Abstract
A 29-year-old man with severe haemophilia A developed right lower quadrant pain. He was diagnosed with jejuno-jejunal intussusception, and he was managed conservatively with an infusion of plasmatic factor VIII, resulting in resolution of symptoms, and reduction of the jejuno-jejunal intussusception, and complete regression of hematoma. This case highlights a rare clinical manifestation in patients with haemophilia, and also indicates the effectiveness of factor VIII instead of exploratory surgery for intramural hematoma.
Keywords: Haemophilia, Jejunum, Intussusception, Factor VIII
Introduction
Haemophilia A is a congenital bleeding disorder caused by deficiency of coagulation factor VIII [1].
It’s occurred in approximately one in 10,000 male births and characterized by bleeding into the joints and muscles. When a patient with haemophilia is injured, complications depend on the trauma, the severity of the disease, and the location of the injury [2,3].
Gastrointestinal bleeding is a well-known complication of haemophilia, with an incidence of 25% [4,5], and lead to mortality in 4% [6].
Patients with haemophilia can develop all types of gastrointestinal bleeding including intramural intestinal hematomas [7], that occur in 4.85% of patients with severe haemophilia [8].
Management of adult intussusception is almost always surgical, due to the presence of underlying pathology in 90% of cases [9,10,11].
We report a case of patient with severe haemophilia A who developed an intramural hematoma of jejunum which served as a lead point for a jejuno-jejunal intussusception, and which has been managed without surgery.
Case Report
A 29-year-old man, who had been diagnosed with severe haemophilia A 26 years ago.
The patient was managed in hematology department since 1995, and received plasmatic factor VIII for bleeding episodes with no prophylaxis treatment.
In 2012, the patient underwent an appendectomy, and in 2015 he had a right psoas hematoma which has been treated with plasmatic factor VIII infusion with a good improvement.
In 2018, the patient presented a retroperitoneal hematoma secondary to minimal trauma.
In November 2019, the patient presented with severe abdominal pain, vomiting, and complete ileus, 24 hours before his admission to the emergency department, and without trauma or anticoagulant therapy history.
Physical examination showed conscious patient, his temperature was 37.3°C, his blood pressure was 118/65mmHg and abdominal examination showed diffuse abdominal tenderness and distension with muscular rigidity in the right lower quadrant.
Laboratory investigations revealed a hemoglobin concentration at 14g/dL, a platelet count at 320 10³/L, and white blood cell count at 9.2 10³/L.
The prothrombin time was normal at 12.7 sec (control, 12.3 sec), and the activated partial thromboplastin time (APTT) was prolonged at 52 sec (control, 25 sec).
The plasma fibrinogen level was 467mg/dL (normal range, 200-400mg/dL). Factor VIII activity was less than 1%, and testing for factor VIII inhibitor was negative.
C-reactive protein was elevated at 22mg/dL. Electrolytes and blood urea nitrogen, and liver function tests were normal.
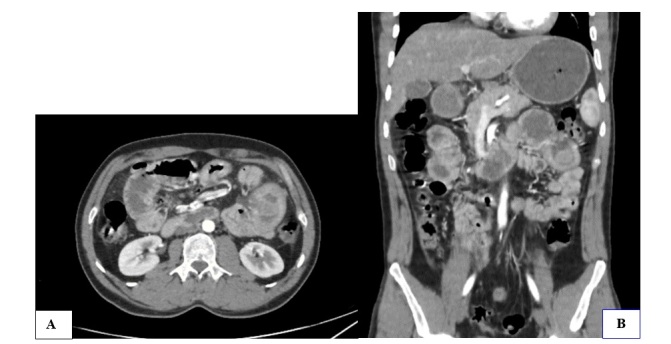
Computed tomography (CT) of the abdomen and pelvis showed an intramural thickening of jejunum, with concentric rings, consistent with the appearance of jejuno-jejunal intussusception, related with an intramural hematoma of jejunum (Figure 1), and with no sign of intestinal wall necrosis (Figure 2).
Figure 1.

CT scan of the abdomen and pelvis without iodine contrast media injection; A: transverse section; B: coronal section: intramural thickening of jejunum related with intramural hematoma of jejunum, with concentric rings, consistent with the appearance of jejuno-jejunal intussusceptions
Figure 2.
CT scan of the abdomen and pelvis with iodine contrast media injection; A: transverse section; B: coronal section: intramural thickening takes iodine contrast media, homogeneously, in favor of no sign of intestinal wall necrosis
The patient was treated with plasmatic factor VIII 50UI/dL for 3 days with analgesic, and antiemetic treatment, and discontinuation of oral feeding. 48 hours later, the evolution was marked by a good improvement of abdominal pain, vomiting resolution, and resumption of transit.
At day 4, infusion of plasmatic factor VIII was reduced to 30UI/dL.
At day 7, abdominal ultrasound performed showed complete intussusception reduction with partial regression of the jejunal intramural hematoma.
The patient was discharged from the hospital at day 10. Follow-up abdominal CT scan at day 30 was normal.
A written informed consent of the patient has been obtained before the publication of these data.
Discussion
Intussusception is defining by penetration of a segment of intestine into an adjacent segment, leading to obstruction, inflammation, and possible ischemia.
After childhood, intussusception is relatively rare and accounts for less than 5% of intestinal obstruction in adults [12].
In haemophilia, gastrointestinal hemorrhage is a well-known complication, with an incidence as high as 25% [4,5].
It includes mucosal bleeding, due mainly to gastric or duodenal peptic ulcers, esophagitis, and gastritis [4].
In contrast, mural and perimural hematomas are very rare [13,14].
The two most common sites for spontaneous intramural gastrointestinal hematomas are the duodenum and jejunum [15,16].
Patients typically present with sudden-onset abdominal pain, nausea, and vomiting due to intestinal obstruction after a large meal.
Patients may also present with signs of peritoneal irritation when hematoma has ruptured [17].
Since 1964, 31 cases with intramural hematoma of gastrointestinal tract in patients with haemophilia were reported [18].
The fourteenth case of jejuno-jejunal intussusception in young patient with severe haemophilia A was reported in this paper, and the lead point of intussusception was an intramural hematoma.
Early diagnosis of intramural hematoma and intussusception as well as rapid and adequate administration of hemostatic agents can provide medical management without surgery [18,19].
Our patient was diagnosed during the first 24 hours, and he doesn’t have factor VIII inhibitors.
The decision was to manage him conservatively by plasmatic factor VIII infusion resulting in the resolution of symptoms, and the reduction of the jejuno-jejunal intussusception, and complete regression of intramural hematoma.
The management of the acute abdomen in a patient with haemophilia must combine rapid diagnosis and conservative approach to avoid emergency surgery.
Especially, if the patient has no indication for emergency surgery like ischemia or perforation, and if the patient doesn’t have factor VIII inhibitors indicating that he will be a low responder [20,21].
Conclusions
Although intramural hematoma of the gastrointestinal tract is a rare and represents an atypical source of bleeding in patients with haemophilia, it requires wakefulness and special intention in assessing abdominal pain in patients with haemophilia.
The main goal is to correct quickly and effectively the factor VIII allowing for hematoma resolution,and to ensure a conservative approach.
Conflict of interest
Conflict of interest
None to declare.
Patient informed consent
A written informed consent of the patient has been obtained before the publication of these data.
References
- 1.Mannucci PM, Tuddenham EGD. The hemophiliasc-from royal genes to gene therapy. N Engl J Med. 2001;344(23):1773–1779. doi: 10.1056/NEJM200106073442307. [DOI] [PubMed] [Google Scholar]
- 2.Cahill MR, Colvin BT. Hemophilia. Postgrad Med J. 1997;73(858):201–206. doi: 10.1136/pgmj.73.858.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guthrie Jr, Sacra JC. Emergency care of the hemophiliac patient. Ann Emerg Med. 1980;9(9):476–479. doi: 10.1016/s0196-0644(80)80307-6. [DOI] [PubMed] [Google Scholar]
- 4.Mittal R, Spero JA, Lewis JH, Taylor F, Ragni MV, Bontempo FA, Van Thiel DH. Patterns of gastrointestinal hemorrhage in hemophilia. Gastroenterology. 1985;88(2):515–522. doi: 10.1016/0016-5085(85)90515-3. [DOI] [PubMed] [Google Scholar]
- 5.Ramadan KMA, Lowry JP, Wilkinson A, McNulty O, McMullin MF, Jones FGC. Acute intestinal obstruction due to intramural haemorrhage in small intestine in a patient with severe haemophilia A and inhibitor. Eur J Haematol. 2005;75(2):164–166. doi: 10.1111/j.1600-0609.2005.00445.x. [DOI] [PubMed] [Google Scholar]
- 6.Aronson DL. Cause of death in haemophilia A patients in the United States from 1968-1979. Am J Hematol. 1988;27(1):7–12. doi: 10.1002/ajh.2830270103. [DOI] [PubMed] [Google Scholar]
- 7.Abbas MA, Collins JM, Olden KW, Kelly KA. Spontaneous intramural small-bowel hematoma: clinical presentation and long-term outcome. Arch Surg. 2002;137(3):306–310. doi: 10.1001/archsurg.137.3.306. [DOI] [PubMed] [Google Scholar]
- 8.Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226(2):134–138. doi: 10.1097/00000658-199708000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173(2):88–94. doi: 10.1016/S0002-9610(96)00419-9. [DOI] [PubMed] [Google Scholar]
- 10.Eisen LK, Cunningham JD, Aufses AH. Intussusception in adults: institutional review. J Am Coll Surg. 1999;188(4):390–395. doi: 10.1016/s1072-7515(98)00331-7. [DOI] [PubMed] [Google Scholar]
- 11.Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou L, Theodosopoulos T. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009;15(4):407–411. doi: 10.3748/wjg.15.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Janic D, Smoljanic Z, Krstovski N, Dokmanovic L, Rodic P. Ruptured intramural intestinal hematoma in an adolescent patient with severe hemophilia A. Int J Hematol. 2009;89(2):201– 203. doi: 10.1007/s12185-008-0236-7. [DOI] [PubMed] [Google Scholar]
- 13.Leonardou P, Kierans AS, Elazazzi M, Shaikh F, Semelka RC. MR imaging findings of small bowel hemorrhage: two cases of mural involvement and one of perimural. J Magn Reson Imaging. 2009;29(5):1185–1189. doi: 10.1002/jmri.21698. [DOI] [PubMed] [Google Scholar]
- 14.Hughes CE, Conn J, Sherman JO. Intramural hematoma of the gastrointestinal tract. Am J Surg. 1977;133(3):276–279. doi: 10.1016/0002-9610(77)90528-1. [DOI] [PubMed] [Google Scholar]
- 15.Jewett TC, Caldarola V, Karp MP, Allen JE, Cooney DR. Intramural hematoma of duodenum. Arch Surg. 1988;123(1):54–58. doi: 10.1001/archsurg.1988.01400250064011. [DOI] [PubMed] [Google Scholar]
- 16.Abbas MA, Collins JM, Olden KW. Spontaneous intramural small‐bowel hematoma: imaging findings and outcome. AJR Am J Roentgenol. 2002;179(6):1389–1394. doi: 10.2214/ajr.179.6.1791389. [DOI] [PubMed] [Google Scholar]
- 17.Katsumi A, Matsushita T, Hirashima K, Iwasaki T, Adachi T, Yamamoto K, Kojima T, Takamatsu J, Saito H, Naoe T. Recurrent Intramural Hematoma of the Small Intestine in a Severe Hemophilia A Patient with a High Titer of Factor VIII Inhibitor: A Case Report and Review of the Literature. Int. J. Hematol. 2006;84(2):166–169. doi: 10.1532/IJH97.06053. [DOI] [PubMed] [Google Scholar]
- 18.Eiland M, Han SY, Hicks GM. Intramural hemorrhage of the small intestine. JAMA. 1978;239(2):139–142. [PubMed] [Google Scholar]
- 19.Fripp RR, Karabus CD. Intussusception in haemophilia: a case report. S Afr Med J. 1977;52(15):617– 618. [PubMed] [Google Scholar]
- 20.Allen G, Aledort L. Therapeutic decision-making in inhibitor patients. Am J Hematol. 2006;81(1):71–72. doi: 10.1002/ajh.20474. [DOI] [PubMed] [Google Scholar]
- 21.Berntorp E, Donfield S, Waters J, Mattson E, DiMichele D, Gringeri A, Astermark J. The FEIBA NovoSeven Comparative Study (FENOC)-a randomized evaluation of bypassing agents in hemophilia complicated by inhibitors. Blood. 2005;106(11):324–324. doi: 10.1182/blood-2006-04-017988. [DOI] [PubMed] [Google Scholar]


