Abstract
Background:
Globally, there has been a marked decline in neonatal mortality and overall child mortality indicators from 1990 to date. In Kenya, neonatal deaths remain unacceptably high, contributing to 40% of under-five mortality rates (U5MR) making it an important health priority. The objective of this study was to identify the determinants of neonatal mortality in Kenya. An understanding of the determinants of neonatal mortality will provide evidence for better interventions to reduce these deaths.
Methods:
Neonatal deaths from singleton live-born infants were extracted from women’s dataset collected for the 5-year period preceding the study published in the Kenya Demographic and Health Survey (KDHS), 2014. Data were obtained from 18,951 births. There were 356 neonatal deaths recorded. Data were weighted using an individual weighting factor to adjust for the study design and reduce sample variability. Data were analyzed using SPSS version 20.0. Logistic regression was conducted to adjust for confounding factors.
Results:
Neonatal mortality rate was established at 19/1000 (95% CI: 16.8-20.7). Mothers with no education had higher odds of experiencing deaths of neonates with adjusted Odds Ratio (aOR)=2.201, 95% CI: 1.43-4.15,p=0.049) compared to mothers with higher education. Low Birth Weight (LBW) neonates were 3.2 times likely to die in the first 28 days (aOR=3.206, 95% CI: 1.85-12.08, p=0.006) compared to neonates with >3.5 kilograms at birth. Mothers who did not attend ANC during pregnancy and those who attended between 1-3 ANC visits had higher odds of losing their infants (aOR=3.348, 95% CI: 1.616-8.53, p=0.041, and aOR=2.316, 95% CI: 1.10-4.88, p=0.027) respectively, compared to mothers who attended >4 ANC visits.
Conclusion and Global Health Implications:
Improving maternal health and nutrition during pregnancy should be enhanced to ensure adequate weight gain and reduce instances of low birth weight. Community referrals and follow-up for expectant women to take up the requisite 4 ANC visits should be encouraged. Girls’ education should be emphasized to reduce the proportion of illiterate mothers.
Keywords: Neonatal Mortality, Determinants, Low Birth Weight, Antenatal Care
1. Introduction
Neonatal mortality is defined as the death of a newborn within the first 28 days of life.1 This period is the most vulnerable time for the child’s survival. Neonatal mortality remains a significant public health problem worldwide and accounts for 60% of newborn deaths in middle- and lower-income countries (LMICs).2 In 2017, 2.5 million children died in the first month of life globally.2 Of these deaths, approximately one million infants died within the first week of life. Whereas there has been a recorded decline in neonatal deaths globally, the reduction of neonatal mortality is much slower compared to the other child mortality indicators among children between 1-11 months and those between 12-59 months.2 The neonatal mortality rates fell by 51% from 37 deaths per 1000 live births in 1990 to 18 deaths per 1000 live births in 2017.2 Disparities in neonatal deaths exist across the regions with 99% of neonatal deaths recorded in LMICs with Sub–Saharan Africa (SSA) and Southeast Asia (SEA) being the most affected. For countries to stay on track towards achieving Sustainable Development Goal (SDG) 2 on child mortality, the reduction of neonatal deaths must be prioritized.
In Kenya, the neonatal mortality rate (NMR) is 22 deaths per 1000 live births with the urban areas having a higher rate of 26 per 1000 live births compared to 21 deaths per 1000 live births in the rural areas.3 Although Kenya has made positive progress in the overall childhood indicators over time, the country continues to lag in the neonatal mortality indicators which have only marginally reduced from 33 per 1000 live births in 20034 to 31 per 1000 live births in 2008/95 and 22 deaths per 1000 live births in 2014.3 Whereas the Kenya government had established a health framework6 that was aimed at reducing both neonatal and under 5 mortality rates, the reduction in childhood mortality, especially for children in the neonatal period have remained insignificant. As a result, Kenya may not realize its SDG targets on child mortality.
Common causes of neonatal mortality include pre-term birth complications, intrapartum growth restrictions, infections such as tetanus, low birth weight, congenital malformations and neonatal sepsis among other factors.7,8,9 In addition, there exists a relationship between maternal health and neonatal survival. Poor maternal nutritional and health status has been linked to poor neonatal outcomes and this is influenced by determinants such as socio-economic, demographic and biological factors. Other maternal-related factors such as age and level of education have also shown significance in neonatal birth outcomes. For instance, cultural practices that restrict access to health facilities after birth have a negative influence on neonatal outcomes.10 Ultimately, factors related to maternal health like essential antenatal care (ANC), access to emergency obstetric care, access to skilled attendance at birth, adequate maternal nutrition, postpartum care, neonatal care and early initiation of breastfeeding if adequately implemented can ensure neonatal survival. It is for this reason that the study seeks to establish the determinants of neonatal death with a focus on the nationally representative data from the KDHS 2014.
In this study, secondary data was obtained from the Kenya Demographic and Health Survey KDHS 2014 database with authorization from the DHS program, then analyzed to establish the determinants of neonatal mortality in Kenya.3 The study conceptual framework was adopted from Mosley and Chen’s framework for child survival and contextualized to the variables of interest in this study.11,12,13,14 Risk factors associated with neonatal deaths include household socioeconomic status, place of residence, education levels, number of ANC visits, birth weights, place of delivery and birth order of the neonate.15 The objective of the study was to determine factors associated with neonatal mortality using KDHS 2014 data.
2. Methods
2.1. Study Design
The Kenya Demographic and Health Survey (KDHS) is a nationally representative household survey that provides data for monitoring population indicators including population, health and nutrition. This data was collected by the Kenya National Bureau of Statistics in collaboration with the Ministry of Health, National AIDS Control Council (NACC), National Council for Population and Development (NCPD) and Kenya Medical Research Institute (KEMRI). ICF Macro provided technical assistance for the survey through the DHS program. The sample design for the KDHS 2014 was drawn from the master sampling of the fifth National Sample Survey and evaluation program (NASSEP V).3 KDHS is designed as a stratified 2 stage cluster design with the first sampling stage involving a random selection of 1,612 clusters from the NASSEP V spread across the country (995 in the rural areas and 617 in the urban areas). In the second stage, 25 households are randomly selected from each of the already selected enumeration areas (EAs). Data was collected using a structured household and women’s questionnaire administered by an enumerator. The women’s questionnaire collected information including the women’s birth history, childhood mortality, fertility preferences, antenatal and post-natal care, place of delivery, childhood diseases and childhood vaccinations. Conceptual frameworks for analyzing child survival for developing countries have been used by other authors including the Mosley and Chen framework which has been widely used.11,12,13,14 In this study, the conceptual framework based on the Mosley and Chen framework was developed to guide the potential explanatory variables (determinants) to neonatal mortality as shown in Figure 1.
Figure 1.
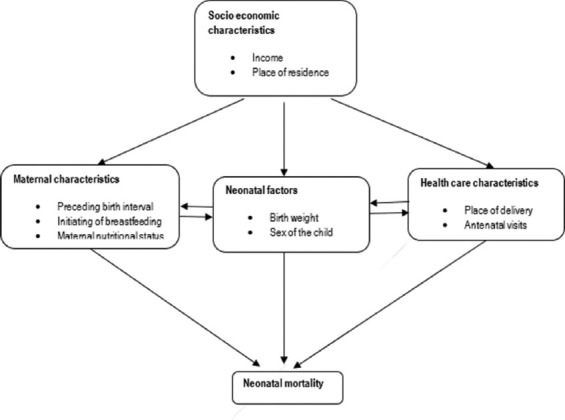
Conceptual framework for neonatal mortality Source: Authors own work
2.2. Study Variables
The outcome variable for this study is neonatal deaths as reported by the mothers. It was defined as the death of a neonate between birth and 28 days of life. The variable took a binary form such that neonatal death was a success and coded as= 1 and neonatal survival in the 28 days was a failure and coded as=0. The variable was examined against the explanatory variables categorized into 4 categories i.e., socioeconomic and demographic characteristics, maternal characteristics, child characteristics and health facility characteristics. The explanatory variables included in this study are in Table 1.
Table 1.
Variable names and definitions
| Variable | Definition |
|---|---|
| Demographic characteristics | |
|
| |
| Household income | 0=Poorest 1 =poor, 2=Middle, 3=Richer, 4=Richest. |
|
| |
| Place of residence | 0=Urban, 1=Rural |
|
| |
| Maternal characteristics | |
|
| |
| Mothers’ education | 0=No education, 1=Primary, 2=Secondary, 3=Tertiary education or higher |
|
| |
| Age at first birth | Age of the mother at the first birth 0=<19 years, 1=20-29 years, 2=30-39 years, 4= > 40 years. |
|
| |
| 0=1st child, 2=2nd and 3rd child, 3=>4th child | |
|
| |
| Birth spacing | 0=<2 years, 1=>2 years |
|
| |
| Birth order | 0=First child, 1=2 and 3rd child, 3>4th child |
|
| |
| Initiation of breastfeeding | 0=Immediately, 1=1hr-24 hours, 2=>24 hours |
|
| |
| Child characteristics | |
|
| |
| Sex of the child | 0=Male, 1=Female |
|
| |
| Birth weight | 0=LBW, 1=Normal BW, 2=>Normal |
|
| |
| Health service characteristics | |
|
| |
| Place of delivery | 0 Home, 1=Public and private hospital, |
|
| |
| Number of ANC visits | 0= None, 1=<1-3 ANC visits, 2=> 4 ANC visits |
2.3. Statistical Analysis
Statistical analysis was done using SPSS V 20.0.16 Descriptive statistics was used to explain the characteristics of the mothers and neonates captured in the study. Frequency distribution tables were used to present the descriptive statistics. Neonatal mortality was computed using the formula defined by Rutstein and Rojas17 in the guide to analyzing demographic health surveys and the results presented in Table 2. Univariate and multivariate analyses were conducted to establish associations between the potential explanatory variables and the study outcome. Logistic regression models were fitted using SPSS regression functions. The weights used for the adjustment of the KDHS data are recommended in the guide to analyzing DHS statistics.17 Odds Ratios (OR) and 95% confidence intervals (CI) were calculated to assess the adjusted risk factors that affected the study outcomes and those with p=0.05 were retained in the final model.
Table 2.
Sociodemographic and Economic, Maternal, child and health service characteristics
| Sociodemographic and economic | No of women | Percentage (%) |
|---|---|---|
| Household income | ||
|
| ||
| Poor | 8,418 | 44.4 |
|
| ||
| Middle | 3,385 | 17.9 |
|
| ||
| Rich | 7,149 | 37.7 |
|
| ||
| Place of residence | ||
|
| ||
| Rural | 12,168 | 64.2 |
|
| ||
| Urban | 6,783 | 35.8 |
|
| ||
| Maternal characteristics | ||
|
| ||
| Mother’s education | ||
|
| ||
| No education | 2,244 | 11.8 |
|
| ||
| Primary | 10,652 | 56.2 |
|
| ||
| Secondary | 4,485 | 23.7 |
|
| ||
| Higher | 1,571 | 8.4 |
|
| ||
| Age at first birth | ||
|
| ||
| <19 years | 10,573 | 55.8 |
|
| ||
| 20-29 years | 8,122 | 42.9 |
|
| ||
| 30-39 years | 247 | 1.4 |
|
| ||
| >40 years | 9 | 0. |
|
| ||
| Birth spacing | ||
|
| ||
| <2 years | 3,003 | 21.6 |
|
| ||
| >2 years | 10,917 | 78.4 |
|
| ||
| Initiation of breastfeeding | ||
|
| ||
| Immediately after birth | 4,207 | 68.2 |
|
| ||
| >1 hour -24 hours | 1,955 | 31.8 |
|
| ||
| Child characteristics | ||
|
| ||
| Sex of the child | ||
|
| ||
| Male | 9,601 | 50.8 |
|
| ||
| Female | 9,350 | 49.2 |
|
| ||
| Birth weight | ||
|
| ||
| Not weighed | 3,021 | 33.6 |
|
| ||
| <2.5 kg | 372 | 5 |
|
| ||
| 2.5-3.5 kg | 3,124 | 34.7 |
|
| ||
| >3.5 kgs | 2,447 | 26.7 |
|
| ||
| Health service characteristics | ||
|
| ||
| Place of delivery | ||
|
| ||
| Home deliveries | 7,159 | 38.3 |
|
| ||
| Facility deliveries | 11,524 | 61.7 |
|
| ||
| Number of ANC visits | ||
|
| ||
| No ANC visits | 563 | 4 |
|
| ||
| 1-3 visits | 5,419 | 38.2 |
|
| ||
| >4 Visits | 8,161 | 57.8 |
Approval to utilize data for this study was obtained from the DHS program, Rockville Maryland, USA. Approval was also obtained from Egerton University, Njoro, Kenya.
3. Results
3.1. Neonatal Mortality Characteristics
Table 2 presents a description and distribution of neonatal deaths across the explanatory variables. The study results show that 64.1% of the births occurred in rural areas whereas 35.9% occurred in urban areas. In addition, 11.9% of women had no education, 56.4% of women had primary education, 19.2% of women had secondary level education and 12.4% of the women had tertiary education. Regarding mothers’ age, 46.8% were below 19 years, 50% were between 20-29 years and 2.6% were above 30 years as presented in Table 2.
Table 3 presents the total live births and Neonatal Mortality Rate (NMR) by socio-demographic and economic characteristics, maternal, child and health facility characteristics. We found that NMR was higher in rural areas than in urban areas (NMR:19.6 vs 17.4). Neonates born to poor mothers had a higher NMR compared to mothers from middle-class households (NMR: 20.6 vs 19.2). Neonates with low birth weight had a higher NMR compared to those with normal birth weight (NMR:45.7 vs 9.0). Mothers with a shorter interpregnancy interval < 2 years, had a higher NMR compared though those with interpregnancy intervals >2 years (NMR: 23.6 vs 15.9). Mothers who delivered at home experienced higher NMR compared to those who delivered at health facilities (NMR:19.3 vs 17.9). Mothers who did not attend any ANC at the time of their pregnancy had a higher NMR compared to those who attended between 1-3 visits and those who attended the requisite minimum of 4 ANC visits (NMR: 42.6 vs 14.8 vs 10.7).
Table 3.
Neonatal mortality rates with 95% Confidence intervals
| Variables | Neonatal deaths | Total births | NMR 95% C.I |
|---|---|---|---|
| Place of residence | |||
|
| |||
| Urban | 118 | 6,783 | 17.4(14.3-20.5) |
|
| |||
| Rural | 238 | 12,168 | 19.6 (17.1-22.0) |
|
| |||
| Wealth | |||
|
| |||
| Poor | 168 | 8,418 | 20.6(16.9-23.0) |
|
|
|||
| Middle | |||
|
| |||
| Rich | 65 | 3,385 | 19.2(14.5-23.9) |
|
| |||
| Mothers’ education | 124 | 7,149 | 17.3(14.3-20.4) |
|
|
|||
| No education | 45 | 2,244 | 20.1(14.2-25.9) |
|
| |||
| Primary | 217 | 10,652 | 20.4(17.7-23.1) |
|
| |||
| Secondary | 57 | 4,485 | 12.9 (9.4-16.0) |
|
| |||
| higher | 37 | 1,571 | 23.6(16.0-31.1) |
|
| |||
| Mother’s age | |||
|
|
|||
| < 19 years | 24 | 983 | 24.4(14.6-34.2) |
|
| |||
| 20-29 years | 180 | 10,487 | 17.2(14.7-19.4) |
|
| |||
| 30-39 years | 115 | 6,212 | 18.5(15.1-21.9) |
|
| |||
| >40 years | 38 | 1,271 | 29.9 (20.4-39.4) |
|
| |||
| Birth spacing | |||
|
|
|||
| <2 years | 71 | 3,003 | 23.6 (18.1-29.1) |
|
| |||
| >2 years | 174 | 10,917 | 15.9 (13.6-18.3) |
|
| |||
| Sex | |||
|
|
|||
| Male | 185 | 9,601 | 19.3 (16.5-22.0) |
|
| |||
| Female | 171 | 9,350 | 18.3 (15.5-21.0) |
|
| |||
| Birth weight | |||
|
|
|||
| Underweight | 17 | 372 | 45.7(24.0-67.4) |
|
| |||
| Normal weight | 28 | 3,124 | 9.0 (5.6-12.3) |
|
| |||
| Above N W | 26 | 2,447 | 10.6 (6,5-14.7) |
|
| |||
| Not weighed at birth | 79 | 3,021 | 26.2 (20.4-31.9) |
|
| |||
| Place of delivery | |||
| Facility | 206 | 11,524 | 17.9 (15.4-20.3) |
|
| |||
| Home | 138 | 7,159 | 19.3 (16.1-22.5) |
|
| |||
| No. of ANC visits | |||
|
|
|||
| No ANC visits | 24 | 563 | 42.6(25.6-59.7) |
|
| |||
| 1-3 ANC visits | 80 | 5,419 | 14.8 (11.5-18.0) |
| >4 ANC visits | 87 | 8,161 | 10.7 (8.4-12.9) |
N.W=Normal Weight
3.2. Factors Associated with Neonatal Mortality
Logistic regression analysis was conducted in 2 stages as presented in Table 4. In the first step of the logistic regression model, each of the explanatory variables was entered individually into the regression model. The analysis showed that infants whose mothers had no education were 1.4 times more likely to die in the first 28 days compared to mothers with higher education levels Crude Odds Ratio (cOR)=1.44, 95% CI: 1.21-2.94, p=0.003. First-borns were 1.4 times more likely to die in the first month of life (cOR=1.43, 95% CI: 1.01- 2.08, p=0.043) compared to 4th order infants. Low birth weight infants (<2.5 kgs) were 3.5 times more likely to die (cOR=3.58, 95% CI:1.47- 8.75, p=0.005) compared to infants with a birth weight >3.5 kgs. Mothers who did not attend ANC clinic were 4 times more likely to experience deaths of their neonates (cOR=4.05, 95% CI:1.72-9.51, p=0.001) compared to mothers attending more than 4 visits. Infants of mothers who attended between 1-3 ANC visits were 1.7 times more likely to die (cOR=1.70, 95% CI: 1.10- 2.63, p=0.017) in the first month of life.
Table 4.
Logistic regression analysis of the determinants of neonatal mortality, KDHS 2014.
| Variables | cOR | C.I | p-value | aOR | C.I | P value |
|---|---|---|---|---|---|---|
| Residence | ||||||
|
| ||||||
| Rural (ref) | ||||||
|
| ||||||
| Urban | 1.005 | 0.971 | ||||
|
| ||||||
| Wealth status | ||||||
|
| ||||||
| Richest (ref) | ||||||
|
| ||||||
| Poorest | 0.741 | 0.191 | ||||
|
| ||||||
| Poor | 0.670 | 0.088 | ||||
|
| ||||||
| Middle | 0.927 | 0.763 | ||||
|
| ||||||
| Rich | 0.748 | 0.235 | ||||
|
| ||||||
| Mothers’ characteristics | ||||||
|
| ||||||
| Mothers’ education | ||||||
|
| ||||||
| Higher (ref) | ||||||
|
| ||||||
| No education | 1.437 | 1.206-2.937 | 0.031* | 2.202 | 1.43-4.15 | 0.049* |
|
| ||||||
| Primary | 0.332 | 0.001* | 0.809 | 0.256 | ||
|
| ||||||
| Secondary | 0.218 | 0.000* | 0.039 | 0.128 | ||
|
| ||||||
| Mother’s age | ||||||
|
| ||||||
| <19 years | 0.841 | 0.807 | ||||
|
| ||||||
| 20-29 years | 1.608 | 0.501 | ||||
|
| ||||||
| 30-39 years | 0.803 | 0.753 | ||||
|
| ||||||
| Birth spacing | ||||||
|
| ||||||
| >2 years(ref) | ||||||
|
| ||||||
| <2 years | 1.001 | 0.997 | ||||
|
| ||||||
| Birth Order | ||||||
|
| ||||||
| > 4th child | ||||||
|
| ||||||
| First child | 1.451 | 1.011-2.083 | 0.043* | 0.972 | 0.954 | |
|
| ||||||
| 2nd or 3rd child | 0.998 | 0.712-1.399 | 0.990 | 1.064 | 0.885 | |
|
| ||||||
| Child Characteristics | ||||||
|
| ||||||
| Sex of the child | ||||||
|
| ||||||
| Female (ref) | ||||||
|
| ||||||
| Male | 0.968 | 0.823 | ||||
|
| ||||||
| Birth weight | ||||||
|
| ||||||
| >NBW (ref) | ||||||
|
| ||||||
| Not weighed | 2.497 | 1.425-4.375 | 0.001* | 2.662 | 1.004-7.058 | 0.049* |
|
| ||||||
| LBW | 3.582 | 1.467-8.748 | 0.005* | 3.206 | 1.849-12.08 | 0.006* |
|
| ||||||
| NBW | 1.725 | 0.113 | 2.228 | 0.082-6.037 | 0.115 | |
|
| ||||||
| Health facility characteristics | ||||||
|
| ||||||
| Place. of delivery | ||||||
|
| ||||||
| Home (ref) | ||||||
|
| ||||||
| Facility | 0.761 | 0.761-1.028 | 0.075 | |||
|
| ||||||
| ANC visits | ||||||
|
| ||||||
| >4ANCvisits (ref) | ||||||
|
| ||||||
| No ANC visits | 4.054 | 1.728-9.511 | 0.001* | 3.384 | 1.616-8.53 | 0.041* |
|
| ||||||
| 1-3ANC visits | 1.704 | 1.102-2.634 | 0.017* | 2.316 | 1.101-4.875 | 0.027* |
cOR= Crude Odds ratio, aOR= p=Level of significance
In the second stage logistic regression model, only the variables that were significant at the first analysis were entered in the final model. After adjusting for confounding factors, the mother’s education, birth weight and the number of ANC visits were established to be significant determinants of neonatal mortality. Mothers with no education were 2.2 times more likely to lose their infants in the neonatal period compared to those with higher education levels Adjusted Odds Ratio (aOR=2.20, 95% CI: 1.43-4.15, p=0.049). Low birth weight infants were 3.2 times more likely to die in the neonatal period (aOR=3.21, 95% CI: 1.85-12.08, p=0.006) compared to those with >3.5 kgs at birth. Mothers who attended >4 ANC had a lower risk of experiencing neonatal mortality. Those who only attended between 1-3 ANC visits were three times more likely to lose their infants (aOR=3.35, 95% CI:1.62-8.53, p=0,041 in the first 28 days, compared to those with >4 ANC visits. Similarly, mothers who did not attend any ANC visits were twice as likely to experience neonatal deaths (aOR=2.32, 95% CI: 1.10-4.88, p=0.027) compared to mothers who attended >4 ANC visits.
4. Discussion
The overall aim of the study was to establish and identify the risk factors associated with neonatal mortality in Kenya using the nationally representative KDHS data. After adjusting for confounding factors, 3 factors were significantly associated with neonatal mortality and they have been discussed below.
Maternal education was significantly associated with neonatal mortality. Mothers with no formal education and those with primary level education had a higher likelihood of experiencing neonatal deaths compared to mothers with tertiary levels of education. These findings are consistent with previous literature which has demonstrated that higher levels of education are associated with better chances of neonatal survival.18,19,20 The benefits of mothers’ education have been shown to influence mothers’ reproductive health choices and fertility preferences such as uptake of contraception, better health-seeking behaviors, better nutrition knowledge and practices that increase the likelihood of neonatal survival.21
This study also established that LBW infants have a higher likelihood of dying in the first 28 days of life. These findings are consistent with studies conducted in other parts of the world especially in Brazil and Ethiopia.22,23,24,25 The increased likelihood of mortality in LBW infants may be linked to neonatal illness and lack of specialized care for the infants. In addition, increased risk of death is associated with low Apgar scores and congenital abnormalities that increase the risk of mortality.26 Our study findings showed a significant relationship between the number of ANC visits and neonatal deaths. These findings are consistent with similar cross-sectional studies conducted in India, Nigeria and Uganda, which showed that women who did not take up maternal care during pregnancy had a higher odds of experiencing neonatal deaths. The benefits of early commencement of prenatal care are the detection of possible health concerns which are likely to result in complications for both the mother and the child. In addition, women who are consistent with their ANC appointments and received the requisite minimum of 4 ANC visits, were more likely to be healthy and more compliant to health recommendations as demonstrated by studies in India, Bangladesh and Ethiopia.27,28,29,30
4.1. Limitations
The strength and weaknesses of this study need to be considered when drawing conclusions and inferences. This study is a nationally representative survey with a 2-stage stratified sampling that presents generally representative data and findings. Limitations of this study should also be considered when drawing conclusions and interpretations of the results. KDHS collects data up to 5 years before the survey and recalls errors are a possibility especially on information related to neonatal mortality. Some variables such as birth weight had missing data and as such should be interpreted with caution. Information on the pregnancy-related complications and other underlying comorbidities that may influence pregnancy outcomes such as pre-existing health conditions before delivery was not available.
4.2. Recommendation for Further Studies
The findings from this study indicate the need to continuously educate the communities on the importance of girls’ education. Whereas the Kenyan government is implementing free primary education, cultural inclinations, and practices such as female genital cutting predispose girls to early marriages, thus pushing them out of school.
The government of Kenya, through the community health strategy, should facilitate continuous sensitizations and referral mechanisms on the uptake and follow-up of prenatal care to at least meet the recommended threshold of a minimum of 4 visits.
5. Conclusion and Global Health Implications
This study intended to establish the determinants of neonatal mortality in Kenya in 2014. The findings from the analysis showed that mothers’ level of education, birth weight and the number of ANC visits were significantly related to neonatal deaths. The findings of the study contribute to the body of knowledge toward the reduction of neonatal mortality and overall childhood mortality in the country and even globally.
Key Messages.
► Health service determinants such as the num-ber of ANC visits a mother attended during pregnancy, maternal level of education and neonatal weight at birth have an influence on the neonatal outcomes.
► When mothers attend 4+ ANC visits during the prenatal period, their neonates have a higher chance of survival attributable to care received at the health facilities.
► Neonates born of uneducated mothers have an elevated risk of dying in the neonatal period 2.2 times higher than mothers who have pri-mary, secondary and higher education levels.
► Low birth weight neonates were 3 times more likely to die compared to normal birth weight neonates.
► Multi-sectoral policy action that ensures com-munity sensitization to increase uptake of an-tenatal care, promotion of basic education and improved health and nutrition is crucial in the realization of reduction in neonatal deaths.
Acknowledgments:
The authors acknowledge ICF International and the DHS program for allowing and authorizing download and use of the data for this analysis.
Compliance with Ethical Standards
Conflicts of Interest: None.
Financial Disclosure: None.
Funding/Support: None.
Ethics Approval: This study received ethical approval from Egerton University, Njoro, Kenya. Approval to utilize data for further analysis was obtained from the DHS program, ICF International.
Disclaimer: None
References
- 1.United Nations Children's Fund. The State of the World's Children 2008. Child Survival. UNICEF. [Accessed February 2021]. http: //www.unicef.org/sowc08/docs/sowc08.pdf.2008 .
- 2.United Nations Children's Fund. Levels and Trends in Child Mortality Report 2017. UNICEF. [Accessed February 2021]. https: //www.unicef.org/reports/levels-and-trends-child-mortality-report-2017.pdf .
- 3.Republic of Kenya, Kenya National Bureau of Statistics, Kenya Demographic Health Survey. Ministry of Health Kenya and ICF international. 2015 [Google Scholar]
- 4.Republic of Kenya, Kenya National Bureau of Statistics, Kenya Demographic Health Survey. Ministry of Health Kenya and ICF international. 2003 [Google Scholar]
- 5.Republic of Kenya, Kenya National Bureau of Statistics, Kenya Demographic Health Survey. Ministry of Health Kenya and ICF international. 2010 [Google Scholar]
- 6.Republic of Kenya, Ministry of Health. Kenya Health Policy Framework 1994-2010. Ministry of Health. 1994 [Google Scholar]
- 7.Jehan I, Harris H, Salat S, Zeb A, et al. Neonatal mortality, risk factors and causes:a prospective population-based cohort study in urban Pakistan. Bull World Health Organ. 2009;87:130–138. doi: 10.2471/BLT.08.050963. doi:10.2471/blt.08.050963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khatun F, Rasheed S, Moran C, et al. Causes of neonatal and maternal deaths in Dhaka slums:Implications of service delivery. BMC Public Health. 2012;12:84. doi: 10.1186/1471-2458-12-84. doi:10.1186/1471-2458-12-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. World Health Statistics 2011. WHO. [Accessed February 2021]. https: //www.who.int .
- 10.Paudel D, Thapa A, Shedain P, Paudel B. Trends and determinants of neonatal mortality in Nepal:further analysis of the Nepal demographic health survey, 2001-2011. DHS Further Analysis Reports No.75. Nepal Ministry of Health and Population, New Era, and ICF International. 2013 [Google Scholar]
- 11.Houweling P, Klaveren D, Das S, et al. A prediction model for neonatal mortality in low- and middle-income countries:An analysis of data from population surveillance sites in India, Nepal, and Bangladesh. Int J Epidemiol. 2019;48(1):186–198. doi: 10.1093/ije/dyy194. doi:10.1093/ije/dyy194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gortmaker SL. Poverty and infant mortality in the United States. Am Sociol Rev. 1979;44:280–297. [PubMed] [Google Scholar]
- 13.Sharma RK. Causal pathways to infant mortality;linking social variables to infant mortality through intermediate variables. J Health Soc Policy. 1998;9(3):15–28. [PubMed] [Google Scholar]
- 14.Mosley WH, Chen LC. An analytical framework for study of child survival in developing countries. Population and Development Review. 1984;10:25–45. [PMC free article] [PubMed] [Google Scholar]
- 15.Ettarh RR, Kimani J. Determinants of under-five mortality in rural and urban Kenya. The International Electronic x. 2012;1445 [PubMed] [Google Scholar]
- 16.IBM Corp. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp; Released 2011. [Google Scholar]
- 17.Rutstein O, Rojas G. Guide to DHS Statistics. Rockville, Maryland, USA: ICF; 2006. [Google Scholar]
- 18.Kiross GT, Chojenta C, Barker D, Tiyurie TY, Loxton D. The effect of maternal education on infant mortality in Ethiopia:A systematic review and meta-analysis. PLoS One. 2019;14(7):e0220079. doi: 10.1371/journal.pone.0220076. doi:10.1371/journal.pone.0220076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kamal M. Maternal education as a determinant of neonatal mortality in Bangladesh. Journal of Health Management. 2012;14(3):269–281. [Google Scholar]
- 20.Fonceca SC, Flores PV, Camargo KR, Pinheiro RS, Coeli C M. Maternal education, and age:Inequities in neonatal death. Revista de Saude Publica. 2017;51(94) doi: 10.11606/S1518-8787.2017051007013. doi:10.11606/S1518-8787.2017051007013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ansem W, Schrijvers C, Rodenburg G, Van de Mheem D. Maternal education level and children's healthy eating behaviour:Role of home environment. Int J Behav Nutr Phys Act. 2014;11:113. doi: 10.1186/s12966-014-0113-0. doi:10.1186/s12966-014-0113-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Horbar J, Carpenter J, Badget G, et al. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Paediatrics. 2012;129(6):1019–1026. doi: 10.1542/peds.2011-3028. doi:10.1542/peds.2011-3028. [DOI] [PubMed] [Google Scholar]
- 23.Da Silva Lopes K, Ota E, Shakaya P, et al. Effects of nutrition interventions during pregnancy on low birth weight:an overview of systematic reviews. BMJ Glob Health. 2017;2:e000389. doi: 10.1136/bmjgh-2017-000389. doi:10.1136/bmjgh-2017-000389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nepuane D, Dawson P, Houston R, et al. Lower mortality is observed among low-birth weight young infants who have received home based care by female community health volunteer in rural Nepal. BMC Pregnancy Childbirth. 2017;17(1):218. doi: 10.1186/s12884-017-1355-z. doi:10.1186/s12884-017-1355-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Suparmi S, Chiera B, Pradono J. Low birth weights and the risk of neonatal mortality. Health Science Journal of Indonesia. 2016;7(2):113–117. [Google Scholar]
- 26.Getachew B, Etefa T, Asefa A, Terefe B, Dereje D. Determinants of low fifth minute agpar score among newborns delivered in Jimma University Medical Center, Southwest Ethiopia. Int J Pediatr. 2020;2020:9896127. doi: 10.1155/2020/9896127. doi:10.1155/2020/9896127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tekelab T, Chojenta C, Smith R, Loxton D. The impact of antenatal care on mortality in sub–Saharan Africa:a systematic review and meta-analysis. PloS One. 2019;14(9):e0222566. doi: 10.1371/journal.pone.0222566. doi:10.1371/journal.pone.0222566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arunda M, Emmelin A, Asamoah BO. Effectiveness of Antenatal care services in reducing neonatal mortality in Kenya:An analysis of national survey data. Glob Health Action. 2017;10(1):1328796. doi: 10.1080/16549716.2017.1328796. doi:10.1080/16549716.2017.1328796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ajaari J, Masanja H, Weiner R, Abokyi SA, Owusu-Agyei S. Impact of place of delivery on neonatal mortality in rural Tanzania. Int J MCH AIDS. 2012;1(1):49–59. doi: 10.21106/ijma.10. doi:10.21106/ ijma.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kitui J, Lewis S, Davey G. Factors influencing place of delivery for women in Kenya:an analysis of the Kenya demographic health survey 2008/2009. BMC Pregnancy Childbirth. 2013;13:40. doi: 10.1186/1471-2393-13-40. doi:10.1186/1471-2393-13-40. [DOI] [PMC free article] [PubMed] [Google Scholar]


