NOT’) to combine and refine search terms. Given the complexities associated with implementing CKD early identification programmes, and that post-programme implementation policies may not have been included in primary publications, we will search for secondary publications and documents and where necessary contact authors of selected studies to ascertain if such programmes became health policy.
Box 1. Medline search strategy.
exp Renal Insufficiency, Chronic/
Chronic Kidney disease*.mp.
chronic kidney insufficienc*.mp.
chronic renal disease*.mp.
chronic renal insufficienc*.mp.
CKD.mp.
Renal fail*.mp.
Kidney fail*.mp.
or/1–8
Multiphasic Screening/ and (programprogramme* or campaign* or strateg* or initiative*).mp.
Mass Screening/
(screen* adj2 (programprogramme* or strateg* or campaign* or initiative*)).mp.
(awareness adj3 (programprogramme* or campaign* or strateg* or initiative*)).mp.
(detect* adj3 (programprogramme* or campaign* or strateg* or initiative*)).mp.
(National Health and Nutrition Examination Survey).mp.
Kidney Early Evaluation ProgramProgramme.mp.
(Prevention of Renal and Vascular End-Stage Disease).mp.
World Kidney Day.mp.
national kidney foundation.mp.
(Screening and Early Evaluation of Kidney disease).mp.
or/15–20
21 and (screen* or detect* or awareness).mp.
or/10–14,22
9 and 23
((detect* or screen* or awareness) adj2 (“chronic kidney” or “chronic renal”)).mp.
24 or 25
exp animals/ not humans.sh.
26 not 27
Stage 3. Study selection
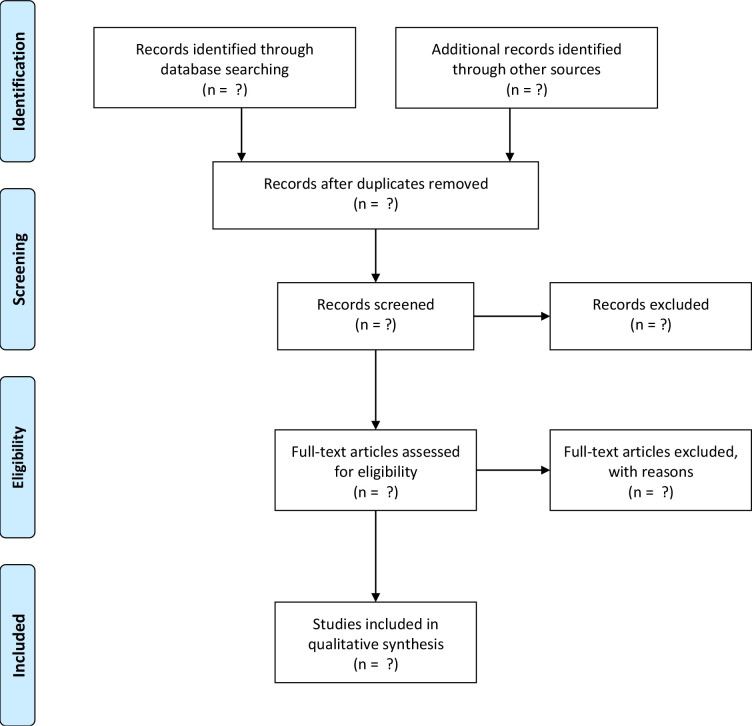
We will include studies that report the results of CKD screening. We will group the studies based on the World Bank country income groups and type of screening. Two reviewers (ET and AG) will independently screen all identified citations for potential inclusion. When agreement on a citation cannot be reached between the two reviewers, a third reviewer (MMa) will be consulted for reconciliation. The review process will first involve screening of the titles and abstracts and then a detailed review of all selected full texts to ascertain eligibility for inclusion (figure 1). An article will be included if it meets the following criteria:
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analysis flowchart for study selection.
Population: studies that provided results of CKD screening (with or without an intervention) carried out in any adult (≥18 years) population. For studies in the same population with multiple years of publications, the result of the latest study will be used, and studies conducted across multiple countries will be reported as ‘multinational’ with the list of participating countries provided.
Intervention: CKD screening, or CKD early detection programmes or CKD awareness programmes.
Comparator: standard of care (if applicable).
Outcomes: CKD early identification programmes/studies reporting at least one of the following: CKD detection rate (with or without risk factor detection rate), methods used for screening, people who carried out the screening, interventions used (eg, proportion referred to nephrology clinics, proportion that started treatment, etc), cost-effectiveness of the programme and CKD screening policies implemented.
Study design: all screening study designs that reported at least one of the outcomes.
Limits: all databases will be searched from inception with no language restrictions.
Limits: all databases will be searched from inception with no language restrictions.
The following studies will be excluded:
Screening studies in children.
Screening studies for acute kidney injury, urological diseases (eg, prostate cancer awareness programmes) or CKD risk factors (eg, hypertension and diabetes), if no attempt was made to specifically screen for CKD.
Organ donor screening or awareness programmes.
Review articles, editorials, commentaries, letters to the editor and guidelines and recommendations on CKD screening.
Stage 4. Data extraction
Results of the search will be collated in a Microsoft Excel spreadsheet. We will follow recommended data charting methods47 to capture relevant details for included studies (table 2). The data items collected will follow four themes: (1) population screened and screening methods used (eg, duration of screening, country of study, type of programme: ‘national’ or ‘other’, screening type: mass (community based)/targeted (within a known CKD risk factor cohort), workforce involved in screening, repeat evaluation, motivation for the programme (eg, World Kidney Day programme, public health concerns for rising kidney disease, etc)). We will also extract data on race/ethnicity of the population screened. Although, race is not often well defined in numerous studies, we will capture data using the following races (if reported): Arabs/Middle Easterners, Asians, Black Africans/African Americans, Caucasians, Hispanics, Indigenous groups, Latin Americans, others, (2) measurements used for assessing CKD (eg, urine dipsticks, serum creatinine, eGFR, etc), (3) interventions used in those identified with CKD (eg, referral to nephrology or specialist care, initiation of specific treatment (lifestyle measures, ACE-i, attempts to follow-up patients offered interventions, etc) and (4) health systems and economic factors associated with screening (eg, implementation programmes, cost-effectiveness, etc). All extracted data will be reviewed for accuracy and completeness.
Table 2.
Data extraction items from empirical literature sources
| Population screened | Measurements | Interventions | Implementation |
| Country, income group | Number of measurements (1x/2x) | Lifestyle measures* | Cost measures reported |
| Type of programme (national/others) | Urine dipsticks (protein ±blood) | RAAS blockade | Reported to be cost-effective |
| Demographic features (age, gender, ethnicity, rural/urban setting) | Urine ACR/PCR only | Antidiabetic medications (any) | Screening strategy adopted or not implemented due to lack of efficacy (eg, policy document) |
| Workforce involved in screening | SCR/eGFR only | Anti-hypertensive medications (separate from RAAS) | |
| Screening type | Urine+SCR/eGFR | Lipid treatment | |
| Mass screening (yes/no) | POCT | Avoidance of nephrotoxins | |
| Targeted screening (yes/no) | Other tests (eg, cystatin C) | Referral to nephrology service | |
|
Reported CKD prevalence (yes/no) | Referral for KRT | |
| |||
| |||
| |||
| |||
| |||
|
|||
| Risk factors assessed and reported: | |||
| |||
| |||
| |||
| |||
| |||
| Risk stratification (yes/no) | |||
*Smoking cessation, weight reduction measures, dietary measures, etc.
ACR, albumin-creatinine ratio; BMI, body mass index; BP, blood pressure; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; HIV, human immunodeficiency virus; KRT, kidney replacement therapy (any of haemodialysis, peritoneal dialysis, kidney transplantation); PCR, protein creatinine ratio; POCT, point of care test (eg, saliva); RAAS, renin-angiotensin aldosterone system; SCR, serum creatinine.
Stage 5. Collating, summarising and reporting of the results
We will follow recommendations to extend the scoping review process by adding thematic analysis.48 Hence, extracted data will be analysed qualitatively using both deductive (preidentified themes) and inductive (new identified themes) approaches. Primary analysis of data will be based on four themes identified by KDIGO:37 (1) population screened, (2) diagnostic characteristics of tests for kidney disease used, (3) treatments (interventions) used to reduce the risk of CKD progression and cardiovascular disease and (4) implementation strategies for early CKD identification programmes. These approaches will enable us to answer the broad research question and allow us to expand our response with new findings that were not previously included. Although specific data (eg, CKD detection rate) will be collected, such data will not be pooled for further analysis. Textual data from included papers will be coded individually using simple ‘yes’ or ‘no’ responses and other broad-based coding scheme by (EKT) and (AG) to look for common themes across papers. We will present overall results using percentages of ‘yes’ responses.
Stage 6. Consultation exercise
Consultation is an optional part of conducting a scoping review, however, where necessary, we will contact primary authors, regional nephrology leaders or Departments/Ministries of Health for policy documents on implementation of CKD screening programmes. Consultation will be necessary after selecting studies to be included and only if we are unable to identify online policy documents on early CKD identification for countries represented in selected studies. This process will be facilitated by members of the International Society of Nephrology (ISN) Regional Board (https://www.theisn.org/about-isn/governance/regional-boards/) for countries represented in selected studies.
Patient and public involvement
Patients and the public will not be involved in this scoping review; however, the ISN is seeking to establish a globally representative patient advisory group. It would be appropriate for such a group to make input into subsequent, more specific research questions that are generated from studies identified in this scoping review.
Discussion, ethics and dissemination
The findings from our planned scoping review will enable us to identify items in screening and early identification programmes that can be used in developing screening toolkits for CKD. The results will also enable us to understand what is feasible and the capacity of countries in different income groups for conducting and sustaining screening programmes. Various reviews and recommendations have suggested using different screening approaches in LLMICs, given the lack of capacity to integrate identified CKD cases into the broader health system and the general lack of capacity to measure the quality of care in existing CKD cases.29 37 Thus, based on our results, this scoping review will be able to suggest components for consideration for inclusion in screening toolkits for countries in different income groups, though these are likely to need testing for effectiveness. Furthermore, we anticipate that this scoping review will likely lead to more specific questions (eg, how sensitive and specific are urine dipsticks findings for screening?) that require detailed interrogation through systematic reviews or randomised controlled study designs. A potential limitation of this scoping review could be our inability to access policy documents backing the implementation/integration strategies of early identification programmes to health systems, particularly in LLMICs. We hope that by contacting nephrology leaders and experts in those regions, we will be able to obtain information on the availability of such policy documents. Finally, ethical approval will not be needed for this study as data used will be extracted from already published studies. Our dissemination strategy will use traditional approaches, including open-access peer-reviewed publication(s), scientific presentations and a report.
Supplementary Material
Footnotes
Contributors: VJ, AL, IGO and FJC conceived the study design. The first version of the protocol was drafted by IGO and was revised by FJC, AG, EKT, LNH, GA, J-AD, AF, RI, MMa, CM, MMo, RP-F, VT, AL and VJ. The search strategy was developed and performed by LNH. AG and EKT will perform the screening, study selection and collect data from all included studies and MMa will adjudicate any conflicts in study selection. All authors revised and critically reviewed this manuscript and approved the final version.
Funding: This is an International Society of Nephrology (ISN) initiative supported by an unrestricted educational grant from AstraZeneca (no grant number).
Competing interests: RP-F reports grants from Fresenius Medical Care, provides scientific leadership to George Clinical, and consultancy fees for Astra Zeneca, B-I, Bayer, Akebia, Novo Nordisk, all paid to his institution, outside the submitted work. VT reports consultancy fee from Boehringer-Ingelheim, Calliditas, Fresenius Medical Care, Novartis and Travere. VJ reports grants from GlaxoSmithKline and Baxter Healthcare, provides scientific leadership to George Clinical, and consultancy fees for Biocon, Zudis Cadilla and NephroPlus, all paid to his institution, outside the submitted work.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.GBD Chronic Kidney Disease Collaboration . Global, regional, and national burden of chronic kidney disease, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet 2020;395:709–33. 10.1016/S0140-6736(20)30045-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . The top 10 causes of death. Available: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death [Accessed 19 Mar 2021].
- 3.Foreman KJ, Marquez N, Dolgert A, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet 2018;392:2052–90. 10.1016/S0140-6736(18)31694-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bello AK, Levin A, Lunney M, et al. Status of care for end stage kidney disease in countries and regions worldwide: international cross sectional survey. BMJ 2019;367:l5873. 10.1136/bmj.l5873 [DOI] [PubMed] [Google Scholar]
- 5.Tang SCW, Yu X, Chen HC, et al. Dialysis care and dialysis funding in Asia. Am J Kidney Dis 2020;75:772–81. 10.1053/j.ajkd.2019.08.005 [DOI] [PubMed] [Google Scholar]
- 6.Crosby L, Baker P, Hangoma P, et al. Dialysis in Africa: the need for evidence-informed decision making. Lancet Glob Health 2020;8:e476–7. 10.1016/S2214-109X(20)30058-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Riaz P, Caskey F, McIsaac M, et al. Workforce capacity for the care of patients with kidney failure across world countries and regions. BMJ Glob Health 2021;6:e004014. 10.1136/bmjgh-2020-004014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bello AK, Alrukhaimi M, Ashuntantang GE, et al. Global overview of health systems oversight and financing for kidney care. Kidney Int Suppl 2018;8:41–51. 10.1016/j.kisu.2017.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lunney M, Alrukhaimi M, Ashuntantang GE, et al. Guidelines, policies, and barriers to kidney care: findings from a global survey. Kidney Int Suppl 2018;8:30–40. 10.1016/j.kisu.2017.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Htay H, Alrukhaimi M, Ashuntantang GE, et al. Global access of patients with kidney disease to health technologies and medications: findings from the global kidney health atlas project. Kidney Int Suppl 2018;8:64–73. 10.1016/j.kisu.2017.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Divyaveer SS, Ramachandran R, Sahay M, et al. International Society of nephrology global kidney health atlas: structures, organization, and services for the management of kidney failure in South Asia. Kidney Int Suppl 2021;11:e97–105. 10.1016/j.kisu.2021.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jankowski J, Floege J, Fliser D, et al. Cardiovascular disease in chronic kidney disease: pathophysiological insights and therapeutic options. Circulation 2021;143:1157–72. 10.1161/CIRCULATIONAHA.120.050686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet 2013;382:339–52. 10.1016/S0140-6736(13)60595-4 [DOI] [PubMed] [Google Scholar]
- 14.Cho Y, Bello AK, Levin A, et al. Peritoneal dialysis use and practice patterns: an international survey study. Am J Kidney Dis 2021;77:315–25. 10.1053/j.ajkd.2020.05.032 [DOI] [PubMed] [Google Scholar]
- 15.George C, Mogueo A, Okpechi I, et al. Chronic kidney disease in low-income to middle-income countries: the case for increased screening. BMJ Glob Health 2017;2:e000256. 10.1136/bmjgh-2016-000256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perico N, Plata R, Anabaya A, et al. Strategies for national health care systems in emerging countries: the case of screening and prevention of renal disease progression in Bolivia. Kidney Int Suppl 2005;97:S87–94. 10.1111/j.1523-1755.2005.09715.x [DOI] [PubMed] [Google Scholar]
- 17.Perico N, Remuzzi G. Prevention programs for chronic kidney disease in low-income countries. Intern Emerg Med 2016;11:385–9. 10.1007/s11739-016-1425-7 [DOI] [PubMed] [Google Scholar]
- 18.Sharma SK, Ghimire A, Carminati S, et al. Management of chronic kidney disease and its risk factors in eastern Nepal. Lancet Glob Health 2014;2:e506–7. 10.1016/S2214-109X(14)70281-5 [DOI] [PubMed] [Google Scholar]
- 19.Gansevoort RT, Verhave JC, Hillege HL, et al. The validity of screening based on spot morning urine samples to detect subjects with microalbuminuria in the general population. Kidney Int Suppl 2005;94:S28–35. 10.1111/j.1523-1755.2005.09408.x [DOI] [PubMed] [Google Scholar]
- 20.Coresh J, Astor BC, Greene T, et al. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: third National health and nutrition examination survey. Am J Kidney Dis 2003;41:1–12. 10.1053/ajkd.2003.50007 [DOI] [PubMed] [Google Scholar]
- 21.Komenda P, Lavallee B, Ferguson TW, et al. The prevalence of CKD in rural Canadian Indigenous peoples: results from the first nations community based screening to improve kidney health and prevent dialysis (finished) screen, triage, and treat program. Am J Kidney Dis 2016;68:582–90. 10.1053/j.ajkd.2016.04.014 [DOI] [PubMed] [Google Scholar]
- 22.Takahashi S, Okada K, Yanai M. The kidney early evaluation program (keep) of Japan: results from the initial screening period. Kidney Int Suppl 2010;116:S17–23. 10.1038/ki.2009.539 [DOI] [PubMed] [Google Scholar]
- 23.Fink HA, Ishani A, Taylor BC. Screening for, monitoring, and treatment of chronic kidney disease stages 1 to 3: a systematic review for the U. S. Preventive Services Task Force and for an American College of Physicians Clinical Practice Guideline. Annals of internal medicine 2012;156:570–81. [DOI] [PubMed] [Google Scholar]
- 24.Manns B, Hemmelgarn B, Tonelli M, et al. Population based screening for chronic kidney disease: cost effectiveness study. BMJ 2010;341:c5869. 10.1136/bmj.c5869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qaseem A, Wilt TJ, Cooke M, et al. The paucity of evidence supporting screening for stages 1-3 CKD in asymptomatic patients with or without risk factors. Clin J Am Soc Nephrol 2014;9:1993–5. 10.2215/CJN.02940314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kliger AS. Screening for CKD: a pro and con debate. Clin J Am Soc Nephrol 2014;9:1987. 10.2215/CJN.08990914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berns JS. Routine screening for CKD should be done in asymptomatic adults… selectively. Clin J Am Soc Nephrol 2014;9:1988–92. 10.2215/CJN.02250314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cepoi V, Onofriescu M, Segall L, et al. The prevalence of chronic kidney disease in the general population in Romania: a study on 60,000 persons. Int Urol Nephrol 2012;44:213–20. 10.1007/s11255-011-9923-z [DOI] [PubMed] [Google Scholar]
- 29.Tonelli M, Dickinson JA. Early detection of CKD: implications for low-income, middle-income, and high-income countries. J Am Soc Nephrol 2020;31:1931–40. 10.1681/ASN.2020030277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Garcia-Garcia G, Marquez-Magaña I, Renoirte-Lopez K, et al. Screening for kidney disease on world kidney day in Jalisco, Mexico. J Nephrol 2010;23:224–30. [PubMed] [Google Scholar]
- 31.Galbraith LE, Ronksley PE, Barnieh LJ, et al. The see kidney disease targeted screening program for CKD. Clin J Am Soc Nephrol 2016;11:964–72. 10.2215/CJN.11961115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gayoso-Diz P, Otero-González A, Rodríguez-Álvarez MX, et al. Strategy to estimate risk progression of chronic kidney disease, cardiovascular risk, and referral to nephrology: the EPIRCE study. Nefrologia 2013;33:223–30. 10.3265/Nefrologia.pre2013.Jan.11792 [DOI] [PubMed] [Google Scholar]
- 33.Sharma SK, Zou H, Togtokh A, et al. Burden of CKD, proteinuria, and cardiovascular risk among Chinese, Mongolian, and Nepalese participants in the International Society of nephrology screening programs. Am J Kidney Dis 2010;56:915–27. 10.1053/j.ajkd.2010.06.022 [DOI] [PubMed] [Google Scholar]
- 34.Diercks GF, Janssen WM, van Boven AJ, et al. Rationale, design, and baseline characteristics of a trial of prevention of cardiovascular and renal disease with fosinopril and pravastatin in nonhypertensive, nonhypercholesterolemic subjects with microalbuminuria (the Prevention of REnal and Vascular ENdstage Disease Intervention Trial [PREVEND IT]). Am J Cardiol 2000;86:635–8. 10.1016/S0002-9149(00)01042-0 [DOI] [PubMed] [Google Scholar]
- 35.Jaar BG, Khatib R, Plantinga L, et al. Principles of screening for chronic kidney disease. Clin J Am Soc Nephrol 2008;3:601–9. 10.2215/CJN.02540607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.de Jong PE, van der Velde M, Gansevoort RT, et al. Screening for chronic kidney disease: where does Europe go? Clin J Am Soc Nephrol 2008;3:616–23. 10.2215/CJN.04381007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shlipak MG, Tummalapalli SL, Boulware LE, et al. The case for early identification and intervention of chronic kidney disease: conclusions from a kidney disease: improving global outcomes (KDIGO) controversies conference. Kidney Int 2021;99:34–47. 10.1016/j.kint.2020.10.012 [DOI] [PubMed] [Google Scholar]
- 38.Johnson DW, Atai E, Chan M, et al. KHA-CARI guideline: early chronic kidney disease: detection, prevention and management. Nephrology 2013;18:340–50. 10.1111/nep.12052 [DOI] [PubMed] [Google Scholar]
- 39.National Institute for Health and Care Excellence (NICE) . Assessment and monitoring of chronic kidney disease, 2020. Available: http://pathways.nice.org.uk/pathways/chronic-kidney-disease
- 40.National Kidney Foundation . K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002;39:S1–266. [PubMed] [Google Scholar]
- 41.American Society of Nephrology . ASN emphasizes need for early detection of kidney disease, a silent killer, 2013. Available: https://www.asn-online.org/news/2013/ASN_COMM_ACP_Screening_Response_102213_R12.pdf
- 42.Garcia-Garcia G, Jha V, Tao Li PK, et al. Chronic kidney disease (CKD) in disadvantaged populations. Clin Kidney J 2015;8:3–6. 10.1093/ckj/sfu124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vassalotti JA, Li S, McCullough PA, et al. Kidney early evaluation program: a community-based screening approach to address disparities in chronic kidney disease. Semin Nephrol 2010;30:66–73. 10.1016/j.semnephrol.2009.10.004 [DOI] [PubMed] [Google Scholar]
- 44.Obrador GT, García-García G, Villa AR. Prevalence of chronic kidney disease in the kidney early evaluation program (keep) México and comparison with keep us. Kidney Int 2010;03:S2–8. 10.1038/ki.2009.540 [DOI] [PubMed] [Google Scholar]
- 45.Liu Q, Li Z, Wang H, et al. High prevalence and associated risk factors for impaired renal function and urinary abnormalities in a rural adult population from southern China. PLoS One 2012;7:e47100. 10.1371/journal.pone.0047100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tummalapalli SL, Vittinghoff E, Crews DC, et al. Chronic kidney disease awareness and longitudinal health outcomes: results from the reasons for geographic and racial differences in stroke study. Am J Nephrol 2020;51:463–72. 10.1159/000507774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 48.Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Colquhoun HL, Levac D, O'Brien KK, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol 2014;67:1291–4. 10.1016/j.jclinepi.2014.03.013 [DOI] [PubMed] [Google Scholar]
- 50.Daudt HML, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team's experience with Arksey and O'Malley's framework. BMC Med Res Methodol 2013;13:48. 10.1186/1471-2288-13-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Implement 2021;19:3–10. 10.1097/XEB.0000000000000277 [DOI] [PubMed] [Google Scholar]
- 52.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 53.Peters MDJ GC, McInerney P, Munn Z. Chapter 11: Scoping Reviews (2020 version). In: Aromataris E MZE, ed. Joanna Briggs Institute Reviewer’s Manual, JBI, 2020, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.